Empirical evidence suggests that there are marked associations between positive psychological states and health outcomes, including reduced cardiovascular disease risk and increased resistance to infection. These observations have stimulated the investigation of behavioral and biological processes that might mediate protective effects. Evidence linking positive affect with health behaviors has been mixed, though recent cross-cultural research has documented associations with exercising regularly, not smoking, and prudent diet. At the biological level, cortisol output has been consistently shown to be lower among individuals reporting positive affect, and favorable associations with heart rate, blood pressure, and inflammatory markers such as interleukin-6 have also been described. Importantly, these relationships are independent of negative affect and depressed mood, suggesting that positive affect may have distinctive biological correlates that can benefit health. At the same time, positive affect is associated with protective psychosocial factors such as greater social connectedness, perceived social support, optimism, and preference for adaptive coping responses. Positive affect may be part of a broader profile of psychosocial resilience that reduces risk of adverse physical health outcomes.
There is growing evidence that positive psychological well-being is associated with reduced risk of physical illness and prolonged survival. In one sense this is not surprising, because serious illness frequently leads to deterioration in mood or sense of vitality. The intriguing issue is whether psychological well-being protects against future illness or inhibits the progression of chronic disease. Central to this research is the question of whether positive psychological factors simply reflect the absence of depression, anxiety, and other negative states or contribute independently to health outcomes. Depression, stress, and anxiety are known to be associated with health impairment and increased risk for a variety of physical illnesses (Steptoe, 2006b), but there is growing evidence that the effects of positive affect may be present even after depression and anxiety are taken into account.
The first aim of this article is to outline the evidence that positive affect and other positive dispositions predict future health. A variety of different terms have been used to describe positive states and traits in the literature, including happiness, positive affective style, and emotional vitality (Lyubomirsky, King, & Diener, 2005). These are in turn related to traits such as hopefulness, cheerfulness, and life satisfaction. Although there may be important distinctions between these characteristics in terms of their duration and developmental antecedents, in practice there is considerable overlap between the constructs (Kashdan, Biswas-Diener, & King, 2008), and their associations with health outcomes are closely correlated. The present article therefore addresses a broad range of positive affective states and dispositions. Second, we address the behavioral and biological pathways through which such effects may be mediated, highlighting recent research carried out by our group. We have placed particular emphasis on assessments of positive affect made using ecological momentary assessment (EMA) techniques, because these relate to everyday life experiences that may be particularly relevant to concepts of resilience in ordinary life. Third, we position this research in the broader context of protective psychosocial factors that have been identified as relevant to physical health outcomes. We conclude by addressing the question of whether positive affect is likely to make an independent contribution to disease prevention or whether it is a summary indicator of other protective and resilience factors such social connectedness, social support, adaptive coping and high-esteem
POSITIVE AFFECT AND PHYSICAL HEALTH
The research literature relating positive affect and psychological well-being with physical health is growing (Howell, Kern, & Lyubomirsky, 2007; Pressman & Cohen, 2005; Veenhoven, 2008). The strongest research design definitively to establish causality is the experimental study, in which participants are assigned at random to different levels of positive affect and tracked for health outcomes. In its pure form, such a design is rarely feasible or ethical, but a small number of quasi-experimental studies have been conducted. Notably, S. Cohen, Doyle, Turner, Alper, and Skoner (2003) and S. Cohen, Alper, Doyle, Treanor, and Turner (2006) have used experimental exposure to infectious organisms such as rhinovirus (common cold) and influenza virus and analyzed responses to the virus in relation to emotional state. In these studies, volunteers were administered standard doses of virus and monitored in quarantine for the development of objective illness. Participants with a more positive emotional style (those whose affect remained very positive over several days) had reduced risk of developing upper respiratory illness (S. Cohen et al., 2006). Interestingly, these effects were independent of optimism, extraversion, self-esteem, and purpose in life, suggesting a rather specific association between positive affect and health outcome.
The strongest population-based research design for studying factors predicting the development of physical illness is the prospective epidemiological cohort study. This involves recruiting a large sample of initially healthy individuals, assessing positive well-being (along with traditional risk factors for disease), then tracking the cohort over several years. The relationship between positive psychological factors and future illness can then be investigated. Central to such design is as complete a census of participants as possible, because loss to follow-up may distort the results, as well as adequate assessment of potential confounders. For example, positive well-being could be associated with higher socioeconomic status (SES) or cigarette smoking, both of which contribute to health risk.
Kubzansky and Thurston’s (2007) recent study of emotional vitality and coronary heart disease (CHD) illustrates this method. A cohort of 6,025 men and women aged 25–75 years who were free of CHD at baseline were followed for an average 15 years. Over this period, 1,141 developed CHD. A measure of “emotional vitality,” an amalgam of vitality (sense of energy and pep), positive well-being (happiness and life satisfaction), and emotional self-control (feeling emotionally stable and secure), was derived from the General Well-Being Schedule (Fazio, 1977). Participants with greater emotional vitality were at markedly reduced risk for CHD, and this effect remained significant after accounting statistically for age, gender, ethnicity, marital status, educational attainment, blood pressure, cholesterol, body mass index (BMI), smoking, alcohol use, physical activity level, diabetes, hypertension, and psychological illness. All three components of the emotional vitality construct appeared to contribute to the health outcomes in this study. In the model adjusting for risk factors, the relative risk of CHD in the highest compared with lowest tertile of emotional vitality was .74 (95% confidence intervals [C.I.] .64 to .85), indicating a 26% reduction in relative risk. To put this into perspective, the relative risk was increased by 33% in the lowest compared with the highest physical activity category.
Chida and Steptoe (2008) recently conducted a meta-analysis of prospective studies relating psychological well-being with mortality. Twenty-six studies of initially healthy populations and 28 studies targeting people with an established illnesses such as HIV/Aids were identified. Follow-up periods ranged between 2 and 44 years in the healthy population studies and 1–20 years in studies of people with established illness. Positive affect and positive traits such as optimism and hopefulness were associated with reduced mortality, with stronger effects in healthy population (adjusted hazard ratio .82, 95% C.I. .76 to .89, p < .001), than in those with existing illnesses (hazard ratio .98, C.I. .95 to 1.00, p = .03). Effects persisted when negative affect was controlled and were as strong in studies that were higher quality in terms of measurement of covariates and outcome ascertainment. However there were indications of publication bias, implying that studies finding a positive association were more likely to be published than those that did not. Nevertheless, the “fail-safe” statistics were high and indicated that there would have to be 2,444 studies of healthy populations and 1,397 studies of ill populations that were nonsignificant and unpublished to be added to the meta-analyses to reduce the overall effects to nonsignificance. The evidence to date, therefore, suggests that there are important associations between positive affect and health outcomes.
Mediating Processes
A central issue is understanding what mediates the effects of positive affect on health. There are at least four possibilities. The first is a common genetic substrate. Positive affect is moderately heritable (Nes, Roysamb, Reichborn-Kjennerud, Harris, & Tambs, 2007), and genetic factors also contribute to risk of common diseases such as CHD and type 2 diabetes. Theoretically, there might be genetic factors common to positive affect and health risk. Such genetic associations could be functional, reflecting, for example, the role of central neurotransmitters both in mood regulation and physiological dysfunction, or might be due to coaggregation of alleles. As far as we are aware, there is no direct evidence for such a pathway at present. The second possibility is that lifestyle factors are responsible, with happy individuals having more favorable health habits and making healthier behavioral choices than less happy people. Numerous lifestyle factors, including smoking, alcohol consumption, regular physical exercise, dietary choice, and sexual risk behavior are potentially associated with positive affect. The third possible pathway is through psychobiological activation and variation in neuroendocrine, autonomic, immune, and inflammatory pathways. Finally, positive affect may be a marker of a broader set of psychosocial factors that are independently related to health, including social support, effective coping, optimism, and self-esteem.
PSYCHOLOGICAL WELL-BEING AND HEALTH BEHAVIORS
Associations between positive affect and healthy behavior choices are quite mixed. Although relationships between positive affect or more enduring traits such as life satisfaction and physical activity, smoking, and alcohol consumption have been documented (Dear, Henderson, & Korten, 2002; Patterson, Lerman, Kaufmann, Neuner, & Audrain-McGovern, 2004; Schnohr, Kristensen, Prescott, & Scharling, 2005), results have been inconsistent (Diener & Seligman, 2002; Murphy, McDevitt-Murphy, & Barnett, 2005). Even less is known about associations between well-being and other health behaviors such as dietary choice. We therefore recently carried out a study of the relationship between life satisfaction and seven health behaviors using data collected from more than 17,000 young adults in 21 countries (Grant, Wardle, & Steptoe, 2009). A subsidiary aim was to test the consistency of the association across cultures, because most research has been carried out in Western societies. The 21 countries in this study were therefore divided into three categories: Western Europe and the United States (Belgium, England, France, Germany, Greece, Iceland, Ireland, Italy, Netherlands, Portugal, Spain, and the United States), Central and Eastern Europe (Bulgaria, Hungary, Poland, Romania, and Slovakia), and Pacific Asian countries (Japan, Korea, Taiwan, and Thailand).
