Abstract
Background:
It is controversial whether physical activity is protective against first stroke among older persons. We sought to examine whether physical activity, as measured by intensity of exercise and energy expended, is protective against ischemic stroke.
Methods:
The Northern Manhattan Study is a prospective cohort study in older, urban-dwelling, multiethnic, stroke-free individuals. Baseline measures of leisure-time physical activity were collected via in-person questionnaires. Cox proportional hazards models were constructed to examine whether energy expended and intensity of physical activity were associated with the risk of incident ischemic stroke.
Results:
Physical inactivity was present in 40.5% of the cohort. Over a median follow-up of 9.1 years, there were 238 incident ischemic strokes. Moderate- to heavy-intensity physical activity was associated with a lower risk of ischemic stroke (adjusted hazard ratio [HR] 0.65, 95% confidence interval [0.44–0.98]). Engaging in any physical activity vs none (adjusted HR 1.16, 95% CI 0.88–1.51) and energy expended in kcal/wk (adjusted HR per 500-unit increase 1.01, 95% CI 0.99–1.03) were not associated with ischemic stroke risk. There was an interaction of sex with intensity of physical activity (p = 0.04), such that moderate to heavy activity was protective against ischemic stroke in men (adjusted HR 0.37, 95% CI 0.18–0.78), but not in women (adjusted HR 0.92, 95% CI 0.57–1.50).
Conclusions:
Moderate- to heavy-intensity physical activity, but not energy expended, is protective against risk of ischemic stroke independent of other stroke risk factors in men in our cohort. Engaging in moderate to heavy physical activities may be an important component of primary prevention strategies aimed at reducing stroke risk.
GLOSSARY
- CI
= confidence interval;
- HR
= hazard ratio;
- MET
= metabolic equivalents.
Stroke is the leading cause of serious disability and the third leading cause of mortality in the United States.1 The greatest impact on stroke morbidity and mortality has been made by identifying modifiable risk factors and intervening when possible.2
The incidence of stroke increases with age, but particularly so for women after age 85 years; women now constitute 69.7% of all admissions for stroke.1 Because women live longer than men, stroke is a greater public health burden in women.
Physical activity, especially at vigorous intensity for 20 to 40 minutes for 3 to 5 d/wk, is an important component of primary prevention for cardiovascular disease and stroke, particularly in the elderly.3 Leisure-time physical activity has been consistently established as strongly protective against atherosclerotic coronary heart disease,4 whereas it is a less well-established modifiable risk factor for ischemic stroke. Several studies have examined the association between physical activity and stroke, with some results indicating a protective effect independent of established risk factors such as diabetes and hypertension.5–11 Moreover, there is no consensus as to the optimal amount of physical activity in the elderly to prevent vascular disease. In the Northern Manhattan Stroke Study, a retrospective case-control study of stroke in Northern Manhattan, leisure-time physical activity was found to be protective against ischemic stroke.12 Our goal was to explore whether physical activity is protective against ischemic stroke in a methodologically more robust prospective study in the same community, thereby avoiding the biases inherent in a retrospective case-control study.
METHODS
Recruitment of the cohort.
The Northern Manhattan Study is a population-based prospective cohort study designed to evaluate the effects of medical, socioeconomic, and other risk factors on the incidence of vascular disease in a stroke-free multiethnic community cohort. Methods of participant recruitment, evaluation, and follow-up have been previously reported.13 A total of 3,298 participants were recruited. In-person evaluations were performed at Columbia University Medical Center or at home for those who could not come in person (6% were performed at home). The study was approved by the institutional review boards at Columbia University Medical Center and the University of Miami. All participants gave informed consent to participate in the study.
Cohort evaluation.
