Abstract
The human hepatoma cell lines HepG2 and Huh7 have been used extensively to study hepatitis B virus (HBV) transcription and replication. Both cell lines support transcription of the 3.5-kb viral pregenomic RNA and subsequent viral DNA synthesis by reverse transcription. The effects of the coactivator peroxisome proliferator-activated receptor γ coactivator 1α (PGC1α) and corepressor small heterodimer partner (SHP) on HBV transcription and replication mediated by nuclear receptors were examined in the context of individual nuclear receptors in nonhepatoma cells and in hepatoma cells in an attempt to determine the relative contribution of the various nuclear receptors to viral biosynthesis in the hepatoma cells. PGC1α and SHP modulated viral biosynthesis differently in the human hepatoma cell lines HepG2 and Huh7, indicating distinct modes of transcriptional regulation. Consistent with this suggestion, it appears that retinoid X receptor α/farnesoid X receptor α and liver receptor homolog 1 or estrogen-related receptor β (ERRβ) may contribute to the majority of the viral replication observed in HepG2 cells, whereas ERRα and ERRγ are probably responsible for the majority of viral biosynthesis in Huh7 cells. Therefore, this approach indicates that the transcriptional regulation of HBV biosynthesis in HepG2 and Huh7 cells is primarily controlled by different transcription factors.
Hepatitis B virus (HBV) replicates efficiently in hepatocytes in vivo and in hepatoma cells in culture because these cells have the appropriate composition of transcription factors to support the expression of the 3.5-kb viral pregenomic transcript, which is reverse transcribed to generate the relaxed circular genomic DNA present in infectious viral particles (4, 11, 26, 27, 29). In contrast, HBV transcription and replication does not occur in the majority of nonhepatic tissues in vivo or nonhepatoma cell lines in culture due to the absence of transcription of the 3.5-kb viral pregenomic RNA (11, 27). However, complementation of nonhepatoma cells with several nuclear receptors but not other liver-enriched transcription factors leads to robust HBV transcription and replication (see Fig. 1 to 3) (18a, 27). These observations have led to the suggestion that transcriptional regulation of HBV biosynthesis is an important determinant of viral tropism, which may be just as significant as the presumptive cell type-specific expression of the viral receptor (22, 27).
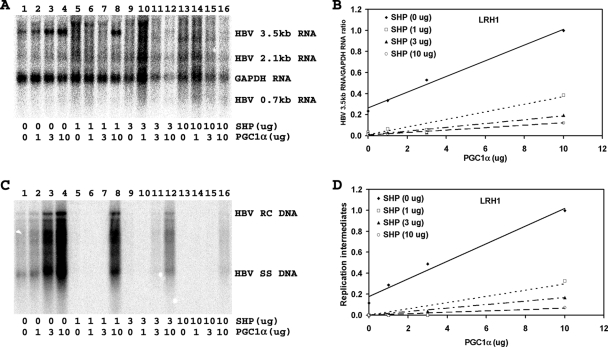
FIG. 1.
Effect of PGC1α and SHP expression on HBV biosynthesis in the human hepatoma cell line HepG2. Cells were transfected with the HBV DNA (4.1-kbp) construct alone (lane 1) or the HBV DNA (4.1-kbp) construct plus the PGC1α and SHP expression vectors (lanes 2 to 16), as indicated. (A) RNA (Northern) filter hybridization analysis of HBV transcripts. The glyceraldehyde-3-phosphate dehydrogenase (GAPDH) transcript was used as an internal control for RNA loading per lane. (B) Quantitative analysis of the 3.5-kb HBV RNA results from three independent experiments. Trend lines were calculated using linear regression analysis. (C) DNA (Southern) filter hybridization analysis of HBV replication intermediates. HBV RC DNA, HBV relaxed circular DNA; HBV SS DNA, HBV single-stranded DNA. (D) Quantitative analysis of the HBV replication intermediate results from three independent experiments. Trend lines were calculated using linear regression analysis.
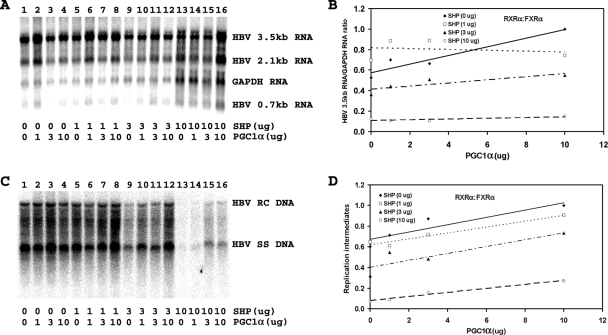
FIG. 3.
