Abstract
Cassia tora L. seeds have previously been reported to reduce blood glucose level in human and animals with diabetes. In the present study, the effects of Cassia tora L. seed butanol fraction (CATO) were studied on postprandial glucose control and insulin secretion from the pancreas of the normal and diabetic rats. Diabetes was induced by an i.p. injection of Streptozotocin (55 mg/kg BW) into the male Sprague-Dawley rats. The postprandial glucose control was monitored during a 240 min-period using a maltose loading test. In normal rats, rats fed CATO (20 mg/100 g BW/d) showed lower postprandial glucose levels in all the levels from 30 min up to 180 min than those in the control rats without CATO (p<0.05). In diabetic rats, those levels in the CATO group seemed to be lower during the 30~180 min, but only glucose level at 30 min showed significant difference compared to that in the control group. Moreover, CATO delayed the peak time of the glucose rise in both normal and diabetic rats in the glucose curves. On the other hand, when CATO was administered orally to the diabetic rats for 5 days, 12 hr fasting serum glucose level was decreased in the diabetic rats (p<0.05). Degree of a decrease in 12 hr fasting serum insulin levels was significantly less in the diabetic CATO rats as compared to diabetic control rats. On the last day of feeding, β cells of the pancreas were stimulated by 200 mg/dL glucose through a 40 min-pancreas perfusion. Amounts of the insulin secreted from the pancreas during the first phase (11~20 min) and the second phase (21~40 min) in the CATO fed diabetic rats were significantly greater than those in the diabetic control group (p<0.05). These findings indicated that constituents of Cassia tora L. seeds have beneficial effect on postprandial blood glucose control which may be partially mediated by stimulated insulin secretion from the pancreas of the diabetic rats.
Keywords: Diabetes, Cassia tora L., seeds butanol fraction, pancreas perfusion, insulin secretion
Introduction
The seeds of Cassia tora L. have been conventionally used throughout the Asian region for several centuries. Its roasted seeds have a favorable flavor, so it is used popularly as a tea in Korea. Cassia tora L. has been also prescribed in oriental herb medicine to treat night blindness, hypertension, hypercholesterolemia, and constipation (Ahn, 1998; Kim et al., 1990). It was reported that Cassia tora L. possesses various functional properties including antioxidative (Choi et al., 1994; Lim & Han, 1997; Na et al., 2004; Yen et al., 1998), hypoglycemic (Lim et al., 1995; Lim & Han, 1997), less cadmium-accumulating (Kim et al., 2002), antimutagenic (Choi et al., 1997), and anticlastogenicity (Kim et al., 1998) activities. Cassia tora L. contains many active substances, including nor-rubrofusarin, aurantio-obtusin, chrysoobtusin, obtusin, emoidin, obrusifolin, chrysophanol, physcion, and chryso-obtusin-2-Ο-β-D-glucoside (Jang et al., 2007). A study with streptozotocin-induced diabetic rats (Lim et al., 1995) reported that 10% of Cassia tora L. in diet lowered plasma glucose, and this lowering effect was as acute as seen even at the first week of feeding. They reported that a butanol fraction of the methanol extract was the one that decreased plasma glucose levels, and this decrease was shown so early even at the 4th day of feeding (Lim & Han, 1997). Recently, Jang et al. (2007) suggested that emodin and obtusifolin in Cassia tora L. might be the components having antidiabetic functions since they exhibited a significant inhibitory activity on advanced glycation end products (AGEs) formation. However, this study was performed in vitro. In order to claim an herb or agent as the therapeutics for the diabetes, the in vivo activity of lowering blood glucose should be observed. In addition to that, it would be prefer to study effects on the insulin secretion from the pancreas in type 1 diabetes mellitus. Process in the insulin synthesis and secretion is disregulated and is related with the destruction of the β cells in Langerhan's islets (Gorsuch et al., 1981; Steele et al., 2004; Weir & Bonner-weir, 2004). Clinically, insulin activities have been assessed by peripheral blood insulin and C-peptide measurements. However, those measurements may not accurately reflect amounts of insulin secreted directly from the pancreas. Over time, there are relatively little studies on insulin secretion from the pancreas in type 1 diabetes. Therefore, in the present study, type 1 diabetes was induced by destroying β cells with Streptozotocin injection and direct insulin secretion was evaluated using a pancreas perfusion.
Materials and Methods
Preparation of Cassia tora L. seeds butanol fraction
Cassia tora L. seeds (cultivated in Youngcheon, Korea) were purchased from the local oriental herbs market. The seeds were ground into the fine powder and extracted with 85% methanol (5 volumes of MeOH) in a stainless steel extraction tank for 24 hours at room temperature. This methanol mixture was filtered in the funnels and centrifuged (4℃, 3000 rpm, 20 min), which was repeated three times. All the precipitate was eliminated, and the MeOH extract portion was collected and then concentrated using a rotary evaporator. This methanol extract was subsequently partitioned with hexane (1: 1 by volume) and then with dichloromethane (1: 1 by volume) for 24 hours. The aqueous layer was further partitioned using butanol (1: 1 by volume) and separated into the aqueous layer for 24 hours. Finally, Cassia tora L. seeds butanol fraction (CATO) was collected, condensed by a rotary evaporator, and freeze-dried.
