Abstract
To investigate the longitudinal course of cognitive functions in boys with persistent and remittent ADHD from childhood into young adult years. Males (n=217) 15-31 years with and without ADHD were assessed at 3 time points over 10 years into young adulthood. Subjects were stratified into Remittent ADHD, and Persistent ADHD based on the course of ADHD. Cognitive domains included: 1) overall IQ (overall IQ, block design IQ, vocabulary IQ, 2) achievement scores in reading and math and measures of executive function (Wechsler arithmetic, digit span, digit symbol, Rey-Osterrieth, Wisconsin Card Sorting Test, and the Stroop Test). Cognitive outcomes were modeled as a function of group (Controls, Remittent ADHD, and Persistent ADHD), age, group by age interaction, and any demographic confounders using linear growth-curve models. There were no significant interaction effects of group by time. Main group effects indicated that persistent and remittent ADHD groups both had significantly lower scores on all cognitve outcomes compared to Controls and these did not differ between them. Psychometrically-defined cognitive deficits are relatively stable into young adult years and appear to be independent of the course of ADHD. More work is needed to help define the implications of these deficits in individuals with a remitting course of ADHD.
Keywords: COGNITIVE DEFICITS, ADHD, STABILITY
1. Introduction
An extensive literature documents that children with ADHD have significant cognitive deficits relative to non-ADHD controls, including lower IQs, lower achievement scores in reading and mathematics and more impaired scores on tests of executive functions (EFs). Yet the relationship between ADHD and its cognitive correlates remains unclear.
Certainly, there is extensive empirical support for this range of impairments in ADHD. Regarding IQ, significant differences have been documented in large samples of boys (Biederman et al., 1996) and girls (Biederman et al., 1999) with ADHD when compared with youth of the same age and sex without the disorder. Likewise, Abikoff and Gittleman have found significant IQ differences between ADHD and healthy control subjects (Abikoff and Gittelman, 1985). Frazier et al. (2004) conducted a meta-analysis of 123 studies and concluded that overall cognitive ability was significantly lower among persons with ADHD, with a decrement roughly equivalent to a 9 point difference (0.6 of a standard deviation [SD]) on standardized tests. Recently, a meta-analysis of studies of adults suggested worse performance in adults with ADHD than controls on measures of intellectual functioning, albeit with a decrement of smaller magnitude (0.2 SD) (Bridgett and Walker, 2006).
Likewise the extant literature documents that children with ADHD are at significantly higher risk to manifest deficits in educational achievements. Faraone et al. (1993) found that learning disabilities, repeated grades, placement in special classes, and receiving academic tutoring were more likely in children with ADHD. Further, studies of ADHD have consistently documented that ADHD is associated with high levels of grade retention, need for tutoring and placement in special classes (Biederman et al., 1996; Biederman et al., 1999; Barkley et al., 2006). A recent meta-analysis by Frazier et al. (2007) also found that ADHD was associated with lower levels of overall achievement when compared with control subjects.
A consistent literature of published studies addressing neuropsychological performance in children with ADHD has also found a pattern of neuropsychological deficits in the executive system (Pennington and Ozonoff, 1996; Barkley, 1997; Seidman et al., 1997; Faraone and Biederman, 1998; Seidman et al., 2000). This literature, which has been recently summarized by several meta analyses (Hervey et al., 2004; Lijffijt et al., 2005; Martinussen et al., 2005; Willcutt et al., 2005), showed that individuals with ADHD commonly exhibit deficits in a wide range of executive functions including sustained attention, inhibition, working memory, verbal fluency, as well as executive processing speed (Lovejoy et al., 1999; Gallagher and Blader, 2001; Hervey et al., 2004).
Despite the contributions of these studies to the literature on cognitive deficits in ADHD, an important question remains unanswered: are ADHD-associated neurocognitive impairments trait or state dependent deficits? Since ADHD remits in a sizeable number of children with ADHD grown up, one way to address this important issue is to examine the course of neurocognitive deficits as a function of the course of ADHD in its persistent and remitting form. Considering the morbidity associated with neurocognitive deficits, knowledge about their stability in individuals with ADHD with and without persistent form of the disorder would be beneficial to clinicians dealing with individuals with ADHD for treatment planning.
To date very few studies examined the stability of cognitive functions in general in children with ADHD, regardless of persistence. Our group recently reported that IQ and achievement scores in reading and mathematics are very stable from childhood into young adult years in boys with ADHD (intraclass correlations: 0.79-0.84). Likewise, Hopkins et al. (1979) found that boys with hyperactivity continued to display deficits in executive functioning relative to the control group. Fischer et al. (2005) found that some neuropsychological deficits persisted into young adulthood in a follow-up sample of boys with ADHD grown up. Consistent with the notion of persistence of neurocognitive deficits in subjects with ADHD are the findings documenting cognitive deficits in adults with ADHD.
