Abstract
The QTc interval is a complex quantitative trait and a strong prognostic indicator of cardiovascular mortality in general, healthy people. The aim of this study was to identify non-genetic factors and quantitative trait loci that govern the QTc interval in an isolated Mongolian population. We used multiple regression analysis to determine the relationship between the QTc interval and non-genetic factors including height, blood pressure, and the plasma lipid level. Whole genome linkage analyses were performed to reveal quantitative trait loci for the QTc interval with 349 microsatellite markers from 1,080 Mongolian subjects. Among many factors previously known for association with the QTc interval, age, sex, heart rate, QRS duration of electrocardiogram and systolic blood pressure were also found to have influence on the QTc interval. A genetic effect for the QTc interval was identified based on familial correlation with a heritability value of 0.31. In a whole genome linkage analysis, we identified the four potential linkage regions 7q31-34, 5q21, 4q28, and 2q36.
Keywords: electrocardiography; linkage (genetics); long QT syndrome; quantitative trait, heritable; quantitative trait loci; regression analysis
Introduction
An individual with a prolonged QTc interval is prone to ventricular arrhythmia. The QTc interval is also a strong prognostic indicator of cardiovascular mortality in patients both with and without cardiac disease (Peters et al., 1990; Algra et al., 1991; Siscovick et al., 1996). Several epidemiological studies (Schouten et al., 1991; Dekker et al., 1994, 2004; De Bruyne et al., 1999) have reported a relationship between QTc interval prolongation and increased risk of cardiovascular mortality in healthy individuals, although controversy exists (Goldberg et al., 1991).
The QTc interval is a complex quantitative trait. Many factors, both genetic and non-genetic, affect the QTc interval. The heritability of the QTc interval ranges between 0.25 and 0.40 (Russell et al., 1998; Friedlander et al., 1999; Carter et al., 2000; Newton-Cheh et al., 2005), and at least seven genes involved in the congenital long QT syndrome (LQTS) have been identified (Keating et al., 1991a; 1991b; Jiang et al., 1994; Schott et al., 1995; Wang et al., 1995; Splawski et al., 2000; Shah et al., 2005). Six of these genes encode potassium or sodium ion channel proteins. The seventh gene, the ANK2 gene, encodes the structural protein ankyrin-B. The molecular mechanisms of these rare form Mendelian diseases have been identified. However, QTc interval values in the general population can not be fully explained by these LQTS genes. Therefore, it is possible that there are other genes that regulate the QTc interval. Most previous studies focused on candidate regulation genes (Busjahn et al., 1999; Liu et al., 2002) already known as LQTS genes, but in order to identify unknown genes that regulate the QTc interval in the general population, a population-based whole genome study is necessary.
An isolated population is appropriate for identifying genes that are responsible for complex traits because such a population reduces genetic heterogeneity and environmental diversity. Also, a large extended pedigree provides much genetic information. Mongolians, especially rural people, are regionally and genetically isolated with many large extended families.
We identified genetic factors involved in the QTc interval based on familial aggregation and heritability, and conducted a genome-wide linkage analysis with 1,080 Mongolian subjects. We also evaluated the association of many non-genetic factors with the QTc interval using multiple regression analysis.
Results
Mongolian people comprise several major and many minor tribes. Table 1 shows the tribal distribution of our study participants, including three larger tribes and ten smaller ones. The Khalkha is the majority tribe in Mongolia and in our study. Table 2 shows the sex-specific mean ± SD of age, heart rate, QRS duration, and other characteristics of the study participants. The average age of our population was 29 years with females being slightly older than males. Values for heart rate, height, plasma total cholesterol, and fasting plasma glucose revealed significant differences between the two sexes.
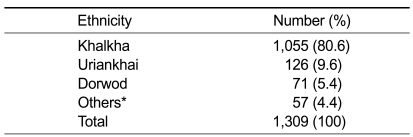
Table 1.
Ethnic composition of the study population.
*Other 10 ethinicities: Bayad, Buryat, Darhad, Hoton, Kazakh, Oold, Oros, Shanga, Tuva, and Zahchi.
