Abstract
BACKGROUND:
Coronary artery disease (CAD) remains the number one killer in the western world. Genetics accounts for greater than 50% of the risk for CAD. Genetic screening and early prevention in individuals identified as being at increased risk could dramatically reduce the prevalence of CAD, thus necessitating the identification of genes predisposing to CAD. Studies of genes identified by the candidate gene approach have not been replicated due, in part, to inadequate sample size. Genome-wide scan association studies have been limited by the use of thousands of markers rather than the hundreds of thousands required, and by the use of hundreds of individuals rather than the thousands required. Replication of positive findings in an independent population is essential. To detect a minor allele frequency of 5% or greater with an odds ratio for risk of 1.3 or greater and 90% power, an estimated 14,000 (9000 affected and 5000 control) subjects are required.
METHODS:
The Affymetrix GeneChip Human Mapping 500K Array Set (Affymetrix Inc, USA) provides a marker every 6000 base pairs as required, and is being used to genotype 1000 cases of premature CAD and 1000 normal subjects, followed by replication in 8000 affected individuals and 4000 control subjects. The phenotype is confirmed or excluded by coronary arteriograms by catheterization or multislice computed tomography.
RESULTS:
Since 2005, more than 800 million genotypes have been performed and analyses performed on 500 control subjects and 500 affected individuals. Several thousand significant single nucleotide polymorphisms and 130 clusters associated with CAD have been identified.
CONCLUSIONS:
This is the first genome-wide scan using the 500,000 marker set in a case-control association study for CAD genes. Several genes associated with CAD appear promising.
Keywords: Cardiovascular genes, Coronary artery disease, Genetics, Genome-wide scan
Abstract
CONTEXTE :
Les coronaropathies (CP) constituent la principale cause de mortalité dans le monde occidental, et le patrimoine génétique représente plus de 50 % du risque de CP. Le dépistage génétique et la prévention précoce chez les personnes reconnues comme étant à risque élevé pourraient diminuer considérablement la prévalence des CP, mais, pour ce faire, il faut d’abord découvrir les gènes prédisposants. Les études géniques fondées sur l’examen des gènes candidats n’ont pas été reproduites pour cause, en partie, de la taille inadéquate des échantillons. Les études collectives sur l’ensemble du génome ont été limitées par le nombre insuffisant de marqueurs, soit des milliers au lieu des centaines de milliers nécessaires, et le nombre insuffisant d’individus, soit des centaines au lieu des milliers nécessaires. Pourtant, il est essentiel de reproduire les résultats positifs dans une population indépendante. Pour détecter un allèle d’importance secondaire ayant une fréquence d’au moins 5 %, un risque relatif indirect égal ou supérieur à 1,3 et une puissance de 90 %, il faut examiner environ 14 000 sujets (9000 personnes touchées; 5000 témoins).
MÉTHODE :
Les jeux de puces Affymetrix GeneChip Human Mapping 500K Array Set (Affymetrix Inc., É.-U.) fournissent un marqueur pour chacune des 6000 paires de bases, comme l’exigent les besoins de la recherche; ils servent au génotypage de 1000 cas de CP précoce et de 1000 témoins normaux, puis à la reproduction des résultats chez 8000 personnes touchées et 4000 témoins. Le phénotype est confirmé ou infirmé par une coronarographie par cathétérisme ou par une tomodensitométrie multicoupe.
RÉSULTATS :
Depuis 2005, on a effectué plus de 800 milliards de typages géniques et d’analyses chez 500 témoins et 500 personnes touchées. Plusieurs milliers de polymorphismes de nucléotides simples, importants et 130 familles associées aux CP ont été identifiés.
CONCLUSION :
Il s’agit là de la première analyse de l’ensemble du génome réalisée à l’aide d’un jeu de 500 000 marqueurs, dans une étude collective cas/témoins, à la recherche des gènes responsables des CP. L’identification de plusieurs gènes associés aux CP semble prometteuse.
The 21st century ushers in a new era. The potential to understand and treat disease based on a specific etiological molecule or its molecular pathogenesis exceeds anything we have known. The blueprint for life, namely, the human genome DNA sequence, was available in draft form in 2000, and has now been completed and verified. It is estimated that humans have between 20,000 and 25,000 genes, which, with any luck, will be identified over the next 10 years, with their roles in health and disease simultaneously determined. This achievement has such vast implications for the future of mankind, it is worthy of comparison to great epochs that have shaped our civilization. One, of course, is the development of the Phoenician alphabet and the addition of the vowels by the Greeks, which greatly facilitated the transition from the spoken to the written word and the documentation of Western philosophy and democracy (1). Another analogy may be the development of the periodic table at the beginning of the 20th century, which indirectly contributed to putting the first man on the moon. Completion of the DNA sequence of the human genome provides a giant leap forward, whereby it will be possible to sequence all of the genes that lead to the development of a human being and, in turn, to provide a molecular genetic basis for the fragility of mankind and its vulnerability to disease.
A GENETIC SUCCESS: IDENTIFYING GENES FOR SINGLE GENE DISORDERS
The application of molecular genetics to inherited cardiovascular disorders has met with great success (2,3), particularly in the field of single gene disorders. A single gene disorder is defined as one in which a single gene is both adequate and sufficient to induce the phenotype. It is estimated that there are 6000 single gene disorders, of which more than 2000 have been identified. The first gene identified in cardiology for a single gene disorder was that for hypertrophic cardiomyopathy (4), followed by multiple other genes for the cardiomyopathies (2), and genes for the long QT syndrome (5), Wolff-Parkinson-White syndrome (6,7), Brugada syndrome (7,8), atrial fibrillation (9,10) and others (11,7). There are more than 1200 mutations recognized to be responsible for single gene disorders that induce cardiovascular disease.
The phenotypes of single gene disorders exhibit specific patterns, such as autosomal dominant or autosomal recessive. The approach to identifying the gene responsible for these disorders is to collect a pedigree of two or three generations with preferably 10 or more affected individuals. The pedigree is genotyped with 300 DNA markers (markers of known chromosomal location) selected to span the human genome at intervals averaging 10,000,000 base pairs (bps). Analysis is performed to determine whether one or more of the DNA markers is inherited more frequently than by chance in the affected individuals, which would indicate that the marker segregates with the phenotype. Segregation indicates that the gene and the marker are genetically linked, meaning that the gene is on the same chromosome, and in such close physical proximity to the marker, they are always coinherited. Thus, knowing the chromosomal location (locus) of the DNA marker provides an approximate chromosomal position of the responsible gene. Once the locus is mapped, refined mapping can be performed to narrow the region, enabling one to clone and sequence the gene to identify the responsible mutation (11,12). This is an ongoing and exciting area of research. While single gene disorders are rare, most with a prevalence of less than 0.1%, they serve as paradigms to understanding acquired disease. Animal models of these diseases, generated by the insertion of the human mutant gene into the pronucleus of the recipient so that it is transmitted to subsequent offspring, have facilitated the development of novel therapies. Studies of familial hypercholesterolemia (HCM) led to the development of statins, the main treatment today for both acquired and familial HCM (13). The recent identification of genes responsible for HCM and the generation of transgenic animal models have shown that the phenotype can be reversed with angiotensin II blockers (14), statins (15) and aldosterone inhibitors (16) and, more recently, have shown to be preventable by the early administration of statins (17). These therapies have yet to be assessed for efficacy in humans. Nevertheless, they show great promise as the first potential therapy for the leading cause of sudden cardiac death in young adults.