The main aim of this study was to assess whether the longitudinal course of neurocognitive functions in children with ADHD grown up is dependent or independent from the course of ADHD. To address these issues, we evaluated the longitudinal course of IQ, achievement scores in reading and math, and tests of executive functions in a large sample of well-characterized boys with and without ADHD ascertained from pediatric and psychiatric sources followed up from childhood into young adult years. Based on the literature documenting that adults with persistent ADHD have neurocognitive deficits, we hypothesized that deficits in psychometrically defined cognitive, neuropsychological, and achievement scores in reading and mathematics would be persistent over time. To the best of our knowledge, this study represents the most comprehensive evaluation of the longitudinal course of neurocognition in subjects with ADHD.
2. Methods
2.1. Subjects
Detailed methodological findings have been previously reported (Biederman et al., 1992; Biederman et al., 1996). Briefly, subjects were derived from a longitudinal case-control family study of Caucasian boys aged 6-17 years with (N=140) and without (N=120) DSM-III-R ADHD (Biederman et al., 1992; Biederman et al., 1996) ascertained from pediatric and psychiatric sources. Potential subjects were excluded if they had been adopted, or if their nuclear family was not available for study. We also excluded potential subjects if they had major sensorimotor handicaps (paralysis, deafness, blindness), psychosis, autism, inadequate command of the English language, or a Full Scale IQ less than 80. This sample was followed-up four and ten years after baseline assessment. At the 4-year follow-up 128 ADHD (91%) and 109 control (91%) subjects were retained. At the 10-year follow-up, 112 ADHD (80%) and 105 control (88%) subjects were successfully re-ascertained. Parents and adult offspring provided written informed consent to participate, and parents provided consent for offspring under the age of 18 years. Children and adolescents provided written assent to participate. The human research committee at Massachusetts General Hospital approved this study.
2.2. Assessment procedures
Psychiatric assessments relied on the Schedule for Affective Disorders and Schizophrenia for School-Aged Children – Epidemiologic Version (K-SADS-E) (Orvaschel, 1985; Orvaschel and Puig-Antich, 1987) for subjects younger than 18 years of age and the Structured Clinical Interview for DSM-IV (SCID) (Spitzer et al., 1990) (supplemented with modules from the K-SADS-E to assess childhood diagnoses) for subjects 18 years of age and older (Orvaschel, 1985; Orvaschel and Puig-Antich, 1987). Because this study had begun prior to the finalization of DSM-IV, our baseline assessment used DSM-III-R-based structured interviews but we supplemented these with questions that would allow us to make DSM-IV diagnoses. We conducted direct interviews with subjects and indirect interviews with their mothers (i.e., mothers complete the structured interview about their offspring). We combined data from direct and indirect interviews by considering a diagnostic criterion positive if it was endorsed in either interview.
Diagnoses of the subjects were based on independent interviews with the mothers and direct interviews with the children if they were older than 12 years of age. All assessments were made by raters who were blind to the youth's diagnosis (ADHD or non-ADHD control) and ascertainment site. Different interviewers met with mothers and youth in order to maintain blindness to case-control status and in order to prevent information from one informant influencing the assessment of the other. We computed kappa coefficients of agreement by having experienced, board certified child and adult psychiatrists and licensed clinical psychologists diagnose subjects from audio taped interviews. Based on 500 assessments from interviews of children and adults, the median kappa coefficient was 0.98. Kappa coefficients for individual diagnoses included: ADHD (0.88), conduct disorder (1.0), major depression (1.0), mania (0.95), separation anxiety (1.0), agoraphobia (1.0), panic (0.95), substance use disorder (1.0), and tics/Tourette's (0.89).
We considered a disorder positive if diagnostic criteria were unequivocally met. Diagnostic uncertainties were resolved by a review committee of at least two board-certified child and adult psychiatrists who were blind to the subject's ascertainment group, the ascertainment site, all data collected from other family members, and all non-diagnostic data (e.g., SES). We estimated the reliability of the diagnostic review process by computing kappa coefficients of agreement between clinician reviewers. For these clinical diagnoses, the median reliability between individual clinicians and the diagnoses assigned by the review committee was 0.87. Kappa coefficients for individual diagnoses included: ADHD (1.0), CD (1.0), ODD (0.90), ASPD (1.0), major depression (1.0), bipolar disorder (0.78), separation anxiety (0.89), agoraphobia (0.80), panic (0.77), OCD (0.73), GAD (0.90), specific phobia (0.85), PTSD (0.80), social phobia (0.90), substance use disorder (1.0), and tics/Tourette's (0.68).