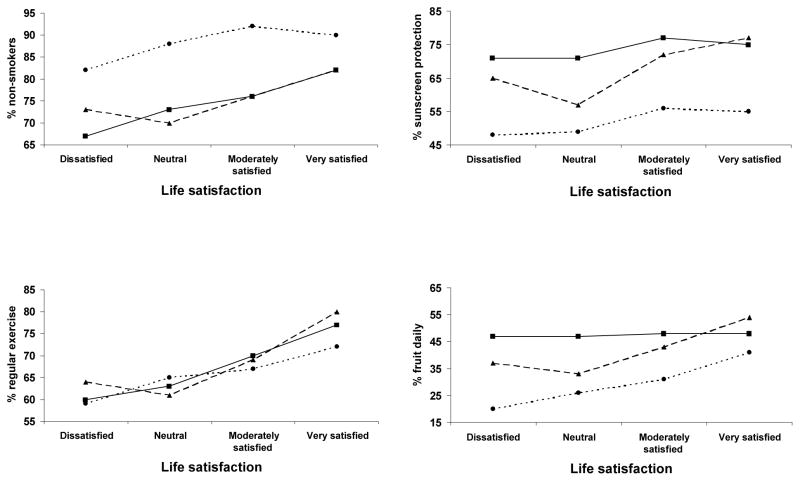
Results for four health behaviors are summarized in Figure 1. The sample was divided into people who said they were very satisfied with their lives, moderately satisfied, neutral, or dissatisfied. Greater life satisfaction was consistently associated with being less likely to smoke and more likely to take regular exercise in all three regions of the world. These patterns were confirmed by more formal statistical analyses that controlled for age, gender, and clustering within countries. Effects were less consistent for daily fruit consumption, being positive in some regions of the world but not in others.
Figure 1.
Proportion of young adults in Western Europe and the United States (solid line), Central and Eastern Europe (dashed line), and Pacific Asian countries (dotted line) reporting not smoking, using sunscreen, exercising regularly, and eating fruit daily in relation to life satisfaction. Adapted from Grant et al. (2009).
Bidirectional processes are probably involved in many of these relationships. For example, intervention studies have shown that increased physical activity has beneficial effects on mood, whereas depressed people are typically sedentary but show increases in physical activity as their depression lifts (Steptoe, 2006a). The evidence is therefore consistent with the notion that lifestyle factors might partly mediate associations between positive psychological state and health outcomes. However, it is striking that several of the studies of positive affect and mortality alluded to earlier in this article controlled statistically for health behaviors such as smoking and physical activity without compromising the effects of positive affect from the model (e.g., Chida & Steptoe, 2008; Giltay, Kamphuis, Kalmijn, Zitman, & Kromhout, 2006; Kubzansky & Thurston, 2007; Ostir, Markides, Black, & Goodwin, 2000). Consequently, it is worth exploring whether more direct psychobiological pathways are involved.
BIOLOGICAL CORRELATES OF POSITIVE AFFECT
Three distinct research methodologies can be used to examine the biological correlates of positive affect, and each has strengths and limitations. The epidemiological or population approach involves measuring biological functioning in large samples, allowing statistically sophisticated adjustment for covariates and the possibility of tracking objective disease endpoints. More fine-grained analyses of between- and within-person associations between biology and positive affect are possible using naturalistic monitoring with methods such as salivary cortisol sampling. The third technique is psychophysiological stress testing, in which the influence of individual differences in positive affect on biological responses can be examined under highly controlled conditions. All these methods have contributed to understanding the nature of the biological correlates of positive affect.
A related issue is how positive affect is measured. Many studies have used questionnaire measures such as the Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988), the General Well-Being Schedule, or a life satisfaction scale, asking participants how they generally feel or have felt over a specific time period such as 1 week. These methods have been criticized for recall bias, the influence of current mood states, and focusing illusions (Kahneman & Krueger, 2006; Shiffman, Stone, & Hufford, 2008). They also may miss important variables in affective state in everyday life. A second technique used in this field is ecological momentary assessment (EMA), with periodic measures of affective states within or between days. There are other variations, such as the repeated administration of questionnaire measures on several days (S. Cohen et al., 2006) or the newly developed Day Reconstruction Method (Kahneman, Krueger, Schkade, Schwarz, & Stone, 2004; Krueger & Stone, 2008). There is now evidence that the strength of associations between positive affect and biology may vary across methods and that EMA is particularly sensitive to biological correlates.
Cortisol Profiles
Cortisol is a well-established stress hormone, so relationships with affective state have been studied for many years (Biondi & Picardi, 1999). Cortisol is involved in a range of chronic diseases, including type 2 diabetes, hypertension, CHD, depression, and autoimmune conditions (McEwen, 2007; Raison & Miller, 2003). The introduction of salivary cortisol sampling has greatly facilitated investigations of cortisol profiles in everyday life. But interpreting findings that positive well-being is associated with cortisol profiles over the day is complicated by differences in the phase of cortisol profile that is examined. There is marked diurnal variation in cortisol, with high levels early in the day declining into the afternoon and evening. The day begins with the cortisol awakening response (CAR), the change in levels (typically an increase) that takes place over the first 30–45 min following waking in the morning. Its magnitude has been related to stress processes (Steptoe, 2007). It is followed by a fall over the rest of the day, and both the rate of decline, or slope, and the overall output appear to be significant. The CAR and cortisol output over the rest of the day appear to be regulated differently, with distinctive genetic influences, and are poorly intercorrelated (Schmidt-Reinwald et al., 1999; Wust, Federenko, Hellhammer, & Kirschbaum, 2000). They may therefore show different associations with positive affect.
There have been two approaches to investigating positive affect and cortisol. The first is to test within-person associations, or whether there are relationships between the periods of the day during which people feel happy and their cortisol levels. Studies of this type involve repeated assessment of mood and serial cortisol sampling, with analysis using multilevel models. A number of studies of this type have shown that cortisol tends to be lower when people have greater positive affect (Davydov, Shapiro, Goldstein, & Chicz-DeMet, 2005; Hoppmann & Klumb, 2006; Jacobs et al., 2007; Smyth et al., 1998). However, evidence regarding the extent to which associations between cortisol and positive affect are independent of negative affect has been inconsistent (Hoppmann & Klumb, 2006; Jacobs et al., 2007; van Eck, Berkhof, Nicolson, & Sulon, 1996).
The second approach, which is more relevant to the health outcomes being discussed here, is whether happier individuals or people with greater trait positive affect differ in their cortisol profile from others. Most studies have shown lower cortisol in people with higher levels of positive affect, but there are variations depending on the time of the day, age, and the method of measuring positive affect. In our studies, we have typically used EMA to measure positive affect, aggregating ratings over several times of day or over several days to generate an estimate of general positive affect. In our first study of just over 200 middle-aged working men and women, we found an inverse association between positive affect and cortisol output over the day that was independent of gender, age, grade of employment (a marker of SES), BMI, and smoking (Steptoe, Wardle, & Marmot, 2005). Effects were obtained both on working and nonworking days and persisted in a repeated assessment of the same individuals after 3 years (Steptoe & Wardle, 2005). Effects were also independent of psychological distress, suggesting protective responses that were not simply due to the absence of negative affect.
We have recently replicated these findings in a large sample involving 2,873 healthy men and women aged 60 years on average (Steptoe, O’Donnell, Badrick, Kumari, & Marmot, 2008). Cortisol declined as expected over the day, and output levels were again inversely associated with positive affect. Mean values averaged 5.52 ± 2.7 nmol/l in the lowest happiness third, 5.56 ± 2.5 nmol/l in the moderate happiness third, and 5.16 ± 2.4 nmol/l in the happiest third of the sample after adjustment for age, gender, income, ethnicity, BMI, waist/hip ratio, smoking status, employment status, and time of waking. Additional control for depression did not markedly alter these results.
In the only other large-scale study published to date, Polk, Cohen, Doyle, Skoner, and Kirschbaum (2005) assessed trait positive affect in 334 adults by aggregating mood measurements taken over 7 days. This study yielded slightly different findings from ours, with high positive affect in men being associated with steeper cortisol slopes, whereas the cortisol differences in women tended to be greater early in the day. We do not know what accounts for these variations, but they may be related to the fact that participants were kept in a hotel over the study period instead of going about their normal lives.
