SYNOPSIS
Objectives
Chat room-based prevention interventions for human immunodeficiency virus (HIV) are being implemented to reduce the risk of HIV exposure, infection, and re-infection among men who have sex with men (MSM).
Methods
Our community-based participatory research partnership implemented a chat room-based intervention known as Cyber-Based Education and Referral/Men for Men (CyBER/M4M). We collected both quantitative and qualitative data to describe the characteristics of chat-room participants (“chatters”) and their HIV risks and prevention needs, and to document intervention delivery.
Results
Of the 1,851 chatters who participated in the 18-month intervention, 210 completed the online assessment. The mean age was 30 years. Although the majority self-identified as gay, 25.8% self-identified as bisexual. More than half self-identified as white and one-third as black or African American. A total of 8.6% reported being HIV-positive and 14.8% reported never having been tested for HIV.
Grounded theory analysis of transcripts from chat-room instant-message discussions identified 13 thematic categories related to chatter characteristics, prevention needs, and intervention delivery. Chatters were looking for sexual partners, were not open about their orientation, lacked basic information about HIV, had questions about how to be tested, and perceived a lack of general community resources to meet their needs. Furthermore, CyBER educators had to understand and respect the online culture, build trust, and deliver well-crafted and focused messages.
Conclusions
Chat room-based interventions hold promise to systematically reach Internet communities of MSM, a group that is particularly at risk for infection with HIV and other sexually transmitted diseases.
Internet usage has reached 73% for all American adults, and well over 70 million people in the United States log on to the Internet during a typical day.1,2 Internet communities, news and discussion groups, e-mail lists, websites, electronic bulletin boards, and chat rooms are examples of Internet applications that offer unique and seemingly limitless opportunities for electronic communication. Internet applications can expedite the process for individuals searching for -others with similar interests or for those who want to connect with others, either electronically or in person. For many men who have sex with men (MSM), the Internet has emerged as an important tool for social networking and support, meeting friends and sexual partners, and building community.3–5 Although there has been evidence of a digital divide—which suggests that in the U.S., younger, more educated, and higher-income white men have increased access to the Internet1,6,7—this trend may be changing as the number of individuals online increases.8–11 Further, MSM appear to be early adopters of the Internet for both sexual and nonsexual communication;5 thus, Internet use by MSM does not mirror aggregate trends.9–14
Although the Internet is an important tool in the development of social and sexual identity for some MSM,15–18 seeking sex on the Internet has been found to be a risk factor for human immunodeficiency virus (HIV) and sexually transmitted disease (STD) infection among MSM in North America10,19–24 and Europe.8,11,25,26 For example, MSM who seek sexual partners online tend to be more likely to report bisexual behaviors,10,27 unprotected anal intercourse,10,28 more sexual partners,29 and a history of STD infection10 when compared with those who meet one another in traditional physical spaces.
Because evidence suggests that men who seek sexual partners online are at increased risk for HIV exposure and transmission through their risk behaviors,15,18,19,23,30,31 community-based organizations (CBOs), acquired immunodeficiency syndrome (AIDS) service organizations (ASOs), and public health departments and clinics have responded by providing HIV education via MSM-oriented chat rooms. Our community--university partnership developed an intervention designed to reduce the HIV risks of men who seek male sexual partners in existing chat rooms. The intervention was known as Cyber-Based Education and Referral/Men for Men (CyBER/M4M).
Using two complementary modes of data collection, we sought to describe the characteristics of chat-room participants (“chatters”) who participated in the CyBER/M4M intervention and identify their risk behaviors and prevention needs. We also explored the intervention as it was being delivered to provide insights for designing, implementing, and evaluating future chat room-based interventions.
METHODS
CyBER/M4M was a chat room-based HIV-prevention intervention that was developed using community-based participatory research (CBPR). CBPR is an approach that ensures equitable and true participation by communities affected by the issue being studied, representatives of organizations, and researchers in all aspects of the research process.32 Much of the power and promise of CBPR comes from blending research and practice for the mutual benefit of all partners; knowledge is gained and public health practice is improved.