2.3. Cognitive assessments
Cognitive testing was performed at each wave of data collection. At the baseline and 4-year follow-up we used the WISC-R/WAIS-R (Wechsler, 1974; Wechsler, 1981); the 10-year follow-up assessed IQ with the comparable WISC-III/WAIS-III (Wechsler, 1991; Wechsler, 1997). Using the methods of Sattler (1988) we estimated verbal IQ, performance IQ, and full-scale IQ from the vocabulary and block design subtests of the Wechsler scales. To assess working memory and processing speed we used the arithmetic, digit span, and digit symbol subtests. At baseline, academic achievement was assessed using the Gilmore Oral Reading test (Gilmore and Gilmore, 1968) and WRAT-R Arithmetic Subtest (Jastak and Jastak, 1985). At the 4-year follow-up, the WRAT-R Reading and Arithmetic Subtests (Jastak and Jastak, 1985) were used, and the comparable WRAT-III (Jastak and Jastak, 1993) was used at the 10-year follow-up. A reading achievement z-score was created to standardize the Gilmore and WRAT scales.
In addition, we constructed an aggregate neuropsychological z-score using domains of neuropsychological functioning thought to be important in ADHD and to be indirect indices of frontosubcortical brain systems (Biederman et al., 2004). Data on these measures was available only for the 4-year follow-up and the 10-year follow-up. In addition to the Wechsler arithmetic, digit span, and digit symbol scaled scores, we included: 1) the Rey-Osterrieth Complex Figure Copy (Rey, 1941); 2) perseverative and nonperseverative errors t-scores from the computerized Wisconsin Card Sorting Test (WCST) (Heaton et al., 1993); and 3) color, word, color-word, and interference t-scores from the Stroop Test (Golden, 1978). All assessments at follow-up were blind to baseline data collected on the same subjects.
2.4. Statistical analysis
We compared the baseline characteristics of subjects who were and were not assessed at the 10-year follow-up, separately in ADHD and control subjects. We compared ADHD and control subjects on follow-up demographic factors. Analyses of demographic factors relied on Pearson chi-squared tests and t-tests for binary and continuous variables, respectively.
ADHD remission was assigned to subjects at the10-year follow-up based on the number of symptoms that persisted. ADHD that met either full or subthreshold DSM-IV criteria at the 10-year follow-up assessment was considered to be Persistent ADHD. ADHD that did not meet at least subthreshold criteria for ADHD was considered to be Remittent ADHD. Linear growth curve models were used to estimate cognitive outcomes as a function of group (Controls, Remittent ADHD, and Persistent ADHD), age, group by age interaction, and any demographic confounders. In the event that the interaction of group and age were statistically significant, we analyzed the relationship between age and cognitive outcome separately for each of the three groups. If the interaction of group and age were not statistically significant, we removed the interaction term from the model and assessed the main effect of group independent of age and demographic confounds. All analyses were two-tailed with a significance level of 0.05.
3. Results
As presented elsewhere (Biederman et al., 2006), of the 140 ADHD and 120 control boys recruited at baseline, 112 (80%) and 105 (88%), respectively, were successfully re-assessed at the 10-year follow-up. The rate of successful follow-up did not differ between the groups (χ2(1)=2.6, P=0.11). There were no significant differences between those successfully followed up and those lost to follow-up on age, GAF score, familial intactness, ascertainment source, or psychiatric outcomes.
Only subjects with a cognitive assessment and a current diagnosis of ADHD at the 10-year follow-up were used for this analysis. Therefore, comparisons were made between Controls (N=72), Remittent ADHD (N=33), and Persistent ADHD (N=57). The Persistent ADHD group was significantly younger than the other groups, and both ADHD groups were more likely to have been ascertained from the psychiatric source compared to the Controls (Table 1). Thus, all subsequent statistical analyses corrected for ascertainment source (age was included in all models a priori).
Table 1.
