Abstract
This paper addresses a number of areas related to how effectively science and technology have met Healthy People 2010 goals for tooth decay prevention. In every area mentioned, it appears that science and technology are falling short of these goals. Earlier assessments identified water fluoridation as one of the greatest public health accomplishments of the last century. Yet, failure to complete needed clinical and translational research has shortchanged the caries prevention agenda that incomplete at a critical juncture.
Science has firmly established the transmissible nature of tooth decay. However, there is evidence that tooth decay in young children is increasing although progress has been made in other age groups. Studies of risk assessment have not been translated into improved practice. Antiseptics, chlorhexidine varnish, and PVP-iodine may have value, but definitive trials are needed. Fluorides remain the most effective agents, but are not widely disseminated to the most needy. Fluoride varnish provides a relatively effective topical preventive for very young children, yet definitive trials have not been conducted. Silver diammine fluoride also has potential but requires study in the US. Data support effectiveness and safety of xylitol, but adoption is not widespread. Dental sealants remain a mainstay of public policy, yet after decades of research, widespread use has not occurred.
We conclude that research has established the public health burden of tooth decay, but insufficient research addresses the problems identified in the Surgeon General's Report. Transfer of technology from studies to implementation is needed to prevent tooth decay among children. This should involve translational research and implementation of scientific and technological advances into practice.
INTRODUCTION
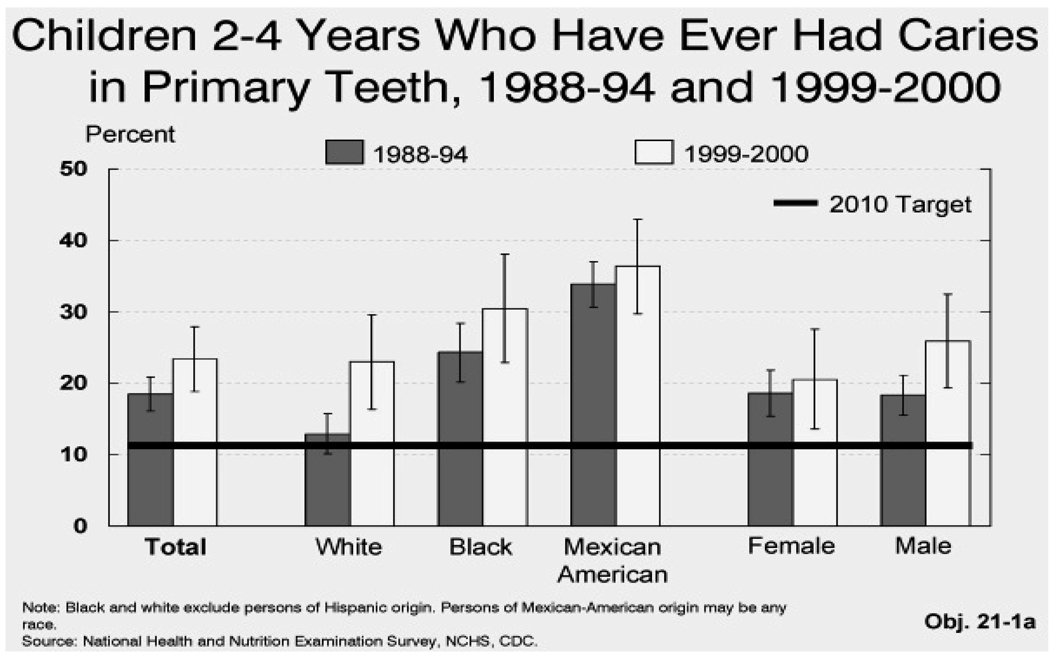
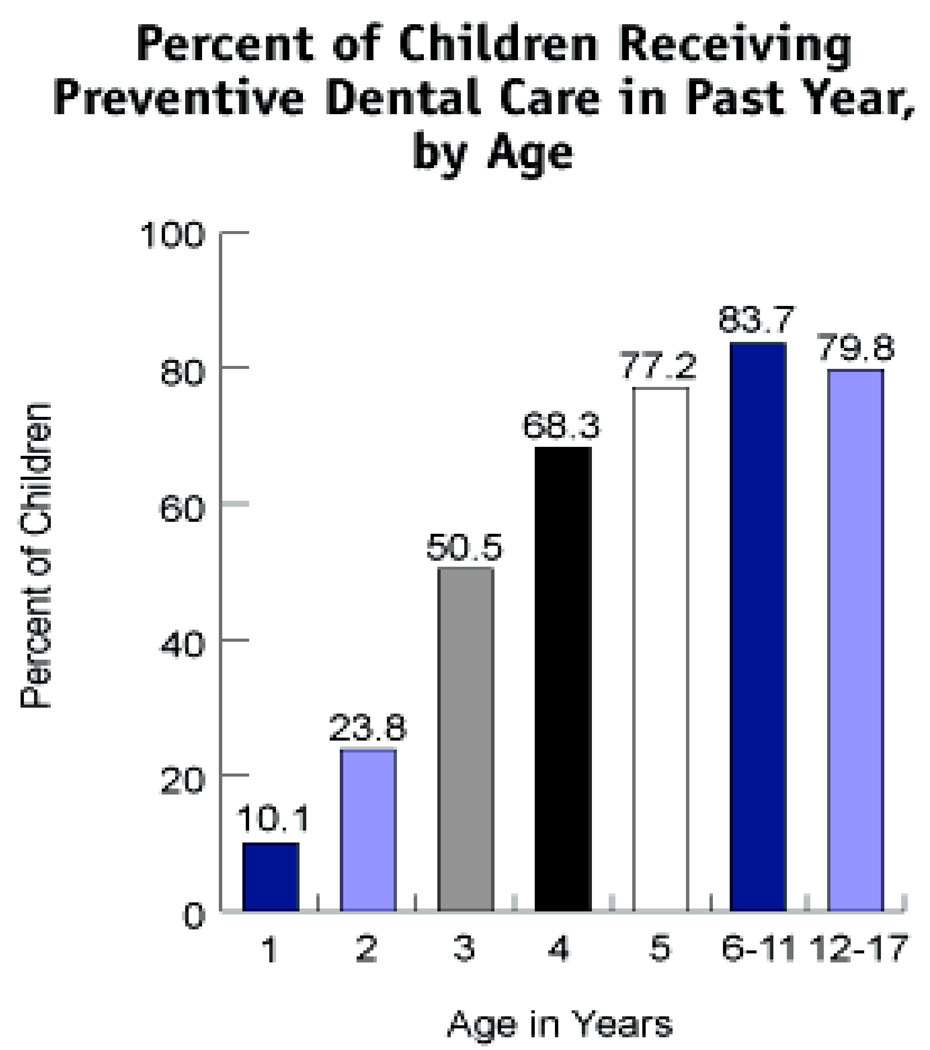
Ample evidence demonstrates that the country is failing to move toward meeting Healthy People 2010 goals to improve the oral health of preschoolers with respect to tooth decay,1 and this problem is expanding with higher disease rates and dental workforce shortages.2 The Midcourse Review for Healthy People 2010 suggested that tooth decay (caries) rates for children 2–5 years old were increasing, primarily among the poor and minorities, and most lesions are untreated, to say nothing of prevented.1 Figure 1 is excerpted from this report. The problem likely extends to older poor and minority children as dental caries lesions are cumulative and untreated decay of primary teeth strongly predicts the same condition of secondary (permanent) teeth.3–8 However, older children are more likely to receive some preventive care (see Figure 2, from the National Survey of Children’s Health).
Figure 1.
Figure 2.
Tooth decay is attributable mostly to the infectious nature of dental caries in humans.9–11 Complicating this problem are workforce shortages12, lack of access to care1, and discrimination against populations served by Medicaid13–14. This paper examines advances in science and technology associated with prevention of tooth decay in young children since the Surgeon General’s Report of 2000.
The Infectious Nature of Caries