Effect of PGC1α and SHP expression on HBV biosynthesis in the human embryonic kidney cell line 293T expressing LRH1. Cells were transfected with the HBV DNA (4.1-kbp) construct plus the LRH1 expression vector (lane 1) or the HBV DNA (4.1-kbp) construct plus the LRH1, PGC1α, and SHP expression vectors (lanes 2 to 16), as indicated. (A) RNA (Northern) filter hybridization analysis of HBV transcripts. The glyceraldehyde-3-phosphate dehydrogenase (GAPDH) transcript was used as an internal control for RNA loading per lane. (B) Quantitative analysis of the 3.5-kb HBV RNA results from three independent experiments. Trend lines were calculated using linear regression analysis. (C) DNA (Southern) filter hybridization analysis of HBV replication intermediates. HBV RC DNA, HBV relaxed circular DNA; HBV SS DNA, HBV single-stranded DNA. (D) Quantitative analysis of the HBV replication intermediate results from three independent experiments. Trend lines were calculated using linear regression analysis.
The molecular characterization of the various steps in the viral life cycle has been largely elucidated, utilizing human hepatoma cell lines (10, 24). In particular, the human hepatoma cell lines HepG2 and Huh7 have been utilized because they can support viral replication when transfected with genomic HBV DNA (4, 26). In addition, these two cell lines lack integrated HBV DNA which is commonly associated with other human hepatoma cell lines (4, 26, 28). As products from integrated HBV sequences might have unidentified effects on viral transcription and replication, the majority of studies aimed at understanding the various aspects of HBV transcription and replication have utilized HepG2 and Huh7 cells. The majority of observations using these two cell lines have been similar with regard to HBV biosynthesis, leading to the general assumption that they are essentially equivalent with respect to HBV biosynthesis (4, 24, 26). However, it is clear that these hepatoma cell lines are morphologically distinct and, consequently, probably display distinct patterns of gene regulation.
Recent studies have indicated that 3.5-kb pregenomic HBV RNA expression and viral replication are regulated by a variety of nuclear receptors (see Fig. 1 to 3) (18a, 27). The observation that several nuclear receptors can potentially contribute to the level of viral biosynthesis raised the critical question of their relative importance both in vivo and in cell culture. In an attempt to address this issue, the effect of expressing the coactivator peroxisome proliferator-activated receptor γ coactivator 1α (PGC1α) and the corepressor small heterodimer partner (SHP) on HBV transcription and replication in both human hepatoma and nonhepatoma cells was quantitatively evaluated with a view to establishing the potential role of distinct nuclear receptors in regulating viral biosynthesis in the HepG2 and Huh7 cells. This analysis demonstrated that each nuclear receptor displayed a unique pattern of responsiveness to PGC1α and SHP in nonhepatoma cells. In addition, it was apparent that the effects of PGC1α and SHP expression on viral biosynthesis in the two hepatoma cell lines were unique and distinct from each other. Theoretical analysis of the nuclear receptors governing HBV transcription and replication in the human hepatoma cells suggested that retinoid X receptor α (RXRα)/farnesoid X receptor α (FXRα) and liver receptor homolog 1 (LRH1) or estrogen-related receptor β (ERRβ) were responsible for the majority of viral replication in HepG2 cells. This contrasts with viral replication in Huh7 cells, where ERRα and ERRγ are responsible for the majority of viral biosynthesis (18a). Therefore, it appears that the nuclear receptors controlling HBV biosynthesis in HepG2 and Huh7 cells are quite different and leaves unanswered which one, if any, of these cell lines reflects the state of differentiation in the hepatocytes of the liver during natural infection.
MATERIALS AND METHODS
Plasmid constructions.
The steps in the cloning of the plasmid constructs used in the transfection experiments were performed by standard techniques (23). HBV DNA sequences in these constructions were derived from the plasmid pCP10, which contains two copies of the HBV genome (subtype ayw) cloned into the EcoRI site of pBR322 (8). The HBV DNA (4.1-kbp) construct that contains 1.3 copies of the HBV genome includes the viral sequence from nucleotide coordinates 1072 to 3182 plus coordinates 1 to 1990 (27). This plasmid was constructed by cloning the NsiI/BglII HBV DNA fragment (nucleotide coordinates 1072 to 1990) into pUC13, generating pHBV(1072-1990). Subsequently, a complete copy of the 3.2-kbp viral genome linearized at the NcoI site (nucleotide coordinates 1375 to 3182 plus coordinates 1 to 1374) was cloned into the unique NcoI site (HBV nucleotide coordinate 1374) of pHBV(1072-1990), generating the HBV DNA (4.1-kbp) construct.