Briefly, a CBPR partnership of community members conceived, conducted, and evaluated CyBER/M4M. The partnership included gay men and representatives from CBOs; two ASOs; local public health departments; a local foundation supporting lesbian, gay, bisexual, and transgender health; Wake Forest University School of Medicine; and the University of North Carolina Center for AIDS Research. The history of this CBPR partnership, the application of partnership principles, and the adherence to CBPR in CyBER/M4M have been described elsewhere.5,33 The Institutional Review Board of Wake Forest University Health Sciences provided human subject review and study oversight.
Chat rooms described
An Internet chat room is a channel of synchronous dialogue between computer users connected through a network of computers. Chatters log in via the Internet to a chat-server computer that hosts a specific chat room. Chatters can type messages that are transferred almost instantaneously by the server to all of the other chatters in the public chat room. Thus, chatters are able to communicate with one another in real time from their individual computers through what is referred to as an instant message (IM). This speed differentiates chat-room discussions from asynchronous computer-mediated communications such as e-mail.
Although some chat rooms may not require registering with a login name, chat rooms designed for social and sexual networking among MSM tend to require registration. However, this registration typically requires an e-mail address (free e-mail accounts with Yahoo', Google's Gmail, and Microsoft Corp.'s Hotmail suffice) and self-reported information such as city and state, which is only available to site administrators. Because many chat rooms are free at basic membership levels, there is no need for other information such as a credit card number. Chatters also may communicate privately to one another using instant messaging, in which only the designated chatter receives the message. Private instant messaging is often used for discussions between two chatters that may include getting to know each other and determining whether to meet in person for social and/or sexual contact.
CyBER/M4M implementation
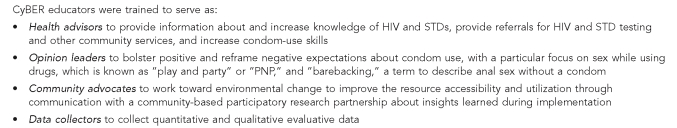
CyBER/M4M was developed as previously described33 and implemented in northwestern North Carolina within a catchment area of more than 1.3 million people. The intervention took place for 18 months in 2004 and 2005. Two interventionists were recruited and trained to enter local chat rooms. The interventionists self-identified as gay; one was African American and aged 28 years and the other was white and aged 24 years. Both were knowledgeable about local MSM communities, including self-identifying gay men and MSM who have female partners. During their 16-hour training, the interventionists, known as CyBER educators, were trained to serve as health advisors, opinion leaders, community advocates, and data collectors. Figure 1 provides an expanded description of their roles and responsibilities. The training and the online intervention protocol were based in social cognitive theory34 and empowerment education,35 as described previously in the literature.33
Figure 1.
Roles and responsibilities of CyBER educators, Cyber-Based Education and Referral/Men for Men intervention, North Carolina, 2004–2005
CyBER = Cyber-Based Education and Referral
HIV = human immunodeficiency virus
STD = sexually transmitted disease
Each CyBER educator entered one of five predetermined chat rooms. These rooms were geographically oriented and known to facilitate in-person social and sexual networking among MSM in northwestern North Carolina. For chatters who are using the chat room to facilitate in-person social and sexual networking, a room must be able to connect them with others who are within a reasonable distance; thus, many hosts of chat rooms organize their rooms by metropolitan area or locality, for example. Because the intervention included referrals to local resources, members of the CBPR partnership knew many and identified other local resources, within the primary catchment area of the chat room, to which the CyBER educators could make referrals.
In the chat room, the CyBER educator followed a standard protocol, announcing his purpose and availability to answer questions and provide education about HIV and AIDS through periodic messages in the public chat room. Messages included: “In the room to answer questions about HIV and AIDS”; “I can answer questions about HIV and AIDS”; “Want to get tested for HIV? IM me. I can help”; and “Need condoms? IM me. I can tell you where to get them free.” According to protocol, only after a chatter privately messaged the educator did the educator respond privately. The intervention was delivered in random two-hour shifts, averaging six to 12 hours a week.
Data collection and measurement
Adhering to CBPR principles, all partners were equitably involved in each phase of this study, including proposal and intervention development, measurement selection, data collection and analysis, and interpretation of findings.32 Both quantitative and qualitative data were collected.
Quantitative data.
