Abstract
Background:
Lower extremity trauma is common. Despite an abundance of literature on severe injuries that can be treated with salvage or amputation, the appropriate management of these injuries remains uncertain. In this situation, a cost-utility analysis is an important tool in providing evidence-based practice an approach to guide treatment decisions.
Methods:
Costs following amputation and salvage were derived from data presented in a study that emerged from the Lower Extremity Assessment Project. We extracted relevant data on projected lifetime costs and analyzed them to include discounting and sensitivity analysis for consider patient age. The utilities for the various health states (amputation or salvage, including possible complications) were previously measured using the standard gamble method and a decision tree simulation to determine quality-adjusted life years (QALYs).
Results:
Amputation is more expensive than salvage independent of varied ongoing prosthesis needs, discount rate, and patient age at presentation. Moreover, amputation yields fewer QALYs than salvage. Salvage is deemed the dominant, cost-saving strategy.
Conclusions:
Unless the injury is so severe that salvage is not a possibility, based on this economic model, surgeons should consider limb salvage, which will yield lower costs and higher utility when compared to amputation.
Keywords: Cost-utility analysis, lower leg trauma, utility, amputation, salvage, reconstruction
Lower extremity trauma is common. Epidemiology studies have shown that open long bone fractures occur at a rate of 11.5 per 100,000 persons per year, and many of these are open tibial shaft fractures1-3. Type III open fractures are the most severe, involving extensive soft tissue trauma and complex fracture patterns4.
Many of these injuries can be managed with salvage involving either local muscle flaps or microvascular free tissue transfer for wound coverage. The alternative to reconstruction for such injuries is amputation. Over the past decades, many studies have sought to delineate the advantages and disadvantages of these two principal options for managing severe lower extremity trauma. A recent systematic review of all available literature demonstrated that, despite the abundance of evidence, neither option is superior with respect to clinical outcomes5.
Because microvascular reconstruction is technically demanding, time-consuming, and fraught with substantial risk of complications, we must look beyond clinical outcomes to evaluate the costs and utilities afforded to patients by this option. Studies have shown that even with successful limb salvage, many patients are still not ambulatory after two years; persistent pain and disability are not uncommon after this type of injury6, 7. Despite the residual problems with reconstruction, however, some studies suggest that patients with salvaged lower limbs have a better quality of life and impose lower costs on the health care system8-10.
As surgeons, we want the best for our patients, but as stewards of modern medicine who work with limited healthcare resources, we are also charged with making evidence-based, fiscally-sound decisions. When dealing with complex operations of uncertain effectiveness, cost-utility analyses can help provide the scientific evidence upon which these decisions can be based. Although costs10 and utilities11 have been measured, a detailed cost-utility analysis with robust sensitivity analysis, which is needed to consider the wide-range of assumptions in clinical decision-making, has not been conducted. This study presents a cost-utility analysis for management of severe open tibial fractures, and will serve to guide surgeons and patients in deciding between the two competing management options.
Materials and Methods
Cost is typically measured in currency, and it should reflect the present value of total future expenditures that would be incurred by making a certain decision. Utilities are typically measured in quality-adjusted life years (QALYs). A QALY is used to account for the morbidity of a health state, based on the assumption that a year of life with morbidity is not equal to a year of life without morbidity. For example, if a year of life with blindness is only three-fourths as valuable to patients as a year with perfect vision, each year of life with blindness will equal 0.75 QALYs. The value of a year with morbidity, referred to as the “utility weight,” can be determined through validated surveys including the standard gamble method, the time-tradeoff method, or the Short Form-36, among others12.
Cost-utility ratios are normalized values that reveal how much money (cost) must be paid for a single extra QALY (utility). Thus, if making Decision 1 costs $200,000 and yields an extra 3 QALYs, it costs $66,667 per QALY ($200,000 / 3 QALYs). When deciding between two management options, one should consider the incremental cost for the incremental gain of QALYs. This ratio, the incremental cost-effectiveness ratio, is calculated as (Cost1 – Cost2) / (QALY1 – QALY2) and is only useful when Decision 1 costs more but yields increased QALYs. If one of the interventions costs less and yields increased QALYs, that decision is “cost-saving” and “dominates” the other decision.
To calculate the cost-utility ratios for salvage and amputation following IIIB and IIIC tibial fractures, we combined the authors' previous work on utility, based on a survey of reconstructive microsurgeons and physical medicine and rehabilitation (PM&R) physicians,11 with reworked cost data from the Lower Extremity Assessment Project (LEAP) study10.