RATIONALE TO EXPLORE THE GENETICS OF CARDIOVASCULAR DISEASE
Diseases of the cardiovascular system are the leading cause of morbidity and mortality in the developed world and are predicted to overtake infectious disease as the predominant cause of mortality worldwide (18). It is claimed that 49% of all deaths in Europe are due to cardiovascular disease (19–21). The high prevalence of heart disease is related primarily to coronary artery disease (CAD), which is associated with multiple risk factors: obesity, diabetes, smoking, hypertension, poor diet and an increasingly aging population (18,22). It is also well recognized that over one-half of patients with the clinical manifestations of CAD do not exhibit any of the traditional risk factors (23). The major pathological component of CAD is atherosclerosis, a generalized vascular disease that affects all organs but whose sequelae are more prevalent and devastating for organs such as the heart and the brain. Increasing evidence in recent decades suggests that CAD is preventable and may be markedly attenuated, if not eliminated, in this century (22,24).
Secondary prevention in multiple clinical trials (22) has shown a 20% to 30% reduction in morbidity and mortality by treating major risk factors. The major risk factors for CAD result from the interaction of environmental and genetic risk factors. While it remains to be determined what proportion of risk is due to genetic versus environmental factors, epidemiological studies (25) suggest over 50% of risk for CAD is due to genetic predisposition. It is evident from most of the risk factors, such as hyperlipidemia, hypertension and diabetes, that there is a major genetic component. Thus, if one is to provide comprehensive prevention, it will be necessary to identify genetic risk factors, as well as internal and external environmental factors. In addition, the identification of risk factors is expected to lead to targets that will provide more specific and novel therapy.
Secondary prevention following a myocardial infarction, while effective, is far from adequate from a public health viewpoint. Sudden cardiac death (SCD) accounts for most of the deaths from heart disease, and inherent in the problem is the need for novel therapy, but SCD will probably necessitate prevention to be effective. It is well recognized that essentially all SCDs occurring in individuals younger than 36 years are due to genetic causes, with familial HCM accounting for greater than 40% of the deaths (7). Furthermore, most of these patients are asymptomatic, with SCD being their first and only symptom. Genetic screening to select for prophylactic implantable cardioverter-defibrillator placement or medical therapy is self-evident. In adults older than 36 years, the predominant cause of SCD is CAD. Each year, more than 400,000 people die from SCD in the United States and 40,000 die in Canada (26,27). It is noteworthy that these numbers have not changed in the past three decades, in part because most die suddenly within hours of symptoms, before therapy can be accessed. Heart failure, the most common cardiac diagnosis, is associated with SCD in over 50% of patients (26). Prevention is the only hope for these individuals. It is evident that individuals screened at an early age and found to have a genetic predisposition would benefit most from preventive strategies. Thus, it is important to identify the genetic modifiers and to determine their function; only then can more appropriate and comprehensive therapies be developed. Genetic evaluation of individuals with CAD should enable physicians to individualize comprehensive preventive strategies, including therapy. The choice of therapy and dose of medication for CAD will be determined, in part, by the individual’s genome. Within the next decade, cardiac therapy will be personalized largely on the basis of the individual’s genomic variants. It is likely that the genome has other hidden secrets to be exploited in the treatment of this pandemic disease. The role of individual genomic variants in the screening, prevention and treatment of CAD is yet to be elucidated.
REASONS FOR THE DELAY IN IDENTIFYING GENES FOR COMMON DISEASES, SUCH AS CAD
Remarkable progress has been made using the techniques of modern molecular genetics in the area of single gene disorders (2,3). Common diseases, such as CAD, have remained elusive to the pursuit of genetic predisposition. This is primarily because genetic predisposition is carried by several genes rather than a predominant single gene. CAD, due primarily to atherosclerosis, and its resulting clinical sequelae involve several biochemical processes, including lipid metabolism, inflammatory responses, endothelial function, coagulation and blood pressure. Genetic factors that contribute to CAD are prevalent in the population but are of low penetrance (28). However, elucidating the genetic determinants of CAD remain problematic, partly because of the multiple genes involved and, more importantly, it appears each gene contributes only a minor effect to the ultimate phenotype (Table 1). Although copy number polymorphisms – including deletions, duplications and inversions – may comprise up to 10% of the genetic variability among humans (29), the difference in the DNA sequence of the genome among humans is less than 0.1%, most of which is due to single nucleotide polymorphisms (SNPs). SNPs are mutations that occur as single nucleotide substitutions or deletions at a frequency of one in 1000 bps throughout the human genome. It is believed that most human variation and susceptibility to disease is due to these SNPs (Table 2). It is anticipated that each SNP responsible may contribute only 5% to 10% of the susceptibility to the CAD phenotype. Thus, in multigene disorders, no single gene is necessary or sufficient to induce the phenotype. This is in marked contrast to single gene disorders, in which a single gene is both necessary and sufficient to induce the phenotype. Genome-wide genotyping of these polygenic disorders to detect a gene with minimal effect requires a marker at intervals of at least every 6000 bps compared with only 10,000,000 bps for single gene disorders (30). This would require the DNA sample from each individual to be genotyped for 500,000 markers and, furthermore, would require several thousand patients. Until recently, such high-throughput genotyping and phenotyping was prohibitive.
TABLE 1.
Identifying the genes responsible for coronary artery disease has been prohibitive until recently. Why?
|
TABLE 2.
Individual genetic variation and susceptibility to polygenic diseases
|
RECENT AVAILABILITY OF 500,000 SNP CASSETTE ENABLES GENOME-WIDE GENOTYPING FOR CASE-CONTROL ASSOCIATION STUDIES
For single gene disorders, families are collected and analysis for a genetic linkage between a DNA marker and the responsible gene is performed. Linkage analysis is unlikely to have the power or sensitivity to detect genes contributing minimal risk. It has been realized for some time that case-control association studies would be more appropriate and sensitive to detect genes responsible for common polygenic disorders, such as CAD. This technique can be implemented by two approaches: the candidate gene approach, commonly referred to as the direct approach; and the indirect approach, requiring genome-wide genotyping (Table 3). Both techniques require analysis of unrelated individuals as opposed to families. The underlying principle of both approaches is to compare the SNP frequency in control subjects with that in affected individuals. In the direct candidate gene approach, the frequency of a particular SNP in a candidate gene, selected on the basis of its function, in control subjects is compared with that in affected individuals. There have been hundreds of publications (30–32) assessing genetic predisposition to CAD using the candidate gene approach. However, either because of an inadequate sample size or lack of replication in an independent population, none of these studies have provided robust candidates that can be used in the clinical management of CAD (31,33). It is now recognized that genome-wide genotyping for an association provides greater sensitivity and is the preferred method. This is an unprejudiced approach that makes no presumptions and is all-inclusive. Several studies (31,32) have been performed using 50,000 to 100,000 markers. Very little reliable data have been obtained, in part because 100,000 markers probably provides inadequate genome coverage and the sample size has been in the hundreds, rather than the thousands required (31,33). Nevertheless, studies using the 50,000 to 100,000 SNPs as markers, such as the one genotyping for low-density lipoprotein phenotypes (34), have provided very promising results.
