Abstract
This study aimed to describe the intraosseous blood supply of the distal radius and its clinical implications in distal radius fractures. Twelve adult wrists from fresh cadavers (six males, six females, 50–90 years of age, mean 68 years) were injected through the brachial artery with latex. Dissections were performed using magnifying loupes and hands were processed using the Spalteholz technique. The distal radius was supplied by three main vascular systems: epiphyseal, metaphyseal, and diaphyseal. The palmar epiphyseal vessels branched from the radial artery, palmar carpal arch, and anterior branch of the anterior interosseous artery. These vessels entered the bone through the radial styloid process at level of the Lister's tubercle but palmar and sigmoid notch. The dorsal contribution to Lister's tubercle is to the dorsal epiphyseal vessels. The intraosseous point of entry to the dorsal epiphyseal vessels was from the fourth and fifth extensor compartment arteries. In the metaphyseal area, we found numerous periosteal and cortical branches originating deep in the pronator quadratus and the anterior interosseous artery. These branches provided the main supply to the distal radius. Vessels perforated the bone and formed an anastomotic network. In the diaphyseal area, only the nutrient vessel provided intraosseous vascularity in the distal radius. Numerous metaphyseal–epiphyseal branches arise within the pronator quadratus and the anterior interosseous artery and course towards the distal radius. These branches may be fundamental to the healing of the distal radius fractures and make nonunion a rare complication.
Keywords: Distal radius, Intraosseous vascularization, Radius vascularity, Spalteholz technique
Introduction
Most studies on wrist fractures stress the importance of extraosseous and intraosseous vascularization of the distal radius and ulna. Those that do [1, 3, 5, 9, 16] discuss wrist problems or surgical treatment in relation to pedicled bone grafts from the dorsal or volar surfaces of the distal radius. The specific works of Shin and Bishop [10–12], Sheetz et al. [9], Haerle et al. [1], and Zaidemberg et al. [17] discuss the external vascularization applied to pedicled vascularized bone graft for scaphoid nonunion or Kienböck's disease. The importance of the distal radius vascularity and the surgical approach has been emphasized by Orbay et al. [6] in the description of the new approach or the distal radius and new techniques of osteosynthesis.
The present study was performed to determine (1) the internal vascularization of the distal radius using the Spalteholz technique [13] and (2) its clinical application to distal radius fractures.
Materials and Methods
Twelve wrists from fresh cadavers, 50 to 90 years old (mean age 68 years), were injected through the brachial artery with latex. Arms were amputated proximal to the elbow joint. The brachial artery was cannulated with a catheter and irrigated with normal saline. Transverse incisions were made over the distal phalanges of all digits. Liquid latex (40–50 cc) was then injected into the brachial artery under firm manual pressure. The adequacy of injection was determined by the appearance of the latex through the transverse incisions in the fingertips. The injected specimens were refrigerated for 12 h to ensure consolidation of the latex. The specimens were then fixed in formalin for 48 h. Dissections were performed using magnifying loupes and all the soft tissues were removed leaving only the wrist joints and bones. The main arteries were dissected and their branches (radial, ulnar, posterior, and anterior interosseous arteries) identified. Wrists were then prepared using the Spalteholz technique [13] so as to clearly reveal the vascularization of the area without dissection artifacts. We took cross and coronal sections of the distal radius and ulna, including the wrist. The sections were immersed in ethanol and dehydrated. The process of dehydration consisted of leaving the sections in 50% ethanol for 1 week and then changing them each week for higher ethanol concentrations up to 100% ethanol. The cross and coronal sections were then immersed in methylbenzene for 2 weeks. Finally, they were placed in a liquid mixture made up of one part methyl salicylate and two parts benzyl benzoate for another 2 weeks. The bones were then completely transparent and photographs of the intraosseous vascularity were taken while the specimens were immersed. Using this technique, it was possible to establish the internal vascularization of each area of the bone and its relation with the external surface and main vessel source.
