SYNOPSIS
Objectives
Many youth begin human immunodeficiency virus (HIV) sexual risk behaviors in preadolescence, yet risk-reduction programs are typically implemented in middle or late adolescence, missing an important window for prevention. Parent-based programming may play an important role in reaching youth early with prevention messages. One such program is the Parents Matter! Program (PMP), a five-session theory- and evidence-based intervention for parents of children aged 9 to 12 years. A randomized controlled trial showed PMP to be efficacious in promoting effective parent-child communication about sexuality and sexual risk reduction. We assessed the feasibility and acceptability of PMP when implemented under typical programmatic circumstances in communities at high risk for HIV infection.
Methods
We selected 15 sites (including health departments, local education agencies, community-based organizations, and faith-based organizations) throughout the U.S. and Puerto Rico to participate in delivering PMP. Sites were provided training, program materials, and ongoing technical assistance. We collected multilevel data to assess the feasibility of program implementation and delivery, program relevance, and satisfaction with PMP activities and materials.
Results
PMP was successfully implemented and evaluated in 13 of 15 sites; 76% of parents attended at least four of five sessions. Organization-, facilitator-, and parent-level data indicated the feasibility and acceptability of PMP, and overall high satisfaction with PMP activities and materials.
Conclusion
The results of this project demonstrate that HIV pre-risk prevention programs for parents can be implemented and embraced by a variety of community organizations in HIV at-risk communities. The time to embrace parents as partners in public health HIV-prevention efforts has come.
New incidence data on human immunodeficiency virus (HIV) from the Centers for Disease Control and Prevention (CDC) reveal that the U.S. epidemic is—and has been—worse than previously estimated, and that young African Americans are disproportionately affected.1 In addition, CDC estimates that one in four adolescent women in the general population, and one in two adolescent African American women, are infected with at least one of the most common sexually transmitted diseases (STDs), suggesting that our current sexual risk prevention efforts require new directions and additional tools.2 Furthermore, statistics compiled by the Kaiser Family Foundation3 show that only 4% of the $23 billion the U.S. government is spending this year on all HIV/acquired immunodeficiency syndrome (AIDS) activities (including research, medical care, and overseas programs) goes toward prevention. Taken together, these findings are a clarion call for new approaches to early sexual risk intervention in communities of color.
Two of CDC's primary prevention strategies for HIV in the U.S. include routine, opt-out testing for all people aged 13 to 64 years in all health-care settings,4 and implementation of evidence-based prevention interventions with high-risk youth. For example, of the 18 evidence-based interventions that met CDC's “best evidence” criteria,5 only three were for young people—all of which targeted high-risk (sexually active) or HIV-infected youth. To raise an HIV-free generation, we must shift some of our prevention efforts to address individuals at the pre-risk stage, before risk behaviors are initiated and become ingrained. The focus of these pre-risk prevention efforts would be to help young people develop and adopt safe and healthy behaviors and sexuality, not to change already existing behaviors that put them at risk for HIV. We must begin our prevention efforts well before behaviors are initiated and established.
In this article, we first examine the need for and utility of a pre-risk approach to HIV prevention and introduce the Parents Matter! Program (PMP). PMP is an innovative pre-risk HIV-prevention program for parents of children aged 9 to 12 years that has been shown through a randomized controlled trial (RCT) to be efficacious in promoting effective parent-child communication about sexuality and sexual risk reduction.6 We then use data from an operational research study of PMP collected from sites throughout the U.S. and Puerto Rico to evaluate the relevance, usefulness, and feasibility of PMP in real-world settings to help address the HIV-prevention needs of affected communities.
BACKGROUND
A pre-risk approach to HIV prevention
Research shows that it is easier to prevent risk behaviors before their onset than to change established behavioral patterns.7 This pre-risk approach has been embraced in a number of public health efforts to prevent smoking, obesity, drug use, partner violence, and vehicular accidents and deaths.8–15 In addition, research examining sexual risk outcomes has found that behavior at sexual debut is an important determinant of subsequent behavior, where condom use at first penile-vaginal intercourse is associated with a 20-fold increase in rates of continued regular condom use.16 This suggests that during the pre-risk stage, we have the opportunity not only to reduce HIV risk during the initial acts of sexual behaviors, but also to help young people establish lifelong patterns of safe, healthy sexual behaviors.