Strategies for dental caries prevention and management can take advantage of the infectious nature of the disease or choose to view it as independent of its infectious nature. The evidence of transmission, initially from mother to child, is demonstrated not only by the correlation of maternal salivary titers of mutans streptococci (referred to hereafter as Streptococcus mutans or S. mutans) with the early colonization of her child and the early inception of caries lesions in the child, but also by the identity of S. mutans colonizing mother and her child, based on bacteriocin typing, endonuclease, and ribo-typing.11,15–18 A strong scientific basis supports evaluation of the microbial status of young mothers as predictors of the colonization of their young children’s’ teeth.11 Interventions in the mother to suppress her S. mutans prolong the time to colonization of her children and prolong the time and reduce the severity of carious lesion inception.19–21 The notion of a discrete window of infectivity until about 26 months of age during which transmission occurs22 has been expanded following studies that showed colonization at younger ages and prior to tooth eruption. It is estimated in one study that S. mutans is harbored by at least 20 percent of children under 14 months of age23 and at least 25 percent of predentate children in another.24 The source of the S. mutans after 5 years of age is not known, but is likely to include siblings and caretakers, at least.
This review focuses on the preventive strategies and technologies applicable to individual children that address goals of Health People 2010 and if applied might mitigate the inequities identified by the Surgeon General’s Report on Oral Health (SGROH). The science and technologies to be reviewed are:
Detection and Risk Assessment
Interventions to Improve Prevention of Tooth Decay
DETECTION AND RISK ASSESSMENT
Early Tooth Decay Lesion Detection
Industry has developed high technology devices that allow detection of early signs of decay lesions. Early detection could increase opportunity to arrest and reverse tooth damage using a “medical” approach25 and prevent the need for traditional “surgical” interventions that partially remove and reconstruct (fill) the teeth, or extract them. The devices generally have high sensitivity but inadequate specificity. Their clinical application is further limited because one method cannot be used for all tooth surfaces and under all circumstances.26 Presently they appear to add little to competent visual/tactile examination.27–28 Moreover, these devices may be misused to justify surgical interventions and fabrication of fillings, sometimes mislabeled “minimally invasive”, instead of intensifying efforts to arrest early lesions. Devices with the best performance are expensive and cumbersome, their use time consuming, with little application in typical dental practice, community practice, or community health centers. Simpler approaches, such as fiber-optic transillumination, may be more readily adopted.29
A multinational academic group has begun testing a totally visual caries lesion assessment scheme (ICDAS, International Caries Detection and Assessment System II) that focuses on early lesion detection, before cavitation has begun.30–31 As with the technology-based systems, the rationale is that earlier detection will increase opportunity to arrest and reverse lesions and prevent need for surgical interventions. The ICDAS has acceptable reliability and validity, but requires rigorous training, and remains in development.32
To date there has been limited impact on training of dental students, community or health center practice adoption, although this situation could rapidly change if research demonstrated how best to achieve this aim. These methods, whether high tech or visual, rely on detection of lesions after they have occurred.