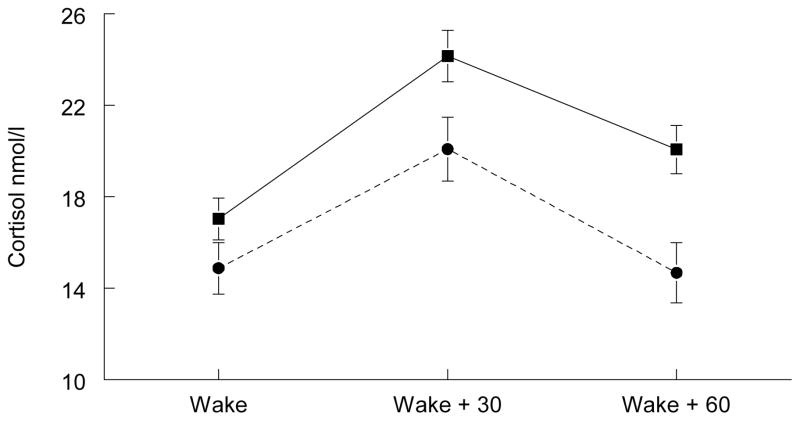
Our work with middle-aged and older adults has not found associations between positive affect and the CAR. But Lai et al. (2005) showed that positive affect was associated with reduced cortisol on waking and throughout the day in a sample of young Chinese adults. In a study of young men, we also found that the CAR was heightened in those experiencing lower positive affect, independently of negative affect (Steptoe, Gibson, Hamer, & Wardle, 2007). This is illustrated in Figure 2, with cortisol values adjusted for age, BMI, time of waking in the morning, and negative affect. Participants who were either low and high in positive affect showed the typical CAR, with values peaking at 30 min after waking up. But the increase in cortisol was greater in the low positive affect group. Even 1 hr after waking, cortisol remained elevated in the low positive affect group, whereas it had fallen to waking levels in participants reporting high positive affect. Interestingly, we observed stronger associations between cortisol and positive affect measured with EMA than with PANAS assessments of how participants had been feeling over the past week.
Figure 2.
Mean cortisol sampled on waking and 30 min and 60 min later in young men divided on the basis of EMA assessments into low (solid line) and high (dotted line) positive affect groups. Values are adjusted for age, BMI, time of waking, and negative affect. Error bars are standard error of the mean. Adapted from Steptoe et al. (2007)
Cardiovascular Function
Associations between positive affect and cardiovascular function can be studied both in the psychophysiological laboratory and in everyday life, thanks to the development of ambulatory blood pressure and Holter monitors. Studies of cardiovascular function are complicated by the fact that positive affect may be accompanied by physical activation. Physical activity itself increases heart rate and blood pressure, and this may be the explanation of why happy moods in everyday life have been associated with slightly greater blood pressure than neutral moods in within-person studies (Schwartz, Warren, & Pickering, 1994). Similarly, experimental studies have shown that the positive affect engendered by interpersonal interaction stimulated heightened cardiovascular reactivity (Warner & Strowman, 1995), whereas, in other studies, positive affect has been related to increased cardiovascular responses because of greater engagement with challenge (Maier, Waldstein, & Synowski, 2003).
In our first study of middle-aged adults, we measured blood pressure and heart rate every 20 min over a working day and evening using ambulatory blood pressure monitors. In men but not women, we found a significant association between positive well-being and heart rate; the higher the aggregate level of positive affect, the lower the heart rate over the day (Steptoe et al., 2005). This association held after adjustment for physical activity, BMI, and other factors that influence heart rate. Three years after the original ambulatory monitoring phase, we collected the same measures on around 75% of the original sample (Steptoe & Wardle, 2005). The association between heart rate and positive affect in men was replicated, but, in addition, systolic blood pressure was inversely associated with positive affect after controlling for age, gender, SES, smoking, and BMI.
Another interesting study of older adults (mean age 74 years) involved daily measurement of blood pressure and positive and negative affect over 60 days (Ong & Allaire, 2005). The results of multilevel modeling showed that, at the within-person level, daily positive well-being was associated with reduced cardiovascular reactivity to negative emotional arousal. Further, feelings of positive well-being reduced the cardiovascular activation that followed episodes of negative emotion, even after controlling for individual differences in mood states. Rapid recovery, indexed either by heart rate variability or cortisol, from a stressful experience has been conceptualized as an adaptive response built upon high levels of positive affect and traits associated with positive affect such as benefit finding (Bower, Low, Moskowitz, Sepah, & Epel, 2008).
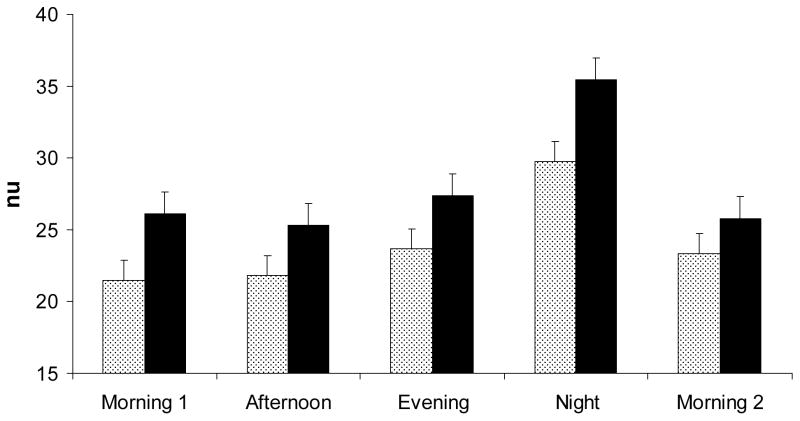
An additional cardiovascular measure that provides important information about autonomic regulation and health is heart rate variability. Heart rate variability is the short-term variation in beat-to-beat interval and is controlled through the interplay between the sympathetic nervous system (which increases heart rate) and the parasympathetic or vagal system (which stimulates reduced heart rate). There is growing evidence that higher levels of parasympathetic control are healthier, not only for the cardiovascular system, but also for mood, stress regulation, and cognitive function (Rottenberg, 2007; Thayer & Sternberg, 2006). Our group recently carried out 24-hr monitoring of heart rate variability in a group of patients with suspected coronary artery disease (Bhattacharyya, Whitehead, Rakhit, & Steptoe, 2008). Positive affect was assessed retrospectively using the Day Reconstruction Method, which guides individuals to systematically reconstruct their activities and experiences of the preceding day with procedures designed to reduce recall biases. We found that greater positive affect over the monitoring period was associated with a healthier profile of heart rate variability assessed using power spectrum analysis. This is illustrated in Figure 3, which shows power in the high frequency component (0.15–0.4 Hz) of the spectrum, which is linked with parasympathetic activity. It can be seen that high frequency heart rate variability increased from the daytime to nighttime, as sympathetic nervous system withdrawal during sleep led to a dominance of parasympathetic tone. Throughout the monitoring period, participants with higher positive affect had greater high frequency heart rate variability, and this difference remained significant after controlling for age, gender, cardiovascular disease status, and the use of medication. Ongoing studies are now investigating whether similar relationships hold among healthy individuals.
Figure 3.
Mean power in the high frequency (0.15–0.40 Hz) waveband of the power spectrum of heart rate variability in normalized units (nu) in patients reporting high (solid bars) and low (stippled bars) positive affect. The 24-hr monitoring period began at 9:00 a.m. and is divided into five time segments. Values are adjusted statistically for age, gender, cardiovascular disease status, and use of medications, including beta-blockade. Error bars are standard error of the mean. Adapted from Bhattacharyya et al. (2008).
There is also accumulating evidence from laboratory studies that cardiovascular reactivity to challenge varies with levels of positive affect. A series of studies by Tugade and Fredrickson (2004) examined the contribution of positive well-being to cardiovascular recovery from negative emotion arousal states, including a deliberate manipulation of the degree of positive affect engendered by negative circumstances. The results suggest that positive well-being contributes to an accelerated cardiovascular recovery profile after the experience of negative emotions.
This finding is consistent with our study of the relationship between positive well-being and cardiovascular responses to laboratory mental stress tests in young men (Steptoe, Gibson, et al., 2007). Positive affect was measured both by questionnaire and by aggregating EMA assessments over 2 days. Blood pressure recovery following standard laboratory stress challenges was more rapid among people with higher levels of positive affect, with stronger associations emerging for aggregate EMA assessments than questionnaire measures of well-being. Differences in poststress recovery may be important because they could be indicative of chronic allostatic load (McEwen, 1998). Delayed recovery has been found to predict increased levels of clinical blood pressure prospectively and are related to impaired hemostatic (clotting) processes and to subclinical atherosclerosis (Steptoe, Donald, O’Donnell, Marmot, & Deanfield, 2006; Steptoe & Marmot, 2006).