Demographic characteristics by ADHD status. Mean ± SD or N (%)
| Controls (N=72) |
Remittent ADHD (N=33) |
Persistent ADHD (N=57) |
Test statistic |
P-value | |
|---|---|---|---|---|---|
| Age | |||||
| Baseline | 10.8 ± 3.8 | 11.7 ± 2.8 | 9.5 ± 2.7 a*b*** | F(2,159)=5.5 0 |
0.005 |
| 4-year follow-up | 14.6 ± 3.9 | 15.5 ± 2.9 | 13.3 ± 2.7 b** | F(2,139)=4.0 6 |
0.02 |
| 10-year follow-up | 22.0 ± 4.0 | 22.4 ± 3.1 | 20.5 ± 3.2 a*b** | F(2,159)=4.1 9 |
0.02 |
| Family socioeconomic status | 1.5 ± 0.7 | 1.7 ± 1.0 | 1.7 ± 0.9 | χ2(2)=2.26 | 0.32 |
| Ascertainment source, psychiatric | 21 (29) | 17 (52) a* | 32 (56) a** | χ2(2)=10.60 | 0.005 |
a=vs. Controls; b=vs. Remittent ADHD
P≤0.05
P≤0.01
P≤0.001
Lifetime rates of placement in a special class were lowest for the Controls (1.4%), followed by the Remittent ADHD group (30.3%, P<0.001 vs. Controls), and highest in the Persistent ADHD group (56.1%, P<0.001 vs. Controls and P=0.02 vs. Remittent ADHD). Lifetime rates of a repeated grade were higher in the Remittent and Persistent ADHD groups (36.4% and 38.6%, respectively) compared to the Controls (13.9%, P=0.009 vs. Remittent ADHD and P<0.001 vs. Persistent ADHD). Likewise, lifetime rates of extra tutoring were higher in the Remittent and Persistent ADHD groups (81.8% and 93.0%, respectively) compared to the Controls (38.9%, both P<0.001).
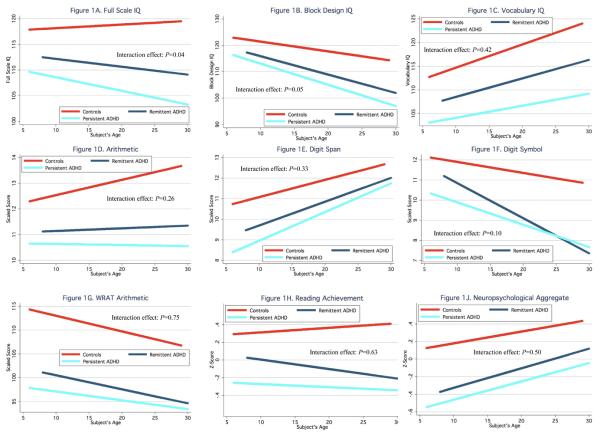
Table 2 provides the means and standard deviations for each of the nine cognitive variables by group and assessment time. Figure 1 depicts fitted lines of linear growth curves of cognitive outcomes by age for Controls, Remittent ADHD, and Persistent ADHD. Only estimated full scale IQ and block design IQ had a nominal significant interaction effect of group and age (χ2(2)=6.34, P=0.04 and χ2(2)=5.99, P=0.05, respectively). This full scale IQ interaction effect was accounted for by the relative steeper decline in IQ scores among the Persistent ADHD subjects over time. The block design IQ interaction was accounted for by the steeper declines over time in block design IQ for both ADHD groups compared to the Controls. However, there were no meaningful differences between the two ADHD groups and both groups significantly differed from controls on full scale and block design IQ. In contrast, there were no interaction effects with any other measure of cognition assessed. Main group effects indicated that both ADHD groups had significantly lower scores on all of the remaining cognitive outcomes compared to Controls. There were no significant differences between Persistent ADHD and Remittent ADHD on any of the cognitive outcomes assessed (all P>0.05).
Table 2.
Means and standard deviations of cognitive variables by group and assessment time.
