Abstract
OBJECTIVE
The purpose of this work was to identify the proportions of publicly (Medicaid and State Child Health Insurance Program) insured and uninsured children who did not identify a usual source of care from 1998 to 2006, spanning the State Children’s Health Insurance Program (1997 to present) and the President’s Health Center Initiative (2002 to present), and to characterize unmet medical need as it relates to insurance and a usual source of care for publicly insured and uninsured children.
METHODS
We conducted a secondary data analysis of multiple years of the National Health Interview Survey. We identified the proportion of publicly insured and uninsured children aged 0 to 17 years who did not identify a usual source of care and stratified according to the site of care. We described the odds of reporting an unmet medical need according to insurance status and usual source of care, compared with privately insured children with a usual source of care. Sample weights were used to derive national estimates.
RESULTS
From 1998 through 2006, there were significant increases in the proportions of children enrolled in Medicaid (16.7%–24.5%) and the State Child Health Insurance Program (2.0%–5.3%). The proportion of uninsured children has remained stable from 2002 to 2006 at ~10%. However, the proportion of uninsured reporting no usual source of care increased from 17.8% to 23.3%. Hispanic children had significant increases in the proportions of the uninsured and reporting no usual source of care by 2006. Hispanics constituted the largest proportion in both groups. Uninsured children and children without a usual source of care reported the highest odds of unmet need. Among the insured, publicly insured children had twice the odds of reporting an unmet need compared with privately insured children.
CONCLUSIONS
During the State Child Health Insurance Program and the President’s Health Center Initiative, growing proportions of uninsured children reported no usual source of care. Unmet medical need was the highest for the uninsured and those without a usual source of care. These findings suggest that initiatives designed to improve access to care must combine broadened insurance coverage with enhanced access to usual sources of care.
Keywords: usual source of care, Medicaid, SCHIP, uninsured, children, health center
Having a usual source of care (USC) has been associated with higher rates of preventive care and fewer acute care visits and hospitalizations.1 These benefits are central to a medical home, defined by the American Academy of Pediatrics as a place promoting access to and coordinating care.2 Other than a medical home, health insurance is also important for children, because differences in insurance are associated with markedly different use of health care and with unmet medical need.3 In turn, lower use of primary care by publicly insured and uninsured children is associated with higher use of emergency department (ED) services for nonurgent illness.4
The primary care safety net in the United States is composed of locally funded hospital outpatient departments, physician offices, and community clinics and health centers that seek to provide accessible, timely, and effective care to medically vulnerable populations.5 Two major federal government programs have been launched with potential implications for the safety net and its role in providing access to a USC for children. The first is the State Children’s Health Insurance Program (SCHIP), instituted in 1997 with an annual federal budget of approximately $4 billion, designed to expand insurance coverage for low-income but non–Medicaid-eligible children with federal and state funds. SCHIP has improved health care use among previously uninsured children.6–8
The second and more recent governmental program is the President’s Health Center Initiative (PHCI), launched in 2002, designed to increase health care access for medically vulnerable children and adults by supporting new health care access points and expanding the medical capacity of federally qualified community health centers in 1200 communities. With a budget of $2 billion by fiscal year 2007, 1236 communities had either new federally qualified community health center sites or expanded capacity at existing sites, with service to >15 million patients in 2006, an increase of >4.7 million since 2001.9,10 Trends in health care use for vulnerable children have not been characterized in light of the PCHI. We hypothesized that the cumulative influence of SCHIP and the PCHI would broadly increase the proportion of children over time who identify a USC.
Therefore, the purpose of this analysis was to examine the influence of SCHIP and the PCHI over the past decade on the proportions of publicly insured and uninsured children and adolescents who identify a USC. In addition, we sought to characterize the degree of unmet medical need for publicly insured and uninsured children and adolescents according to insurance status and reported USC. We examined the interaction of insurance status and USC as it bears on unmet medical need, which has not been described previously in the literature.
METHODS
The National Health Interview Survey (NHIS), conducted by the National Center for Health Statistics, Centers for Disease Control and Prevention, and administered annually by the US Census Bureau, is an ongoing, nationwide, in-person survey of ~40 000 households. The NHIS provides data for broad health and health care use trends, as well as the ability to determine unmet medical need across various populations.11 For our work, we analyzed children aged 0 to 17 years whose households were sampled in even years of the NHIS from 1998 to 2006, encompassing years before and during SCHIP and the PHCI. The person-level, family, and sample child files were merged for analysis to bring into 1 data set standard sociodemographic information that is not included in the sample child file alone. The insurance variable was created based on the type of insurance that the child had at the time of interview. A small number of respondents chose both SCHIP and Medicaid or SCHIP and private insurance. Those children were classified as having SCHIP. Those who chose both Medicaid and private insurance were designated as having Medicaid. Of note, in the NHIS, the SCHIP variable was not available for analysis until 1999 (ie, 2000 was the first year for which it was available in this study).