Data regarding baseline status and risk factors were collected through interviews of participants. Race/ethnicity was determined by self-identification. Standardized questions were asked regarding the following conditions: hypertension, diabetes, hypercholesterolemia, peripheral vascular disease, TIA, cigarette smoking, and cardiac conditions. Standard techniques were used to measure blood pressure, height, weight, and fasting serum glucose and lipid panels. Hypertension was defined as systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg based on the average of 2 blood pressure measurements, physician diagnosis of hypertension, or patient self-report of a history of hypertension or antihypertensive use. Diabetes mellitus was defined as fasting blood glucose ≥126 mg/dL, patient self-report of diabetes mellitus, or insulin and/or hypoglycemic agent use.
Assessment of physical activity.
Physical activity was measured by an in-person questionnaire adapted from the National Health Interview Survey of the National Center for Health Statistics.14 This questionnaire records the duration and frequency of various leisure-time/recreational activities for the 2 weeks before the interview is conducted. The participants were asked whether this level of activity was typical of other weeks. The participants were then asked whether they engaged in any physical activity in the preceding 2 weeks, and those who answered no were coded as physically inactive. For each activity, the participant was asked the duration of activity and the times they engaged in this activity; if the duration of activity was less than 10 minutes, it was coded as “no activity.” This questionnaire has been previously reported as reliable and validated in this population, demonstrating a crude concordance rate of 0.69 when proxies of the participants were asked.12 This same measure also correlated with body mass index, activities of daily living scores, and quality of well-being activity scores.12
Questionnaires were correlated with compendia of physical activity to allow calculation of energy expenditure in kilocalories, as well as metabolic equivalents (MET) for the intensity of activity.15 Physical activity can be further classified based on MET as light (between 1 and 5.5 MET, such as golfing or bowling), moderate (5.5–8 MET, such as bicycling or swimming), or heavy activity (>8 MET, such as racquetball).15 In the present analysis, we estimated intensity based on the sum of all of the MET for each activity for each individual to account for the entirety of the physical activity that each participant was able to perform. Energy expenditure per week was estimated based on the sum of the MET of each activity times body weight times the number of hours per week it was performed. Objective measures of physical fitness, as measured by exercise and treadmill testing or maximum oxygen uptake, correlate well with physical activity questionnaires.16
Follow-up of the cohort.
All participants were followed up annually via phone screening to detect any new neurologic or cardiac symptoms and events, as well as to review any interval hospitalizations. Any participant who responded positively on screening was scheduled for an in-person assessment. Neurologic events that were deemed to be possible strokes were adjudicated by 2 neurologists independently after review of all data. The final diagnosis and stroke subtype were decided by consensus of the 2 neurologists; any disagreements were adjudicated by a third neurologist. Ischemic strokes were classified as extracranial atherosclerotic, intracranial atherosclerotic, small vessel (lacunar), cardioembolic, cryptogenic, or other.17
Statistical analysis.
Cox proportional hazard models were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between physical activity and ischemic stroke. The parameter estimates were calculated unadjusted, and after adjusting for demographics (age, sex, race/ethnicity, and education) and vascular risk factors (hypertension, diabetes mellitus, and smoking).18 Parameter estimates and standard errors were calculated for physical activity using energy expenditure in kcal/wk as a continuous variable per 500-unit increase. Models were also constructed using physical activity as a categorical variable with no activity as the reference group, and comparing in separate models 1) any activity and 2) light intensity and moderate to heavy intensity. The likelihood ratio test was used to test for improved model fit when interaction terms were positive.
RESULTS
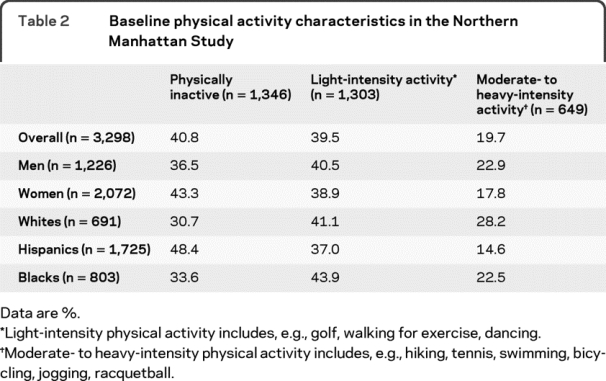
Baseline demographics of the cohort are presented in table 1. The average age was 69.2 ± 10.3 years, and 62.9% were women; 54.2% of the cohort was Hispanic, 25.0% was non-Hispanic black, and 20.8% was non-Hispanic white. Physical inactivity was common in the cohort (40.8% overall) but differed by race/ethnicity. Hispanics were more likely to be physically inactive (48.4%) and less likely to engage in moderate- to heavy-intensity activity (14.6%) compared with whites (30.7% were physically inactive, 28.2% participated in moderate- to heavy-intensity activity). There were significant differences by sex in the baseline physical activity characteristics as well. Women were more likely than men to be physically inactive (43.3% vs 36.5%) and to engage less in moderate- to heavy-intensity activities (table 2).
