Abstract
Purely electrical heart diseases, defined by the absence of any structural cardiac defects, are responsible for a large number of sudden, unexpected deaths in otherwise healthy, young individuals. These conditions include the long QT syndrome, Brugada syndrome, catecholaminergic polymorphic ventricular tachycardia and the short QT syndrome. Collectively, these conditions have been referred to as channelopathies. Ion channels provide the molecular basis for cardiac electrical activity. These channels have specific ion selectivity and are responsible for the precise and timely regulation of the passage of charged ions across the cell membrane in myocytes, and the summation of their activity in cardiac muscle defines the surface electrocardiogram. Impairment in the flow of these ions in heart cells may mean the difference between a normal, prosperous life and the tragedy of a sudden, unexpected death due to ventricular arrhythmia. The present paper reviews the current clinical and molecular understanding of the electrical diseases of the heart associated with sudden cardiac death.
Keywords: Arrhythmias, Genetics, Sudden cardiac death
Abstract
Les troubles purement électriques, définis comme l’absence de lésions cardiaques structurales, entraînent la mort subite d’un grand nombre de jeunes, par ailleurs en bonne santé. Ces troubles comprennent notamment le syndrome de l’allongement de l’intervalle QT, le syndrome de Brugada, la tachycardie ventriculaire polymorphe catécholaminergique et le syndrome du raccourcissement de l’intervalle QT. Ce type d’arythmie est désigné par le terme de maladie des canaux ioniques. Ceux-ci constituent la base moléculaire de l’activité électrique du cœur; ils ont une sélectivité ionique spécifique et ils sont responsables du passage régulier des ions chargés par la membrane cellulaire dans les myocytes, et l’ensemble de leur activité dans le muscle cardiaque est rendu visible par l’électrocardiogramme de surface. Ainsi, les troubles de la circulation des ions dans les cellules du cœur peuvent faire toute la différence entre une vie normale, heureuse et une mort subite, tragique, causée par l’arythmie ventriculaire. Le présent article fait le point sur les facteurs cliniques et moléculaires des troubles de la conduction électrique, liés à la mort cardiaque subite.
Over the past decade, molecular genetics research has established a link between a number of inherited, lethal cardiac arrhythmias and mutations in genes encoding for ion channels or other membrane components. These purely electrical heart diseases may manifest at any age, and are responsible for a large number of sudden, unexpected deaths in otherwise healthy, young individuals. These conditions include the long QT syndrome (LQTS) (1,2), Brugada syndrome (3), catecholaminergic polymorphic ventricular tachycardia (CPVT) (4–6) and the short QT syndrome (7). In addition, idiopathic atrial fibrillation, a common cause of stroke (8), has now been proven to have a genetic basis (6).
Collectively, these conditions have been referred to as channelopathies. Ion channels provide the molecular basis for cardiac electrical activity. These channels have specific ion selectivity and allow the passage of charged ions, such as sodium, potassium and calcium, across the cell membrane. The precision and timeliness of the passage of these charged ions, as mediated by their specific ion channel proteins, is the basis for a normal cardiac action potential in myocytes, and the summation of their activity in cardiac muscle defines the surface electrocardiogram (ECG). A genetic mutation altering the protein structure of an ion channel may perturb the precise regulation in the flow of ions across the cell membrane, leading to alterations in cardiac action potential duration or vulnerability of the cell to abnormal afterdepolarizations, triggering dangerous ventricular arrhythmias. Thus, impairment in the flow of these basic minerals in heart cells may mean the difference between a normal, prosperous life and the tragedy of a sudden, unexpected death.
The knowledge of the genetic cause and specific proteins responsible for these conditions has now allowed a more in-depth understanding of the molecular mechanisms involved in disease susceptibility, enabling researchers to target specific molecular pathways in drug development, such as the proposed use of the novel compound JTV519 in the treatment of CPVT (9) or the use of mexiletine to prevent arrhythmia in patients with the LQTS type 3 (LQT3) (10). In addition, genotype-phenotype correlations demonstrated in clinical observation studies have enabled clinicians to risk stratify patients (11,12) and to offer the most appropriate treatment options. Lastly, knowledge of the culprit genes provides the opportunity to genetically screen asymptomatic family members who may have subclinical disease, possibly preventing the tragedy of sudden cardiac death. The present paper reviews the current clinical and molecular understanding of the electrical diseases of the heart associated with sudden cardiac death.
LQTS
History
In 1856, Meissner (13) described the sudden death of a young, deaf girl who was being berated at her school academy. Inadvertently, this was perhaps the first reported description of the LQTS. A more detailed clinical characterization of deafness, prolonged QT interval on ECG and propensity to sudden cardiac death followed more than a century later when Jervell and Lange-Nielsen (14) described a series of patients. A similar syndrome, but without deafness, was identified to run in families and was first described by Romano et al (15) in 1963 and later by Ward (16) in 1964. The clinical spectrum of the LQTS is now well characterized, with affected patients vulnerable to recurrent syncope or cardiac arrest from a polymorphic ventricular tachycardia known as torsade de pointes (17).
Genetics
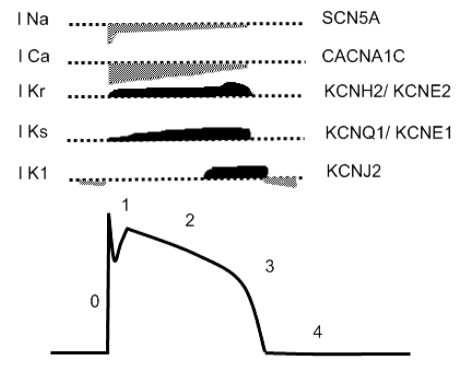
In 1995, Sanguinetti et al (18) and Wang et al (19) reported the first two genes responsible for the LQTS. Since these seminal findings, molecular genetic studies over the past decade have revealed a total of six additional genes responsible for this inherited arrhythmia syndrome (Figure 1). These genes encode for potassium, sodium and calcium ion channels or a membrane localizing protein, and are located on chromosomes 3, 4, 7, 11, 12, 17 and 21. LQTS type 1 (LQT1) is caused by mutations in the KCNQ1 gene, which encodes the alpha subunit of a voltage-gated potassium channel responsible for a slowly activating potassium current (IKs) necessary for rectifying the transmembrane voltage potential to baseline during an action potential. Coassembly of the KCNQ1 protein with a beta-subunit protein encoded for by the KCNE1 gene results in functional IKs channels. Thus, genetic mutations in either KCNQ1 (LQT1) or KCNE1 (LQT5) may alter the passage of potassium flow across the cell membrane, specifically leading to loss of function or decreased current, resulting in prolongation of the action potential duration – the molecular hallmark of the LQTS (20,21). Homozygous mutations of either gene are responsible for the additional phenotype of deafness (Jervell and Lange-Nielson syndrome).