After communicating with a chatter according to protocol, the CyBER educator provided a password and Web address and encouraged him to complete an online assessment. The chatter completed an online consent form and the assessment, which were visually and functionally similar to a paper assessment. A common gateway interface (CGI) script was used for automatic compilation and exportation of data into SPSS®.36 Upon completion of the assessment, the chatter could download a $5 gift certificate.
The self-administered online assessment comprised 36 items, which elicited self-reports using predefined response options with binary, categorical, or Likert-scale response options. Demographic characteristics assessed included age in years, gender, educational attainment, medical insurance, estimated annual income, and sexual orientation. Behaviors assessed included sex with men and women; number of sexual partners; engagement in oral sex and receptive-anal and insertive-anal intercourse; condom use during oral sex, receptive-anal, and insertive-anal intercourse during the past three months; and condom use with oral sex and receptive-anal and insertive-anal intercourse with men met online. The study also measured the number of hours spent during the past seven days in chat rooms designed for social and sexual networking of MSM, and assessed the chatter's history of STDs.
Chatters also were asked whether they had ever used methamphetamine (“crystal”), cocaine, crack, heroin, ecstasy, amyl nitrite (“poppers”), and drugs developed to enhance sexual satisfaction (i.e., Viagra®, Cialis®, and Levitra®). Chatters answering yes to any of these substances were also asked to estimate their frequency of use in the past 30 days of each drug. Although a final item assessed whether the chatter had completed the assessment previously, data were analyzed to identify potential duplications.
Univariate analyses were used to describe frequencies, percentages, and means of demographic and behavioral characteristics. Bivariate analyses using Chi-square tests explored key subgroup differences. SPSS 11.5 was used for the analyses.36
Qualitative data.
Qualitative transcript data were collected to document the public chat room and the private IM discussions between a chatter and the CyBER educator. The transcripts were copied and imported into Microsoft Word, where they were prepared for analysis using NVivo qualitative research software.37 Grounded theory, which relies on an inductive approach to data analysis, was used. This approach focused on building understanding grounded in real-world patterns found within the chat room during intervention implementation.38
A multistage, inductive, interpretative thematic process was used by three coders to identify codes, create a data dictionary, assign agreed-upon codes to relevant text, and begin the process of developing and interpreting themes. These themes were presented to the CBPR partnership for refinement and interpretation during five iterative discussions.
RESULTS
Quantitative findings
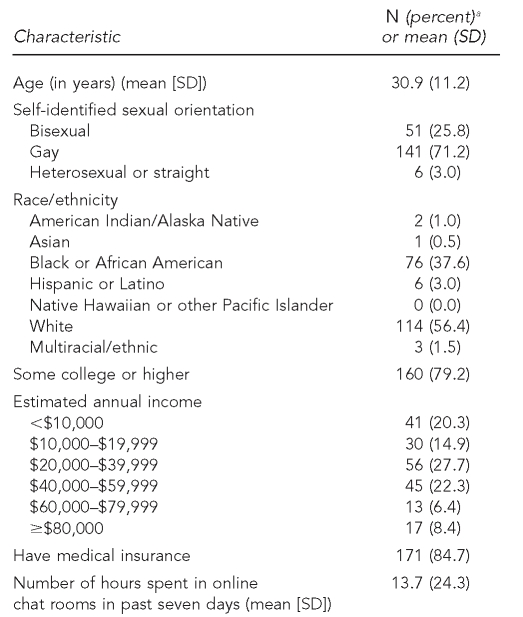
Up to 100 chatters were in public chat rooms at any given time during the intervention implementation. These chatters may have attended to what was happening in the public chat room, but chose not to actively engage through IMs. However, the CyBER educators had extended interactions through private IMs with 1,851 chatters, and of these, 210 completed the online assessment. During each two-hour block of intervention implementation, the educator interacted with an average of 11 chatters through private IMs. Table 1 illustrates the demographic characteristics of the chatters who interacted with the CyBER educators and completed the online assessment.
Table 1.
Demographic characteristics of chatters who interacted with CyBER educators and completed the online assessment (n=210), Cyber-Based Education and Referral/Men for Men intervention, North Carolina, 2004–2005
aPercentages based on number of chatters who answered the question
CyBER = Cyber-Based Education and Referral
SD = standard deviation
The mean age of chatters was 30.9 years (±11.2) with a range of 18–61 years. Although the majority self-identified as gay, one-quarter self-identified as bisexual. More than half self-identified as white, while one-third self-identified as black or African American. The mean number of hours chatters spent in chat rooms during the past seven days was 13.7 hours (±24.3).