The sexual trajectories of youth begin well before onset of intercourse. Findings from the few studies that explore pre-intercourse behaviors suggest that sexual thoughts, intentions, and precoital behaviors are precursors to intercourse debut and that preadolescence is a critical moment in this trajectory when young people begin to view sexuality in a self-relevant way.17–19 For instance, 73% of sixth graders in a school-based sample of primarily African American and Hispanic young people had ever engaged in at least one precoital behavior.19 These findings suggest that preadolescence is a critical period of sexual development, and that these sexual experiences signal the beginning of a sexual trajectory toward higher-risk sexual behaviors. To effectively intervene before sexual risk behaviors take hold, we need to better understand preadolescent sexuality, and develop and implement interventions that address young people in the pre-risk phase of their sexual risk trajectory.
Behavioral data from the Youth Risk Behavior Survey indicate that African American and Latino young people are engaging in behaviors that put them at risk for HIV, and that for many, risk behaviors begin early, in preadolescence, especially for African American males (26% of in-school African American males initiated sexual intercourse prior to age 13).20 Most sexual risk-reduction interventions, however, are implemented in high school, after many young people have already begun their sexual trajectories toward sexual initiation or have already initiated sexual intercourse. These programs, which often focus on delaying the onset of sexual activity, reach young people too late. By high school, high-risk behavior patterns have often become firmly established and are not easily changed. Beginning sexual risk prevention efforts this late misses important opportunities to intervene with young people before the risk of HIV, STDs, and pregnancy becomes a reality and associated behavior patterns become entrenched.
Pre-risk prevention in practice
Although a pre-risk approach is critical to addressing the HIV/AIDS crisis in youth, it has proved to be a difficult one to implement. A great deal of controversy is associated with providing young people with sexual health and sexual risk-reduction knowledge and skills. These sometimes contentious issues have been debated in virtually all aspects of society. Some community-based organizations (CBOs) have implemented early sexual risk-prevention programs for youth. But in more far-reaching arenas such as schools, health departments, and faith-based organizations, many constraints exist, limiting our ability to reach substantial segments of young people. To implement large-scale pre-risk prevention efforts for adolescents, new approaches are needed that are politically palatable, acceptable to a wide range of values, and relevant to communities, and that can be transferred from research environments to real-world implementation in a range of venues, from small, private community organizations to large public school districts.
One type of pre-risk prevention program that meets this tall order is a program for parents to learn how to effectively communicate with their children about sexual topics and sexual risk. Parent-adolescent communication about sex is associated with decreased sexual risk-taking behavior among adolescents21–25 and is particularly effective when these discussions occur prior to sexual debut.16 Parents are in a unique position to engage their children in dialogues about sexuality-related issues early, before the initiation of sexual activity. Unlike other information sources, parent-child discussions can be continuous, building one upon the next as the child's development and experiences change, and such discussions are also time-sensitive, allowing a parent to immediately respond to the child's questions and anticipated needs rather than waiting for a programmed discussion, such as in a school curriculum. In addition, parents may be better suited to engaging in discussions that are focused on their values and beliefs about sexual behavior than other information sources. If implemented effectively and on a broad scale, this pre-risk prevention strategy has the potential to significantly impact the HIV epidemic in communities disproportionately affected by HIV.
One such parenting program—PMP26—is a parent-focused intervention CDC developed to promote positive parenting and effective parent-child communication about sexuality and sexual risk reduction for parents and guardians of children aged 9 to 12 years. PMP can address pre-risk behaviors in a noncontroversial way and help young people acquire the necessary skills to develop healthy behaviors and make positive life choices. PMP recognizes that many parents and guardians may need support to effectively convey values and expectations about sexual behavior and to communicate important HIV, STD, and pregnancy prevention messages to their children.