The pRS-hRXRα, pCMV-rFXRα, pCMX-mLRH1, pcDNA3-HA-hPGC1α, and pCMXSHP vectors express RXRα, FXRα, LRH1, PGC1α, and SHP polypeptides from the human RXRα, rat FXRα, mouse LRH1, human PGC1α, and mouse SHP cDNAs, respectively, using the Rous sarcoma virus long terminal repeat (pRS) or the cytomegalovirus immediate-early promoter (pCMV, pCMX, and pcDNA3) (12, 15, 16).
Cells and transfections.
The human hepatoma HepG2 cell line and human embryonic kidney 293T cell line were grown in RPMI 1640 medium and 10% fetal bovine serum at 37°C in 5% CO2/air. Transfections for viral RNA and DNA analysis were performed as previously described (17), using 10-cm plates containing approximately 1 × 106 cells. DNA and RNA isolation was performed 3 days posttransfection. In 293T cells, the transfected DNA mixture was composed of 5 μg of HBV DNA (4.1 kbp) plus 1.5 μg of the nuclear receptor expression vectors pRS-hRXRα, pCMV-rFXRα, and pCMX-mLRH1 and various amounts of the pcDNA3-HA-hPGC1α and pCMXSHP expression vectors (2, 5, 12, 15, 16, 18). In HepG2 cells, 1.5 μg of the nuclear receptor expression vector was omitted. Controls were derived from cells transfected with HBV DNA and the expression vectors lacking a nuclear receptor cDNA insert (20). All-trans-retinoic acid and chenodeoxycholic acid at 1 μM and 100 μM, respectively, were used to activate the nuclear receptors RXRα and FXRα (27).
Characterization of HBV transcripts and viral replication intermediates.
Transfected cells from a single plate were divided equally and used for the preparation of total cellular RNA and viral DNA replication intermediates as described previously (25), with minor modifications. For RNA isolation (6), the cells were lysed in 1.8 ml of 25 mM sodium citrate at pH 7.0, 4 M guanidinium isothiocyanate, 0.5% (vol/vol) sarcosyl, and 0.1 M 2-mercaptoethanol. After addition of 0.18 ml of 2 M sodium acetate at pH 4.0, the lysate was extracted with 1.8 ml of water-saturated phenol plus 0.36 ml of chloroform-isoamyl alcohol (dilution of 49:1). After centrifugation for 30 min at 3,000 rpm in a Sorvall RT6000, the aqueous layer was precipitated with 1.8 ml of isopropanol. The precipitate was resuspended in 0.3 ml of 25 mM sodium citrate at pH 7.0, 4 M guanidinium isothiocyanate, 0.5% (vol/vol) sarcosyl, and 0.1 M 2-mercaptoethanol and precipitated with 0.6 ml of ethanol. After centrifugation for 20 min at 14,000 rpm in an Eppendorf 5417C microcentrifuge, the precipitate was resuspended in 0.3 ml of 10 mM Tris hydrochloride at pH 8.0, 5 mM EDTA, and 0.1% (wt/vol) sodium lauryl sulfate and precipitated with 45 μl of 2 M sodium acetate plus 0.7 ml of ethanol.
For the isolation of viral DNA replication intermediates, the cells were lysed in 0.4 ml of 100 mM Tris hydrochloride at pH 8.0 and 0.2% (vol/vol) NP-40. The lysate was centrifuged for 1 min at 14,000 rpm in an Eppendorf 5417C microcentrifuge to pellet the nuclei. The supernatant was adjusted to 6.75 mM magnesium acetate plus 200 μg/ml DNase I and incubated for 1 h at 37°C to remove the transfected plasmid DNA. The supernatant was readjusted to 100 mM NaCl, 10 mM EDTA, 0.8% (wt/vol) sodium lauryl sulfate, and 1.6 mg/ml pronase and incubated for an additional 1 h at 37°C. The supernatant was extracted twice with phenol, precipitated with 2 volumes of ethanol, and resuspended in 100 μl of 10 mM Tris hydrochloride at pH 8.0 and 1 mM EDTA. RNA (Northern) and DNA (Southern) filter hybridization analyses were performed using 10 μg of total cellular RNA and 30 μl of viral DNA replication intermediates, respectively, as described previously (23).
Statistical analysis.
Trend lines were calculated using linear regression analysis using the method of least squares (Microsoft Excel chart of a linear regression trend line). Correlation coefficients were optimized using an iterative process that identified the maximum possible r value for each combination of nuclear receptors at all expression levels of PGC1α and SHP (Microsoft Excel CORREL). Initially, theoretical levels of replication intermediates predicted for all pair-wise combinations of nuclear receptors were compared with the observed level of replication in HepG2 cells and were optimized at a 1% level of resolution for each pair of nuclear receptors. The optimal percentages for any two nuclear receptors yielding r values of greater than 0.95 were reported. Similarly, the levels of replication for all three-way combinations of nuclear receptors were compared with the observed level of replication in HepG2 cells and were optimized at a 1% level of resolution for each of the three nuclear receptors. The optimal percentages for any three nuclear receptors yielding r values greater than the maximum r value for any pair of these nuclear receptors were reported. This process was repeated with the inclusion of additional nuclear receptors until no further increase in r value was observed.
