Abstract
Background
Data on the association between air pollution and cerebrovascular disease in the US are limited. The objective of this study was to investigate the association between short-term exposure to ambient air pollution and risk of ischemic cerebrovascular events in a US community.
Methods
Daily counts of ischemic strokes/TIAs (2001–2005) were obtained from the population-based Brain Attack Surveillance in Corpus Christi (BASIC) Project. Daily particulate matter <2.5μm in diameter (PM2.5), ozone (O3), and meteorological data were obtained from Texas Commission on Environmental Quality. To examine the association between PM2.5 and stroke/TIA risk, Poisson regression was used. Separate models included same day PM2.5, PM2.5 lagged 1–5 days, and an averaged lag effect. All models were adjusted for temperature, day of week and temporal trends in stroke/TIA. The effects of O3 were also investigated.
Results
Median PM2.5 was 7.0 μg/m3 (Inter Quartile Range (IQR): 4.8–10.0). There were borderline significant associations between same day (RR=1.03, 95% CI:0.99–1.07 for an IQR increase in PM2.5) and previous day (RR=1.03, 95% CI:1.00–1.07) PM2.5 and stroke/TIA risk. These associations were independent of O3, which demonstrated similar associations with stroke/TIA risk (same day RR=1.02, 95% CI: 0.97–1.08 and previous day RR=1.04, 95% CI: 0.99–1.09) in two pollutant models.
Inference
We observed associations between recent PM2.5 and O3 exposure and ischemic stroke/TIA risk even in this community with relatively low pollutant levels. This study provides data on environmental exposures and stroke risk in the US and suggests future research on ambient air pollution and stroke is warranted.
Background
Air pollution is linked to cardiovascular disease in general,1–6 and cardiac disease specifically.1, 7–13 Data on the association between air pollution and stroke are more limited, although the underlying biologic mechanisms linking air pollution to ischemic heart disease and cerebrovascular disease may be similar. Most of the evidence linking air pollution and stroke is from time series analyses relating daily air pollution levels to daily counts of stroke deaths obtained from vital statistics or similar data sources.2, 14–20 Studies have been conducted outside of the United States (US)14–17, 19, 20, with most demonstrating positive associations with one or more air pollutants. An association between air pollution and stroke mortality has also been noted in certain areas of the US.4
To date, research on air pollution and incident stroke has primarily relied on routinely collected data sources, such as discharge diagnoses, to identify strokes.19, 21–25 In the United Kingdom, Canada and China, stroke admissions have been shown to be associated with higher levels of air pollution.19, 22, 24, 25 US studies of Medicare claims data and other billing data have also demonstrated associations between air pollution levels and hospital admissions for total cerebrovascular disease and ischemic stroke specifically.21, 23, 26 A recent analysis from the Dijon Stroke Register in France found an association between air pollution levels and ischemic stroke risk using population-based data.27 Data considering the relationship between air pollution and incident stroke risk from population-based stroke studies in the US are not available.
While several air pollutants have been studied for their links to stroke and stroke mortality, including carbon monoxide, sulfur dioxide, nitrogen dioxide and ozone, fine particulate matter (PM2.5) has emerged as a pollutant of interest. PM2.5 is composed of particles measuring <2.5μm in aerodynamic diameter in contrast to PM10 which is composed of larger particles measuring <10μm, the majority of which are <2.5μm. PM2.5, because of its smaller size and chemical activity, can penetrate the small airways and alveoli of the lung and enter the blood circulation.28 Exact biologic mechanisms by which recent PM2.5 exposure may increase risk of acute cerebrovascular events are not known but possible mechanisms include acute arterial vasoconstriction,29 acute increases in blood pressure30 and acute increases in plasma viscosity.31
Ambient PM2.5 is a complex mixture and is comprised not only of primary emissions from stationary and distributed sources, but also of secondary aerosol formed via atmospheric transformation. The production of fuels from crude oil is an example of a combustion process yielding primary emissions of fine particulate matter. Areas with a large petroleum and petrochemical industry presence provide an opportunity to study the health effects of PM2.5. Southeast Texas is home to several large oil refineries. The objective of this study was to investigate the association between short-term exposure to ambient PM2.5 and risk of ischemic cerebrovascular events in a southeast Texas community with a heavy fossil fuel industry presence using data from a population-based stroke surveillance study to capture stroke events.