Results
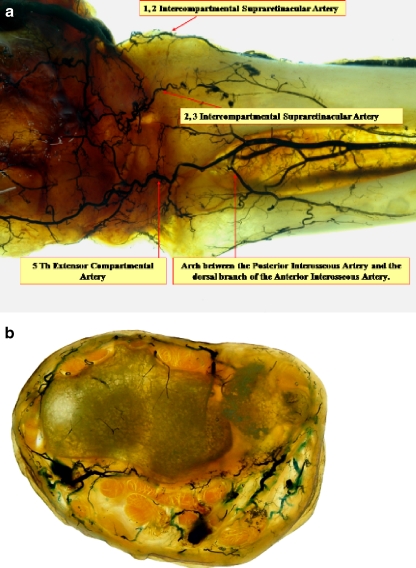
Blood supply to the distal radius includes the radial, ulnar, anterior interosseous, and posterior interosseous arteries. In all specimens, anastomoses between the anterior branch of the anterior interosseous artery and the palmar carpal arch (Fig. 1) and also between the anterior and posterior interosseous arteries and the dorsal carpal arch were always present. Small vessels coming from the anterior interosseous artery and the insertion of the deep part of the pronator quadratus over the sigmoid notch of the radius were also present. The intraosseous areas of vascularization came from these adjacent small branches. The distal radius was supplied by three main vascular systems: epiphyseal, metaphyseal, and diaphyseal. The palmar epiphyseal vessels branched from the radial artery, palmar carpal arch, and anterior branch of the anterior interosseous artery. They entered the bone through three points: the radial styloid process, Lister's tubercle, and the sigmoid notch (Fig. 2). The intraosseous point of entry to the dorsal epiphyseal vessels was from the fourth and fifth extensor compartment arteries (ECA) (Fig. 3). The fourth ECA is located on the radial aspect of the fourth extensor compartment floor. It originates from the posterior division of the anterior interosseous artery or its fifth extensor compartment branch and anastomoses with the dorsal intercarpal arch and the radiocarpal arch. The fifth ECA is supplied by the posterior division of the anterior interosseous artery and anastomoses distally with the dorsal intercarpal arch (Fig. 4). It also may make distal connections to the fourth ECA and the dorsal radiocarpal arch. The fifth ECA provides direct nutrient branches to the radius.
Figure 1.
The anastomoses between the palmar carpal arch and the anterior branch of the anterior interosseous artery.
Figure 2.
Epiphyseal vascularity: penetrating branches in the radial styloid, Lister's tubercle, and sigmoid notch.
Figure 3.
a Extraosseous vascularity: dorsal intercompartmental branches to the distal radius. b Cross section: remark the intraosseous areas of vascularity in the medial and distal part of the radius.
Figure 4.
The fifth ECA is supplied by the posterior division of the anterior interosseous artery and anastomoses distally with the dorsal intercarpal arch.
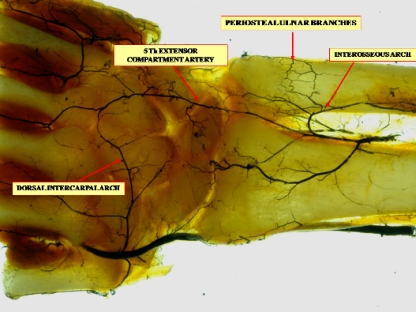
More proximally, in the metaphyseal area, numerous periosteal and cortical branches originated from the anterior interosseous artery as it courses through the pronator quadratus. These branches provided the main supply to the distal radius. The vessels perforated the bone-forming and anastomotic network (Figs. 5, 6, and 7). The metaphyseal arteries are multiple and enter all the periosteal surfaces of the proximal and distal metaphyses. They provide the entire supply of the metaphyses, and their terminal branches anastomose with the terminal branches of the medullary arterioles at each end of the medullary cavity.
Figure 5.
Anatomy to the pronator quadratus (PQ). These branches arise within the PQ and the anterior interosseous artery (AIA) to an anastomotic network in the metaphyseal area of the distal radius.
Figure 6.
Coronal section: the small vessels were coming from the insertion of the deep pronator quadratus (PQ) over the sigmoid notch and radial styloid process.