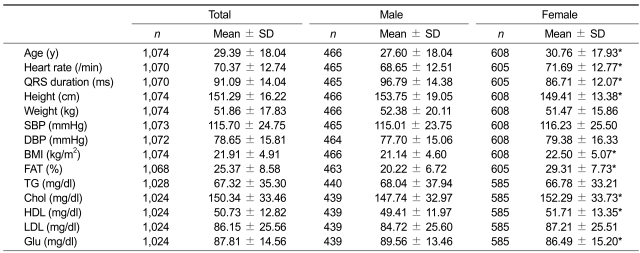
Table 2.
Characteristics of subjects.
SBP, systolic blood pressure; DBP, diastolic blood pressure; BMI, body mass index; Chol, plasma total cholesterol; HDL, HDL-cholesterol; LDL, LDL-cholesterol; TG, fasting plasma triglycerides; Glu, fasting plasma glucose. *significant difference by sex P < .05.
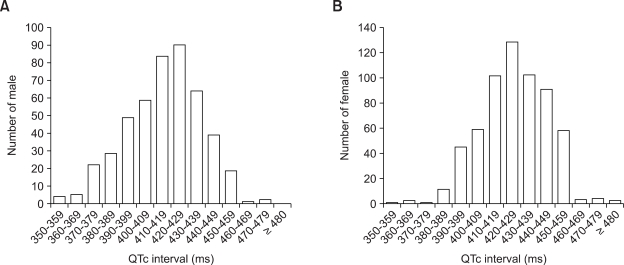
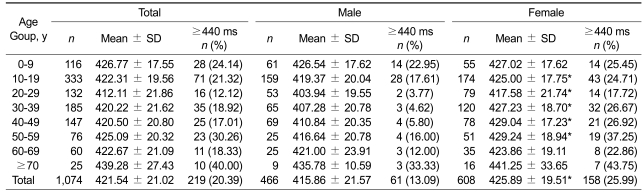
The QTc interval exhibited a normal distribution within each sex group (Figure 1). The mean QTc interval was 421.54 ms in total, 415.86 ms in males, and 425.89 ms in females. The mean QTc interval for females was significantly longer than for males (P < 0.0001). As seen in Table 3, the QTc interval decreased with age until the twenties, and then increased afterward. The difference in the QTc interval between females and males was significant for ages between the teens to the fifties (asterisks, P < 0.05), but not for ages < 10 or ≥ 60. Table 3 also shows the age- and sex-specific distribution of abnormal QTc intervals. Generally, 440 ms is accepted as the upper limit of a normal QTc interval (Garson, 1993). Using this criterion, among 1,074 individuals (466 men and 608 women), 219 (61 men and 158 women) were classified as abnormal. The proportion of persons with an elongated QTc interval was higher in females than in males because the mean QTc interval for females was longer than for males. This pattern was observed in every age range.
Figure 1.
Distribution of the QTc interval by sex. QTc intervals for males (A) and females (B) show normal distributions within each sex group.
Table 3.
Age- and sex-specific distribution of the QTc and abnormal QTc intervals (> = 440 ms).
*Significant difference by sex P < .05.
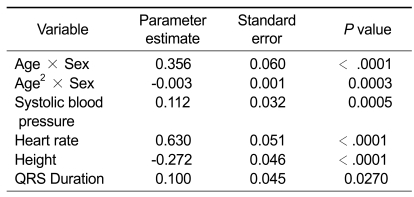
Table 4 summarizes results of the multiple regression analysis using many factors that may affect the QTc interval, including age, sex, electrocardiogram findings (heart rate, QRS duration), height, weight, BMI, fat, blood pressure (systolic and diastolic), lipid (TG, total cholesterol, HDL, LDL), and fasting plasma glucose. In a univariate analysis, all of these factors showed significant association with the QTc interval (data not shown), but in a multiple regression analysis, the QTc interval was influenced only by age × sex, age2 × sex, systolic blood pressure, heart rate, height, and QRS duration.