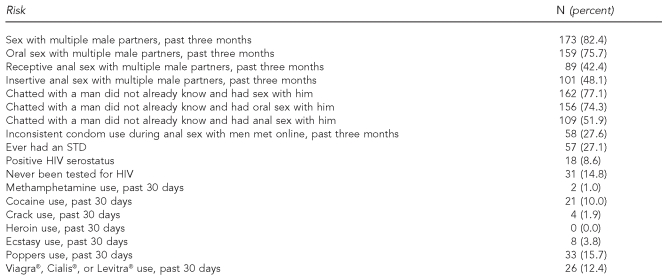
Table 2 illustrates the risk behaviors of chatters. More than 80.0% of chatters reported having had multiple male sex partners during the past three months, more than 70.0% reported having chatted with a man they did not already know and having oral sex with him, and more than half reported having chatted with a man they did not already know and having anal sex with him.
Table 2.
Risk behaviors of chatters who interacted with CyBER educators and completed the online assessment (n=210), Cyber-Based Education and Referral/Men for Men intervention, North Carolina, 2004–2005
CyBER = Cyber-Based Education and Referral
STD = sexually transmitted disease
HIV = human immunodeficiency virus
More than a quarter of the sample (27.6%) reported inconsistent condom use during anal sex with a man met online during the past three months. Significant differences in condom use were found among subgroups of chatters; 77.7% of HIV-positive chatters and 25.9% of HIV-negative chatters reported inconsistent condom use during anal sex with a man met online during the past three months (p=0.001).
Furthermore, 14.8% of the sample reported never having been tested for HIV. Of those who had never been tested for HIV, 71.4% reported inconsistent condom use during anal sex with a man met online during the past three months, while among those who reported having been tested, 31.9% reported inconsistent condom use during anal sex with a man met online during the past three months (p=0.009).
One quarter of the sample (n=52) reported any type of illicit drug use during the past 30 days; and 12.4% of the sample (n=26) reported using drugs to enhance sexual satisfaction (i.e., Viagra, Cialis, and Levitra) during the past 30 days.
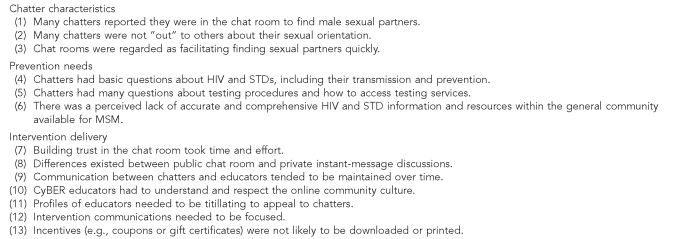
Qualitative findings
Qualitative data analysis of chat-room transcripts identified 13 thematic categories related to chatter characteristics, prevention needs, and intervention delivery, as presented in Figure 2.
Figure 2.
Qualitative thematic categories related to chatter characteristics, prevention needs, and intervention delivery, Cyber-Based Education and Referral/Men for Men intervention, North Carolina, 2004–2005
HIV = human immunodeficiency virus
STD = sexually transmitted disease
MSM = men who have sex with men
CyBER = Cyber-Based Education and Referral
Chatter characteristics.
First, many chatters reported being in the chat room in search of male sexual partners. Chatters reported that they were “only on[line] to find sex,” “looking for a quickie,” “wanting release,” and “looking for sex now'”
Second, many chatters reported that they were not open or “out” about their sexual orientation. Many reported being married, bisexual, and/or uncomfortable with others knowing about their same-sex behavior. As a chatter reported, “I can't let others know what I am looking for.” Chatters also indicated that the chat room served as an efficient and fast mode of finding sexual partners. As a chatter reported, “When you have an hour at lunch, where else are you going to go to find a dude and get off [have sex]?”
Prevention needs.
Chatters had basic questions about HIV and STDs and their prevention. The CyBER educators clarified how HIV is transmitted and how condoms should be used. They also answered questions about signs and symptoms, transmission, and treatment of STDs besides HIV, including syphilis, chlamydia, and human papillomavirus.
Chatters had questions about testing procedures and how to access local testing services. The CyBER educators offered information about how to access local testing options for HIV and STDs. They explained the testing process, how to make appointments, what bus to take or where to park, and whom to ask for at the testing site.
Chatters also reported a lack of accurate and comprehensive HIV and STD information and resources within the general community available for men. Statements that reflected the lack of local information and resources included: “No one is talking about HIV anymore,” “It is only a problem in Africa,” “I don't know where to get AIDS info around here,” and “No place exists for men like me to get answers I want.”
Intervention delivery.
Seven themes were identified that provided insight into delivery of online interventions in general and the CyBER/M4M intervention in particular. First, the CyBER educators had to prove they were open and nonjudgmental to build trust within the chat rooms. This took time and effort because this had to be done through text; trust could not be built through body language or eye contact. Rather, it was completed through consistent participation in the chat room and careful wording of IMs.
Furthermore, discussions in the public chat rooms tended to be less personal than discussions during private IMs in which chatters disclosed more detailed information about their own risks and worries to the CyBER educator. Interestingly, no differences were found in the frequency of actual chats with the educator and the disclosure of sensitive information. The CyBER educator would receive private IMs initiated by chatters with whom they had not communicated previously; often these messages included sensitive questions about risks and behaviors. Thus, the CyBER educators' regular presence in the public chat room may have been the key to their success in private IMs with chatters about sensitive topics, whether they had interacted previously or not.
Because the chat rooms tended to function like a physical space (e.g., a bar or a gym), chatters tended to communicate with the CyBER educators over time; some communicated more consistently, some communicated less consistently, but most chatters who interacted with the educators maintained at least sporadic communication over time.
Similarly, CyBER educators had to understand and respect the online community and culture. They were more successful when they were flirtatious and engaged in public chat-room discussions that were not focused on HIV. For example, they talked about movies, the opening of a gay club, and what the chatter was looking for online in terms of a sexual partner.
The profiles of the CyBER educators needed to be titillating to attract the interest of those within the chat rooms. These profiles were developed after initial implementation based on feedback from the CyBER educators to the CBPR partnership. The profiles were not deceptive; they were designed to accurately portray the purposes of the educators. Stock photos (not head shots) were used that were interesting but not revealing; for example, one CyBER educator used a chest photo. It was later determined that multiple profiles designed to appeal to different types of chatters might be beneficial as well.
Furthermore, intervention communications were most successful if they were focused. The online communication process required messages to be simple and concise. Examples included locations chatters could access testing, get free condoms, and find more information online or in the local community.
Chatters were not likely to download gift certificates or coupons. Many chatters reported not having printers, ink, and/or paper available, or feeling uncomfortable about printing anything that documented their presence in a chat room.
DISCUSSION
Several findings from this study should be highlighted. First, the interventionists, known as CyBER educators, interacted with more than 1,800 chatters during the implementation period. These interactions were private discussions facilitated through ongoing back-and-forth IMs between the educator and the chatter. However, the educators reached and may have impacted many more chatters through their messages to public chat rooms because all chatters can see messages in the public chat rooms whether or not they choose to participate in private IMs.
Many MSM reported using chat rooms to find sexual partners. Three out of four chatters who completed the assessment reported having chatted with a man they did not already know and having sex with him. Furthermore, a substantial proportion of chatters who completed the online assessment self-identified as bisexual. Post-hoc analyses to compare HIV testing rates by sexual identity found that those who self--identified as bisexual were significantly more likely to have never been tested for HIV: 60.1% of chatters who self-identified as bisexual (n=31) compared with 11.3% of those who self-identified as gay (n=16) reported never having been tested for HIV (p=0.002). This finding is particularly important because these chatters may be putting both their male and female sexual partners at risk for HIV and STDs.
Furthermore, 27.1% of chatters who completed the assessment reported ever having had an STD. This finding supports current Centers for Disease Control and Prevention recommendations that promote annual HIV and STD screening for MSM.39 Online promotion of this recommendation coupled with increased access to (and guidance on how to access) screening may reduce infection rates among MSM.
Review of the chat-room transcripts also indicated that many chatters were not open to informing others about their orientation, had informational needs, and lacked knowledge of resources for HIV testing. Chat-room transcripts also indicated that implementing such an intervention was feasible but took time and effort to build trust, appeal to chatters, and tailor focused messages to individuals and groups.