RESULTS
PGC1α and SHP modulate HBV biosynthesis in human hepatoma HepG2 cells.
Transfection of the HBV DNA (4.1-kbp) construct into HepG2 cells supports HBV transcription and replication (Fig. 1A and C, lane 1). Expression of increasing levels of PGC1α activates, whereas that of SHP inhibits, 3.5-kb HBV RNA synthesis and viral replication in a dose-dependent manner (Fig. 1). The effects of PGC1α and SHP on HBV DNA and RNA synthesis were quantitatively similar, indicating that the effects of PGC1α and SHP on transcription were reflected in the levels of observed viral replication (Fig. 1). Increasing the levels of PGC1α enhanced viral biosynthesis at the lower levels of SHP expression but was relatively ineffective at increasing HBV replication in the presence of higher levels of SHP expression (Fig. 1D). This suggests that the effect of these coregulators on viral replication in HepG2 cells is quite sensitive to their relative levels of expression (Fig. 1D). However, the observation that PGC1α and SHP modulated HBV biosynthesis in HepG2 cells is consistent with the suggestion that nuclear receptors control viral transcription in these hepatoma cells.
PGC1α and SHP modulate RXRα/FXRα-dependent HBV biosynthesis in human embryonic kidney 293T cells.
Transfection of the HBV DNA (4.1-kbp) construct with the RXRα and FXRα expression vectors into 293T cells supports HBV transcription and replication (Fig. 2A and C, lane 1). Expression of increasing levels of PGC1α activates, whereas that of SHP inhibits, 3.5-kb HBV RNA synthesis and viral replication in a dose-dependent manner (Fig. 3). Increasing the levels of PGC1α enhanced viral biosynthesis at all levels of SHP expression in a similar manner (Fig. 3D). However, SHP inhibition was relatively ineffective at the lower levels examined and was readily apparent only at the highest level of SHP expression (Fig. 3D), suggesting that RXRα/FXRα-mediated viral replication in 293T cells is relatively insensitive to SHP-mediated inhibition. These observations indicate that the effects of PGC1α and SHP on HBV biosynthesis in HepG2 cells (Fig. 1) are quantitatively different from those seen in 293T cells expressing RXRα/FXRα (Fig. 2). Therefore, it appears unlikely that RXRα/FXRα alone controls HBV biosynthesis in HepG2 cells.
FIG. 2.
Effect of PGC1α and SHP expression on HBV biosynthesis in the human embryonic kidney cell line 293T expressing RXRα/FXRα. Cells were transfected with the HBV DNA (4.1-kbp) construct plus the RXRα and FXRα expression vectors (lane 1) or the HBV DNA (4.1-kbp) construct plus the RXRα, FXRα, PGC1α, and SHP expression vectors (lanes 2 to 16), as indicated. (A) RNA (Northern) filter hybridization analysis of HBV transcripts. The glyceraldehyde-3-phosphate dehydrogenase (GAPDH) transcript was used as an internal control for RNA loading per lane. (B) Quantitative analysis of the 3.5-kb HBV RNA results from three independent experiments. Trend lines were calculated using linear regression analysis. (C) DNA (Southern) filter hybridization analysis of HBV replication intermediates. HBV RC DNA, HBV relaxed circular DNA; HBV SS DNA, HBV single-stranded DNA. (D) Quantitative analysis of the HBV replication intermediate results from three independent experiments. Trend lines were calculated using linear regression analysis. All-trans-retinoic acid and chenodeoxycholic acid at 1 μM and 100 μM, respectively, were used to activate the nuclear receptors RXRα and FXRα.
PGC1α and SHP modulate LRH1-dependent HBV biosynthesis in human embryonic kidney 293T cells.
Transfection of the HBV DNA (4.1-kbp) construct with the LRH1 expression vector into 293T cells supports limited HBV transcription and replication (Fig. 3A and C, lane 1). Expression of increasing levels of PGC1α activates, whereas that of SHP inhibits, 3.5-kb HBV RNA synthesis and viral replication in a dose-dependent manner (Fig. 3). The effects of PGC1α and SHP on LRH1-mediated HBV DNA and RNA synthesis in 293T cells were quantitatively similar, indicating that the effects of PGC1α and SHP on transcription were reflected in the levels of observed viral replication (Fig. 3). Increasing the levels of PGC1α enhanced viral biosynthesis at all levels of SHP expression (Fig. 3D). Additionally, LRH1-dependent viral biosynthesis was highly sensitive to SHP inhibition at all levels of PGC1α expression (Fig. 3D). These observations indicate that the effects of PGC1α and SHP on HBV biosynthesis in HepG2 cells (Fig. 1) are quantitatively different from those seen in 293T cells expressing LRH1 (Fig. 3). Therefore, it appears unlikely that LRH1 alone controls HBV biosynthesis in HepG2 cells.