Table 4.
Results of multiple regression analyses for the QTc interval.
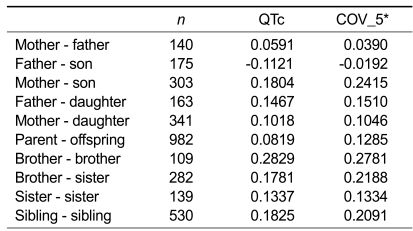
The genetic component of a phenotype can be assumed based on familial aggregation and heritability. Based on results of the familial correlation study (Table 5), among the main types of familial relationships (spouse-spouse, parent-offspring, and sibling-sibling), the sibling-sibling pair showed the most significant correlation and the spouse-spouse pair showed the least correlation, implying a genetic effect for the QTc interval.
Table 5.
Familial correlations for the QTc interval.
*Adjusted for age, sex, age2, age × sex and age2 × sex.
The heritability of the QTc interval, adjusted for age and sex, was 0.31, suggesting a moderate genetic effect. A heritability estimate of 0.31 for the adjusted QTc interval indicates that 31% of the inter-individual variance in the QTc interval duration is attributable to additive genetic effects.
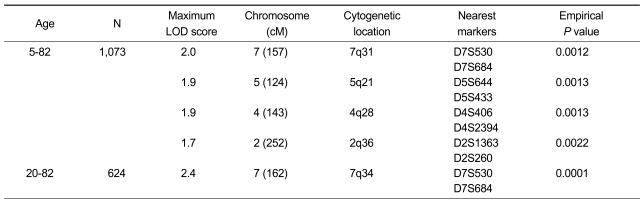
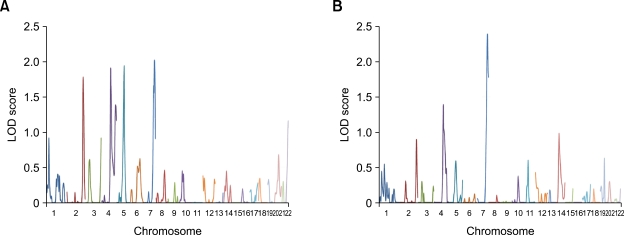
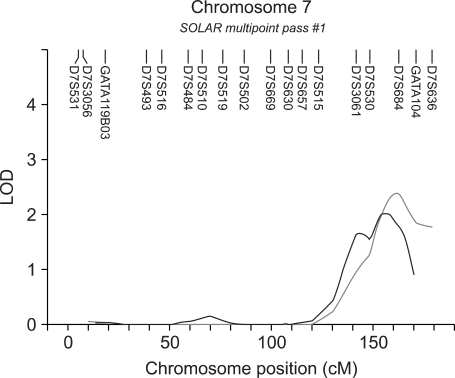
Table 6 and Figure 2 show results of a genome-wide multipoint linkage analysis of the QTc interval using the variance component method in SOLAR across 22 autosomes. Age and sex were used as covariates in this analysis. The highest LOD score was 2.0 for the chromosome 7q31 region (Figure 2 and 3). The second and third peaks represent chromosomes 5q21 and 4q28, where the maximum LOD scores were 1.9 for both peaks. An additional narrow peak was identified for chromosome 2q36 with a maximum LOD score of 1.7.
Table 6.
Results of linkage analyses for the QTc interval.
Figure 2.
Results of a multipoint linkage analysis across 22 autosomes for the all ages group (A) and the adult age group (B). The horizontal line (x axis) shows 22 autosomes sequentially. The vertical line (y axis) shows multipoint LOD scores.
Figure 3.
Results of the multipoint linkage analysis for chromosome 7. The highest peak is on chromosome 7 (maximum LOD score 2.0 in black; 2.4 in gray). The x axis shows the genetic position on chromosome 7 and the y axis shows the multipoint LOD score. The upper part is the position of the markers. Black : all age group; Gray : adult group (≥ 20 yr).