Limitations
A CBPR partnership designed these analyses to explore the implementation of an intervention that utilized emerging technology. Further research using longitudinal or prospective cross-sectional designs will be necessary to test more rigorously whether such interventions can impact the behavioral mediators and outcomes of chatters. Second, although this study reached a large number of chatters, only a small percentage of those with whom the CyBER educator interacted agreed to complete the online assessment. This weakness is understandable given that chat rooms are used for rapid and efficient networking communications. Our CBPR partnership developed the assessment to be short; however, other methods of evaluation could include a more condensed assessment or assessment of chatters through limited number of items within the chat room. Because of the success CyBER educators had in engaging chatters in discussions, the latter approach may be more promising.
The generalizability of these findings to other populations of MSM is unclear. However, these data provide unique insights into the potentials to harness Internet chat rooms and reach a population disproportionately affected by HIV infection rates.
CONCLUSIONS
Although research has suggested that MSM who use chat rooms may be at greater risk for HIV and other STDs, it is important to recognize the positive aspects of chat rooms. For example, chat rooms have been found to offer important resources for “coming out” and referrals and nonsexual support for isolated -populations or youth.13,15,18,40 Thus, Internet chat rooms should be viewed as a community resource and, based on our experiences with CyBER/M4M, a potentially effective mode to deliver tailored, theoretically sound, and culturally appropriate interventions to communities that may be missed by other interventions. Currently, our CBPR partnership is testing another chat room-based intervention that is focused on promoting HIV testing among online MSM. The intervention, known as CyBER/testing, is based on social cognitive theory with lay health advisors using the ask-advise-assess-assist-arrange models.41
As the HIV epidemic evolves, so must prevention efforts. To improve health and well-being among vulnerable communities, especially those disproportionately affected by the HIV epidemic such as MSM, we must act creatively. Developing new community partnerships, utilizing mixed frameworks, and using existing community resources and social structures, such as Internet chat rooms, text messaging, and Twitter, may have potential to improve health by reducing infection and re-infection rates, increasing testing rates, and initiating early access to treatment for those with HIV. Further research is clearly needed, and this study provides initial guidance and insight into the development, implementation, and evaluation of a chat room-based HIV-prevention intervention.
Footnotes
This study was funded by a grant to Dr. Rhodes from the University of North Carolina Center for AIDS Research, a National Institutes of Health-funded program, #P30A150410. This study also was supported by a grant to Dr. Rhodes from the National Institute of Mental Health, #R21082689.
REFERENCES
- 1.Lorence DP, Park H, Fox S. Racial disparities in health information access: resilience of the Digital Divide. J Med Syst. 2006;30:241–9. doi: 10.1007/s10916-005-9003-y. [DOI] [PubMed] [Google Scholar]
- 2.Madden M. Internet penetration and impact. Washington: Pew Internet – American Life Project; 2006. [Google Scholar]
- 3.Minkler M, Wallerstein N. Improving health through community organization and community building: a health education perspective. In: Minkler M, editor. Community organizing and community building for health. New Brunswick (NJ): Rutgers University Press; 1997. pp. 30–52. [Google Scholar]
- 4.Nartz M, Schoech D. Use of the Internet for community practice: a Delphi study. J Community Pract. 2000;8:37–59. [Google Scholar]