Table 1 Baseline demographics of the Northern Manhattan Study Cohort (n = 3,298)
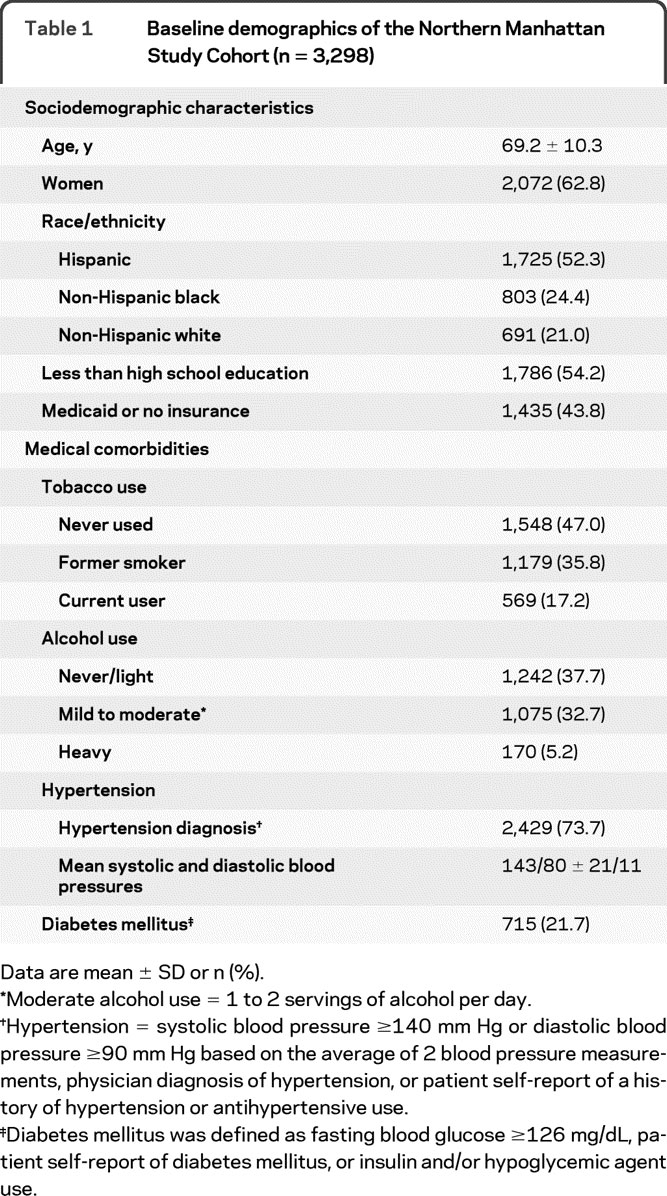
Table 2 Baseline physical activity characteristics in the Northern Manhattan Study
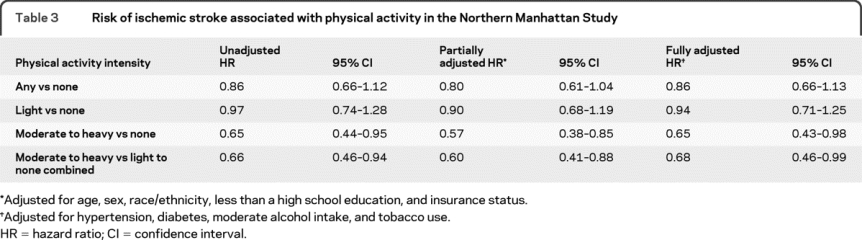
Subjects were followed up for a median of 9.1 years, and there were 238 incident ischemic strokes. Any physical activity, compared with no activity, was not associated with ischemic stroke in univariate or multivariable analyses (adjusted HR 1.16, 95% CI 0.88–1.51). In univariate analyses of levels of activity, moderate to heavy physical activity, compared with no physical activity, was associated with a lower risk of ischemic stroke (unadjusted HR 0.65, 95% CI 0.44–0.95), whereas light-intensity activity was not (unadjusted HR 0.97, 95% CI 0.74–1.28). In a model adjusting for sociodemographic factors (age, sex, race/ethnicity, insurance status, and education), the association with moderate- to heavy-intensity activity remained (adjusted HR 0.57, 95% CI 0.38–0.85). The association between ischemic stroke risk and moderate to heavy activity was slightly attenuated but remained significant after also including hypertension, diabetes, alcohol use, and tobacco use (adjusted HR 0.65, 95% CI 0.44–0.98). Light-intensity activity was not associated with the risk of ischemic stroke in any of the multivariable models. When we compared moderate to heavy activity with no activity and light-intensity activity combined, our results were not appreciably different (fully adjusted HR 0.68, 95% CI 0.46–0.99; table 3).
Table 3 Risk of ischemic stroke associated with physical activity in the Northern Manhattan Study