Discussion
Although QTc interval values for various populations have been reported, most studies have been performed with Westerners and there is scant information for Asians. Racial differences in the QTc interval have been reported (Vitelli et al., 1998; Grandinetti et al., 2005); The QTc interval is longer in Asians than in Caucasians, and longer in Caucasians than in African-Americans. However, our results show the mean QTc interval values in males and females are 415.82 and 425.91, respectively, and the proportion of prolonged QTc intervals is 13.09% in males and 25.99% in females. This is similar to results in other studies (Friedlander et al., 1999; Crow et al., 2003; Benoit et al., 2005). However, direct comparison is impossible because there are differences in study design and population composition. Several studies have reported on the heritability of the QTc interval with results ranging from 0.25 to 0.40 (Russell et al., 1998; Friedlander et al., 1999; Carter et al., 2000; Newton-Cheh et al., 2005). Our heritability value of 0.31 is comparable.
As seen in Table 3, the QTc interval increases with age in adults. Although well known, the mechanism of this increase is not known (Reardon and Malik, 1996; Mangoni et al., 2003). The difference in the QTc interval by sex is significant only in middle age (aged 10-59) and may be a hormonal effect.
Many factors are known to be associated with the QTc interval, including age and sex, which are well known, and heart rate, height, weight, blood pressure (systolic and diastolic), lipid (TG, total cholesterol, HDL, LDL), fasting plasma glucose, which are controversial (Dekker et al., 1994, 2004; De Bruyne et al., 1999; Mangoni et al., 2003; Benoit et al., 2005). Our results showed that weight, BMI, fat, diastolic blood pressure, lipid (TG, total cholesterol, HDL, LDL), and fasting plasma glucose are not statistically meaningful in a multiple regression analysis, suggesting these factors do not independently affect the QTc interval.
Familial correlation analysis was performed to evaluate genetic effects in the variation of the QTc interval. In this analysis, correlation of the phenotype in parent-offspring pairs and sibling-sibling pairs reflects both the familial and environmental effects, and spouse-spouse pairs reflect an environmental effect because parent-offspring pairs and sibling-sibling pairs share genetic and environmental factors while spouse-spouse pairs share only environmental factors. Therefore, our results indicate a genetic effect on the QTc interval.
Correlation in mother-son pairs is stronger than in father-son pairs, and correlation in brother-brother pairs is stronger than in sister-sister pairs. Hong et al. (2001) found similar results and suggested they are due to mitochondrial and/or pre-natal effects. However, we think it could be an X-chromosomal effect because a son has only one X chromosome, from his mother. Father and son do not share an X chromosome while mother and son always share one. Similarly, brother-brother pairs have a lower chance of sharing an X chromosome than sister-sister pairs. Brother-brother and sister-sister pairs have the same chances of receiving the same X chromosome from their mother, but sister-sister pairs always share one X chromosome from their father. Therefore, candidate genes could be located on the X chromosome. We did not type genetic markers on the X chromosome so this hypothesis could not be tested.
Genome-wide linkage analysis of the QTc interval in a general population was performed in one previous study (Newton-Cheh et al., 2005). Evidence was found suggestive of linkage of the QT interval 19 to 48 cM from the tip of the short arm of chromosome 3 (maximum two-point LOD score 3.00, maximum multipoint LOD score 2.71). The region of linkage contains potassium and sodium channel genes, including the SCN5A gene that has been implicated in one form of the long QT syndrome. Our linkage analysis results identified peaks on different chromosomes. The regions of the highest three peaks, on chromosomes 7q31, 5q21, and 4q28, contain ANK2 and ankyrin repeat genes. Most LQTS genes encode potassium or sodium channel proteins and one gene encodes the structural protein ankyrin-B, which is thought to anchor ion channels to the cellular membrane. Either a decrease in the potassium efflux due to a loss of function of the potassium channel or an increase in the sodium influx due to a gain of function of the sodium channel, is thought to be a mechanism of LQTS. Impairment of the ankyrin-B protein leads to deterioration of the channels and yields the same result. Therefore, we think that the ankyrin gene family is a strong candidate for control of the QTc interval.
