ABSTRACT
Purpose: To identify current practice for elderly individuals who have sustained a fall-related injury and subsequently presented to the emergency department (ED) of a community-based hospital in Toronto, Ontario.
Methods: A retrospective longitudinal chart review was conducted for 300 persons, 65 years of age and older, who presented to the ED of a community-based teaching hospital with a fall from June 2004 through May 2005. Data were collected using a tool created by the investigators (based on information gathered through a literature review) to capture information related to risk factors for falling.
Results: Our study sample was demographically similar to elderly individuals in other fall-related studies. Most patients discharged directly from the ED did not receive multidisciplinary care. In the ED, all patients saw a nurse or physician, while only 1.3% (n = 4) saw a physical therapist, 3.0% (n = 9) saw an occupational therapist, and 5.3% (n = 16) saw a social worker. At discharge, 62% (n = 152) had no documented referral for follow-up care. Abilities related to falls in elderly individuals were not consistently assessed in the ED. Frequency of assessment for these abilities was as follows: (1) gait, 10.2%; (2) balance, 4.1%; (3) lower-extremity range of motion, 4.9%; (4) lower-extremity strength, 2.0%; (5) cognition, 26.1%; (6) vision, 2.0%; (7) ability to perform activities of daily living, 7.3%. In the 6 months following the index fall, 8.3% of patients returned to the ED of the same hospital because of a subsequent fall.
Conclusions: In the ED, fall-related risk factors were not consistently assessed or documented, and few patients received multidisciplinary management. Since elderly individuals who fall commonly present to the ED, the implementation of evidence-based strategies aimed at preventing repeat falls should be considered.
Key Words: emergency department management, falls in the elderly, fall prevention, fall-related injuries, fall risk
RÉSUMÉ
Objectif : Définir les modalités des soins fournis aux personnes âgées qui se sont présentées au service des urgences d'un hôpital communautaire de Toronto, en Ontario, après s'être blessées en tombant.
Méthode : On a procédé à l'analyse rétrospective longitudinale des dossiers de 300 personnes de 65 ans et plus qui s'étaient présentées, de juin 2004 à mai 2005, au service des urgences d'un hôpital communautaire universitaire après avoir fait une chute. La collecte des données s'est effectuée au moyen d'un outil mis au point par les enquêteurs (selon ce qu'a révélé une analyse documentaire), en vue de faire ressortir les facteurs de risque de chute.
Résultats : L'échantillon étudié s'apparentait, sur le plan démographique, à la population des personnes âgées prise en compte dans d'autres études sur le sujet. La plupart des patients qui ont été congédié directement du service des urgences n'ont pas eu accès à des soins multidisciplinaires. Tous ont pu consulter un médecin ou un membre du personnel infirmier, mais à peine 1,3 % (n = 4) ont vu un physiothérapeute, 3,0 % (n = 9), un ergothérapeute et 5,3 % (n = 16), un travailleur social. Au congé, 62 % des patients (n = 152) n'avaient reçu aucune demande de consultation écrite aux fins de suivi. Au service des urgences, les aptitudes jouant un rôle dans les chutes, plutôt que de faire l'objet d'une évaluation systématique, ont été mesurées à des fréquences diverses : (1) démarche = 10,2 %; (2) équilibre = 4,1 %; (3) amplitude de mouvement des membres inférieurs = 4,9 %; (4) force des membres inférieurs = 2,0 %; (5) cognition = 26,1 %; (6) vision = 2,0 %; (7) capacité de d'exécuter les activités de la vie quotidienne = 7,3 %. Au cours des 6 mois qui ont suivi la chute de référence, une autre chute a obligé 8,3 % des patients à se rendre de nouveau au service des urgences du même hôpital.
Conclusions : Les facteurs de risque de chute n'ont pas été systématiquement évalués et/ou documentés, et peu de patients ont bénéficié d'une prise en charge multidisciplinaire après s'être présentés au service des urgences. Comme il est fréquent que des personnes âgées se rendent au service des urgences après une chute, la mise en place de stratégies fondées sur des données probantes et destinées à prévenir les chutes à répétition devrait être envisagée.
Mots clés : blessures liées à une chute, chutes chez les personnes âgées, gestion d'un service des urgences, prévention des chutes, risque de chute
INTRODUCTION
Falls are a major health concern in the elderly population. Currently, individuals over the age of 65 make up an estimated 13% (4.2 million) of the 32 million people living in Canada,1 and this number is expected to grow to approximately 6.7 million (20%) by 2021 and to approximately 9.2 million (25%) by 2041.2 The rapid growth of the over-65 age group highlights the importance of addressing health issues, such as falls, which are more common among elderly persons. It is estimated that fall-related injuries currently cost the Canadian health care system $2.8 billion per year.3 The Public Health Agency of Canada has determined that even a 20% reduction in the rate of falls among Canadian seniors would translate into approximately 7,500 fewer hospitalizations and 1,800 fewer permanently disabled seniors, for an overall national savings of as much as $138 billion per year.1
The American Geriatrics Society (AGS), the American Academy of Orthopaedic Surgeons (AAOS), and the British Geriatrics Society (BGS) created a guideline intended to assist health care professionals in the management of elderly persons who have fallen or who are at risk of falling.4 The authors stressed that performing a fall-risk assessment will likely reduce future falls, especially when coupled with a fall-related intervention. However, this guideline is not specific to the emergency department (ED).
Elderly individuals who sustain fall-related injuries commonly present to hospital EDs, yet few studies describe ED management practices for this population, and none of these studies are specific to the province of Ontario. Currently it is not known what management practices are routine for elderly persons presenting to EDs in Ontario with fall-related injuries.
LITERATURE REVIEW
The factors that place elderly individuals at increased risk for falling can be divided into four categories: (1) biological, (2) behavioural, (3) environmental, and (4) socio-economic.5 These groupings are not mutually exclusive, as several risk factors may be applicable to more than one category. Biological risk factors include advanced age, female gender, chronic and acute health conditions, cognitive impairments, lower-extremity weakness, physical limitations, gait abnormalities, balance deficits, and altered sensation.1,5–10 A history of previous falls is a behavioural risk factor,4 as is the use of medications, especially for persons using four or more prescription drugs.11,12 Other behavioural risk factors include the use of alcohol and other non-medical drugs, fear of falling, poor diet, insufficient exercise, inappropriate footwear, the use of assistive devices, and frequent toileting.5,8,10,11,13 Environmental risk factors are extremely varied and include poor weather conditions, uneven sidewalk surfaces, slippery floors, cluttered furniture, poor lighting, and use of unsafe equipment such as wheeled beds or chairs.5,11 Finally, socio-economic factors that increase the risk of falling include inadequate housing, low income, lack of social support, social isolation, and lower levels of education.5 Because falls sustained by elderly individuals are generally caused by a combination of risk factors, it is important that health care practitioners consider all four categories when developing management strategies to prevent future falls.