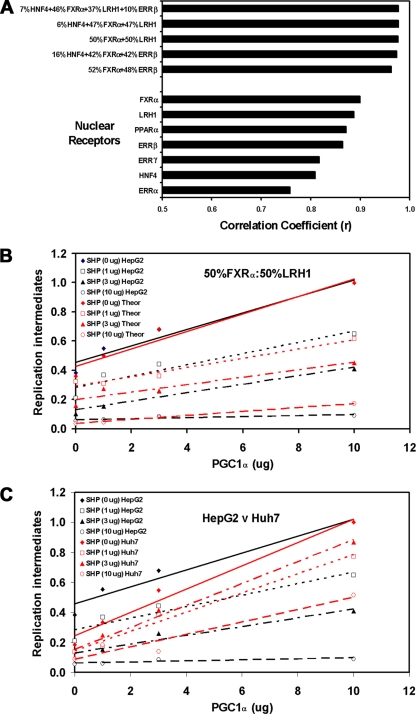
Relative importance of individual nuclear receptors to HBV biosynthesis in the human hepatoma HepG2 cells.
Qualitative comparison of the effects of PGC1α and SHP on HBV biosynthesis in the human hepatoma HepG2 cells and the human embryonic kidney 293T cells in the presence of nuclear receptors indicated that neither RXRα/FXRα nor LRH1 alone might be controlling the majority of viral RNA and DNA synthesis in the HepG2 cells (Fig. 1 to 3). However, in an attempt to more precisely define the relative contributions of the various nuclear receptors to viral biosynthesis in HepG2 cells, the effects of PGC1α and SHP on viral replication in HepG2 cells were compared quantitatively to their effects on viral biosynthesis in 293T cells expressing individual nuclear receptors (Fig. 4A). Direct comparison of the individual replication profiles (Fig. 1 to 3) (18a) indicated that the effects of PGC1α and SHP on viral replication in HepG2 cells were most similar to those observed in 293T cells expressing RXRα/FXRα (Correlation coefficient r = 0.90) and could be ordered as follows: RXRα/FXRα (r = 0.90), LRH1 (r = 0.89), RXRα/PPARα (r = 0.87), ERRβ (r = 0.86), ERRγ (r = 0.82), hepatocyte nuclear factor 4α (HNF4α) (r = 0.81), and ERRα (r = 0.76). This analysis suggests that none of the responses of the single nuclear receptors to PGC1α and SHP expression represents precisely the regulation observed in HepG2 cells (Fig. 1 to 4). Therefore, it is very probable that more than one nuclear receptor is contributing to viral biosynthesis in HepG2 cells. Consequently, optimal theoretical combinations of transcription factors were identified, and the similarities of their replication profiles were compared with the effects of PGC1α and SHP on viral replication in HepG2 cells (Fig. 4). Only two pair-wise combinations displayed correlation coefficients with r values ranging from 0.96 to 0.98. In each case, RXRα/FXRα contributed to approximately half the total viral replication observed, and the other half of the viral replication was controlled by either LRH1 or ERRβ (Fig. 4A). The additional nuclear receptors HNF4α, RXRα/PPARα, ERRα, and ERRγ appear to contribute to viral replication to a very limited extent only based on this analysis, even when combinations of three or more factors were evaluated (Fig. 4A). Therefore, it appears that HBV transcription and replication in HepG2 cells are governed primarily by RXRα/FXRα and LRH1 or ERRβ, with potentially a minor contribution also coming from HNF4α (Fig. 4A). The other nuclear receptors examined appear not to contribute greatly to viral biosynthesis in HepG2 cells (Fig. 4). This conclusion is consistent with previous findings that suggested that an SHP-sensitive and an SHP-insensitive nuclear receptor, presumably corresponding to LRH1 (or ERRβ) and RXRα/FXRα, respectively, contribute approximately equally to HBV biosynthesis in HepG2 cells (19).
FIG. 4.