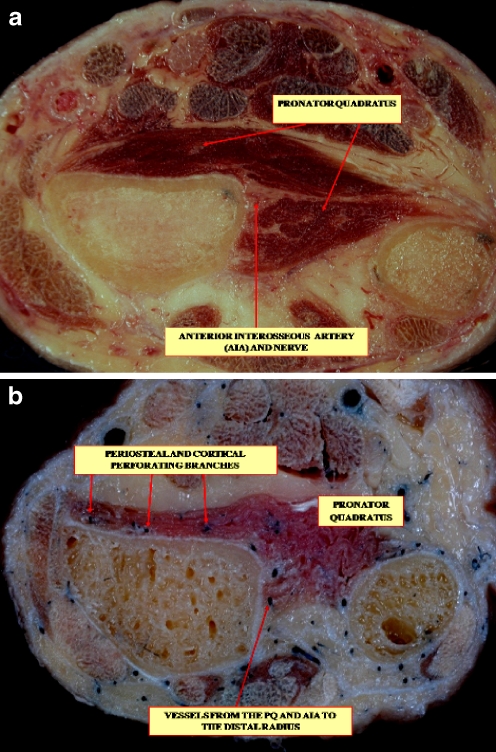
Figure 7.
Cross section: apronator quadratus (PQ) muscle: superficial and deep parts. b Vessels from the PQ and anterior interosseous artery (AIA) to the distal radius.
The nutrient artery provides intraosseous vascularity only to the diaphyseal part of the distal radius. The principal nutrient artery approaches the diaphysis under the protection of a fascial attachment. It traverses the full thickness of the cortex to enter the bone where it divides into the ascending and descending branches of the medullary artery. These branches subdivide into arterioles, which enter the endosteal surface of all portions of the diaphysis.
Discussion
In the present study, we sought information about the internal vascularization of the distal radius and its clinical implications in distal radius fractures. In this anatomical study, our findings were similar to those reported by Trueta [15] in his experimental work concerning radius fractures in rabbits. We observed that in the radius, the periosteum and cortical metaphyseal vessels appeared to be the most important contributors to the intraosseous blood supply. The epiphyseal system was the second group of intraosseous vessels. The diaphyseal group had a few anastomoses with a small caliber to the nutrient vessel. Malunion is the most common complication of the distal radius fracture and is usually the result of lack of treatment. Nonunion, on the other hand, is an extremely rare complication and is most likely to occur in patients with conditions such as diabetes, peripheral vascular disease, or alcoholism [7, 14]. Other common causes are infection and fractures treated with operative intervention. Diagnosis of nonunion is based on the absence of radiographic signs of union at 6 months. Treatment should be individualized but options are reconstructive procedures or wrist arthrodesis [7]. In volar plating and often by the fracture injury itself, the complete pronator quadratus is stripped off the volar radius. Thus, the intraosseous collateral circulation must be sufficient for clinical healing. Any operative approach to the distal radius fracture should not compromise both volar radial and the dorsoulnar arteries [4]. Also, while the branches to the pronator quadratus must be sacrificed in a palmar approach, the distal perforator can and should be spared. This is true even in the flexor carpi radialis extended approach. In distal radius fractures, when the normal outward flow of blood through the cortex is blocked, the periosteal arterioles have more ability than medullary arterioles to function and proliferate [8]. During the healing of undisplaced closed fractures, the medullary circulation remains dominant throughout. With displaced fractures, however, when the main medullary vessels are disrupted, an enhanced periosteal circulation, derived from torn muscles in the vicinity, becomes at first the primary source of blood for the area of healing [8, 15]. As healing progresses, the medullary circulation is re-established across the fracture [8]. The anterior interosseous artery, as the main artery of the periosteal and endosteal supply of the human radius, is important in transplantation and reconstruction, especially with a view to reducing the rate of pseudarthrosis [8, 15].
An angiosome is a composite block of tissue that is supplied anatomically by source (segmental or distributing) vessels that span between the skin and bone. In this way, the angiosomes in the forearm, provided by the brachial, radial, ulnar, and interosseous arteries, were defined by Inoue and Taylor [2]. Results showed that, in most cases, the connections between adjacent angiosomes occurred within tissues, not between them. The skin, the bones, and most muscles received branches from the source arteries of at least two angiosomes, thus revealing one of the important anastomotic pathways by which the circulation is reconstituted in those cases where a source artery is interrupted by disease or trauma [2, 4].