TABLE 3.
Mapping and identification of genes for common multigene disorders
| Case-control association studies |
|---|
|
The realization that there are SNPs distributed throughout the human genome averaging one SNP per 1000 bps (3,000,000 SNPs per genome) provided the opportunity to use them as markers for dense genome-wide genotyping or ‘scans’. The availability of 500,000 SNPs on a chip, and more recently 1,000,000 SNPs, provides, on average, a marker at intervals of 6000 bps and 3000 bps, respectively. Studies by Hinds et al (30) and the International HapMap Project (35,36) indicate that a minimum of 375,000 properly placed markers are required to genotype an American-European population. The pursuit of such case-control, genome-wide association studies in an African-American population would require at least 475,000 markers. The HapMap database indicates that more than 13,000,000 SNPs have been identified in the general population, with each individual having approximately 3,000,000. Most of these SNPs have a frequency of less than 1%, which would make detection almost impossible. However, the HapMap Project showed that most of the SNPs responsible for human individual variation, which should include susceptibility to disease, is due to SNPs that occur at a frequency of 5% or greater. The following sections discuss the evidence for genetic predisposition to CAD, calculation of the sample size for genome-wide genotyping with the Affymetrix GeneChip Human Mapping 500K Array Set (Affymetrix Inc, USA) and progress to date in the first ongoing study, the Ottawa Heart Genomic Study (University of Ottawa Heart Institute, Ottawa, Ontario [95]), using the 500,000 marker set to identify genes contributing to CAD.
GENETIC BASIS FOR CAD
Familial aggregation studies
Studies investigating case-control families (37–41) have shown, on average, a two- to threefold increase in risk for CAD in first-degree relatives of affected individuals. The extent of coronary occlusion in patients with CAD also relates to a parental history of myocardial infarction (42). The earlier the age of onset of CAD in a particular individual, the greater the risk of relatives developing CAD (40). In families with CAD onset before age 46, heritability was estimated to be 92% to 100%, whereas in families of older cases, the heritability ranged from 15% to 30% (41). It is also of note that the risk of disease is typically several times greater in relatives of female cases than in relatives of male cases (40,41). Premature CAD in the young reflects a multi-hit genetic inheritance, and these individuals transmit an even greater genetic load to their offspring (43). The Danish twin registry, which includes more than 8000 twin pairs, showed a higher incidence of CAD and deaths in monozygotic twins than in dizygotic twins (44% versus 14% [44]). Other registry data from Sweden and Norway showed similar concordance rates for fatal and nonfatal CAD (45–51).
Genetic-induced animal models of atherosclerosis
Atherosclerosis has been extensively studied by crossbreeding in mouse models, and the results indicate a strong genetic component to atherosclerosis (52). The apolipoprotein E knockout mouse, in which susceptibility to CAD is markedly increased, is much more vulnerable to a diet high in cholesterol (53). Expression in this mouse of human genes and polymorphisms known to increase susceptibility to CAD have been shown to induce a phenotype of increased CAD (53).
Case-control studies using the candidate gene approach
As indicated above, while association studies have been suggestive, they remain suspect because of the small sample size and lack of functional evidence (54). Using the candidate gene approach, investigators have generally selected genes associated with pathways known to be involved in atherosclerosis. Numerous studies have used genes implicated in known risk factors for atherosclerosis, such as hypertension (55,56), obesity (57–63) and diabetes (33,64–68).
Mendelian inheritance of atherosclerosis
In certain families with severe premature CAD, there appears to be a predominant gene, and the phenotype is inherited as an autosomal or recessive trait. Linkage analysis has been performed and several chromosomal loci have been linked to chromosome regions 2q21, Xq23 (69), 1p34 (70), 16p13, 14qter (71) and 15q26 (72). The gene at chromosome region 15q26 has been identified as MEF-2A, which has a small deletion (72). Other investigators have not been able to confirm MEF-2A and conclude that it is benign, showing it occurs in normal individuals (73). Several other chromosomal loci have been identified that associate with known risk factors for CAD, such as hyperlipidemia, hypertension, homocysteine defects and diabetes.
Premature CAD is a genetic disease
The onset of CAD before the age of 50 years occurs in approximately 10% of individuals with this disease (18,74). Myocardial infarction occurring in a first-degree relative before the age of 55 years is said to increase the risk of myocardial infarction by 7.1-fold. The present study estimated the heritability for early-onset of CAD at 0.63; after the exclusion of apparent lipid abnormalities, the heritability estimate was 0.56, suggesting that more than one-half of CAD cases diagnosed before the age of 55 years are genetic.
Family history is highly predictive of CAD
A family history of CAD in a first-degree relative before the age of 60 years is an independent risk factor for early myocardial infarction, even after controlling for traditional risk factors (75,76). Several prospective studies (77–82) have shown up to a twofold increase in CAD risk associated with a family history of CAD after adjusting for traditional risk factors. There is also a clustering of susceptibility to CAD in families that have risk factors (eg, abnormalities of lipid metabolism, hypertension, diabetes or obesity), indicating a genetic basis for these conditions and risk factors (83–89). A family history of CAD is also an independent risk factor for angiographic documented CAD (42,90). In Utah, 14% of the population has a family history of CAD, which accounts for 72% of early CAD cases (younger than 50 years) and 48% of all CAD events at any age. Similarly, 11% of the Utah population has a family history of stroke, which accounts for 86% of all early strokes (91). In the Framingham study (80), a family history of CAD, cerebral vascular accidents or peripheral arterial disease was associated with a 2.4-fold increased risk of CAD in men and a 2.2-fold increased risk in women. In the Interheart study (92), having a family history of CAD resulted in a 1.55-fold increased risk, and after correction for other risk factors, a 1.45-fold increased risk. In the Prospective Cardiovascular Münster (PROCAM) study (93), a family history of myocardial infarction was an independent risk factor for CAD.
PRINCIPLES UNDERLYING CASE-CONTROL, ASSOCIATION, GENOME-WIDE STUDIES
A new era has emerged with the availability of the Affymetrix 500K and 1,000K gene chips (Affymetrix Inc, USA) (Figure 1). These marker sets enable rapid genotyping of the whole genome in large sample sizes. It is worth noting that of the 3,000,000 SNPs present in humans, it is anticipated that only approximately 20,000 to 40,000 are located in protein or RNA coding regions (35). Another 20,000 to 40,000 are in conserved, noncoding regions that may alter the DNA binding elements for promoters and, thus, alter gene transcription and protein function. Thus, most of these SNPs are benign, and use of the 500K and 1,000K gene chips is primarily as DNA markers, which are hoped to be in close proximity to SNPs that contribute to CAD susceptibility. The 500K or 1,000K marker set is selected to detect or be in disequilibrium with most of the common SNPs (frequency of 5% or greater) that occur in the human genome (30–32,94). The overall principle is to genotype unrelated individuals (affected individuals and control subjects) to compare the frequency of the SNPs in control subjects with the frequency in individuals affected with CAD in an initial population. Those chromosomal regions showing an association with CAD would be genotyped in an independent population to determine whether there was replication. Replication is absolutely essential in at least one or more independent populations. In the initial population, because 500,000 markers are being used, 25,000 associations are expected by chance alone at P=0.05, 5000 associations at P=0.01 and 50 associations at P=0.001. To avoid false-positive results in the replication population, it is preferable to have a larger sample size so that a more stringent P value for association may be selected.