Methods
Ischemic Stroke and Transient Ischemic Attack Case Identification
Ischemic strokes and transient ischemic attacks (TIAs) were identified from the Brain Attack Surveillance in Corpus Christi Project (BASIC). BASIC is a population-based stroke surveillance project designed to capture all strokes in Nueces County, Texas, a geographically isolated, urban, bi-ethnic community in southeast Texas. Nueces County has a population of roughly 310,000 and is over half Mexican American. Nueces County serves as the regional referral medical center for southeast Texas and is approximately 150 miles from Houston and San Antonio. BASIC methodology has been described in detail elsewhere.32 Briefly, between January 1, 2001 and December 31, 2005, trained abstractors, using validated screening procedures, identified ischemic stroke and TIA cases through active and passive surveillance of emergency room logs, hospital admissions records, and discharge diagnosis codes. Using published criteria,33 study neurologists blinded to age and ethnicity validated cases as ischemic stroke or TIA using source documentation. TIAs were included due to the similar underlying pathophysiology of TIAs and ischemic strokes; intracerebral hemorrhage cases were excluded as the pathophysiology differs from ischemic events. Individuals under age 45, non-Nueces County residents, and those with traumatic strokes were excluded. The BASIC project was approved by the University of Michigan Institutional Review Board and each of the Nueces County hospitals.
Air Pollutant/Meteorological Data
Nueces County, Texas is located on the gulf coast and is home to a large petroleum and petrochemical industry. Several refineries and chemical plants are located within close proximity to the 1,500 oil wells located in this region. Nineteen facilities in Nueces County were involved in the production/manufacturing of chemicals/petrochemicals in the years 1997–2002, as identified by the following Standard Industrial Classification (SIC) industry codes: 1311 Operation of oil and gas field properties (4), 1321 Production of liquid hydrocarbons from oil and gas fields (3), 2819 Manufacturing industrial inorganic chemicals (1), 2869 Manufacturing industrial organic chemicals (3), 2911 Production of gasoline, kerosene, distillate fuel oils, residual fuel oils, and lubricants (7) and 9711 Armed forces establishment (1).34 There were 20 additional air pollutant emission point sources identified in the county. These facilities belonged to various industries including hardwood/plywood (1), paint (1), warehousing and storage (1), marine cargo handling (4), electrical (5) and natural gas services (3), refuse (1), chemicals (1), and petroleum stations (3).
Historical air pollutant and meteorological data for years 2001–2005 were obtained from the Texas Commission on Environmental Quality’s Monitoring Operations Texas Historical Environmental Records (MOTHER) database.35 Six air quality monitors are located within the city of Corpus Christi, Texas. Data on PM2.5 were available from one monitor, Corpus Christi West C4, which is geographically-centered within the urban population. PM2.5 was measured in micrograms per cubic meter (μg/m3) and summarized as the hourly average per 24-hour time period. Of the 1,826 days in the study period, there were missing PM2.5 values for 12 days (0.7%). One day with unusually high average (64.4 μg/m3) and peak PM2.5 (771.3 μg/m3) measurements was excluded. Data on ozone (O3) was obtained from the same monitor. O3 was measured in parts per billion (ppb) and summarized as the hourly average per 24-hour time period. Ozone data was missing for 3 days. Ambient temperature was measured in degrees Celsius and summarized as the average peak hourly temperature per 24-hour time period. There were 35 days for which temperature data were not available (1.9%). Wind direction and wind speed (meters/second) were also obtained, and wind rose analyses were conducted using WRPLOT View version 5.3.0.