Costs
The costs following amputation and salvage were derived from the data presented in an outcome study from the LEAP study. LEAP is the largest primary analysis of limb-threatening injuries. The project is a prospective, longitudinal, multicenter study funded by the National Institutes of Health, and it has resulted in numerous publications7, 13, 14 6, 10, 15-25. The authors of the cost study estimate two-year costs and lifetime costs for amputation and salvage. For secondary amputation, data on amputations performed within three months of injury were aggregated in the amputation group. Data for amputations performed after three months were aggregated in the salvage group. Two-year costs include initial hospitalization, all re-hospitalizations for acute care related to the limb injury, inpatient rehabilitation, outpatient doctor visits, outpatient physical and occupational therapy, and the purchases and maintenance of prosthetic devices. Projected lifetime costs include ongoing clinical needs, such as clinic visits and prosthetic needs. To better reflect true cost of care, billed rates are multiplied by Medicare cost-to-charge ratios or cost-recovery ratios as appropriate. All dollar amounts are inflated to 2002 US dollars using the medical service Cost Price Index10.
By correcting only for inflation, the LEAP study ignores the time value of money (i.e., the fact that a dollar tomorrow is worth less than a dollar today even after adjusting for inflation). Discounting takes this value into account and is necessary in order to compare the actual or true values of the alternative interventions. This is an essential practice when alternative interventions have different costs occurring at different times over the remaining life of the patient. Procedures that involve a large fraction of long-term expenses, such as ongoing prosthetic needs, are likely to be more overstated in past studies that do not discount. Discounting reduces the costs of these interventions because of the process of compounding, year after year. To obtain estimates of the true costs of salvage versus amputation, we have discounted the costs by the risk-free rate. The risk-free rate is the minimum discount rate and can be used because it is assumed that the costs of the medical interventions are perfectly predictable. Because costs are likely to change in the future, the estimates in this study should be regarded as a conservative estimate of the effects of discounting.
The risk-free rate, Rf, used to discount future cash flows that are certain, is typically the 20-year U.S. Treasury rate. Because the study has already accounted for inflation, we need to employ a rate of return that has been normalized for inflation. The nominal rate can be normalized to account for inflation by subtracting the inflation rate, i. The newly obtained value, Rf – i, is called the real risk-free rate. Real Treasury bill rates have been reported since 2004. Since that time, the real risk-free rate has ranged from 1.58% to 3.35%26.
For discounting purposes, two-year costs were simplified by assuming that they take place at the beginning of year one. This is a reasonable assumption for two reasons. First, 60-80% of the two-year costs result from the initial hospitalization. Second, discounting at relatively low risk-free rates will only have a clinically meaningful effect over a period of time much longer than two years.
Annual lifetime costs were extracted from the available cost data from the LEAP study 10. Prosthetic device costs, based on a frequency of purchase of every 2.3 years and annual maintenance costs of 20% of the prosthetic cost, as noted in the study, were annualized by taking into account the time value of money and then added to ongoing lifetime costs.
The LEAP study did not account for non-medical costs. A robust assessment of the true cost difference between two interventions must account for all costs that vary between the two options. According to a systematic review of all available literature, loss of income with these injuries can be severe: only two-thirds of patients return to work, and this is only after an average delay of 14 months5. However, the percent of patients returning to work and the average delay until return to work did not differ significantly between salvage and amputation patients. Therefore, although these costs are important in determining the true cost of an intervention, they will not affect the comparison of salvage with amputation. For this reason, we exclude these costs in our comparison of these two interventions.
Utility
In 2008, we conducted a survey of randomly selected physicians from the American Society for Reconstructive Microsurgery (ASRM) and Physical Medicine and Rehabilitation (PM&R) physicians from the authors' home institution11. In this study, a web-based survey was deployed based on our prior experiences with utility surveys27, 28, using the standard gamble method. The standard gamble is based on von Neumann and Morgenstern's utility theory, and involves a survey in which participants are asked to compare specific outcomes with a probability of certain death. From this, we are able to determine how much “death” one is willing to risk in order to avoid a morbid health state. For example, if someone would rather risk a 25% chance of death than be blind with 100% certainty, then the utility of being blind is 75% (100% - 25%), and a year of this morbid life would be worth 0.75 QALYs. To avoid double counting, survey takers in the utility study are explicitly asked to ignore any financial burdens when comparing outcomes.