Inflammatory Processes
The immune system is an important line of defense against infection and other external threats to the organism, and inflammatory processes are increasingly recognized as central to the development of chronic diseases such as CHD (Steptoe & Brydon, 2007). The relationship between immune function and positive affect has recently been reviewed by Marsland, Pressman, and Cohen (2007). Positive affect is associated with increased cellular immune competence assessed in terms of natural killer cell cytotoxicity independently of negative affect (Lutgendorf et al., 2001; Valdimarsdottir & Bovbjerg, 1997). More recently, Marsland, Cohen, Rabin, and Manuck (2006) measured antibody responses following vaccination for hepatitis B. Greater antibody responses indicate more effective immune function in this model, and trait positive affect was associated with heightened antibody responses independently of age, gender, health behavior, and negative affect.
Inflammatory pathways have not been extensively studied to date, but are potentially important to understanding the relationship between positive affect and chronic disease. We have recently investigated associations with interleukin 6 (IL-6), C-reactive protein, and plasma fibrinogen. IL-6 is a cytokine that is relatively abundant in the circulation and is crucial for leukocyte and endothelial cell activation. High levels of circulating IL-6 predict future CHD and type 2 diabetes and are related to obesity, depression, and frailty in older adults (Papanicolaou, Wilder, Manolagas, & Chrousos, 1998). IL-6 also promotes the production of the acute phase protein C-reactive protein. C-reactive protein is a marker of cardiovascular disease risk and is related to the metabolic syndrome and future CHD, although there is controversy over whether its role is functional (Nilsson, 2005). IL-6 and C-reactive protein are related to psychosocial factors such as chronic stress, social isolation, and childhood adversity (Danese, Pariante, Caspi, Taylor, & Poulton, 2007; Kiecolt-Glaser et al., 2003; Loucks, Berkman, Gruenewald, & Seeman, 2006; Ranjit et al., 2007). IL-6 also increases in response to acute stress, although changes may take several hours to emerge (Steptoe, Hamer, & Chida, 2007). In our study of nearly 3,000 healthy middle-aged adults, we observed inverse associations between positive affect and both plasma IL-6 and C-reactive protein concentration, but only in women (Steptoe, Gibson, et al., 2008). These effects were independent of covariates such as age, ethnicity, SES, BMI, smoking, and depressed mood. We do not know why effects were only present in women, although we have previously found that women showed larger IL-6 responses to acute stress than men (Steptoe, Owen, Kunz-Ebrecht, & Mohamed-Ali, 2002). Additionally, IL-6 was found to be inversely associated with factors associated with other positive affective resources, such as purpose in life and positive relationships, in a sample of elderly women (Friedman, Hayney, Love, Singer, & Ryff, 2007).
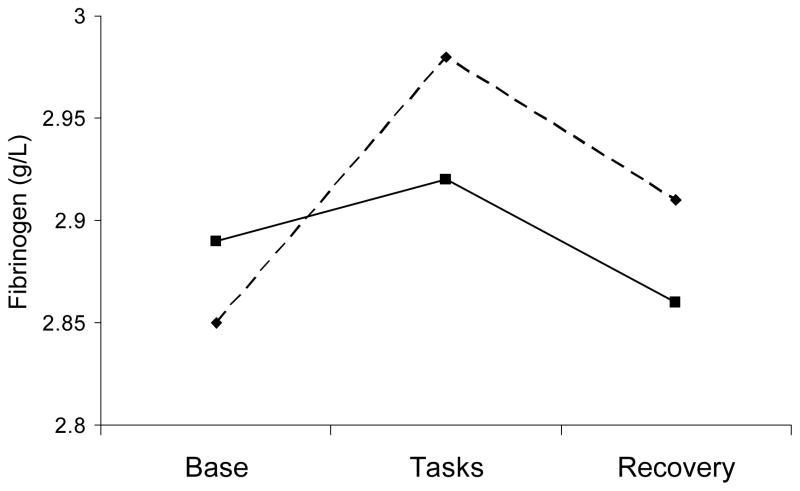
Another biological measure that is relevant both to inflammation and hemostasis is fibrinogen. Fibrinogen is a precursor of fibrin, one of the main constituents of vascular thrombi, but is also relevant to cardiovascular disease through its influence on blood viscosity, atherogenic cell proliferation, and platelet aggregation (Danesh, Collins, Appleby, & Peto, 1998; Rauch et al., 2001). Unlike IL-6, fibrinogen responds rapidly to mental stress, so it can be readily monitored in experimental settings. We found an inverse association between positive affect and fibrinogen stress responsivity, with smaller stress responses in happier individuals (Steptoe et al., 2005). This finding is illustrated in Figure 4, which shows fibrinogen levels adjusted for covariates in participants in the highest and lowest quintiles of positive affect. Fibrinogen concentrations did not differ at baseline, but the less happy participants showed substantially larger fibrinogen stress responses than the happiest group. Interestingly, plasma fibrinogen remained elevated 45 min poststress in the least happy quintile, whereas it had fallen below baseline in the highest positive affect group. This suggests not only that fibrinogen stress responsivity greater in people with low positive affect, but that their responses are more prolonged. This pattern is consistent with the findings related to poststress cardiovascular recovery noted earlier.
Figure 4.
Mean plasma fibrinogen sampled at baseline (base), immediately following challenging behavioral tasks (tasks), and 45-min posttasks (recovery) in participants in the highest (solid line) and lowest (dashed line) of a cohort of 209 individuals. Values are adjusted for age, gender, grade of employment, smoking, BMI, and hematocrit. Adapted from Steptoe et al. (2005).
SLEEP DISTURBANCE
Sleep occupies a special position in relation to health and biology, because it is both a fundamental biologically driven process and a health behavior. Disturbances of sleep are very common, with more than one quarter of adults complaining of insomnia, insufficient sleep, or disturbed sleep (Foley, Ancoli-Israel, Britz, & Walsh, 2004; Strine & Chapman, 2005). Sleep problems are associated with reduced mental health, impaired cognitive function, and chronic illness and have also been linked with premature mortality (Kripke, Garfinkel, Wingard, Klauber, & Marler, 2002). Although there is extensive literature linking sleep problems with anxiety and depression (Roberts, Shema, Kaplan, & Strawbridge, 2000), there has been surprisingly little work evaluating associations with positive affect. However, a recent study of more than 3,500 adults from the National Survey of Mid-Life Development in the United States (MIDUS) found that subjective well-being (an amalgam of high positive affect, low negative affect, and life satisfaction) was inversely associated with two questions concerning difficulty in sleeping (Hamilton et al., 2007). The relationship was independent of age, gender, somatic symptoms, and emotional problems. We carried out a study of 736 of men and women that involved the administration of a standard sleep problems inventory. We found that positive affect, estimated by the aggregation of four EMA ratings over a single day, was inversely related to sleep problems independently of age, gender, SES, employment status, self-rated health, and reported psychological distress (Steptoe, O’Donnell, Marmot, & Wardle, 2008b). These findings are corroborated by another EMA study that showed lower levels of positive affect in people suffering from primary insomnia compared with controls (Buysse et al., 2007). It would therefore appear that positive affect is associated with good sleep in the general population, at least as measured using self-report instruments. Because sleep patterns impact on biological rhythms, this effect might contribute to some of the disturbances in diurnal profiles of biological variables detailed earlier.
POSITIVE AFFECT AND OTHER PSYCHOSOCIAL FACTORS
The literature summarized in the previous sections indicates that positive affect is associated with a potentially health protective biological profile in terms of neuroendocrine, cardiovascular, and immunological function. However, positive affect does not exist in isolation and is often included in theoretical models of resilience. Resilience is generally regarded as a dynamic process of effective adaptation to adversity, resulting in thriving, even flourishing, in the face of life’s challenges (Luthar, Sawyer, & Brown, 2006). It incorporates the notion of rapid recovery following stress that may occur both at the psychological and biological levels (Charney, 2004). Resilience is also aligned with community- and population-level factors such as high SES, social capital, and social connectedness and with psychological factors such as optimism, social support, coping disposition, and extraversion. People with high resilience also report greater psychosocial resources, and it has been argued that resilient individuals use positive affect to facilitate adaptation to stress (Fredrickson, Tugade, Waugh, & Larkin, 2003; Ong, Bergeman, Bisconti, & Wallace, 2006; Tugade & Fredrickson, 2007). The relationship between potentially health protective psychosocial factors and positive affect is therefore important.