Figure 1).
The Affymetrix GeneChip Human Mapping 500K Array Set (Affymetrix Inc, USA). Each chip comprises 250,000 single nucleotide polymorphisms (SNPs), and together, they comprise the 500,000 SNPs that scan the human genome at an interval of 6000 base pairs
CALCULATION OF SAMPLE SIZE TO PURSUE GENES FOR CAD USING THE CASE-CONTROL, ASSOCIATION, GENOME-WIDE APPROACH
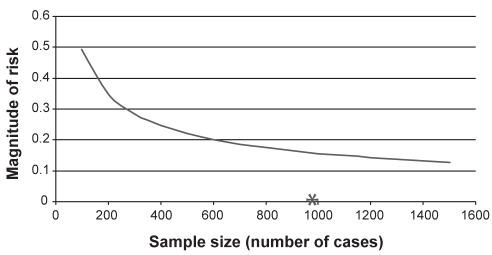
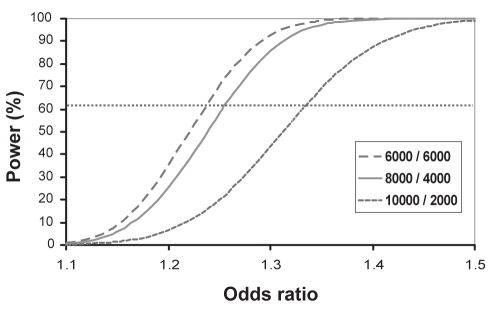
Several parameters must be selected before estimating the sample size, as indicated in Table 4. First, it is reasonable to assume that any gene that increases the risk for CAD by 30% or more over that of control subjects would be clinically significant. Risk factors currently identified increase risk by at least onefold (32). Second, it would be reasonable to power the study to detect alleles with a minor allele frequency of 5% or greater because, as indicated previously, these are predominantly alleles expected to contribute to CAD susceptibility (32). Third, to obtain high sensitivity, the study should be powered to detect a size difference between control subjects and affected individuals of 0.2 or greater. Thus, sample size was calculated assuming 90% power, a minor allele frequency of 5% or greater, an odds ratio of 1.3 or greater, and a 0.2 or greater size difference between control subjects and affected individuals. The initial population, estimated at 2000 individuals (1000 affected individuals and 1000 control subjects), would be genotyped with the 500,000 marker set to detect associations at P≤0.001 (Figure 2). This population would then be genotyped with 500,000 SNPs as markers to detect those showing a significant association with the phenotype. Those markers showing an association (P=0.001) in the initial population would be genotyped in a second independent population to ascertain the degree of replication. It was estimated that a second sample size of 12,000 (8000 affected individuals and 4000 control subjects) would provide the power necessary to detect SNPs showing stronger associations at P≤10−6 (Figure 3). It may be helpful and necessary to genotype additional SNPs customized to the regions of those SNPs showing an association to detect the actual causative gene. This is an unbiased approach without any prior assumptions to identify genetic variants that contribute as little as 5% to the overall phenotype. These studies are now possible, and it is expected that several such studies will soon be pursued to unravel the genetic variants of many common polygenic disorders, such as CAD, hypertension, obesity and diabetes. One such study is the Ottawa Heart Genomics Study (95), which is attempting to identify genes responsible for CAD. To the authors’ knowledge, this is the first study using the 500,000 marker set as a genome-wide scan for CAD detected on coronary arteriography.
TABLE 4.
Parameters used to calculate sample size
|
Figure 2).
Sample size versus magnitude of difference in risk between control subjects and affected cases (P≤0.001). The graph shows the calculation of the sample size to detect a size difference of 0.2. The asterisk indicates that it will require 1000 patients in the control group and 1000 patients in the affected group based on a minor allele frequency of 5% and a minimum P value of 0.001
Figure 3).
Calculation of sample size using a minor allele frequency of 1.3 or greater at a power of 90% to map genetic loci associated with coronary artery disease (P≤0.000001). This analysis was the same as that in phase I but with a more stringent P value for association
THE CANADIAN CARDIOVASCULAR GENETICS CENTRE AND THE OTTAWA HEART GENOMICS STUDY
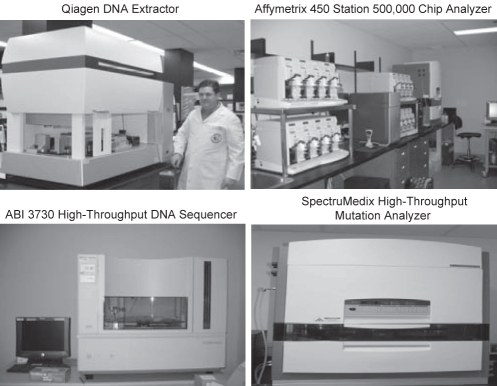
In 2004, the Canadian Cardiovascular Genetics Centre was established at the University of Ottawa Heart Institute. The centre is dedicated to the pursuit of genes responsible for cardiovascular disease. The emphasis is on identifying genes responsible for CAD, as well as genes responsible for arrhythmias, SCD and familial cardiomyopathies. It is equipped with the latest equipment for high-throughput DNA extraction, high-throughput genotyping, including SNP detection with the Affymetrix platform (GeneChip Fluidics 450 station, Affymetrix Inc, USA) using the 500,000 chip for genome-wide scans (Figure 4). The centre currently has the capacity to perform 48 million genotypes per day and the sequencing power of approximately one million bases per day. The sequencing capacity will soon be markedly increased with the acquisition of a G20–454 Roche sequencer (Roche Applied Science, Canada), which has the capacity to sequence up to 20 million bases per day. In 2005, the Institute also acquired a 64-slice, fast computed tomography (CT) scanner to perform noninvasive coronary angiograms. This technique, along with the Institute’s four existing catheterization laboratories, performs more than 10,000 angiograms per year, which provides the necessary high-throughput phenotyping (Figure 5). The Institute, which serves a population of 1.8 million, currently has more than 100,000 coronary angiograms from individuals followed in the Institute’s outpatient clinics (Figure 6). The Ottawa Heart Genomics Study, which is pursuing genome-wide, case-control association studies to identify genes responsible for CAD, was initiated in August 2005 using the 500,000 marker set scan. The sample size (Table 5), based on the estimates discussed in the previous section, consists of 14,000 individuals (9000 affected individuals and 5000 control subjects). The initial phase consisting of 2000 subjects (1000 affected individuals and 1000 control subjects) will be genotyped with the 500,000 SNPs and will include one billion genotypes. The designation of subjects as being affected with the CAD phenotype is based on 50% or more coronary obstruction as determined by coronary angiography performed either by cardiac catheterization or noninvasively by 64-slice, fast CT. The affected individuals are selected to enrich for genetic predisposition by including only men younger than 55 years and women younger than 65 years (Table 6). The control subjects are asymptomatic with normal coronary angiograms, as determined by cardiac catheterization or 64-slice, fast CT (Table 7).