Because the majority of individuals over the age of 65 seek medical treatment in the ED within 48 hours following a fall-related injury,1 the ED is a critical location for the identification of underlying risk factors and problems. Fall-related risk factors have been shown to be under-diagnosed in this high-risk population.14 A systematic review by Weigand and Gerson15 evaluating ED-based prevention and screening interventions found no literature examining primary or secondary prevention of falls in older persons presenting to the ED and only one study dealing with tertiary prevention—the Prevention of Falls in the Elderly Trial (PROFET).16 This randomized controlled trial studied 397 community-dwelling persons older than 65 years of age who presented to the ED with a fall-related injury. Persons in the control group (n = 213) received conventional treatment consisting of “usual care only,” which was not described in the study. Those in the intervention group (n = 184) received a detailed medical and occupational therapy (OT) assessment as well as conventional treatment. Results at 12-month follow-up showed that the total number of reported falls was significantly higher for the control group than for the intervention group, with 510 falls (2.4 per person) and 183 (1.0 person) falls respectively. Additionally, the intervention group had a lower risk of falling, a lower risk of recurrent falls, and fewer admissions to hospital. The authors underscored the dynamic interaction between intrinsic risk factors (i.e., age, gender, comorbidities) and extrinsic risk factors (i.e., environmental hazards and home supports), as well as the importance of a multidisciplinary assessment.
A similar study was conducted in an accident and emergency department in the United Kingdom by Davidson et al.13 This study compared conventional care (not described by the study) with a multi-factorial assessment and intervention programme—including medical treatment, physical therapy (PT), and OT—to prevent falls in cognitively intact, older (>65 years) persons with a history of recurrent falls. Follow-up revealed that the intervention group (n = 159) had 36% fewer falls over a 1-year period than the control group (n = 154). Both studies provide evidence to suggest that multidisciplinary assessment and interventions have a significant effect on reducing the number and risk of falls, as well as reducing readmissions to the ED.13,15
Our literature review also identified a study that found no significant differences between control and intervention groups for persons presenting to the ED with fall-related injuries.17 In this study, all participants (n = 274) received a multi-factorial baseline assessment, including medical, cardiovascular, PT, and OT. Following the assessment, the control group (n = 144) received conventional care (not defined by the study) while the intervention group (n = 130) received a multi-factorial intervention that included treatment of underlying medical problems, drug modification, education, and a 3-month home exercise programme.17 The results indicated that there were no significant differences between groups for any of the study outcomes, including the proportion of participants who fell and the number of falls. The lack of statistically significant results may be due to the fact that the study was limited to participants with cognitive impairments. Persons with cognitive impairments may have different needs than the general population of elderly individuals, and thus require different strategies for fall prevention.17 Therefore, it may be inappropriate to generalize these results to the elderly population as a whole.
Despite literature showing the effectiveness of multi-factorial fall-related interventions for elderly persons presenting to the ED, these interventions are not routinely being implemented. A study conducted in the United Kingdom found that the majority of women aged 70 years and older who presented to the ED with a fall-related injury did not receive care consistent with the guidelines for fall prevention set out by the AGS, BGS, and AAOS.18 A similar study conducted in British Columbia found that only 3.7% of elderly patients presenting to the ED with a fall received care consistent with these guidelines, and only 11% received partial guideline care.19 It is not known whether the recommended evidence-based practices for elderly individuals who fall are being implemented in Ontario EDs. In this study we examined a community-based hospital ED in Ontario that handles a considerable number of elderly persons who fall (approximately 100 per month).20
The purpose of this study was to identify current practice for elderly individuals who sustain a fall-related injury and subsequently present to the ED of a community-based hospital in Toronto, Ontario. The study addressed the following objectives:
to describe elderly patients presenting to the ED with a fall-related injury by identifying patient demographics and fall descriptors;
to identify current practice for the management of these patients (i.e., data collection, involvement of health care practitioners, treatment, discharge home or hospital admission), including how they were screened, assessed, treated, and discharged;
to identify which health care practitioners were managing this patient population; and
to determine the percentage of study participants who returned to the ED within 6 months of their initial index fall.
For the purposes of this study, a fall-related injury was defined as “an injury which resulted from a person coming to rest inadvertently on the ground or floor or other lower level, excluding injuries due to assault, intentional self-harm, animals, burning buildings, transport vehicles, and falls into fire, water and machinery.”21
METHODS
Setting
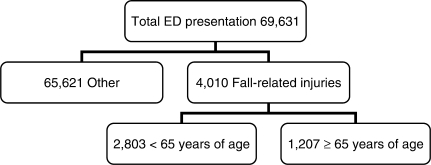
The study was conducted at a community-based teaching hospital located in Toronto, Ontario. This hospital's ED handles an average of 5,803 patient presentations each month. In 2004, an average of 334 patients per month presented with fall-related injuries, and 30% of these individuals were over the age of 65 (see Figure 1).20 Ethics approval for this study was provided by the Research Ethics Boards at the University of Toronto and the participating community-based teaching hospital.
Figure 1.
Patients presenting to the ED of a community-based teaching hospital in 20045
Study Design
A longitudinal retrospective chart review was conducted with patient records obtained over a 12-month period from June 2004 through May 2005.
A master list was generated by the participating hospital's Health Records Department for all persons 65 years of age and older who were triaged in the ED with a fall-related injury from June 2004 through May 2005. From the master list, 25 charts from each month were selected using a random number generator to allow for seasonal variations that may have affected the frequency, duration, type, and severity of the fall-related injuries. To ensure confidentiality, a unique identification number was assigned to each chart selected for inclusion; no other identifying information was included in the data collected for the study. The list containing the original identifiers was stored in a locked cabinet at the study hospital and was destroyed on completion of data collection.
Each chart selected was included in the study if, at the time of presentation to the ED, the person was 65 years of age or older, had sustained a fall-related injury (as defined by the World Health Organization),21 and presented to the ED within the study's selected time frame (June 2004 through May 2005). Occasionally a chart was selected from the master list that did not meet the study's eligibility criteria. When this occurred, the chart was excluded and replaced by another randomly selected chart from the same month.