Quality-adjusted life years are calculated from the utility values in the standard fashion29, 30. The utilities of the different outcomes following salvage (no complications, secondary amputation, osteomyelitis, etc.) and those following below-the-knee amputation (no complications, secondary revision, etc.) are combined by weighting each of the utilities with the rates of occurrence as determined by a systematic review of the literature5. This yields the utility weights of each of the two management options. By multiplying the utility weights by the expected lifespan of a patient, we derive the total QALYs remaining following salvage or amputation.
Sensitivity Analyses
Sensitivity analyses were performed by varying the assumptions of costs, discount rates, utilities, and expected patient lifespan. Performing sensitivity analyses is integral in any economic analysis model in an effort to consider extreme values of the initial assumptions. The stability of a conclusion is predicated on the sensitivity analyses in order to understand whether changing values can affect the results. As in the LEAP cost study, the need to purchase a new prosthetic device was varied from once every 2.3 years to once every 5 years, and annual device maintenance costs were varied from 20% to 10% of the device cost. Because real discount rates have historically varied from 1.58% to 3.35%, we performed our calculations over a range of 1% to 4%. For illustrative purposes, we also included a 0% discount rate to show the problems that arise when discounting is not taken into consideration. Additionally, we varied expected patient lifespan to account for patients of all ages. Resultant values were correlated with patients' ages based on the 2003 US Life Expectancy Table31. Finally, as in the original utility study, we also employed a range of utilities based on sensitivities on the complication rates used to calculate utility.
Results
Costs
Ongoing annual costs for salvage were calculated as follows. Total average lifetime costs for reconstruction patients are reported to be $163,28210. Because costs for the first two years following injury are $81,316, this leaves $81,966 in medical costs after year 2. The average LEAP patient age is 35.26 and 76.7% of the patients included in the cost study were male. Combining these data with the 2003 US Life Expectancy Table used in the cost study, the weighted average of expected years of life remaining for each patient is 42.8 years. Distributing the $81,966 over the remaining years of life after year 2 yields a yearly average, ongoing medical cost of $1913 per patient. Ongoing costs after year 2 are discounted at 2% and combined with initial two year costs. In total, lifetime cost of salvage for a patient with 40 years of life remaining is $133,704.
The total average lifetime costs for amputation patients are reported as $509,27510. Because costs for the first two years following injury are reported as $91,105, this leaves $418,170 in medical costs for year 3 onward. Assuming 42.8 years of remaining life, and a frequency of prosthetic purchase of every 2.3 years after year 2, yields an expected purchase of 17.4 prosthetics. The weighted average prosthetic cost is $10,232, so total prosthetic device costs after year 2 are $181,500. The annual prosthetic maintenance costs are assumed to be 20% of the prosthetic cost, for a total of $83,490 after year 2. Therefore, non-prosthesis-related medical costs after year 2 are $153,181, which amounts to annual ongoing costs of $3,754. These non-prosthetic-related costs are then added to the appropriately discounted prosthetic costs to calculate the lifetime cost. Ongoing costs after year 2 are discounted at 2% and combined with initial two year costs. In total, lifetime cost of amputation for a patient with 40 years of life remaining is $350,465.
Utility
Mean utility values for each major clinical outcome from the utility study are shown in Table 1. After running a simulation to incorporate the probabilities of complication, we determine the overall utility weights to be 0.954 for amputation and 0.969 for salvage. The result is that for every year of life left, salvage patients enjoy an extra 0.016 QALYs.
Table 1.
Mean Utility Values Following Salvage and Amputation of IIIB and IIIC Tibial Fractures
| Clinical outcome | Utility |
|---|---|
| Reconstruction without complications | 0.975 |
| Reconstruction with secondary amputation | 0.907 |
| Reconstruction with osteomyelitis | 0.971 |
| Reconstruction with nonunion | 0.976 |
| Reconstruction with flap failure | 0.968 |
| Amputation without complications | 0.963 |
| Amputation with secondary revision | 0.967 |
| Amputation with osteomyelitis | 0.850 |
The standard gamble method was employed to assess utility values for major clinical outcomes. Values were calculated by assessing users' willingness to avoid them in exchange for risking known probabilities of certain death.
Sensitivity Analyses
To ensure our results are robust, we performed the various sensitivity analyses. First, ongoing prosthesis needs were decreased by reducing both the frequency of purchase from every 2.3 years to every 5 years and by reducing the annual maintenance cost from 20% to 10% of the cost of the prosthetic. This reduces the cost difference between amputation and salvage, especially for younger patients (Table 2). Despite this decrease, however, amputation remains the more expensive option.
Table 2.
Sensitivity Analysis for Prosthesis Maintenance Needs
| Expected Prosthesis Need |
Lower Prosthesis Need |
||
|---|---|---|---|
| Varied values | |||
| Frequency of Purchase (Years) | 2.3 | 5 | |
| Cost of Annual Maintenance | 20% | 10% | |
| Excess cost of amputation with 2% discount rate | |||
| 18-year-old patient | $279,586 | $166,413 | |
| 40-year-old patient | $216,761 | $129,124 | |
| 63-year-old patient | $123,405 | $73,714 | |
Lower ongoing prosthesis need (i.e., reduced frequency of purchase from every 2.3 years to every 5 years and reduced annual maintenance cost from 20% to 10% of the cost of the prosthesis) reduces the cost difference between reconstruction and amputation, especially for younger patients.
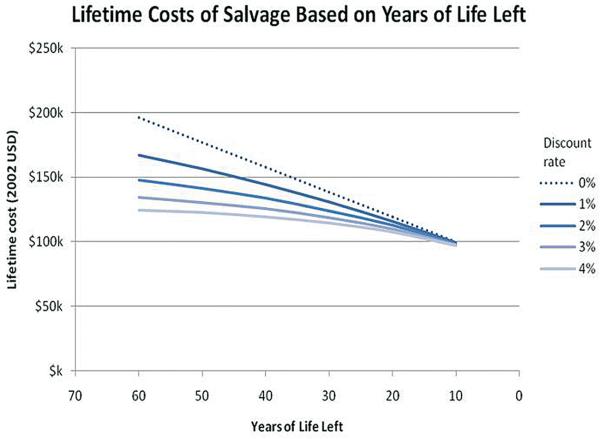
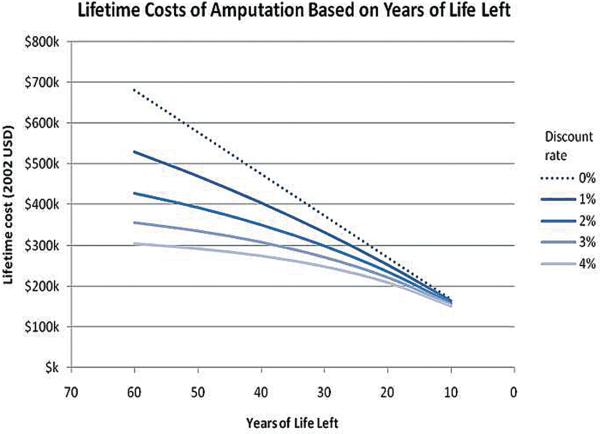
To assess whether varying patient ages or discounting rates changed our result, we recalculated the cost of each intervention for patients with 10 to 60 years of life remaining at discount rates ranging from 1% to 4% (Tables 3 and 4) (Figures 1 and 2). For reference, according to the 2003 US Life Expectancy Table, a person with 60 years of life remaining is approximately 18 years old, a person with 40 years of life remaining is approximately 40 years old, and a person with 20 years of life remaining is approximately 63 years old. Therefore, at a 2% discount rate, the medical costs of salvage and amputation, respectively, are $147,870 and $427,457 for an 18-year-old patient, $133,704 and $350,465 for a 40-year-old patient, and $112,654 and $236,059 for a 63-year-old patient.
Table 3.
Lifetime Costs of Limb Salvage Following IIIB and IIIC Fractures.
| Real discount rate (Rf - i) | |||||
|---|---|---|---|---|---|
| Years Remaining | 0% | 1% | 2% | 3% | 4% |
| 60 | $ 196,039 | $ 166,894 | $ 147,036 | $ 133,131 | $ 123,122 |
| 50 | $ 176,910 | $ 155,878 | $ 140,652 | $ 129,409 | $ 120,939 |
| 40 | $ 157,780 | $ 143,709 | $ 132,870 | $ 124,407 | $ 117,707 |
| 30 | $ 138,651 | $ 130,267 | $ 123,384 | $ 117,684 | $ 112,923 |
| 20 | $ 119,522 | $ 115,418 | $ 111,820 | $ 108,649 | $ 105,842 |
| 10 | $ 100,393 | $ 99,017 | $ 97,724 | $ 96,507 | $ 95,360 |
Both higher discount rates and lower life expectancy reduce lifetime cost of reconstruction.