The conceptual framework that guides PMP is grounded in four well-tested social and behavioral theories:26 social learning theory,27 problem behavior theory,28 reasoned action theory,29 and social cognitive theory.30 The ultimate goal of PMP is to reduce sexual risk behaviors among young people, including delaying the onset of sexual debut, by giving parents and guardians tools to deliver sexuality and sexual risk reduction information to their children. PMP is delivered in five 2.5-hour sessions over a five-week period. Sessions include activities for increasing parents' awareness of the sexual risks many teens face today; encouraging general parenting practices (e.g., relationship building and monitoring) that increase the likelihood that children will not engage in risky sexual behaviors; and improving parents' ability to effectively communicate with their children about sexuality and sexual risk reduction. An RCT showed PMP to be efficacious in promoting effective parent-child communication about sexuality and sexual risk reduction at six months and one year post intervention.6 Given the low level of sexual behaviors among the preadolescent study population, we were unable to assess PMP effects on child outcomes.
Merely offering strong evidence-based HIV--prevention programs is not enough. For these programs to make an impact on the HIV epidemic, they need to actually reach parents of the most affected youth populations, and parents must buy into and attend the programs. Thus, the success lies not just in the provision of HIV-prevention programming, but also in the type of programs we offer and the way we involve and engage the target community in the process.
Often, time and resource constraints may make it difficult for parents to attend multisession interventions. This, however, was not our experience when conducting the PMP RCT.6 Demographic data collected at enrollment showed that the 378 parents eligible for the PMP intervention arm had time and resource constraints, yet, despite these constraints, 90% (n=339) attended one or more PMP intervention sessions. Of the 339 participating, 86% (n=293) attended four or more sessions, and 67% (n=227) attended all five sessions. Program participant data at post-intervention assessment (n=313–315 due to missing values) revealed that 97% (n=304) of participants had a “very positive” overall experience in the PMP. When asked, “How important do you think the information and skills covered in the Parents Matter! Program are to families like yours?” 94% (n=295) found the program information and skills “very important.” The program's high retention rates and reported relevancy suggest that if we provide programming that resonates with the needs and experiences of parents in high HIV-risk communities, it is feasible to implement such programs.
Although RCTs provide critical information on the effectiveness of prevention programs, the programs are typically implemented under ideal circumstances with extensive support from the research team. To determine how the results of our RCT translated to program implementation under typical programmatic circumstances, CDC conducted an operational research project in 15 sites throughout the U.S. and Puerto Rico. We conducted the project with CBOs and faith-based organizations, health departments, and local education agencies (LEAs) to assess their ability to implement PMP; the relevancy of the program and program materials; and the organizational, facilitator, and parental satisfaction with the program.
METHODS
Site selection
We asked implementation sites to participate based on geographic region, type of organization (LEAs, CBOs, faith-based groups, and health departments), target populations served (African American and Latino), and organizational capacity. Eligibility criteria included organizations with adequate staffing resources; adequate meeting space; access to African American and Latino families and parents of adolescents aged 9 to 12 years; a working knowledge and understanding of adolescent and child development; a history of providing services to parents and family; staff with experience facilitating parent sessions, such as trainings or parent education programs; and experience and understanding of HIV/STD issues, particularly HIV-prevention strategies. A convenience sample of 15 qualifying organizations agreed to participate and have two staff members be trained as PMP facilitators. Five LEAs (in Houston, Dallas, Georgia, California, and New York), six CBOs (in Florida, Ohio, Puerto Rico, New York, and two Washington, D.C., sites), three health departments (in North Carolina, Texas, and Utah), and one faith-based organization (in Georgia) were selected for participation. In addition to program sites, a contractor was funded to conduct the training and evaluation for this project.
Procedures and measures
We conducted facilitator training using two methods: an instructor-led training and a CD-ROM training (for more information about our findings comparing the effects of these two modes of training and fidelity of intervention delivery, contact the authors). Sites selected for instructor-led training sent two facilitators to a five-day training in Atlanta, and sites selected for CD-ROM training received materials by mail to have two facilitators conduct a self-directed training. Facilitators were asked to provide written feedback and evaluation of training materials and modalities.