A data-collection tool (see Appendix A) was created by the investigators prior to the commencement of data extraction to ensure consistency among investigators. This tool was based on the study objectives. It was designed to capture information on the risk factors for falling identified in the literature5 as well as information on the management and outcomes of elderly individuals in the ED. It included variables such as patient demographics (e.g., age, sex, marital status), past medical history (e.g., history of falls, comorbidities, medication use), circumstances surrounding the fall (e.g., location of fall, type of injury sustained, time of day), management provided (e.g., what functional abilities were assessed, which health care practitioners were involved), and patient outcomes (e.g., patient returning to the ED in the following 6-month period). Five individuals (including the three primary investigators), all of whom were MScPT students at University of Toronto at the time of data collection, extracted the data. The data-collection tool was tested before the study began. The testing was done collaboratively by all five individuals involved in data collection, using five patient charts that were not included in the study. Testing the tool provided an opportunity for the investigators to practise using the tool and to clarify potential discrepancies between investigators with respect to data input. Where there were discrepancies, consensus was achieved through general discussion. During testing it was decided that for the purposes of this study, abilities would be deemed to have been assessed if any health care practitioner documented having performed any type of assessment (observation, patient report, or formal tool) of the abilities listed in the data-collection tool at any time during the patient's visit to the community-based teaching hospital.
Data Analysis
Descriptive statistics, including means, medians, standard deviations, and frequencies, were calculated for each variable. The descriptive statistics were used to address all four study objectives by identifying demographic characteristics and fall descriptors, ED management, involvement of health care practitioners, and patient outcomes for elderly individuals who sustained a fall-related injury. Statistical analysis was performed using SPSS version 13.0 (SPSS Inc., Chicago, IL).
RESULTS
Patient Demographics and Fall Descriptors
Demographics of the sample are presented in Table 1. The majority of the sample (n = 300) was female (63.7%), and the mean age of the sample was 78.2 years (SD = 7.4 years). Using a list of postal codes obtained from the hospital, we found that 76% (n = 229) of the patients lived within the hospital's catchment area. Housing information was not documented for the majority of individuals (57.3%, n = 172). Similarly, the number of patients using stairs in the home, the availability of home supports, and the use of gait aids prior to admission could not be accurately obtained, as this information was not documented in the majority of the charts. Most patients (81.7%, n = 245) were discharged directly home from the ED.
Table 1.
Demographics and Characteristics of Patients Presenting to ED with a Fall-related Injury*
| Discharged from ED (n = 245) n (%) | Admitted to Hospital (n = 55) n (%) | Total Sample (n = 300) n (%) | |
|---|---|---|---|
| Age: | |||
| Age [Mean (SD)] | 77.3 (7.3) | 82.13 (6.3) | 78.19 (7.4) |
| 65–74 | 93 (38.0) | 5 (9.1) | 98 (32.7) |
| 75–84 | 115 (46.9) | 28 (50.9) | 143 (47.7) |
| 85–94 | 37 (15.1) | 22 (40.0) | 59 (19.7) |
| Sex: | |||
| Male | 84 (34.3) | 20 (36.4) | 104 (34.7) |
| Female | 156 (63.7) | 35 (63.6) | 191 (63.7) |
| Catchment area: | |||
| Yes | 188 (76.7) | 41 (74.5) | 229 (76.3) |
| No | 48 (19.6) | 11 (20.0) | 59 (19.7) |
| Not documented | 2 (0.8) | 1 (1.8) | 3 (1.0) |
| Home supports:** | |||
| Yes | 51 (20.8) | 35 (63.6) | 86 (28.7) |
| No | 15 (6.1) | 15 (27.3) | 30 (10.0) |
| Not documented | 177 (72.2) | 2 (3.6) | 179 (59.7) |
| Housing: | |||
| House | 33 (13.5) | 23 (41.8) | 56 (18.7) |
| Apartment | 27 (11.0) | 20 (36.4) | 47 (15.7) |
| Retirement home | 14 (5.7) | 6 (11.0) | 20 (6.6) |
| Other | 1 (0.4) | 1 (1.8) | 2 (0.7) |
| Not documented | 168 (68.6) | 4 (7.3) | 172 (57.3) |
| Use of stairs in home: | |||
| Yes | 23 (9.4) | 24 (43.6) | 47 (15.7) |
| No | 5 (2.0) | 15 (27.3) | 20 (6.7) |
| Not documented | 216 (88.2) | 15 (27.3) | 231 (77.0) |
| Use of gait aid: | |||
| Yes | 29 (11.8) | 24 (43.6) | 53 (17.7) |
| No | 9 (3.7) | 20 (36.4) | 29 (9.7) |
| Not documented | 207 (84.5%) | 9 (16.4) | 216 (72.0) |
If percentages do not add up to 100%, this is due to missing data.
Home supports include joint living situations, family or friends available when needed, community assistance, and supported living environments (e.g., retirement homes)
Table 2 presents information obtained regarding the past medical history of the study sample. The total sample had a mean of 1.8 (SD = 1.5) comorbidities out of a possible 13 recorded by the investigators, which were identified based on the available literature regarding fall risk factors.6,8,9,12 The most common comorbidities were cardiovascular disease (57.7%, n = 173), osteoarthritis (19.7%, n = 59), and osteoporosis (18.0%, n = 54). A mean of 3.7 (4.0) medications per patient was reported in the ED, and 43.0% (n = 129) were taking four or more medications. Table 2 also shows that 29.3% of patients (n = 88) had a previous history of falls and that 9.3% (n = 28) had come to the hospital's ED following a fall in the 6 months prior to the index fall.
Table 2.
Medical History of Patients Presenting to the ED with a Fall-related Injury*
| Discharged from ED (n = 245) n (%) | Admitted to Hospital (n = 55) n (%) | Total Sample (n = 300) n (%) | |
|---|---|---|---|
| Comorbidities: | |||
| # of comorbidities [Mean (SD)] | 1.62 (1.4) | 2.65 (1.5) | 1.81 (1.5) |
| Diabetes | 29 (11.8) | 11 (20.0) | 40 (13.3) |
| Cardiovascular disease | 136 (55.5) | 37 (67.3) | 173 (57.7) |
| Incontinence | 5 (2.0) | 2 (3.6) | 7 (2.3) |
| Osteoarthritis | 43 (17.6) | 16 (29.1) | 59 (19.7) |
| Depression | 11 (4.5) | 5 (9.1) | 16 (5.3) |
| Cancer | 21 (8.6) | 11 (20.0) | 32 (10.7) |
| Stroke | 25 (10.2) | 7 (12.7) | 32 (10.7) |
| Neurological condition | 8 (3.3) | 11 (20.0) | 19 (6.3) |
| Osteoporosis | 37 (15.1) | 17 (30.9) | 54 (18.0) |
| Respiratory illness | 27 (11.0) | 9 (16.4) | 36 (12.0) |
| Hypo/hyperthyroidism | 20 (8.2) | 6 (10.9) | 26 (8.7) |
| Dementia | 17 (6.9) | 11 (20.0) | 28 (9.3) |
| Visual problems | 19 (7.8) | 3 (5.5) | 22 (7.3) |
| None or not documented | 36 (14.7) | 2 (3.6) | 38 (12.7) |
| Previous history of falls: | |||
| Yes | 72 (29.4) | 16 (29.1) | 88 (29.3) |
| No | 173 (70.6) | 31 (56.4) | 204 (68.0) |
| Medications: | |||
| # of medications [mean (SD)] | 3.39 (4.0) | 4.87 (3.7) | 3.66 (4.0) |
| 4 + medications | 95 (38.8) | 34 (61.8) | 129 (43.0) |
| Presented or admitted due to a fall in previous 6 months: | |||
| Yes | 21 (8.6) | 7 (12.7) | 28 (9.3) |
| No | 221 (90.2) | 48 (87.3) | 269 (89.7) |
| Presented or admitted for reason other than fall in previous 6 months: | |||
| Yes | 44 (18.0) | 12 (21.8) | 56 (18.7) |
| No | 200 (81.6) | 43 (78.2) | 243 (81.0) |
If percentages do not add up to 100%, this is due to missing data
The characteristics of the index falls sustained by the study sample are presented in Table 3. Falls were equally likely to occur inside the home (35.4%, n = 106) and outside the home (35.7%, n = 107), and often no explanation for the fall was given (21.3%, n = 64). The most common diagnosis upon presentation to the ED was fracture (37.7%, n = 113).
