ABSTRACT
Purpose: Programme evaluation has been defined as “the systematic process of collecting credible information for timely decision making about a particular program.” Where possible, findings are used to develop, revise, and improve programmes. Theory-based programme development and evaluation provides a comprehensive approach to programme evaluation.
Summary of key points: In order to obtain meaningful information from evaluation activities, relevant programme components need to be understood. Theory-based programme development and evaluation starts with a comprehensive description of the programme. A useful tool to describe a programme is the Sidani and Braden Model of Program Theory, consisting of six programme components: problem definition, critical inputs, mediating factors, expected outcomes, extraneous factors, and implementation issues. Articulation of these key components may guide physiotherapy programme implementation and delivery and assist in the development of key evaluation questions and methodologies. Using this approach leads to a better understanding of client needs, programme processes, and programme outcomes and can help to identify barriers to and enablers of successful implementation. Two specific examples, representing public and private sectors, will illustrate the application of this approach to clinical practice.
Conclusions: Theory-based programme development helps clinicians, administrators, and researchers develop an understanding of who benefits the most from which types of programmes and facilitates the implementation of processes to improve programmes.
Key words: evaluation, methodology, outcome measurement, programme evaluation, theory
RÉSUMÉ
Objectif: L’évaluation des programmes a été définie comme « le processus systématique de collecte de renseignements crédibles pour la prise de décision en temps opportun sur un programme particulier ». Lorsque c’est possible, les résultats servent à l’élaboration, à la révision et à l’amélioration des programmes. L’élaboration et l’évaluation des programmes fondées sur la théorie fournissent une approche complète de l’évaluation des programmes.
Résumé des points clés: Pour extraire des renseignements significatifs des activités d’évaluation, il faut comprendre les éléments des programmes pertinents. L’élaboration et l’évaluation des programmes fondées sur la théorie commencent par une description détaillée du programme. Le modèle de la théorie des programmes de Sidani et Braden est un outil pratique pour la description d’un programme. Il comporte six éléments: la définition des problèmes, les intrants critiques, les facteurs médiateurs, les résultats prévus, les facteurs extérieurs et les problèmes de mise en œuvre. L’articulation de ces éléments clés peut guider la mise en œuvre et la prestation des programmes de physiothérapie et aider à la formulation des questions d’évaluation et des méthodologies clés. Cette démarche mène à une meilleure compréhension des besoins des clients, des processus et résultats des programmes. Elle aide aussi à identifier les obstacles à la mise en application réussie et les déclencheurs. Deux exemples spécifiques, représentant les secteurs public et privé, illustrent l’application de cette approche de la pratique clinique.
Conclusions: L’élaboration des programmes fondée sur la théorie aide les cliniciens, les administrateurs et les chercheurs à acquérir une compréhension des personnes qui sont le plus avantagées par certains types de programmes et facilite la mise en œuvre des processus d’amélioration des programmes.
Mots clés: évaluation, méthodologie, mesure de résultat, évaluation des programmes, théorie
INTRODUCTION
Physiotherapists have been involved in the evaluation of their clinical practice for many years, primarily through the administration of outcome measures in clinical care. The literature clearly reflects the strong contribution made by the physiotherapy community in the move toward outcome measurement.1,2 This approach has led physiotherapists to focus on the causal connection between the intervention and the intended outcome; outcome findings have been the main criteria in determining whether a programme was effective. Recently there has been increased emphasis on accountability and efficiency, requiring an understanding of outcomes as well as of the processes underlying those outcomes.
The theory-based programme development and evaluation model provides a practical approach to understanding the how and the why of a given programme, thereby providing insight into how to develop, refine, and improve it. This model helps to identify the various components of a programme in order to determine, through evaluation, what is working and what is not; this provides the basis for decisions about whether and how to modify the programme.
A programme has been defined as “any organized or purposeful activity or set of activities delivered to a designated individual or target group.”3 In a physiotherapy context, a programme can consist of a class, an educational pamphlet, a prescribed regimen, individual or group treatments, or a combination of interventions. According to this definition, all physiotherapists delivering professional services are involved in a programme.
Programme evaluation has been defined as “the systematic process of collecting and using credible information for timely decision making about implementing, operating, modifying, continuing, and/or expanding a program.”3 Of critical importance in this definition is that data are collected in a systematic, consistent manner and that they provide valid and reliable information that can be used to make informed decisions about a programme.
As identified earlier, physiotherapists have used outcome measures in their practice to report on client- and programme-specific benefits of interventions. For example, in a balance improvement programme, changes in number of falls or scores on a balance measure are used to reflect benefits. There has been less focus on the factors that may explain why or how a client benefits from the programme. These factors may be client-related (e.g., client attitude toward exercise), programme-related (e.g., staffing requirements), or system-related (e.g., access to funding). In describing these other factors, we are moving toward an understanding of the theory underlying the programme. If available, sound theory provides insight into the active components of our practice. It is the authors’ experience that, as physiotherapists, we are not always clear on what we do, for whom, and why. This phenomenon is not uncommon in rehabilitation and, in the literature, is referred to as the “black-box approach” to intervention.4
Several different frameworks to describe a programme's theoretical basis have been provided.5 Any of these frameworks can facilitate the development of a comprehensive programme description. Where they differ is in the specific components or factors used for description. Examples of programme theories are the “theory of cause and effect” and “theory of implementation” described by Grembowski.5 The framework found by the authors to be most clinically relevant was originally developed by Lipsey6 and modified by Sidani and Braden.7 The modified model, referred to as the programme description7 in this paper, consists of six components: problem definition, critical inputs, mediating processes, expected outcomes, extraneous variables, and implementation issues. These will be discussed in detail in the next section. Determining the most suitable framework and completing the different components are important first steps in developing a new programme or in refining or understanding an existing programme. The completed framework should reflect the context of the particular programme and articulate what the current evidence supports. This will also help identify where there is strong evidence supporting a programme and where there are gaps in theory and knowledge that limit the direct application of literature findings into practice.