- 5.Rhodes SD, Hergenrather KC, Yee LJ, Ramsey B. Comparing MSM in the southeastern United States who participated in an HIV prevention chat room-based outreach intervention and those who did not: how different are the baseline HIV-risk profiles? Health Educ Res. 2008;23:180–90. doi: 10.1093/her/cym015. [DOI] [PubMed] [Google Scholar]
- 6.Bernhardt JM. Health education and the digital divide: building bridges and filling chasms. Health Educ Res. 2000;15:527–31. doi: 10.1093/her/15.5.527. [DOI] [PubMed] [Google Scholar]
- 7.Whaley KC. America's digital divide: 2000–2003 trends. J Med Syst. 2004;28:183–95. doi: 10.1023/b:joms.0000023301.09308.d9. [DOI] [PubMed] [Google Scholar]
- 8.Hospers HJ, Harterink P, Van Den Hoek K, Veenstra J. Chatters on the Internet: a special target group for HIV prevention. AIDS Care. 2002;14:539–44. doi: 10.1080/09540120208629671. [DOI] [PubMed] [Google Scholar]
- 9.Koch NS, Schockman HE. Democratizing Internet access in the lesbian, gay, and bisexual communities. In: Ebo B, editor. Cyberghetto or cybertopia? Race, class and gender on the Internet. Westport (CT): Praeger Publishers; 1998. pp. p. 171–84. [Google Scholar]
- 10.Rhodes SD, DiClemente RJ, Cecil H, Hergenrather KC, Yee LJ. Risk among men who have sex with men in the United States: a comparison of an Internet sample and a conventional outreach sample. AIDS Educ Prev. 2002;14:41–50. doi: 10.1521/aeap.14.1.41.24334. [DOI] [PubMed] [Google Scholar]
- 11.Ross MW, Tikkanen R, Mansson SA. Differences between Internet samples and conventional samples of men who have sex with men: implications for research and HIV interventions. Soc Sci Med. 2000;51:749–58. doi: 10.1016/s0277-9536(99)00493-1. [DOI] [PubMed] [Google Scholar]
- 12.Fields SD, Wharton MJ, Marrero AI, Little A, Pannell K, Morgan JH. Internet chat rooms: connecting with a new generation of young men of color at risk for HIV infection who have sex with other men. J Assoc Nurses AIDS Care. 2006;17:53–60. doi: 10.1016/j.jana.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 13.Horvath KJ, Bowen AM, Williams ML. Virtual and physical venues as contexts for HIV risk among rural men who have sex with men. Health Psychol. 2006;25:237–42. doi: 10.1037/0278-6133.25.2.237. [DOI] [PubMed] [Google Scholar]
- 14.Rhodes SD, Bowie DA, Hergenrather KC. Collecting behavioural data using the World Wide Web: considerations for researchers. J Epidemiol Community Health. 2003;57:68–73. doi: 10.1136/jech.57.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bolding G, Davis M, Sherr L, Hart G, Elford J. Use of gay Internet sites and views about online health promotion among men who have sex with men. AIDS Care. 2004;16:993–1001. doi: 10.1080/09540120412331292453. [DOI] [PubMed] [Google Scholar]
- 16.Chiasson MA, Parsons JT, Tesoriero JM, Carballo-Dieguez A, Hirsh-field S, Remien RH. HIV behavioral research online. J Urban Health. 2006;83:73–85. doi: 10.1007/s11524-005-9008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Macias W, Lewis LS, Smith TL. Health-related message boards/chat rooms on the Web: discussion content and implications for pharmaceutical sponsorships. J Health Commun. 2005;10:209–23. doi: 10.1080/10810730590934235. [DOI] [PubMed] [Google Scholar]
- 18.Rhodes SD. Hookups or health promotion? An exploratory study of a chat room-based HIV prevention intervention for men who have sex with men. AIDS Educ Prev. 2004;16:315–27. doi: 10.1521/aeap.16.4.315.40399. [DOI] [PubMed] [Google Scholar]
- 19.Benotsch EG, Kalichman S, Cage M. Men who have met sex partners via the Internet: prevalence, predictors, and implications for HIV prevention. Arch Sex Behav. 2002;31:177–83. doi: 10.1023/a:1014739203657. [DOI] [PubMed] [Google Scholar]
- 20.Bull SS, McFarlane M. Soliciting sex on the Internet: what are the risks for sexually transmitted diseases and HIV? Sex Transm Dis. 2000;27:545–50. doi: 10.1097/00007435-200010000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Chiasson MA, Hirshfield S, Remien RH, Humberstone M, Wong T, Wolitski RJ. A comparison of on-line and off-line sexual risk in men who have sex with men: an event-based on-line survey. J Acquir Immune Defic Syndr. 2007;44:235–43. doi: 10.1097/QAI.0b013e31802e298c. [DOI] [PubMed] [Google Scholar]