We found evidence of an interaction between moderate to heavy activity and sex (p value for interaction term = 0.04), indicating that moderate to heavy activity was associated with a protective effect against ischemic stroke in men (adjusted HR for men 0.37, 95% CI 0.18–0.77), whereas there was no evidence of an interaction between light activity and sex (p value for interaction = 0.30). In addition, the likelihood ratio test showed that the model with those interaction terms improved the fit (χ2 with 2 degrees of freedom, p = 0.02), suggesting that there are sex differences in the effect on ischemic stroke. There was no evidence of interactions with race/ethnicity, age, or tobacco use.
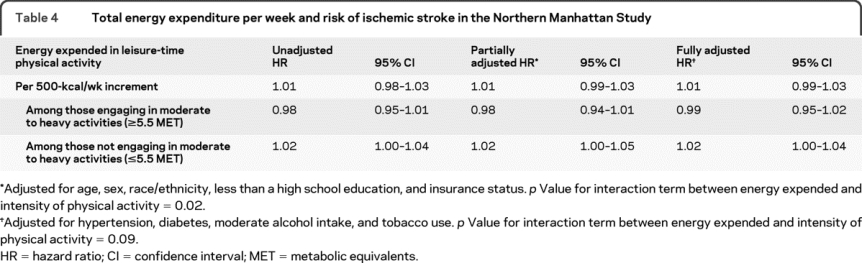
We also examined whether physical activity as measured by kcal/wk expended was associated with a lower risk of ischemic stroke. In univariate (HR per 500 kcal/wk 1.01, 95% CI 0.98–1.03) and multivariable models adjusting for sociodemographics and medical risk factors, kcal/wk as a continuous variable was not associated with ischemic stroke risk (adjusted HR per 500-kcal/wk unit increase 1.01, 95% CI 0.99–1.03; table 4). Prior literature indicates that energy expenditure may only be protective against ischemic stroke in those individuals who engage in physical activity that is more vigorous.11 We found evidence for effect modification based on our defined cutoff for moderate to heavy intensity of 5.5 MET in univariate analysis (p value for interaction term = 0.03) and a trend in fully adjusted models (p value for interaction term = 0.09). In stratified models, energy expended was not associated with a lower risk of ischemic stroke among individuals who engaged in moderate- to heavy-intensity activity (adjusted HR per 500 kcal/wk 0.99, 95% CI 0.95–1.02). There was no evidence of interaction with sex, age, race/ethnicity, or tobacco use in these models.