Theoretical evaluation of the nuclear receptor combinations governing HBV biosynthesis in HepG2 cells. (A) Correlation coefficient values were determined for optimal combinations of nuclear receptors based on their effects on viral replication in 293T cells compared with that in HepG2 cells in the presence of the different levels of the PGC1α and SHP coregulators. The combinations of nuclear receptors are reported in a descending order, with respect to their correlation coefficient values. Data used to determine the correlation coefficient values for HNF4α, RXRα/PPARα, ERRα, ERRβ, and ERRγ are included in the companion study (18a). 7% HNF4α plus 46% RXRα/FXRα plus 37% LRH1 plus 10% ERRβ, r = 0.977; 8% HNF4α plus 47% RXRα/FXRα plus 47% LRH1, r = 0.977; 50% RXRα/FXRα plus 50% LRH1, r = 0.976; 16% HNF4α plus 42% RXRα/FXRα plus 42% ERRβ, r = 0.974; 52% RXRα/FXRα plus 48% ERRβ, r = 0.963; 100% RXRα/FXRα, r = 0.900; 100% LRH1, r = 0.888; 100% RXRα/PPARα, r = 0.872; 100% ERRβ, r = 0.865; 100% ERRγ, r = 0.817; 100% HNF4α, r = 0.809; 100% ERRα, r = 0.758. (B) Example of the theoretical optimal best fit of the levels of viral replication obtained with RXRα/FXRα plus LRH1 in 293T compared with that in HepG2 cells in the presence of the different levels of the PGC1α and SHP coregulators. Trend lines were calculated using linear regression analysis. (C) Comparison of the levels of viral replication observed in HepG2 cells compared with those observed in Huh7 cells in the presence of the different levels of the PGC1α and SHP coregulators. Trend lines were calculated using linear regression analysis.
DISCUSSION
HBV is hepatotropic, and its biosynthesis is regulated at the transcriptional level by several nuclear receptors (Fig. 1 to 3) (18a, 27). Nuclear receptors have a critical role in the liver in controlling whole-body energy homeostasis (9, 14). Therefore, these transcription factors represent potential targets for modulating metabolic process associated with significant human disease such as the metabolic syndrome (9). In addition, as HBV appears to have co-opted this regulatory system to control its own biosynthesis, nuclear receptors might also serve as important targets for the antiviral therapies that are essential if chronic hepatitis associated with this viral infection is to be efficiently controlled (7). The central questions that emerge from these observations are as follows. First, which nuclear receptors primarily control HBV transcription and replication under various physiological conditions, and second, can these nuclear receptors be regulated such that viral replication is inhibited but normal liver physiological function is not compromised to an unacceptable extent? Before these questions can be addressed, it is essential that the nuclear receptors governing HBV biosynthesis in vivo during natural infection be identified.
As an initial step toward identifying the nuclear receptors controlling HBV biosynthesis in vivo during natural infection, the hepatoma cell lines which can support viral biosynthesis from transfected DNA were evaluated for their ability to support HBV transcription and replication in the presence of the coactivator PGC1α and the corepressor SHP. These coregulators are important modulators of nuclear receptor activity in hepatocytes and mediate the effects of various physiological stimuli on energy homeostasis through their interaction with nuclear receptors (1, 14). Consequently, it was also of interest to determine if these coregulators could modulate nuclear receptor-mediated viral biosynthesis in nonhepatoma cells. This analysis demonstrated that each nuclear receptor was uniquely responsive to the various levels of PGC1α and SHP expression (Fig. 2 and 3) (18a).
The unique effects of PGC1α and SHP expression on nuclear receptor-mediated viral biosynthesis suggested that their effects on HBV transcription and replication in hepatoma cells could be exploited to evaluate the relative importance of these transcription factors to viral biosynthesis in HepG2 and Huh7 cells. A direct comparison of the effect of PGC1α and SHP expression on viral biosynthesis in these hepatoma cells clearly demonstrates that HBV transcription and replication in these cells is affected in a distinctly different manner (Fig. 4C). This implies that the nuclear receptors in these cells that govern viral biosynthesis must be distinct.
A comparison of the modulation of HBV biosynthesis by PGC1α and SHP in HepG2 cells and nonhepatoma cells expressing individual nuclear receptors allows for a theoretical determination of the transcription factors directing HBV RNA synthesis and replication (Fig. 4). This analysis suggests that RXRα/FXRα is responsible for approximately half of the observed viral biosynthesis in HepG2 cells (Fig. 4). The remainder of the HBV biosynthesis appears to be controlled by either LRH1 or ERRβ (Fig. 4). Whereas RXRα, FXRα, and LRH1 are highly expressed in the liver, ERRβ is not (3), suggesting that it is unlikely that this nuclear receptor has an important role in HBV biosynthesis during a natural infection in vivo.