| Controls | Remittent ADHD | Persistent ADHD | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline (N=72) |
4-year (N=65) |
10-year (N=72) |
Baseline (N=33) |
4-year (N=31) |
10-year (N=33) |
Baseline (N=57) |
4-year (N=46) |
10-year (N=57) |
|
| Full scale IQ | 118.8±10.6 | 117.1±10.7 | 119.0±10.0 | 112.7±13.2 | 109.7±14.5 | 110.8±14.6 | 109.6±13.0 | 106.9±12.7 | 106.0±12.7 |
| Block design IQ | 122.4±13.7 | 117.5±13.7 | 117.2±12.6 | 116.4±16.3 | 108.8±17.5 | 108.1±16.9 | 115.2±14.8 | 108.7±15.9 | 105.3±15.8 |
| Vocabulary IQ | 115.2±11.8 | 116.8±11.4 | 120.8±10.6 | 109.0±15.0 | 110.6±15.4 | 113.4±17.7 | 103.9±14.6 | 105.1±13.7 | 106.8±15.0 |
| Arithmetic | 12.5 ± 2.8 | 12.8 ± 2.9 | 13.2 ± 2.4 | 11.1 ± 3.2 | 11.2 ± 3.1 | 11.3 ± 3.4 | 10.8 ± 3.5 | 10.2 ± 2.8 | 10.7 ± 3.2 |
| Digit span | 10.8 ± 2.5 | 12.0 ± 3.0 | 11.9 ± 2.9 | 9.9 ± 2.6 | 10.2 ± 3.2 | 11.2 ± 3.6 | 8.9 ± 2.8 | 9.4 ± 2.9 | 10.5 ± 2.5 |
| Digit symbol | 11.9 ± 2.9 | 11.8 ± 3.0 | 11.0 ± 2.8 | 10.6 ± 3.6 | 10.4 ± 3.3 | 8.8 ± 3.2 | 10.0 ± 3.6 | 9.8 ± 3.3 | 8.6 ± 3.0 |
| WRAT arithmetic | 113.8±15.2 | 111.8±15.4 | 108.6±13.0 | 100.7±19.2 | 97.2±18.3 | 97.2±18.0 | 97.7±16.4 | 94.8±17.4 | 95.2±15.7 |
| Reading achievement |
0.3 ± 0.8 | 0.4 ± 0.7 | 0.3 ± 0.6 | 0.0 ± 1.2 | −0.1 ± 1.3 | −0.1 ± 1.3 | −0.3 ± 1.0 | −0.4 ± 1.2 | −0.3 ± 0.9 |
| Neuropsychological aggregate |
NA | 0.2 ± 0.5 | 0.3 ± 0.5 | NA | −0.2 ± 0.7 | −0.1 ± 0.7 | NA | −0.4 ± 0.6 | −0.2 ± 0.6 |
NA=not assessed at baseline
Figure 1.
IQ, neuropsychological, and achievement scores by age in subjects with persistent ADHD, remittent ADHD, or without ADHD
4. Discussion
This 10-year follow-up of boys with and without ADHD grown up found that measures of IQ, achievement and executive functions are largely stable from childhood into young adult years. Results also document the relative independence of neurocognitive function from the course of ADHD supporting the hypothesis that cognitive functions in subjects with ADHD represent a trait component of the disorder. To the best of our knowledge, this is the first study documenting the relative independence of cognitive deficits in subjects with ADHD from the course of the disorder.
The findings showing that ADHD boys grown up continue to manifest cognitive deficits are consistent with an extensive literature documenting that children and adults with ADHD have significant cognitive deficits including lower IQs, lower achievement scores in reading and mathematics (Frazier et al., 2004; Frazier et al., 2007) and more impaired scores on tests of executive functions (EFs) than controls without this disorder (Willcutt et al., 2005). Faraone et al. (1993) found that learning disabilities, repeated grades, placement in special classes, and receiving academic tutoring were more likely in children with ADHD and studies of neuropsychological functioning consistently document that individuals with ADHD commonly exhibit deficits in a wide range of executive functions including sustained attention, working memory, verbal fluency, as well as executive processing speed (Lovejoy et al., 1999; Gallagher and Blader, 2001; Hervey et al., 2004; Lijffijt et al., 2005; Martinussen et al., 2005; Willcutt et al., 2005).
However, while persistence of neurocognitive deficits in persistent cases of ADHD is not surprising, their persistence in remitting cases is novel. From our own work as well as a recent meta-analysis of follow-up studies (Faraone et al., 2006) we know that although ADHD is a persistent disorder in a majority of affected subjects, some cases of ADHD remit over time. The fact that cognitive deficits can remain in such cases adds to a growing literature indicating the complexity of the relationship between the behavioral and cognitive features of the disorder. For example, twin and family studies (Doyle, 2006; Willcutt, 2006) suggest that ADHD symptoms and executive function impairments share some but not all etiological risk factors. It is also the case that standard pharmacologic treatments for ADHD do not ameliorate cognitive dysfunction (Biederman et al., 2008). The current data serve to further underscore the separability of these behavioral and cognitive constructs and highlight the need to develop more effective ways to intervene in the face of cognitive impairments. For example, there is a clear need for novel pharmacological agents. Moreover, it would be useful for future studies to examine whether the timing of behavioral and pharmacologic interventions that produce symptom remission can improve long-term cognitive outcome in these individuals as well.
Although further work should determine the functional implication of persistent cognitive deficits in children with a remitting course of ADHD, they may not be minor. The transition from adolescence to adulthood is fraught with many challenges that stress neurocognitive functions and may possibly lead to functional deficits. Moreover, our prior work showed that cognitive deficits predicted compromised educational functioning in childhood and occupational attainments in adults (Biederman et al., 2004). More work is needed to determine if such deficits will extend to subjects without persistent ADHD. Irrespective of this knowledge, the assessment of cognitive functions clearly provides information that cannot be extracted from assessments of psychopathology.