Figure 1).
Long QT syndrome genes and their currents comprising the normal cardiac action potential. Prolongation of the cardiac action potential may occur by impaired flow of potassium ions out of the cell during phase 3 of the action potential, or due to an increased inward sodium or calcium current during the plateau phase. Action potential phases: 0 = depolarization, 1 = fast repolarization, 2 = plateau, 3 = repolarization and 4 = resting potential. ICa Inward calcium current; IK1 Inward rectifier potassium current; IKr Rapidly activating potassium current; IKs Slowly activating potassium current; INa Inward sodium current
LQTS type 2 is caused by mutations in the KCNH2 gene, resulting in the loss of function of another action potential repolarizing or rectifying potassium current, the rapidly activating potassium current (IKr). Function of this current also requires an additional protein subunit encoded for by the KCNE2 gene. Therefore, this potassium ion channel is also impaired by mutations in the KCNE2 gene, identified as the LQTS type 6 (LQT6) (18,22).
Genetic defects in the SCN5A gene, which encodes the alpha subunit of the major ion channel responsible for the passage of sodium ions in heart cells, are the culprit for LQT3 (19). In contrast to the loss-of-function mutations of potassium channels, mutations of the sodium channel lead to an increase in sodium current. However, this effect also leads to prolonged action potential duration, predominantly by prolonging the plateau phase of the action potential (Figure 1).
More rare forms of LQTS include types 7 (LQT7), 8 (LQT8) and 4 (LQT4). LQT7 is caused by mutations in the KCNJ2 gene encoding for the inward rectifier potassium current (IK1). This form of LQTS is found in association with Andersen-Tawil syndrome, a condition with an array of extracardiac congenital abnormalities (23,24). Most recently, a mutation in the CACNA1C gene was reported to be responsible for a defect in the L-type calcium current (ICa-L) underlying the rare LQT8 form, an arrhythmic disorder associated with dysfunction in multiple organ systems, including congenital heart disease, syndactyly, immune deficiency and autism.
LQT4 is the exception to the ‘channelopathy’ basis for the LQTS. The causative gene is ANK2, which encodes ankyrin B, a protein responsible for the appropriate cellular localization of various proteins involved in electrical signalling cascades in electrically active cells. Specifically, evidence suggests that mutations in ANK2 impair pathways important in the regulation of intracellular calcium (25).
In all its genetic forms, LQTS decreases outward potassium currents (IKs, IKr and IK1) or increases inward sodium or calcium current (late INa or ICa-L), both effects that result in prolongation of the action potential duration. Of the eight genes described, responsible mutations are identified in approximately 70% of clinically diagnosed LQTS probands (26). The absence of a genetic diagnosis in a proportion of probands is likely related to an incorrect diagnosis in some cases and/or rare forms due to yet undiscovered causative genes. When a genetic diagnosis is confirmed, the LQT1 and LQT2 forms are the two most commonly identified, each accounting for approximately 40% of genotyped patients (27). The LQT3 form accounts for approximately 10% of genotyped patients.
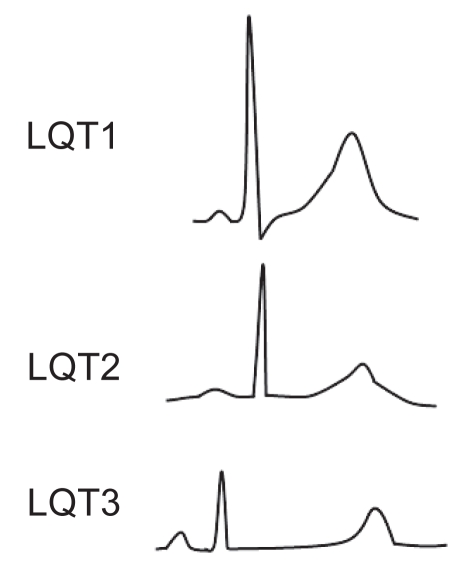
Because the LQT1, LQT2 and LQT3 forms constitute more than 90% of genotyped patients with LQTS, the genotype-phenotype correlation has been investigated in detail in the LQT1, LQT2 and LQT3 forms (27). Broad-based, prolonged T waves are more commonly observed in the LQT1 form, whereas low-amplitude T waves with a notched or bifurcated configuration are seen more frequently in the LQT2 form. LQT3 patients often show late-appearing T waves with a prolonged isoelectric ST segment (Figure 2). However, exceptions are present in all three genotypes (28), and the T wave pattern varies with time, even in the same patient with a specific mutation.
Figure 2).
Genotype-phenotype electrocardiogram (ECG) characteristics in the three most common forms of inherited long QT syndrome (LQTS). Typical T wave morphological abnormalities in LQTS are best seen in the precordial ECG leads. LQTS type 1 (LQT1) commonly shows a broad-based T wave pattern, LQTS type 2 (LQT2) shows notched or bifurcated T waves, and LQTS type 3 (LQT3) shows a late-appearing T wave with a prolonged ST segment
Previous observational studies have reported differential triggers for cardiac events, clinical course and risk stratification between each genotype, especially in the LQT1, LQT2 and LQT3 syndromes. Clinical evidence has suggested genotype-specific triggers for cardiac events in patients with the LQT1, LQT2 and LQT3 syndromes (29,30). Schwartz et al (29) analyzed data from the International LQTS Registry and reported that cardiac events most frequently occur during exercise (62%) but only rarely during sleep and rest (3%) in LQT1 patients. Swimming is a common trigger in LQT1. In contrast to the pattern shown in LQT1 patients, cardiac events principally occur during sleep and rest (39%), and exercise-related cardiac events are uncommon (13%) in LQT3 patients. In LQT2 patients, cardiac events occur equally during exercise (13%) and during sleep/rest (15%). More importantly, a sudden startle in the form of an auditory stimulus (eg, telephone, alarm clock or ambulance siren) is a specific trigger in LQT2.