Figure 4).
The images show the equipment for high-throughput genotyping as established in the Ruddy Canadian Cardiovascular Genetics Centre (University of Ottawa Heart Institute, Ottawa, Ontario). The Qiagen extractor (Qiagen Inc, Canada) is capable of extracting more than 400 DNA samples per day. The Affymetrix GeneChip Fluidics 450 station (Affymetrix Inc, USA) is the platform to analyze the 500,000 chip (Affymetrix GeneChip Human Mapping 500K Array Set, Affymetrix Inc, USA). Four of these setups make it possible to genotype roughly 20 million genotypes per day. The ABI 3730 (Applied Biosystems, USA) provides DNA sequencing power of one million bases per day. The SpectruMedix LLC (SpectruMedix, USA) is used in known mutations and contains 96 wells that can be analyzed within a few hours
Figure 5).
The figure shows the new, noninvasive, 64-slice fast computed tomography scanner for performing coronary angiograms. It requires approximately 45 s to image the coronary arteries and a total time of approximately 20 min from entry of the patient until completion. This makes it possible to perform coronary angiograms on asymptomatic control subjects
Figure 6).
The circled areas on the map indicate the population of the city of Ottawa, Champlain Region and Baffin Island served by the University of Ottawa Heart Institute, Ottawa, Ontario
TABLE 5.
Demographics of the Ottawa Heart Genomics Study sample
| Total sample size | 14,000 (9000 affected individuals, 5000 control subjects) |
| Sample size for screening | 2000 (1000 affected individuals, 1000 control subjects) |
| Sample size for replication | 12,000 (8000 affected individuals, 4000 control subjects) |
TABLE 6.
Criteria for diagnosis of premature coronary artery disease (CAD)
|
TABLE 7.
Criteria of control subjects without coronary artery disease
|
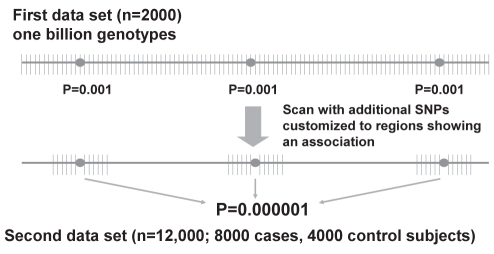
More than 800 million genotypes have been completed on 1600 individuals, and phase I (n=2000) is soon expected to be completed. Unfiltered analysis of the first 500 control subjects and 500 affected individuals indicates several thousand SNPs with associations significant at P≤0.001 and more than 130 clusters with P values ranging from 10−3 to 10−12. Analysis will be performed in the second population (n=12,000) to determine replication, coupled with further customized SNP genotyping as shown in Figure 7. However, it is recognized that many of these associations are false-positives and are not expected to be confirmed in the replication analysis.
Figure 7).
Case-control association study two-stage analysis. Shown here is the overall approach of the two-stage analysis. The first data set of 2000 is genotyped with the Affymetrix GeneChip Human Mapping 500K Array Set (Affymetrix Inc, USA). Each sample undergoes genotyping with the 500,000 marker set for a total of one billion genotypes. Those regions showing an association significant at P≤0.001 are taken forward and genotyped in the greater population of 12,000 to ascertain replication. In addition, customized single nucleotide polymorphisms (SNPs) are genotyped for each regional significant SNP
Completion of the initial phase provides for a well phenotyped and genotyped population with an all-inclusive set of SNPs exhibiting strong associations to the CAD phenotype. It will require extensive efforts to confirm or exclude these genes as causative and it is the authors’ hope to obtain collaboration with several other investigators in Canada and other countries to identify and functionally analyze the genes contributing the most risk for CAD. It is a unique opportunity to provide the armamentarium for comprehensive genetic screening and prevention of the world’s number one killer. Subsequent to completing the replication studies, it will be possible to compare these genes to those in specific risk cohorts, such as hypertension, obesity and hyperlipidemia.
Acknowledgments
The assistance of Fran Baas, Susan Slater and Kimberley Allen on the preparation of this manuscript was greatly appreciated.
Footnotes
FUNDING: This work is supported by grants from the National Heart, Lung and Blood Institute (SCOR – RFA-HL-98-007), Specialized Centers of Research, the National Institutes of Health Training Center in Molecular Cardiology (HL07706-09), Canadian Institutes of Health Research (IGI-94947), (145322), (MOP-44360), Heart and Stroke Foundation of Ontario (NA-5413) and the Canadian Foundation for Innovation (11966).
REFERENCES
- 1.Van Doren C. A History of Knowledge. New York: Ballentine Books; 1991. [Google Scholar]
- 2.Marian AJ, Roberts R. The molecular genetic basis for hypertrophic cardiomyopathy. J Mol Cell Cardiol. 2001;33:655–70. doi: 10.1006/jmcc.2001.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geisterfer-Lowrance AA, Christe M, Conner DA, et al. A mouse model of familial hypertrophic cardiomyopathy. Science. 1996;272:731–4. doi: 10.1126/science.272.5262.731. [DOI] [PubMed] [Google Scholar]
- 4.Geisterfer-Lowrance AA, Kass S, Tanigawa G, et al. A molecular basis for familial hypertrophic cardiomyopathy: A beta cardiac myosium heavy chain gene missense mutation. Cell. 1990;62:999–1006. doi: 10.1016/0092-8674(90)90274-i. [DOI] [PubMed] [Google Scholar]
- 5.Keating M, Atkinson D, Dunn C, Timothy K, Vincent GM, Leppert M. Linkage of a cardiac arrhythmia, the long QT syndrome, and the Harvey ras-1 gene. Science. 1991;252:704–6. doi: 10.1126/science.1673802. [DOI] [PubMed] [Google Scholar]
- 6.Gollob MH, Green MS, Tang AS, et al. Identification of a gene responsible for familial Wolff-Parkinson-White syndrome N Engl J Med 20013441823–31.(Errata in 2001;345:552 and 2002;346:300) [DOI] [PubMed] [Google Scholar]
- 7.Roberts R. Genomics and cardiac arrhythmias. J Am Coll Cardiol. 2006;47:9–21. doi: 10.1016/j.jacc.2005.08.059. [DOI] [PubMed] [Google Scholar]
- 8.Brugada R, Roberts R. Brugada syndrome: Why are there multiple answers to a simple question? Circulation. 2001;104:3017–9. [PubMed] [Google Scholar]
- 9.Gollob MH, Jones DL, Krahn AD, et al. Somatic mutations in the connexin 40 gene (GJA5) in atrial fibrillation. N Engl J Med. 2006;354:2677–88. doi: 10.1056/NEJMoa052800. [DOI] [PubMed] [Google Scholar]
- 10.Brugada R, Tapscott T, Czernuszewicz GZ, et al. Identification of a genetic locus for familial atrial fibrillation. N Engl J Med. 1997;336:905–11. doi: 10.1056/NEJM199703273361302. [DOI] [PubMed] [Google Scholar]