Timely Risk Assessment
As cited above, detection of carious lesions of young children is a strong risk predictor of carious lesions of older children. Also, early carious lesions (“white spots”) are strong predictors of frank cavitation of the teeth.11 Dietary risk factors are also important. Risk assessment tools have been promoted to guide clinicians.33–34 These strategies may be helpful to primary care providers who see infants and toddlers on a regular basis. One example is the CAMBRA Caries Risk Assessment Form for Age 0 to 5 Years.35 However, assessments of the children’s mothers or caretakers in terms of microbiology or caries experience, or on their infection status, may be appropriate as well.18
At the extremes, the level of colonization by Streptococcus mutans is an indicator and a predictor of caries activity.11 High levels are typical of children with ECC.24,36 At lower levels of colonization the relationship is poorer; no doubt due, at least in part, to the confounding effect of fluoride exposure and the diverse testing methods used. Testing is relatively simple and cost effective if it leads to sound anticipatory guidance and prevention of disease in children. Nevertheless, bacterial testing in U.S. dental practices does not appear widespread. Research on the adoption of these technologies in both primary medicine and dentistry practice is needed.
INTERVENTIONS TO IMPROVE PREVENTION OF TOOTH DECAY
Vaccines, Bacterial Replacement, and Targeted Antimicrobial Peptides
Efforts to develop vaccines against dental caries based on both active and passive immunization continue. Secretory immune response to antigens of S. mutans can influence caries pathogenesis.37–42 With some exceptions, most work has been done in animal models. Protection is attributable to salivary sIgA antibodies (active). Antibodies made in another host and delivered to humans (passive immunity) are also of interest. By selection of different antigens as the target for immunization, both active and passive strategies seek to inhibit a variety of functions critical to S. mutans in the biofilm on teeth (dental plaque). Replacement of virulent (cariogenic) S. mutans with non-virulent streptococci is also being investigated in experimental animals and humans.43 Early in vitro work on specifically targeted antimicrobial peptides44 continues but no in vivo validation has been reported. FDA approval of specific immunization and clinical application are still problematic because of unresolved risk-benefit questions and commercial investment required to fund extensive trials to meet regulatory requirements.
Antiseptics
There are several studies of the utility of antiseptic agents to inhibit caries in older, self compliant individuals.19,45 With regard to preschoolers, some are strong advocates for combining fluorides with various antimicrobials, especially for those with disparities and whose families are mobile, because topical fluorides do not provide complete protection against tooth decay.46 Two topical antimicrobials have been investigated to some extent: chlorhexidine di-gluconate (CH) and polyvinylpyrollidone iodine (PVP-I).
Chlorhexidine
Chlorhexidine (CH) rinses, available in the U.S., are sold by prescription but are lower in concentration (to reduce staining of teeth) than products sold in other countries. Approved by the FDA for gingivitis control, no formulation has FDA approved for caries control in children. Research, particularly in Europe and China, has examined the effectiveness of a CH varnish coating for the teeth, with mixed results. A recent systematic review of 14 publications of controlled clinical trials concluded there was a moderate caries reducing effect when the varnish was applied every three to four months.47 The variability in CH varnish formulations may have strongly influenced bioavailability and thus effect of CH. While CH varnish and other CH-containing vehicles may have value in caries prevention for very young children, the evidence is inconclusive; no child-products are available in the U.S., and none can be recommended.
I2/KI and PVP Iodine
The in vitro and in vivo iodine antiseptic literature on dental caries of three decades ago was promising, but most human studies were very small.48–49 Pilot and small scale clinical studies of utility of PVP-I in young children, some with established active ECC, show strongly encouraging data.50–53 Larger scale evaluations are warranted and timely.
Topical Fluorides
The benefits of fluoride delivery via professional in-office applications, home-use mouthrinses, gels and toothpastes are well established. These strategies have had limited impact on populations with little access to the dentist. Community water fluoridation is highly effective but depends upon public water supplies and political approval of their fluoridation. Mouth rinses, gels and toothpastes are individual compliance-dependent, and dependent on economic and access feasibility. In the late 1990s, manufacturers gained approval from the FDA to market topical sodium fluoride varnishes first available in Europe in the 1960s. Although indicated formally for tooth sensitivity reduction primarily in adults, they are being used for decay prevention and arrest in children, and good data suggest that they are more effective than the older technologies.54–55 The varnishes are safe for infants and toddlers.
Manufacturers have not sought, however, an indication for prevention of decay, perhaps because they see the market as small and return on investment not large. The formulation of the varnishes is largely unregulated, and manufacturers have produced various forms of varnish that alter their properties. No data show that these competing products are equivalent.
The varnishes are important because they provide an easy to use, safe, and cheap fluoride vehicle for preschoolers, our most vulnerable population. While the varnishes are being adopted in public health practice, use in private dental practice lags. There has been movement for physicians and nurses to apply varnish, and in some states Medicaid reimburses these primary care practitioners in addition to dentists and dental hygienists for this service.56 The Preventive Services Task Force, Centers for Disease Control and Prevention (CDC), American Dental Association (ADA) and American Academy of Pediatrics (AAP) have not endorsed topical fluoride treatment for primary prevention in children before 24 months of age and AAP guidelines specifically note the lack of a definitive trial.57 Thus, a multi-center clinical trial is needed to demonstrate the effectiveness of fluoride varnish delivered during well-baby visits by primary care physicians and nurses.
New studies on the adoption of this technology in practice are needed. There have been almost no attempts to study ways to spread adoption.58
Diammine silver fluoride
Research outside the U.S. has highlighted the value of diammine silver fluoride to both arrest and prevent recurrences of ECC. This product has been available in Japan and several other countries for years but was never brought to the U.S. Evidence suggests that it is at least twice as effective as sodium fluoride varnish.59–60 One drawback, staining of the cavity/tooth after treatment, appears preventable.61 Research is needed to learn about how this compound works. NIH is just beginning to sponsor research regarding this potentially helpful approach but lack of FDA approval is a barrier.