Animals and diabetes induction
Adult male Sprague-Dawley rats, weighing 330-390 g, were obtained from an animals company (Daehan Biolink Co., Ltd, Korea) and placed in the individual cage in order to acclimate to the environment for 7 days. Animals were maintained under the condition controlled with a 12 hour light-12 hour dark cycle (light in at 06:00 and light out at 18:00), temperature of 25 ± 2℃, and humidity of 50 ± 5%. The commercial rodent pellet diet and water were fed ad libitum during the experimental period. Diabetes was induced by intraperitoneal injection of Streptozotocin (55 mg/kg BW, Sigma Chemical Co., St. Louis, MO, USA) dissolved freshly in 0.01 M citrate buffer (pH 4.5). Rats showing above 300 mg/dL of 12 hours fasting serum glucose level were used for the diabetic groups. All experimental procedures were approved by Inje University Animal Care and Use Committee (IUACUC) and met all the guidelines in the Care and Use of Animals.
Blood glucose control after loading maltose orally
Control of blood glucose was evaluated by an oral maltose loading test in order to assess postprandial glycemic control. Normal (n=12) and diabetic (n=12) rats were fasted for 12 hours overnight. They were divided into two groups of CATO group and control group (CONT). Rats in the CATO group were orally administrated 2 g of maltose per kg body weight and 20 mg/ml/100 g BW of Cassia tora L. seeds butanol fraction. In the CONT group, rats were orally administrated the same dosage of maltose and water. Blood samples were collected from the tail vein at 0, 30, 60, 90, 120, 180, and 240 min after loading maltose. Serum was separated from blood by centrifuge (3000 rpm, 10 min), and serum glucose levels were determined by glucose oxidase method using a kit (Sigma Chemical Co., Saint Louis, MO, USA).
Fasting serum glucose and insulin levels
Three days after performing the maltose loading test, rats in the CATO groups were fed Cassia tora L. butanol extract (20 mg/100 g BW/d) for 5 days using a gavage. Only water was supplied for rats in the CONT group. After rats were fasted for 12 hours overnight, blood samples were collected from the tail vein at day 0 for the initial levels and day 5 for the final levels. Serums were separated and frozen at -20℃ for the glucose and insulin assays.
Insulin secretion from the pancreas
At the end of the CATO feeding (day 5), rats were anesthetized with an intraperitoneal injection of urethane (300 mg/100 g BW). Pancreas was carefully removed and perfused to determine amounts of insulin secreted directly from the pancreas. The perfusate preparation and pancreas perfusion procedure have been shown in other studies (Choi, 2000; Choi, 2005). Briefly, the components of the perfusate were as follows: 0.18% bovine serum albumin (fraction V), 4.00% of dextran, 0.110 M of CaCl2, 0.154 mM of KCl, KH2PO4, NaHCO3, NaCl, and MgSO4. The perfusate was continually oxygenated with a 95% O2-5% CO2 gas and maintained at 37℃ using a circulating water bath. Inflow rate of the perfusate was constantly maintained at 5 ml/min using a perfusion apparatus (Cole-Parmer Inst. Co., Chicago, IL, USA). During the first 0~10 min of the equilibration period, glucose was not included in the perfusate. During the 11~40 min of the perfusion period, glucose (200 mg/dL) was infused into the perfusate using a side arm-infusion pump (Harvard Apparatus, Holliston, MA, USA), thus the pancreas was stimulated by the glucose level of hyperglycemic condition. The inflow began via the heparinized celiac arterial cannula. Total outflow from the pancreas was collected via a heparinized portal vein cannula during the total 40 min period with 2~5 min time intervals, and volumes of these effluent samples were measured. The effluent samples were kept on ice until centrifuged (3000 rpm, 4℃, 20 min). The supernatants of these samples were decanted and frozen at -20℃ until insulin amounts were determined.
Glucose and insulin measurements
Glucose levels in the serum were determined by a kit (Sigma Chemical Co., Saint Louis, MO, USA). Insulin amounts in the serum and perfusion effluent samples were determined by the rat insulin radioimmunoassay kit (Linco Research, Inc. Saint Charles, MO, USA). Radioisotope detection was carried out using an auto gamma counting system (Hewlett Packard Instrument Co, Palo Alto, CA, USA). The cpms were counted from triplicated standard tubes and duplicated sample tubes, and the count of the nonspecific binding was subtracted. The bound/free triplicates for each point on the standard curve were averaged and plotted versus insulin amounts. For each sample duplicate, the bound/free was read off as insulin amounts (ng/ml) from the standard curve. Insulin secretion rates (ng/min) were calculated by using the measured perfusate effluent flow rate (ml/min).