In programme evaluation literature, the word “development” is used both when planning for a new programme and when revising or refining an existing programme. The term “programme development,” as applied to the examples in this paper, refers to the ongoing development or refinement of an existing programme.
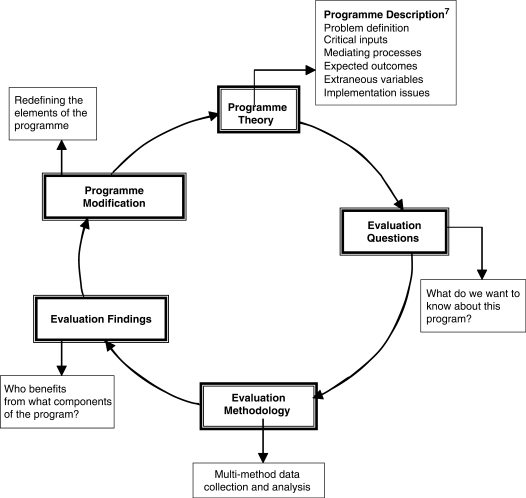
The Theory-Based Development and Evaluation Cycle is shown in Figure 1. Programme theory is clearly articulated, using the model of programme description discussed by Sidani and Braden.7 Details of these six components provide a rich, evidence-based, and practice-related description of the programme and form the basis for programme implementation.8 Programme theory, broken down in this way, helps us to identify the strong components of the programme as well as any deficits in knowledge or understanding, leading to relevant and pertinent evaluation questions. These questions then guide what evaluation methodology should be used for data collection and analysis. The results or evaluation findings will identify what is (or is not) effective in a programme, provide an evidence-based impetus for changes to the programme, and guide modification of the appropriate programme elements. The completion of the cycle is a refined articulation of programme theory.
Figure 1.
Programme development and evaluation cycle
In summary, this evaluation cycle takes us through the process of describing the elements of a programme that provide the theoretical basis of the programme, determining what questions to ask, and, through analysis of the data, redefining the programme elements. When these changes in theory are operationalized through changes in programme implementation, we are effectively improving the programme. This cycle provides a strong connection between programme theory and evaluation. The programme theory is the foundation for this cycle, and its clinical applicability is therefore essential. Sidani and Braden's model of programme description has been shown to be clinically useful in the development of an exercise and education programme for adults with diabetes8 and in nursing and interprofessional team practice.7,9,10 When applied to a particular client population, the six components in the model help to specify a detailed description of the problem (problem definition), articulate specific programme activities that may address the problem (critical inputs) and the reasons for the particular interventions and approach taken (mediating processes), predict the expected benefits to clients (expected outcomes), and identify factors affecting clients’ ability to benefit (extraneous factors) and programme resources (implementation issues).
This model is described below and two practical, clinical examples used to illustrate its application to physiotherapy programmes. The first example is a community-based self-management programme for persons who have had a stroke and their care partners, the Moving On after STroke (MOST) programme, delivered within the public health care system. The second example is a Community Clinic Back (CCB) programme for patients with non-specific low back pain (LBP) in a private orthopaedic practice. The examples do not provide a comprehensive overview of all theoretical aspects of these programmes but, rather, serve to illustrate how the framework facilitates the articulation of the programme's theory and how the theory supports programme development and evaluation. Tables 1 and 2 provide a summary of the essential elements for the MOST and CCB programmes respectively.
Table 1.
Summary Programme Components of the Moving On after STroke (MOST) Programme
| Problem Definition | Critical Inputs | Mediating Processes | Expected Outcomes | Extraneous Factors | Implementation Issues |
|---|---|---|---|---|---|
|
|
|
|
|
|
↑ = increased; ↓ = decreased
Table 2.
Summary Components of a Community Clinic Back (CCB) Programme
| Problem | Critical Inputs | Mediating Processes | Expected Outcomes | Extraneous Factors | Implementation Issues |
|---|---|---|---|---|---|
|
|
|
|
|
|
ADL = activities of daily living
LBP = low back pain
OT = occupational therapist
PT = physiotherapist
ROM = range of motion
WSIB = Workplace Safety & Insurance Board
↑ = increased
↓ = decreased
Problem Definition
The problem definition clarifies the specific issues that are being addressed by the programme and includes information on the condition, the target population, and specific circumstances.6,7 It also includes information on different interventions aimed at addressing the problem as well as barriers to their successful implementation.