Positive Affect and Social Support
There is converging evidence that social support and social integration are strongly associated with positive affect. Social support has multiple facets that can be measured quantitatively, including a division of the support into types such as instrumental and emotional support, or by the appraisal of the quality of the connections. In an early study, Baldassare, Rosenfield, and Rook (1984) obtained measures of both subjective and objective social connectedness and also calculated social network density in a population of older people. Even after controlling for health and demographic characteristics, connectivity to others in the social network was associated with positive affect. In a similar study, Chan and Lee (2006) examined positive affect in a group of older people in China and found that social network support was a strong contributor to positive affect. These associations were evident even after controlling for factors such as income and education, and the findings are paralleled in other studies of older populations (Pinquart & Sorensen, 2000). Membership in a social network has been shown to contribute to higher levels of positive well-being across many domains of life (Helliwell, 2003), and overall these findings indicate that, at least in older populations, positive affect tends to increase with the number of people available for instrumental support and feelings of social connectivity.
Much of the work on positive affect and social support has focused on older individuals. Social support and social connectedness appear to be important determinants of the maintenance of a life free of disability in old age (Mendes de Leon et al., 1999). This group may also constitute a population for whom instrumental support, as a component of social connectedness, contributes directly to well-being. In a study of informal social support networks, Taylor, Chatters, Hardison, and Riley (2001) reported that the association between social support and positive well-being depended on the degree of need and availability of instrumental support. The association between social support and positive affect in younger people or those who have less need for instrumental support is limited, but both familial and extrafamilial social connections are associated with positive affect in adolescence and early adulthood (Lyubomirsky, Tkach, & DiMatteo, 2006).
It is plausible that positive affect and social support have a bidirectional association; those with higher levels of positive affect may be more adept at eliciting positive emotions in others. This, in turn, can actively influence social networks. It has not always been clear that the association of positive affect and social support is independent of levels of negative affect or socioeconomic status, but in a study of just over 700 middle-aged men and women, we showed that positive affect was related to greater social connectedness and social support after controlling for age, gender, household income, paid employment, and negative affect (Steptoe, O’Donnell, Marmot, & Wardle, 2008a). Interestingly, people experiencing greater negative affect reported more social conflict and had fewer social connections, but neither of these factors detracted from the significant, positive association between social support and positive affect.
Positive Affect and Personality
Positive affect is related to several fundamental personality dimensions, such as extraversion, neuroticism, and conscientiousness (Steel, Schmidt, & Shultz, 2008). Neuroticism is a close correlate of negative affect such that more neurotic people are likely to report greater negative affect. There is debate about the extent to which positive and negative affect are partly independent inversely correlated dimensions or polar opposites on a single dimension (Russell & Carroll, 1999; Watson & Clark, 1997). But inasmuch as positive and negative affect are inversely associated, neuroticism is related to positive affect in a similar fashion. More interesting is the relationship with extraversion. One of the defining features of extraversion is engagement with others and the external environment, so it is not surprising that higher levels of extraversion are associated with higher levels of positive affect. McNiel and Fleeson (2006) have demonstrated that deliberate adoption of a state of extraversion has effects on positive affect such that the more extraverted a person behaves, the higher the levels of subjective and objectively measured positive affect. This association has also been demonstrated in other studies of personality traits and positive affect (Campbell-Sills, Cohan, & Stein, 2006; Shiota, Keltner, & John, 2006). However, analyses of the association of extraversion with positive affect seldom incorporate controls for negative affect, potentially overestimating the strength of the relationship (Vitterso & Nilsen, 2002). Additionally, Steel et al. (2008) recently argued that much of the association between extraversion and positive affect may be due to conceptual overlap and criterion contamination because of common method variance. Without an expansion of research into the association of affect and extraversion, it is difficult to determine the unique contribution of extraversion to positive well-being. The relationship may be confounded further by culture (Lynn & Steel, 2006) and gender (Schmitt, Realo, Voracek, & Allik, 2008).
Other personality traits may also be related to positive affect. In their recent meta-analytic review, Steel et al. (2008) showed that positive affect is related to greater agreeableness, greater conscientiousness, and greater openness to experience, but has inconsistent associations with defensiveness. However, when different personality traits were examined in multivariate analyses, the relationship between positive affect and agreeableness was no longer significant, suggesting that it may have been confounded by neuroticism and extraversion.
The association of positive affect with personality has often been examined within the framework of the broad Five Factor model of personality. Dispositions, such as optimism and coping style, may conceptually overlap the five-factor model of personality, but they are discriminable, and are often considered as distinct in studies of positive affect (Fredrickson & Joiner, 2002; O’Brien & DeLongis, 1996), so they are presented separately here.
Positive Affect and Optimism
The association between optimism and positive affect is less well understood than that between other personality factors and positive affect, although there appear to be consistent positive relationships (Diener, Suh, Lucas, & Smith, 1999; Lyubomirsky et al., 2005). One problem with the findings that relate positive affect with personality is that many of the studies parcel out the influence of pessimism but not of subclinical negative affect on the association. But in our recent study, we showed that the association between positive affect and optimism remained strong even after controlling for negative affect and other demographic variables such as socioeconomic status (Steptoe et al., 2008a). Similar studies of the general population are few in number compared with studies of optimism and affect in clinical populations or in people experiencing serious life threat (e.g. Pinquart, Frohlich, & Silbereisen, 2007; Riolli, Savicki, & Cepani, 2002).
Positive Affect and Coping Dispositions
Associations between coping dispositions and positive affect are often studied within a framework of major life stress or challenge. They have been examined in people experiencing stressors such as bereavement (Rogers, Hansen, Levy, Tate, & Sikkema, 2005), diagnosis of cancer (Chen et al., 1996; Pinquart et al., 2007), or long-term role stressors such as caregiving (Folkman, 1997). In our study, active types of coping such as problem engagement and solicitation of social support were associated with positive affect as measured by EMA, whereas avoidant coping had little relationship with the level of positive affect (Steptoe et al., 2008a). These results support the findings of earlier work that postulate that a disposition to more action-oriented coping dispositions such as rational action and seeking help are associated with higher levels of positive affect (Campbell-Sills et al., 2006; McCrea & Costa, 1986; Salovey, Rothman, Detweiler, & Steward, 2000). Interestingly, we have also found that coping by problem engagement and seeking social support are associated with reduced cortisol output over the day (O’Donnell, Badrick, Kumari, & Steptoe, 2008).
Positive Affect, Biology, and Other Resilience Factors
Many of the biological parameters related to positive affect are also associated with other resilience factors. For example, social support is related to changes in cardiovascular, neuroendocrine and immune function (Uchino, 2006), optimism has been associated with immune up-regulation (F. Cohen et al., 1999), and adaptive coping is linked with reduced cortisol output (O’Donnell et al., 2008). The question therefore arises of whether the biological correlates of positive affect are distinctive or whether positive affect is a marker of a combination of protective resilience factors that, in turn, influence biology. There is little evidence concerning this issue at present. As noted earlier, Marsland et al. (2006) showed that positive affect predicted larger antibody responses to hepatitis B vaccination, and this response was independent not only of negative affect but also of optimism and extraversion. In our study of sleep disturbance, we found that the association with positive affect was largely unchanged after we had controlled statistically for stress exposure, social factors such as social support and conflicted social interactions, and negative affect (Steptoe et al., 2008a). Unfortunately, this latter study was based on self-report rather than objective biological indicators. It remains to be seen, therefore, whether other biological measures are related to positive affect independently of social and personal resilience factors.
CONCLUSIONS
The burgeoning interest in positive psychology and in health protective factors in the psychological and social environments has stimulated research linking positive affect with healthy lifestyles and biological responses. Results are complex, but there is now some evidence that positive affect is an independent predictor of health outcomes, that it may be associated with positive health behaviors, and that it is correlated with health-protective biological responses. These studies of behavioral and biological mediators have been largely cross-sectional, so causal sequences have not been documented. It is possible that sustained positive affect leads to reductions in neuroendocrine, autonomic, and immune activation through deactivation of the prefrontal-limbic circuits responsible for stress reactivity (Lovallo, 2004), or that some personality traits are associated with restorative processes after stressful experiences (Epel, McEwen, & Ickovics, 1998), but these have not been demonstrated directly. Interventions that are directly targeted at modifying positive affect have not yet been used to modify these biological correlates, although cognitive behavioral methods such as stress management and pharmacological treatments that indirectly influence positive affect are known to influence neuroendocrine and immune parameters (e.g., Antoni et al., 2000). Future research will therefore determine whether techniques for enhancing positive well-being will have beneficial effects on biological and behavioral mediators. Nonetheless, this is an exciting field of research that offers promise both in the understanding of connections between the mind and body, and for the relief of suffering and the postponement of ill health.
Acknowledgments
This research was supported by the Medical Research Council, Economic and Social Research Council, British Heart Foundation, Cancer Research UK, and the National Institute on Aging.