- 11.Roberts R. Mechanisms of disease: Genetic mechanisms of atrial fibrillation. Nat Clin Pract Cardiovasc Med. 2006;3:276–82. doi: 10.1038/ncpcardio0509. [DOI] [PubMed] [Google Scholar]
- 12.Roberts R, Gollob M. Molecular cardiology and genetics in the 21st century – a primer. Curr Probl Cardiol. 2006;31:637–701. doi: 10.1016/j.cpcardiol.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 13.Brown MS, Goldstein JL. A receptor-mediated pathway for cholesterol homeostasis. Science. 1986;232:34–47. doi: 10.1126/science.3513311. [DOI] [PubMed] [Google Scholar]
- 14.Lim DS, Lutucuta S, Bachireddy P, et al. Angiotensin II blockade reverses myocardial fibrosis in a transgenic mouse model of human hypertrophic cardiomyopathy. Circulation. 2001;103:789–91. doi: 10.1161/01.cir.103.6.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patel R, Nagueh SF, Tsybouleva N, et al. Simvastatin induces regression of cardiac hypertrophy and fibrosis and improves cardiac function in a transgenic rabbit model of human hypertrophic cardiomyopathy. Circulation. 2001;104:317–24. doi: 10.1161/hc2801.094031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsybouleva N, Zhang L, Chen S, et al. Aldosterone, through novel signaling proteins, is a fundamental molecular bridge between the genetic defect and the cardiac phenotype of hypertrophic cardiomyopathy. Circulation. 2004;109:1284–91. doi: 10.1161/01.CIR.0000121426.43044.2B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Senthil V, Chen SN, Tsybouleva N, et al. Prevention of cardiac hypertrophy by atorvastatin in a transgenic rabbit model of human hypertrophic cardiomyopathy. Circ Res. 2005;97:285–92. doi: 10.1161/01.RES.0000177090.07296.ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Heart Association . Dallas: American Heart Association; 2000. 2000 Heart and Stroke Statistical Update. [Google Scholar]
- 19.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349:1436–42. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 20.De Backer G, Ambrosioni E, Borch-Johnsen K, et al. European Society of Cardiology American Heart Association. American College of Cardiology. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts) Atherosclerosis. 2004;173:381–91. [PubMed] [Google Scholar]
- 21.Goodacre S, Cross E, Arnold J, Angelini K, Capewell S, Nicholl J. The health care burden of acute chest pain. Heart. 2005;91:229–30. doi: 10.1136/hrt.2003.027599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wald NJ, Law MR.A strategy to reduce cardiovascular disease by more than 80% BMJ 20033261419(Errata in 2003;327:586 and 2006;60:823) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.EUROASPIRE II Study Group Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries; principal results from EUROASPIRE II Euro Heart Survey Programme. Eur Heart J. 2001;22:554–72. doi: 10.1053/euhj.2001.2610. [DOI] [PubMed] [Google Scholar]
- 24.Yusuf S, Hawken S, Ounpuu S, et al. INTERHEART Study Investigators Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 25.Chan L, Boerwinkle E. Gene-environment interactions and gene therapy in atherosclerosis. Cardiol Rev. 1994;2:130–7. [Google Scholar]
- 26.Bristow MR, O’Connell JB. Myocardial diseases. In: Kelley WN, Watanabe AM, editors. Textbook of Internal Medicine. Philadelphia: JB Lippincott; 1992. pp. 150–7. [Google Scholar]
- 27.Zipes DP, Wellens HJ. Sudden cardiac death. Circulation. 1998;98:2334–51. doi: 10.1161/01.cir.98.21.2334. [DOI] [PubMed] [Google Scholar]
- 28.Risch N, Merikangas K. The future of genetic studies of complex human diseases. Science. 1996;273:1516–7. doi: 10.1126/science.273.5281.1516. [DOI] [PubMed] [Google Scholar]
- 29.Redon R, Ishikawa S, Fitch KR, et al. Global variation in copy number in the human genome. Nature. 2006;444:444–54. doi: 10.1038/nature05329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hinds DA, Stuve LL, Nilsen GB, et al. Whole-genome patterns of common DNA variation in three human populations. Science. 2005;307:1072–9. doi: 10.1126/science.1105436. [DOI] [PubMed] [Google Scholar]
- 31.Wang WY, Barratt BJ, Clayton DG, Todd JA. Genome-wide association studies: Theoretical and practical concerns. Nat Rev Genet. 2005;6:109–18. doi: 10.1038/nrg1522. [DOI] [PubMed] [Google Scholar]
- 32.Hirschhorn JN, Daly MJ. Genome-wide association studies for common diseases and complex traits. Nat Rev Genet. 2005;6:95–108. doi: 10.1038/nrg1521. [DOI] [PubMed] [Google Scholar]
- 33.Altshuler D, Hirschhorn JN, Klannemark M, et al. The common PPARgamma Pro12Ala polymorphism is associated with decreased risk of type 2 diabetes. Nat Genet. 2000;26:76–80. doi: 10.1038/79216. [DOI] [PubMed] [Google Scholar]
- 34.Cohen JC, Kiss RS, Pertsemlidis A, Marcel YL, McPherson R, Hobbs HH. Multiple rare alleles contribute to low plasma levels of HDL cholesterol. Science. 2004;305:869–72. doi: 10.1126/science.1099870. [DOI] [PubMed] [Google Scholar]
- 35.The International HapMap Consortium The International HapMap Project. Nature. 2003;426:789–96. doi: 10.1038/nature02168. [DOI] [PubMed] [Google Scholar]
- 36.The International HapMap Consortium A haplotype map of the human genome. Nature. 2005;437:1299–320. doi: 10.1038/nature04226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gertler MM, White PD. Coronary Heart Disease in Young Adults: A Multidisciplinary Study. Cambridge: Harvard University Press; 1954. [Google Scholar]
- 38.Thomas CB, Cohen BH. The familial occurrence of hypertension and coronary artery disease, with observations concerning obesity and diabetes. Ann Intern Med. 1955;42:90–127. doi: 10.7326/0003-4819-42-1-90. [DOI] [PubMed] [Google Scholar]
- 39.Rose G. Familial patterns in ischaemic heart disease. Br J Prev Soc Med. 1964;18:75–80. doi: 10.1136/jech.18.2.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Slack J, Evans KA. The increased risk of death from ischaemic heart disease in first degree relatives of 121 men and 96 women with ischaemic heart disease. J Med Genet. 1966;3:239–57. doi: 10.1136/jmg.3.4.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rissanen AM. Familial occurrence of coronary heart disease: Effect of age at diagnosis. Am J Cardiol. 1979;44:60–6. doi: 10.1016/0002-9149(79)90251-0. [DOI] [PubMed] [Google Scholar]