We also performed an additional linkage analysis using only the adult population (≥ 20 years old) (Table 7, Figure 2 and 3). The maximum LOD score of the highest peak on chromosome 7 rose to 2.4 in the adult population from 2.0 in whole population, and other peaks on chromosomes 2, 4, and 5 became smaller (Figure 2). The peak on chromosome 7q34 in the adult population was located slightly closer to telomere than the previous peak in the whole population. This region contains KCND2 and KCNH2 genes that encode potassium voltage-gated channels. These potassium channel genes KCND2 and KCNH2 are also candidate control genes.
In conclusion, our study confirmed a genetic effect on the QTc interval, and identified four regions of potential linkage and candidate control genes in those regions. Several non-genetic factors affecting the QTc interval were identified. Further studies, such as linkage analyses covering the X chromosome in other populations, association studies, and biological function studies of candidate genes will elucidate details of QTc regulation. Our results can be used as a basis for future studies, and contributes to an improvement in risk assessment and treatment of ventricular arrhythmia and cardiovascular mortality.
Methods
Study population and baseline measurement
A total of 1,309 individuals from 142 families were recruited from a rural community in Selenge Province, Mongolia, as part of a GENDISCAN (GENe DIScovery for Complex traits in Asians of the Northeast) study (Gombojav et al., 2008). Study participants were members of 13 ethnic groups between 5 and 82 years of age. Basic individual information (age and sex), pedigree information, and self-reported medical histories were ascertained using questionnaires. Blood was collected from most subjects in both fasting and non-fasting states using heparin tubes. Values for total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, and glucose were measured from fasting plasma. Body weight (kg) and height (cm) were checked and the body mass index (BMI, kg/m2) was calculated using the formula BMI = body weight/(body height)2. After subjects rested for 5 minutes, the blood pressure (systolic blood pressure, SBP, and diastolic blood pressure, DBP) was measured by a physician using a standardized mercury sphygmomanometer, and the mean of 2 measurements was used in our analyses. Less informative subjects, such as members of small families, were excluded, after which 1,098 phenotyped subjects remained. The study was approved by an institutional review committee and the participants gave informed consent.
Electrocardiogram measurement
A standard 12-lead electrocardiogram (Bionet Co., LTD, Korea) was recorded from 1,074 subjects at a paper speed of 25 mm/s and a gain of 10 mm/mV and read manually by a cardiologist. The QT interval was determined as the onset of the QRS wave to the end of the T wave in lead II. The QRS duration was measured in an identical manner from the onset of the Q wave to the endpoint of the S wave. We used a corrected QT interval (QTc interval), which was the QT interval length corrected for heart rate using Bazett's formula of QTc=QT/(RR)1/2 (Bednar et al., 2001).
DNA extraction and genotyping
Leukocyte DNA was extracted from buffy coat specimens using a Gentra DNA isolation kit according to the manufacturer's protocol and we obtained at least 30 µg of high purity DNA from each subject. All subjects were genotyped for 384 short tandem repeat (STR) microsatellite markers with an average spacing interval of 10 cM (ABI co., LMS v2.5 HD10) excluding markers on the X chromosome. After PCR amplification (GeneAmp PCR System 9600), multiplex running of the PCR set was performed using internal standard DNA for high efficiency and data stability (GeneScan-500 LIZ, CEPH 1347-02, ABI Prism 3730 DNA analyzer). We then determined the size of the running results and genotypes using GeneMapper software (Applied Biosystems (ABI), ver. 3.7). A total of 317 markers remained after we excluded markers with genotyping errors. The calling rate was 99.9%. We added 13 markers in chromosomal areas where the inter-marker distance was larger than 25 cM because inclusion of these areas could reduce the power of the linkage analysis. Among the genotyping-error markers, 19 markers that had inter-marker distances larger than 15 cM were replaced with new markers. Final genotyping of 349 markers was performed in 1,080 subjects from the 1,098 phenotyped subjects.