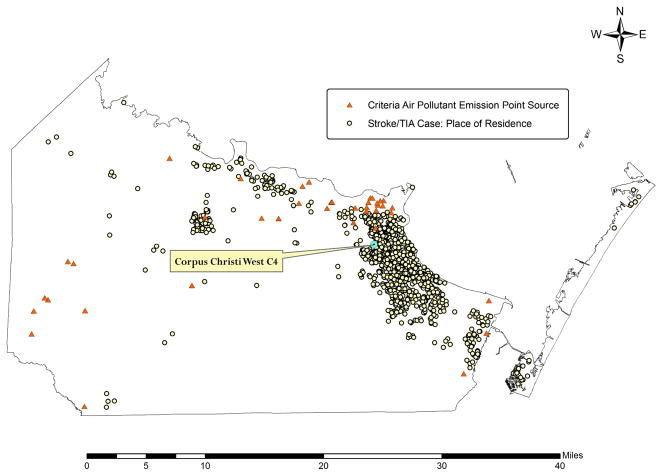
The 39 air pollutant point emission sources were geocoded into GIS using their latitude/longitude coordinate data. Figure 1 shows the criteria air pollutant point sources and the air quality monitor in relation to place of residence of stroke/TIA cases. Analysis of the frequency of occurrence of winds in each of the specified wind direction sectors and wind speed classes for the Corpus Christi West C4 monitor for 2001–2005 demonstrated that the predominant winds were from the southeast. As seen in Figure 1, this predominant wind flow placed the monitor, and the majority of stroke/TIA cases, upwind of the local industrial facilities.
Figure 1.
Air pollutant point emission sources in Nueces County, Texas.
Statistical Methods
Stroke/TIA counts, air pollution, and temperature data were examined individually with descriptive statistics and time series plots. To examine the association between PM2.5 and stroke/TIA risk, Poisson regression models were used. A semiparametric model was fit with daily stroke/TIA counts as the dependent variable. Parametric effects included same day (midnight to midnight on day of stroke/TIA) PM2.5 modeled as a continuous covariate and day of the week modeled as indicator variables with Sunday as the referent. Time in days was modeled using a natural cubic spline with three degrees of freedom to account for temporal trends in stroke/TIA events over the study period; we opted for a small number of degrees of freedom because strong seasonal trends in the number of events were not found. Same day average peak hourly temperature was modeled using a natural cubic spline with three degrees of freedom to account for the potential confounding effects of temperature. In additional models, PM2.5 was separately modeled as lagged variables up to 5 days prior to the date of stroke/TIA as the effects of PM2.5 on stroke/TIA may be delayed. For example, the lag 1 model represented PM2.5 levels for the 24 hours preceding the day of the stroke/TIA. Finally, an unconstrained distributed lag Poisson regression model was used to estimate the marginal effect on stroke/TIA risk associated with a unit increase in a 5-day weighted average of PM2.5.36 This marginal effect was calculated by averaging coefficients of PM2.5 lags 0–5 after simultaneously including them in a single regression model. An advantage to the unconstrained distributed lag model is that it makes no assumptions about the functional form of the lag structure in estimating the marginal association of a unit increase in the weighted average of pollution and stroke rates.
Additionally, we explored the potential confounding effects of O3 on the PM2.5 and stroke/TIA association given O3 has been linked to stroke.27 This was done by first considering the independent association between O3 and stroke/TIA in single pollutant models. O3 was then added to the PM2.5 models (two pollutant models) to determine the degree to which O3 confounded the PM2.5 and stroke/TIA association. Finally, we considered possible effect modification between season and PM2.5 on stroke/TIA risk given evidence that air pollution and temperature may have synergistic effects on health outcomes.17, 22, 37 Based on visual inspection of temperature data over the study time period, season was defined as summer (June through September) versus non-summer (all other months). Effect modification was assessed by including an interaction term for PM2.5 and season in the single pollutant PM2.5 models. To limit the number of models considered, investigation of confounding and effect modification was limited to models of same day and previous day PM2.5. All models were adjusted for day of the week, temperature, and temporal trends as described above.
The Poisson regression models were estimated without the use of an offset term, reflecting the assumption that the population at risk was relatively constant over the study period. To test this assumption, we conducted a sensitivity analysis using yearly inter-Census population estimates as the offset term. The offset term was the estimated (log-transformed) population 45 and older for Nueces County for a given year. The effects of PM2.5 were summarized as relative risk (RR) or percent change for an interquartile range (IQR) increase in PM2.5 levels, and robust standard errors were used to compute confidence intervals for the effect estimates.38 All models were run in S-plus 7.0 for Windows, using the glm() function with stringent convergence criteria (data analyzed by LDL, BNS and DLB).
Results
There were 3,508 stroke/TIAs (2,350 ischemic strokes (67.0%) and 1,158 TIAs (33.0%)) during the study time period. Median age of the stroke/TIA cases was 72 years (IQR: 62–81). Fifty-four percent of the cases were female (n=1,887). Fifty percent were Mexican American, 44% non-Hispanic white, 5% African American and 1% were other or undetermined race-ethnicity. Median number of stroke/TIAs per day was 2 (IQR: 1–3). For 287 (15.7%) of the 1,826 days, there were no stroke/TIAs.