It is noteworthy that our findings are partly inconsistent with those reported by Fisher et al. (2005) in a long-term follow-up of boys with ADHD grown up. Although these investigators found that remittance of ADHD symptoms reduced cognitive deficits, the tests that were found to improve were proxies of the symptoms of ADHD rather than IQ or executive function scores. More work is needed to reconcile these apparent discrepant findings.
The strengths of this report include the well-characterized sample, the reliance on well-established neuropsychological battery, and the long-term follow-up period of the sample into young adult years. This is especially important since very few other studies have followed children with ADHD into adulthood with longitudinal assessments of their neurocognitive functions. Also, our sample was ascertained from both pediatric and psychiatric sources enhancing the generalizability of our findings.
On the other hand, our results should be considered in light of some methodological limitations. Since the majority of our subjects were Caucasians, our results may not generalize to other ethnic groups. Because the sample was referred, we do not know if our results will generalize to children with ADHD in the general population. However, because we sampled from both psychiatric and pediatric referrals, our results should generalize to a wide range of referred cases, which are of most interest to clinicians. While our aim was to assess the young adult outcome of children with ADHD, a small portion of our sample had not yet reached adulthood. Also of note, the discrepancy between affected and control subjects was generally consistent with Frazier et al.'s meta-analysis (2004), though greater than differences found in Bridgett and Walker (2006). Based on data from this latter study, it is possible that sample characteristics such as comorbidities and learning disabilities have influenced the magnitude of the group differences. The effect of such moderators (e.g., learning disabilities) on cognitive deficits was not addressed in this analysis because of the complexity they would add with regard to interpretation of findings and because our definition of learning disabilities relied upon IQ and achievement scores, which were used as outcome variables. Future research should investigate the role of such factors on the course of other cognitive deficits. Additionally, the current data derive from longitudinal family genetic studies of ADHD that excluded probands with IQ < 80 due to the potential for subjects with low IQ to have a differing genetic etiology for their disorder and/or cognitive dysfunction. Therefore, we did not assess subjects at the lowest end of the range. Nonetheless, the overall variability and range of IQ scores in our sample suggest that our data are appropriate for the current analyses. Finally, it is noteworthy that our measure of IQ was based on only the Vocabulary and Block Design subtests. Correlations between Vocabulary and Block Design and Verbal and Performance IQ, respectively are approximately 0.9 (Sattler, 1988). Thus, we felt that these subtests were more conservative and unbiased approximations of FSIQ than the other available subtests, including Digit Span, Arithmetic, and Coding, which reflect constructs (e.g., working memory) that are known to be impaired in ADHD and thought to be linked to the underlying etiology of the disorder.
Despite these considerations, our 10-year follow-up study of boys with ADHD grown up show that psychometrically-defined cognitive deficits are relatively stable into young adult years and appear to be independent of the course of ADHD. More work is needed to help define the implications of these deficits in individuals with a remitting course of ADHD.
Acknowledgement
This study was supported by grant 5R01HD036317 from the National Institute of Child Health and Human Development. Support also came, in part, from the Neal-Kimmerly Fund for the Study of Cognition Boston, MA, USA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Abikoff H, Gittelman R. Hyperactive children treated with stimulants. Archives of General Psychiatry. 1985;42:953–961. doi: 10.1001/archpsyc.1985.01790330033004. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychological Bulletin. 1997;121(1):65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: adaptive functioning in major life activities. J Am Acad Child Adolesc Psychiatry. 