Statistical analysis
All data were expressed as means ± SE. Student's t-test or one way ANOVA followed by Scheffé test was conducted to determine statistical significances in difference at p<0.05 among mean values of the groups.
Results
Blood glucose control after loading maltose orally
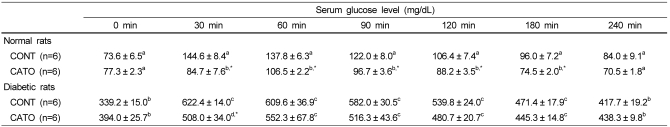
Blood glucose levels after loading maltose orally in the normal and diabetic rats were shown in Table 1. Serum glucose levels of normal control rats were 73.6 ± 6.5 mg/dL at 0 min. After 30 min, serum glucose was increased up to 144.6 ± 8.4 mg/dL, and then declined to 84.0 ± 9.1 mg/dL at the end of 240 min-period. In the normal CATO rats, serum glucose level at 0 min was 77.3 ± 2.3 mg/dL and increased up to 106.5 ± 2.2 mg/dL at 60 min, and then declined to 70.5 ± 1.8 mg/dL at 240 min. The peak time in the CATO group was 60 min, while it was 30 min in the CONT group; showing a slower uprising in the glucose curve due to CATO. These normal CATO rats showed lower serum glucose levels from 30 min up to 180 min than the CONT rats (p<0.05). In the diabetic rats, serum glucose level in the CONT group was 339.2 ± 15.0 mg/dL at 0 min, and increased up to 622.4 ± 14.0 mg/dL at 30 min, and then declined to 417.7 ± 19.2 mg/dL at 240 min. In the diabetic CATO group, serum glucose level was 394.0 ± 25.7 mg/dL at 0 min, 552.3 ± 67.8 mg/dL at 60 min, and then declined to 438.3 ± 9.8 mg/dL at 240 min. Therefore, the peak time in the CATO group was 60 min, while it was 30 min in the CONT group, showing a slower uprising in the glucose curve. The serum glucose levels at 30 min were significantly different between the diabetic CONT group and diabetic CATO group (p<0.05). Therefore, the postprandial rise of glucose was significantly reduced and delayed by CATO in diabetic rats.
Table 1.
Postprandial glucose levels in normal and diabetic rats administered Cassia tora. L. butanol fraction
Values are mean ± SE.
n: number of rats in the group
Within the same column, values with different superscripts are significantly different by ANOVA and Scheffé test at p<0.05.
*p<0.05 compared to the value of the corresponding CONT using a Student's t-test
CONT: control group of rats orally administrated maltose (0.2 g/ml/100 g BW)
CATO: group of rats orally administrated maltose (0.2 g/ml/100 g BW) and Cassia tora. L. butanol fraction (20 mg/ml/100 g BW)
Body weights, fasting serum glucose, and fasting serum insulin levels
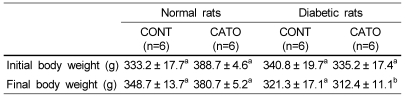
Initial body weights were similar in normal and diabetic rats as shown in Table 2. There was no significant difference in the final body weight between the CONT and CATO groups in normal rats. The final body weight in the diabetic CATO group was low significantly among all the groups by ANOVA and Scheffé test, but this value did not differ significantly compared to the value of the diabetic CONT group by a Student's t-test.
Table 2.
Body weights in normal and diabetic rats administered Cassia tora L. butanol fraction for 5 days
Values are mean ± SE.
n: number of rats in the group
Within the same row, values with different superscripts are significantly different by ANOVA and Scheffé test at p<0.05.
CONT: Rats were fed on pellet diet and water for 5 days.
CATO: Rats were fed on pellet diet and administered Cassia tora. L. butanol fraction (20 mg/100 g BW/d) for 5 days.