LQT1 and LQT2 patients show a higher frequency and cumulative probability of cardiac events (syncope and cardiac arrest) than LQT3 patients. However, the lethality of the cardiac events is higher in LQT3 patients. Male patients are generally younger than female patients at first cardiac events. It is noteworthy that many first cardiac events occur before the age of 15 years in male patients, particularly in LQT1 males, whereas female patients may experience first cardiac events after the age of 20 years. More recently, risk stratification according to genotype, age, sex and corrected QT interval has been recommended (11) (Table 1). In general, heart rate-corrected QT intervals in the range of 500 ms or greater are a significant risk marker for cardiac events, regardless of other clinical characteristics.
TABLE 1.
Risk stratification for first cardiac event according to genotype, sex and corrected QT interval (QTc)
| QTc | Men | Women | |
|---|---|---|---|
| High risk (≥50%) | ≥500 ms | LQT1 | LQT1 |
| LQT2 | LQT2 | ||
| LQT3 | |||
| Intermediate risk (30% to 49%) | ≥500 ms | LQT3 | |
| <500 ms | LQT3 | LQT2 | |
| LQT3 | |||
| Low risk (<30%) | <500 ms | LQT2 | LQT1 |
| LQT1 |
Risk = first cardiac event (syncope, cardiac arrest or sudden death) before the age of 40 years and before therapy. LQT1 Long QT syndrome (LQTS) type 1; LQT2 LQTS type 2; LQT3 LQTS type 3. Adapted from reference 11
Therapeutic considerations
It is empirically believed that beta-blockers and strict exercise restriction are the most effective therapy for all patients with congenital LQTS. However, beta-blockers are known not to be protective in all patients. Undoubtedly, the use of beta-blockers has proven effective in reducing cardiac events in patients with genetically proven LQT1 and LQT2. However, breakthrough events may still occur, particularly in patients with events before treatment (31,32), and frank discussion of the option of an implantable cardioverter-defibrillator is always reasonable.
Beta-blockers are not effective in patients with LQT3. Alternatively, in 1995, Schwartz et al (33) demonstrated that sodium channel blockade with mexiletine, a class 1B anti-arrhythmic, is much more effective in abbreviating the QT interval in LQT3 patients than in LQT2 patients. Short-term efficacy data exist to suggest that mexiletine may prevent lethal events (34,35). However, there are no long-term prospective data demonstrating that mexiletine improves survival in LQT3 patients. Nonetheless, the development of novel sodium channel blocking agents remains a promising approach for the treatment of LQT3 patients.
Although beta-blockers are the mainstay of treatment for LQT1 and LQT2, anecdotal observations in some patients and in experimental models have raised the possibility of alternative or adjunctive pharmacological strategies. Potassium channel activators, such as nicorandil or pinacidil, have been shown to reverse epinephrine-induced QT prolongation and suppress ventricular arrhythmias (36,37). In LQT2, short-term, exogenously administered potassium was reported to correct QT abnormalities in affected patients (38), presumably by enhancing IKr in the outward direction across the cell membrane. Recently, long-term oral potassium administration was shown to improve repolarization abnormalities in LQT2 patients (39). Although these therapeutic strategies show promise, their effect on cardiac outcomes in the LQTS await long-term, prospective studies.
BRUGADA SYNDROME
History
The electrocardiographic pattern of ST segment elevation in the right precordial leads was described as early as 1953 (40). The relationship of this ECG pattern to sudden cardiac death was first described by Martini et al (41) in 1989. In 1992, Brugada and Brugada (42) provided detailed clinical and electrophysiological characteristics in eight patients and proposed this clinical entity as a distinct clinical syndrome, later to become known as the Brugada syndrome. The Brugada syndrome is characterized by sudden cardiac death from ventricular fibrillation, in association with a typical ECG signature of ST segment elevation in the right precordial leads (42,43). It is inherited in an autosomal dominant fashion and may commonly be observed as a sporadic, non-familial disorder.
Clinical characteristics
Since its recognition as a distinct subgroup of idiopathic ventricular fibrillation, Brugada syndrome has been described increasingly worldwide. The clinical presentation is heterogeneous, including palpitations, dizziness, syncope and (aborted) sudden death, although many subjects are asymptomatic (44,45). It is believed to cause 4% to 12% of all sudden cardiac deaths and up to 20% among patients without identifiable structural abnormalities in some regions of the world (46). Men have a higher disease prevalence, particularly in regions where Brugada syndrome is endemic (southeast Asia), despite equal genetic transmission between both sexes (47). Sex hormones may underlie this gender disparity (48). Sudden death typically occurs at rest, when the vagal tone is augmented (49), often at night (50).
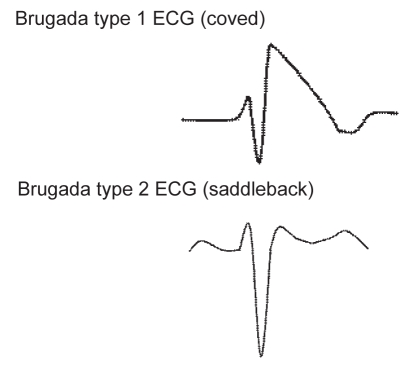
The diagnosis revolves around characteristic ST segment elevations. However, the ST segment in Brugada syndrome may be highly dynamic, exhibiting profound day-to-day and beat-to-beat variation in amplitude and morphology. Two predominant morphologies of ST segment elevation exist (Figure 3). The coved-type morphology is required for the diagnosis (51), while the saddleback type is an intermediate form that requires confirmation using pharmacological challenge (conversion into coved type) or genetic analysis (52).