Table 4 Total energy expenditure per week and risk of ischemic stroke in the Northern Manhattan Study
DISCUSSION
We found that engaging in moderate- to heavy-intensity physical activity (such as jogging, tennis, or swimming) was associated with a lower risk of ischemic stroke, but that light activity (such as walking) was not. Only 19.7% of our participants engaged in moderate- to heavy-intensity activity. We also found that the protective effect of moderate- to heavy-intensity activity was only present for men. There was a possible dose-response relationship, with a weak trend toward a protective effect in the light-intensity category and a stronger effect for the moderate to heavy activity.
One possible explanation for physical activity being protective against ischemic stroke is its modulation of conventional medical risk factors. The protective effect of physical activity, however, remained after adjusting for these medical comorbidities. We cannot exclude the possibility of residual confounding, however. Physical activity has independent health benefits through modulation of inflammation, endothelial function, and vascular reactivity.19 Our analyses provide evidence that the intensity of physical activity is more strongly protective than the absence of activity or the calculated energy expended. Our finding that the protective effect of energy expenditure is modified by intensity of physical activity has been noted in prior studies.11 One possible explanation for intensity modifying the protective effect of energy expenditure relates to the manner in which the exposure was measured. We used a self-report questionnaire, and participants may have been better able to recall the actual amount of physical activity they performed depending on the intensity of activity they chose or could engage in.
Our results were notable for the presence of an interaction between moderate to heavy activity and sex. We found that the protective effect of physical activity was only present in men, a finding also noted in the Framingham Study.9 Observational studies among men have found protective effects of physical activity.11,20,21 Women were more likely to be physically inactive in our study, a phenomenon noted in prior studies starting from young adulthood,22 and our study may therefore be underpowered to detect more subtle protective effects among women. Alternatively, competing causes or unmeasured confounders, such as dietary patterns in men vs women or the use of hormone therapy in more active women,23 may be masking the association.
Our prospective study results are contrary to some other studies, including our earlier case-control study, which found that even engaging in light-intensity activity, such as leisure walking, reduces the risk of ischemic stroke.5,12,21,24 It is plausible that stroke cases in our case-control study underreported light physical activity (i.e., recall bias). In the Nurses’ Health Study and the Women’s Health Initiative Observational Study, even mild intensity activity as measured by walking was associated with a reduction in stroke risk.25,26 These studies included smaller proportions of Hispanics and blacks and had large sample sizes. The women in our study were more likely to be older, nonwhite, overweight, and diabetic and to have less than a high school education. Given our smaller sample size, the study also may have been underpowered to detect more subtle differences in the light-intensity activity group. In the Atherosclerosis Risk in Communities Study, leisure-time physical activity (as measured by the Baecke questionnaire) was not found to be protective against ischemic stroke overall, and there was no evidence of effect modification by sex.7 Our study used a different instrument to measure physical activity, and it included Hispanics and a higher proportion of subjects with diabetes. Our cohort is also older compared with others in which both intermediate and heavy activity were protective against stroke.8 We did not analyze stroke mortality, which some have found to be reduced in more physically active individuals,6 whereas others have not.27
This analysis has some important limitations. We did not assess occupational physical activity in a large proportion of the cohort; the majority of our participants, however, were retired. We used a self-reported physical activity questionnaire, which may be subject to information bias due to misclassification. In a prior analysis, our study had found a good correlation between physical activity reported by participants and their family, making this less likely. We also did not include in this analysis trends over time in the physical activity pattern of our participants. Our study also did not include more objective measures of fitness, which others have found to be protective, and which may be less influenced by known or unmeasured confounders.28–30 The differences between prior studies of objective measures and our own may be due to misclassification or to an actual difference in our population. Our questionnaires may allow subjects to accurately recall what type of activity they perform, but perhaps not the frequency or duration of various activities. Future studies using objective measures of fitness in older, urban-dwelling, and nonwhite populations are required to help address this difference.