Each site developed an implementation plan to deliver three rounds of the five-session intervention. Sites carefully considered the needs of their communities in planning and scheduling delivery of the program. Sites conducted onsite data collection activities, such as documenting parent participation in each session and administering surveys to the facilitators and parent participants. Study sites' training, technical assistance, and evaluation needs were supported during all phases of the study by bimonthly check-in calls from the CDC-hired contractor, monthly group conference calls (where sites could call in and talk to others implementing the program), and access to the CDC contractor at any time via telephone. Activities were conducted during a six-month period. Sites were compensated $5,000 per completed round through a contractual agreement with the CDC contractor. Sites used the money for a range of activities, such as paying facilitators, rental space, program advertisement, and parent incentives, which included food, transportation vouchers, childcare, and giveaways (e.g., a backpack full of school supplies). Each site determined how the funds were used, and if and what incentives were offered.
Evaluation data were collected at the site, organization, facilitator, and parent levels. Site data included the number of sites participating, number of rounds implemented, number of participants enrolled in the program, and number of participants attending each round.
Organization-level data were collected with key personnel using a standardized interview guide. One senior-level administrator and one person with significant involvement with planning and implementing PMP were selected from each site. Senior-level management at the site determined who would participate in the interview, based on level of project involvement. The contractor conducted the interviews by telephone following the third or final round of PMP delivery. For this article, we focused on questions related to the value and relevance of the program to the target population (“Overall, how well does PMP meet the needs of the population your organization serves?” and “What benefit and value has PMP offered your community?”) and key informants' satisfaction with the materials and plans for future use (“Overall, how satisfied are you with PMP materials?” and “Do you have plans for future PMP implementation in your community?”).
For facilitator-level evaluation data, both facilitators at a site completed a brief survey after each session on the use of PMP materials with the target audience and their perception of parent acceptance of session activities. We examined two survey items in this article: “The PMP tools (e.g., slides, posters, videos, and handouts) were effective and well received by my audience” and “The activities during this session were effective with my audience.” Responses were measured on a five-point rating scale, from 1 = strongly disagree to 5 = strongly agree.
Evaluation at the participant level came from brief surveys given to all parents who attended the final day of the program. Parents provided demographic information and responded to six questions that assessed their perceptions of how satisfied they were with the program and how useful they found the program: (1) “Did the program meet your expectations?” (yes, no, not sure); (2) “How satisfied are you with the overall program?” (from 1 = very dissatisfied to 5 = very satisfied); (3) “The program gave me information and skills to talk to my child” (yes, no, not sure); (4) “How useful was the information provided in the program?” (from 1 = not at all useful to 5 = very useful); (5) “Do you plan to use what you have learned during the program with your child?” (yes, no, not sure); and (6) “Would you recommend this program to a friend?” (yes, no, not sure). Parents also reported on the number of intervention sessions they attended.
RESULTS
Site level
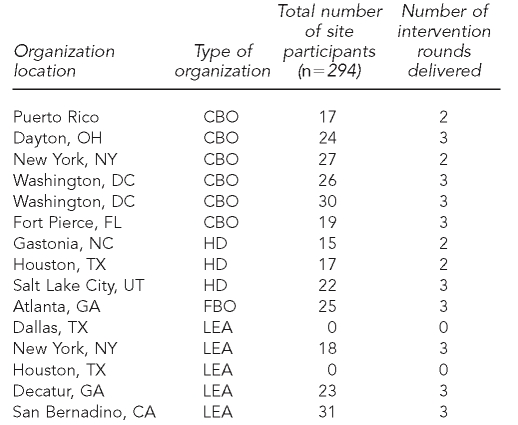
Table 1 summarizes participating organizations by location, type of organization, total number of parent participants, and number of intervention rounds delivered. Thirteen of the 15 sites provided evaluation data. One LEA site was unable to deliver PMP; due to a change in school board leadership, the site was unable to obtain new school board approval in a timely manner. Another LEA site participated in program delivery activities, but did not collect and send the survey data, and did not fully participate in the key personnel interviews. Thus, the results presented in this article are based on the remaining 13 sites. Nine sites successfully executed the program and delivered all three rounds of the PMP, and four sites (two health departments and two CBOs) were only able to complete two rounds of the program in the allocated time period. Due to contractual agreements and resource constraints, for this study, sites were required to complete delivery of three rounds of the program in a very compressed amount of time (six months). These restrictions did not mimic a real-world setting where a funded organization could offer the program on its own schedule. For some sites, the program was rolled out during late fall and winter holidays, and while some sites were able to capitalize on this time frame, for others it was a difficult time to recruit program participants.