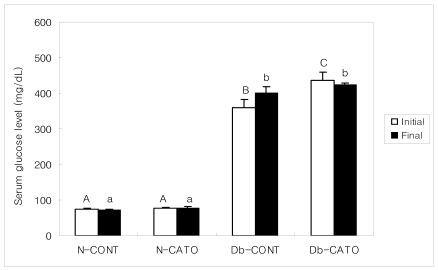
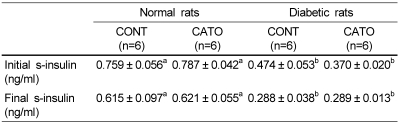
Fasting serum glucose levels were shown in Fig. 1. In normal rats, the initial and final fasting serum glucose levels were similar between CONT and CATO groups. In diabetic rats, the initial fasting serum glucose levels were different between CONT and CATO groups (358.17 ± 24.62 mg/dL and 434.80 ± 23.69 mg/dL, respectively). The final serum glucose level was 399.17 ± 18.83 mg/dL in diabetic CONT group, and 422.20 ± 7.12 mg/dL in diabetic CATO group. Therefore, serum glucose levels were increased in diabetic CONT group after 5 days of feeding, while those levels were decreased in diabetic CATO group. Fasting serum insulin levels were shown in Table 3. Initial and final serum insulin levels were similar in the CONT and CATO groups in normal rats. In the diabetic rats, the initial serum insulin levels did not differ significantly between the diabetic CONT and diabetic CATO groups (0.474 ± 0.053 ng/ml and 0.370 ± 0.020 ng/ml, respectively). The final serum insulin levels were also similar between the CONT (0.288 ± 0.038 ng/ml) and CATO groups (0.289 ± 0.013 ng/ml). However, change in the fasting serum insulin levels during the 5 day feeding period was -0.186 ± 0.046 ng/ml in the CONT group, which was a 39% decrease compared to the initial level. In the diabetic CATO group, change in the fasting serum insulin levels was -0.083 ± 0.02 ng/ml (p<0.05) during the same feeding period, which was a 22% decrease from the initial level. These data demonstrated that CATO may affect to reduce less in serum insulin in the diabetic rats.
Fig. 1.
Fasting serum glucose levels in normal and diabetic rats administered Cassia tora L. butanol fraction for 5 days. Values are mean ± SE. Number of rats is 6 per each group. Bars with different letters are significantly different by ANOVA and Scheffé test at p<0.05. CONT: Rats were fed on pellet diet and water for 5 days. CATO: Rats were fed on pellet diet and administered Cassia tora. L. butanol fraction (20 mg/100 g BW/d) for 5 days.
Table 3.
Fasting serum insulin levels in normal and diabetic rats administered Cassia tora L. butanol fraction for 5 days
Values are mean ± SE.
n: number of rats in the group
Within the same row, values with different superscripts are significantly different by ANOVA and Scheffé test at p<0.05.
CONT: Rats were fed on pellet diet and water for 5 days.
CATO: Rats were fed on pellet diet and administered Cassia tora. L. butanol fraction (20 mg/100 g BW/d) for 5 days.
Insulin secretion amounts from the pancreas
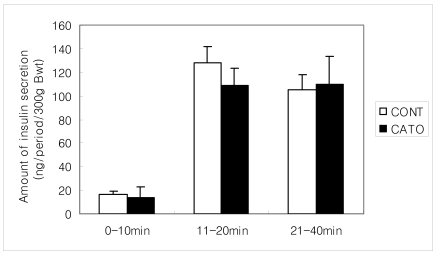
The amounts of insulin secretion during the 40 min of perfusion period were shown in Fig. 2 and Fig. 3. In normal rats, the amounts of insulin secretion during the first 10 min of the equilibration period were comparable between the CONT and CATO groups. During the next 11~20 min of the first secretory phase and the following 21~40 min of the second secretory phase, significant differences in insulin amounts were not seen between the CONT and CATO groups. Therefore, CATO may not influence the insulin secretion from the pancreas of normal rats.
Fig. 2.
Insulin amounts secreted from the pancreas of the normal rats administered Cassia tora L. butanol fraction for 5 days. Values are mean ± SE. Number of rats is 6 per each group. There were no significant differences between the CONT and CATO by Student's t-test. 0-10 min: perfusion period of no glucose stimulation. 11-20 and 21-40 min: perfusion period of 200 mg/dL glucose stimulation. CONT: Rats were fed on pellet diet and water for 5 days. CATO: Rats were fed on pellet diet and administered Cassia tora. L. butanol fraction (20 mg/100 g BW/d)) for 5 days.
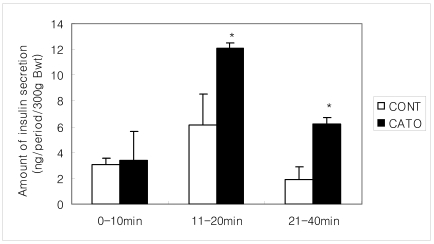
Fig. 3.
Insulin amounts secreted from the pancreas of the diabetic rats administered Cassia tora L. butanol extract for 5 days. Values are mean ± SE. Number of rats is 6 per each group. Bars with an asterisk are significantly different compared to the value of CONT by Student's t-test at p<0.05. 0-10 min: perfusion period of no glucose stimulation. 11-20 and 21-40 min: perfusion period of 200 mg/dL glucose stimulation. CONT: Rats were fed on pellet diet and water for 5 days. CATO: Rats were fed on pellet diet and administered Cassia tora. L. butanol fraction (20 mg/100 g BW/d) for 5 days.