Finally, the intensity of physical activity that our participants engaged in may not be related to choice as much as ability. In older populations, the ability to engage in more physically intense activities may be more indicative of overall well-being or the absence of frailty.31 Conversely, the protective effects of physical activity may have been related to prevention of frailty, which has been reported to be an important cardiovascular disease risk factor in the elderly.32,33 Our study did not collect information often used to ascertain frailty, such as walking speed, slowness, or weight loss.34
Nonetheless, our study has important public health implications and adds to the body of literature on the multiple health benefits of exercise even in older individuals.3,35 Engaging in moderate to heavy activities may be an important component of primary prevention in populations such as ours. Physical inactivity was very common in our cohort and it is likely to be so in other elderly urban dwellers, living within a constricted space, who are also likely to be socially isolated. Interventions targeted to high-risk populations such as ours to improve physical activity continue to be important.
DISCLOSURE
Dr. Willey has received research support from the NIH/NINDS [T 32 NS 07153 (Trainee)]. Ms. Moon reports no disclosures. Dr. Paik has received honoraria for lectures or educational activities not funded by industry. Dr. Boden-Albala serves on speakers’ bureaus for the American Heart Association and National Stroke Association. Dr. Sacco has received speaker honoraria from Boehringer Ingelheim and Sanofi-aventis; served as a past consultant to Boehringer Ingelheim, Sanofi-aventis, and GlaxoSmithKline; and receives research support from the NIH [NINDS R37 NS29993 (PI), NINDS R01 NS 040807 (PI), NINDS R01 047655 (Coinvestigator), and NHLBI HC-98-08-HC-83169701 (Coinvestigator)]. Dr. Elkind serves as Resident and Fellow Section Editor for Neurology; serves as a consultant to Bristol-Myers Squibb/Sanofi Pharmaceuticals Partnership, GlaxoSmithKline, Jarvik Heart, Tethys Bioscience, Inc., and Daiichi-Sankyo; serves on speakers’ bureaus for Boehringer-Ingelheim, Inc. and Bristol-Myers Squibb/Sanofi Pharmaceuticals Partnership; receives research support from diaDexus, Inc., Bristol-Myers Squibb/Sanofi Pharmaceuticals Partnership, and the NIH/NINDS [R01 NS050724 (PI), NS048134 (PI), P50 NS049060 (Project PI), R37 NS029993 (Co-PI), R01 NS55809 (Coinvestigator), and R01 NS062820 (Coinvestigator)]; and has given expert testimony on behalf of Merck Serono (Vioxx® litigation), Pfizer Inc. (Shiley valve and Celebrex®/Bextra® litigation), and Novartis (Zelnorm® and stroke litigation).
Address correspondence and reprint requests to Dr. Joshua Z. Willey, 710 West 168th St., Box 30, New York, NY 10032 jzw2@columbia.edu
Supported by NIH/NINDS R37 NS 29993.
Disclosure: Author disclosures are provided at the end of the article.
Received May 22, 2009. Accepted in final form August 25, 2009.