Problem Definition in MOST
There is a high incidence of stroke in Toronto.11 Many individuals who survive stroke and appear to have good recovery from an impairment perspective continue to have significant limitations from the perspectives of activity and social participation.12 When these individuals return to the community, they have often not learned to live with the impact of their stroke,13 and their care partners struggle with the changes in their relationship and in other aspects of their lives.14,15
Successful return to community living and social participation after a stroke requires an ability to deal with the consequences of the stroke, such as fatigue, difficulty in moving around in the community, difficulty with transportation in general, increased need for physical assistance in activities of daily living (ADL), and return to meaningful activity. Educational programmes for persons with chronic stroke have been effective in improving patient and care partner knowledge but have not been successful in enhancing health behaviours and well-being.16–18 Psychosocial interventions that focus on problem-solving skills appear to be more effective in changing behaviour or improving well-being,13,16,19 and the benefits of community exercise programmes post-stroke have been well established.20,21 In other chronic conditions, self-management programmes (SMPs) have been more successful than traditional educational programmes in meeting clients’ needs. SMPs empower clients to take responsibility for managing their condition, with guidance and support from peers and health professionals.22 This approach appears to be relevant to stroke rehabilitation, but its effectiveness in this population has not yet been tested.
Problem Definition in the CCB Programme
There is a high incidence of non-specific, non-radiating LBP in the workforce between the ages of 20 and 55 years.23 This usually presents as localized pain; decreased range of motion (ROM); muscle weakness; and functional limitations at work, at home, and in leisure activities.23 Typical physiotherapy treatment includes mobilization, stretching, and strengthening exercises. More recently, it has been identified that advice to stay active, education and reassurance, and a behavioural approach to treatment may decrease the time between onset and return to social participation (i.e., work and previous levels of activity).24,25 Overall, more evidence to guide intervention is required.
Critical Inputs
Critical inputs embody a detailed articulation of key components or activities that should be present in the programme. The critical inputs address the nature of the intervention—what should be done or is necessary to produce the expected effects.6,7 Furthermore, they guide the implementation of the intervention and specify the activities to be performed in delivering it; ideally, they detail the procedures to be followed and the amount, frequency, duration, and intensity of the intervention activities.7
Critical Inputs for MOST
Pre and post- programme client assessment is an integral part of programme activities in MOST. The general constructs captured in the assessment are discussed under “Expected Outcomes.”
MOST includes information sharing, problem solving, exercise, and goal setting.26,27 Participants meet for two hours, twice a week, for eight weeks. Six weeks after the end of the programme, they get together again for a booster session. The literature indicates that areas of interest to survivors of stroke and their care partners include, but are not limited to, information on stroke, primary and secondary prevention, medications,14 leisure, transportation, fatigue, intimacy,28 cognition,29 aphasia and other communication issues, physical and psychosocial coping, exercise, and community resources.28
The educational component promotes learning through interactive and practical problem solving and skill mastery. This is facilitated by the group format, whereby clients are encouraged to share experiences, to learn from each other, and to receive and provide social support.30 Goal setting with regular feedback and support is an additional strategy used in the programme. Early on in the programme, participants set one long-term goal for completion by the end of the programme, as well as biweekly short-term goals. During every session, participants exercise for about 50 minutes on land or in the water. The exercise programme includes stretching, strengthening, balance, and cardiovascular activities.20,31
Critical Inputs for the CCB Programme
Because of the client-specific nature of non-specific LBP, an individual client assessment is essential to determine the most pertinent issues from the perspectives of impairment, activity, and participation, including fear–avoidance beliefs.32,33 The specific assessment will be addressed in greater detail under “Expected Outcomes.” Client intervention typically includes advice to stay active,24 individualized exercise programmes,34 weekly or biweekly goal setting, functional restoration, and facilitation of timely return to work.35 Clients require specific opportunities to practise the exercises and functional activities and are encouraged to carry out the programme activities independently and with sufficient frequency to optimize return to normal functioning. Sufficient frequency is usually on a daily basis but is reviewed and revised based on progress and weekly goal attainment. The time required to complete assigned programme activities varies according to assessment findings and the demands of the client's functional activities. Client education consists of individual sessions as well as the provision of relevant print materials. These interventions are provided within a behavioural approach32,33 in which positive health behaviours are encouraged.25
Mediating Processes
Mediating processes represent the series of changes that occur in participants as a result of the intervention and form the linkages or connections between the critical inputs or programme activities and the expected or desired outcomes.8 Mediating processes can be interpreted as a series of changes that ultimately lead from the intervention to the desired outcome.