Table 4.
Lifetime Costs of Amputation Following IIIB and IIIC Fractures
| Real discount rate (Rf - i) | |||||
|---|---|---|---|---|---|
| Years Remaining | 0% | 1% | 2% | 3% | 4% |
| 60 | $ 680,701 | $ 529,540 | $ 426,611 | $ 354,740 | $ 303,269 |
| 50 | $ 578,209 | $ 470,092 | $ 391,914 | $ 334,365 | $ 291,233 |
| 40 | $ 475,716 | $ 404,424 | $ 349,619 | $ 306,984 | $ 273,418 |
| 30 | $ 373,223 | $ 331,885 | $ 298,062 | $ 270,186 | $ 247,047 |
| 20 | $ 270,731 | $ 251,758 | $ 235,214 | $ 220,733 | $ 208,011 |
| 10 | $ 168,238 | $ 163,248 | $ 158,602 | $ 154,271 | $ 150,228 |
Higher discount rates and lower life expectancy reduce lifetime cost of amputation. Discount rate has a larger effect on amputation because of the high long-term costs associated with prosthetic purchase and maintenance.
Figure 1.
Lifetime Costs of Salvage Based on Years of Life Remaining. Both higher discount rates and lower life expectancy reduce lifetime cost of reconstruction.
Figure 2.
Lifetime Costs of Amputation Based on Years of Life Remaining. Higher discount rates and lower life expectancy reduce lifetime cost of amputation. Discount rate has a larger effect on amputation because of the high long-term costs associated with prosthetic purchase and maintenance. This figure also illustrates the importance of discounting. By not taking into account the time value of money (the dotted line, “0%”), the true present value of treatment is overestimated.
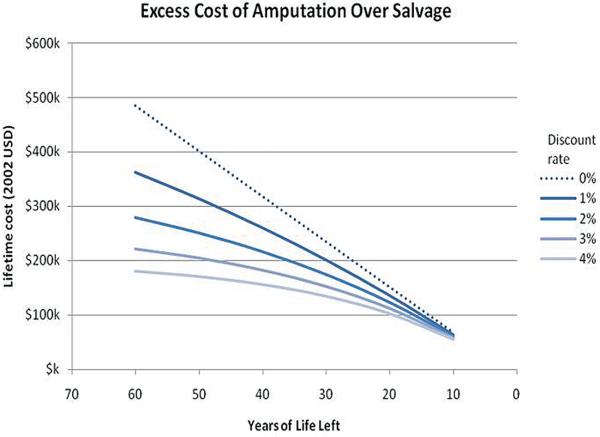
Discounting appropriately decreases the difference between the true cost of salvage and amputation. This is because the more expensive option, amputation, is associated with higher ongoing costs, and these long-term costs are impacted more substantially by discounting. Because amputation is also associated with higher short-term costs, however, it remains more expensive across all sensitivities. As expected, the long-term expenses have more impact for younger patients, making amputation even more relatively expensive for this group. (Table 5) (Figure 3) The difference between the two treatment options is diminished with age, and it would not be surprising to find that the burden of attempted salvage could be too high in a much older patient.
Table 5.
Excess Lifetime Costs of Amputation over Salvage Following IIIB and IIIC Fractures.
| Real discount rate (Rf - i) | |||||
|---|---|---|---|---|---|
| Years Remaining | 0% | 1% | 2% | 3% | 4% |
| 60 | $ 484,663 | $ 362,646 | $ 279,575 | $ 221,609 | $ 180,147 |
| 50 | $ 401,299 | $ 314,214 | $ 251,262 | $ 204,957 | $ 170,295 |
| 40 | $ 317,936 | $ 260,715 | $ 216,749 | $ 182,578 | $ 155,711 |
| 30 | $ 234,572 | $ 201,619 | $ 174,678 | $ 152,502 | $ 134,123 |
| 20 | $ 151,209 | $ 136,340 | $ 123,394 | $ 112,083 | $ 102,169 |
| 10 | $ 67,846 | $ 64,231 | $ 60,878 | $ 57,764 | $ 54,868 |
Because amputation is associated with higher short-term costs, it remains more expensive across all sensitivities. As expected, the long-term expenses have more impact for younger patients, making amputation even more relatively expensive for this group.