- 22.Klausner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. JAMA. 2000;284:447–9. doi: 10.1001/jama.284.4.447. [DOI] [PubMed] [Google Scholar]
- 23.McFarlane M, Bull SS, Rietmeijer CA. The Internet as a newly emerging risk environment for sexually transmitted diseases. JAMA. 2000;284:443–6. doi: 10.1001/jama.284.4.443. [DOI] [PubMed] [Google Scholar]
- 24.Rietmeijer CA, Bull SS, McFarlane M. Sex and the Internet. AIDS. 2001;15:1433–4. doi: 10.1097/00002030-200107270-00013. [DOI] [PubMed] [Google Scholar]
- 25.Elford J, Bolding G, Sherr L. Seeking sex on the Internet and sexual risk behaviour among gay men using London gyms. AIDS. 2001;15:1409–15. doi: 10.1097/00002030-200107270-00010. [DOI] [PubMed] [Google Scholar]
- 26.Tikkanen R, Ross MW. Technological tearoom trade: characteristics of Swedish men visiting gay Internet chat rooms. AIDS Educ Prev. 2003;15:122–32. doi: 10.1521/aeap.15.3.122.23833. [DOI] [PubMed] [Google Scholar]
- 27.Elford J, Bolding G, Davis M, Sherr L, Hart G. Web-based behavioral surveillance among men who have sex with men: a comparison of online and offline samples in London, UK. J Acquir Immune Defic Syndr. 2004;35:421–6. doi: 10.1097/00126334-200404010-00012. [DOI] [PubMed] [Google Scholar]
- 28.Garofalo R, Herrick A, Mustanski BS, Donenberg GR. Tip of the iceberg: young men who have sex with men, the Internet, and HIV risk. Am J Public Health. 2007;97:1113–7. doi: 10.2105/AJPH.2005.075630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ogilvie GS, Taylor DL, Trussler T, Marchand R, Gilbert M, Moniruzzaman A, et al. Seeking sexual partners on the Internet: a marker for risky sexual behaviour in men who have sex with men. Can J Public Health. 2008;99:185–8. doi: 10.1007/BF03405470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bull SS, McFarlane M, Lloyd L, Rietmeijer C. The process of seeking sex partners online and implications for STD/HIV prevention. AIDS Care. 2004;16:1012–20. doi: 10.1080/09540120412331292426. [DOI] [PubMed] [Google Scholar]
- 31.Hospers HJ, Kok G, Harterink P, de Zwart O. A new meeting place: chatting on the Internet, e-dating and sexual risk behaviour among Dutch men who have sex with men. AIDS. 2005;19:1097–101. doi: 10.1097/01.aids.0000174457.08992.62. [DOI] [PubMed] [Google Scholar]
- 32.Cashman SB, Adeky S, Allen AJ, 3rd, Corburn J, Israel BA, Montano J, et al. The power and the promise: working with communities to analyze data, interpret findings, and get to outcomes. Am J Public Health. 2008;98:1407–17. doi: 10.2105/AJPH.2007.113571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rhodes SD, Hergenrather KC, Duncan J, Ramsey B, Yee LJ, Wilkin AM. Using community-based participatory research to develop a chat room-based HIV prevention intervention for gay men. Progress in Community Health Partnerships: Research, Education, and Action. 2007;1:175–84. doi: 10.1353/cpr.2007.0013. [DOI] [PubMed] [Google Scholar]
- 34.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs (NJ): Prentice-Hall; 1986. [Google Scholar]
- 35.Freire P. Education for critical consciousness. New York: Seabury Press; 1973. [Google Scholar]
- 36.SPSS Inc. SPSS®: Version 11.5. Chicago: SPSS Inc.; 2002. [Google Scholar]
- 37.QSR International Inc. NVivo: Version 3. Cambridge (MA): QSR International (Americas) Inc.; 2003. [Google Scholar]
- 38.Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Chicago: Aldine; 1967. [Google Scholar]
- 39.Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep. 2002;51(RR-6):1–78. [PubMed] [Google Scholar]
- 40.Hallett J, Brown G, Maycock B, Langdon P. Changing communities, changing spaces: the challenges of health promotion outreach in cyberspace. Promot Educ. 2007;14:150–4. [PubMed] [Google Scholar]
- 41.Goldstein MG, DePue J, Kazura AN. Models of provider-patient interaction and shared decision making. In: Shumaker SA, Ockene JK, Riekert KA, editors. The handbook of health behavior change. 3rd ed. New York: Springer; 2009. pp. p. 107–25. [Google Scholar]