Mediating Processes in MOST
Within MOST, the most important theoretical framework for understanding the mediating processes involved in acquiring and maintaining the skills and attitudes needed for successful living with stroke in the community is social cognitive theory.36,37 In social cognitive theory, self-efficacy, or a person's confidence in his or her ability to perform a particular activity, is considered the personal characteristic that is most important in influencing behaviour change.37,38 Self-efficacy is enhanced through skill mastery, observing practice and success in others, verbal persuasion, and appropriate interpretation of physical cues. Studies have shown that social support has an effect on aspects of well-being such as self-reported psychological distress.30,39 MOST can facilitate self-efficacy and social support by bringing together people with similar concerns; by providing opportunities for goal setting, group problem solving, and practising new skills, including exercise; and by promoting linkages to other community groups.30,39
Mediating Processes in the CCB Programme
In the programme for non-specific LBP, the connections between critical inputs or programme activities and expected outcomes are captured in theories that consider physiological and psychosocial processes that facilitate attainment of the expected outcomes, in particular return to ADL and work. From a physical perspective, actual physical capacity plays an important role. Physical aspects of the intervention, such as exercise and functional restoration, are effective in improving ROM, core stability, and aerobic capacity, which, in turn, are expected to restore physical capacity.33 Motor learning theory supports the repeated practice of functional activities in order to enhance the competence and skill required in ADL and at work.40 Some of the psychosocial theories supporting the physiotherapy interventions are theories of knowledge,41 behaviour modification, self-efficacy, and self-determination.42 During the physiotherapy intervention, positive behaviours conducive to a return to activity are encouraged. Self-efficacy and self-determination also play a role in enhancing outcomes. Clients’ confidence in their ability to return to work successfully and their intrinsic motivation are optimized through participation in goal setting, practice of exercise and functional activities, therapist feedback, and a better understanding of physical cues such as pain.26,37,43 Knowledge alone does not lead to changes in behaviours and well-being,43 but it is a prerequisite for behaviour change. With this understanding, a patient is encouraged to make positive changes by adhering to recommendations around exercise prescription and work-related practices and habits.44
Expected Outcomes
Expected outcomes represent the desired changes in the client's status and behaviour following the intervention. Outcomes need to be linked to the problem definition, critical inputs, and mediating factors. For a full assessment of programme impact, not only the nature of the intended outcomes but also the anticipated patterns, timing, and sequence of change need to be described. Some changes occur immediately after the intervention, whereas others take longer to appear.7 These outcomes can be assessed by administration of specific outcome measures or scales. For many physiotherapy-related outcomes, times and patterns of improvement are not known.
Expected Outcomes in MOST
The primary desired outcome for MOST is a reduction in the burden of stroke at the personal, family, and community levels. For the individual, this involves improvements in level of self-efficacy, activity, well-being, participation in formal exercise, and social participation. For the family, it means improvements in the care partner's well-being and in the burden of care. For the community, a reduction in burden can be interpreted as improved social participation, reductions in risk factors and stroke recurrence, a decrease in unnecessary medical visits, and decreased rates of hospitalization and institutionalization.
Expected Outcomes for the CCB Programme
For the CCB programme, the outcomes relate to changes in physical impairments, fear–avoidance beliefs, activity levels, and participation. Initially, improvements in ROM, muscle recruitment, pain, and amount of pain medication taken are anticipated. These changes may lead to improvements in functional status and in clients’ perceptions of their functional ability. The ultimate outcomes relate to areas of social participation, such as successful return to work and participation in leisure activities. Furthermore, the time between onset and return to activity, including work, may be an important indicator of programme effectiveness, especially from an employer's perspective. An additional important outcome is the level of recidivism or recurrence of back pain and absence from work.
Extraneous Factors
Extraneous factors include those related to the treatment conditions, the external health care environment, and the personal and cultural characteristics of the client and of the person providing the intervention.6–8 These factors are all outside the direct influence of the programme and may affect treatment processes and client outcomes, either directly or indirectly, by moderating intervention effects.7,45
Extraneous Factors in MOST
Some of the environmental factors influencing health behaviours and programme participation are cultural and religious beliefs and practices, such as attitude toward aging, disability, and exercise.46 Factors affecting referral include a lack of understanding among health care providers of the possible benefits of community-based stroke education programmes.47 Access to the programme may be affected by programme costs when there is a lack of funding through provincial or private health insurance plans.48 Practical issues such as the availability of transportation, the accessibility of programme location, and the need for specific exercise clothing will also affect participation.48
Participant characteristics such as age, gender, level of education, literacy, language issues, pre-morbid lifestyle,7 socio-economic status,49 level of impairment and activity, cognition, communication,18 and pre-morbid levels of functioning may all influence the ability to benefit from a group programme.
Extraneous Factors in the CCB Programme
The Ontario Health Insurance Plan provides limited coverage for physiotherapy. Unless they have personal financial resources, have private insurance, or qualify for Workplace Safety and Insurance Board (WSIB) benefits, people with LBP will have limited access to comprehensive services. The ability to attend the programme and to have a graduated return to work is also influenced by the expectations of employers, WSIB, and insurance agencies.
Many other personal and work-related attributes may influence clients’ return to activity and work. These include the specific physical demands of the job, the employer's support for graduated or modified duties, workplace satisfaction, and the client's personal support system. Personal characteristics of the intervener are also very important in the delivery of the CCB programme. Therapists need to reassure and encourage these clients successfully as well as to engage them in goal setting and problem solving.
Implementation Issues
Implementation issues relate to the resources required for delivering the programme—not only the setting, equipment, and programme materials but also the professional qualifications of the interveners,7 as well as including the costs involved. Professional qualifications, including educational expertise, professional background, specialty training, and competence, will affect the technical and interpersonal aspects of care.7
Implementation Issues in MOST
Group educational programmes for persons who have had a stroke require space that can accommodate all participants and their assistive devices. The facility needs to be wheelchair accessible, with appropriate exercise space and equipment. A programme manual needs to be developed for participants and for the facilitators. Development of the manual requires interdisciplinary collaboration to ensure that content, format, and reading level are accurate and appropriate for the target group.26 Audiovisual resources may need to be included. If the programme is not completely funded under the public health insurance system, subsidies may need to be available to those who cannot otherwise afford to participate.
