Abstract
Optimal acute management of the highly comminuted distal ulna head/neck fracture sustained in conjunction with an unstable distal radius fracture requiring operative fixation is not well established. The purpose of the present study was to determine the clinical, radiographic, and functional outcomes following acute primary distal ulna resection for comminuted distal ulna fractures performed in conjunction with the operative fixation of unstable distal radius fractures. Between 2000 and 2007, 11 consecutive patients, mean age 62 years (range, 30–75) were treated for concomitant closed, comminuted, unstable fractures of the distal radius and ulna metaphysis. All 11 patients underwent distal ulna resection through a separate dorsal ulnar incision with ECU tenodesis following surgical fixation of the distal radius fracture. According to the Q modifier of the Comprehensive Classification of Fractures, there were six comminuted fractures of the ulnar neck (Q3) and five fractures of the head/neck (Q5). Operative fixation of the distal radius fracture included volar plate fixation in four patients and spanning external fixation with supplemental percutaneous Kirschner wires in seven patients. At a mean of 42 months (range, 18–61 months) postoperatively, clinical, radiographic, and wrist-specific functional outcome with the modified Gartland and Werley wrist score were evaluated. At latest follow-up, mean wrist range of motion measured 53° flexion (range, 35–60°), 52° extension (range, 30–60°), 81° pronation (range, 75–85°), and 77° supination (range, 70–85°). Mean grip strength measured 90% of the contralateral, uninjured extremity (range, 50–133%). No patient had distal ulna instability. Final radiographic assessment demonstrated restoration of distal radius articular alignment. According to the system of Gartland and Werley as modified by Sarmiento, there were seven excellent and four good results. No patient has required a secondary surgical procedure. Acute primary distal ulna resection yields satisfactory clinical, radiographic, and functional results in appropriately selected patients and represents a reliable alternative to open reduction and internal fixation when anatomic restoration of the distal ulna/sigmoid notch cannot be achieved. Primary distal ulna resection with distal radius fracture fixation may help avoid secondary procedures related to distal ulna fixation or symptomatic post-traumatic distal radioulnar joint arthrosis.
Keywords: Darrach distal ulna resection, Distal ulna fracture, Distal radius fracture, Wrist trauma
Introduction
Comminuted unstable metaphyseal fractures of the distal ulna may be seen in up to 6% of patients with unstable fractures of the distal radius [1], and have been reported following both high- and low-energy mechanisms of injury [1, 10, 20]. Several classification systems [1, 2, 6, 17] characterize distal radius fractures together with complex injury patterns involving the distal radioulnar joint (DRUJ) or distal ulna metaphyseal and/or articular segments.
Optimal management of the comminuted distal ulna articular head and/or metaphyseal neck fracture sustained in conjunction with an unstable distal radius fracture requiring operative fixation is not well established, and series reporting outcomes following operative treatment of these injuries remain limited [1, 5, 9, 10, 20, 22]. Failure to achieve stable anatomic reduction and distal radioulnar joint congruity compromises the ability to re-establish ulnar variance and DRUJ stability, and thus increases the risk of distal ulna nonunion [7, 16, 19], DRUJ dysfunction, ulnar-sided wrist pain, and post-traumatic arthrosis [12].
Fixation of comminuted distal ulna head/neck fractures remains technically challenging. Angular-stable implants, such as minicondylar blade plates [20] or minifragment locked plates [5], have been introduced as solutions to obtaining fixation within small, osteopenic, metaphyseal fragments and the short non-articular arc of the ulnar head. Although Ring et al. [20] reported good-to-excellent results in the majority of their cohort at a mean of 26 months following operative fixation of unstable distal ulna fractures with a minicondylar blade plate construct, seven patients (29%) required re-operation for removal of symptomatic ulnar-sided hardware and one patient underwent revision fixation and bone grafting for a distal ulna nonunion. Even with angular-stable plate technology, anatomic restoration of the ulnar head–sigmoid notch articular relationship and stable fixation of the metaphyseal segments may not be achieved [5].
Ablative procedures of the distal ulna—partial ulnar resection, Darrach resection, or Sauve–Kapandji [3, 4, 11, 13, 15] procedures—have been regarded as salvage-type delayed reconstructive options to address sequelae of distal radius fractures and symptomatic post-traumatic DRUJ arthrosis or instability. Only recently, a limited number of series [10, 22] have reported satisfactory results following utilization of these “salvage” options as index procedures for irreparable distal ulna head/neck fractures at the time of operative fixation of concomitant unstable fractures of the distal radius.
The purpose of the present study was to determine the clinical, radiographic, and wrist-specific functional outcomes following acute primary distal ulna resection for comminuted distal ulna fractures performed in conjunction with the operative fixation of unstable distal radius fractures. We hypothesized that the Darrach resection performed as a primary procedure with distal radius fixation yields satisfactory results in appropriately selected patients, represents a reliable alternative when anatomic restoration and stable fixation of distal ulna articular and/or metaphyseal segments cannot be achieved, and may help avoid early or late secondary procedures related to distal ulna fixation or symptomatic post-traumatic DRUJ arthrosis.
Methods
Following Institutional Review Board approval, retrospective evaluation of collected medical and radiographic data from our upper extremity trauma database between 2000 and 2007 identified a cohort of 11 consecutive patients diagnosed and treated surgically for closed, unstable fractures of the distal radius sustained with a concomitant comminuted, unstable fracture of the distal ulna metaphysis (ulna head and/or neck fracture). The cohort was comprised of six females and five males, with a mean age of 62 years (range, 30–75 years). Nine of the 11 patients were right-hand dominant, and the dominant wrist was injured in seven of the 11 cases. All fractures were closed. A single patient sustained an ipsilateral closed elbow dislocation, and a single patient suffered from rheumatoid arthritis. There were no associated neurovascular insults.
All distal radius fractures in this cohort were unstable displaced fractures indicated for operative treatment. Instability was defined as dorsal comminution extending volar to the mid-axial plane of the radius on the lateral radiograph, a greater than 20° change in sagittal plane alignment, radiocarpal involvement, associated ulna fracture, and patient age greater than 60 years. According to the Q modifier for distal ulna fractures associated with distal radius fractures within the Comprehensive Classification of Fractures [17], there were six comminuted fractures of the ulnar neck (Q3) and five fractures of the head/neck (Q5).
Operative treatment was performed in all cases by the senior authors (K.B.R. and M.E.R.) and the distal radius fracture fixation construct was based upon the fracture type and degree of instability. Volar plate fixation of the distal radius fractures was performed in four patients (Fig. 1). These patients were managed postoperatively with 6 weeks of cast immobilization in order to protect the distal ulnar resection arthroplasty. Following removal of the cast, active and active-assisted motion of the forearm and wrist was initiated. Standard spanning external fixation [18] (EBI distal radius fixator, Parsippany, NJ, USA) with supplemental percutaneous Kirschner wires was performed in seven patients (Fig. 2). Active and active-assisted digital motion was initiated immediately postoperatively. A protective short arm splint was worn for the duration of external fixation. Following removal of the external fixator at 8 weeks, active and active-assisted motion of the forearm and wrist was initiated. Resistance exercises were started following fracture union in both fixation groups.
Figure 1.
Anteroposterior (a), oblique (b), and lateral (c) injury radiographs of a comminuted distal radius fracture with a concomitant unstable metaphyseal distal ulna fracture. Note the sigmoid notch and distal radioulnar joint involvement, and the palmar–rotatory displacement of the ulna articular head fragment. One year postoperative anteroposterior (d), oblique (e), and lateral (f) radiographs demonstrate osseous union. There is no evidence of ulnar stump instability, radioulnar impingement, or carpal translocation following the distal ulna resection.
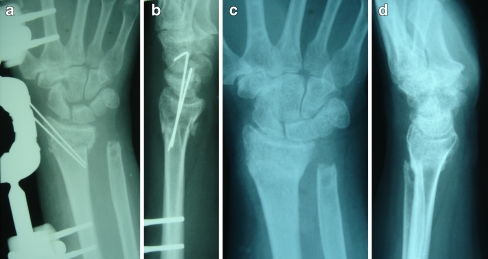
Figure 2.
Intraoperative anteroposterior (a) and lateral (b) radiographs following spanning distal radius external fixation, percutaneous Kirschner-wire fixation, and simultaneous distal ulna resection. Anteroposterior (c) and lateral (d) radiographs demonstrate osseous union at latest follow-up.
Operative Technique
All 11 patients underwent acute primary distal ulna resection for irreparable, comminuted distal ulnar articular/metaphyseal fractures that remained displaced and unstable [5, 20, 23, 25] following reduction and definitive fixation of the distal radius fracture. The distal ulnar resection was performed through a separate dorsal ulnar incision. The dorsal ulnar sensory nerve was identified and protected. After incision of the extensor retinaculum, the extensor digiti minimi is elevated radially and the extensor carpi ulnaris subsheath is protected as the floor of the sixth extensor compartment is elevated. A dorsal DRUJ capsulotomy may be performed, but often a traumatic capsulotomy is present secondary to the acute trauma. With subperiosteal dissection, the metaphyseal fracture fragments are mobilized and the attachments of the triangular fibrocartilage complex are gently elevated off of the most distal fragments. The resection is performed at the most proximal extent of the ulnar neck fracture, usually at the level of the proximal sigmoid notch. The most distal aspect of the ulnar shaft is then contoured is a proximal–radial to distal–ulnar orientation to avoid radioulnar impingement. Tenodesis of the extensor carpi ulnaris [14, 24] is then completed with a distally based 8 cm slip of the ulnar one-half of the extensor carpi ulnaris. The proximal end of the tendon is passed from the distal ulnar aspect of the resected ulna through a dorsal cortical drill hole 1 cm proximal to the resected end. The extensor carpi ulnaris is then sutured to itself with the wrist in mild extension. The periosteal sleeve and dorsal capsule are imbricated, and the extensor retinaculum is repaired.
Evaluation
All 11 patients were available for clinical and radiographic evaluation at a minimum of 1 year postoperatively, with a mean duration of follow-up of 42 months (range, 18–61). Ten of the 11 patients obtained greater than 2-year follow-up. Clinical examination was performed by the treating surgeon. Wrist range of motion, including arcs of flexion–extension and pronation–supination, were measured with a handheld goniometer. Range of motion of the injured wrist at latest follow-up is reported. Grip strength was measured using a Jamar dynamometer (Asimov Engineering, Los Angeles, CA, USA). All patients were examined for stability of the ulnar stump and the presence of symptoms related to the dorsal ulnar sensory nerve. Serial postoperative radiographs were evaluated for radial height, radial inclination, and volar tilt [6] as well as radiographic evidence of ulnar stump instability and ulnar translocation of the carpus. At latest follow-up, wrist-specific functional outcome was evaluated with the Gartland and Werley [8] wrist score as modified by Sarmiento [21]. Results are categorically defined within this demerit point system according to the total point range assigned to the injured wrist as excellent (0–2), good (3–8), fair (9–20), and poor (≥21). Complications and secondary procedures were catalogued.
Results
At latest follow-up, mean wrist flexion measured 53° (range, 35–60°); wrist extension 52° (range, 30–60°); pronation 81° (range, 75–85°); and supination 77° (range, 70–85°). The mean wrist flexion–extension arc measured 105° (range, 65–120°) and the mean pronosupination arc measured 158° (range, 145–170°). Mean grip strength was 51 lb (range, 15–90 lb) and measured 90% of the contralateral, uninjured extremity (range, 50%–133%). Eight of the 11 patients (73%) achieved grip strength equal to the strength of the contralateral, uninjured upper extremity. No patient had clinical evidence of ulnar stump instability or symptoms related to the dorsal ulnar sensory nerve.
All distal radius fractures achieved osseous union. Final radiographic assessment demonstrated restoration of distal radius length, inclination, and tilt as well as articular congruity. There was no radiographic evidence of ulnar stump instability or ulnar carpal translocation in any case. According to the system of Gartland and Werley [8] as modified by Sarmiento [21], there were seven excellent and four good results. There were no postoperative complications, and no patient required a secondary surgical procedure at latest follow-up.
Discussion
Concomitant distal radius and distal ulna metaphyseal/articular fractures are uncommon injuries [1, 5, 10, 20, 22]. As these fractures typically involve the sigmoid notch and ulnar head/neck regions, obtaining anatomic reduction and re-establishing the articular congruity at the radiocarpal and distal radioulnar joints is recommended to ensure an optimal recovery. Despite the availability of angular-stable and locked plating fixation constructs [5, 20] for distal ulnar articular/metaphyseal fractures, non-anatomic reduction [1, 5], loss of fixation in multi-fragmentary fractures, and symptomatic hardware necessitating additional surgery [20] remain significant problems with these fracture patterns.
Distal ulna mal-alignment (≥10° angulation, ≥3 mm of ulnar shortening, or translation ≥1/3–1/2 of the diaphysis), instability of the distal ulna head/neck fracture (fracture fragment motion with passive forearm motion), articular displacement, and DRUJ instability (≥50% distal ulna subluxation) have been reported [5, 20, 23, 25] as indications for ORIF of distal ulna fractures associated with distal radius metaphyseal fractures. Our indication to perform a primary Darrach resection in the acute setting include irreparable, comminuted distal ulnar articular/metaphyseal fractures that remain displaced and unstable following reduction and definitive fixation of the distal radius fracture. The resection is completed at the most proximal extent of the ulnar neck fracture, usually at the level of the proximal sigmoid notch. Resection proximal to the sigmoid notch is more likely to result in distal ulna instability or impingement. We recommend re-assessment of the distal ulna fracture pattern following definitive fixation of the distal radius and restoration of radial length. If the fracture pattern dictates a more proximal resection, surgical fixation should be strongly considered.
When performed in conjunction with operative fixation of unstable distal radius fractures, acute primary Darrach resection for the irreparable distal ulna head/neck fracture yields satisfactory outcomes. The results of the present study are similar to those of Seitz and Raikin [22], who reported good–excellent results in 14 of 15 patients with a mean age of 61 years (range, 34–77 years) at a minimum of 3 years follow-up following acute Darrach resection. Furthermore, good–excellent results are reported in both series [22] with this technique in younger patients with increased demands with regard to their activities of daily living. The clinical, radiographic, and functional outcomes in the present study also compare favorably with those reported [5, 20] following ORIF of the associated distal ulna fracture with angular-stable constructs.
In conclusion, acute Darrach resection in the properly selected patient with concomitant unstable distal radius and comminuted distal ulna fractures is a reliable index procedure and alternative to percutaneous Kirschner-wire fixation, ORIF, or non-operative treatment of the distal ulna fracture. The comminuted distal ulna can be excised following distal radius fracture management with minimal complications. Excision at the proximal level of the sigmoid notch, ECU tenodesis, and attention to capsular closure minimize problems commonly reported with Darrach resection. Further, distal ulna resection as an index procedure may help to avoid complications related to painful or failed distal ulna fixation, symptomatic post-traumatic DRUJ arthrosis or instability, incongruity between the ulna seat and sigmoid notch, or ulnocarpal abutment. The retrospective design and cohort size of this study reflect the relatively rare nature of these injuries. Published clinical series [5, 10, 20, 22] reporting outcomes following operative management of these injuries are similarly limited by cohort size and level IV evidence. Prospective or case-controlled series may help to elucidate the optimal management of these fractures when associated with distal radius metaphyseal fractures requiring operative fixation.
Acknowledgments
Disclosure Statement The authors have no financial or proprietary interest in the subject matter or materials discussed.
Footnotes
This paper was presented in its entirety at the 2009 AAHS Annual Meeting.
Investigation performed at Division of Hand Surgery, New York University Hospital for Joint Diseases, New York, New York, USA
Contributor Information
David E. Ruchelsman, Phone: +1-212-5986000, FAX: +1-212-6852667, Email: david.ruchelsman@nyumc.org
Keith B. Raskin, Phone: +1-212-2634263, FAX: +1-212-6852667, Email: raskik01@med.nyu.edu
Michael E. Rettig, Phone: +1-212-2634263, FAX: +1-212-6852667, Email: DrRettig@aol.com
References
- 1.Biyani A, Simison AJ, Klenerman L. Fractures of the distal radius and ulna. J Hand Surg [Br] 1995;20(3):357–64. doi:10.1016/S0266-7681(05)80094-4. [DOI] [PubMed]
- 2.Bowers WH. Instability of the distal radioulnar articulation. Hand Clin 1991;7(2):311–27. [PubMed]
- 3.Carter PB, Stuart PR. The Sauve–Kapandji procedure for post-traumatic disorders of the distal radio-ulnar joint. J Bone Joint Surg Br 2000;82(7):1013–8. doi:10.1302/0301-620X.82B7.10674. [DOI] [PubMed]
- 4.Darrach W. Anterior dislocation of the head of the ulna. Ann Surg 1912;56:802–3.
- 5.Dennison DG. Open reduction and internal locked fixation of unstable distal ulna fractures with concomitant distal radius fracture. J Hand Surg [Am] 2007;32(6):801–5. doi:10.1016/j.jhsa.2007.03.010. [DOI] [PubMed]
- 6.Fernandez DL, Jupiter JB. Functional and radiographic anatomy. In: Fernandez DL, editors. Fractures of the distal radius. A practical approach to management. New York: Springer; 1995. p. 53–66.
- 7.Fernandez DL, Ring D, Jupiter JB. Surgical management of delayed union and nonunion of distal radius fractures. J Hand Surg [Am] 2001;26(2):201–9. doi:10.1053/jhsu.2001.22917. [DOI] [PubMed]
- 8.Gartland JJ, Werley CW. Evaluation of healed Colles’ fractures. J Bone Joint Surg Am 1951;33(4):895–907. [PubMed]
- 9.Geissler WB, Fernandez DL, Lamey DM. Distal radioulnar joint injuries associated with fractures of the distal radius. Clin Orthop Relat Res 1996;327:135–46. doi:10.1097/00003086-199606000-00018. [DOI] [PubMed]
- 10.Horii E, Ohmachi T, Nakamura R. The primary Sauve–Kapandji procedure—for treatment of comminuted distal radius and ulnar fractures. J Hand Surg [Br] 2005;30(1):60–6. doi:10.1016/j.jhsb.2004.09.004. [DOI] [PubMed]
- 11.Kapandji IA. The Kapandji–Sauve operation. Its techniques and indications in non rheumatoid diseases. Ann Chir Main 1986;5(3):181–93. doi:10.1016/S0753-9053(86)80057-6. [DOI] [PubMed]
- 12.Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am 1986;68(5):647–59. [PubMed]
- 13.Lamey DM, Fernandez DL. Results of the modified Sauve–Kapandji procedure in the treatment of chronic posttraumatic derangement of the distal radioulnar joint. J Bone Joint Surg Am 1998;80(12):1758–69. [DOI] [PubMed]
- 14.Leslie BM, Carlson G, Ruby LK. Results of extensor carpi ulnaris tenodesis in the rheumatoid wrist undergoing a distal ulnar excision. J Hand Surg [Am] 1990;15(4):547–51. [DOI] [PubMed]
- 15.Lichtman DM, Ganocy TK, Kim DC. The indications for and techniques and outcomes of ablative procedures of the distal ulna. The Darrach resection, hemiresection, matched resection, and Sauve–Kapandji procedure. Hand Clin 1998;14(2):265–77. [PubMed]
- 16.McKee MD, Waddell JP, Yoo D, Richards RR. Nonunion of distal radial fractures associated with distal ulnar shaft fractures: a report of four cases. J Orthop Trauma 1997;11(1):49–53. doi:10.1097/00005131-199701000-00015. [DOI] [PubMed]
- 17.Muller ME, Nazarian S, Koch P, Schatzker J. The comprehensive classification of fractures of long bones. Berlin: Springer; 1990. p. 106–15.
- 18.Raskin KB, Rettig ME. Distal radius fractures: external fixation and supplemental K-wires. Atlas Hand Clin 2006;11(2):187–96.
- 19.Ring D. Nonunion of the distal radius. Hand Clin 2005;21(3):443–7. doi:10.1016/j.hcl.2005.01.005. [DOI] [PubMed]
- 20.Ring D, McCarty LP, Campbell D, Jupiter JB. Condylar blade plate fixation of unstable fractures of the distal ulna associated with fracture of the distal radius. J Hand Surg [Am] 2004;29(1):103–9. doi:10.1016/j.jhsa.2003.10.019. [DOI] [PubMed]
- 21.Sarmiento A, Pratt GW, Berry NC, Sinclair WF. Colles’ fractures. Functional bracing in supination. J Bone Joint Surg Am 1975;57(3):311–7. [PubMed]
- 22.Seitz WH, Raikin SM. Resection of comminuted ulna head fragments with soft tissue reconstruction when associated with distal radius fractures. Tech Hand Up Extrem Surg 2007;11(4):224–30. doi:10.1097/BTH.0b013e31805752f8. [DOI] [PubMed]
- 23.Tarr RR, Garfinkel AI, Sarmiento A. The effects of angular and rotational deformities of both bones of the forearm. An in vitro study. J Bone Joint Surg Am 1984;66(1):65–70. [PubMed]
- 24.Tsai TM, Shimizu H, Adkins P. A modified extensor carpi ulnaris tenodesis with the Darrach procedure. J Hand Surg [Am] 1993;18(4):697–702. doi:10.1016/0363-5023(93)90321-S. [DOI] [PubMed]
- 25.Yasutomi T, Nakatsuchi Y, Koike H, Uchiyama S. Mechanism of limitation of pronation/supination of the forearm in geometric models of deformities of the forearm bones. Clin Biomech (Bristol, Avon) 2002;17(6):456–63. doi:10.1016/S0268-0033(02)00034-7. [DOI] [PubMed]