Usual Source of Care
To ascertain where publicly insured and uninsured children usually go for their usual care, we created a composite variable to include all of the respondents who answered “yes” to having the same place for sick and preventive care, as well as those who identified where they go for preventive care. The respondent had multiple choices, including a doctor’s office, clinic/health center, ED, or not receiving care anywhere. Using survey weights provided in the NHIS to permit extrapolation to the US population, the proportion of children and adolescents who cited a USC overall, as well as specific USCs, were determined for each of the study years. Of note, we included “none” (no USC) as 1 of the categories in all of the analyses to examine this group alongside all others.
On the basis of these designations, trends in the distribution of USC according to insurance status were ascertained across the study years. To assess for statistically significant differences in the study period, survey-weighted commands in Stata 10 (Stata Corp, College Station, TX) were used to estimate 95% confidence intervals around point estimates.
Unmet Medical Need
In the sample child file, there are questions that have been used in the literature to characterize unmet medical need.12 Based on this precedent, a composite variable was created based on questions evaluating unmet medical need regarding prescription medicines, mental health care, dental, and eye care. The composite variable was then dichotomized based on these 4 questions (any unmet medical need versus none). We calculated the odds of reporting an unmet medical need for children in groups characterized according to the combination of their insurance status and USC (eg, publicly insured children without a USC), using privately insured children with a USC as the reference group in the model. We hypothesized that privately insured children with a USC would have the lowest odds of reporting an unmet need and that uninsured children without a USC would have the highest odds.
What’s Known on This Subject
A USC has been associated with higher rates of preventive care and fewer acute care visits and hospitalizations. Health insurance is important for children, because differences in insurance are associated with different use of health care and unmet need.
What This Study Adds
This study examined the influence of SCHIP and the PHCI on the proportions of publicly insured and uninsured children who identified a USC. We characterized unmet medical need according to insurance status and USC.
RESULTS
Insurance Status of US Children
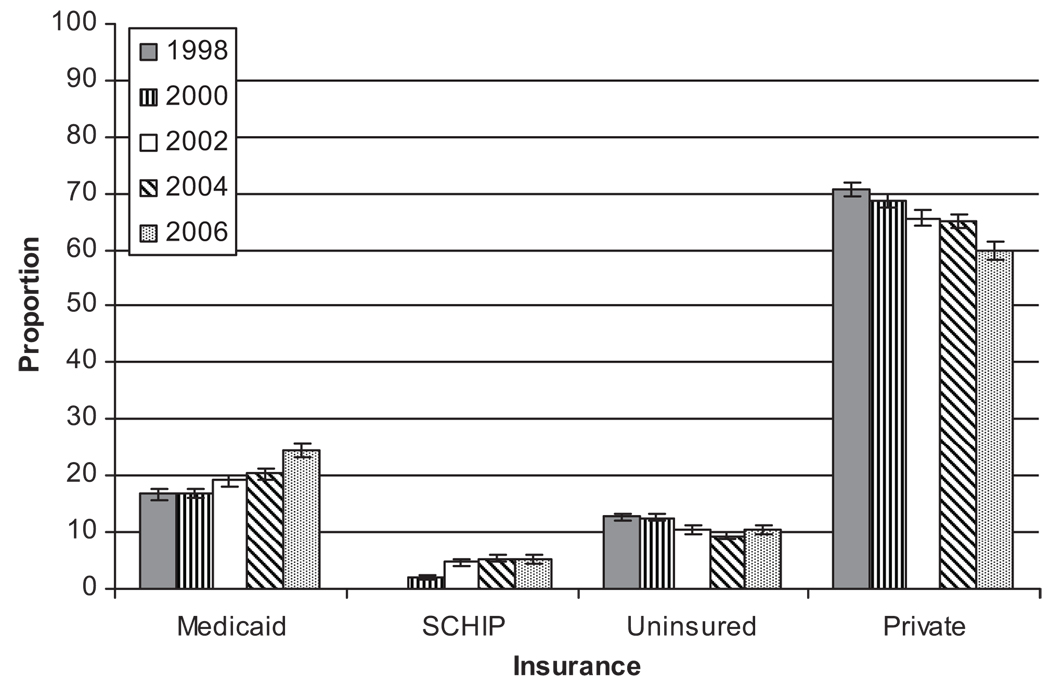
The distribution of children according to insurance status (Fig 1) differed significantly in 2006 vs 1998, with higher proportions enrolled in Medicaid (24.5% vs 17.0%; P < .05) and lower proportions uninsured (10.3% vs 13.0%; P < .05) and privately insured (59.8% vs 70.6%; P < .05). In 2006, the proportion of US children who were enrolled in SCHIP was significantly higher than in 2000 (5.3% vs 2.0%; P < .05; Fig 1).