Because of the limited understanding of the benefits of stroke group programming, client recruitment and screening are ongoing issues. Programme staff members need appropriate knowledge and group facilitation skills; therefore, training may be required. Programme delivery, including assessment, educational and exercise sessions, and goal-setting procedures, requires large amounts of staff time. In cases of non-attendance, timely professional contact may be an important strategy to facilitate programme participation.8 Long-term adherence to new health behaviours may require follow-up or booster sessions.50 Collaboration between professional and support staff is required to ensure that the programme is delivered most effectively and efficiently.
Implementation Issues in the CCB Programme
Intervention for patients with non-specific LBP requires physiotherapists who can provide standardized assessments, analysis, and evidence-based treatment approaches. However, kinesiologists or physiotherapy assistants may also be involved to ensure the most appropriate staffing mix from skill and cost perspectives.
From the perspective of physical resources, space for individual interventions and assessments is needed. Equipment that allows for activity progression is beneficial, particularly when the client is close to returning to work or is involved in the heavier aspects of a work-conditioning programme. Appropriate educational materials are required. Funding organizations such as WSIB have significant requirements for documentation of client assessment, interventions, and the recovery protocol. These can be time consuming for the treating therapist and support personnel. Timely reimbursement is also a concern requiring dedicated staff time.
THE ITERATIVE LOOP OF THEORY-BASED PROGRAMME DEVELOPMENT → EVALUATION
As the foregoing examples illustrate, the Sidani and Braden model provides a guide to detailed programme description.7 These descriptions guide programme development, clarify the different components of a programme and minimize the “black-box approach” to intervention. They also help us understand where our clinical practice deviates from best practice as described in the literature. These gaps or discrepancies may provide optimal opportunities for programme evaluation, as is illustrated below with examples from the MOST and CCB programmes.
Figure 1 illustrates the iterative cycle of programme development and evaluation. As identified earlier, programme theory, as articulated in the detailed programme description, is the foundation of the cycle. In ideal circumstances, programme theory is an evidence-based guide to programme implementation. The state of knowledge is fluid, however, and all programme processes and mechanisms may have to be re-adjusted as new evidence becomes available.45 Moreover, rarely, if ever, do client populations, resources, and environmental conditions all match the controlled research situation. Local adjustments and adaptations are almost always necessary when applying programme theory to any local health care programme, including physiotherapy programmes. These adjustments provide the most meaningful opportunities for evaluation and for building new knowledge.
Programme Development and Evaluation Cycle for MOST
When MOST was implemented, self-management programmes were new for persons who had experienced stroke. There were many gaps in knowledge, and it was decided that initial evaluation questions needed to address programme implementation and client outcomes. Specific questions pertain to specific elements articulated in the programme description:
What is the profile of individuals who indicate initial interest in the programme and who subsequently enrol in and complete the programme?
What are the barriers to initial and continued participation?
What are the benefits of participation in MOST?
Questions 1 and 2 address perceived problem definition and extraneous factors, while question 3 addresses expected outcomes. The method chosen to explore the first two questions was a semi-structured survey, completed by the programme intake coordinator when persons with stroke or their care partners contacted the programme. The survey addressed client demographics, stroke specifics, reason for registration, and issues that could affect attendance (e.g., transportation, subsidy needs, and language). Clients were also asked how they found out about the programme, whether anyone had referred them, and what made them decide to contact the programme. Health professionals contacting the programme were asked about perceived needs, typical referral patterns in their practice, and suggestions for recruitment. To find out about the benefits of MOST, specific outcome measures were administered, and, in a focus group setting, clients were asked about their perceived benefits. Clients also were asked why they were successful in certain areas of goal setting and not in others.
Some of the evaluation findings indicated that potential clients who learned about the programme from a health professional were more likely to register and that transportation affected initial enrolment and adherence to the programme. These findings have subsequently changed how the programme is advertised and how recruitment and screening activities are carried out. The outcome evaluation indicated improvements in exercise levels, confidence to move around in the community, and social participation. The focus group also indicated that participants highly valued the opportunities for social support in the group and that it was hard for them to make independent contacts with community agencies. These findings have affected how goal setting and community participation are facilitated, as well as the need for a more objective measure of social support as an outcome indicator. Ongoing evaluation will determine whether these changes have been successful. Moreover, some of the evaluation activities, particularly the focus groups, provided additional insights into participants’ post-stroke lives and will further contribute to programme development of MOST.
Programme Development and Evaluation Cycle for the CCB Programme
Initially, CCB programme clients received primarily individual education and one-on-one intervention, with a focus on mobility and strengthening activities. As the programme evolved, it became more comprehensive in scope, adding education, reassurance, and advice on returning to regular activities, as well as addressing fear–avoidance issues. During reassessments, therapists noted that clients’ adherence to exercise prescriptions was variable and generally less than expected, and that this seemed to be true consistently across clients. Consequently, the programme addressed the following evaluation questions:
What is the actual level of adherence to exercise prescriptions?