Table 3.
Fall Description at Time of Presentation to ED for Patients with a Fall-related Injury
| Discharged from ED (n = 245) n (%) | Admitted to Hospital (n = 55) n (%) | Total Sample (n = 300) n (%) | |
|---|---|---|---|
| Fall description: | |||
| Fell on stairs | 50 (20.4) | 7 (12.7) | 57 (19.0) |
| Fell on ice | 27 (11.0) | 2 (3.6) | 29 (9.7) |
| Fell on curb/sidewalk | 28 (11.4) | 4 (7.3) | 32 (10.7) |
| Fell from bed/chair/couch/ wheelchair | 22 (9.0) | 10 (18.1) | 32 (10.7) |
| Tripped on other object | 34 (13.9) | 9 (16.4) | 43 (14.3) |
| Unexplained fall | 49 (20.0) | 15 (27.3) | 64 (21.3) |
| Other | 34 (13.9) | 8 (14.6) | 42 (16.7) |
| Fall location: | |||
| Inside home | 78 (31.8) | 28 (50.9) | 106 (35.4) |
| Outside home | 92 (37.6) | 15 (27.3) | 107 (35.7) |
| Not documented | 67 (27.3) | 11 (20.0) | 78 (26.0) |
| Diagnosis: | |||
| Laceration | 42 (17.1) | 0 (0.0) | 42 (14.0) |
| Fracture | 71 (29.0) | 42 (76.3) | 113 (37.7) |
| Head injury | 25 (10.2) | 4 (7.3) | 29 (9.7) |
| Soft-tissue injury | 49 (20.0) | 3 (5.5) | 52 (17.3) |
| No diagnosed injury | 50 (20.4) | 2 (3.6) | 52 (17.3) |
| Other | 6 (2.4) | 4 (7.3) | 10 (3.3) |
| Loss of consciousness: | |||
| Yes | 6 (2.4) | 6 (10.9) | 12 (4.0) |
| No | 138 (56.3) | 32 (58.2) | 170 (56.7) |
| Unknown | 8 (3.3) | 2 (3.6) | 10 (3.3) |
| Not documented | 90 (36.7) | 15 (27.3) | 105 (35.0) |
| Alcohol use at time of fall: | |||
| Yes | 6 (2.4) | 2 (3.6) | 8 (2.7) |
| No | 9 (3.7) | 9 (16.4) | 18 (6.0) |
| Not documented | 229 (99.6) | 44 (80.0) | 273 (91.0) |
If percentages do not add up to 100%, this is due to missing data
Patient Management
Table 4 presents a summary of how patients were managed in hospital. For patients discharged directly from the ED, abilities were assessed as follows: gait, 10.2% of patients; balance, 4.1%; lower-extremity range of motion, 4.9%; lower-extremity strength, 2.0%; cognition, 26.1%; vision, 2.0%; and ability to perform activities of daily living, 7.3%. Of patients discharged directly from the ED, 62.0% (n = 152) had no documented referral at the time of discharge. Of those who did receive a referral 9.0% were referred to their family physician, 1.2% to PT, 1.6% to OT, 24.1% to a specialty clinic (e.g., fracture clinic), 1.2% to a rehabilitation hospital, and 3.7% to another health care service (e.g., homecare). Referral for ambulatory aids at discharge was not documented in the majority of cases (76.3%, n = 229).
Table 4.
Summary of Care Received by Patients Presenting to the ED with a Fall-related Injury
| Discharged from ED (n = 245) n (%) | Admitted to Hospital (n = 55) n (%) | Total Sample (n = 300) n (%) | |
|---|---|---|---|
| Seen by physical therapist in ED: | |||
| Yes | 3 (1.2) | 1 (1.8) | 4 (1.3) |
| No | 241 (98.4) | 53 (96.4) | 294 (98.0) |
| Seen by occupational therapist in ED: | |||
| Yes | 7 (2.9) | 2 (3.6) | 9 (3.0) |
| No | 237 (96.7) | 52 (94.5) | 289 (96.3) |
| Seen by social worker in ED: | |||
| Yes | 13 (5.3) | 3 (5.5) | 16 (5.3) |
| No | 231 (94.3) | 51 (92.7) | 282 (94.0) |
| Time spent in ED: | |||
| Mean time (hours:minutes) | 5:36 | 9:51 | 6:15 |
| Seen by physical therapist in hospital:** | |||
| Yes | 3 (1.2) | 46 (83.6) | 49 (16.3) |
| No | 241 (98.4) | 9 (16.4) | 251 (83.7) |
| Seen by occupational therapist in hospital:** | |||
| Yes | 7 (2.9) | 43 (78.2) | 50 (16.7) |
| No | 237 (96.7) | 12 (21.8) | 250 (83.3) |
| Seen by social worker in hospital:** | |||
| Yes | 13 (5.3) | 39 (70.9) | 48 (16.0) |
| No | 231 (94.3) | 16 (29.1) | 252 (84.0) |
| Functional abilities documented: | |||
| Gait | 25 (10.2) | 37 (67.3) | 62 (20.7) |
| Balance | 10 (4.1) | 35 (63.6) | 45 (15.0) |
| Lower-extremity range of motion (ROM) | 12 (4.9) | 21 (38.2) | 33 (11.0) |
| Lower-extremity strength | 5 (2.0) | 16 (29.1) | 21 (7.0) |
| Cognition | 64 (26.1) | 43 (78.2) | 107 (35.7) |
| Vision | 5 (2.0) | 20 (36.4) | 25 (8.3) |
| Ability to perform activities of daily living (ADL) | 18 (7.3) | 48 (87.3) | 68 (22.0) |
| No functional abilities assessed | 163 (66.5) | 2 (3.6) | 165 (55.0) |
| Ambulation aid referral at discharge: | |||
| Yes | 4 (1.6) | 20 (36.4) | 24 (8.0) |
| No | 34 (13.9) | 9 (16.4) | 43 (14.3) |
| Not documented | 206 (84.1) | 23 (41.8) | 229 (76.3) |
| Referrals at discharge: | |||
| Family physician | 22 (9.0) | 6 (10.9) | 28 (9.3) |
| Physical therapy | 3 (1.2) | 8 (14.5) | 11 (3.7) |
| Occupational therapy | 4 (1.6) | 2 (3.6) | 6 (2.0) |
| Specialty clinic | 59 (24.1) | 8 (14.5) | 67 (22.3) |
| Rehabilitation hospital | 3 (1.2) | 18 (32.7) | 21 (7.0) |
| Other (e.g., home care) | 9 (3.7) | 12 (21.8) | 21 (7.0) |
| No referral documented | 152 (62.0) | 15 (27.3) | 167 (55.7) |
If percentages do not add up to 100%, this is due to missing data.