Xylitol
Xylitol is a sugar substitute that is “generally regarded as safe” by FDA. In teens and young adults, it is not only non-cariogenic but also anti-cariogenic. Its use is limited, like that of other sugar alcohols, by its limited absorbability from the gut. Its benefit cannot be attributed merely to a salivation stimulatory effect of chewing gum use.62 Xylitol is a safe and effective tooth decay preventive agent when incorporated into chewing gum or other confections used habitually.63–65 Its use, like that of fluoride, is associated with promotion of remineralization of white spots and established lesions. Considerable evidence indicates that it inhibits the metabolism of S. mutans.66–67 The American Academy of Pediatric Dentistry supports use of xylitol chewing gum as a caries inhibitor, but recommends further research. It emphasizes the need for proper labeling of xylitol products so that parents and professionals can make appropriate choices.68 Nevertheless, application has been limited by absence of formulations that demand minimal adherence and are acceptable in a greater variety of settings, such as in preschools/schools. A minimum of five to six grams and three exposures per day from chewing gum or candies are needed for clinical effect in adults.69 A recent study found that xylitol oral syrup administered topically two or three times per day at a total dose of 8 g was effective in preventing early childhood caries.70
A landmark study showed that when mothers of preschoolers chewed high content xylitol chewing gum habitually, their preschoolers had delayed colonization and lower levels of S. mutans, and similarly delayed and much reduced caries experience.71–72 In spite of the large body of data supporting the effectiveness and safety of xylitol and a growing number of products, its adoption—particularly in the period immediately post-partum, is not widespread. The cost of xylitol-sugar free products for daily use is relatively high by comparison with other sugar-free products, but modest by comparison with the cost of filling of carious lesions.
Occlusal Sealants
While there were convincing data at the time of the SGROH for the application of sealants as a key objective of Healthy People 2010, the actual adoption of sealants by dentists has not been achieved.1 Sealants are designed to be placed when the permanent molars erupt (around 7–8 and 13–14 years old). Data up to 2004 suggests no more than 32 percent of children receive this service, up from 23 percent during 1988–94. The equivalent rate for age 14 is 21 percent.73 In part, this is because up to one-third of permanent molars are cavitated by the time the teeth erupt enough to be sealed, depending on the risk group, and most dentists will not seal caries lesions in spite of evidence that this strategy can be effective in arresting them.74–75
The only innovation since the SGROH has been the development and marketing of glass ionomer sealants. The argument for this strategy is that glass ionomers can be placed on partially erupted permanent teeth where they release small amounts of fluoride, putatively inhibiting local lesion development. However, only limited pilot studies of these materials exist and their potential remains unexplored. Retention rates of the glass ionomer cement sealants are lower than current generation of conventional resin-based sealants. The limited literature on sealing primary molars is not encouraging.76 Definitive studies are needed.
Non-fluoride remineralization strategies
There has been considerable interest in developing novel remineralizing agents that complement or substitute for the clinical effectiveness of fluoride. Studies largely sponsored by industry have been conducted to promote products claiming to remineralize early caries lesions.77–79 These products are formulated as professionally applied pastes, toothpastes and gums. Conceptually, the work is interesting. Nevertheless, the work is not focused on control of early lesions of ECC and claims of effectiveness are not well substantiated. Little has been done to establish how such products would be used to benefit children.
CONCLUSIONS
This review has focused on the role of science and technology in achieving the goals of Healthy People 2010. Tooth decay is a serious and growing problem for very young children. It impacts quality of life. It especially affects the poor, ethnic minorities, Native Americans and Alaska Native populations.
Dental caries is an infectious disease yet the application of this concept in practice is limited. Accordingly, antimicrobial approaches, directed at both mothers and at young children, have an important place in tooth decay prevention and control. Antiseptics, chlorhexidine varnish and PVP-iodine, as well as xylitol chewing gum used by mothers, have been shown to be effective in inhibiting carious lesion incidence, but definitive trials are needed.
Fluorides remain the most effective agents but are not widely disseminated to the neediest. Fluoride varnish provides a relatively effective topical preventive for very young children, yet definitive trials of its application in primary care practice have not been conducted. Scientific advances outside the U.S. have suggested the potential of silver diammine fluoride, but it is not FDA approved and no research has been carried out in the U.S. Data support effectiveness and safety of xylitol, but adoption is not widespread and additional research is needed on formulations and vehicles to increase access. Dental sealants are of unquestioned benefit and remain a mainstay of public policy yet, after decades of research, widespread use has not occurred. Definitive trials are needed of new materials that can be used on erupting teeth.
The research in the U.S. to address the growing level of tooth decay in our youngest children is too limited. Research and adoption have not kept pace with the problems identified in the Surgeon General’s Report on Oral Health. Transfer of technology from studies to implementation lags.
Acknowledgments
Supported, in part, by Grant Nos. U54DE14254 and U54DE019346 from the National Institute of Dental and Craniofacial Research, NIH
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No conflicts of interest
Contributor Information
Peter Milgrom, Northwest Center to Reduce Oral Health Disparities, Box 357475, University of Washington, Seattle, WA 98195-7475, USA. dfrc@u.washington.edu; Telephone +1 206 685 4183; Fax +1 206 685 4258.
Domenick T. Zero, Preventive and Community Dentistry, Director, Oral Health Research Institute, Indiana University School of Dentistry, Indianapolis, IN 46202. dzero@iupui.edu; Telephone +1 317 274 8822.
Jason M. Tanzer, Depts. Oral Health and Diagnostic Sciences, and Pathology and Laboratory Medicine, University of Connecticut Health Center, Farmington, CT 06030-1605. tanzer@nso.uchc.edu; Telephone 1+ 860-679-2855.
References
- 1.US DHHS. HP 2010 Midcourse Review. [Accessed September 3, 2007];Progress Quotient Chart for Focus Area 21: Oral Health. Available at: http://www.healthypeople.gov/Data/midcourse/html/tables/pq/PQ-21.htm.