What are the reasons for limited adherence?
Do programme activities need to be changed or added to enhance adherence?
Questions 1 and 3 addressed the critical inputs of the programme. The reasons for limited adherence (question 2) may lie in shortcomings in the problem definition, in mediating processes, or in extraneous factors. The data-collection method chosen to answer the first question was a client survey exploring the frequency and number of exercises clients performed outside of scheduled therapy time. In addition, clients were asked during treatment to demonstrate each exercise, in order for the physiotherapist to observe the techniques. In most instances, it was evident that clients had practised their exercise routines differently from how they had been instructed. It was concluded that exercise prescription adherence was low. In order to answer questions 2 and 3, the literature was reviewed to identify factors important in programme adherence. These factors were used to explore clients’ reasons for limited adherence and to develop strategies for enhancing adherence. The most important findings were that clients found it difficult to find the space, time, and motivation to exercise at home; that they found it difficult to perform unfamiliar exercises without guidance; and that they had difficulty appreciating the relationship between the individual exercises and their ability to perform their work- and home-related activities. While the lack of space and time would be considered extraneous factors, the other reasons can be considered mediating processes. Understanding these extraneous factors and mediating processes led to a change in critical inputs. The programme was then modified such that gym facilities were made available to clients, physiotherapists reduced the exercise recommendations to one or two exercises per session, handouts and video educational materials were made available to clients, diagrams of exercises were provided, and, at specific times, a kinesiologist was available to provide assistance with the exercise programmes. Moreover, therapists spent more time explaining the purpose of specific exercises in terms of reducing pain, increasing mobility, or increasing strength and their relevance to the client's specific functional requirements, such as prolonged sitting or repetitive forward reaching. Currently the clinic is collecting data to determine whether there is a change in reported exercise adherence and whether further changes in practice need to be made.
IMPLICATIONS FOR PHYSIOTHERAPY PRACTICE
Recent emphasis on outcome measurement in the physiotherapy literature has strengthened physiotherapy practice. However, outcome measurement highlights only one aspect of the clinical picture and does not explain why certain programmes are effective while others are not, nor why some clients benefit within a programme and others do not. A comprehensive description of a programme using the six essential elements of Sidani and Braden's model of programme theory7 clarifies what the programme is about and allows for development of pertinent questions that can be addressed within the programme development and evaluation cycle. Conducting evaluation in a clinical practice environment and applying best-practice principles may further clinical knowledge, may better explain specific clinical outcomes, and will guide ongoing programme development as well as ongoing evaluation.
In the current “accountability climate,” rehabilitation professionals are often required to report to funding agencies on specific client outcomes and on the intensity and duration of interventions.51 Reports produced by these funding bodies inform organizations of whether or not they are meeting the benchmark. It is important for programmes to be able to identify client-specific issues (e.g., co-morbidities) or programme-delivery issues (e.g., delays in admittance or shortages in skilled programme staff) that may influence these outcomes. Such information is useful in explaining deviations from the standard or expected outcome. Understanding the factors that influence client outcomes and programme delivery is essential. In effect, knowledge of programme theory may explain why a programme is or is not effective or why one programme is more effective than another for specific client populations. This is important not only in accounting for current practices and outcomes but also in optimizing practice.
SUMMARY AND CONCLUSION
Application of a theory-driven framework facilitates a comprehensive understanding of the clinical context of physiotherapy practice and guides the choice of evaluation methods. This enhances the credibility and usefulness of evaluation findings in the clinical setting, ultimately resulting in more effective and efficient programmes.
ACKNOWLEDGMENT
We wish to acknowledge Dr. Anita Myers for her inspiration and ongoing mentorship in program evaluation, and Anne Levin and Rebecca Gruber for their support and constructive feedback during the preparation of this manuscript.
Huijbregts MPJ, Kay T, Klinck B. Theory-Based Programme Development and Evaluation in Physiotherapy. Physiother Can. 2008;60:40–50.