- 42.Anderson AJ, Loeffler RF, Barboriak JJ, Rimm AA. Occlusive coronary artery disease and parental history of myocardial infarction. Prev Med. 1979;8:419–28. doi: 10.1016/0091-7435(79)90019-7. [DOI] [PubMed] [Google Scholar]
- 43.Falconer DS. The inhertiance of liability to certain diseases, estimated from the incidence among relatives. Ann Hum Genet. 1965;29:51–76. [Google Scholar]
- 44.Allen G, Harvald B, Shields J. Measures of twin concordance. Acta Genet Stat Med. 1967;17:475–81. doi: 10.1159/000152101. [DOI] [PubMed] [Google Scholar]
- 45.Berg K. Twin studies of coronary heart disease and its risk factors. Acta Genet Med Gemellol (Roma) 1987;36:439–53. doi: 10.1017/s0001566000006814. [DOI] [PubMed] [Google Scholar]
- 46.Cederlof R, Friberg L, Jonsson E. Hereditary factors and “angina pectoris”. A study on 5,877 twin-pairs with the aid of mailed questionnaires. Arch Environ Health. 1967;14:397–400. doi: 10.1080/00039896.1967.10664761. [DOI] [PubMed] [Google Scholar]
- 47.Liljefors I. Coronary heart disease in male twins. Hereditary and environmental factors in concordant and discordant pairs. Acta Med Scand Suppl. 1970;511:1–90. [PubMed] [Google Scholar]
- 48.de Faire U, Friberg L, Lundman T. Concordance for mortality with special reference to ischaemic heart disease and cerebrovascular disease. A study on the Swedish Twin Registry. Prev Med. 1975;4:509–17. doi: 10.1016/0091-7435(75)90036-5. [DOI] [PubMed] [Google Scholar]
- 49.Marenberg ME, Risch N, Berkman LF, Floderus B, de Faire U. Genetic susceptibility to death from coronary heart disease in a study of twins. N Engl J Med. 1994;330:1041–6. doi: 10.1056/NEJM199404143301503. [DOI] [PubMed] [Google Scholar]
- 50.Mosteller M. A genetic analysis of cardiovascular disease risk factor clustering in adult female twins. Genet Epidemiol. 1993;10:569–74. doi: 10.1002/gepi.1370100640. [DOI] [PubMed] [Google Scholar]
- 51.Reed T, Quiroga J, Selby JV, et al. Concordance of ischemic heart disease in the NHLBI twin study after 14–18 years of follow-up. J Clin Epidemiol. 1991;44:797–805. doi: 10.1016/0895-4356(91)90132-s. [DOI] [PubMed] [Google Scholar]
- 52.Lusis AJ, Rotter JL, Sparkes RS. Genetic markers for studies of atherosclerosis and related risk factors. In: Lusis AJ, Rotter JL, Sparkes RS, editors. Molecular Genetics of Coronary Artery Disease: Candidate Genes and Processes in Atherosclerosis. New York: Karger; 1992. pp. 363–418. [Google Scholar]
- 53.Breslow JL. Genetics of lipoprotein abnormalities associated with coronary artery disease susceptibility. Annu Rev Genet. 2000;34:233–54. doi: 10.1146/annurev.genet.34.1.233. [DOI] [PubMed] [Google Scholar]
- 54.Kruglyak L. Prospects for whole-genome linkage disequilibrium mapping of common disease genes. Nat Genet. 1999;22:139–44. doi: 10.1038/9642. [DOI] [PubMed] [Google Scholar]
- 55.Krushkal J, Xiong M, Ferrell R, Sing CF, Turner ST, Boerwinkle E. Linkage and association of adrenergic and dopamine receptor genes in the distal portion of the long arm of chromosome 5 with systolic blood pressure variation. Hum Mol Genet. 1998;7:1379–83. doi: 10.1093/hmg/7.9.1379. [DOI] [PubMed] [Google Scholar]
- 56.Frossard PM, Lestringant GG, Malloy MJ, Kane JP. Human renin gene BglI dimorphism associated with hypertension in two independent populations. Clin Genet. 1999;56:428–33. doi: 10.1034/j.1399-0004.1999.560604.x. [DOI] [PubMed] [Google Scholar]
- 57.Heinonen P, Koulu M, Pesonen U, et al. Identification of a threeamino acid deletion in the alpha2B-adrenergic receptor that is associated with reduced basal metabolic rate in obese subjects. J Clin Endocrinol Metab. 1999;84:2429–33. doi: 10.1210/jcem.84.7.5818. [DOI] [PubMed] [Google Scholar]
- 58.Large V, Hellstrom L, Reynisdottir S, et al. Human beta-2 adrenoceptor gene polymorphisms are highly frequent in obesity and associate with altered adipocyte beta-2 adrenoceptor function. J Clin Invest. 1997;100:3005–13. doi: 10.1172/JCI119854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nagase T, Aoki A, Yamamoto M, et al. Lack of association between the Trp64 Arg mutation in the beta 3-adrenergic receptor gene and obesity in Japanese men: A longitudinal analysis. J Clin Endocrinol Metab. 1997;82:1284–7. doi: 10.1210/jcem.82.4.3872. [DOI] [PubMed] [Google Scholar]
- 60.Mitchell BD, Blangero J, Comuzzie AG, et al. A paired sibling analysis of the beta-3 adrenergic receptor and obesity in Mexican Americans. J Clin Invest. 1998;101:584–7. doi: 10.1172/JCI512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sina M, Hinney A, Ziegler A, et al. Phenotypes in three pedigrees with autosomal dominant obesity caused by haploinsufficiency mutations in the melanocortin-4 receptor gene. Am J Hum Genet. 1999;65:1501–7. doi: 10.1086/302660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ristow M, Muller-Wieland D, Pfeiffer A, Krone W, Kahn CR. Obesity associated with a mutation in a genetic regulator of adipocyte differentiation. N Engl J Med. 1998;339:953–9. doi: 10.1056/NEJM199810013391403. [DOI] [PubMed] [Google Scholar]
- 63.Walder K, Norman RA, Hanson RL, et al. Association between uncoupling protein polymorphisms (UCP2-UCP3) and energy metabolism/obesity in Pima indians. Hum Mol Genet. 1998;7:1431–5. doi: 10.1093/hmg/7.9.1431. [DOI] [PubMed] [Google Scholar]
- 64.Horikawa Y, Oda N, Cox NJ, et al. Genetic variation in the gene encoding calpain-10 is associated with type 2 diabetes mellitus Nat Genet 200026163–75.(Erratum in 2000;26:502) [DOI] [PubMed] [Google Scholar]
- 65.Stone LM, Kahn SE, Fujimoto WY, Deeb SS, Porte D., Jr A variation at position −30 of the beta-cell glucokinase gene promoter is associated with reduced beta-cell function in middle-aged Japanese-American men. Diabetes. 1996;45:422–8. doi: 10.2337/diab.45.4.422. [DOI] [PubMed] [Google Scholar]
- 66.Vinik A, Bell G.Mutant insulin syndromes Horm Metab Res 1988201–10.(Erratum in 1988;20:191) [DOI] [PubMed] [Google Scholar]
- 67.Hart LM, Stolk RP, Dekker JM, et al. Prevalence of variants in candidate genes for type 2 diabetes mellitus in The Netherlands: The Rotterdam study and the Hoorn study. J Clin Endocrinol Metab. 1999;84:1002–6. doi: 10.1210/jcem.84.3.5563. [DOI] [PubMed] [Google Scholar]