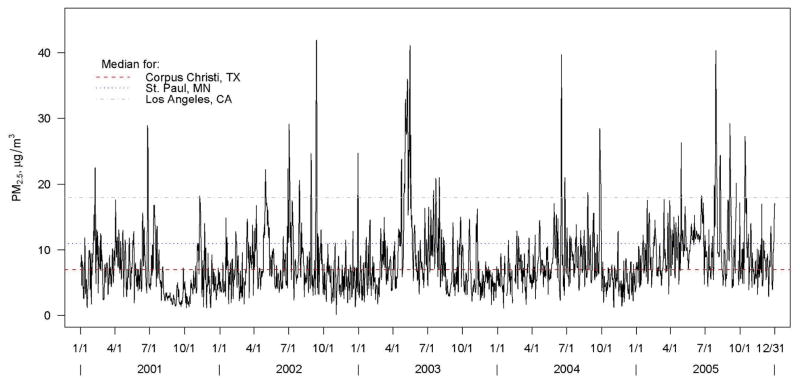
Median PM2.5 during the study time period was 7.0μg/m3 (IQR: 4.8–10.0), which is well below the USEPA National Ambient Air Quality Standard (NAAQS) of 15 μg/m3 for annual PM2.5. Figure 2 displays daily levels and median level of PM2.5 over the study time period with median levels for two other US cities included for reference.39 Median temperature during the study time period was 27.1°C (IQR: 22.4–30.9).
Figure 2.
Daily and median level of PM2.5 over the study time period (2001–2005) with median PM2.5 levels for two referent US cities.
Figure 3 displays percent change in stroke/TIA risk associated with an IQR (5.1 μg/m3) increase in PM2.5. There were borderline significant associations between same day (RR=1.03, 95% CI: 0.99–1.07 for an IQR increase in PM2.5) and previous day (RR=1.03, 95% CI: 1.00–1.07) PM2.5 exposure and stroke/TIA risk. PM2.5, modeled as lagged variables 2–5 days prior to the stroke/TIA, was not significant. PM2.5 modeled as an averaged lag effect was also not significant. Parameter estimates were minimally impacted (<1% change) by inclusion of an offset term reflecting an average annual increase in the population of roughly 2% during the study time period.
Figure 3.
Percent change in stroke/TIA risk associated with an IQR (5.1 μg/m3) increase in PM2.5.
Median O3 was 25.6 ppb (IQR: 18.1–33.8). Results of the analysis including O3 are included in Table 1. The associations between same-day (RR=1.02, 95% CI: 0.97–1.08) and previous day (RR=1.04, 95% CI: 0.99–1.09) O3 exposure and stroke/TIA risk were similar in magnitude to PM2.5. When O3 was added to the PM2.5 models, parameter estimates for PM2.5 were largely unchanged (same day PM2.5 RR=1.03, 95% CI: 0.99–1.07; previous day PM2.5 RR=1.03, 95% CI: 0.99–1.06). Season did not modify the association of PM2.5 on stroke/TIA risk (p=0.49).
Table 1.
Stroke/TIA risk ratios associated with an IQR increase in pollutant levels.
| Lag 0 Models | Lag 1 Models | ||||||
|---|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | ||||
| Single Pollutant Models | PM2.5 | 1.03 | 0.99 | 1.07 | 1.03 | 1.00 | 1.07 |
| O3 | 1.02 | 0.97 | 1.08 | 1.04 | 0.99 | 1.09 | |
| Two Pollutant Models | PM2.5 | 1.03 | 0.99 | 1.07 | 1.03 | 0.99 | 1.06 |
| O3 | 1.02 | 0.97 | 1.07 | 1.03 | 0.98 | 1.09 | |
RR = Relative risk, CI = confidence interval, IQR = interquartile range
Discussion
We observed borderline significant associations between same day and previous day PM2.5 exposures and ischemic stroke/TIA risk accounting for temperature, day of the week and temporal trends in stroke/TIA events. These results were not confounded by O3 and the effects of PM2.5 on stroke/TIA risk did not differ based on season. Similar associations between same day and previous day O3 and stroke/TIA risk were also observed. These data contribute to the literature as there is currently a scarcity of data on the effect of environmental exposures on risk of stroke in the US. The relationship between PM2.5 and stroke/TIA was observed in this US community with a heavy fossil fuel industry presence but with relatively low exposure to PM2.5 relative to other regions in the US.39 This finding is consistent with previous research demonstrating an association between PM2.5 and stroke mortality even in a low air pollution area in Europe.17 Although the magnitude of elevated risk of stroke/TIA due to PM2.5 exposure (3% per 5μg/m3 increase in PM2.5) was relatively small, the vast majority of the public is exposed to ambient air pollution at the levels observed in this community or greater every day, suggesting a potentially large public health impact.
This is the first report linking PM2.5 to ischemic stroke/TIA in the US using data from a population-based stroke surveillance study with active and passive surveillance methods and rigorous case validation procedures. Use of these methods to identify events ensures complete case capture of stroke/TIAs in comparison to passive surveillance alone which has been used in the majority of studies to date but has also been shown to miss a considerable proportion of stroke/TIAs.32 Further, the case ascertainment methods used eliminate the possibility of including events that are not stroke or TIA. Dominici et al reported a roughly 1% change in hospital admissions for total cerebrovascular disease for a 10 μg/m3 increase in same day PM2.5 levels.21 This study was conducted in 204 US counties with an average PM2.5 level considerably higher than the current study (13.4 μg/m3). Wellenius et al reported a 1% change in hospital admissions for ischemic stroke but for a roughly 20 μg/m3 increase in same day PM10 levels.23 Both studies reported no association for air pollution levels measured 1–2 days prior to stroke admission. Our effect size was larger likely due to the different case ascertainment methods and inclusion of TIAs.
Several studies have considered total cerebrovascular disease or total stroke deaths, although the different stroke types are likely to be affected by air pollution through different biologic mechanisms and may have different critical periods of exposure. Our findings support the hypothesis that recent exposure to PM2.5 may increase risk of acute ischemic cerebrovascular events specifically. Experimental evidence suggests that particulate air pollution is associated with acute artery vasoconstriction29 and also with increases in plasma viscosity,31 processes which may enhance the potential for thrombosis but this requires further study. We did not have data on ischemic stroke subtypes but investigation into the associations between PM2.5 and ischemic stroke subtypes could shed light on the specific biologic mechanisms linking PM2.5 and risk of ischemic stroke. Due to the high case fatality associated with intracerebral hemorrhage and the inconsistent findings with regard to the effect of air pollution on this stroke type,22, 23, 25, 27 additional studies on this topic are also warranted.
The USEPA NAAQS for annual PM2.5 is 15 μg/m3, and the current NAAQS for 24-hour average PM2.5 is 65 μg/m3. In this community, the 99th percentile of the distribution of PM2.5 levels was well below the 24-hour standard at roughly 28μg/m3 likely due to the coastal location of the community and prevailing wind patterns (see Figure 3). While our observed association between PM2.5 and stroke/TIA risk requires further study in additional regions in the US with varying types of climates and possibly with alternative study designs, it does call into question current standards for fine particulate matter and whether these standards are sufficient to protect the public with regard to stroke, our nation’s third leading cause of death. Critical to this issue is the further study of the specific components of PM2.5, the geographic variability in PM2.5 chemical composition, and the pathways by which these components directly affect ischemic stroke/TIA risk. We did not have data on the specific composition of PM2.5 in this study population, although this could shed light on the observed association despite the low levels of PM2.5. Previous research suggests regional differences in the association between PM2.5 and stroke hospitalizations likely due to differences in PM2.5 composition.21
Although the focus of this study was PM2.5, the observed borderline association between low levels of O3 and stroke/TIA risk suggests that ambient air pollution, in general, may affect stroke risk. While some studies looking at multiple pollutants within the same population have found similar associations with stroke endpoints across pollutants,14, 15, 23 this has not been a consistent finding.17, 27 Most recently, investigators from the Dijon Stroke Register, a population-based stroke registry, reported on the association between short-term exposure to various air pollutants and ischemic stroke/TIA risk using a case-crossover approach.27 This study found a significant association between previous day O3 and ischemic stroke/TIA risk but did not find associations for PM10, sulfur dioxide, nitrogen dioxide or carbon monoxide. Additional studies are required to understand whether specific air pollutants and their constituents are particularly harmful for stroke or whether air pollution in general affects stroke risk.
Limitations
This was an ecologic study and should be used primarily for hypothesis generation. While the findings are intriguing, they should be replicated. Given the study findings, future work should focus on confirming that the observed association was not due to additional unmeasured variables. For example, we were unable to determine the possible confounding or interaction effects of gender and race-ethnicity on stroke/TIA risk due to the ecological design. If the findings are confirmed, the identification of any susceptible subgroups of the population will be an important next step. Assessment of PM2.5 is subject to measurement error on various levels. Exposures were estimated from average PM2.5 measurements from a single monitor for the Corpus Christi area and may not accurately reflect PM2.5 levels across small geographic areas within the county. In addition, the measurement of PM2.5 from fixed monitors may be subject to error, although USEPA standardized methods were used to collect the ambient PM2.5 data. Some research suggests that the effects of air pollution on mortality, stroke and stroke outcomes are limited to or enhanced by warm weather perhaps due to greater exposure to outdoor air.17, 22, 37 Within our study, we did not find that season modified the effect of PM2.5 on stroke/TIA risk; however, this study was conducted in a coastal area with relatively high year round temperatures and humidity so the findings may not be generalizable to areas with varying climates. Our analysis focused primarily on PM2.5 given its plausible biologic link to the cardiovascular system and adjusted for the confounding effects of O3; however, residual confounding by other pollutants is possible.
Conclusion
We observed an association between same day and previous day PM2.5 exposure and risk of ischemic stroke/TIA using data from a population-based stroke surveillance study in a US community with relatively low PM2.5 levels. This study contributes data on environmental exposures and stroke risk in the US and suggests that additional research on this topic is warranted.
Acknowledgments
This study was funded by NIH RO1 NS38916.
The authors would like to thank Drs. Marie Oneill and Nalini Ranjit for their advice on unconstrained distributed lag Poisson regression models.
References
- 1.Kunzli N, Jerrett M, Mack WJ, et al. Ambient air pollution and atherosclerosis in Los Angeles. Environ Health Perspect. 2005;113:201–206. doi: 10.1289/ehp.7523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moolgavkar SH. Air pollution and daily mortality in three U.S. counties. Environ Health Perspect. 2000;108:777–784. doi: 10.1289/ehp.00108777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moolgavkar SH. Air pollution and hospital admissions for diseases of the circulatory system in three U.S. metropolitan areas. Journal of the Air & Waste Management Association (1995) 2000;50:1199–1206. doi: 10.1080/10473289.2000.10464162. [DOI] [PubMed] [Google Scholar]
- 4.Samet JM, Dominici F, Curriero FC, et al. Fine particulate air pollution and mortality in 20 U.S. cities, 1987–1994. N Engl J Med. 2000;343:1742–1749. doi: 10.1056/NEJM200012143432401. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz J. Air pollution and hospital admissions for cardiovascular disease in Tucson. Epidemiology. 1997;8:371–377. doi: 10.1097/00001648-199707000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Kelsall JE, Samet JM, Zeger SL, Xu J. Air pollution and mortality in Philadelphia, 1974–1988. American journal of epidemiology. 1997;146:750–762. doi: 10.1093/oxfordjournals.aje.a009351. [DOI] [PubMed] [Google Scholar]
- 7.Dockery DW, Luttmann-Gibson H, Rich DQ, et al. Particulate air pollution and nonfatal cardiac events. Part II. Association of air pollution with confirmed arrhythmias recorded by implanted defibrillators. Research report (Health Effects Institute) 2005:83–126. discussion 127–148. [PubMed] [Google Scholar]
- 8.Liao D, Duan Y, Whitsel EA, et al. Association of higher levels of ambient criteria pollutants with impaired cardiac autonomic control: a population-based study. American journal of epidemiology. 2004;159:768–777. doi: 10.1093/aje/kwh109. [DOI] [PubMed] [Google Scholar]
- 9.Peters A, Liu E, Verrier RL, et al. Air pollution and incidence of cardiac arrhythmia. Epidemiology. 2000;11:11–17. doi: 10.1097/00001648-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Peters A, Perz S, Doring A, et al. Increases in heart rate during an air pollution episode. American journal of epidemiology. 1999;150:1094–1098. doi: 10.1093/oxfordjournals.aje.a009934. [DOI] [PubMed] [Google Scholar]
- 11.Peters A, von Klot S, Heier M, et al. Particulate air pollution and nonfatal cardiac events. Part I. Air pollution, personal activities, and onset of myocardial infarction in a case-crossover study. Research report (Health Effects Institute) 2005:1–66. discussion 67–82, 141–148. [PubMed] [Google Scholar]
- 12.Schwartz J, Dockery DW, Neas LM. Is daily mortality associated specifically with fine particles? Journal of the Air & Waste Management Association (1995) 1996;46:927–939. [PubMed] [Google Scholar]
- 13.von Klot S, Peters A, Aalto P, et al. Ambient air pollution is associated with increased risk of hospital cardiac readmissions of myocardial infarction survivors in five European cities. Circulation. 2005;112:3073–3079. doi: 10.1161/CIRCULATIONAHA.105.548743. [DOI] [PubMed] [Google Scholar]
- 14.Hong YC, Lee JT, Kim H, et al. Effects of air pollutants on acute stroke mortality. Environ Health Perspect. 2002;110:187–191. doi: 10.1289/ehp.02110187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hong YC, Lee JT, Kim H, Kwon HJ. Air pollution: a new risk factor in ischemic stroke mortality. Stroke; a journal of cerebral circulation. 2002;33:2165–2169. doi: 10.1161/01.str.0000026865.52610.5b. [DOI] [PubMed] [Google Scholar]
- 16.Kan H, Jia J, Chen B. Acute stroke mortality and air pollution: new evidence from Shanghai, China. J Occup Health. 2003;45:321–323. doi: 10.1539/joh.45.321. [DOI] [PubMed] [Google Scholar]
- 17.Kettunen J, Lanki T, Tiittanen P, et al. Associations of fine and ultrafine particulate air pollution with stroke mortality in an area of low air pollution levels. Stroke; a journal of cerebral circulation. 2007;38:918–922. doi: 10.1161/01.STR.0000257999.49706.3b. [DOI] [PubMed] [Google Scholar]
- 18.Kim H, Kim Y, Hong YC. The lag-effect pattern in the relationship of particulate air pollution to daily mortality in Seoul, Korea. Int J Biometeorol. 2003;48:25–30. doi: 10.1007/s00484-003-0176-0. [DOI] [PubMed] [Google Scholar]
- 19.Maheswaran R, Haining RP, Brindley P, et al. Outdoor air pollution and stroke in Sheffield, United Kingdom: a small-area level geographical study. Stroke; a journal of cerebral circulation. 2005;36:239–243. doi: 10.1161/01.STR.0000151363.71221.12. [DOI] [PubMed] [Google Scholar]
- 20.Maheswaran R, Haining RP, Pearson T, et al. Outdoor NOx and stroke mortality: adjusting for small area level smoking prevalence using a Bayesian approach. Stat Methods Med Res. 2006;15:499–516. doi: 10.1177/0962280206071644. [DOI] [PubMed] [Google Scholar]
- 21.Dominici F, Peng RD, Bell ML, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. Jama. 2006;295:1127–1134. doi: 10.1001/jama.295.10.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsai SS, Goggins WB, Chiu HF, Yang CY. Evidence for an association between air pollution and daily stroke admissions in Kaohsiung, Taiwan. Stroke; a journal of cerebral circulation. 2003;34:2612–2616. doi: 10.1161/01.STR.0000095564.33543.64. [DOI] [PubMed] [Google Scholar]
- 23.Wellenius GA, Schwartz J, Mittleman MA. Air pollution and hospital admissions for ischemic and hemorrhagic stroke among Medicare beneficiaries. Stroke; a journal of cerebral circulation. 2005;36:2549–2553. doi: 10.1161/01.STR.0000189687.78760.47. [DOI] [PubMed] [Google Scholar]