Consistent with the observations that PGC1α and SHP expression affects viral biosynthesis differently in HepG2 and Huh7 cells, it appears that ERRα and ERRγ control the majority of HBV transcription and replication in Huh7 cells (18a). Therefore, it is apparent that the two hepatoma cell lines, HepG2 and Huh7, which have been used extensively to study various aspects of the HBV replication cycle, differ in a dramatic manner with respect to their transcriptional regulation of viral biosynthesis (Fig. 4). Consequently, it is likely that viral biosynthesis in these two hepatoma cell lines will also be subject to distinct modes of physiological regulation. More importantly, it is impossible to determine the nature of the nuclear receptors governing HBV transcription and replication in vivo during natural infection using these two cell lines. Therefore, it will be essential to establish in vivo models of HBV infection to determine the relative importance of the various nuclear receptors known to be capable of modulating HBV transcription, and hence viral biosynthesis, under both normal and altered physiological conditions. From these in vivo models, it will be possible to identify the critical nuclear receptors controlling viral biosynthesis and to use this information to develop the most relevant cell culture systems that more precisely reflect the transcriptional environment present in the liver. Utilizing in vivo systems of viral biosynthesis, such as the HBV transgenic mouse model of chronic persistent infection, to establish the importance of specific nuclear receptors in combination with appropriate cell culture systems (11, 13, 21), antagonists of specific nuclear receptors might be developed as antiviral agents to treat the approximately 300 million chronic HBV carriers worldwide (7).
Acknowledgments
We are grateful to Anastasia Kralli (The Scripps Research Institute, La Jolla, CA) for the plasmid pcDNA3-HA-hPGC1α, Ronald M. Evans (Salk Institute, La Jolla, CA) for the plasmids pRS-hRXRα and pCMV-rFXRα, and David Mangelsdorf (Southwestern Medical Center, Dallas, TX) for the plasmids pCMX-mLRH1 and pCMX-SHP. We thank Harel Dahari for his assistance with the statistical analysis.
This work was supported by Public Health Service grant AI30070 from the National Institutes of Health.
Footnotes
Published ahead of print on 30 September 2009.
REFERENCES
- 1.Bavner, A., S. Sanyal, J. A. Gustafsson, and E. Treuter. 2005. Transcriptional corepression by SHP: molecular mechanisms and physiological consequences. Trends Endocrinol. Metab. 16:478-488. [DOI] [PubMed] [Google Scholar]
- 2.Bonnelye, E., J. M. Vanacker, T. Dittmar, A. Begue, X. Desbiens, D. T. Denhardt, J. E. Aubin, V. Laudet, and B. Fournier. 1997. The ERR-1 orphan receptor is a transcriptional activator expressed during bone development. Mol. Endocrinol. 11:905-916. [DOI] [PubMed] [Google Scholar]
- 3.Bookout, A. L., Y. Jeong, M. Downes, R. M. Evans, and D. J. Mangelsdorf. 2005. Tissue-specific expression patterns of nuclear receptors. NURSA www.nursa.org/10.1621/datasets.02001.
- 4.Chang, C., K. Jeng, C. Hu, S. J. Lo, T. Su, L.-P. Ting, C.-K. Chou, S. Han, E. Pfaff, J. Salfeld, and H. Schaller. 1987. Production of hepatitis B virus in vitro by transient expression of cloned HBV DNA in a hepatoma cell line. EMBO J. 6:675-680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen, D., G. Lepar, and B. Kemper. 1994. A transcriptional regulatory element common to a large family of hepatic cytochrome P450 genes is a functional binding site of the orphan receptor HNF-4. J. Biol. Chem. 269:5420-5427. [PubMed] [Google Scholar]
- 6.Chomczynski, P., and N. Sacchi. 1987. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal. Biochem. 162:156-159. [DOI] [PubMed] [Google Scholar]
- 7.Dienstag, J. L. 2008. Hepatitis B virus infection. N. Engl. J. Med. 359:1486-1500. [DOI] [PubMed] [Google Scholar]
- 8.Dubois, M. F., C. Pourcel, S. Rousset, C. Chany, and P. Tiollais. 1980. Excretion of hepatitis B surface antigen particles from mouse cells transformed with cloned viral DNA. Proc. Natl. Acad. Sci. USA 77:4549-4553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Evans, R. M., G. D. Barish, and Y. X. Wang. 2004. PPARs and the complex journey to obesity. Nat. Med. 10:355-361. [DOI] [PubMed] [Google Scholar]
- 10.Ganem, D., and R. Schneider. 2001. Hepadnaviridae: the viruses and their replication, p. 2923-2970. In D. M. Knipe and P. M. Howley (ed.), Fields virology. Lippincott Williams & Wilkins, Philadelphia, PA.