Indicates that patient was seen by the specified health care professional at any time during the hospital visit/stay
Health Care Practitioners
Of the total study population, 1.3% (n = 4) saw a PT, 3.0% (n = 9) saw an OT, and 5.3% (n = 16) saw a social worker (SW) in the ED.
Return Visits to the ED
The outcomes of patients in the 6-month period following the index fall can be seen in Table 5. Eight percent (n = 25) returned to the participating hospital's ED with a subsequent fall, and 17.7% (n = 53) returned to the ED for a reason other than a fall.
Table 5.
Outcomes of Elderly Patients Presenting to the ED with a Fall-related Injury
| Discharged from ED (n = 245) n (%) | Admitted to Hospital (n = 55) n (%) | Total Sample (n = 300) n (%) | |
|---|---|---|---|
| Subsequently presented or admitted because of a fall within 6 months: | |||
| Yes | 20 (8.2) | 5 (9.1) | 25 (8.3) |
| No | 223 (91.0) | 49 (89.1) | 272 (90.7) |
| Subsequently presented or admitted for a reason other than a fall within 6 months: | |||
| Yes | 47 (19.2) | 6 (10.9) | 53 (17.7) |
| No | 195 (79.6) | 48 (87.3) | 243 (81.0) |
DISCUSSION
The population of elderly persons examined in this study who fell were demographically similar to the seniors in other fall-related research, supporting the generalizability of our results. Although the ED reports examined in this study provided only a limited amount of patient information, results showed that the study sample had many of the fall-related risk factors previously identified in the literature.1,5–8,10 The study sample was 63% female, similar to samples used in other Canadian studies.9 The Public Health Agency of Canada found that women have an increased risk of falls and also that women are at a higher risk for sustaining fall-related injuries.1 This increased risk of injury may be linked to the higher incidence of osteoporosis in women, as a result of which even a minor fall can result in serious injury such as a fracture.22 Fittingly, the most common diagnosis upon presentation to the ED in our study was a fracture (37.7%), and the majority of these were sustained by female patients. This increased risk makes women an important group to target with fall-related interventions.
The use of four or more medications has also been cited as a risk factor for falling.5 The results of our study showed a mean of 3.7 (SD = 4.0) medications per patient, while 43.0% were taking four or more medications. It is important to recognize that both the number and the type of medications contribute to fall risk. A more detailed analysis of these data through future studies would be required to further examine potential interactions.
Our data showed that only 29.3% of patients presenting to the ED had a previous history of falls. This is much lower than expected: Close et al.16 and Salter et al.19 found that 65% and 50% of their study participants, respectively, had fallen in the previous year. This discrepancy may reflect a lack of comprehensive assessment or a lack of documentation by health care practitioners in the ED in this study.
The most common comorbidities among our study sample were cardiovascular disease (CVD), osteoarthritis (OA), and osteoporosis. The high incidence of CVD in our study sample is similar to that found in Salter et al.'s study,19 in which one or more cardiovascular disorders may have been a contributing factor in 57% of subjects who sustained a fall. Our findings for other comorbidities were considerably lower than those of similar studies. For example, Salter et al.19 found the incidence of visual impairments and OA among fallers to be 94% and 50%, respectively. By contrast, only 7.3% of our study participants had visual impairments and only 19.7% had OA. These findings may reflect actual variations between the study samples; however, given that both samples had similar characteristics (i.e., elderly persons who fall presenting to a Canadian ED, mean age 78.5 versus 78.2 years, 63.0% versus 63.7% female), the differences may also reflect a lack of comprehensive assessment or a lack of documentation by health care practitioners in the ED in our study sample.
Abilities were also largely either not assessed or not documented in our study sample. In a study of health care consequences for elderly individuals who fall, Wilkins23 reported a higher frequency of falls in those individuals who were dependent in their activities of daily living (ADL). Yet in our study sample, ability to perform ADL was assessed for only 7.3% of individuals discharged directly from the ED. Additionally, although decreased mobility in elderly individuals post-fall often leads to further decline in health status,1 only 10.2% of patients had their gait assessed and only 4.1% had their balance assessed in the ED.
We were unable to ascertain whether or not alcohol played a role in any of the falls, because in 91.0% of cases alcohol use was not documented in the ED report. Similarly, we were unable to determine what percentage of the study sample used gait aids prior to the index fall and whether or not there were stairs in the home. The lack of documented information pertaining to these fall risk factors highlights the need to implement strategies that promote the collection of more information on fall-related risk factors and the integration of this information into the subsequent management of these patients in the ED.