REFERENCES
- 1.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics–2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2008;117:e25–e146. [DOI] [PubMed] [Google Scholar]
- 2.Gorelick PB. Stroke prevention: an opportunity for efficient utilization of health care resources during the coming decade. Stroke 1994;25:220–224. [DOI] [PubMed] [Google Scholar]
- 3.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 2007;116:1094–1105. [DOI] [PubMed] [Google Scholar]
- 4.Thompson PD, Buchner D, Pina IL, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Circulation 2003;107:3109–3116. [DOI] [PubMed] [Google Scholar]
- 5.Bijnen FC, Caspersen CJ, Feskens EJ, Saris WH, Mosterd WL, Kromhout D. Physical activity and 10-year mortality from cardiovascular diseases and all causes: the Zutphen Elderly Study. Arch Intern Med 1998;158:1499–1505. [DOI] [PubMed] [Google Scholar]
- 6.Ellekjaer H, Holmen J, Ellekjaer E, Vatten L. Physical activity and stroke mortality in women: ten-year follow-up of the Nord-Trondelag Health Survey, 1984–1986. Stroke 2000;31:14–18. [DOI] [PubMed] [Google Scholar]
- 7.Evenson KR, Rosamond WD, Cai J, et al. Physical activity and ischemic stroke risk: the Atherosclerosis Risk in Communities Study. Stroke 1999;30:1333–1339. [DOI] [PubMed] [Google Scholar]
- 8.Hu G, Sarti C, Jousilahti P, Silventoinen K, Barengo NC, Tuomilehto J. Leisure time, occupational, and commuting physical activity and the risk of stroke. Stroke 2005;36:1994–1999. [DOI] [PubMed] [Google Scholar]
- 9.Kiely DK, Wolf PA, Cupples LA, Beiser AS, Kannel WB. Physical activity and stroke risk: the Framingham Study. Am J Epidemiol 1994;140:608–620. [DOI] [PubMed] [Google Scholar]
- 10.Lee CD, Folsom AR, Blair SN. Physical activity and stroke risk: a meta-analysis. Stroke 2003;34:2475–2481. [DOI] [PubMed] [Google Scholar]
- 11.Lee IM, Paffenbarger RS Jr. Physical activity and stroke incidence: the Harvard Alumni Health Study. Stroke 1998;29:2049–2054. [DOI] [PubMed] [Google Scholar]
- 12.Sacco RL, Gan R, Boden-Albala B, et al. Leisure-time physical activity and ischemic stroke risk: the Northern Manhattan Stroke Study. Stroke 1998;29:380–387. [DOI] [PubMed] [Google Scholar]
- 13.Sacco RL, Anand K, Lee HS, et al. Homocysteine and the risk of ischemic stroke in a triethnic cohort: the Northern Manhattan Study. Stroke 2004;35:2263–2269. [DOI] [PubMed] [Google Scholar]
- 14.Moss AJ, Parsons VL. Current estimates from the National Health Interview Survey: United States, 1985. Vital Health Stat 10 1986:i–iv, 1–182. [PubMed] [Google Scholar]
- 15.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 2000;32:S498–S504. [DOI] [PubMed] [Google Scholar]
- 16.Siconolfi SF, Lasater TM, Snow RC, Carleton RA. Self-reported physical activity compared with maximal oxygen uptake. Am J Epidemiol 1985;122:101–105. [DOI] [PubMed] [Google Scholar]
- 17.Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial. TOAST Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993;24:35–41. [DOI] [PubMed] [Google Scholar]
- 18.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–3421. [PubMed] [Google Scholar]
- 19.Green DJ, O’Driscoll G, Joyner MJ, Cable NT. Exercise and cardiovascular risk reduction: time to update the rationale for exercise? J Appl Physiol 2008;105:766–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abbott RD, Rodriguez BL, Burchfiel CM, Curb JD. Physical activity in older middle-aged men and reduced risk of stroke: the Honolulu Heart Program. Am J Epidemiol 1994;139:881–893. [DOI] [PubMed] [Google Scholar]
- 21.Lee IM, Hennekens CH, Berger K, Buring JE, Manson JE. Exercise and risk of stroke in male physicians. Stroke 1999;30:1–6. [DOI] [PubMed] [Google Scholar]
- 22.Caspersen CJ, Pereira MA, Curran KM. Changes in physical activity patterns in the United States, by sex and cross-sectional age. Med Sci Sports Exerc 2000;32:1601–1609. [DOI] [PubMed] [Google Scholar]
- 23.Cauley JA, Cummings SR, Black DM, Mascioli SR, Seeley DG. Prevalence and determinants of estrogen replacement therapy in elderly women. Am J Obstet Gynecol 1990;163:1438–1444. [DOI] [PubMed] [Google Scholar]
- 24.Paffenbarger RS Jr, Hyde RT, Wing AL, Steinmetz CH. A natural history of athleticism and cardiovascular health. JAMA 1984;252:491–495. [PubMed] [Google Scholar]
- 25.Hu FB, