Abstract
Madelung’s deformity is a well-known congenital anomaly of the wrist. A number of procedures have been described to correct the deformity and thus improve function at the wrist. Most of these procedures have to a large extent addressed the alignment and consequent function of the radiocarpal joint but not the persistent problem of painful stiffness at the distal radioulnar joint (DRUJ). The availability of a total DRUJ prosthesis appears to provide a solution to this problem. This article discusses our early experience with total DRUJ arthroplasty using the Scheker prosthesis for managing pain and decreased range of motion in three adult patients with symptomatic Madelung’s deformity.
Keywords: Madelung’s, Distal radioulnar joint, Arthroplasty, Prosthesis
Introduction
Madelung’s deformity is a well-known congenital anomaly of the wrist. The primary pathology has been attributed to inhibition of growth of the ulnar and volar portions of the radial epiphysis, thereby affecting the radiocarpal and distal radioulnar articular surfaces. A consequence of these bony changes is a painful reduction in range of motion (ROM) at the radiocarpal joint and distal radioulnar joint (DRUJ). A number of procedures have been described to correct the deformity and thus improve function at the wrist. These include corrective osteotomy of the radius, epiphysiolysis of the distal radius, release of Vickers’ ligament, Darrach’s procedure, the Sauvé-Kapandji procedure, matched resection of the ulna, and the Ilizarov method [2–4]. While these procedures have to a large extent addressed the alignment and consequent function of the radiocarpal joint, a persistent problem has been painful stiffness at the DRUJ [2, 8]. The availability of a total DRUJ prosthesis appears to provide a solution to this problem. This article discusses our early experience with total DRUJ arthroplasty using the Scheker prosthesis for managing pain and decreased ROM in adult patients with symptomatic Madelung’s deformity.
Materials and Methods
Three patients with long-standing Madelung’s deformity who presented with persistent pain at the DRUJ underwent total DRUJ arthroplasty in five extremities. All three patients were female and the average age at surgery was 30 years (27–35 years). One of the patients had previously undergone bilateral corrective radial osteotomies to obtain a better radiocarpal alignment. Another patient had previously undergone synovectomy and dorsal capsulodesis of the wrist followed by an ulnar shortening procedure. Nonetheless, all patients presented with a persistent painful instability at the DRUJ with a positive “piano key” sign. They also experienced painful limitation of pronosupination and had difficulty lifting objects with their forearms in neutral rotation.
Preoperative evaluation included assessment of ROM, disabilities of the arm, shoulder, and hand (DASH) score, patient-rated wrist evaluation (PRWE) score, visual analog pain scores, and a self-evaluation patient questionnaire.
All three patients underwent total DRUJ arthroplasty with the Scheker prosthesis (APTIS Medical, Louisville, KY, USA). This prosthesis is a total joint replacement system and provides for a semiconstrained replacement system for both the radial and ulnar parts of the distal radioulnar joint (i.e., both the sigmoid notch and the ulnar head). The radial component is made of cobalt chrome while the ulnar head comprises a high-density polyethylene ball with a central pivot made once of cobalt chrome. The standard procedure as described by Scheker et al. [7] was used. Following surgery, patients were placed in a short arm splint for 3 weeks surgery, after which active ROM was encouraged. One patient underwent bilateral procedures with a 3-month interval. Another patient underwent bilateral procedures with a 15-month interval; however, the second joint was excluded from this study because it has not yet had 2 years of follow-up. Postoperative data were recorded at 6 months and at 1 and 2 years and included ROM, grip strength, lifting capacity, DASH score, PRWE score, pain questionnaire, and patient satisfaction survey.
Results
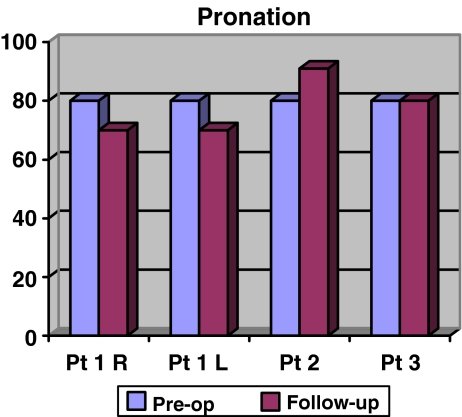
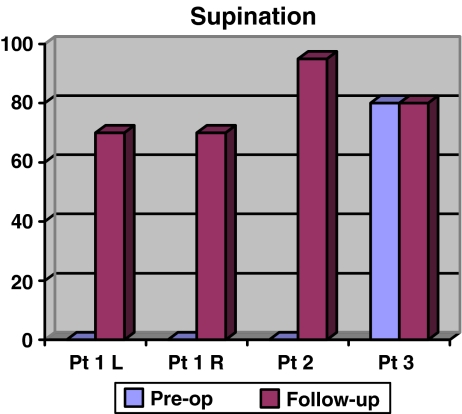
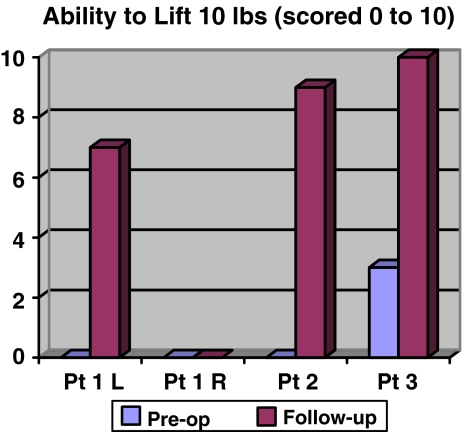
At 2 years of follow-up, the four extremities had a mean decrease in pronation of 2.25° (range −10° to +11°; Fig. 1); however, there were large gains in supination, with an average increase of 58.75° (range 0°–95°; Fig. 2). Patient 1’s left and right wrists had a preoperative pronation of 80°, which decreased to 70° bilaterally at 2 years of follow-up. However, supination in both wrists increased from 0° preoperatively to 70° at 2 years following surgery. Patient 2’s preoperative pronation was 80°, which increased to 91° at 2 years following surgery. Patient 2 also had a large increase in supination from 0° preoperatively to 95° at 2 years follow-up. Patient 3 had no change in either pronation (80°) or supination (80°) at 2 years following surgery. In terms of lifting capacity, patients were asked to rate their ability to lift 10 lb with their affected extremity on a scale of 0 to 10 (0 signifying “unable” and 10 signifying “no problem whatsoever”), with a mean preoperative rating of 0.75 (range 0–3) and a mean postoperative rating of 6.75 (range 0–10; Fig. 3).
Figure 1.
Pre and post-op pronation.
Figure 2.
Gains in supination.
Figure 3.
Ability to lift 10 lb with the affected extremity.
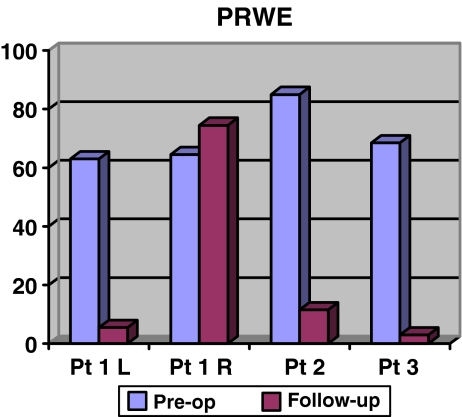
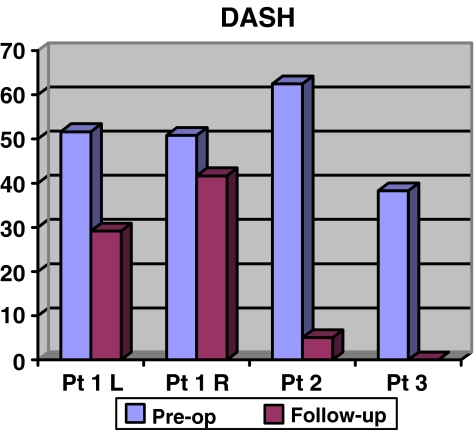
Patients showed improvement in subjective self-assessments as well. The mean preoperative PRWE score was 70.25 (range 63–85), which improved to a postoperative mean of 23.63 (range 5.5–74.5; Fig. 4). The mean preoperative DASH score was 50.83 (range 38.3–62.5), which improved to a postoperative mean of 18.96 (range 0–41.67; Fig. 5). The average preoperative pain score on a scale of 1–10 was 4.5 (range 3 –5). This reduced to 1.5 after surgery (range 1 – 2). Finally, all of our patients indicated on a patient satisfaction questionnaire that they “strongly agree” with the following statement: “If I knew another person with my same type of problem, I would recommend this procedure.”
Figure 4.
Mean preoperative and postoperative PRWE score.
Figure 5.
Mean preoperative and postoperative DASH score.
Discussion
Otto Madelung’s original description in 1878 of the deformity that would later bear his name begins with these words “Under the normal, rather stretched skin, the distal end of the ulna juts out clearly,” [1] which is essentially a description of a dysplastic DRUJ. The problem of persistent pain and instability at the DRUJ in patients with Madelung’s deformity is well recognized. While radial osteotomy has largely succeeded in reestablishing a painless and functional radiocarpal joint, the DRUJ remains unaddressed by this procedure. A partial solution has been to perform an ulnar shortening osteotomy, a Darrach’s procedure, or a Sauvé-Kapandji procedure. The problem of persistent pain remains in many patients and, to date, none of the available surgical procedures have been able to successfully restore a stable, mobile, and painless distal radioulnar joint. In addition, all of these ulna-shortening procedures can also cause a painful dynamic ulnar impingement syndrome, which has been demonstrated clinically and radiographically by Lees and Scheker [6].
Total DRUJ arthroplasty has already been proven effective in restoring ROM and relieving pain in patients with other types of DRUJ problems such as prior fusion or degenerative arthritis of the DRUJ [5]. We have been able to demonstrate a similar improvement in function in all the patients in our current series with painful DRUJ problems following Madelung’s disease (Figs. 6, 7, 8, 9, and 10). We are aware that this study has its shortcomings. The most obvious limitation is a very small cohort of patients. It is also true that this study establishes a new indication for a relatively new prosthesis, further compounded by the fact that the patient population is relatively young. Based on these, our study can best be described as a pilot project to address problems at the DRUJ in patients with Madelung’s disease. Nonetheless, it remains that currently there are no other procedures available for the DRUJ that provide both stability and painless mobility. The DRUJ prosthesis shows benefits of providing a stable and mobile joint, restoring pronosupination, restoring lifting capacity, and achieving overall patient satisfaction. These results have been achieved soon after surgery and have persisted at 2 years of follow-up. Total DRUJ arthroplasty, therefore, should be considered a viable treatment option, with the goal of improving quality of life in patients with Madelung’s deformity who have undergone previous procedures and continue to have pain and limited range of motion.
Figure 6.

Pre-op picture showing a dysplastic distal radio-ulnar joint.
Figure 7.

Same patient as in Fig. 6 after implantation of the DRUJ prosthesis.
Figure 8.
Full supination (post-op).
Figure 9.
Full pronation (post-op).
Figure 10.

A patient implanted with DRUJ prosthesis lifting a dumbbell (20 lbs).
Footnotes
Disclaimer
Dr. Michael Coffey and Dr. Sunil Thirkannad have not received any financial benefits for any part of this study nor do they have any financial interests in any of the devices used as part of this study.
Dr. Luis R. Scheker has a financial interest and is part owner of Aptis Medical which manufactures the Scheker Distal Radioulnar Joint Prosthesis.
References
- 1.Arora AS, Chung KC, Otto W. Madelung and the recognition of Madelung’s deformity. J Hand Surg [Am]. 2006;31(2):177–82. doi:10.1016/j.jhsa.2005.09.001. [DOI] [PubMed]
- 2.Carter PR, Ezaki M. Madelung’s deformity. Surgical correction through the anterior approach. Hand Clin. 2000;16(4):713–21. x–xi. [PubMed]
- 3.dos Reis FB, Katchburian MV, Faloppa F, Albertoni WM, Laredo Filho J Jr. Osteotomy of the radius and ulna for the Madelung deformity. J Bone Joint Surg Br. 1998;80(5):817–24. doi:10.1302/0301-620X.80B5.8691. [DOI] [PubMed]
- 4.Houshian S, Schroder HA, Weeth R. Correction of Madelung’s deformity by the Ilizarov technique. J Bone Joint Surg Br. 2004;86(4):536–40. [PubMed]
- 5.Laurentin-Perez LA, Goodwin AN, Babb BA, Scheker LR. A study of functional outcomes following implantation of a total distal radioulnar joint prosthesis. J Hand Surg Eur Vol. 2008;33(1):18–28. doi:10.1177/1753193408087118. [DOI] [PubMed]
- 6.Lees VC, Scheker LR. The radiological demonstration of dynamic ulnar impingement. J Hand Surg [Br]. 1997;22B(4):448–50. doi:10.1016/S0266-7681(97)80264-1.
- 7.Scheker LR, Babb BA, Killion PE. DRUJ prosthetic replacement. Orthop Clin North Am. 2001;32(2):365–76. doi:10.1016/S0030-5898(05)70256-X. [DOI] [PubMed]
- 8.Schmidt-Rohlfing B, Schwobel B, Pauschert R, Niethard FU. Madelung deformity: clinical features, therapy and results. J Pediatr Orthop B. 2001;10(4):344–8. doi:10.1097/00009957-200110000-00015. [DOI] [PubMed]