Our results showed that only 1.3% (n = 4) of individuals saw a PT in the ED. This lack of assessment or treatment from a PT can be explained by the fact that at the time of the study, the investigating hospital did not have a dedicated PT resource in the ED. Fall intervention strategies that address multiple factors, including exercise, balance training, gait training, appropriate use of assistive devices, and environmental modifications, have been shown to help reduce the incidence of subsequent falls in elderly individuals.24,25 Assessing functional abilities and addressing modifiable fall-related risk factors is currently within the scope of PT practice; therefore, there may be a role for PTs in the ED to help in the management of elderly persons who fall. Salter et al.19 reported that 28% of individuals discharged directly from the ED did not receive a follow-up referral at discharge. Our results showed a higher percentage (62.0%) for this same group. The lack of follow-up referrals is a critical issue, as elderly patients show an increase in dependency for ADL post-discharge after presenting to the ED with a fall.26 As well, in a study of elderly patients discharged from the ED, Khan et al.14 suggested that patients presenting to the ED with a fall represent a high-risk group for missed diagnosis and would therefore benefit from follow-up services. Those individuals who did receive a referral at discharge were most likely to be referred to a specialty clinic (24.1%), commonly a fracture clinic; the second-largest group (9.0%) was referred to a family physician. Recent literature has shown that little is being done in terms of fall prevention at either of these referral sites.19,22
In addition to the 8.3% of patients who re-presented to the ED with a fall within 6 months of the index fall, 17.7% returned to the ED for a reason other than a fall. Return visits are costly to the Canadian health care system, and a reduction in the number of patients presenting and re-presenting to the ED has the potential to considerably reduce the costs to the health care system incurred by these individuals.
Baraff et al.27 explored the use of a fall-prevention intervention that educated ED staff about fall guidelines, but they found poor adherence to the guidelines by staff and no reduction in subsequent falls. The authors suggested several reasons why they did not see significant results. Primarily, the ED staff had only one educational session on fall prevention, and this was not followed up with quality management to determine whether the fall-prevention guidelines were being implemented. The ED staff also stated that often they did not have enough time to comply with the guidelines. Furthermore, the intervention consisted only of giving patients information on preventive health measures and relied upon the patients themselves to initiate changes. As a result, the intervention group had no more access to other health care practitioners or to follow-up treatments than the control group had.
A more appropriate way to address falls in the ED may be to implement a screening/assessment tool to help direct appropriate management of elderly persons who fall. To be effective, the tool should capture information about the various risk factors associated with falling; such a tool could potentially be organized according to the four risk-factor categories outlined by Manitoba Health: biological, behavioural, environmental, and socio-economic.5 This tool could help busy health care practitioners in the ED to be more efficient and accurate in identifying patients at risk for future falls and in need of fall-prevention management.
Limitations
Our study had several limitations. Many of the charts reviewed contained entries that were difficult for the investigators to decipher. The investigators worked collaboratively to decipher illegible handwriting, but sections of some charts may have been misinterpreted, while others simply had to be omitted. In addition, our study relied on the accuracy of information documented by health care practitioners working in a busy environment. It is possible that certain pieces of pertinent information were discussed with patients but not captured in the charts. Variations were occasionally found between health care practitioners with respect to patient demographics and fall descriptors. In the case of conflicting information, the ED report was used as the primary data source. Language barriers may also have been an issue that influenced the accuracy of data collected in the charts, given that a multicultural, community-based ED was chosen for this study. Out-of-catchment individuals who fell were another limitation: almost one in five individuals who fell in our study did not live within the hospital's catchment area. This may have led to the under-reporting of previous and subsequent falls, because these individuals may have been more likely to go to an ED within their own catchment area for a previous or subsequent fall. We may also have under-reported the number of persons who had repeat falls, since study participants may have sought no treatment or presented to another health care setting, such as a family physician's office, following a subsequent fall.
CONCLUSION
Our study found that, in the participating hospital's ED, fall-related risk factors were not consistently assessed or documented and few of the study participants received multidisciplinary management. As well, within 6 months of the index fall, 8.3% of patients had returned following a subsequent fall. Because elderly individuals who fall commonly present to the ED, the implementation of fall-reduction strategies in this location should be considered. Improved fall-risk assessment and management may help to reduce the overall costs associated with managing fall-related injuries and increase the safety and level of independence of our elderly population. Further investigation is needed to explore the implementation of fall-prevention strategies in the ED.
KEY MESSAGES
What Is Already Known on This Subject
The risk factors for falls in an elderly population are known and have been reported extensively in the literature. Evidence-based guidelines have been created by the American Geriatrics Society, the American Academy of Orthopaedic Surgeons, and the British Geriatrics Society to assist health care professionals in the management of elderly persons who have fallen. Proper fall-risk assessment and intervention have been shown to reduce the incidence of falls in an elderly population. Many elderly individuals who have fallen present to hospital-based emergency departments (EDs). Previous studies have shown that these individuals are not receiving care consistent with the fall-prevention guidelines after presenting to the ED.
What This Study Adds
This retrospective chart review showed that at an Ontario-based ED, information regarding fall risks was not consistently assessed and/or documented. Few elderly individuals who fell received multidisciplinary management in the ED, and referrals upon discharge for further follow-up were not consistently made and/or documented.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Selina Hirji and Tiffany Zaplitney for their assistance in this research.