REFERENCES
- 1.Mayo N. Outcome measures or measuring outcome. Physiother Can. 1994;46:145–8. [PubMed] [Google Scholar]
- 2.Mayo N, Cole B, Dowler J, Finch E. Use of outcome measurement in physiotherapy: survey of current practice. Can J Rehabil. 1993;7:81–2. [Google Scholar]
- 3.Myers A. Program evaluation for exercise leaders. Champaign, IL: Human Kinetics; 1999. [Google Scholar]
- 4.Hart E. Evaluating a pilot community stroke service using insights from medical anthropology. J Adv Nurs. 1998;27:1177–83. doi: 10.1046/j.1365-2648.1998.00646.x. [DOI] [PubMed] [Google Scholar]
- 5.Grembowski D. The practice of health program evaluation. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- 6.Lipsey MW. Theory as method: small theories of treatments. New Dir Program Eval. 1993;57(Spring):5–38. [Google Scholar]
- 7.Sidani S, Braden CJ. Evaluating nursing interventions: a theory-driven approach. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 8.Tudor-Locke CE, Myers AM, Rodger NW. Development of a theory-based daily activity intervention for individuals with type 2 diabetes. Diabetes Educ. 2001;27(1):85–93. doi: 10.1177/014572170102700110. [DOI] [PubMed] [Google Scholar]
- 9.Sidani S, Epstein DR, Moritz P. An alternative paradigm for clinical nursing research: an exemplar. Res Nurs Health. 2003;26:244–55. doi: 10.1002/nur.10086. [DOI] [PubMed] [Google Scholar]
- 10.Sidani S, Sechrest L. Putting program theory into operation. Am J Eval. 1999;20:227–38. [Google Scholar]
- 11.Joint Stroke Strategy Working Group . Towards an integrated stroke strategy for Ontario. Toronto: Ministry of Health and Long-Term Care; 2000. Jun, [Google Scholar]
- 12.McEwen S, Mayo N, Wood-Dauphinee S. Inferring quality of life from performance based assessments. Disabil Rehabil. 2000;22:456–63. doi: 10.1080/09638280050045938. [DOI] [PubMed] [Google Scholar]
- 13.Glass TA, Dym B, Greenberg S, Rintell D, Roesch C, Berkman LF. Psychosocial intervention in stroke: families in recovery from stroke trial (FIRST) Am J Orthopsychiatr. 2000;70:169–81. doi: 10.1037/h0087746. [DOI] [PubMed] [Google Scholar]
- 14.Johnson J, Pearson V, McDivitt L. Stroke rehabilitation: assessing stroke suvivors’ long-term learning needs. Rehabil Nurs. 1997;22:243–8. doi: 10.1002/j.2048-7940.1997.tb02110.x. [DOI] [PubMed] [Google Scholar]
- 15.van Veenendaal H, Grinspun D, Adriaanse HP. Educational needs of stroke survivors and their family members, as perceived by themselves and by health professionals. Patient Educ Couns. 1996;28:265–76. doi: 10.1016/0738-3991(95)00853-5. [DOI] [PubMed] [Google Scholar]
- 16.Johnson J, Pearson V. The effects of a structured education course on stroke survivors living in the community. Rehabil Nurs. 2000;25:59–65. [Google Scholar]
- 17.Rausch M, Turkoski B. Developing realistic treatment standards in today's economic climate: stroke survivor education. J Adv Nurs. 1999;30:329–34. doi: 10.1046/j.1365-2648.1999.01080.x. [DOI] [PubMed] [Google Scholar]
- 18.Rodgers H, Atkinson C, Bond S, Suddes M, Dobson R, Curless R. Randomised controlled trial of a comprehensive stroke education program for patients and caregivers. Stroke. 1999;30:2585–91. doi: 10.1161/01.str.30.12.2585. [DOI] [PubMed] [Google Scholar]
- 19.Lovett S, Gallager D. Psychoeducational interventions for caregivers: preliminary efficacy data. Behav Ther. 1988;19:321–30. [Google Scholar]
- 20.Eng J, Chu KS, Kim CM, Dawson AS, Carswell A. A community-based group exercise program for persons with stroke. Med Sci Sports Exerc. 2003;35:1271–8. doi: 10.1249/01.MSS.0000079079.58477.0B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salbach NM, Mayo NE, Wood-Dauphinee SL, Hanley JA, Richards CL, Cote R. A task-orientated intervention enhances walking distance and speed in the first year post stroke: a randomised controlled trial. Clin Rehabil. 2004;18:509–19. doi: 10.1191/0269215504cr763oa. [DOI] [PubMed] [Google Scholar]
- 22.Lorig K. Self-management of chronic illness: a model for the future. Generations. 1993;17(3):11–4. [Google Scholar]
- 23.Spitzer W, LeBlanc F, Dupuis M. Scientific approach to the assessment and management of activity related spinal disorders: a monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. 1987;12:SI–S59. Spine. [PubMed] [Google Scholar]
- 24.Abenhaim L, Rossignol M, Valat J, Nordin M, Avouac B, Blotman F, et al. The role of activity in the therapeutic management of back pain. Report of the International Paris Task Force on Back Pain. 2000;25(4):1S–33S. doi: 10.1097/00007632-200002151-00001. Spine. [DOI] [PubMed] [Google Scholar]
- 25.Lundstrom I, Ohlund C, Eek C, Wallin L, Peterson L, Fordyce W, et al. The effect of graded activity on patients with subacute low back pain: a randomized prospective clinical study with an operant-conditioning behavioural approach. Phys Ther. 1992;72:279–93. doi: 10.1093/ptj/72.4.279. [DOI] [PubMed] [Google Scholar]
- 26.Lorig K. Patient education: a practical approach. Thousand Oaks, CA: Sage Publications; 1996. [Google Scholar]