Data analysis
Univariate analysis and multiple regression analysis were performed using SAS version 8.1 software (SAS Institute, Cary, NC). The familial correlation was analyzed using S.A.G.E. (Statistical Analysis for Genetic Epidemiology, http://darwin.cwru.edu/sage). IBD and MIBD matrices were calculated using the Loki package, a linkage analysis package using Markov chain Monte Carlo (MCMC) techniques (Heath, 1997). Loki supports estimation of IBD relationship matrices for use with variance component programs, such as SOLAR. Heritability estimates and multipoint linkage analysis were performed using a variance-component method implemented in the SOLAR (Sequential Oligogenic Linkage Analysis Routines) package (Almasy and Blangero, 1998).
Acknowledgements
This work was supported by a grant (M10305030000-08N503-00000) from the Korean Ministry of Education, Science and Technology. Some of the results of this paper were obtained using the software package S.A.G.E., which is supported by a U.S. Public Health Service Resource Grant (RR03655) from the National Center for Research Resources.
Abbreviations
- BMI
body mass index
- DBP
diastolic blood pressures
- LQTS
long QT syndrome
- SBP
systolic blood pressures
- STR
short tandem repeat
References
- 1.Algra A, Tijssen JG, Roelandt JR, Pool J, Lubsen J. QTc prolongation measured by standard 12-lead electrocardiography is an independent risk factor for sudden death due to cardiac arrest. Circulation. 1991;83:1888–1894. doi: 10.1161/01.cir.83.6.1888. [DOI] [PubMed] [Google Scholar]
- 2.Almasy L, Blangero J. Multipoint quantitative-trait linkage analysis in general pedigrees. Am J Hum Genet. 1998;62:1198–1211. doi: 10.1086/301844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bednar MM, Harrigan EP, Anziano RJ, Camm AJ, Ruskin JN. The QT interval. Prog Cardiovasc Dis. 2001;43:1–45. doi: 10.1053/pcad.2001.21469. [DOI] [PubMed] [Google Scholar]
- 4.Benoit SR, Mendelsohn AB, Nourjah P, Staffa JA, Graham DJ. Risk factors for prolonged QTc among US adults: Third National Health and Nutrition Examination Survey. Eur J Cardiovasc Prev Rehabil. 2005;12:363–368. doi: 10.1097/01.hjr.0000173110.21851.a9. [DOI] [PubMed] [Google Scholar]
- 5.Busjahn A, Knoblauch H, Faulhaber HD, Boeckel T, Rosenthal M, Uhlmann R, Hoehe M, Schuster H, Luft FC. QT interval is linked to 2 long-QT syndrome loci in normal subjects. Circulation. 1999;99:3161–3164. doi: 10.1161/01.cir.99.24.3161. [DOI] [PubMed] [Google Scholar]
- 6.Carter N, Snieder H, Jeffery S, Saumarez R, Varma C, Antoniades L, Spector TD. QT interval in twins. J Hum Hypertens. 2000;14:389–390. doi: 10.1038/sj.jhh.1001026. [DOI] [PubMed] [Google Scholar]
- 7.Crow RS, Hannan PJ, Folsom AR. Prognostic significance of corrected QT and corrected JT interval for incident coronary heart disease in a general population sample stratified by presence or absence of wide QRS complex: the ARIC Study with 13 years of follow-up. Circulation. 2003;108:1985–1989. doi: 10.1161/01.CIR.0000095027.28753.9D. [DOI] [PubMed] [Google Scholar]
- 8.de Bruyne MC, Hoes AW, Kors JA, Hofman A, van Bemmel JH, Grobbee DE The Rotterdam Study. Prolonged QT interval predicts cardiac and all-cause mortality in the elderly. Eur Heart J. 1999;20:278–284. doi: 10.1053/euhj.1998.1276. [DOI] [PubMed] [Google Scholar]