Figure 3).
The two predominant electrocardiogram (ECG) repolarization abnormalities observed in the Brugada syndrome. Brugada syndrome ECG pattern abnormalities are observed in the anterior precordial leads (V1 and/or V2). ECG abnormalities may be dynamic, and alternate between normal or abnormal ECG patterns. The coved-shaped pattern is suggested to be associated with an increased risk of cardiac events
Brugada syndrome is often accompanied by some degree of conduction system disease. Signs of conduction defects are found at many levels, particularly in patients with SCN5A mutations (53). This is not surprising because genetic defects in the SCN5A gene are also known to cause familial conduction system disease in the absence of ECG repolarization abnormalities.
Genetics
The first and only gene to be linked to Brugada syndrome is SCN5A, the gene that encodes for the alpha subunit of the cardiac sodium channel gene (3). More than 80 mutations in SCN5A have been linked to the syndrome since 2001 (54–56). Approximately 20 of these mutations have been studied in expression systems and shown to result in loss of function by various mechanisms, including failure of the sodium channel to express; a shift in the voltage and time dependence of sodium channel current activation, inactivation or reactivation; entry of the sodium channel into an intermediate state of inactivation from which it recovers more slowly; or accelerated inactivation of the sodium channel.
A second locus on chromosome 3, close to but apart from the SCN5A locus, was linked recently to Brugada syndrome (57) in a large pedigree in which the syndrome was also inherited in an autosomal dominant manner and associated with progressive conduction disease, a low sensitivity to procainamide and a relatively benign prognosis. SCN5A mutations account for approximately 18% to 30% of Brugada syndrome cases. A higher incidence of SCN5A mutations has been reported in familial cases than in sporadic cases (58).
At present, knowledge of a specific mutation does not provide guidance in determining a prognosis. Genetic testing may be useful for early detection of relatives at potential risk who may harbour normal ECGs. While genetic results may not predict risk of events, clinical characteristics alone may suggest a higher risk of sudden death. Specifically, it is proposed that a spontaneous coved-shape ECG pattern and a history of syncope predict a higher risk of sudden death in contrast to a saddleback pattern or a provocable coved-shaped pattern (55). Currently, there are no drugs available that clearly show an efficacious effect in suppressing arrhythmias associated with Brugada syndrome, and consequently, for patients considered to be at high risk for events, an implantable cardioverter-defibrillator should be considered.
CPVT
History
CPVT is an inherited cardiac arrhythmia disorder showing a highly malignant clinical course in the absence of visible morphological alterations of the heart. This condition is the latest of the purely electrical conditions of the heart to have a proven genetic basis, inherited as an autosomal dominant (59,60) or recessive (61) genetic disease. The clinical phenotype of bidirectional or polymorphic ventricular tachycardia occurring with physical or emotional stress in patients with structurally normal hearts and normal resting ECGs was first described in isolated case studies in the 1960s and 1970s (62–64). In 1978, Coumel et al (65) described a series of young patients presenting with catecholamine-induced polymorphic ventricular arrhythmias.
Genetics and disease mechanism
In 1997, Nakajima et al (66) reported on the electrophysiological study of a patient with CPVT, demonstrating polymorphic ventricular arrhythmias induced by isoprotenerol infusion and failure to induce arrhythmias by programmed electrical stimulation. Arrhythmias were suppressed by injections of verapamil, a calcium channel blocker. Monophasic action potentials recorded at the right ventricle inflow demonstrated delayed afterdepolarizations, the amplitude of which increased with isoprotenerol infusion, culminating in the appearance of polymorphic premature ventricular beats (66). These data implicated impaired intracellular calcium homeostasis as a mechanism for arrhythmia vulnerability.
The gene locus for familial CPVT was first mapped by Swan et al (67) to chromosome 1q42–q43. Subsequently, two groups simultaneously identified the disease-causing gene for CPVT to be the cardiac ryanodine receptor type 2 (RyR2) (4,5,68), confirming the regulation of calcium fluxes as critical to the disease state.
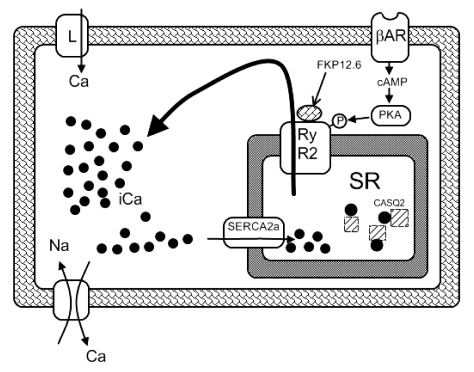
RyR2 occupies a central position in cardiomyocyte excitation-contraction coupling. Upon opening of the cell membrane L-type (dihydropyridine) calcium channels by the depolarizing action potential, small amounts of calcium ions permeate the cardiomyocyte and trigger a 10-fold increased release of calcium ions through the RyR2 channels situated at the sarcoplasmic reticulum, the organelle responsible for intracellular calcium storage. This chain of events is known as calcium-induced calcium release (Figure 4). The calcium ions released interact with the contractile proteins and, thus, initiate cardiac systole. During diastole, the calcium ions are pumped back into the sarcoplasmic reticulum via the sarcoplasmic reticulum calcium ATPase-2a or into the extra-cellular fluid via the sarcolemmal sodium-calcium exchanger. Mutations in the RyR2 channel lead to a gain-of-function effect, whereby calcium ions are released through the channel at a lower activation threshold, leading to inappropriate calcium release and delayed afterdepolarizations triggering arrhythmias.
Figure 4).
Simplified schemata of relevant proteins involved in intracellular calcium (iCa) regulation. Coupling of myocyte excitation-contraction is mediated through calcium (Ca), initiated by the inward L-type Ca channel. This current leads to sarcoplasmic reticulum (SR) release of Ca via the ryanodine receptor type 2 (RyR2) and the subsequent contractile process. βAR Beta-adrenergic receptor; cAMP Cyclic AMP; Na Sodium; PKA Protein kinase A; SERCA2a Sarcoplasmic reticulum calcium ATPase-2a
Therapeutic considerations
The very high mortality rate associated with CPVT, amounting to 30% to 35% by the age of 30 years, calls for novel effective preventive measures. Unfortunately, sudden death may constitute the first manifestation of the disease. Because Holter recordings are of limited value, exercise stress testing or intravenous epinephrine infusion is the method of choice for clinical diagnosis.
The molecular pathogenesis of RyR2-mediated CPVT stresses the role of increased adrenergic activity as a culprit in triggering arrhythmias. In fact, administration of beta-adrenergic blocking drugs remains the standard treatment for CPVT. Leenhardt et al (59) encountered 10 fatalities among 21 untreated patients (48%) but only four sudden deaths among 38 nadolol-treated patients (11%); the exact molecular type of CPVT, however, was not studied at that time. Priori et al (69) gave nadolol, metoprolol or propranolol to 19 patients with RyR2 mutations, but seven (37%) remained symptomatic. Bauce et al (70) administered beta-blockers to 26 patients with RyR2 mutations. A repeated stress test demonstrated disappearance of symptoms in 17 patients, while in the remaining nine patients, the drug dose was increased. During the mean follow-up of 6.5 years, there were no syncopal episodes or sudden deaths.
RyR2 activity is modulated by the protein FKP12.6. Dissociation of FKBP12.6 from RyR2 increases the probability of the calcium channel being open and induces subconductance states (ie, RyR2 becomes more leaky) (71). Experimental studies (9) of three known CPVT mutations have shown decreased binding affinity of RyR2 for FKBP12.6 with subsequent gain of function (leakiness). A novel pharmacological compound, JTV519 (also known as K201), has been shown to stabilize the closed state of RyR2. The exact method of action remains controversial (72). Nonetheless, it has been postulated that JTV519 may provide an alternative pharmacological therapy for CPVT patients (73).
In patients with continued syncope or frequent arrhythmias not suppressed by medical therapy, implantable cardioverter-defibrillators remain a reasonable alternative (4,68,69).
Footnotes
SUPPORT: Dr Gollob’s research is supported by the Heart and Stroke Foundation of Ontario.
REFERENCES
- 1.Keating M, Atkinson D, Dunn C, Timothy K, Vincent GM, Leppert M. Linkage of a cardiac arrhythmia, the long QT syndrome, and the Harvey ras-1 gene. Science. 1991;252:704–6. doi: 10.1126/science.1673802. [DOI] [PubMed] [Google Scholar]
- 2.Donger C, Denjoy I, Berthet M, et al. KVLQT1 C-terminal missense mutation causes a forme fruste long-QT syndrome. Circulation. 1997;96:2778–81. doi: 10.1161/01.cir.96.9.2778. [DOI] [PubMed] [Google Scholar]
- 3.Chen Q, Kirsch GE, Zhang D, et al. Genetic basis and molecular mechanism for idiopathic ventricular fibrillation. Nature. 1998;392:293–6. doi: 10.1038/32675. [DOI] [PubMed] [Google Scholar]
- 4.Priori SG, Napolitano C, Tiso N, et al. Mutations in the cardiac ryanodine receptor gene (hRyR2) underlie catecholaminergic polymorphic ventricular tachycardia. Circulation. 2001;103:196–200. doi: 10.1161/01.cir.103.2.196. [DOI] [PubMed] [Google Scholar]
- 5.Laitinen PJ, Brown KM, Piippo K, et al. Mutations of the cardiac ryanodine receptor (RyR2) gene in familial polymorphic ventricular tachycardia. Circulation. 2001;103:485–90. doi: 10.1161/01.cir.103.4.485. [DOI] [PubMed] [Google Scholar]
- 6.Gollob MH, Jones DL, Krahn AD, et al. Somatic mutations in the connexin 40 gene (GJA5) in atrial fibrillation. N Engl J Med. 2006;354:2677–88. doi: 10.1056/NEJMoa052800. [DOI] [PubMed] [Google Scholar]
- 7.Brugada R, Hong K, Dumaine R, et al. Sudden death associated with short-QT syndrome linked to mutations in HERG. Circulation. 2004;109:30–5. doi: 10.1161/01.CIR.0000109482.92774.3A. [DOI] [PubMed] [Google Scholar]
- 8.Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: National implications for rhythm management and stroke prevention: The AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 9.Lehnart SE, Wehrens XH, Laitinen PJ, et al. Sudden death in familial polymorphic ventricular tachycardia associated with calcium release channel (ryanodine receptor) leak. Circulation. 2004;109:3208–14. doi: 10.1161/01.CIR.0000132472.98675.EC. [DOI] [PubMed] [Google Scholar]
- 10.Schulze-Bahr E, Fenge H, Etzrodt D, et al. Long QT syndrome and life threatening arrhythmia in a newborn: Molecular diagnosis and treatment response. Heart. 2004;90:13–6. doi: 10.1136/heart.90.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Priori SG, Schwartz PJ, Napolitano C, et al. Risk stratification in the long-QT syndrome. N Engl J Med. 2003;348:1866–74. doi: 10.1056/NEJMoa022147. [DOI] [PubMed] [Google Scholar]
- 12.Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003;108:3092–6. doi: 10.1161/01.CIR.0000104568.13957.4F. [DOI] [PubMed] [Google Scholar]
- 13.Meissner FL. Heidelberg: Leipzig and Heidelberg; 1856. Taubstummheit und Taubstummenbildung. [Google Scholar]
- 14.Jervell A, Lange-Nielsen F. Congenital deaf-mutism, functional heart disease with prolongation of the Q-T interval and sudden death. Am Heart J. 1957;54:59–68. doi: 10.1016/0002-8703(57)90079-0. [DOI] [PubMed] [Google Scholar]
- 15.Romano C, Gemme G, Pongiglione R. [Rare cardiac arrythmias of the pediatric age. II. Syncopal attacks due to paroxysmal ventricular fibrillation. (Presentation of 1st case in Italian pediatric literature)] Clin Pediatr (Bologna) 1963;45:656–83. [PubMed] [Google Scholar]
- 16.Ward OC. A new familial cardiac syndrome in children. J Ir Med Assoc. 1964;54:103–6. [PubMed] [Google Scholar]
- 17.Moss AJ, Schwartz PJ, Crampton RS, Locati E, Carleen E. The long QT syndrome: A prospective international study. Circulation. 1985;71:17–21. doi: 10.1161/01.cir.71.1.17. [DOI] [PubMed] [Google Scholar]
- 18.Sanguinetti MC, Jiang C, Curran ME, Keating MT. A mechanistic link between an inherited and an acquired cardiac arrhythmia: HERG encodes the IKr potassium channel. Cell. 1995;81:299–307. doi: 10.1016/0092-8674(95)90340-2. [DOI] [PubMed] [Google Scholar]
- 19.Wang Q, Shen J, Splawski I, et al. SCN5A mutations associated with an inherited cardiac arrhythmia, long QT syndrome. Cell. 1995;80:805–11. doi: 10.1016/0092-8674(95)90359-3. [DOI] [PubMed] [Google Scholar]
- 20.Sanguinetti MC, Curran ME, Zou A, et al. Coassembly of K(V)LQT1 and minK (IsK) proteins to form cardiac I(Ks) potassium channel. Nature. 1996;384:80–3. doi: 10.1038/384080a0. [DOI] [PubMed] [Google Scholar]
- 21.Barhanin J, Lesage F, Guillemare E, Fink M, Lazdunski M, Romey G. K(V)LQT1 and lsK (minK) proteins associate to form the I(Ks) cardiac potassium current. Nature. 1996;384:78–80. doi: 10.1038/384078a0. [DOI] [PubMed] [Google Scholar]
- 22.Abbott GW, Sesti F, Splawski I, et al. MiRP1 forms IKr potassium channels with HERG and is associated with cardiac arrhythmia. Cell. 1999;97:175–87. doi: 10.1016/s0092-8674(00)80728-x. [DOI] [PubMed] [Google Scholar]
- 23.Andersen ED, Krasilnikoff PA, Overvad H. Intermittent muscular weakness, extrasystoles, and multiple developmental anomalies. A new syndrome? Acta Paediatr Scand. 1971;60:559–64. doi: 10.1111/j.1651-2227.1971.tb06990.x. [DOI] [PubMed] [Google Scholar]
- 24.Tawil R, Ptacek LJ, Pavlakis SG, et al. Andersen’s syndrome: Potassium-sensitive periodic paralysis, ventricular ectopy, and dysmorphic features. Ann Neurol. 1994;35:326–30. doi: 10.1002/ana.410350313. [DOI] [PubMed] [Google Scholar]
- 25.Mohler PJ, Schott JJ, Gramolini AO, et al. Ankyrin-B mutation causes type 4 long-QT cardiac arrhythmia and sudden cardiac death. Nature. 2003;421:634–9. doi: 10.1038/nature01335. [DOI] [PubMed] [Google Scholar]
- 26.Napolitano C, Priori SG, Schwartz PJ, et al. Genetic testing in the long QT syndrome: Development and validation of an efficient approach to genotyping in clinical practice. JAMA. 2005;294:2975–80. doi: 10.1001/jama.294.23.2975. [DOI] [PubMed] [Google Scholar]
- 27.Splawski I, Shen J, Timothy KW, et al. Spectrum of mutations in long-QT syndrome genes. KVLQT1, HERG, SCN5A, KCNE1, and KCNE2. Circulation. 2000;102:1178–85. doi: 10.1161/01.cir.102.10.1178. [DOI] [PubMed] [Google Scholar]
- 28.Zhang L, Timothy KW, Vincent GM, et al. Spectrum of ST-T-wave patterns and repolarization parameters in congenital long-QT syndrome: ECG findings identify genotypes. Circulation. 2000;102:2849–55. doi: 10.1161/01.cir.102.23.2849. [DOI] [PubMed] [Google Scholar]
- 29.Schwartz PJ, Priori SG, Spazzolini C, et al. Genotype-phenotype correlation in the long-QT syndrome: Gene-specific triggers for life-threatening arrhythmias. Circulation. 2001;103:89–95. doi: 10.1161/01.cir.103.1.89. [DOI] [PubMed] [Google Scholar]
- 30.Moss AJ, Robinson JL, Gessman L, et al. Comparison of clinical and genetic variables of cardiac events associated with loud noise versus swimming among subjects with the long QT syndrome. Am J Cardiol. 1999;84:876–9. doi: 10.1016/s0002-9149(99)00458-0. [DOI] [PubMed] [Google Scholar]
- 31.Moss AJ, Zareba W, Hall WJ, et al. Effectiveness and limitations of beta-blocker therapy in congenital long-QT syndrome. Circulation. 2000;101:616–23. doi: 10.1161/01.cir.101.6.616. [DOI] [PubMed] [Google Scholar]
- 32.Dorostkar PC, Eldar M, Belhassen B, Scheinman MM. Long-term follow-up of patients with long-QT syndrome treated with beta-blockers and continuous pacing. Circulation. 1999;100:2431–6. doi: 10.1161/01.cir.100.24.2431. [DOI] [PubMed] [Google Scholar]
- 33.Schwartz PJ, Priori SG, Locati EH, et al. Long QT syndrome patients with mutations of the SCN5A and HERG genes have differential responses to Na+ channel blockade and to increases in heart rate. Implications for gene-specific therapy. Circulation. 1995;92:3381–6. doi: 10.1161/01.cir.92.12.3381. [DOI] [PubMed] [Google Scholar]
- 34.Schwartz PJ, Priori SG, Dumaine R, et al. A molecular link between the sudden infant death syndrome and the long-QT syndrome. N Engl J Med. 2000;343:262–7. doi: 10.1056/NEJM200007273430405. [DOI] [PubMed] [Google Scholar]
- 35.Kehl HG, Haverkamp W, Rellensmann G, et al. Images in cardiovascular medicine. Life-threatening neonatal arrhythmia: Successful treatment and confirmation of clinically suspected extreme long QT-syndrome-3. Circulation. 2004;109:e205–6. doi: 10.1161/01.CIR.0000128874.43908.CA. [DOI] [PubMed] [Google Scholar]
- 36.Fujimoto Y, Morita H, Fukushima KK, Ohe T. Nicorandil abolished repolarisation alternans in a patient with idiopathic long QT syndrome. Heart. 1999;82:e8. doi: 10.1136/hrt.82.5.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fish FA, Prakash C, Roden DM. Suppression of repolarization-related arrhythmias in vitro and in vivo by low-dose potassium channel activators. Circulation. 1990;82:1362–9. doi: 10.1161/01.cir.82.4.1362. [DOI] [PubMed] [Google Scholar]
- 38.Compton SJ, Lux RL, Ramsey MR, et al. Genetically defined therapy of inherited long-QT syndrome. Correction of abnormal repolarization by potassium. Circulation. 1996;94:1018–22. doi: 10.1161/01.cir.94.5.1018. [DOI] [PubMed] [Google Scholar]
- 39.Etheridge SP, Compton SJ, Tristani-Firouzi M, Mason JW. A new oral therapy for long QT syndrome: Long-term oral potassium improves repolarization in patients with HERG mutations. J Am Coll Cardiol. 2003;42:1777–82. doi: 10.1016/j.jacc.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 40.Osher HL, Wolff L. Electrocardiographic pattern simulating acute myocardial injury. Am J Med Sci. 1953;226:541–5. [PubMed] [Google Scholar]
- 41.Martini B, Nava A, Thiene G, et al. Ventricular fibrillation without apparent heart disease: Description of six cases. Am Heart J. 1989;118:1203–9. doi: 10.1016/0002-8703(89)90011-2. [DOI] [PubMed] [Google Scholar]
- 42.Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: A distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391–6. doi: 10.1016/0735-1097(92)90253-j. [DOI] [PubMed] [Google Scholar]
- 43.Brugada J, Brugada R, Brugada P. Right bundle-branch block and ST-segment elevation in leads V1 through V3: A marker for sudden death in patients without demonstrable structural heart disease. Circulation. 1998;97:457–60. doi: 10.1161/01.cir.97.5.457. [DOI] [PubMed] [Google Scholar]
- 44.Atarashi H, Ogawa S, Harumi K, et al. Idiopathic Ventricular Fibrillation Investigators Three-year follow-up of patients with right bundle branch block and ST segment elevation in the right precordial leads: Japanese Registry of Brugada Syndrome. J Am Coll Cardiol. 2001;37:1916–20. doi: 10.1016/s0735-1097(01)01239-6. [DOI] [PubMed] [Google Scholar]
- 45.Hermida JS, Lemoine JL, Aoun FB, Jarry G, Rey JL, Quiret JC. Prevalence of the brugada syndrome in an apparently healthy population. Am J Cardiol. 2000;86:91–4. doi: 10.1016/s0002-9149(00)00835-3. [DOI] [PubMed] [Google Scholar]
- 46.Antzelevitch C, Brugada P, Brugada J, et al. Brugada syndrome: A decade of progress. Circ Res. 2002;91:1114–8. doi: 10.1161/01.res.0000046046.53721.90. [DOI] [PubMed] [Google Scholar]
- 47.Atarashi H, Ogawa S, Harumi K, et al. Characteristics of patients with right bundle branch block and ST-segment elevation in right precordial leads. Idiopathic Ventricular Fibrillation Investigators. Am J Cardiol. 1996;78:581–3. doi: 10.1016/s0002-9149(96)00360-8. [DOI] [PubMed] [Google Scholar]
- 48.Matsuo K, Akahoshi M, Seto S, Yano K.Disappearance of the Brugada-type electrocardiogram after surgical castration: A role for testosterone and an explanation for the male preponderance Pacing Clin Electrophysiol 200326(7 Pt 1):1551–3. [DOI] [PubMed] [Google Scholar]
- 49.Matsuo K, Kurita T, Inagaki M, et al. The circadian pattern of the development of ventricular fibrillation in patients with Brugada syndrome. Eur Heart J. 1999;20:465–70. doi: 10.1053/euhj.1998.1332. [DOI] [PubMed] [Google Scholar]
- 50.Itoh H, Shimizu M, Ino H, et al. Hokuriku Brugada Study Group Arrhythmias in patients with Brugada-type electrocardiographic findings. Jpn Circ J. 2001;65:483–6. doi: 10.1253/jcj.65.483. [DOI] [PubMed] [Google Scholar]
- 51.Wilde AA, Antzelevitch C, Borggrefe M, et al. Study Group on the Molecular Basis of Arrhythmias of the European Society of Cardiology Proposed diagnostic criteria for the Brugada syndrome: Consensus report. Circulation. 2002;106:2514–9. doi: 10.1161/01.cir.0000034169.45752.4a. [DOI] [PubMed] [Google Scholar]
- 52.Plunkett A, Hulse JA, Mishra B, Gill J. Variable presentation of Brugada syndrome: Lessons from three generations with syncope. BMJ. 2003;326:1078–9. doi: 10.1136/bmj.326.7398.1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Smits JP, Eckardt L, Probst V, et al. Genotype-phenotype relationship in Brugada syndrome: Electrocardiographic features differentiate SCN5A-related patients from non-SCN5A-related patients. J Am Coll Cardiol. 2002;40:350–6. doi: 10.1016/s0735-1097(02)01962-9. [DOI] [PubMed] [Google Scholar]