- 27.Taal E, Rasker JJ, Wiegman O. Patient education and self management in the rheumatic diseases: a self-efficacy approach. Arthrit Care Res. 1996;9:229–30. doi: 10.1002/1529-0131(199606)9:3<229::aid-anr1790090312>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 28.Wiles R, Pain H, Buckland S, McLellan L. Providing appropriate information to patients and carers following a stroke. J Adv Nurs. 1998;28:794–801. doi: 10.1046/j.1365-2648.1998.00709.x. [DOI] [PubMed] [Google Scholar]
- 29.Hanger HC, Walker G, Paterson LA, McBride S, Saisbury R. What do patients and their carers want to know about stroke? A two year follow up study. Clin Rehabil. 1998;12:45–52. doi: 10.1191/026921598668677675. [DOI] [PubMed] [Google Scholar]
- 30.Gonzalez VM, Goeppinger J, Lorig K. Four psychosocial theories and their application to patient education and clinical practice. Arthrit Care Res. 1990;3:132–43. [PubMed] [Google Scholar]
- 31.Chu KS, Eng J, Dawson AS, Harris JE, Ozkaplan A, Gylfadottir S. Water-based exercise for cardiovascular fitness in people with chronic stroke: a randomised controlled trial. Arch Phys Med Rehabil. 2004;85:870–4. doi: 10.1016/j.apmr.2003.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bekkering GE, Hendriks HJM, Koes BW, Oostendorp RAB, Ostelo RWJG, Thomassen JMC, et al. Dutch physiotherapy guidelines for low back pain. Physiotherapy. 2003;89:82–96. [Google Scholar]
- 33.Swinkels ICS, van den Ende CHM, van den Bosch W, Dekker J, Wimmers RH. Physiotherapy management of low back pain: does practice match the Dutch guidelines? Aust J Physiother. 2005;51:35–41. doi: 10.1016/s0004-9514(05)70051-9. [DOI] [PubMed] [Google Scholar]
- 34.Philadelphia Panel. Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for low-back pain. Phys Ther. 2001;81:1641–74. [PubMed] [Google Scholar]
- 35.Grimmer K, Milanese S, Bialocerkowski A. Clinical guidelines for low back pain: physiotherapy perspective. Physiother Can. 2003;55:185–94. [Google Scholar]
- 36.Baranowski T, Perry CL, Parcel GS. How individuals, environments, and health behaviour interact. In: Glanz K, Marcus Lewis F, Rimer BK, editors. Health behaviour and health education: theory, research, and practice. San Francisco: Jossey-Bass; 1997. pp. 153–78. [Google Scholar]
- 37.Bandura A. Self efficacy: the exercise of control. New York: W.H. Freeman; 1997. [Google Scholar]
- 38.Lorig KR, Mazonson PD, Holman HR. Evidence suggesting that health education for self management in patients with chronic arthritis has sustained health benefits while reducing health care costs. Arthritis Rheum. 1993;36:439–46. doi: 10.1002/art.1780360403. [DOI] [PubMed] [Google Scholar]
- 39.Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Marcus Lewis F, Rimer BK, editors. Health behaviour and health education: theory, research, and practice. San Francisco: Jossey-Bass; 1997. pp. 179–205. [Google Scholar]
- 40.Schmidt RA, Lee TD, editors. Motor control and learning: a behavioural emphasis. 3rd. Windsor (Ontario): Human Kinetics; 1999. [Google Scholar]
- 41.Kole-Snijders A, Goossens M, Heuts P, Vlaeyen J, Rutten-van Molken M, van Breukelen G, et al. Chronic low back pain: what does cognitive coping skills training add to operant behavioural treatment: results of a randomized controlled trial. J Consult Clin Psychol. 1999;67:931–44. doi: 10.1037//0022-006x.67.6.931. [DOI] [PubMed] [Google Scholar]
- 42.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 43.Lorig K, Konkol L, Gonzalez VM. Arthritis patient education: a review of the literature. Patient Educ Couns. 1987;10:207–52. doi: 10.1016/0738-3991(87)90126-1. [DOI] [PubMed] [Google Scholar]
- 44.Rollnick S, Heather N, Bell A. Negotiating behaviour change in medical settings: the development of brief motivational interviewing. J Mental Health. 1992;1:25–37. [Google Scholar]
- 45.Pawson R, Tilley N. Realistic evaluation. Thousand Oaks, CA: Sage Publications; 1997. [Google Scholar]
- 46.Rowe JW, Kahn R. Successful aging. Gerontologist. 1997;37:433–40. doi: 10.1093/geront/37.4.433. [DOI] [PubMed] [Google Scholar]
- 47.Houghton A, Logan S, Mahoney H, Wong S. Community resources for stroke survivors: an implementation strategy to facilitate change of practice in acute care. Toronto: University of Toronto; 2001. Apr, [Google Scholar]
- 48.Rimmer JH, Hedman GA. A health promotion program for stroke survivors. Top Stroke Rehabil. 1998;5(2):30–44. [Google Scholar]
- 49.Clark DO, Patrick DL, Grembowski D, Durham M. Socioeconomic status and exercise self-efficacy in late life. J Behav Med. 1995;18:335–76. doi: 10.1007/BF01857660. [DOI] [PubMed] [Google Scholar]
- 50.Tennstedt S, Chang B. A randomised, controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol B Psychol Sci. 1998;53B:384–92. doi: 10.1093/geronb/53b.6.p384. [DOI] [PubMed] [Google Scholar]
- 51.Ministry of Health and Long-Term Care (Ontario) Five hospitals recognized for benchmark rehabilitation care and service. Toronto: The Ministry; 2005. Jul 20, [cited 2005 Jul 25]. Available from: http://ogov.newswire.ca/ontario/GPOE/2005/07/20/c3000.html?lmatch=&lang=_e.html. [Google Scholar]