The numerous metaphyseal–epiphyseal branches arise within the pronator quadratus and the anterior interosseous artery and course towards the distal radius. These branches may be fundamental to the healing of the distal radius fractures and make nonunion a rare complication.
References
- 1.Haerle M, Schaller HE, Mathoulin C. Vascular anatomy of the palmar surfaces of the distal radius and ulna: its relevance to pedicled bone grafts at the distal palmar forearm. J Hand Surg Br. 2003;28(2):131–6. [DOI] [PubMed]
- 2.Inoue Y, Taylor GI. The angiosomes of the forearm: anatomic study and clinical implications. Plast Reconstr Surg. 1996;98(2):195–210. [DOI] [PubMed]
- 3.Larson AN, Bishop AT, Shin AY. Dorsal distal radius vascularized pedicled bone grafts for scaphoid nonunions. Tech Hand Up Extrem Surg. 2006;10(4):212–23. [DOI] [PubMed]
- 4.Matthew MK, Hausman MR. Surgical approaches from the angiosomal perspective. Chapter 9. In: Slutsky DJ, Osterman AL, editors. Fractures and injuries of the distal radius and carpus: the cutting edge. Philadelphia: Saunders; 2009. p. 103–23.
- 5.Mih AD. Vascularized bone graft for scaphoid nonunions. Tech Hand Up Extrem Surg. 2004;8(3):156–60. [DOI] [PubMed]
- 6.Orbay J, Badia A, Khoury RK, Gonzalez E, Indriago I. Volar fixed-angle fixation of distal radius fractures: the DVR plate. Tech Hand Up Extrem Surg. 2004;8(3):142–8. [DOI] [PubMed]
- 7.Ovidiu A. Management of complication of distal radius and ulna fractures. IX Instructional Course Lectures of EFORT. J Bone Jt Surg Br. 2002;84(supp III):358–9.
- 8.Rhinelander FW. The normal microcirculation of diaphyseal cortex and its response to fracture. J Bone Jt Surg Am. 1968;50:784–800. [DOI] [PubMed]
- 9.Sheetz KK, Bishop AT, Berger RA. The arterial blood supply of the distal radius and ulna and its potential use in vascularized pedicled bone grafts. J Hand Surg Am. 1995;20:902–14. [DOI] [PubMed]
- 10.Shin AY, Bishop AT. Treatment of Kienböck's disease with dorsal distal radius pedicled vascularized bone grafts. Atlas Hand Clin. 1999;4:91–118.
- 11.Shin AY, Bishop AT. Vascularized bone grafts from the distal radius for disorders of the carpus. J Am Acad Orthop Surg. 2002;2(4):181–94. [DOI] [PubMed]
- 12.Shin AY, Bishop AT. Pedicled vascularized bone grafts for disorders of the carpus: scaphoid nonunion and Kienböck's disease. J Am Acad Orthop Surg. 2002;10(3):210–6. [DOI] [PubMed]
- 13.Spalteholz W. Ueber das Durchsichtigmachen von menschlichen und tierischen Präparaten; nebst Anhang: Ueber Knochenfärburg. Leipzig: S. Hirzel; 1911. p. 3–220.
- 14.Taleisnik J, Kelly P. The extraosseous and intraosseous blood supply of the scaphoid bone. J Bone Jt Surg Am. 1966;48:1125–37. [PubMed]
- 15.Trueta J. Osteogénesis reparadora. In: La estructura del cuerpo humano. Estudio sobre el desarrollo y decadencia. Barcelona, Editorial Labor S.A., 1975. p. 241–251.
- 16.Waitayawinyu T, Robertson C, Chin SH, Schlenker JD, Pettrone S, Trumble TE. The detailed anatomy of the 1,2 intercompartmental supraretinacular artery for vascularized bone grafting of scaphoid nonunions. J Hand Surg Am. 2008;33:168–74. [DOI] [PubMed]
- 17.Zaidemberg C, Siebert JW, Angrigiani C. A new vascularized bone graft for scaphoid nonunion. J Hand Surg Am. 1991;16:474–8. [DOI] [PubMed]