FIGURE 1.
Proportions of US children according to insurance status, NHIS 1998–2006.
The absolute number of uninsured children was lower in 2006 (7.3 million) than in 1998 (8.7 million; Table 1). Comparison of the uninsured in 2006 vs 1998 (Table 1) revealed that the patterns of uninsurance among children were changing. Younger children were a significantly smaller proportion of the uninsured in 2006 than they were in 1998. Moreover, Hispanic children constituted a significantly larger proportion of uninsured children in 2006 compared with 1998 (42.5% vs 33.0%) and became the largest racial/ethnic group among the uninsured.
TABLE 1.
Age and Race of Uninsured Children, and Children Reporting no USC, NHIS 1998 and 2006
| Demographics | Uninsured 1998 (N = 8 746 854; n = 1993), Proportion (95% CI) |
Uninsured 2006 (N = 7 250 542; n = 1080), Proportion (95% CI) |
No USC 1998 (N = 2 208 722; n = 552), Proportion (95% CI) |
No USC 2006 (N = 2 358 232; n = 345), Proportion (95% CI) |
|---|---|---|---|---|
| Age, y | ||||
| 0–5 | 30.1 (27.7–32.7) | 25.9 (22.7–29.5) | 16.5 (13.1–20.5) | 17.8 (13.3–23.6) |
| 6–11 | 34.7 (32.0–37.5) | 35.3 (30.0–40.9) | 34.0 (28.8–39.5) | 28.2 (21.9–35.5) |
| 12–17 | 35.2 (32.8–37.7) | 33.6 (29.1–38.6) | 49.6 (44.3–54.9) | 54.0 (47.0–60.8) |
| Race/ethnicity | ||||
| White | 46.0 (42.8–49.2) | 39.2 (35.0–43.6) | 37.0 (31.6–42.7) | 32.7 (25.5–40.8) |
| Black | 15.3 (13.1–17.) | 12.7 (10.4–15.5) | 13.7 (10.3–18.0) | 11.1 (7.1–16.8) |
| Hispanic | 33.0 (30.2–36.0) | 42.5 (38.2–46.8) | 41.6 (36.3–47.2) | 50.9 (43.5–58.4) |
| Asian | 5.7 (4.1–8.0) | 5.6 (4.5–5.8) | 7.7 (5.2–11.2) | 5.0 (2.6–9.4) |
Usual Source of Care