Figure 3.
Excess Lifetime Cost of Amputation over Salvage. Because amputation is more expensive even in the short term, it remains more expensive than salvage through the entire range. The difference is less exaggerated when we account for discounting and when we consider patients with fewer remaining years to live.
Complication rates are used in calculating utility rates. These rates were varied in order to find a point at which the utility of amputation is greater than that of reconstruction. However, even under the most extreme conditions – when the complication rate of reconstruction is assumed to be 100% and the complication rate of amputation is expected to be 0% – reconstruction continues to yield higher utility than amputation11.
Discussion
Our analysis shows that amputation is more expensive independent of ongoing prosthesis needs, discounting effect, and years of life remaining. For example, even under the most favorable prosthesis maintenance conditions, amputation will cost a 40-year-old patient at least $93,606 (assuming a 4% real discount rate) and up to $154,636 (assuming a 1% real discount rate) more than limb salvage. Furthermore, we found that utility is increased with salvage; a similar patient with an estimated 40 years of life remaining will enjoy an additional 0.63 QALYs after undergoing salvage instead of amputation. The cost and utility differences between these two interventions are even more pronounced for younger patients.
Salvage is the dominating strategy – it is less expensive and provides higher utility. Therefore, surgeons should select limb salvage more aggressively in patients where amputation is not absolutely necessary, especially those patients with higher life expectancies. This policy should, of course, be followed up to a point, because more aggressive salvage of more severe cases will eventually lead to decreased utility for the patient and increased costs. This will happen as more severe cases will require increased healthcare resources and lead to healthcare utilities that are lower than the current expectations included in our measurement of utility.
This study has several limitations. Most notably, we face many of the same limitations of the original articles. Because cost estimates were based partly on patient surveys, they are subject to recall bias. Furthermore, although we have accounted for costs related to loss of income, we have not accounted for other costs such as the possible need for institutional care, residential adaptations, and pharmacy-related costs. Given the relative magnitude of these expenditures, however, we do not expect that these factors would meaningfully change the cost figures we employed in our analysis. Furthermore, even if these expenditures were greater, we do not expect that they would substantially impact one group more than the other. Therefore, our conclusion regarding the comparison of these two groups is still valid.
Furthermore, because not all data were presented in the LEAP cost study, we made certain assumptions with respect to ongoing medical costs of each intervention. Specifically, by asserting that the average annual cost per patient is equal to the average lifetime cost divided by average lifespan, we assume that ongoing annual costs and age at presentation are statistically independent. Even though it is likely that age at presentation has some effect on ongoing medical costs, our assumptions yield data consistent with the LEAP study's data. Therefore, any effect is likely to be clinically negligible. By discounting prostheses at the real rate of inflation, we assume that prosthetic costs will grow at the same rate as inflation. However, if the costs outpace inflation, our results are conservative and underestimate the cost of amputation. Alternatively, if the costs rise more slowly than inflation, amputation will still remain more expensive because of the higher non-prosthetic annual costs.
Our study assumes that life expectancy following IIIB and IIIC tibial fractures is similar to life expectancy of the normal population. By performing sensitivities across years of remaining life, however, we were able to confirm our results independent of remaining years of life. Therefore, even if life expectancy differs, as long as the differences in life expectancy are similar between salvage and amputation, our conclusion still stands. Unfortunately, long-term data to answer this question are currently lacking. Finally, because our data are based on observational studies, it is possible that patients who underwent amputation inherently have more severe injuries that would require more costly treatment and lead to decreased utility if salvage would have been attempted. It is for this reason that our recommendations for surgeons are targeted only at borderline patients.
Despite these limitations, this unique economic analysis paper can help guide surgeons' decisions for patients with open tibial fractures. Our comprehensive modeling and robust sensitivity analyses reveal a consistent result, which strengthens and supports the generalizability our conclusion. Furthermore, because we have stratified our results by patient age, surgeons will be able to make evidence-based decisions that are more patient-specific.
With the nation's increasing focus on healthcare costs, it is even more important that the conclusion of this study be brought to the forefront of discussion. We have found that, across a range of robust sensitivities, salvage currently dominates amputation as a strategy for the management of IIIB and IIIC tibial fractures. We therefore recommend that surgeons become more aggressive in their attempts to save limbs in patients whose management choice is unclear. For these borderline patients, we will continue to incur higher costs and provide less utility by routinely taking recourse to amputation.