Table 1.
Key characteristics of participating organizations in the Parents Matter! Program, 15 sites in the U.S. and Puerto Rico, 2007–2008
CBO = community-based organization
HD = health department
FBO = faith-based organization
LEA = local education agency
A total of 330 participants enrolled in the program. The mean number of participants for each round was as follows:
Round 1: mean = 7.07 (range 4–14 participants), n=13 sites
Round 2: mean = 7.15 (range 5–13 participants), n=13 sites
Round 3: mean = 7.44 (range 4–10 participants), n=9 sites
Sites employed a number of strategies to engage the target population and provide PMP at a time or in a way that met the needs of the participants. One site held informational sessions to make sure participants fully understood the nature of the program and could commit to sessions over a five-week period. Another site provided childcare and homework help, and another site delivered the program in a residential center, bringing the program to the parents.
Organization level: key informant interviews
Value to the target population.
Interviews with 26 key informants from 13 sites indicated that the organizations that implemented the program felt that PMP served their target populations well. In response to the question of how well PMP meets the needs of their population, all but one of the respondents had either a positive (38%, n=10/26) or a very positive (58%, n=15/26) response. As one respondent stated, “[PMP is] undeniably, indisputably, and overwhelmingly beneficial.” The one respondent who provided a neutral assessment stated that although the program meets some needs of the population, many of them have much greater, more basic needs, such as food and shelter, to consider. Some respondents also gave more information about how the program meets the needs of their population. One stated, “It is a great tool to encourage parents to initiate dialogue,” and another person said, “I believe this will help a lot on the target age.”
In response to the question of the benefit and value PMP offers their target population, key informant responses centered primarily on the core goals of PMP—to increase parent awareness of their preadolescent children's sexual risks and needs and to provide parents with the knowledge, comfort, skills, and confidence to effectively communicate with their children about sex. Related to increasing awareness, respondents made statements such as “[PMP] helped parents to know when to start a conversation with their kids” and “[PMP] gave them the opportunity to see themselves, to see what they can do to make things right, are they communicating effectively.” The most common response (35%, n=9/26) was that the program provided parents with the encouragement, knowledge, skills, or tools to talk to their children about sex. For instance, “[PMP] helped parents develop their communication skills” and “[PMP] offers a change in their behavior, hope, communication with the children.” Key informants also stated that the program went beyond skills development, empowering parents and giving them the comfort to discuss sex topics with their children.
PMP also seeks to encourage parents to see themselves as the sex educators of their children and use their own values to guide their discussions. These goals were represented in some key informant responses regarding the perceptions of the benefits of PMP for parents: “[PMP] offers for the first time, the opportunity for parents to become the educators for their children,” and “[PMP] informs parents that they should choose their own values when talking to kids about sex.”
Several respondents identified benefits on a broader, community level. One person stated that “[PMP] addressed an unmet need in HIV prevention,” and another observed, “Youth seeking services and HIV-related services increased.” Several key informants (19%, n=5/26), rather than providing specific benefits to participants, stated that PMP should be disseminated widely in the community. Examples include, “It's a good program—every parent should go through a program like this and start the conversation,” and “We have to saturate the community with PMP.”
Satisfaction and future plans for PMP.
When asked how satisfied they were with the PMP materials, key informants were primarily satisfied (23%, n=6/26) or very satisfied (58%, n=15/26) and used terms such as “very satisfied,” “good,” and “fabulous” in their responses. Two respondents were neutral about the materials, stating simply that “It's okay,” and “[The materials] seem complete.” One stated, “[The] evaluation was too scripted.” The remaining two participants had not looked at the materials.