In contrast to patterns of uninsurance, the absolute number of children without a USC was higher in 2006 (2.4 million) than in 1998 (2.2 million; Table 1). However, there were no significant changes in the age characteristics of those without a USC. Hispanic children constituted a significantly larger proportion of the group without a USC at 50.9% in 2006 vs 41.6% in 1998 (Table 1).
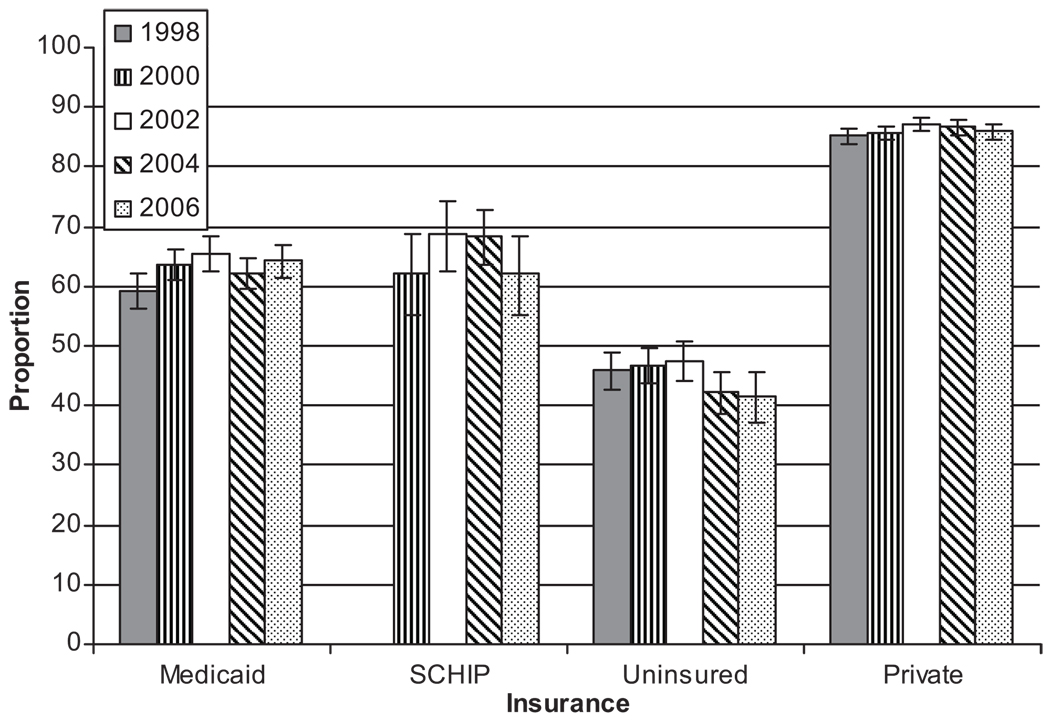
Private Offices
Private offices are the most common USC for privately insured children, at >80% (Fig 2). However, the proportion of Medicaid-enrolled children who identify private offices as a USC steadily increased from 59.2% (95% confidence interval [CI]: 56.1–62.3) in 1998 to 64.3% (95% CI: 61.5–66.9) in 2006. Meanwhile, the proportion of SCHIP-enrolled children using private offices as a USC remained >60% during the study period. Although the proportion of uninsured children who identified a private office as their USC was >40% throughout the study period, the proportion was less in 2006 than in 1998 (Fig 2).
FIGURE 2.
Proportions of children who report a private office as a USC according to insurance status, NHIS 1998–2006.
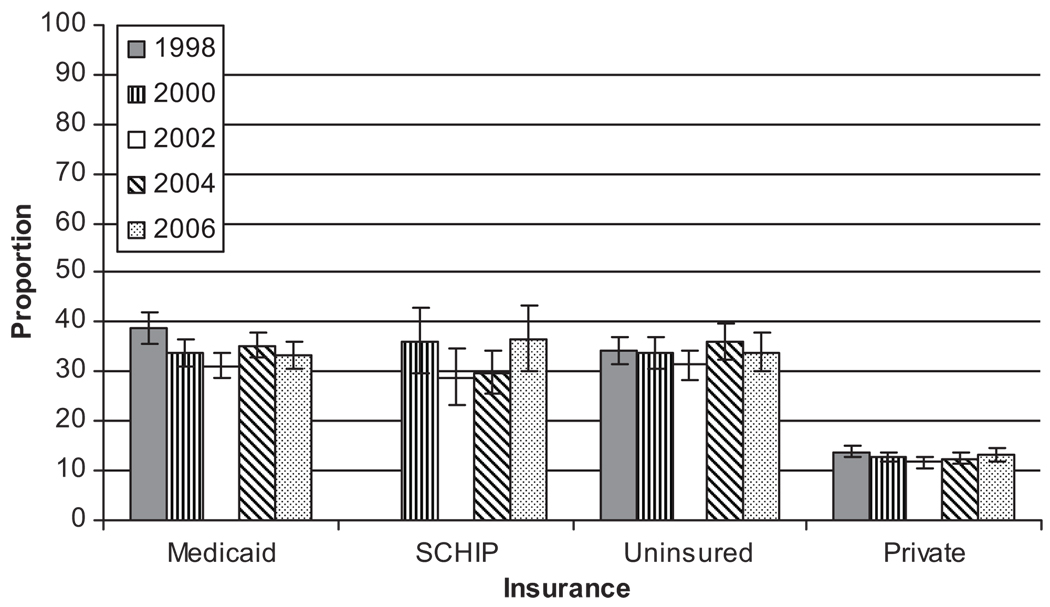
Clinics/Health Centers
Uninsured and publicly insured children identified clinics/health centers as a USC in similar proportions, between 30% and 40% in most study years (Fig 3). In contrast, <15% of children with private insurance identified clinics/health centers as their USC (Fig 3). There were no significant changes in proportions identifying clinics/health centers as a USC for children in any of the insurance groups.
FIGURE 3.
Proportions of children who report a clinic/health center as a USC according to insurance status, NHIS 1998–2006.
Emergency Department
Overall, the proportions of children who identified the ED as a USC were low, regardless of insurance. Uninsured children had the highest proportion reporting the ED as a USC in all of the study years: 2.2% (95% CI: 1.5–3.0) in 1998 and 1.6% (95% CI: 0.9–2.7) in 2006.