APPENDIX A: DATA COLLECTION TOOL
DATA COLLECTION FORM—EMERGENCY DEPARTMENT FALLS
| Record Identifier: ___________________ | Arrival Month: ___________________ | ||
| Arrival Day: _______________________ | Arrival Year: _______________________ | ||
| Arrival Time: _______________(hh/mm) | Discharge Time: _____________(hh/mm) | ||
| Note: 00:00 = Time Missing00:01 = Actual time 00:00 | Note: 00:00 = Time Missing00:01 = Actual time 00:00 | ||
| Age: ____________ | Sex: 1 = Male 2 = Female | ||
| Within catchment? 1 = Yes 2 = No 3 = Not documented | English speaking: 1 = Yes 2 = No 3 = Not documented | ||
| Section 1: Presenting Fall History | |||
| Fall description / activity being performed when fall occurred: | 1 = Ladder 2 = Fell on ice 3 = Fell out of bed 4 = Tripped on curb/sidewalk/road | 5 = Syncope / dizzy 6 = Tripped on other object(s) 7 = Unexplained fall 8 = Other | |
| Fall location: | 1 = Bedroom | 5 = Living room | 9 = Not documented |
| 2 = Bathroom | 6 = Stairs | ||
| 3 = Hallway | 7 = Outside home | ||
| 4 = Kitchen | 8 = Other | ||
| Time fall occurred: | 1 = Day: 06:00–18:00 2 = Night: 18:00–06:00 3 = Not documented | ||
| Sequelae / diagnosis: | 1 = Laceration 2 = Upper extremity fracture 3 = Lower extremity fracture 4 = Trunk fracture (pelvis, ribs, spine) 5 = Head injury | 6 = Soft tissue injury 7 = No diagnosed injury 8 = Other 9 = Multiple site fracture | |
| Was there a loss of consciousness? | 1 = Yes 2 = No | 3 = Not documented 4 = Unknown | |
| Was the person under the influence of alcohol at the time of the fall? | 1 = Yes 2 = No | 3 = Not documented 4 = Unknown | |
| What members of the medical team played a role in the screening/ assessment of the patient? | 1 = MD and/or RN 2 = MD and/or RN & SW 3 = MD and/or RN & OT 4 = MD and/or RN & OT & SW | 5 = MD and/or RN & Other 6 = MD and/or RN & SW & PT | |
| Did the patient see a physiotherapist? | 1 = Yes 2 = No or Not Documented | ||
| MD = Medical Doctor; RN = Registered Nurse; SW = Social Worker; OT = Occupational Therapist; PT = Physiotherapist | |||
| Section 2: Past Medical History | |||
| Co-morbidities: | |||
| Diabetes? | 1 = Yes | 2 = No | |
| Cardiovascular disease? | 1 = Yes | 2 = No | |
| Incontinence? | 1 = Yes | 2 = No | |
| Osteoarthritis? | 1 = Yes | 2 = No | |
| Depression? | 1 = Yes | 2 = No | |
| Cancer? | 1 = Yes | 2 = No | |
| Stroke? | 1 = Yes | 2 = No | |
| Neurological condition (e.g., Parkinson's, traumatic brain injury) | 1 = Yes | 2 = No | |
| Osteoporosis? | 1 = Yes | 2 = No | |
| Respiratory illness? | 1 = Yes | 2 = No | |
| Hypo/hyperthyroidism | 1 = Yes | 2 = No | |
| Dementia (e.g., Alzheimer's, etc.) | 1 = Yes | 2 = No | |
| Visual | 1 = Yes | 2 = No | |
| None or not documented | 1 = Yes | 2 = No | |
| Other | 1 = Yes | 2 = No | |
| Previous fracture? | 1 = In the last month 2 = 1–3 months ago 3 = 3–6 months ago | 4 = 7–12 months 5 = Over 1 year 6 = No previous fracture documented | |
| Previous surgery? | 1 = In the last month 2 = 1–3 months ago 3 = 3–6 months ago | 4 = 7–12 months ago 5 = Over 1 year documented 6 = No previous surgery | |
| # of medications | |||
| 4 or more medications? | 1 = Yes | 2 = No | |
| Section 3: Psychosocial | |||
| Marital status: | 1 = Married 2 = Single 3 = Widowed | 4 = Divorced 5 = Not documented | |
| Home supports: | 1 = Yes 2 = No | 3 = Not Documented | |
| Housing: | 1 = House 2 = Condo 3 = Apartment 4 = Nursing home | 5 = Retirement home / community assisted 6 = Other 7 = Not documented | |
| Use of stairs in the home? | 1 = Yes 2 = No | 3 = Not documented | |
| Use of ambulation aids pre-admission? | 1 = Yes 2 = No | 3 = Not asked or indicated in chart | |
| Type of ambulation aid | 1 = Cane 2 = Walker 3 = Wheelchair (incl. scooter) 4 = Crutches | 5 = Non-traditional gait aid (e.g., broom, bucket) 6 = Not documented 7 = Multiple aids 81 = Not applicable | |
| Where used? | 1 = Inside the home 2 = Outside the home 3 = Both inside and outside the home | 4 = Not documented 81 = Not applicable | |
| Was there a referral for ambulation aids at discharge? | 1 = Yes 2 = No 3 = Not asked or indicated in chart | ||
| Discharge ambulation type | 1 = Cane 2 = Walker 3 = Wheelchair / Scooter4 = Crutches | 5 = Non-traditional gait aid (e.g., broom) 6 = Not documented 81 = Not applicable | |
| Admitted to hospital? | 1 = Yes 2 = No | ||
| Section 4: Admission Data | |||
| Admit day | (81 = Not applicable) | ||
| Admit month | (81 = Not applicable) | ||
| Admit year | (81 = Not applicable) | ||
| Reason for admission: | 1 = Hospitalization due to injury 2 = Hospitalization for other reasons 3 = Failure to cope 81 = Not applicable | ||
| Complications during admission? | 1 = Yes 2 = No | (81 = Not applicable) | |
| Total length of stay (# days): | 0 = < 24 hours | ||
| Section 5: Management and Patient Outcomes | |||
| Previous history of falls? | 1 = Yes 2 = No 3 = Not asked or indicated in chart | ||
| Falls risk assessment conducted? | 1 = Yes 2 = No | ||
| Falls risk assessment score: | 81 = Not Applicable If applicable, enter score ________. | ||
| Seen by physiotherapist? | 1 = Yes 2 = No | ||
| Seen by occupational therapist? | 1 = Yes 2 = No | ||
| Seen by social worker? | 1 = Yes 2 = No | ||
| Seen by speech language pathologist? | 1 = Yes 2 = No | ||
| Seen by other allied health professional? | 1 = Yes 2 = No | ||
| Not seen by other allied health professional? | 1 = Yes 2 = No | ||
| Referral to family doctor? | 1 = Yes 2 = No | ||
| Referral to physiotherapist? | 1 = Yes 2 = No | ||
| Referral to occupational therapist? | 1 = Yes 2 = No | ||
| Referral to specialty clinic | 1 = Yes 2 = No | ||
| Referral to rehabilitation hospital? | 1 = Yes 2 = No | ||
| Referral to other (includes homecare) | 1 = Yes 2 = No | ||
| No referral documented | 1 = Yes 2 = No | ||
| Previously presented or admitted for a fall within last 6 months? | 0 = 0 or not documented 1 = Once 2 = 2× | 3 = 3× 4 = 4× or more | |
| Subsequently presented or admitted due to a fall in the 6 months following? | 0 = 0 or not documented 1 = Once 2 = 2× | 3 = 3× 4 = 4× | |
| Previously presented or admitted in the last 6 months for a reason other than a fall | 0 = 0 or not documented 1 = Once 2 = 2× | 3 = 3× 4 = 4 | |
| Subsequently presented or admitted in the last 6 months for a reason other than a fall | 0 = 0 or not documented 1 = Once 2 = 2× | 3 = 3× 4 = 4× | |
| Section 6: Abilities | |||
| Gait assessed? | 1 = Yes 2 = No | ||
| Balance assessed? | 1 = Yes 2 = No | ||
| Lower extremity range of motion assessed? | 1 = Yes 2 = No | ||
| Strength assessed? | 1 = Yes 2 = No | ||
| Cognition assessed? | 1 = Yes 2 = No | ||
| Vision assessed? | 1 = Yes 2 = No | ||
| Activities of daily living assessed? | 1 = Yes 2 = No | ||
| Use of 4 or more medications? | 1 = Yes 2 = No | ||
| No risk factors assessed | 1 = Yes 2 = No | ||
Note : Any missing variables throughout the data collection template should be coded MV = 9, 99, 999
Miller E, Wightman E, Rumbolt K, McConnell S, Berg K, Devereaux M, Campbell F. Management of fall-related injuries in the elderly: a retrospective chart review of patients presenting to the emergency department of a community-based teaching hospital. Physiother Can. 2009;61:26–37.
REFERENCES
- 1.Public Health Agency of Canada. Report on seniors' falls in Canada [homepage on the Internet] Ottawa: The Agency; 2005. [updated 2005 Nov 4; cited 2005 Nov 23]. Available from: http://www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/index.htm. [Google Scholar]
- 2.Health Canada. Canada's ageing population [homepage on the Internet] Ottawa: Health Canada; 2002. [cited 2005 Nov 23]. Available from: http://www.phac-aspc.gc.ca/seniors-aines/pubs/fed_paper/pdfs/fedpager_e.pdf. [Google Scholar]
- 3.Canadian Orthopaedic Association. Canada in motion: mobilizing access to orthopaedic care [homepage on the Internet] 2005. [updated 2008 Feb 11; cited 2008 Oct 23]. Available from: http://www.coa-aco.org/library/health_policy/canada_in_motion.html.
- 4.American Geriatrics Society, British Geriatrics Society, American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49:664–72. [PubMed] [Google Scholar]
- 5.Manitoba Health. Preventing falls and fall-related injuries in Manitoba: a review of best practices. Impact. 2005:18–30. [Google Scholar]
- 6.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–6. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- 7.Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls: a prospective study. J Am Med Assoc. 1989;261:2663–8. [PubMed] [Google Scholar]
- 8.Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18:141–58. doi: 10.1016/s0749-0690(02)00002-2. [DOI] [PubMed] [Google Scholar]
- 9.Scott V, Pearce M, Pengelly C. Technical report: injury resulting from falls among Canadians age 65 and over [document on the Internet] Ottawa: Public Health Agency of Canada; 2005. [cited 2005 Nov 23]. Available from: http://www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/pdf/technical-report-injury_e.pdf. [Google Scholar]
- 10.Sherman FT. The cat's meow: a new mnemonic for diagnosis and management of falls in the elderly. Geriatrics. 2005;60:5–6. [PubMed] [Google Scholar]
- 11.Rogers ME, Rogers NL, Takeshima N, Islam MM. Methods to assess and improve the physical parameters associated with fall risk in older adults. Prev Med. 2003;36:255–64. doi: 10.1016/s0091-7435(02)00028-2. [DOI] [PubMed] [Google Scholar]
- 12.Kelly KD, Pickett W, Yiannakoulias N, Rowe BH, Schopflocher DP, Svenson L, et al. Medication use and falls in community-dwelling older persons. Age Ageing. 2003;32:503–9. doi: 10.1093/ageing/afg081. [DOI] [PubMed] [Google Scholar]
- 13.Davison J, Bond J, Dawson P, Steen IN, Kenny RA. Patients with recurrent falls attending Accident and Emergency benefit from multifactorial intervention: a randomized controlled trial. Age Ageing. 2005;34:162–8. doi: 10.1093/ageing/afi053. [DOI] [PubMed] [Google Scholar]
- 14.Khan SA, Miskelly FG, Piatt JS, Bhattachyya BK. Missed diagnosis among elderly patients discharged from an accident and emergency department. J Accid Emerg Med. 1996;13:256–7. doi: 10.1136/emj.13.4.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weigand JV, Gerson LW. Preventative care in the emergency department: should emergency departments institute a falls prevention program for elder patients? a systematic review. J Acad Emerg Med. 2001;8:823–6. doi: 10.1111/j.1553-2712.2001.tb00214.x. [DOI] [PubMed] [Google Scholar]
- 16.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomized controlled trial. Lancet. 1999;353:93–7. doi: 10.1016/S0140-6736(98)06119-4. [DOI] [PubMed] [Google Scholar]
- 17.Shaw FE, Bond J, Richardson DA, Dawson P, Steen IN, McKeith IG, et al. Multifactorial intervention after a fall in older people with cognitive impairment and dementia presenting to the accident and emergency department: randomised controlled trial. Brit Med J. 2003;326:1–6. doi: 10.1136/bmj.326.7380.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donaldson MG, Khan KM, Davis JC, Salter AE, Buchanan J, McKnight D, et al. Emergency department fall-related presentations do not trigger fall risk assessment: a gap in care of high risk outpatient fallers. Arch Gerontol Geriatr. 2005;41:311–7. doi: 10.1016/j.archger.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 19.Salter AE, Khan KM, Donaldson MG, Davis JC, Buchanan J, Abu-Laban RB, et al. Community-dwelling seniors who present to the emergency department with a fall do not receive guideline care and their fall risk profile worsens significantly: a 6-month prospective study. Osteoporos Int. 2006;17:672–83. doi: 10.1007/s00198-005-0032-7. [DOI] [PubMed] [Google Scholar]
- 20.St. Joseph's Health Centre. Emergency Department statistics. Prepared 2005 Sep. Available from: SJHC Emergency Department Database.
- 21.World Health Organization. homepage on the Internet. Falls. Geneva: The Organization; 2005. [cited 2005 Nov 24]. Available from: http://www.who.int/violence_injury_prevention/other_injury/falls/en. [Google Scholar]
- 22.Jaglal SB, Cameron C, Hawker GA, Carroll J, Jaakkimainen L, Cadarette SM, et al. Development of an integrated-care delivery model for post-fracture care in Ontario, Canada. Osteoporos Int. 2006;17:1337–45. doi: 10.1007/s00198-006-0076-3. [DOI] [PubMed] [Google Scholar]
- 23.Wilkins K. Health care consequences of falls for seniors. Health Rep. 1999;10:47–55. [PubMed] [Google Scholar]
- 24.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age Ageing. 1999;28:513–8. doi: 10.1093/ageing/28.6.513. [DOI] [PubMed] [Google Scholar]
- 25.Buchner DM, Cress ME, de Lateur BJ, Esselman PC, Margherita AJ, Price R, et al. The effect of strength and endurance training on gait, balance, fall risk, and health services use in community-living older adults. J Gerontol Med Sci. 1997;52:M218–24. doi: 10.1093/gerona/52a.4.m218. [DOI] [PubMed] [Google Scholar]
- 26.Rowland K, Maitra AK, Richardson DA, Hudson K, Woodhouse KW. The discharge of elderly patients from an accident and emergency department: functional changes and risk of readmission. Age Ageing. 1990;19:415–8. doi: 10.1093/ageing/19.6.415. [DOI] [PubMed] [Google Scholar]
- 27.Baraff LJ, Lee TJ, Kader S, Della Penn R. Effect of a practice guideline for emergency department care of falls in elder patients on subsequent falls and hospitalizations for injuries. Acad Emerg Med. 1999;6:1224–31. doi: 10.1111/j.1553-2712.1999.tb00138.x. [DOI] [PubMed] [Google Scholar]