Nearly half of the key informants (46%, n=12/26) stated that they had plans for future PMP implementation in their community, making statements such as, “Yes, of course,” and “The schools are asking for it.” Another 35% (n=9/26) of the respondents indicated that they would like to continue with the program, but it was contingent on other factors. Funding was of primary concern, with respondents making statements such as “We would love to [continue to implement PMP], when there is funding to continue,” and “I am trying to find funding for the program.” Another respondent stated that he or she planned to wait for the evaluation results before moving forward. The remaining five respondents were either not sure or did not have actual plans in place for future implementation.
Facilitator level: session evaluation forms
A total of 350 session evaluation forms were collected from facilitators, although data were missing for each question. A majority of the time, facilitators strongly agreed (74%, n=253/341) or agreed (25%, n=85/341) that the PMP tools were effective and well received by parents; three times (1%, n=3/341) facilitators disagreed or strongly disagreed. In nearly every instance, facilitators either strongly agreed (76%, n=257/340) or agreed (24%, n=80/340) that “The activities during this session were effective with my audience.” In the remaining three instances, facilitators were neutral (neither agreed nor disagreed).
Parent level
A total of 294 (89%) parent evaluation forms were collected from the 330 parents enrolled in the program. Retention data showed that of the 294 parent participants responding to the evaluation, 147 (50%) attended all five intervention sessions, 76 (26%) attended four sessions, and 71 (24%) attended one to three sessions.
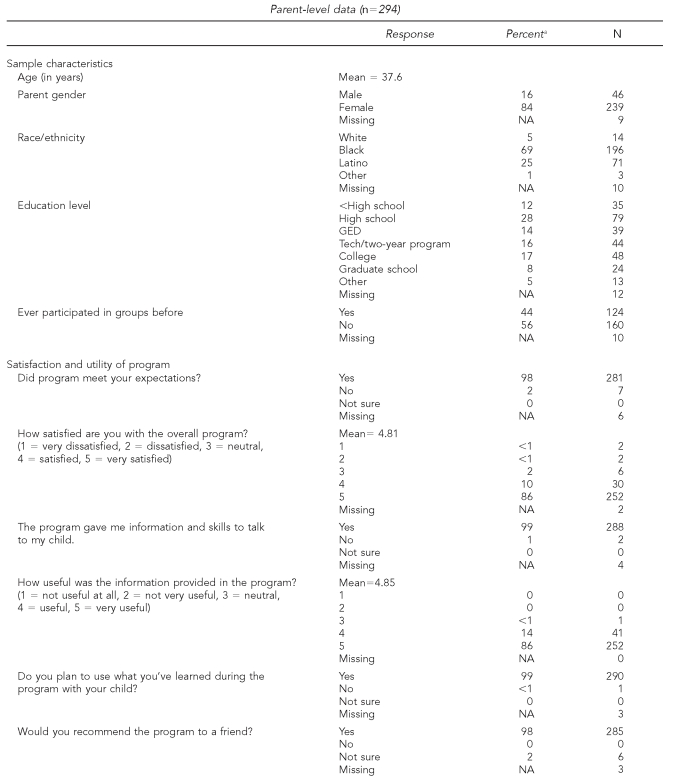
Results of the parent-level data for sample characteristics and satisfaction and usefulness of PMP are presented in Table 2. Most of the participating parents were female (84%) and either black (69%) or Latino (25%), with a mean age of 37.6 years. Forty-two percent of participants had a high school or general educational development diploma/certificate, and 44% had previously participated in parent groups. Parents were very positive about PMP. Almost all parents felt that PMP met their expectations (98%) and gave them information and skills to talk with their child (99%). Parents had a high degree of satisfaction (86% were very satisfied) and thought that the information provided in the program was very useful (86%). Almost all parents planned to use what they learned during the program with their children (>99%), and would recommend the program to a friend (98%).
Table 2.
Parent-level data: demographics and evaluation of satisfaction and usefulness of Parents Matter! Program, collected from U.S. and Puerto Rico sites, 2007–2008
aPercentages are based on the number of parents responding to the question (i.e., percentage does not include “missing”).