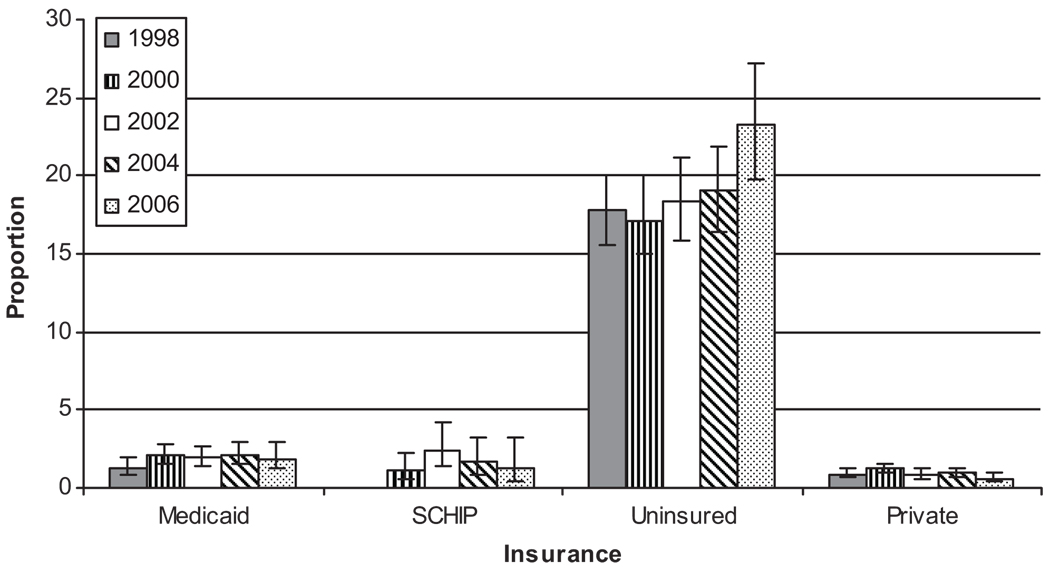
No USC
Uninsured children were the most likely to report no USC, at increasing rates over the study period (Fig 4). By 2006, 23.3% (95% CI: 19.7–27.2) of uninsured children reported no USC, compared with 17.8% (95% CI: 15.6–20.1) in 1998. Privately insured children had the lowest proportions who reported no USC, although Medicaid-enrolled and SCHIP-enrolled children were <5% (Fig 4).
FIGURE 4.
Proportions of children who report no USC according to insurance status, NHIS 1998–2006.
Unmet Medical Need According to Insurance Status and USC Status
Overall, 9.5% (95% CI: 8.4–10.6; n = 6 230 454) of children in 2006 had unmet medical need, compared with 7.1% (95% CI: 6.8–7.7; n = 4 552 163) in 1998. Medicaid-enrolled, SCHIP-enrolled, and uninsured children all had higher odds of reporting an unmet medical need compared with the privately insured, in all of the study years (Table 2). Although the odds of reporting an unmet medical need for Medicaid-enrolled children and SCHIP-enrolled children remained at 2 times higher than privately insured children through the study period, uninsured children had substantially higher odds of unmet need, at 5 to 6 times the odds of the reference group (Table 2).
TABLE 2.
Relative Odds of Reporting an Unmet Medical Need According to Insurance Status and USC, NHIS 1998–2006
| Year | 1998, Odds Ratio (95% CI) |
2000, Odds Ratio (95% CI) |
2002, Odds Ratio (95% CI) |
2004, Odds Ratio (95% CI) |
2006, Odds Ratio (95% CI) |
|---|---|---|---|---|---|
| Insurance status | |||||
| Private | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Medicaid | 2.0 (1.6–2.6) | 2.0 (1.6–1.5) | 2.1 (1.7–2.6) | 1.7 (1.4–2.2) | 1.8 (1.3–2.3) |
| SCHIP | — | 2.1 (1.3–3.3) | 2.5 (1.8–3.5) | 2.1 (1.5–2.8) | 2.1 (1.3–3.3) |
| Uninsured | 4.7 (3.9–5.8) | 5.5 (4.5–6.6) | 4.7 (3.8–5.7) | 5.8 (4.7–7.2) | 6.2 (5.0–7.9) |
| USC | |||||
| Private office | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Clinic/health center | 1.8 (1.5–2.2) | 1.4 (1.2–1.7) | 1.6 (1.3–1.9) | 1.5 (1.2–1.8) | 1.6 (1.2–2.0) |
| ED | 4.2 (2.1–8.5) | 2.0 (0.9–4.8) | 6.2 (3.0–13.2) | 3.0 (1.4–6.1) | 5.4 (2.4–12.2) |
| No USC | 3.7 (2.7–5.0) | 3.9 (3.0–5.1) | 3.8 (2.9–5.1) | 4.5 (3.4–6.1) | 5.3 (3.6–7.6) |
In examining unmet medical need according to USC, children without a USC and those identifying a clinic/health center as USCs were all significantly more likely to have unmet medical need than those who identified a private office as their USC (Table 2). In most study years, children who identified a clinic/health center as their USC were less likely to have unmet need than children who identified EDs as a USC and those without a USC. These differences were not consistently statistically significant.
We also examined unmet need according to USC, adjusting for insurance status. The differences observed with clinic/health centers and the ED were no longer significant. However, children without a USC still had 2 times the odds of reporting an unmet medical need after adjusting for insurance status in 2006 (data not shown).
Compared with the reference group (children with private insurance and a USC), children with private insurance/no USC and those with public insurance/USC were 2 to 3 times more likely to have unmet need in most study years (Table 3). Still worse, children with public coverage/no USC and those uninsured with a USC were 3 to 5 times more likely to have unmet need than the reference group. Uninsured children with no USC had 6 to 9 times the odds of unmet medical need across the study period.
TABLE 3.
Relative Odds of Reporting an Unmet Medical Need According to Insurance Status and USC, NHIS 1998–2006
| Insurance/USC | 1998 Odds Ratio (95% CI) |
2000 Odds Ratio (95% CI) |
2002 Odds Ratio (95% CI) |
2004 Odds Ratio (95% CI) |
2006 Odds Ratio (95% CI) |
|---|---|---|---|---|---|
| Private,+(reference) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Private,− | 1.3 (0.4–3.8) | 2.1 (0.9–5.1) | 3.1 (4.6–9.0) | 2.6 (1.2–5.8) | 3.0 (1.0–8.6) |
| Public,+ | 2.0 (1.6–2.5) | 1.9 (1.6–2.4) | 2.2 (1.8–2.7) | 1.8 (1.5–2.2) | 1.8 (1.4–2.3) |
| Public,− | 4.5 (1.5–13.6) | 3.4 (1.4–8.5) | 3.3 (1.6–7.0) | 3.2 (1.3–7.6) | 5.6 (2.1–15.0) |
| Uninsured,+ | 4.5 (3.7–5.6) | 5.2 (4.2–6.4) | 4.4 (3.5–5.5) | 5.2 (4.1–6.6) | 5.5 (4.3–7.1) |
| Uninsured,− | 6.0 (4.3–8.4) | 7.5 (5.6–10.2 | 6.4 (4.6–9.0) | 9.1 (6.3–13.1) | 8.5 (5.7–12.8) |
+/− represents having a USC or no USC.
DISCUSSION
To our knowledge, this is the first study examining recent trends in the proportions of publicly insured and uninsured children who do and do not identify a USC and where they report getting care in light of 2 major initiatives (SCHIP and the PHCI) with potentially major influence on access to care for children. During the study period, the number and proportion of children who were uninsured decreased, consistent with other national studies of children’s insurance coverage during the SCHIP era.13 However, broader coverage and the PHCI have not translated into more uninsured children reporting USCs. In fact, the proportion reporting no USC increased during the PHCI era. This concerning finding has not been reported previously.
Our findings are consistent with data regarding increasing volumes of care at clinics/health centers during the PHCI era.14 Although it is difficult to directly compare because health center data do not specify volumes of visits for children, we found that the proportion of uninsured children who reported clinics/health centers as a USC was the same (34%) in 1998 and 2006. Because the overall number of children (uninsured and insured) increased, this translated into a larger number of children over time seen at clinics and health centers.
The more salient pattern of change seems to relate to the privately insured and to private offices as a USC. Private offices continued to be a USC for the bulk of children, regardless of insurance status. Even so, it is important to note that, recently, the proportion of uninsured and SCHIP-enrolled children who reported a private office as their USC decreased, as did the proportion of privately insured children overall who were most likely to attend private offices. Concurrently, an increasing proportion of uninsured children reported no USC, although the overall proportion of uninsured children remained stable. Together, these patterns are producing a concerning shift away from private offices as a USC and toward reporting no USC.
There are several possible explanations for these phenomena. Although the proportion of children who are uninsured has remained stable, an increasing proportion reporting no USC may reflect churning of children on and off coverage,15 leading to intermittent lapses and dropped coverage for children enrolled previously in public programs and private plans.16 The mounting losses in employer-based coverage related to the worsening economy and to increasing premium costs may explain the significant drop in private coverage for children during the study period.17 The dropout of publicly insured children from private offices may reflect concerns with private provider reimbursement, administrative policies, or billing related to government programs and its potentially negative effects on providing accessible care to this population.16 It is also possible that the trends for older children and adolescents to be uninsured and have no USC could also be contributing factors to our findings.
The fact that clinics/health centers have remained stable as USCs over time was not consistent with our hypothesis that clinics/health centers would increase as USCs during the PHCI. Flat trends, similar to stable rates of uninsurance among children, may indicate that access to health center care is unlikely to increase unless coverage further increases.18 This connection between coverage and USC identification is highlighted by the increase in SCHIP-enrolled children who reported clinic/health centers as a USC across the study period, consistent with the federally qualified community health center literature reporting increasing numbers of community health center patients enrolled in SCHIP.19
Publicly insured and uninsured children had higher odds of reporting an unmet medical need compared with privately insured children. The uninsured had the highest odds overall, consistent with previous studies examining unmet need.12 What is notable is that the odds of reporting an unmet medical need were stable or increasing over time, despite efforts at state and national levels to improve access to care for the uninsured. Among the insured, Medicaid and SCHIP-enrolled children had ~2 times the odds of reporting an unmet medical need compared with privately insured children. This reveals a dichotomy within the insured that has persisted and warrants attention by legislators and policy-makers on how to address and diminish this continuing disparity.
In comparison with privately insured children with a USC, the uninsured without a USC had the highest odds of reporting an unmet medical need. Uninsured children had significantly higher odds of reporting an unmet need compared with publicly insured children, highlighting the importance of coverage for children in reducing unmet medical need. The publicly insured children without a USC had similar odds of reporting an unmet medical need, as did the uninsured with a USC, illustrating that having a USC somewhat safeguards against unmet need even if uninsured. The safety net exists to provide that care and reduce the unmet need that vulnerable populations experience. A particularly and increasingly vulnerable group is Hispanic children, who are the most likely not only to be uninsured but also to report no USC.20,21
Our results should be interpreted in light of some limitations. First, because of the nature of the data, we cannot determine reasons for changes in an individuals’ USC. Second, serial cross-sectional analyses cannot attribute causality for the trends that we observed.
Third, questions in the NHIS did not distinguish between a clinic or health center as separate answers for the respondents, and that could influence the proportions of children who reported a health center as a USC over the study period. Nevertheless, we believe that federally qualified community health centers are a large subset of the clinic/health center group, and stable proportions of clinic/health center patients do shed light on how major initiatives have influenced the use of health care over time.
Fourth, what is considered an unmet medical need as defined in the data set may be variable. However, we designated unmet medical need based on precedent.12 We also performed analyses that examined the odds of unmet need for prescription medicines and mental health counseling only and found no significant differences in the trends seen by insurance status or USC as compared with the composite variable. There may be other factors that affect the odds of reporting unmet need, such as differences in case mix among providers, and within payer type that could influence these trends. The unmet needs presented are not all encompassing of the potential unmet needs that can be encountered by patients, and this is an acknowledged limitation of these data.
CONCLUSIONS
National patterns of health insurance coverage, usual sources of care, and unmet medical need indicate that SCHIP and the PHCI have not fully addressed health care for vulnerable populations. As the nation continues to focus on the future of health care,22 and, in particular, health care for children, it seems insufficient to focus policy efforts on either coverage or access in isolation. Initiatives must be targeted in tandem to increase access and use of health care and to reduce unmet medical need.
Abbreviations
- USC
usual source of care
- ED
emergency department
- SCHIP
State Children’s Health Insurance Program
- PHCI
President’s Health Center Initiative
- NHIS
National Health Interview Survey
- CI
confidence interval
Footnotes
The authors have indicated they have no financial relationships relevant to this article to disclose.
Reprints Information about ordering reprints can be found online: http://www.pediatrics.org/misc/reprints.shtml
REFERENCES
- 1.Newacheck PW, Hughes DC, Stoddard JJ. Children’s access to primary care: differences by race, income, and insurance status. Pediatrics. 1996;97(1):26–32. [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics. Medical Home Initiatives for Children With Special Needs Project Advisory Committee. The medical home. Pediatrics. 2002;110(1 pt 1):184–186. [Google Scholar]
- 3.Newacheck PW, Stoddard JJ, Hughes DC, Pearl M. Health insurance and access to primary care for children. N Engl J Med. 1998;338(8):513–519. doi: 10.1056/NEJM199802193380806. [DOI] [PubMed] [Google Scholar]
- 4.Luo X, Liu G, Frush K, Hey LA. Children’s health insurance status and emergency department utilization in the United States. Pediatrics. 2003;112(2):314–319. doi: 10.1542/peds.112.2.314. [DOI] [PubMed] [Google Scholar]
- 5.Lipson DJ, Naierman N. Effects of health system changes on safety-net providers. Health Aff (Millwood) 1996;15(2):33–48. doi: 10.1377/hlthaff.15.2.33. [DOI] [PubMed] [Google Scholar]
- 6.Szilagyi PG, Dick AW, Klein JD, Shone LP, Zwaniger J, McInerny T. Improved access and quality of care after enrollment in the New York State Children’s Health Insurance Program (SCHIP) Pediatrics. 2004;113(5) doi: 10.1542/peds.113.5.e395. Available at: www.pediatrics.org/cgi/content/full/113/5/e395. [DOI] [PubMed] [Google Scholar]
- 7.Kaiser Commission on Medicaid and Uninsured. [Accessed December 13, 2007];A decade of SCHIP experience and issues for reauthorization. Available at: www.kff.org/medicaid/upload/7574-2.pdf.
- 8.Duderstadt KG, Hughes DC, Soobader MJ, Newacheck PW. The impact of public insurance expansions on children’s access and use of care. Pediatrics. 2006;118(4):1676–1682. doi: 10.1542/peds.2006-0004. [DOI] [PubMed] [Google Scholar]
- 9.Bureau of Primary Health Care. [Accessed December 23, 2008];The Health Center Program: The President’s Health Center Initiative. Available at: http://bphc.hrsa.gov/presidentsinitiative/
- 10.National Association of Community Health Centers, Inc. [Accessed December 23, 2008];Fact sheet: America’s health centers. 2008 August; Available at: www.nachc.org/client/documents/America’s_Health_Centers_updated_8.13.08.pdf.
- 11.National Center for Health Statistics. Data File Documentation, National Health Interview Survey, 2006. Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention; 2007. [machine readable data file and documentation] [Google Scholar]
- 12.Newacheck PW, Hughes DC, Hung YY, Wong S, Stoddard JJ. The unmet health needs of America’s children. Pediatrics. 2000;105(4 pt 2):989–997. [PubMed] [Google Scholar]
- 13.White House Press Release. [Accessed July 23, 2008];Meeting the health care needs of uninsured and underserved. 2007 December 5; Available at: http://whitehouse.gov/news/releases/2007/12/20071205-2.html.
- 14.Sommers BD. Why millions of children eligible for Medicaid and SCHIP are uninsured: poor retention versus poor take-up. Health Aff (Millwood) 2007;26(5):w560–w567. doi: 10.1377/hlthaff.26.5.w560. [DOI] [PubMed] [Google Scholar]
- 15.Sommers BD. From Medicaid to uninsured: Drop-out among children in public insurance programs. Health Serv Res. 2005;40(1):59–78. doi: 10.1111/j.1475-6773.2005.00342.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeVoe JE, Krois L, Edlund C, Smith J, Carlson N. Uninsured but eligible children are their parents insured? Recent findings from Oregon. Med Care. 2008;46(1):3–8. doi: 10.1097/MLR.0b013e31815b97ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shi L. Type of health insurance and the quality of primary care experience. Am J Public Health. 2000;90(12):1848–1855. doi: 10.2105/ajph.90.12.1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Association of Community Health Centers. [Accessed December 23, 2008];Fact sheet: health centers and SCHIP—improving access to care for kids. Available at: www.nachc.org/client/documents/issues-advocacy/policy-library/research-data/fact-sheets/SCHIP_Fact_Sheet.pdf.
- 19.Flores G, Abreu M, Olivar MA, Kastner B. Access barriers to health care for Latino children. Arch Pediatr Adolesc Med. 1998;152(11):1119–1125. doi: 10.1001/archpedi.152.11.1119. [DOI] [PubMed] [Google Scholar]
- 20.Flores G, Abreu M, Tomany-Korman SC. Why are Latinos the most uninsured racial/ethnic group of US children? A community-based study of risk factors for and consequences of being an uninsured Latino child. Pediatrics. 2006;118(3) doi: 10.1542/peds.2005-2599. Available at: www.pediatrics.org/cgi/content/full/118/3/e730. [DOI] [PubMed] [Google Scholar]
- 21.US Department of Health and Human Services, Health Resources and Services Administration (HRSA) [Accessed July 2, 2008];2002 community health center (CHC) user survey. Available at: www.hrsa.gov.
- 22.Commonwealth Fund. The Commonwealth Fund Commission on a High Performance Health System, Why not the Best? Results From the National Scorecard on U.S. Health System Performance 2008. New York, NY: Commonwealth Fund; 2008. [Google Scholar]