- 11.Guidotti, L. G., B. Matzke, H. Schaller, and F. V. Chisari. 1995. High-level hepatitis B virus replication in transgenic mice. J. Virol. 69:6158-6169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knutti, D., A. Kaul, and A. Kralli. 2000. A tissue-specific coactivator of steroid receptors, identified in a functional genetic screen. Mol. Cell. Biol. 20:2411-2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li, L., C. E. Oropeza, Jr., B. Sainz, S. L. Uprichard, F. J. Gonzalez, and A. McLachlan. 2009. Developmental regulation of hepatitis B virus biosynthesis by hepatocyte nuclear factor 4α. PLoS ONE 4:e5489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin, J., C. Handschin, and B. M. Spiegelman. 2005. Metabolic control through the PGC-1 family of transcription coactivators. Cell Metab. 1:361-370. [DOI] [PubMed] [Google Scholar]
- 15.Lu, T. T., M. Makishima, J. J. Repa, K. Schoonjans, T. A. Kerr, J. Auwerx, and D. J. Mangelsdorf. 2000. Molecular basis for feedback regulation of bile acid synthesis by nuclear receptors. Mol. Cell 6:507-515. [DOI] [PubMed] [Google Scholar]
- 16.Mangelsdorf, D. J., E. S. Ong, J. A. Dyck, and R. M. Evans. 1990. Nuclear receptor that identifies a novel retinoic acid response pathway. Nature 345:224-229. [DOI] [PubMed] [Google Scholar]
- 17.McLachlan, A., D. R. Milich, A. K. Raney, M. G. Riggs, J. L. Hughes, J. Sorge, and F. V. Chisari. 1987. Expression of hepatitis B virus surface and core antigens: influences of pre-S and precore sequences. J. Virol. 61:683-692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muerhoff, A. S., K. J. Griffin, and E. F. Johnson. 1992. The peroxisome proliferator-activated receptor mediates the induction of CYP4A6, a cytochrome P450 fatty acid omega-hydroxylase, by clofibric acid. J. Biol. Chem. 267:19051-19053. [PubMed] [Google Scholar]
- 18a.Ondracek, C. R., C. N. Rushing, V. C. Reese, C. E. Oropeza, and A. McLachlan. 2009. Peroxisome proliferator-activated receptor γ coactivator 1α and small heterodimer partner differentially regulate nuclear receptor-dependent hepatitis B virus biosynthesis. J. Virol. 83:12535-12544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oropeza, C. E., L. Li, and A. McLachlan. 2008. Differential inhibition of nuclear hormone receptor-dependent hepatitis B virus replication by small heterodimer partner. J. Virol. 82:3814-3821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raney, A. K., J. L. Johnson, C. N. A. Palmer, and A. McLachlan. 1997. Members of the nuclear receptor superfamily regulate transcription from the hepatitis B virus nucleocapsid promoter. J. Virol. 71:1058-1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raney, A. K., E. F. Kline, H. Tang, and A. McLachlan. 2001. Transcription and replication of a natural hepatitis B virus nucleocapsid promoter variant is regulated in vivo by peroxisome proliferators. Virology 289:239-251. [DOI] [PubMed] [Google Scholar]
- 22.Raney, A. K., and A. McLachlan. 1991. The biology of hepatitis B virus, p. 1-37. In A. McLachlan (ed.), Molecular biology of the hepatitis B virus. CRC Press, Boca Raton, FL.
- 23.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY.
- 24.Schlicht, H. J., and H. Schaller. 1989. Analysis of hepatitis B virus gene functions in tissue culture and in vivo. Curr. Top. Microbiol. Immunol. 144:253-263. [DOI] [PubMed] [Google Scholar]
- 25.Summers, J., P. M. Smith, M. Huang, and M. Yu. 1991. Morphogenetic and regulatory effects of mutations in the envelope proteins of an avian hepadnavirus. J. Virol. 65:1310-1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sureau, C., J.-L. Romet-Lemonne, J. I. Mullins, and M. Essex. 1986. Production of hepatitis B virus by a differentiated human hepatoma cell line after transfection with cloned circular HBV DNA. Cell 47:37-47. [DOI] [PubMed] [Google Scholar]
- 27.Tang, H., and A. McLachlan. 2001. Transcriptional regulation of hepatitis B virus by nuclear hormone receptors is a critical determinant of viral tropism. Proc. Natl. Acad. Sci. USA 98:1841-1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Twist, E. M., H. F. Clark, D. P. Aden, B. B. Knowles, and S. A. Plotkin. 1981. Integration pattern of hepatitis B virus DNA sequences in human hepatoma cell lines. J. Virol. 37:239-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Will, H., W. Reiser, T. Weimer, E. Pfaff, M. Buscher, R. Sprengle, R. Cattaneo, and H. Schaller. 1987. Replication strategy of human hepatitis B virus. J. Virol. 61:904-911. [DOI] [PMC free article] [PubMed] [Google Scholar]