NA = not applicable
GED = general educational development
DISCUSSION
The results of this project demonstrate the ability to transfer an evidence-based pre-risk prevention program from a research setting to real-world community sites. Training, program materials, and technical assistance were provided to sites as they worked to implement the program in their communities in need of prevention programs. Data analyzed from site, organization, facilitator, and parent levels all demonstrate that the program is relevant, useful, and feasible. Programs such as PMP that consider the target population needs and desires and that employ practical solutions (e.g., offering programs after work hours, having programs located close to home, and offering childcare and homework help) can successfully engage parents, including those with children who may soon be at high risk for unwanted pregnancy, STDs, and HIV.
With 76% of parents attending at least four of the five sessions, it is evident that parents of children aged 9 to 12 years will attend a multisession program that promotes positive parenting and effective parent-child communication about sexuality and sexual risk reduction. Organization-level data from health departments, LEAs, CBOs, and faith-based organizations show that the program meets the needs of the organizations and target population, and that the program was well received. Many sites have current plans to move the program forward, and others will do so with additional funding and support. Facilitator- and parent-level data reveal support for the program in affected communities, high satisfaction with program materials and activities, and overall high satisfaction with the program.
Limitations
Study limitations included the need to complete delivery of three rounds of the program in a six-month time period due to contractual obligations with the CDC contractor. These restrictions did not mimic a real-world setting where a funded organization could offer the program on its own schedule. The time restriction also hampered our ability to engage additional faith-based organizations, which needed ample time to vet and clear program materials with the administrative hierarchy before they could agree to participate in a time-limited activity. Additionally, data were not collected to allow examination of participants who did not come to the final session.
CONCLUSIONS
A variety of data sources suggest the need for new strategies to address the HIV crisis in populations deeply affected by the epidemic. One noncontroversial prevention strategy is to engage parents as partners in our public health prevention efforts. Giving parents tools to parent and protect their children, and a voice to communicate about sexuality and sexual risk reduction, will help lay a strong foundation to build and grow safe and healthy sexual behaviors and decision-making in our next generations of young people.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Hall HI, Song R, Rhodes P, Prejean J, An Q, Lee LM, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–9. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Forhan SE, Gottlieb SL, Sternberg MR, Xu F, Datta D, Berman S, et al. Prevalence of sexually transmitted infections and bacterial vaginosis among female adolescents in the United States. Presented at the 2008 National STD Prevention Conference; 2008 Mar 13; Chicago. [Google Scholar]
- 3.Kaiser Family Foundation. HIV/AIDS policy fact sheet. U.S. federal funding for HIV/AIDS: the FY 2007 budget request. Menlo Park (CA): Kaiser Family Foundation; 2006. [Google Scholar]
- 4.Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–24. [PubMed] [Google Scholar]
- 5.Lyles CM, Kay LS, Crepaz N, Herbst JH, Passin WF, Kim AS, et al. Best-evidence interventions: findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000–2004. Am J Public Health. 2007;97:133–43. doi: 10.2105/AJPH.2005.076182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forehand R, Armistead L, Long N, Wyckoff SC, Kotchick BA, Whitaker D, et al. Efficacy of a parent-based sexual-risk prevention program for African American preadolescents. Arch Pediatr Adolesc Med. 2007;161:1123–9. doi: 10.1001/archpedi.161.12.1123. [DOI] [PubMed] [Google Scholar]
- 7.Botvin GJ, Baker E, Dusenbury L, Tortu S, Botvin EM. Preventing adolescent drug abuse through a multimodal cognitive--behavioral approach: results of a 3-year study. J Consult Clin Psychol. 1990;58:437–46. doi: 10.1037//0022-006x.58.4.437. [DOI] [PubMed] [Google Scholar]
- 8.Baker SP, Chen L-H, Li G. Nationwide review of graduated driver licensing. Washington: AAA Foundation for Traffic Safety; 2007. [Google Scholar]
- 9.Whitaker DJ, Morrison S, Lindquist C, Hawkins SR, O'Neil JA, Nesius AM, et al. A critical review of interventions for the primary prevention of perpetration of partner violence. Aggression and Violent Behavior. 2006;11:151–66. [Google Scholar]
- 10.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108:712–8. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 11.Curry SJ, Hollis J, Bush T, Polen M, Ludman EJ, Grothaus L, et al. A randomized trial of a family-based smoking prevention intervention in managed care. Prev Med. 2003;37(6 Pt 1):617–26. doi: 10.1016/j.ypmed.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 12.Caballero B, Clay T, Davis SM, Ethelbah B, Rock BH, Lohman T, et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78:1030–8. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lucas A, Sampson HA, editors. San Francisco: 57th Nestle Nutrition Workshop, Pediatric Program; 2006. Primary prevention by nutrition intervention in infancy and childhood. [DOI] [PubMed] [Google Scholar]
- 14.Pentz MA, Dwyer JH, MacKinnon DP, Flay BR, Hansen WB, Wang EY, et al. A multicommunity trial for primary prevention of adolescent drug abuse: effects on drug use prevalence. JAMA. 1989;261:3259–66. [PubMed] [Google Scholar]
- 15.Cohen DA, Rice JC. A parent-targeted intervention for adolescent substance use prevention: lessons learned. Evaluation Review. 1995;19:159–80. doi: 10.1177/0193841X9501900203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller KS, Levin ML, Whitaker DJ, Xu X. Patterns of condom use among adolescents: the impact of mother-adolescent communication. Am J Public Health. 1998;88:1542–4. doi: 10.2105/ajph.88.10.1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Butler TH, Miller KS, Holtgrave DR, Forehand R, Long N. Stages of sexual readiness and six-month stage progression among African American pre-teens. J Sex Res. 2006;43:378–86. doi: 10.1080/00224490609552337. [DOI] [PubMed] [Google Scholar]
- 18.O'Sullivan LF, Brooks-Gunn J. The timing of changes in girls' sexual cognitions and behaviors in early adolescence: a prospective, cohort study. J Adolesc Health. 2005;37:211–9. doi: 10.1016/j.jadohealth.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 19.O'Donnell L, Stueve A, Wilson-Simmons R, Dash K, Agronick G, JeanBaptiste V. Heterosexual risk behaviors among urban young adolescents. J Early Adolesc. 2006;26:87–109. [Google Scholar]
- 20.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, et al. Youth risk behavior surveillance—United States, 2007. MMWR Surveill Summ. 2008;57(4):1–131. [PubMed] [Google Scholar]
- 21.Karofsky PS, Zeng L, Kosorok MR. Relationship between adolescent-parental communication and initiation of first intercourse by adolescents. J Adolesc Health. 2000;28:41–5. doi: 10.1016/s1054-139x(00)00156-7. [DOI] [PubMed] [Google Scholar]
- 22.Dutra R, Miller KS, Forehand R. The process and content of sexual communication with adolescents in two-parent families: association with sexual risk-taking behavior. AIDS Behav. 1999;3:59–66. [Google Scholar]
- 23.Dittus PJ, Jaccard J, Gordon VV. Direct and nondirect communication of maternal beliefs to adolescents: adolescent motivations for premarital sexual activity. J Appl Soc Psychol. 1999;29:1927–63. [Google Scholar]
- 24.Kotchick BA, Dorsey S, Miller KS, Forehand R. Adolescent sexual risk-taking behavior in single-parent ethnic minority families. J Fam Psychol. 1999;13:93–102. [Google Scholar]
- 25.Leland N, Barth R. Characteristics of adolescents who have attempted to avoid HIV and who have communicated with parents about sex. J Adolesc Res. 1993;8:58–76. [Google Scholar]
- 26.Dittus P, Miller KS, Kotchick BA, Forehand R. Why Parents Matter!: the conceptual basis for a community-based HIV prevention program for the parents of African American youth. J Child Fam Studies. 2004;13:5–20. [Google Scholar]
- 27.Bandura A. Social learning theory. Englewood Cliffs (NJ): Prentice-Hall; 1976. [Google Scholar]
- 28.Jessor R, Jessor SL. Problem behavior and psychosocial development: a longitudinal study of youth. New York: Academic Press; 1977. [Google Scholar]
- 29.Fishbein M, Ajzen I. Belief, attitude, intention and behavior: an introduction to theory and research. Reading (MA): Addison-Wesley; 1975. [Google Scholar]
- 30.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs (NJ): Prentice-Hall; 1986. [Google Scholar]