- 54.Antzelevitch C. The Brugada syndrome: Ionic basis and arrhythmia mechanisms. J Cardiovasc Electrophysiol. 2001;12:268–72. doi: 10.1046/j.1540-8167.2001.00268.x. [DOI] [PubMed] [Google Scholar]
- 55.Priori SG, Napolitano C, Gasparini M, et al. Natural history of Brugada syndrome: Insights for risk stratification and management. Circulation. 2002;105:1342–7. doi: 10.1161/hc1102.105288. [DOI] [PubMed] [Google Scholar]
- 56.Balser JR. The cardiac sodium channel: Gating function and molecular pharmacology. J Mol Cell Cardiol. 2001;33:599–613. doi: 10.1006/jmcc.2000.1346. [DOI] [PubMed] [Google Scholar]
- 57.Weiss R, Barmada MM, Nguyen T, et al. Clinical and molecular heterogeneity in the Brugada syndrome: A novel gene locus on chromosome 3. Circulation. 2002;105:707–13. doi: 10.1161/hc0602.103618. [DOI] [PubMed] [Google Scholar]
- 58.Schulze-Bahr E, Eckardt L, Breithardt G, et al. Sodium channel gene (SCN5A) mutations in 44 index patients with Brugada syndrome: Different incidences in familial and sporadic disease Hum Mutat 200321651–2.(Erratum in 2005;26:61) [DOI] [PubMed] [Google Scholar]
- 59.Leenhardt A, Lucet V, Denjoy I, Grau F, Ngoc DD, Coumel P. Catecholaminergic polymorphic ventricular tachycardia in children. A 7-year follow-up of 21 patients. Circulation. 1995;91:1512–9. doi: 10.1161/01.cir.91.5.1512. [DOI] [PubMed] [Google Scholar]
- 60.Fisher JD, Krikler D, Hallidie-Smith KA. Familial polymorphic ventricular arrhythmias: A quarter century of successful medical treatment based on serial exercise-pharmacologic testing. J Am Coll Cardiol. 1999;34:2015–22. doi: 10.1016/s0735-1097(99)00438-6. [DOI] [PubMed] [Google Scholar]
- 61.Lahat H, Eldar M, Levy-Nissenbaum E, et al. Autosomal recessive catecholamine- or exercise-induced polymorphic ventricular tachycardia: Clinical features and assignment of the disease gene to chromosome 1p13–21. Circulation. 2001;103:2822–7. doi: 10.1161/01.cir.103.23.2822. [DOI] [PubMed] [Google Scholar]
- 62.Wennevold A, Melchior JC, Sandoe E. Adams-Stokes syndrome in children without organic heart disease: Electrocardiogram after exercise as a diagnostic tool. Acta Med Scand. 1965;177:557–63. doi: 10.1111/j.0954-6820.1965.tb01863.x. [DOI] [PubMed] [Google Scholar]
- 63.Horan M, Venables AW. Paroxysmal tachycardia with episodic unconsciousness. Arch Dis Child. 1962;37:82–5. doi: 10.1136/adc.37.191.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Reid DS, Tynan M, Braidwood L, Fitzgerald GR. Bidirectional tachycardia in a child. A study using His bundle electrography. Br Heart J. 1975;37:339–44. doi: 10.1136/hrt.37.3.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Coumel P, Fidelle J, Lucet V, Attuel P, Bouvrain Y. Catecholamine-induced severe ventricular arrhythmias with Adams-Stokes syndrome in children: Report of four cases. Br Heart J. 1978;40(Suppl):28–37. [Google Scholar]
- 66.Nakajima T, Kaneko Y, Taniguchi Y, et al. The mechanism of catecholaminergic polymorphic ventricular tachycardia may be triggered activity due to delayed afterdepolarization. Eur Heart J. 1997;18:530–1. doi: 10.1093/oxfordjournals.eurheartj.a015281. [DOI] [PubMed] [Google Scholar]
- 67.Swan H, Piippo K, Viitasalo M, et al. Arrhythmic disorder mapped to chromosome 1q42–q43 causes malignant polymorphic ventricular tachycardia in structurally normal hearts. J Am Coll Cardiol. 1999;34:2035–42. doi: 10.1016/s0735-1097(99)00461-1. [DOI] [PubMed] [Google Scholar]
- 68.Tiso N, Stephan DA, Nava A, et al. Identification of mutations in the cardiac ryanodine receptor gene in families affected with arrhythmogenic right ventricular cardiomyopathy type 2 (ARVD2) Hum Mol Genet. 2001;10:189–94. doi: 10.1093/hmg/10.3.189. [DOI] [PubMed] [Google Scholar]
- 69.Priori SG, Napolitano C, Memmi M, et al. Clinical and molecular characterization of patients with catecholaminergic polymorphic ventricular tachycardia. Circulation. 2002;106:69–74. doi: 10.1161/01.cir.0000020013.73106.d8. [DOI] [PubMed] [Google Scholar]
- 70.Bauce B, Rampazzo A, Basso C, et al. Screening for ryanodine receptor type 2 mutations in families with effort-induced polymorphic ventricular arrhythmias and sudden death: Early diagnosis of asymptomatic carriers. J Am Coll Cardiol. 2002;40:341–9. doi: 10.1016/s0735-1097(02)01946-0. [DOI] [PubMed] [Google Scholar]
- 71.Marx SO, Reiken S, Hisamatsu Y, et al. PKA phosphorylation dissociates FKBP12.6 from the calcium release channel (ryanodine receptor): Defective regulation in failing hearts. Cell. 2000;101:365–76. doi: 10.1016/s0092-8674(00)80847-8. [DOI] [PubMed] [Google Scholar]
- 72.Hunt DJ, Jones PP, Wang R, et al. K201 (JTV519) suppresses spontaneous Ca2+ release and [3H]ryanodine binding to RyR2 irrespective of FKBP12.6 association. Biochem J. 2007;404:431–8. doi: 10.1042/BJ20070135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Priori SG, Napolitano C. Intracellular calcium handling dysfunction and arrhythmogenesis: A new challenge for the electrophysiologist. Circ Res. 2005;97:1077–9. doi: 10.1161/01.RES.0000194556.41865.e2. [DOI] [PubMed] [Google Scholar]