References
- Antoni MH, Cruess S, Cruess DG, Kumar M, Lutgendorf S, Ironson G, et al. Cognitive-behavioral stress management reduces distress and 24-hour urinary free cortisol output among symptomatic HIV-infected gay men. Annals of Behavioral Medicine. 2000;22:29–37. doi: 10.1007/BF02895165. [DOI] [PubMed] [Google Scholar]
- Baldassare M, Rosenfield S, Rook KS. The types of social relations predicting elderly well-being. Research in Aging. 1984;6:549–559. doi: 10.1177/0164027584006004006. [DOI] [PubMed] [Google Scholar]
- Bhattacharyya MR, Whitehead DL, Rakhit R, Steptoe A. Depressed mood, positive affect, and heart rate variability in patients with suspected coronary artery disease. Psychosomatic Medicine. 2008;70:1020–1027. doi: 10.1097/PSY.0b013e318189afcc. [DOI] [PubMed] [Google Scholar]
- Biondi M, Picardi A. Psychological stress and neuroendocrine function in humans: The last two decades of research. Psychotherapy and Psychosomatics. 1999;68:114–150. doi: 10.1159/000012323. [DOI] [PubMed] [Google Scholar]
- Bower JE, Low CA, Moskowitz JT, Sepah S, Epel E. Benefit finding and physical health: Positive psychological changes and enhanced allostasis. Social and Personality Psychology Compass. 2008;2:223–244. [Google Scholar]
- Buysse DJ, Thompson W, Scott J, Franzen PL, Germain A, Hall M, et al. Daytime symptoms in primary insomnia: A prospective analysis using ecological momentary assessment. Sleep Medicine. 2007;8:198–208. doi: 10.1016/j.sleep.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L, Cohan SL, Stein MB. Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behavior Research and Therapy. 2006;44:585–599. doi: 10.1016/j.brat.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Chan YK, Lee RPL. Network size, social support and happiness in later life: A comparative study of Beijing and Hong Kong. Journal of Happiness Studies. 2006;7:87–112. [Google Scholar]
- Charney DS. Psychobiological mechanisms of resilience and vulnerability: Implications for successful adaptation to extreme stress. American Journal of Psychiatry. 2004;161:195–216. doi: 10.1176/appi.ajp.161.2.195. [DOI] [PubMed] [Google Scholar]
- Chen CC, David A, Thompson K, Smith C, Lea S, Fahy T. Coping strategies and psychiatric morbidity in women attending breast assessment clinics. Journal of Psychosomatic Research. 1996;40:265–270. doi: 10.1016/0022-3999(95)00529-3. [DOI] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychosomatic Medicine. 2008;70:741–756. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- Cohen F, Kearney KA, Zegans LS, Kemeny ME, Neuhaus JM, Stites DP. Differential immune system changes with acute and persistent stress for optimists vs pessimists. Brain Behavior and Immunity. 1999;13:155–174. doi: 10.1006/brbi.1998.0531. [DOI] [PubMed] [Google Scholar]
- Cohen S, Alper CM, Doyle WJ, Treanor JJ, Turner RB. Positive emotional style predicts resistance to illness after experimental exposure to rhinovirus or influenza A virus. Psychosomatic Medicine. 2006;68:809–815. doi: 10.1097/01.psy.0000245867.92364.3c. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Turner RB, Alper CM, Skoner DP. Emotional style and susceptibility to the common cold. Psychosomatic Medicine. 2003;65:652–657. doi: 10.1097/01.psy.0000077508.57784.da. [DOI] [PubMed] [Google Scholar]
- Danese A, Pariante CM, Caspi A, Taylor A, Poulton R. Childhood maltreatment predicts adult inflammation in a life-course study. Proceedings of the National Academy of Sciences, USA. 2007;104:1319–1324. doi: 10.1073/pnas.0610362104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: Meta-analyses of prospective studies. Journal of the American Medical Association. 1998;279:1477–1482. doi: 10.1001/jama.279.18.1477. [DOI] [PubMed] [Google Scholar]
- Davydov DM, Shapiro D, Goldstein IB, Chicz-DeMet A. Moods in everyday situations: Effects of menstrual cycle, work, and stress hormones. Journal of Psychosomatic Research. 2005;58:343–349. doi: 10.1016/j.jpsychores.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Dear K, Henderson S, Korten A. Well-being in Australia Findings from the National Survey of Mental Health and Well-being. Social Psychiatry and Psychiatric Epidemiology. 2002;37:503–509. doi: 10.1007/s00127-002-0590-3. [DOI] [PubMed] [Google Scholar]
- Diener E, Seligman ME. Very happy people. Psychological Science. 2002;13:81–84. doi: 10.1111/1467-9280.00415. [DOI] [PubMed] [Google Scholar]
- Diener E, Suh EM, Lucas RE, Smith HL. Subjective well-being: Three decades of progress. Psychological Bulletin. 1999;125:276–302. [Google Scholar]
- Epel E, McEwen B, Ickovics J. Embodying psychological thriving: Physical thriving in response to stress. Journal of Social Issues. 1998;54:301–322. [Google Scholar]
- Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: Results of the 2003 National Sleep Foundation Sleep in America Survey. Journal of Psychosomatic Research. 2004;56:497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- Folkman S. Positive psychological states and coping with severe stress. Social Science and Medicine. 1997;45:1207–1221. doi: 10.1016/s0277-9536(97)00040-3. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL, Joiner T. Positive emotions trigger upward spirals toward emotional well-being. Psychological Science. 2002;13:172–175. doi: 10.1111/1467-9280.00431. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. Journal of Personality and Social Psychology. 2003;84:365–376. doi: 10.1037//0022-3514.84.2.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman EM, Hayney M, Love GD, Singer BH, Ryff CD. Plasma interleukin-6 and soluble IL-6 receptors are associated with psychological well-being in aging women. Health Psychology. 2007;26:305–313. doi: 10.1037/0278-6133.26.3.305. [DOI] [PubMed] [Google Scholar]
- Giltay EJ, Kamphuis MH, Kalmijn S, Zitman FG, Kromhout D. Dispositional optimism and the risk of cardiovascular death: The Zutphen elderly study. Archives of Internal Medicine. 2006;166:431–436. doi: 10.1001/archinte.166.4.431. [DOI] [PubMed] [Google Scholar]
- Grant N, Wardle J, Steptoe A. The relationship between life satisfaction and health behaviour: A cross-cultural analysis of young adults. International Journal of Behavioral Medicine. 2009 doi: 10.1007/s12529-009-9032-x. (in press) [DOI] [PubMed] [Google Scholar]
- Hamilton NA, Gallagher MW, Preacher KJ, Stevens N, Nelson CA, Karlson C, et al. Insomnia and well-being. Journal of Consulting and Clinical Psychology. 2007;75:939–946. doi: 10.1037/0022-006X.75.6.939. [DOI] [PubMed] [Google Scholar]
- Helliwell JF. How’s life? Combining individual and national variables to explain subjective well-being. Economic Modelling. 2003;20:331–360. [Google Scholar]
- Hoppmann CA, Klumb PL. Daily goal pursuits predict cortisol secretion and mood states in employed parents with preschool children. Psychosomatic Medicine. 2006;68:887–894. doi: 10.1097/01.psy.0000238232.46870.f1. [DOI] [PubMed] [Google Scholar]
- Howell RT, Kern ML, Lyubomirsky S. Health benefits: Meta-analytically determining the impact of well-being on objective health outcomes. Health Psychology Review. 2007;1:83–136. [Google Scholar]
- Jacobs N, Myin-Germeys I, Derom C, Delespaul P, van Os J, Nicolson NA. A momentary assessment study of the relationship between affective and adrenocortical stress responses in daily life. Biological Psychology. 2007;74:60–66. doi: 10.1016/j.biopsycho.2006.07.002. [DOI] [PubMed] [Google Scholar]
- Kahneman D, Krueger AB. Developments in the measurement of subjective well-being. Journal of Economic Perspectives. 2006;20:3–24. [Google Scholar]
- Kahneman D, Krueger AB, Schkade DA, Schwarz N, Stone AA. A survey method for characterizing daily life experience: The day reconstruction method. Science. 2004;306:1776–1780. doi: 10.1126/science.1103572. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Biswas-Diener R, King LA. Reconsidering happiness: The costs of distinguishing between hedonics and eudaimonia. Journal of Positive Psychology. 2008;3:219–233. [Google Scholar]
- Kiecolt-Glaser JK, Preacher KJ, MacCallum RC, Atkinson C, Malarkey WB, Glaser R. Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proceedings of the National Academy of Sciences, USA. 2003;100:9090–9095. doi: 10.1073/pnas.1531903100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Archives of General Psychiatry. 2002;59:131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- Krueger AB, Stone AA. Assessment of pain: A community-based diary survey in the USA. Lancet. 2008;371:1519–1525. doi: 10.1016/S0140-6736(08)60656-X. [DOI] [PubMed] [Google Scholar]