However, the insulin secretion was quite different in the groups of diabetic rats. The amounts of insulin secretion during the first 10 min were similar as 3.07 ± 0.53 ng/300 g body weight in the CONT and 3.37 ± 2.24 ng/300 g body weight in the CATO group. During the next 11~20 min of the first phase, the amount of insulin was 6.17 ± 2.34 ng/300 g body weight in the CONT group and 12.11 ± 0.44 ng/300 g body weight in the CATO group (p<0.05). The pancreas in the CATO group secreted insulin about two times greater than that in the CONT group during this early perfusion period. During the period of 21~40 min, the amount of insulin secretion was 1.94 ± 0.97 ng/300 g body weight in the CONT group and 6.18 ± 0.50 ng/300 g body weight in the CATO group (p<0.05). Therefore, the pancreas in the CATO group secreted insulin about more than three times greater than that in the CONT group during this second secretory phase. These data showed that CATO significantly stimulated the insulin secretion from the pancreas in the diabetic rats, although the absolute amount was still in the lower range when compared to those in the non-diabetic normal rats.
Discussion
Primary therapeutic purpose for treating type 1 diabetes is to reduce blood glucose levels. Various hypoglycemic medications have been prescribed in the hospitals and clinics; α-glycosidase inhibitor such as acarbose and miglitol, or insulin secretagogue such as sulfonylurea. Other medications are metformin and thiazolidinedione, which promote insulin sensitivity and reduce hepatic glucose output. However, these hypoglycemic medications may have some side effects. In the case of type 1 diabetes, patients who have been treated with insulin therapy for the extended period complained about pain, bruise, and even insulin allergy such as urticaria, angioedema, pruritus, rash, and dyspnea (Lee, 2008). Therefore, natural medicinal foods that may have antidiabetic functions but do not have harmful side effects have been focused and searched in Korea (Park & Wang, 2008). One survey study reported that 70.8% of type 2 diabetes patients had consumed functional foods, and the most frequent ingested food item was silkworm, followed by ginseng, black bean, and pine tree leaves in order (Kim et al., 2000). Recently, kinds of polysaccharides from the edible plants have been reported as antidiabetic agents (Kim et al., 2008; Park et al., 2007). Lim et al. (1995) reported that Cassia tora seeds feeding for one week reduced blood glucose in the streptozotocin-induced diabetic rats, and they suggested that Cassia tora butanol fraction might be the potent fraction among other fractions of the methanol extracts (Lim & Han, 1997).
In the present study, positive effect of CATO on blood glucose control after loading maltose orally was clearly seen in the normal rats. Postprandial serum glucose increment was 96.5% from the baseline of the glucose level at 0 min in the normal CONT group. However, it was only 9.5% in the normal CATO group. Besides, CATO slowed a rise of glucose until 60 min, while a sharp rise was seen at the 30 min in the normal CONT group (Table 1). In the diabetic rats, serum glucose increment was 83.4% from the baseline of the glucose level at 0 min in the CONT group. However, it was 28.9% increment in the diabetic CATO group (Table 1). Delaying peak time in the blood glucose curve seems to appear in the diabetic rats. Therefore, CATO seems to be beneficial to control the postprandial blood glucose.
Changes in body weight were not seen in the normal rats (Table 2). However, in the diabetic rats, 5.7% of the body weight was reduced in the CONT group and 6.8% in the CATO group. In general, body weight loss is a common symptom in the diabetic rats (Kim et al., 2008; Lim & Han, 1997). Fasting serum glucose levels in the diabetic rats were increased in the CONT group after 5 days of feeding and the degree of increase in glucose was less in the CATO group (Fig. 1). In the diabetic rats, change in fasting serum insulin was -39.2% in the CONT group while it was -21.9% in the CATO group (p<0.05). Therefore, the effect of CATO on lessening the blood glucose rise was seen even with a short feeding period of 5 days, and might be related with a degree of decrease in the fasting serum insulin levels.
We examined the effects of CATO on the direct insulin secretion from the pancreas in normal and diabetic rats. There was no significant difference in insulin amounts during the 0~10 min, 11~20 min, and 21~40 min of perfusion periods between the CATO group and CONT group in normal rats (Fig. 2). However, in the diabetic rats, CATO increased insulin secretion during the 11~20 min and 21~40 min periods (Fig. 3). Insulin amounts during the first 0~10 min were not different between the diabetic CATO and diabetic CONT groups. This first 10 min was a period of perfusion without glucose stimulation, and insulin secretion in this period was from the stored pool in the secretory vesicles of the β cells (Curry & Maclachlan, 1987). The next 11~40 min was a period of perfusion with glucose stimulation. The stimulation-secretion coupling process in the pancreatic β-cells is affected by glucose (Curry, 1986; Rossetti et al., 1990; Yki-Jarvenen, 1992) as well as amino acids (Strandgaard & Curry, 1998), manganase (Baly et al., 1984), magnesium (Curry et al., 1977), calcium (Choi, 1997), fatty acid (Brockman, 1982; Nolan et al., 2006), cinnamic acid (Adsakwattana et al., 2008; Yibchok-anun et al., 2008), and oleanolic acid (Hsu et al., 2006). Therefore, the biochemical environment of the pancreas may modulate the insulin secretion from the pancreas (Pørksen et al., 2002). In addition to that, the nervous system is involved in the regulation of insulin secretion from the pancreas (Ahren et al., 1987; Ahren & Taborsky, 1986; Choi, 2000; Curry, 1983; Curry, 1984; Lee et al., 1993; Lee et al., 1989). Therefore, the neural inputs could be important in regulation of the insulin secretion from the pancreas. Other factors influencing the insulin secretion could be hormones (Ahren et al., 1986; Ahren et al., 1987; Curry et al., 1982). The method used in this study was able to determine the direct effect of glucose on the insulin release from the pancreas without any above primary and secondary metabolic, neural, and hormonal influences on the secretory process, since our perfusion method allows the anatomical isolation. In our study, the amount of insulin secreted from the pancreas during the first secretory phase was greater as 1.96 times in the CATO group compared with that in the CONT group (p<0.05). Moreover, the amount of insulin secreted from the pancreas during the second secretory phase was also greater as 3.19 times in the CATO group compared with that in the CONT group (p<0.05). Even though absolute amount of insulin in the diabetic CATO group is not sufficient to cure diabetes, these data suggest that intakes of CATO might improve pancreatic β cells response to the high levels of glucose challenge. Our study could not directly determine how CATO affects the insulin secretion activity in the β cells of the pancreas. Recently, it was reported that β cell failure shown in diabetes could be restored by more expression of insulin receptor substrate-2 (Irs2) since Irs2 mediates replication and survival of the β cells (Hennige et al., 2003; Park et al., 2006). Other possible explanation is that CATO might protect some pancreatic β-cells from further deterioration or even enhancement of the remaining β cell function. While this short-term study has implications in terms of reducing postprandial blood glucose levels and increasing insulin secretion, studies on the long-term effects of CATO may be worthy to perform in the future.
In conclusions, our results show that butanol fraction from the Cassia tora L. seeds has a beneficial effect for the postprandial blood control, thus Cassia tora L. seeds can be used as a diet supplement with a meal. Further studies with pancreatic β-cells are needed to clarify its effects and the mechanism involved.
Footnotes
This work was supported by the Inje Research and Scholarship Foundation in 2005-2007, Brain Korea 21 and FIRST in 2007.
References
- 1.Adisakwattana S, Moonsan P, Yibchok-anun S. Insulin-releasing properties of a series of cinnamic acid derivatives in vitro and in vivo. J Agric Food Chem. 2008;56:7838–7844. doi: 10.1021/jf801208t. [DOI] [PubMed] [Google Scholar]
- 2.Ahn DK. Illustrated book of Korean medicinal herbs. Seoul, Republic of Korea: Kyo-Hak Publishing Co., Ltd; 1998. p. 636. [Google Scholar]
- 3.Ahren B, Taborsky GJ., Jr The mechanism of vagal nerve stimulation of glucagon and insulin secretion in the dog. Endocrinology. 1986;118:1551–1556. doi: 10.1210/endo-118-4-1551. [DOI] [PubMed] [Google Scholar]
- 4.Ahren B, Veith RC, Taborshy GJ., Jr Sympathetic nerve stimulation versus pancreatic norepinephrine infusion in the dog: effects on basal release of insulin and glucagon. Endocrinology. 1987;121:323–331. doi: 10.1210/endo-121-1-323. [DOI] [PubMed] [Google Scholar]
- 5.Baly DL, Curry DL, Keen CL, Hurley LS. Effect of manganese deficiency on insulin secretion and carbohydrate homeostasis in rats. J Nutr. 1984;114:1438–1446. doi: 10.1093/jn/114.8.1438. [DOI] [PubMed] [Google Scholar]
- 6.Brockman RP. Insulin and glucagon responses in plasma to intraportal infusions of propionate and butyrate in sheep (Ovia aries) Comp Biochem Physiol. 1982;73:237–238. doi: 10.1016/0300-9629(82)90062-7. [DOI] [PubMed] [Google Scholar]
- 7.Choi HJ. Calcium modulation of insulin secretion in perfused pancreata of obese Zucker rats. J Food Sci Nutr. 1997;2:144–148. [Google Scholar]
- 8.Choi JS, Lee HJ, Ha JO, Park KY, Kang SS. In vitro antimutagenic effects of anthraquinone alycones and naphthopyrone glycodises from Cassia tora. Planta Med. 1997;63:11–14. doi: 10.1055/s-2006-957593. [DOI] [PubMed] [Google Scholar]
- 9.Choi JS, Lee HJ, Lang SS. Alaternin, cassiaside and rubrofusarin-gentibiodise, radical scavenging principles from the seeds of Cassia tora on 1,1-diphenyl-2-picryhydrazyl (DPPH) radical. Arch Pharm Res. 1994;17:462–466. doi: 10.1007/BF02979126. [DOI] [PubMed] [Google Scholar]
- 10.Choi HJ. Effects of cephalic glucopenia on insulin and glucagons secretion in central nervous system-intact pancreas perfused rats. Korean Journal of Biomedical Laboratory. 2000;6:229–235. [Google Scholar]
- 11.Curry DL. Direct tonic inhibition of insulin secretion by central nervous system. Am J Physiol. 1983;244:E425–E429. doi: 10.1152/ajpendo.1983.244.4.E425. [DOI] [PubMed] [Google Scholar]
- 12.Curry DL. Reflex inhibition of insulin secretion: vagus nerve involvement via CNS. Am J Phsiol. 1984;247:E827–E832. doi: 10.1152/ajpendo.1984.247.6.E827. [DOI] [PubMed] [Google Scholar]
- 13.Curry DL. Insulin content and insulinogenesis by the perfused rat pancreas: effects of long term glucose stimulation. Endocrinology. 1986;118:170–175. doi: 10.1210/endo-118-1-170. [DOI] [PubMed] [Google Scholar]
- 14.Curry DL, Joy RM, Bennett LL. Magnesium modulation of glucose-induced insulin secretion by the perfused rat pancreas. Endocrinology. 1977;101:203–208. doi: 10.1210/endo-101-1-203. [DOI] [PubMed] [Google Scholar]
- 15.Curry DL, Maclachlan SA. Synthesis-secretion coupling of insulin: effect of aging. Endocrinology. 1987;121:241–247. doi: 10.1210/endo-121-1-241. [DOI] [PubMed] [Google Scholar]
- 16.Curry DL, Morris JG, Rogers QR. Dynamics of insulin and glucagon secretion by the isolated perfused cat pancreas. Comp Biochem Physiol. 1982;72:333–338. doi: 10.1016/0300-9629(82)90228-6. [DOI] [PubMed] [Google Scholar]
- 17.Gorsuch AN, Spencer KM, Lister JM, McNally JM, Dean BM, Bottazzo GF, Cudworth AG. Evidence for a long prediabetic period in type I (insulin dependent) diabetes mellitus. Lancet. 1981;2:1363–1365. doi: 10.1016/s0140-6736(81)92795-1. [DOI] [PubMed] [Google Scholar]
- 18.Hennige AM, Burks DJ, Ozcan U, Kulkarni RN, Ye J, Park S, Schubert M, Fisher TL, Dow MA, Leshan R, Zakaria M, Mossa-Basha M, White MF. Upregulation of insulin receptor substrate-2 in pancreatic β cells prevents diabetes. J Clin Invest. 2003;112:1521–1532. doi: 10.1172/JCI18581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hsu JH, Wu YC, Liu IM, Cheng JT. Release of acetylcholine to raise insulin secretion in Wistar rats by oleanolic acid, one of the active principles contained in Cornus offcinalis. Neurosci Lett. 2006;404:112–116. doi: 10.1016/j.neulet.2006.05.025. [DOI] [PubMed] [Google Scholar]
- 20.Jang DS, Lee GY, Kim YS, Lee YM, Kim CS, Yoo JL, Kim JS. Anthraquinones from the seeds of Cassia tora with inhibitory activity on protein glycation and aldose reductase. Biol Pharm Bull. 2007;30:2207–2210. doi: 10.1248/bpb.30.2207. [DOI] [PubMed] [Google Scholar]
- 21.Kim JM, Kim HT, Hwang SM. Instant tea preparation from Cassia tora Seeds. Korean Journal of Food Science and Technology. 1990;22:241–247. [Google Scholar]
- 22.Kim SH, Choi JS, Moon YH. Antioxidative activity and anticlastogenicity of Cassia tora L. seeds extract and its major component, nor-rubrofusarin-6-β-D-glucoside. Journal of Food Hygiene and Safety. 1998;13:394–399. [Google Scholar]
- 23.Kim SH, Ryu DS, Lee MY, Kim KH, Kim YH, Lee DS. Anti-diabetic activity of polysaccharide from Salicornia herbacea. Korean Journal of Microbiology and Biotechnology. 2008;36:43–48. [Google Scholar]
- 24.Kim SJ, Baek SH, Heo JW, Kim US, Lee JD, Kang GW, Park SH, Han JH, Jeong SY, Lee SH. Effect of Cassia tora L. powder aged-diets on the accumulation of cadmium in rat. Journal of East Asian Society of Dietary Life. 2002;12:554–565. [Google Scholar]
- 25.Kim YS, Chun JH, Park JH, Kang CI. Status and associating factors of complementary and alternative medicine among Korean diabetic patients. The Journal of Korean Diabetes Association. 2000;24:7–89. [Google Scholar]
- 26.Lee HC, Curry DL, Stern JS. Direct effect of CNS on insulin hypersecretion in obese Zucker rats: involvement of vagus nerve. Am J Physiol. 1989;256:E439–E444. doi: 10.1152/ajpendo.1989.256.3.E439. [DOI] [PubMed] [Google Scholar]
- 27.Lee HC, Curry DL, Stern JS. Tonic sympathetic nervous system inhibition of insulin is diminished in obese Zucker rats. Obes Res. 1993;1:371–376. doi: 10.1002/j.1550-8528.1993.tb00015.x. [DOI] [PubMed] [Google Scholar]
- 28.Lee JR. Inquiry into the insulin injection. Korean Clinical Diabetes. 2008;9:117–122. [Google Scholar]
- 29.Lim SJ, Han HK. Hypoglycemic effect of fractions of Cassia tora extract in Streptozotocin-induced diabetic Rats. Journal of the Korean Society of Food Science and Nutrition. 1997;13:23–29. [Google Scholar]
- 30.Lim SJ, Kim SY, Lee JW. The effects of Korean wild vegetables on blood glucose levels and liver muscle metabolism of streptozotocin-induced diabetic rats. The Korean Journal of Nutrition. 1995;28:585–594. [Google Scholar]
- 31.Na GM, Han HS, Ye SH, Kim HK. Extraction characteristics and antioxidative activity of Cassia tora L. extracts. Korean Journal of Food Culture. 2004;19:499–505. [Google Scholar]
- 32.Nolan CJ, Madiraju MSR, Delghingaro-Augusto V, Peyot M, Prentki M. Fatty Acid Signaling in the β-cell and Insulin Secretion. Diabetes. 2006;55:S16–S23. doi: 10.2337/db06-s003. [DOI] [PubMed] [Google Scholar]
- 33.Park KJ, Oh YJ, Lee SY, Kim HS, Ha HC. Anti-diabetic effect of crude polysaccharides from Grifola frondosa in KK-Ay diabetic mouse and 3T3-L1 adipocyte. Korean Journal of Food Science and Technology. 2007;39:330–335. [Google Scholar]
- 34.Park S, Dong X, Fisher TL, Dunn S, Omer AK, Weir G, White MF. Exendin-4 Uses Irs2 Signaling to Mediate Pancreatic β-Cell Growth and Function. J Biol Chem. 2006;281:1159–1168. doi: 10.1074/jbc.M508307200. [DOI] [PubMed] [Google Scholar]
- 35.Park SH, Wang SG. A research on anti-diabetic functional food intake of the subjects with type 2 diabetic mellitus in Daejeon. Korean Journal of Human Ecology. 2008;17:797–805. [Google Scholar]
- 36.Pørksen N, Hollingdal M, Juhl C, Butler P, Veldhuis JD, Schmitz O. Pulsatile insulin secretion: detection, regulation, and role in diabetes. Diabetes. 2002;51:S245–S254. doi: 10.2337/diabetes.51.2007.s245. [DOI] [PubMed] [Google Scholar]
- 37.Rossetti L, Giaccari A, DeFronzo RA. Glucose toxicity. Diabetes Care. 1990;13:610–630. doi: 10.2337/diacare.13.6.610. [DOI] [PubMed] [Google Scholar]
- 38.Steele C, Hagopian WA, Gitelman S, Masharani U, Cavaghan M, Rother KI, Donaldson D, Harlan DM, Bluestone J, Herold KC. Insulin secretion in type 1 diabetes. Diabetes. 2004;53:426–433. doi: 10.2337/diabetes.53.2.426. [DOI] [PubMed] [Google Scholar]
- 39.Strandgaard C, Curry DL. Differential insulin secretory responses to cationic and branched-chain amino acids. Pancreas. 1998;17:65–71. doi: 10.1097/00006676-199807000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Weir GC, Bonner-Weir S. Five Stages of Evolving β-Cell Dysfunction During Progression to Diabetes. Diabetes. 2004;53:S16–S21. doi: 10.2337/diabetes.53.suppl_3.s16. [DOI] [PubMed] [Google Scholar]
- 41.Yen GC, Chen HW, Duh PD. Extraction and identification of an antioxidative component from Jue Ming Zi (Cassia tora L.) J Agric Food Chem. 1998;46:820–824. [Google Scholar]
- 42.Yibchok-anun S, Adisakwattana A, Moonsan P, Hsu WH. Insulin - secretagogue activity of p-Methoxycinnamic acid in rats, perfused rat pancreas and pancreatic β-Cell line. Basic Clin Pharmacol Toxicol. 2008;102:476–482. doi: 10.1111/j.1742-7843.2008.00218.x. [DOI] [PubMed] [Google Scholar]
- 43.Yki-Jarvinen H. Glucose toxicity. Endocr Rev. 1992;13:415–431. doi: 10.1210/edrv-13-3-415. [DOI] [PubMed] [Google Scholar]