- 2.Milgrom P, Weinstein P, Huebner C, Graves J, Tut O. Empowering Head Start to improve access to good oral health for children from low income families. Matern Child Health J. 2008 Feb 2; doi: 10.1007/s10995-008-0316-6. PMID: 18246416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frenzel A. Das schicksal der sechsjahrmolaren in der schulzahnpflege. Deutsche Monatsschrift fur Zahnheilkunde. 1933;51:437. [Google Scholar]
- 4.Birkeland JM, Broach L, Jorkjend L. Caries experience as predictor for caries incidence. Community Dent Oral Epidemiol. 1976 Mar;4(2):66–69. doi: 10.1111/j.1600-0528.1976.tb01605.x. [DOI] [PubMed] [Google Scholar]
- 5.Bader JD, Graves RC, Disney JA, Bohannan HM, Stamm JW, Abernathy JR, Lindahl RL. Identifying children who experienced high caries increments. Community Dent Oral Epidemiol. 1986 Aug;14(4):198–201. doi: 10.1111/j.1600-0528.1986.tb01534.x. [DOI] [PubMed] [Google Scholar]
- 6.van Palenstein Helderman WH, van’t Hof MA, van Loveren C. Prognosis of caries increment with past caries experience variables. Caries Res. 2001 May–June;35(3):186–192. doi: 10.1159/000047454. [DOI] [PubMed] [Google Scholar]
- 7.Wang WJ, Li YH, Bian JY. An eight-year longitudinal study for caries status on primary and permanent dentitions in Beijing children. Zhonghua Kou Qikang Yi Xue Za Zhi. 2003 July;38(4):279–281. [PubMed] [Google Scholar]
- 8.Motohashi M, Yamada H, Genkai F, Kato H, Imai T, Sato S, Sugaya A, Maeno M. Employing dmft score as a risk predictor for caries development in the permanent teeth in Japanese primary school girls. J Oral Sci. 2006 Dec;48(4):233–237. doi: 10.2334/josnusd.48.233. [DOI] [PubMed] [Google Scholar]
- 9.Loesche WJ. Role of Streptococcus mutans in human dental decay. Microbiol Rev. 1986 Dec;50(4):353–380. doi: 10.1128/mr.50.4.353-380.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Houte J. Role of micro-organisms in caries etiology. J Dent Res. 1994 Mar;73(3):672–681. doi: 10.1177/00220345940730031301. [DOI] [PubMed] [Google Scholar]
- 11.Tanzer JM, Livingston J, Thompson AM. The microbiology of primary dental caries in humans. J Dent Educ. 2001 Oct;65(10):1028–1037. [PubMed] [Google Scholar]
- 12.Bailit H, Beazoglou T, Demby N, McFarland J, Robinson P, Weaver B. Dental safety net: current capacity and potential for expansion. J Am Dent Assoc. 2006;137:807–815. doi: 10.14219/jada.archive.2006.0294. [DOI] [PubMed] [Google Scholar]
- 13.Guendelman S, Angulo V, Wier M, Oman D. Overcoming the odds: access to care for immigrant children in working poor families in California. Matern Child Health J. 2005;59:351–362. doi: 10.1007/s10995-005-0018-2. [DOI] [PubMed] [Google Scholar]
- 14.Lam M, Riedy CA, Milgrom P. Improving access for Medicaid-insured children: focus on front-office personnel. J Am Dent Assoc. 1999;130:365–373. doi: 10.14219/jada.archive.1999.0206. [DOI] [PubMed] [Google Scholar]
- 15.Berkowitz RJ, Jordan HV. Similarity of bacteriocins of Streptococcus mutans from mother and infant. Arch Oral Biol. 1975 Nov;20(11):725–730. doi: 10.1016/0003-9969(75)90042-4. [DOI] [PubMed] [Google Scholar]
- 16.Li Y, Caufield PW. The fidelity of initial acquisition of mutans streptococci by infants from their mothers. J Dent Res. 1995 Feb;74(2):681–685. doi: 10.1177/00220345950740020901. [DOI] [PubMed] [Google Scholar]
- 17.Masuda N, Shimamoto T, Kitamura K, Sobue S, Hamada S. Transmission of Streptococcus mutans in some selected families. Microbios. 1985;44(181S):223–232. [PubMed] [Google Scholar]
- 18.Köhler B, Bratthall D. Intrafamilial levels of Streptococcus mutans and some aspects of the bacterial transmission. Scand J Dent Res. 1978 Jan;86(1):35–42. doi: 10.1111/j.1600-0722.1978.tb00605.x. [DOI] [PubMed] [Google Scholar]
- 19.Köhler B, Andréen I. Influence of caries-preventive measures in mothers on cariogenic bacteria and caries experience in their children. Arch Oral Biol. 1994 Oct;39(10):907–911. doi: 10.1016/0003-9969(94)90023-x. [DOI] [PubMed] [Google Scholar]
- 20.Söderling E, Isokangas P, Pienihäkkinen K, Tenovuo J, Alanen P. Influence of maternal xylitol consumption on mother-child transmission of mutans streptococci: 6-year follow-up. Caries Res. 2001;35:173–177. doi: 10.1159/000047452. [DOI] [PubMed] [Google Scholar]
- 21.Isokangas P, Söderling E, Pienihäkkinen K, Alanen P. Occurrence of dental decay in children after maternal consumption of xylitol chewing gum, a follow-up from 0 to 5 years of age. J Dent Res. 2000 Nov;79(11):1885–1889. doi: 10.1177/00220345000790111201. [DOI] [PubMed] [Google Scholar]