- 9.Dekker JM, Crow RS, Hannan PJ, Schouten EG, Folsom AR. Heart rate-corrected QT interval prolongation predicts risk of coronary heart disease in black and white middle-aged men and women: the ARIC study. J Am Coll Cardiol. 2004;43:565–571. doi: 10.1016/j.jacc.2003.09.040. [DOI] [PubMed] [Google Scholar]
- 10.Dekker JM, Schouten EG, Klootwijk P, Pool J, Kromhout D. Association between QT interval and coronary heart disease in middle-aged and elderly men. The Zutphen Study. Circulation. 1994;90:779–785. doi: 10.1161/01.cir.90.2.779. [DOI] [PubMed] [Google Scholar]
- 11.Friedlander Y, Lapidos T, Sinnreich R, Kark JD. Genetic and environmental sources of QT interval variability in Israeli families: the kibbutz settlements family study. Clin Genet. 1999;56:200–209. doi: 10.1034/j.1399-0004.1999.560304.x. [DOI] [PubMed] [Google Scholar]
- 12.Garson A., Jr How to measure the QT interval--what is normal? Am J Cardiol. 1993;72:14B–16B. doi: 10.1016/0002-9149(93)90034-a. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg RJ, Bengtson J, Chen ZY, Anderson KM, Locati E, Levy D. Duration of the QT interval and total and cardiovascular mortality in healthy persons (The Framingham Heart Study experience) Am J Cardiol. 1991;67:55–58. doi: 10.1016/0002-9149(91)90099-7. [DOI] [PubMed] [Google Scholar]
- 14.Gombojav B, Park H, Kim JI, Ju YS, Sung J, Cho SI, Lee MK, Ohrr H, Radnaabazar J, Seo JS. Heritability and linkage study on heart rates in a Mongolian population. Exp Mol Med. 2008;40:558–564. doi: 10.3858/emm.2008.40.5.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grandinetti A, Seifried S, Mor J, Chang HK, Theriault AG. Prevalence and risk factors for prolonged QTc in a multiethnic cohort in rural Hawaii. Clin Biochem. 2005;38:116–122. doi: 10.1016/j.clinbiochem.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 16.Heath SC. Markov chain Monte Carlo segregation and linkage analysis for oligogenic models. Am J Hum Genet. 1997;61:748–760. doi: 10.1086/515506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hong Y, Rautaharju PM, Hopkins PN, Arnett DK, Djousse L, Pankow JS, Sholinsky P, Rao DC, Province MA. Familial aggregation of QT-interval variability in a general population: results from the NHLBI Family Heart Study. Clin Genet. 2001;59:171–177. doi: 10.1034/j.1399-0004.2001.590305.x. [DOI] [PubMed] [Google Scholar]
- 18.Jiang C, Atkinson D, Towbin JA, Splawski I, Lehmann MH, Li H, Timothy K, Taggart RT, Schwartz PJ, Vincent GM, et al. Two long QT syndrome loci map to chromosomes 3 and 7 with evidence for further heterogeneity. Nat Genet. 1994;8:141–147. doi: 10.1038/ng1094-141. [DOI] [PubMed] [Google Scholar]
- 19.Keating M, Atkinson D, Dunn C, Timothy K, Vincent GM, Leppert M. Linkage of a cardiac arrhythmia, the long QT syndrome, and the Harvey ras-1 gene. Science. 1991a;252:704–706. doi: 10.1126/science.1673802. [DOI] [PubMed] [Google Scholar]
- 20.Keating M, Dunn C, Atkinson D, Timothy K, Vincent GM, Leppert M. Consistent linkage of the long-QT syndrome to the Harvey ras-1 locus on chromosome 11. Am J Hum Genet. 1991b;49:1335–1339. [PMC free article] [PubMed] [Google Scholar]