Acknowledgments
We appreciate the support from the National Endowment for Plastic Surgery and a National Institute of Arthritis and Musculoskeletal and Skin Diseases Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung).
Footnotes
Financial Disclosures: None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript
REFERENCES
- 1.Court-Brown CM, Rimmer S, Prakash U, McQueen MM. The epidemiology of open long bone fractures. Injury. 1998;29(7):529–534. doi: 10.1016/s0020-1383(98)00125-9. [DOI] [PubMed] [Google Scholar]
- 2.Howard M, Court-Brown CM. Epidemiology and management of open fractures of the lower limb. Brit J Hosp Med. 1997;57(11):582–587. [PubMed] [Google Scholar]
- 3.Emami A, Mjoberg B, Ragnarsson B, Larsson S. Changing epidemiology of tibial shaft fractures. 513 cases compared between 1971-1975 and 1986-1990. Acta Orthop Scand. 1996;67(6):557–561. doi: 10.3109/17453679608997755. [DOI] [PubMed] [Google Scholar]
- 4.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:42–46. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Saddawi-Konefka D, Kim HM, Chung KC. A systematic review of outcomes and complications of reconstruction and amputation for type IIIB and IIIC fractures of the tibia. Plast Reconstr Surg. 2008 Dec;122(6):1796–1805. doi: 10.1097/PRS.0b013e31818d69c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.MacKenzie EJ, Bosse MJ, Castillo RC, et al. Functional outcomes following trauma-related lower-extremity amputation. J Bone Joint Surg. 2004;86A:1636–1645. doi: 10.2106/00004623-200408000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Bosse MJ, MacKenzie EJ, Kellam JF, et al. An analysis of outcomes of reconstruction or amputation of leg-threatening injuries. N Engl J Med. 2002;347:1924–1931. doi: 10.1056/NEJMoa012604. [DOI] [PubMed] [Google Scholar]
- 8.Arangio GA, Lehr S, Reed JFI. Reemployment of patients with surgical salvage of open, high-energy tibial fractures: an outcome study. J Trauma. 1997;42:942–945. doi: 10.1097/00005373-199705000-00027. [DOI] [PubMed] [Google Scholar]
- 9.Hertel R, Strebel N, Ganz R. Amputation versus reconstruction in traumatic defects of the leg: outcome and costs. J Orthop Trauma. 1996;10:223–229. doi: 10.1097/00005131-199605000-00001. [DOI] [PubMed] [Google Scholar]
- 10.MacKenzie EJ, Jones AS, Bosse MJ, et al. Health-care costs associated with amputation or reconstruction of a limb-threatening injury. J Bone Joint Surg Am. 2007 Aug;89(8):1685–1692. doi: 10.2106/JBJS.F.01350. [DOI] [PubMed] [Google Scholar]
- 11.Chung KC, Shauver MJ, Saddawi-Konefka D, Haase SC. A decision analysis of amputation versus reconstruction for severe open tibia fracture. Reconstr Surg. doi: 10.1097/SAP.0b013e3181cbfcce. submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Center for the Evaluation of Value and Risk in Health Glossary. from CEA registry: https://research.tufts-nemc.org/cear/related/glossary.aspx; March 1,2009. Accessed.