- 22.Caufield PW, Cutter GR, Dasanayake AP. Initial acquisition of mutans streptococci by infants: evidence for a discrete window of infectivity. J Dent Res. 1993 Jan;72(1):37–45. doi: 10.1177/00220345930720010501. [DOI] [PubMed] [Google Scholar]
- 23.Mohan A, Morse DE, O'Sullivan DM, Tinanoff N. The relationship between bottle usage/content, age, and number of teeth with mutans streptococci colonization in 6-24-month-old children. Community Dent Oral Epidemiol. 1998 Feb;26(1):12–20. doi: 10.1111/j.1600-0528.1998.tb01918.x. [DOI] [PubMed] [Google Scholar]
- 24.Milgrom P, Riedy CA, Weinstein P, Tanner ACR, Manibusan L, Bruss J. Dental caries and Its relationship to bacterial infection, hypoplasia, diet, and oral hygiene in 6 to 3 6 month old children. Community Dent Oral Epidemiol. 2000 Aug;28(4):295–306. doi: 10.1034/j.1600-0528.2000.280408.x. [DOI] [PubMed] [Google Scholar]
- 25.Köhler B, Andréen I, Jonsson B. The earlier the colonization by mutans streptococci, the higher the caries prevalence at 4 years of age. Oral Microbiol Immunol. 1988 Mar;3(1):14–17. doi: 10.1111/j.1399-302x.1988.tb00598.x. [DOI] [PubMed] [Google Scholar]
- 26.Zandona AF, Zero DT. Diagnostic tools for early caries detection. J Am Dent Assoc. 2006;137:1675–1684. doi: 10.14219/jada.archive.2006.0113. [DOI] [PubMed] [Google Scholar]
- 27.Kavvadia K, Lagouvardos P. Clinical performance of a diode laser fluorescence device for detection of occlusal caries in primary teeth. Int J Paediatr Dent. 2008 May;18(3):197–204. doi: 10.1111/j.1365-263X.2007.00913.x. [DOI] [PubMed] [Google Scholar]
- 28.Kühnisch J, Berger S, Goddon I, Senkel H, Pitts N, Heinrich-Welzien R. Occlusal caries detection in permanent molars according to WHO basic methods, ICDAS II and laser fluorescence measurements. Community Dent Oral Epidemiol. Epub. 2008 Apr 14; doi: 10.1111/j.1600-0528.2008.00436.x. [DOI] [PubMed] [Google Scholar]
- 29.Davies GM, Worthington HV, Clarkson JE, Thomas P, Davies RM. The use of fibre-optic transillumination in general dental practice. Br Dent J. 2001 Aug 11;191(3):145–147. doi: 10.1038/sj.bdj.4801123. [DOI] [PubMed] [Google Scholar]
- 30.Ekstrand KR, Martignon S, Ricketts DJ, Qvist V. Detection and activity assessment of primary coronal caries lesions: a methodologic study. Oper Dent. 2007 May–Jun;32(3):225–235. doi: 10.2341/06-63. [DOI] [PubMed] [Google Scholar]
- 31.Ismail AI, Sohn W, Tellez M, Amaya A, Sen A, Hasson H, Pitts NB. The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol. 2007 Jun;35(3):170–178. doi: 10.1111/j.1600-0528.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 32.Jablonski-Momeni A, Stachniss V, Ricketts DN, Heinzel-Gutenbrunner M, Pieper K. Reproducibility and accuracy of the ICDAS-II for detection of occlusal caries in vitro. Caries Res. 2008;42(2):79–87. doi: 10.1159/000113160. Epub: 2008 Jan 15. [DOI] [PubMed] [Google Scholar]
- 33.Kutsch VK, Milicich G, Domb W, Anderson M, Zinman E. How to integrate CAMBRA into private practice. J Calif Dent Assoc. 2007 Nov;35(11):778–785. [PubMed] [Google Scholar]
- 34. [Accessed July 10, 2009];Caries Management by Risk Assessment. URL www.nnoha.org/goopages/pages_downloadgallery/download.php?filename=5519_8469001.doc&orig_name=CAMBRA%20ECC%20Risk%20Assmt%200-5%20yrs.doc.
- 35.American Academy of Pediatric Dentistry. [Accessed June 25, 2008];Policy on use of a Caries-risk Assessment Tool (CAT) for infants, children, and adolescents. 2006 Available at: http://www.aapd.org/media/Policies_Guidelines/P_CariesRiskAssess.pdf. [PubMed]
- 36.Marchant S, Brailsford SR, Twomey AC, Roberts GJ, Beighton D. The predominant microflora of nursing caries lesions. Caries Res. 2001 Nov–Dec;35(6):397–406. doi: 10.1159/000047482. [DOI] [PubMed] [Google Scholar]
- 37.Taubman MA, Nash DA. The scientific and public-health imperative for a vaccine against dental caries. Nat Rev Immunol. 2006 July;6(7):555–563. doi: 10.1038/nri1857. [DOI] [PubMed] [Google Scholar]
- 38.Smith DJ, Mattos-Graner RO. Secretory immunity following mutans streptococcal infection or immunization. Curr Top Microbiol Immunol. 2008;319:131–156. doi: 10.1007/978-3-540-73900-5_6. [DOI] [PubMed] [Google Scholar]
- 39.Xu OA, Yu F, Fan MW, Bian Z, Chen Z, Peng B, Jia R, Guo JH. Protective efficacy of a targeted anti-caries DNA plasmid against cariogenic bacteria infections. Vaccine. 2007 Jan 26;25(7):1191–1195. doi: 10.1016/j.vaccine.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 40.Canettieri AC, Kretchetoff FY, Kogga Ito CY, Moreira D, Fujarra FJ, Unterkircher CS. Production of monoclonal antibodies against Streptococcus mutans antigen. Braz Oral Res. 2006 Oct–Dec;20(4):297–302. doi: 10.1590/s1806-83242006000400003. [DOI] [PubMed] [Google Scholar]