- 21.Liu W, Yang J, Hu D, Kang C, Li C, Zhang S, Li P, Chen Z, Qin X, Ying K, Li Y, Li Y, Li Z, Cheng X, Li L, Qi Y, Chen S, Wang Q. KCNQ1 and KCNH2 mutations associated with long QT syndrome in a Chinese population. Hum Mutat. 2002;20:475–476. doi: 10.1002/humu.9085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mangoni AA, Kinirons MT, Swift CG, Jackson SH. Impact of age on QT interval and QT dispersion in healthy subjects: a regression analysis. Age Ageing. 2003;32:326–331. doi: 10.1093/ageing/32.3.326. [DOI] [PubMed] [Google Scholar]
- 23.Newton-Cheh C, Larson MG, Corey DC, Benjamin EJ, Herbert AG, Levy D, D'Agostino RB, O'Donnell CJ. QT interval is a heritable quantitative trait with evidence of linkage to chromosome 3 in a genome wide linkage analysis: The Framingham Heart Study. Heart Rhythm. 2005;2:277–284. doi: 10.1016/j.hrthm.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 24.Peters RW, Byington RP, Barker A, Yusuf S The BHAT Study Group. Prognostic value of prolonged ventricular repolarization following myocardial infarction: the BHAT experience. J Clin Epidemiol. 1990;43:167–172. doi: 10.1016/0895-4356(90)90180-w. [DOI] [PubMed] [Google Scholar]
- 25.Reardon M, Malik M. QT interval change with age in an overtly healthy older population. Clin Cardiol. 1996;19:949–952. doi: 10.1002/clc.4960191209. [DOI] [PubMed] [Google Scholar]
- 26.Russell MW, Law I, Sholinsky P, Fabsitz RR. Heritability of ECG measurements in adult male twins. J Electrocardiol. 1998;30(Suppl):64–68. doi: 10.1016/s0022-0736(98)80034-4. [DOI] [PubMed] [Google Scholar]
- 27.Schott JJ, Charpentier F, Peltier S, Foley P, Drouin E, Bouhour JB, Donnelly P, Vergnaud G, Bachner L, Moisan JP, et al. Mapping of a gene for long QT syndrome to chromosome 4q25-27. Am J Hum Genet. 1995;57:1114–1122. [PMC free article] [PubMed] [Google Scholar]
- 28.Schouten EG, Dekker JM, Meppelink P, Kok FJ, Vandenbroucke JP, Pool J. QT interval prolongation predicts cardiovascular mortality in an apparently healthy population. Circulation. 1991;84:1516–1523. doi: 10.1161/01.cir.84.4.1516. [DOI] [PubMed] [Google Scholar]
- 29.Shah M, Akar FG, Tomaselli GF. Molecular basis of arrhythmias. Circulation. 2005;112:2517–2529. doi: 10.1161/CIRCULATIONAHA.104.494476. [DOI] [PubMed] [Google Scholar]
- 30.Siscovick DS, Raghunathan TE, Rautaharju P, Psaty BM, Cobb LA, Wagner EH. Clinically silent electrocardiographic abnormalities and risk of primary cardiac arrest among hypertensive patients. Circulation. 1996;94:1329–1333. doi: 10.1161/01.cir.94.6.1329. [DOI] [PubMed] [Google Scholar]
- 31.Splawski I, Shen J, Timothy KW, Lehmann MH, Priori S, Robinson JL, Moss AJ, Schwartz PJ, Towbin JA, Vincent GM, Keating MT. Spectrum of mutations in long-QT syndrome genes. KVLQT1, HERG, SCN5A, KCNE1, and KCNE2. Circulation. 2000;102:1178–1185. doi: 10.1161/01.cir.102.10.1178. [DOI] [PubMed] [Google Scholar]
- 32.Vitelli LL, Crow RS, Shahar E, Hutchinson RG, Rautaharju PM, Folsom AR. Electrocardiographic findings in a healthy biracial population. Atherosclerosis Risk in Communities (ARIC) Study Investigators. Am J Cardiol. 1998;81:453–459. doi: 10.1016/s0002-9149(97)00937-5. [DOI] [PubMed] [Google Scholar]
- 33.Wang Q, Shen J, Splawski I, Atkinson D, Li Z, Robinson JL, Moss AJ, Towbin JA, Keating MT. SCN5A mutations associated with an inherited cardiac arrhythmia, long QT syndrome. Cell. 1995;80:805–811. doi: 10.1016/0092-8674(95)90359-3. [DOI] [PubMed] [Google Scholar]