2006;45(2):192–202. doi: 10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone S, Milberger S, Guite J, Mick E, Chen L, Mennin D, Marrs A, Ouellette C, Moore P, Spencer T, Norman D, Wilens T, Kraus I, Perrin J. A prospective 4-year follow-up study of attention-deficit hyperactivity and related disorders. Archives of General Psychiatry. 1996;53(5):437–46. doi: 10.1001/archpsyc.1996.01830050073012. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Keenan K, Benjamin J, Krifcher B, Moore C, Sprich-Buckminster S, Ugaglia K, Jellinek MS, Steingard R, Spencer T, Norman D, Kolodny R, Kraus I, Perrin J, Keller MB, Tsuang MT. Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder. Patterns of comorbidity in probands and relatives in psychiatrically and pediatrically referred samples. Archives of General Psychiatry. 1992;49(9):728–38. doi: 10.1001/archpsyc.1992.01820090056010. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Mick E, Williamson S, Wilens TE, Spencer TJ, Weber W, Jetton J, Kraus I, Pert J, Zallen B. Clinical correlates of ADHD in females: findings from a large group of girls ascertained from pediatric and psychiatric referral sources. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(8):966–975. doi: 10.1097/00004583-199908000-00012. [DOI] [PubMed] [Google Scholar]
- Biederman J, Monuteaux M, Mick E, Spencer T, Wilens T, Silva J, Snyder L, Faraone SV. Young Adult Outcome of Attention Deficit Hyperactivity Disorder: A Controlled 10 year Prospective Follow-Up Study. Psychological Medicine. 2006;36(2):167–179. doi: 10.1017/S0033291705006410. [DOI] [PubMed] [Google Scholar]
- Biederman J, Monuteaux M, Seidman L, Doyle AE, Mick E, Wilens T, Ferrero F, Morgan C, Faraone SV. Impact of Executive Function Deficits and ADHD on Academic Outcomes in Children. Journal of Consulting and Clinical Psychology. 2004;72(5):757–766. doi: 10.1037/0022-006X.72.5.757. [DOI] [PubMed] [Google Scholar]
- Biederman J, Seidman LJ, Petty CR, Fried R, Doyle AE, Cohen DR, Kenealy DC, Faraone SV. Effects of Stimulant Medication on Neuropsychological Functioning in Young Adults With Attention-Deficit/Hyperactivity Disorder. J Clin Psychiatry. 2008:e1–e7. doi: 10.4088/jcp.v69n0715. [DOI] [PubMed] [Google Scholar]
- Bridgett DJ, Walker ME. Intellectual functioning in adults with ADHD: a meta-analytic examination of full scale IQ differences between adults with and without ADHD. Psychol Assess. 2006;18(1):1–14. doi: 10.1037/1040-3590.18.1.1. [DOI] [PubMed] [Google Scholar]
- Doyle AE. Familial aggregation of ADHD symptom dimensions and aspects of executive functions; ADHD endophenotypes symposium, International Neuropsychological Society Annual Meeting; Boston, MA. February 3, 2006. [Google Scholar]
- Faraone S, Biederman J, Mick E. The Age Dependent Decline Of Attention-Deficit/Hyperactivity Disorder: A Meta-Analysis Of Follow-Up Studies. Psychological Medicine. 2006;36(2):159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J. Neurobiology of attention-deficit hyperactivity disorder. Biological Psychiatry. 1998;44(10):951–958. doi: 10.1016/s0006-3223(98)00240-6. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Lehman BK, Spencer T, Norman D, Seidman L, Kraus I, Perrin J, Chen W, Tsuang MT. Intellectual performance and school failure in children with attention deficit hyperactivity disorder and in their siblings. Journal of Abnormal Psychology. 1993;102(4):616–623. doi: 10.1037/0021-843X.102.4.616. [DOI] [PubMed] [Google Scholar]
- Fischer M, Barkley RA, Smallish L, Fletcher K. Executive functioning in hyperactive children as young adults: attention, inhibition, response perseveration, and the impact of comorbidity. Dev Neuropsychol. 2005;27(1):107–33. doi: 10.1207/s15326942dn2701_5. [DOI] [PubMed] [Google Scholar]
- Frazier TW, Demaree HA, Youngstrom EA. Meta-analysis of intellectual and neuropsychological test performance in attention-deficit/hyperactivity disorder. Neuropsychology. 2004;18(3):543–55. doi: 10.1037/0894-4105.18.3.543. [DOI] [PubMed] [Google Scholar]
- Frazier TW, Youngstrom EA, Glutting JJ, Watkins MW. ADHD and achievement: meta-analysis of the child, adolescent, and adult literatures and a concomitant study with college students. J Learn Disabil. 2007;40(1):49–65. doi: 10.1177/00222194070400010401. [DOI] [PubMed] [Google Scholar]
- Gallagher R, Blader J. The Diagnosis and Neuropsychological Assessment of Adult Attention Deficit/Hyperactivity Disorder: Scientific Study and Practical Guidelines. Ann NY Acad Sci. 2001;931:148–171. doi: 10.1111/j.1749-6632.2001.tb05778.x. [DOI] [PubMed] [Google Scholar]
- Gilmore JV, Gilmore EC. Gilmore oral reading test. Harcourt, Brace & World, Inc.; New York: 1968. [Google Scholar]
- Golden CJ. Stroop Color and Word Test: A Manual for Clinical and Experimental Use. Stoelting, Co.; Chicago: 1978. [Google Scholar]
- Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G. Wisconsin Card Sort Test Manual: Revised and Expanded. Psychological Assessment Resources, Inc.; Odessa, FL: 1993. [Google Scholar]
- Hervey AS, Epstein J, Curry JF. Neuropsychology of adults with attention-deficit/hyperactivity disorder: a meta-analytic review. Neuropsychology. 2004;18(3):485–503. doi: 10.1037/0894-4105.18.3.485. [DOI] [PubMed] [Google Scholar]
- Hopkins J, Perlman T, Hechtman L, Weiss G. Cognitive style in adults originally diagnosed as hyperactives. Journal of Child Psychology and Psychiatry. 1979;20:209–216. doi: 10.1111/j.1469-7610.1979.tb00504.x. [DOI] [PubMed] [Google Scholar]
- Jastak J, Jastak S. Wide Range Achievement Test-Third Edition. Jastak Associates; Wilmington, DE: 1993. [Google Scholar]
- Jastak JF, Jastak S. The Wide Range Achievement Test-Revised. Jastak Associates; Wilmington, Delaware: 1985. [Google Scholar]
- Lijffijt M, Kenemans JL, Verbaten MN, van Engeland H. A meta-analytic review of stopping performance in attention-deficit/hyperactivity disorder: deficient inhibitory motor control? J Abnorm Psychol. 2005;114(2):216–22. doi: 10.1037/0021-843X.114.2.216. [DOI] [PubMed] [Google Scholar]
- Lovejoy DW, Ball JD, Keats M, Stutts ML, Spain E, Janda L, Janusz J. Neuropsychological performance of adults with attention deficit hyperactivity disorder (ADHD): diagnostic classification estimates for measures of frontal lobe/executive functioning. Journal of the International Neuropsychological Society. 1999;5:222–233. doi: 10.1017/s1355617799533055. [DOI] [PubMed] [Google Scholar]
- Martinussen R, Hayden J, Hogg-Johnson S, Tannock R. A meta-analysis of working memory impairments in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2005;44(4):377–84. doi: 10.1097/01.chi.0000153228.72591.73. [DOI] [PubMed] [Google Scholar]
- Orvaschel H. Psychiatric interviews suitable for use in research with children and adolescents. Psychopharmacol Bull. 1985;21(4):737–45. [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J. Schedule for Affective Disorders and Schizophrenia for School-Age Children: Epidemiologic Version. Nova University; Fort Lauderdale, FL: 1987. [Google Scholar]
- Pennington BF, Ozonoff S. Executive functions and developmental psychopathology. Journal of Child Psychology and Psychiatry. 1996;37(1):51–87. doi: 10.1111/j.1469-7610.1996.tb01380.x. [DOI] [PubMed] [Google Scholar]
- Rey A. L'examen psychologique dans les cas d'encephalopathie traumatique. Les Archives de Psychologie. 1941;28:286–340. [Google Scholar]
- Sattler JM. Assessment of Children. Jerome M. Sattler, Publisher; San Diego, CA: 1988. [Google Scholar]
- Seidman L, Biederman J, Monuteaux M, Weber W, Faraone SV. Neuropsychological functioning in nonreferred siblings of children with attention deficit hyperactivity disorder. Journal of Abnormal Psychology. 2000;109(2):252–265. doi: 10.1037/0021-843X.109.2.252. [DOI] [PubMed] [Google Scholar]
- Seidman LJ, Biederman J, Faraone SV, Weber W, Ouellette C. Toward defining a neuropsychology of attention deficit-hyperactivity disorder: performance of children and adolescents from a large clinically referred sample. Journal of Consulting and Clinical Psychology. 1997;65(1):150–160. doi: 10.1037/0022-006X.65.1.150. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R: Non-Patient Edition (SCID-NP, Version 1.0) American Psychiatric Press; Washington, DC: 1990. [Google Scholar]
- Wechsler D. Manual for the Wechsler Intelligence Scale for Children-Revised. The Psychological Corporation; New York: 1974. [Google Scholar]
- Wechsler D. Manual for the Wechsler Adult Intelligence Scale - Revised. The Psychological Corporation; San Antonio: 1981. [Google Scholar]
- Wechsler D. Manual for the Wechsler Intelligence Scale for Children - Third Edition. The Psychological Corporation, Harcourt Brace Jovanovich, Inc.; San Antonio: 1991. [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale III [manual] The Psychological Corporation; San Antonio, TX: 1997. [Google Scholar]
- Willcutt EG. Twin study of the etiology of the relation between ADHD and executive function; ADHD endophenotypes symposium, International Neuropsychological Society Annual Meeting; Boston, MA. February 3, 2006. [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of ADHD: A meta-analytic review. Biological Psychiatry. 2005;57(11):1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]