- 41.Culshaw S, Larosa K, Tolani H, Han X, Eastcott JW, Smith DJ, Taubman MA. Immunogenic and protective potential of mutans streptococcal glucosyltransferase peptide constructs selected by major histocompatibility complex Class II allele binding. Infect Immun. 2007 Feb;75(2):915–923. doi: 10.1128/IAI.01582-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Childers NK, Li F, Dasanayake AP, Li Y, Kirk K, Michalek SM. Immune response in humans to a nasal boost with Streptococcus mutans antigens. Oral Microbiol Immunol. 2006 Oct;21(5):309–313. doi: 10.1111/j.1399-302X.2006.00302.x. [DOI] [PubMed] [Google Scholar]
- 43.Hillman JD, Mo J, McDonell E, Cvitkovitch D, Hillman CH. Modification of an effector strain for replacement therapy of dental caries to enable clinical safety trials. J App Microbiol. 2007 May;102(5):1209–1219. doi: 10.1111/j.1365-2672.2007.03316.x. [DOI] [PubMed] [Google Scholar]
- 44.Eckert R, He J, Yarbrough DK, Qi F, Anderson MH, Shi W. Targeted killing of Streptococcus mutans by a pheromone-guided “smart” antimicrobial peptide. Antimicrob Agents Chemother. 2006 Nov;50(11):3651–3657. doi: 10.1128/AAC.00622-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zickert I, Emilson CG, Krasse B. Effect of caries preventive measures in children highly infected with the bacterium Streptococcus mutans. Arch Oral Biol. 1982;27(10):861–868. doi: 10.1016/0003-9969(82)90042-5. [DOI] [PubMed] [Google Scholar]
- 46.Featherstone JD. Delivery challenges for fluoride, chlorhexidine and xylitol. BMC Oral Health. 2006;15(6) Suppl 1:58. doi: 10.1186/1472-6831-6-S1-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang Q, van Palenstein Helderman WH, van’t Hof MA, Truin GJ. Chlorhexidine varnish for preventing dental caries in children, adolescents and young adults: a systematic review. Eur J Oral Sci. 2006 Dec;114(6):449–455. doi: 10.1111/j.1600-0722.2006.00392.x. [DOI] [PubMed] [Google Scholar]
- 48.Tanzer JM, Slee AM, Kamay B, Scheer ER. In vitro evaluation of three iodine-containing compounds as antiplaque agents. Antimicrob Agents Chemother. 1977;12:107–113. doi: 10.1128/aac.12.1.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Caufield PW, Wannemuehler YM. In vitro susceptibility of Streptococcus mutans 6715 to iodine and sodium fluoride, singly and in combination, at various pH values. Antimicrob Agents Chemother. 1982. 1982 Jul;2(1):115–119. doi: 10.1128/aac.22.1.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tinanoff N, O’Sullivan DM. Early Childhood caries: overview and recent findings. Pediatr Dent. 1997;19:12–16. [PubMed] [Google Scholar]
- 51.Zahn L, Featherstone JDB, Gansky SA, Hoover CI, Fujino T, Berkowitz RJ, DenBesten PK. Antibacterial treatment needed for severe early childhood caries. J Pub Health Dent. 2006;66:174–179. doi: 10.1111/j.1752-7325.2006.tb02576.x. [DOI] [PubMed] [Google Scholar]
- 52.Amin MS, Harrison RL, Benton TS, Roberts MC, Weinstein P. Effect of povidone-iodine on Streptococcus mutans in children with extensive dental caries. Pediatr Dent. 2004;26:5–10. [PubMed] [Google Scholar]
- 53.Lopez L, Berkowitz RJ, Spiekerman C, Weinstein P. Topical antimicrobial therapy in the prevention of early childhood caries: a follow-up report. Pediatr Dent. 2002;24:204–206. [PubMed] [Google Scholar]
- 54.Marinho VCC, Higgins JPT, Logan S, Sheiham A. Fluoride varnishes for preventing dental caries in children and adolescents. [Accessed September 3, 2007];Cochrane Database of Systematic Reviews. 2002 (Issue 1) doi: 10.1002/14651858.CD002279. Art. No.: CD002279. Available at: http://doi.wiley.com/10.1002/14651858.CD002279. [DOI] [PubMed] [Google Scholar]
- 55.National Institutes of Health (U.S.) Diagnosis and management of dental caries throughout life. NIH Consensus Statement. 2001 Mar 26–28;18(1):1–23. [PubMed] [Google Scholar]
- 56.Slade GD, Rozier RG, Zeldin LP, Margolis PA. Training pediatric health care providers in prevention of dental decay: results from a randomized controlled trial. BMC Health Serv Res. 2007 Nov 2;7:176. doi: 10.1186/1472-6963-7-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.AAP. [Accessed July 10, 2009];Oral Health Risk Assessment Training Program. URL: www.aap.org/commpeds/dochs/oralhealth/cme/course-6.htm.