- 24.Wordley J, Walters S, Ayres JG. Short term variations in hospital admissions and mortality and particulate air pollution. Occupational and environmental medicine. 1997;54:108–116. doi: 10.1136/oem.54.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Villeneuve PJ, Chen L, Stieb D, Rowe BH. Associations between outdoor air pollution and emergency department visits for stroke in Edmonton, Canada. Eur J Epidemiol. 2006;21:689–700. doi: 10.1007/s10654-006-9050-9. [DOI] [PubMed] [Google Scholar]
- 26.Low RB, Bielory L, Qureshi AI, et al. The relation of stroke admissions to recent weather, airborne allergens, air pollution, seasons, upper respiratory infections, and asthma incidence, September 11, 2001, and day of the week. Stroke; a journal of cerebral circulation. 2006;37:951–957. doi: 10.1161/01.STR.0000214681.94680.66. [DOI] [PubMed] [Google Scholar]
- 27.Henrotin JB, Besancenot JP, Bejot Y, Giroud M. Short-term effects of ozone air pollution on ischaemic stroke occurrence: a case-crossover analysis from a 10-year population-based study in Dijon, France. Occupational and environmental medicine. 2007;64:439–445. doi: 10.1136/oem.2006.029306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nemmar A, Hoet PH, Vanquickenborne B, et al. Passage of inhaled particles into the blood circulation in humans. Circulation. 2002;105:411–414. doi: 10.1161/hc0402.104118. [DOI] [PubMed] [Google Scholar]
- 29.Brook RD, Brook JR, Urch B, et al. Inhalation of fine particulate air pollution and ozone causes acute arterial vasoconstriction in healthy adults. Circulation. 2002;105:1534–1536. doi: 10.1161/01.cir.0000013838.94747.64. [DOI] [PubMed] [Google Scholar]
- 30.Urch B, Silverman F, Corey P, et al. Acute blood pressure responses in healthy adults during controlled air pollution exposures. Environ Health Perspect. 2005;113:1052–1055. doi: 10.1289/ehp.7785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peters A, Doring A, Wichmann HE, Koenig W. Increased plasma viscosity during an air pollution episode: a link to mortality? Lancet. 1997;349:1582–1587. doi: 10.1016/S0140-6736(97)01211-7. [DOI] [PubMed] [Google Scholar]
- 32.Piriyawat P, Smajsova M, Smith MA, et al. Comparison of active and passive surveillance for cerebrovascular disease: The Brain Attack Surveillance in Corpus Christi (BASIC) Project. American journal of epidemiology. 2002;156:1062–1069. doi: 10.1093/aje/kwf152. [DOI] [PubMed] [Google Scholar]
- 33.Asplund K, Tuomilehto J, Stegmayr B, et al. Diagnostic criteria and quality control of the registration of stroke events in the MONICA project. Acta medica Scandinavica. 1988;728:26–39. doi: 10.1111/j.0954-6820.1988.tb05550.x. [DOI] [PubMed] [Google Scholar]
- 34.Standard Industrial Classification (SIC) system search. Occupational Safety and Health Administration (OSHA), U.S. Department of Labor; [Accessed November 11, 2006]. http://www.osha.gov/pls/imis/sicsearch.html. [Google Scholar]
- 35.Historical Air Pollutant and Weather Data. Monitoring Operations Texas Historical Environmental Records (MOTHER), Texas Commission on Environmental Quality (TCEQ); [Accessed November 11, 2006]. http://www.tceq.state.tx.us/compliance/monitoring/air/monops/historical_data.html. [Google Scholar]
- 36.Schwartz J. The distributed lag between air pollution and daily deaths. Epidemiology. 2000;11:320–326. doi: 10.1097/00001648-200005000-00016. [DOI] [PubMed] [Google Scholar]
- 37.Katsouyanni K, Pantazopoulou A, Touloumi G, et al. Evidence for interaction between air pollution and high temperature in the causation of excess mortality. Arch Environ Health. 1993;48:235–242. doi: 10.1080/00039896.1993.9940365. [DOI] [PubMed] [Google Scholar]
- 38.Dominici F, McDermott A, Zeger SL, Samet JM. On the use of generalized additive models in time-series studies of air pollution and health. American journal of epidemiology. 2002;156:193–203. doi: 10.1093/aje/kwf062. [DOI] [PubMed] [Google Scholar]
- 39.Diez Roux AV, Auchincloss AH, Astor B, et al. Recent exposure to particulate matter and C-reactive protein concentration in the multi-ethnic study of atherosclerosis. American journal of epidemiology. 2006;164:437–448. doi: 10.1093/aje/kwj186. [DOI] [PubMed] [Google Scholar]