- 13.Pollak AN, McCarthy ML, Burgess AR. Short-term wound complications after application of flaps for coverage of traumatic soft-tissue defects about the tibia. The Lower Extremity Assessment Project (LEAP) Study Group. J Bone Joint Surg Am. 2000 Dec;82-A(12):1681–1691. [PubMed] [Google Scholar]
- 14.Bosse MJ, MacKenzie EJ, Kellam JF, et al. A prospective evaluation of the clinical utility of the lower-extremity injury-severity scores. J Bone Joint Surg. 2001;83A(1):3–14. doi: 10.2106/00004623-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Bosse MJ, McCarthy ML, Jones AL, et al. The insensate foot following severe lower extremity trauma: an indication for amputation? J Bone Joint Surg. 2005;87(12):2601–2608. doi: 10.2106/JBJS.C.00671. [DOI] [PubMed] [Google Scholar]
- 16.MacKenzie EJ, Bosse MJ, Kellam JF, et al. Factors influencing the decision to amputate or reconstruct after high-energy lower extremity trauma. J Trauma. 2002;52(4):641–649. doi: 10.1097/00005373-200204000-00005. [DOI] [PubMed] [Google Scholar]
- 17.MacKenzie EJ, Bosse MJ. Factors influencing outcome following limb-threatening lower limb trauma: lessons learned from the Lower Extremity Assessment Project (LEAP) J Am Acad Orthop Surg. 2006;14(10 Spec No):S205–210. doi: 10.5435/00124635-200600001-00044. [DOI] [PubMed] [Google Scholar]
- 18.MacKenzie EJ, Bosse MJ, Kellam JF, et al. Early predictors of long-term work disability after major limb trauma. J Trauma. 2006 Sep;61(3):688–694. doi: 10.1097/01.ta.0000195985.56153.68. [DOI] [PubMed] [Google Scholar]
- 19.McCarthy ML, MacKenzie EJ, Edwin D, Bosse MJ, Castillo RC, Starr A. Psychological distress associated with severe lower-limb injury. J Bone Joint Surg Am. 2003 Sep;85-A(9):1689–1697. doi: 10.2106/00004623-200309000-00006. [DOI] [PubMed] [Google Scholar]
- 20.MacKenzie EJ, Bosse MJ, Pollak AN, et al. Long-term persistence of disability following severe lower-limb trauma. Results of a seven-year follow-up. J Bone Joint Surg. 2005;87A(8):1801–1809. doi: 10.2106/JBJS.E.00032. [DOI] [PubMed] [Google Scholar]
- 21.Castillo RC, Bosse MJ, MacKenzie EJ, Patterson BM. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma. 2005 Mar;19(3):151–157. doi: 10.1097/00005131-200503000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Castillo RC, MacKenzie EJ, Webb LX, Bosse MJ, Avery J. Use and perceived need of physical therapy following severe lower-extremity trauma. Arch Phys Med Rehabil. 2005 Sep;86(9):1722–1728. doi: 10.1016/j.apmr.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 23.Smith JJ, Agel J, Swiontkowski MF, Castillo R, Mackenzie E, Kellam JF. Functional outcome of bilateral limb threatening: lower extremity injuries at two years postinjury. J Orthop Trauma. 2005 Apr;19(4):249–253. doi: 10.1097/01.bot.0000151813.10046.e4. [DOI] [PubMed] [Google Scholar]
- 24.Castillo RC, MacKenzie EJ, Wegener ST, Bosse MJ. Prevalence of chronic pain seven years following limb threatening lower extremity trauma. Pain. 2006 Oct;124(3):321–329. doi: 10.1016/j.pain.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 25.Archer KR, Castillo RC, Mackenzie EJ, Bosse MJ. Physical disability after severe lower-extremity injury. Arch Phys Med Rehabil. 2006 Aug;87(8):1153–1155. doi: 10.1016/j.apmr.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 26.United States Department of the Treasury U.S. Treasury - Daily Treasury Real Yield Curve. http://ustreas.gov/offices/domestic-finance/debt-management/interest-rate/real_yield_historical.shtml; Retrieved March 1, 2009.
- 27.Cavaliere C, Chung KC. A cost-utility analysis comparing total wrist fusion and total wrist arthroplasty for the rheumatoid wrist. J Bone Joint Surg. Submitted. [Google Scholar]
- 28.Davis EN, Chung KC, Kotsis SV, Lau FH, Vijan S. A cost/utility analysis of open reduction and internal fixation versus cast immobilization for acute nondisplaced mid-waist scaphoid fractures. Plast Reconstr Surg. 2006 Apr;117(4):1223–1235. doi: 10.1097/01.prs.0000201461.71055.83. [DOI] [PubMed] [Google Scholar]
- 29.Naglie G, Krahn MD, Naimark D, Redelmeier DA, Detsky AS. Primer on medical decision analysis: Part 3--Estimating probabilities and utilities. Med Decis Making. 1997 Apr-Jun;17(2):136–141. doi: 10.1177/0272989X9701700203. [DOI] [PubMed] [Google Scholar]
- 30.Cugno S, Sprague S, Duku E, Thoma A. Composite tissue allotransplantation of the face: decision analysis model. Can J Plast Surg. 2007;15(3):145–152. doi: 10.1177/229255030701500304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arias E. United States life tables, 2003. National Vital Statistics Reports. 2006;54(14):1–3. [PubMed] [Google Scholar]