- 58.Grembowski D, Spiekerman C, del Aguila MA, Anderson M, Reynolds D, Ellersik A, Foster J, Choate L. Randomized pilot study to disseminate caries-control services in dentist offices. BMC Oral Health. May;206:6–7. doi: 10.1186/1472-6831-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chu CH, Lo ECM, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res. 2002;81(11):767–770. doi: 10.1177/0810767. [DOI] [PubMed] [Google Scholar]
- 60.Llodra JC, Rodriguez A, Ferrer B, Menardia V, Ramos T, Morato M. Efficacy of silver diamine fluoride for caries reduction in primary teeth and first permanent molars of schoolchildren: 36-month clinical trial. J Dent Res. 2005 Aug;84(8):721–724. doi: 10.1177/154405910508400807. [DOI] [PubMed] [Google Scholar]
- 61.Knight GM, McIntyre JM, Craig GG, Mulyanim, Zilm PS, Gull NJ. Differences between normal and remineralized dentine pretreated with silver fluoride and potassium iodide after an in vitro challenge by Streptococcus mutans. Austral Dent J. 2007;52:16–21. doi: 10.1111/j.1834-7819.2007.tb00460.x. [DOI] [PubMed] [Google Scholar]
- 62.Hildebrandt GH, Sparks BS. Maintaining mutans streptococci suppression with xylitol chewing gum. J Am Dent Assoc. J Amer Dent Assoc. 2000 Jul;131(7):909–916. doi: 10.14219/jada.archive.2000.0309. [DOI] [PubMed] [Google Scholar]
- 63.Milgrom P, Ly KA, Rothen M. Xylitol and its vehicles for public health needs. Adv Dent Res. 2009;21:44–47. doi: 10.1177/0895937409335623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mäkinen KK, Hujoel PP, Bennett CA, Isokangas P, Isotupa K, Pape HR, Jr, Mäkinen PL. A descriptive report of the effects of a 16-month xylitol chewing-gum programme subsequent to a 40-month sucrose gum programme. Caries Res. 1998;32(2):107–112. doi: 10.1159/000016439. [DOI] [PubMed] [Google Scholar]
- 65.Mäkinen KK, Bennett CA, Hujoel PP, Isokangas PJ, Isotupa KP, Pape HR, Jr, Mäkinen PL. Xylitol chewing gums and caries rates: a 40-month cohort study. J Dent Res. 1995 Dec;74(12):1904–1913. doi: 10.1177/00220345950740121501. [DOI] [PubMed] [Google Scholar]
- 66.Tanzer JM, Thompson A, Wen ZT, Burne RA. Streptococcus mutans: fructose transport, xylitol resistance, and virulence. J Dent Res. 2006 Apr;85(4):369–373. doi: 10.1177/154405910608500417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Trahan L. Xylitol: a review of its action on mutans streptococci and dental plaque--its clinical significance. Int Dent J. 1995 Feb;45(1) Suppl 1:77–92. [PubMed] [Google Scholar]
- 68.American Academy of Pediatric Dentistry. [Accessed June 26, 2008];Policy on the use of xylitol in caries prevention. 2006 Available at: http://www.aapd.org/media/Policies_Guidelines/P_Xylitol.pdf. [PubMed]
- 69.Milgrom P, Ly KA, Rothen M. Xylitol and its vehicles for public health needs. Adv Dent Res. 2009;21:44–47. doi: 10.1177/0895937409335623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Milgrom P, Ly KA, Tut OK, Mancl L, Roberts MC, Briand K, Giancio MJ. Xylitol pediatric topical oral syrup to prevent dental caries. A double-blind randomized clinical trial of efficacy. Arch Pediatr Adolesc Med. 2009;163:601–607. doi: 10.1001/archpediatrics.2009.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Söderling E, Isokangas P, Pienihäkkinen K, Tenovuo J, Alanen P. Influence of maternal xylitol consumption on mother-child transmission of mutans streptococci: 6-year follow-up. Caries Res. 2001;35:173–177. doi: 10.1159/000047452. [DOI] [PubMed] [Google Scholar]
- 72.Isokangas P, Söderling E, Pienihäkkinen K, Alanen P. Occurrence of dental decay in children after maternal consumption of xylitol chewing gum, a follow-up from 0 to 5 years of age. J Dent Res. 2000 Nov;79(11):1885–1889. doi: 10.1177/00220345000790111201. [DOI] [PubMed] [Google Scholar]
- 73.CDC Wonder. Data 2010…the Healthy People 2010 Database-May, 2009 Edition-Objective 21-8a and 21-8b. [Accessed July 10, 2009]; [Google Scholar]
- 74.Beauchamp J, Caufield PW, Crall JJ, Donly K, Feigal R, Gooch B, Ismail A, Kohn W, Siegal M, Simonsen R. Evidence-based clinical recommendations for the use of pit-and-fissure sealants: A report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2008;139:257–268. doi: 10.14219/jada.archive.2008.0155. [DOI] [PubMed] [Google Scholar]
- 75.Griffin SO, Oong E, Kohn W, Vidakovic B, et al. The effectiveness of sealants in managing caries lesions. J Den Res. 2008 Feb;87(2):169–174. doi: 10.1177/154405910808700211. [DOI] [PubMed] [Google Scholar]
- 76.Chadwick BL, Treasure ET, Playle RA. A randomised controlled trial to determine the effectiveness of glass ionomer sealants in pre-school children. Caries Res. 2005 Jan–Feb;39(1):34–40. doi: 10.1159/000081654. [DOI] [PubMed] [Google Scholar]
- 77.Reynolds EC, Cai F, Shen P, Walker GD. Retention in plaque and remineralization of enamel lesions by various forms of calcium in a mouthrinse or sugar-free chewing gum. J Dent Res. 2003 Mar;82(3):206–211. doi: 10.1177/154405910308200311. [DOI] [PubMed] [Google Scholar]
- 78.Morgan MV, Adams GG, Bailey DL, Tsao CE, Fischman SL, Reynolds EC. The anticariogenic effect of sugar-free gum containing CPP-ACP nanocomplexes on approximal caries determined using digital bitewing radiography. Caries Res. 2008;42(3):171–184. doi: 10.1159/000128561. [DOI] [PubMed] [Google Scholar]
- 79.Reynolds EC, Cai F, Cochrane NJ, Shen P, Walker GD, Morgan MV, Reynolds C. Fluoride and casein phosphopeptide-amorphous calcium phosphate. J Dent Res. 2008 Apr;87(4):344–348. doi: 10.1177/154405910808700420. [DOI] [PubMed] [Google Scholar]