- 68.Reis A, Ye W-Z, Dubois-Laforgue D, Bellanne-Chantelot C, Timsit J, Velho G. Association of a variant in exon 31 of the sulfonylurea receptor 1 (SUR1) gene with type 2 diabetes mellitus in French Caucasians. Hum Genet. 2000;107:138–44. doi: 10.1007/s004390000345. [DOI] [PubMed] [Google Scholar]
- 69.Pajukanta P, Lilja HE, Sinsheimer JS, et al. Familial combined hyperlipidemia is associated with upstream transcription factor 1 (USF1) Nat Genet. 2004;36:371–6. doi: 10.1038/ng1320. [DOI] [PubMed] [Google Scholar]
- 70.Wang Q, Rao S, Shen G-Q, Li L, Moliterno DJ.Premature myocardial infarction novel susceptibility locus on chromosome 1P34-36 identified by genomewide linkage analysis Am J Hum Genet 200474262–71.(Erratum in 2004;74:1080) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Broeckel U, Hengstenberg C, Mayer B, et al. A comprehensive linkage analysis for myocardial infarction and its related risk factors. Nat Genet. 2002;30:210–4. doi: 10.1038/ng827. [DOI] [PubMed] [Google Scholar]
- 72.Wang L, Fan C, Topol SE, Topol EJ, Wang Q. Mutation of MEF2A in an inherited disorder with features of coronary artery disease. Science. 2003;302:1578–81. doi: 10.1126/science.1088477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Weng L, Kavaslar N, Ustaszewska A, et al. Lack of MEF2A mutations in coronary artery disease. J Clin Invest. 2005;115:1016–20. doi: 10.1172/JCI24186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet. 1999;353:89–92. doi: 10.1016/S0140-6736(98)10279-9. [DOI] [PubMed] [Google Scholar]
- 75.Hamsten A, de Faire U. Risk factors for coronary artery disease in families of young men with myocardial infarction. Am J Cardiol. 1987;59:14–9. doi: 10.1016/s0002-9149(87)80061-9. [DOI] [PubMed] [Google Scholar]
- 76.ten Kate LP, Boman H, Daiger SP, Motulsky AG. Familial aggregation of coronary heart disease and its relation to known genetic risk factors. Am J Cardiol. 1982;50:945–53. doi: 10.1016/0002-9149(82)90400-3. [DOI] [PubMed] [Google Scholar]
- 77.Colditz GA, Rimm EB, Giovannucci E, Stampfer MJ, Rosner B, Willett WC. A prospective study of parental history of myocardial infarction and coronary artery disease in men. Am J Cardiol. 1991;67:933–8. doi: 10.1016/0002-9149(91)90163-f. [DOI] [PubMed] [Google Scholar]
- 78.Barrett-Connor E, Khaw K. Family history of heart attack as an independent predictor of death due to cardiovascular disease. Circulation. 1984;69:1065–9. doi: 10.1161/01.cir.69.6.1065. [DOI] [PubMed] [Google Scholar]
- 79.Colditz GA, Stampfer MJ, Willett WC, Rosner B, Speizer FE, Hennekens CH. A prospective study of parental history of myocardial infarction and coronary heart disease in women. Am J Epidemiol. 1986;123:48–58. doi: 10.1093/oxfordjournals.aje.a114223. [DOI] [PubMed] [Google Scholar]
- 80.Schildkraut JM, Myers RM, Cupples LA, Kiely DK, Kannel WB. Coronary risk associated with age and sex of parental heart disease in the Framingham Study. Am J Cardiol. 1989;64:555–9. doi: 10.1016/0002-9149(89)90477-3. [DOI] [PubMed] [Google Scholar]
- 81.Phillips AN, Shaper AG, Pocock SJ, Walker M. Parental death from heart disease and the risk of heart attack. Eur Heart J. 1988;9:243–51. doi: 10.1093/oxfordjournals.eurheartj.a062492. [DOI] [PubMed] [Google Scholar]
- 82.Hopkins PN, Williams RR, Kuida H, et al. Family history as an independent risk factor for incident coronary artery disease in a high-risk cohort in Utah. Am J Cardiol. 1988;62:703–7. doi: 10.1016/0002-9149(88)91206-4. [DOI] [PubMed] [Google Scholar]
- 83.Nordlie MA, Wold LE, Kloner RA. Genetic contributors toward increased risk for ischemic heart disease. J Mol Cell Cardiol. 2005;39:667–79. doi: 10.1016/j.yjmcc.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 84.Blumenthal S, Jesse MJ, Hennekens CH, Klein BE, Ferrer PL, Gourley JE. Risk factors for coronary artery disease in children of affected families. J Pediatr. 1975;87:1187–92. doi: 10.1016/s0022-3476(75)80134-x. [DOI] [PubMed] [Google Scholar]
- 85.Rissanen AM, Nikkila EA. Identification of the high-risk groups in familial coronary heart disease. Atherosclerosis. 1984;53:37–46. doi: 10.1016/0021-9150(84)90103-5. [DOI] [PubMed] [Google Scholar]
- 86.Hamby RI. Hereditary aspects of coronary artery disease. Am Heart J. 1981;101:639–49. doi: 10.1016/0002-8703(81)90232-5. [DOI] [PubMed] [Google Scholar]
- 87.Berg K, Dahlen G, Borresen AL. La(a) phenotypes, other lipoprotein parameters, and a family history of coronary heart disease in middle-aged males. Clin Genet. 1979;16:347–52. doi: 10.1111/j.1399-0004.1979.tb01014.x. [DOI] [PubMed] [Google Scholar]
- 88.Becker DM, Becker LC, Pearson TA, Fintel DJ, Levine DM, Kwiterovich PO. Risk factors in siblings of people with premature coronary heart disease. J Am Coll Cardiol. 1988;12:1273–80. doi: 10.1016/0735-1097(88)92611-3. [DOI] [PubMed] [Google Scholar]
- 89.Rosengren A, Wilhelmsen L, Eriksson E, Risberg B, Wedel H. Lipoprotein (a) and coronary heart disease: A prospective case-control study in a general population sample of middle aged men. BMJ. 1990;301:1248–51. doi: 10.1136/bmj.301.6763.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sharp SD, Williams RR, Hunt SC, Schumacher MC. Coronary risk factors and the severity of angiographic coronary artery disease in members of high-risk pedigrees. Am Heart J. 1992;123:279–85. doi: 10.1016/0002-8703(92)90635-9. [DOI] [PubMed] [Google Scholar]
- 91.Hunt SC, Gwinn M, Adams TD. Family history assessment: Strategies for prevention of cardiovascular disease. Am J Prev Med. 2003;24:136–42. doi: 10.1016/s0749-3797(02)00586-x. [DOI] [PubMed] [Google Scholar]
- 92.Yusuf S, Hawken S, Ounpuu S, et al. INTERHEART Study Investigators Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 93.Cooper JA, Miller GJ, Humphries SE. A comparison of the PROCAM and Framingham point-scoring systems for estimation of individual risk of coronary heart disease in the Second Northwick Park Heart Study. Atherosclerosis. 2005;181:93–100. doi: 10.1016/j.atherosclerosis.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 94.Kruglyak L. Prospects for whole-genome linkage disequilibrium mapping of common disease genes. Nat Genet. 1999;22:139–44. doi: 10.1038/9642. [DOI] [PubMed] [Google Scholar]
- 95.Roberts R, Stewart AF. Personalized genomic medicine: A future prerequisite for the prevention of coronary artery disease. Am Heart Hosp J. 2006;4:222–7. doi: 10.1111/j.1541-9215.2006.05537.x. [DOI] [PubMed] [Google Scholar]