- Kubzansky LD, Thurston RC. Emotional vitality and incident coronary heart disease: Benefits of healthy psychological functioning. Archives of General Psychiatry. 2007;64:1393–1401. doi: 10.1001/archpsyc.64.12.1393. [DOI] [PubMed] [Google Scholar]
- Lai JC, Evans PD, Ng SH, Chong AM, Siu OT, Chan CL, et al. Optimism, positive affectivity, and salivary cortisol. British Journal of Health Psychology. 2005;10:467–484. doi: 10.1348/135910705X26083. [DOI] [PubMed] [Google Scholar]
- Loucks EB, Berkman LF, Gruenewald TL, Seeman TE. Relation of social integration to inflammatory marker concentrations in men and women 70 to 79 years. American Journal of Cardiology. 2006;97:1010–1016. doi: 10.1016/j.amjcard.2005.10.043. [DOI] [PubMed] [Google Scholar]
- Lovallo WR. Stress and health: Biological and psychological interactions. 2. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- Lutgendorf SK, Reimer TT, Harvey JH, Marks G, Hong SY, Hillis SL, et al. Effects of housing relocation on immunocompetence and psychosocial functioning in older adults. Journal of Gerontology A: Biological Science and Medical Science. 2001;56:M97–105. doi: 10.1093/gerona/56.2.m97. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Sawyer JA, Brown PJ. Conceptual issues in studies of resilience: Past, present, and future research. Annals of the New York Academy of Sciences. 2006;1094:105–115. doi: 10.1196/annals.1376.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynn M, Steel P. National differences in subjective well-being: The interactive effects of extraversion and neuroticism. Journal of Happiness Studies. 2006;7:155–165. [Google Scholar]
- Lyubomirsky S, King L, Diener E. The benefits of frequent positive affect: Does happiness lead to success? Psychological Bulletin. 2005;131:803–855. doi: 10.1037/0033-2909.131.6.803. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, Tkach C, DiMatteo MR. What are the differences between happiness and self-esteem. Social Indicators Research. 2006;78:363–404. [Google Scholar]
- Maier KJ, Waldstein SR, Synowski SJ. Relation of cognitive appraisal to cardiovascular reactivity, affect, and task engagement. Annals of Behavoral Medicine. 2003;26:32–41. doi: 10.1207/S15324796ABM2601_05. [DOI] [PubMed] [Google Scholar]
- Marsland AL, Cohen S, Rabin BS, Manuck SB. Trait positive affect and antibody response to hepatitis B vaccination. Brain Behavior and Immunity. 2006;20:261–269. doi: 10.1016/j.bbi.2005.08.009. [DOI] [PubMed] [Google Scholar]
- Marsland AL, Pressman S, Cohen S. Positive affect and immune function. In: Ader R, editor. Psychoneuroimmunology. 4. San Diego, CA: Academic Press; 2007. pp. 761–779. [Google Scholar]
- McCrea RR, Costa PT. Personality, coping, and coping effectiveness in an adult sample. Journal of Personality. 1986;54:385–405. [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Review. 2007;87:873–904. doi: 10.1152/physrev.00041.2006. [DOI] [PubMed] [Google Scholar]
- McNiel JM, Fleeson W. The causal effects of extraversion on positive affect and neuroticism on negative affect: Manipulating state extraversion and state neuroticism in an experimental approach. Journal of Research in Personality. 2006;40:529–550. [Google Scholar]
- Mendes de Leon CF, Glass TA, Beckett LA, Seeman TE, Evans DA, Berkman LF. Social networks and disability transitions across eight intervals of yearly data in the New Haven EPESE. Journals of Gerontology B: Psychological Science and Social Science. 1999;54:S162–172. doi: 10.1093/geronb/54b.3.s162. [DOI] [PubMed] [Google Scholar]
- Murphy JG, McDevitt-Murphy ME, Barnett NP. Drink and be merry? Gender, life satisfaction, and alcohol consumption among college students. Psychology of Addictive Behavior. 2005;19:184–191. doi: 10.1037/0893-164X.19.2.184. [DOI] [PubMed] [Google Scholar]
- Nes RB, Roysamb E, Reichborn-Kjennerud T, Harris JR, Tambs K. Symptoms of anxiety and depression in young adults: Genetic and environmental influences on stability and change. Twin Research and Human Genetics. 2007;10:450–461. doi: 10.1375/twin.10.3.450. [DOI] [PubMed] [Google Scholar]
- Nilsson J. CRP Marker or maker of cardiovascular disease? Arteriosclerosis, Thrombosis and Vascular Biology. 2005;25:1527–1528. doi: 10.1161/01.ATV.0000174796.81443.3f. [DOI] [PubMed] [Google Scholar]
- O’Brien TB, DeLongis A. The interactional context of problem-, emotion-, and relationship-focused coping: The role of the Big Five personality factors. Journal of Personality. 1996;64:775–813. doi: 10.1111/j.1467-6494.1996.tb00944.x. [DOI] [PubMed] [Google Scholar]
- O’Donnell K, Badrick E, Kumari M, Steptoe A. Psychological coping styles and cortisol over the day in healthy older adults. Psychoneuroendocrinology. 2008;33:601–611. doi: 10.1016/j.psyneuen.2008.01.015. [DOI] [PubMed] [Google Scholar]
- Ong AD, Allaire JC. Cardiovascular intraindividual variability in later life: The influence of social connectedness and positive emotions. Psychology and Aging. 2005;20:476–485. doi: 10.1037/0882-7974.20.3.476. [DOI] [PubMed] [Google Scholar]
- Ong AD, Bergeman CS, Bisconti TL, Wallace KA. Psychological resilience, positive emotions, and successful adaptation to stress in later life. Journal of Personality and Social Psychology. 2006;91:730–749. doi: 10.1037/0022-3514.91.4.730. [DOI] [PubMed] [Google Scholar]
- Ostir GV, Markides KS, Black SA, Goodwin JS. Emotional well-being predicts subsequent functional independence and survival. Journal of the American Geriatric Society. 2000;48:473–478. doi: 10.1111/j.1532-5415.2000.tb04991.x. [DOI] [PubMed] [Google Scholar]
- Papanicolaou DA, Wilder RL, Manolagas SC, Chrousos GP. The pathophysiologic roles of interleukin-6 in human disease. Annals of Internal Medicine. 1998;128:127–137. doi: 10.7326/0003-4819-128-2-199801150-00009. [DOI] [PubMed] [Google Scholar]
- Patterson F, Lerman C, Kaufmann VG, Neuner GA, Audrain-McGovern J. Cigarette smoking practices among American college students: Review and future directions. Journal of American College Health. 2004;52:203–210. doi: 10.3200/JACH.52.5.203-212. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Frohlich C, Silbereisen RK. Optimism, pessimism, and change of psychological well-being in cancer patients. Psychology, Health and Medicine. 2007;12:421–432. doi: 10.1080/13548500601084271. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Influences of socioeconomic status, social network, and competence on subjective well-being in later life: A meta-analysis. Psychology and Aging. 2000;15:187–224. doi: 10.1037//0882-7974.15.2.187. [DOI] [PubMed] [Google Scholar]
- Polk DE, Cohen S, Doyle WJ, Skoner DP, Kirschbaum C. State and trait affect as predictors of salivary cortisol in healthy adults. Psychoneuroendocrinology. 2005;30:261–272. doi: 10.1016/j.psyneuen.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Pressman SD, Cohen S. Does positive affect influence health? Psychological Bulletin. 2005;131:925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Raison CL, Miller AH. When not enough is too much: The role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. American Journal of Psychiatry. 2003;160:1554–1565. doi: 10.1176/appi.ajp.160.9.1554. [DOI] [PubMed] [Google Scholar]
- Ranjit N, Diez-Roux AV, Shea S, Cushman M, Seeman T, Jackson SA, et al. Psychosocial factors and inflammation in the multi-ethnic study of atherosclerosis. Archives of Internal Medicine. 2007;167:174–181. doi: 10.1001/archinte.167.2.174. [DOI] [PubMed] [Google Scholar]
- Rauch U, Osende JI, Fuster V, Badimon JJ, Fayad Z, Chesebro JH. Thrombus formation on atherosclerotic plaques: Pathogenesis and clinical consequences. Annals of Internal Medicine. 2001;134:224–238. doi: 10.7326/0003-4819-134-3-200102060-00014. [DOI] [PubMed] [Google Scholar]
- Riolli L, Savicki V, Cepani A. Resilience in the face of catastrophe: Optimism, personality and coping in the Kosovo crisis. Journal of Applied Social Psychology. 2002;32:1604–1627. [Google Scholar]
- Roberts RE, Shema SJ, Kaplan GA, Strawbridge WJ. Sleep complaints and depression in an aging cohort: A prospective perspective. American Journal of Psychiatry. 2000;157:81–88. doi: 10.1176/ajp.157.1.81. [DOI] [PubMed] [Google Scholar]
- Rogers ME, Hansen NB, Levy BR, Tate DC, Sikkema KJ. Optimism and coping with loss in bereaved HIV-infected men and women. Journal of Social Psychology. 2005;24:341–360. [Google Scholar]
- Rottenberg J. Cardiac vagal control in depression: A critical analysis. Biological Psychology. 2007;74:200–211. doi: 10.1016/j.biopsycho.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Russell JA, Carroll JM. On the bipolarity of positive and negative affect. Psychological Bulletin. 1999;125:3–30. doi: 10.1037/0033-2909.125.1.3. [DOI] [PubMed] [Google Scholar]
- Salovey P, Rothman AJ, Detweiler JB, Steward WT. Emotional states and physical health. American Psychologist. 2000;55:110–121. doi: 10.1037//0003-066x.55.1.110. [DOI] [PubMed] [Google Scholar]
- Schmidt-Reinwald A, Pruessner JC, Hellhammer DH, Federenko I, Rohleder N, Schurmeyer TH, et al. The cortisol response to awakening in relation to different challenge tests and a 12-hour cortisol rhythm. Life Sciences. 1999;64:1653–1660. doi: 10.1016/s0024-3205(99)00103-4. [DOI] [PubMed] [Google Scholar]
- Schmitt DP, Realo A, Voracek M, Allik J. Why can’t a man be more like a woman? Sex differences in Big Five personality traits across 55 cultures. Journal of Personality and Social Psychology. 2008;94:168–182. doi: 10.1037/0022-3514.94.1.168. [DOI] [PubMed] [Google Scholar]
- Schnohr P, Kristensen TS, Prescott E, Scharling H. Stress and life dissatisfaction are inversely associated with jogging and other types of physical activity in leisure time The Copenhagen City Heart Study. Scandinavian Journal of Medicine & Science in Sports. 2005;15:107–112. doi: 10.1111/j.1600-0838.2004.00394.x. [DOI] [PubMed] [Google Scholar]
- Schwartz JE, Warren K, Pickering TG. Mood, location and physical position as predictors of ambulatory blood pressure and heart rate: Application of a multi-level random effects model. Annals of Behavioral Medicine. 1994;16:210–220. [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Shiota MN, Keltner D, John OP. Positive emotion dispositions differentially associated with Big Five personality and attachment style. Journal of Positive Psychology. 2006;2:61–71. [Google Scholar]
- Smyth J, Ockenfels MC, Porter L, Kirschbaum C, Hellhammer DH, Stone AA. Stressors and mood measured on a momentary basis are associated with salivary cortisol secretion. Psychoneuroendocrinology. 1998;23:353–370. doi: 10.1016/s0306-4530(98)00008-0. [DOI] [PubMed] [Google Scholar]
- Steel P, Schmidt J, Shultz J. Refining the relationship between personality and subjective well-being. Psychological Bulletin. 2008;134:138–161. doi: 10.1037/0033-2909.134.1.138. [DOI] [PubMed] [Google Scholar]
- Steptoe A. Depression and physical activity. In: Steptoe A, editor. Depression and physical illness. Cambridge, UK: Cambridge University Press; 2006a. pp. 348–368. [Google Scholar]
- Steptoe A, editor. Depression and physical illness. Cambridge, UK: Cambridge University Press; 2006b. [Google Scholar]
- Steptoe A. Cortisol awakening response. In: Fink G, editor. Encyclopedia of stress. 2. Vol. 1. Oxford: Academic Press; 2007. pp. 649–653. [Google Scholar]
- Steptoe A, Brydon L. Psychosocial factors and coronary heart disease: The contribution of psychoneuroimmunological processes. In: Ader R, editor. Psychoneuroimmunology. 4. San Diego, CA: Academic Press; 2007. pp. 945–974. [Google Scholar]
- Steptoe A, Donald AE, O’Donnell K, Marmot M, Deanfield JE. Delayed blood pressure recovery after psychological stress is associated with carotid intima-media thickness: Whitehall psychobiology study. Arteriosclerosis, Thrombosis and Vascular Biology. 2006;26:2547–2551. doi: 10.1161/01.ATV.0000242792.93486.0d. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Gibson EL, Hamer M, Wardle J. Neuroendocrine and cardiovascular correlates of positive affect measured by ecological momentary assessment and by questionnaire. Psychoneuroendocrinology. 2007;32:56–64. doi: 10.1016/j.psyneuen.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Hamer M, Chida Y. The effects of acute psychological stress on circulating inflammatory factors in humans: A review and meta-analysis. Brain Behavior and Immunity. 2007;21:901–912. doi: 10.1016/j.bbi.2007.03.011. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Marmot M. Psychosocial, hemostatic, and inflammatory correlates of delayed poststress blood pressure recovery. Psychosomatic Medicine. 2006;68:531–537. doi: 10.1097/01.psy.0000227751.82103.65. [DOI] [PubMed] [Google Scholar]
- Steptoe A, O’Donnell K, Badrick E, Kumari M, Marmot MG. Neuroendocrine and inflammatory factors associated with positive affect in healthy men and women: Whitehall II study. American Journal of Epidemiology. 2008;167:96–102. doi: 10.1093/aje/kwm252. [DOI] [PubMed] [Google Scholar]
- Steptoe A, O’Donnell K, Marmot M, Wardle J. Positive affect and psychosocial processes related to health. British Journal of Psychology. 2008a;99:211–217. doi: 10.1111/j.2044-8295.2008.tb00474.x. [DOI] [PubMed] [Google Scholar]
- Steptoe A, O’Donnell K, Marmot M, Wardle J. Positive affect, psychological well-being, and good sleep. Journal of Psychosomatic Research. 2008b;64:409–415. doi: 10.1016/j.jpsychores.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Owen N, Kunz-Ebrecht S, Mohamed-Ali V. Inflammatory cytokines, socioeconomic status, and acute stress responsivity. Brain Behavior and Immunity. 2002;16:774–784. doi: 10.1016/s0889-1591(02)00030-2. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Wardle J. Positive affect and biological function in everyday life. Neurobiology of Aging. 2005;26(Suppl 1):108–112. doi: 10.1016/j.neurobiolaging.2005.08.016. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Wardle J, Marmot M. Positive affect and health-related neuroendocrine, cardiovascular, and inflammatory processes. Proceedings of the National Academy of Sciences, USA. 2005;102:6508–6512. doi: 10.1073/pnas.0409174102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Medicine. 2005;6:23–27. doi: 10.1016/j.sleep.2004.06.003. [DOI] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, Hardison CB, Riley A. Informal social support networks and subjective well-being among African Americans. Journal of Black Psychology. 2001;27:439–463. [Google Scholar]
- Thayer JF, Sternberg E. Beyond heart rate variability: Vagal regulation of allostatic systems. Annals of the New York Academy of Sciences. 2006;1088:361–372. doi: 10.1196/annals.1366.014. [DOI] [PubMed] [Google Scholar]
- Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology. 2004;86:320–333. doi: 10.1037/0022-3514.86.2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tugade MM, Fredrickson BL. Regulation of positive emotions: Emotion regulation strategies that promote resilience. Journal of Happiness Studies. 2007;8:311–333. [Google Scholar]
- Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Valdimarsdottir HB, Bovbjerg DH. Positive and negative mood: Association with natural killer cell activity. Psychology and Health. 1997;12:319–327. [Google Scholar]
- van Eck M, Berkhof H, Nicolson N, Sulon J. The effects of perceived stress, traits, mood states, and stressful daily events on salivary cortisol. Psychosomatic Medicine. 1996;58:447–458. doi: 10.1097/00006842-199609000-00007. [DOI] [PubMed] [Google Scholar]
- Veenhoven R. Healthy happiness: Effects of happiness on physical health and the consequences for preventive health care. Journal of Happiness Studies. 2008;9:449–469. [Google Scholar]
- Vitterso J, Nilsen F. The conceptual and relational structure of subjective well-being, neuroticism, and extraversion: Once again, neuroticism is the important predictor of happiness. Social Indicators Research. 2002;57:89–118. [Google Scholar]
- Warner RM, Strowman SR. Cardiovascular reactivity and positive/negative affect during conversations. Journal of Behavioral Medicine. 1995;18:141–159. doi: 10.1007/BF01857866. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Measurement and mismeasurement of mood: Recurrent and emergent issues. Journal of Personality Assessment. 1997;68:267–296. doi: 10.1207/s15327752jpa6802_4. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wust S, Federenko I, Hellhammer DH, Kirschbaum C. Genetic factors, perceived chronic stress, and the free cortisol response to awakening. Psychoneuroendocrinology. 2000;25:707–720. doi: 10.1016/s0306-4530(00)00021-4. [DOI] [PubMed] [Google Scholar]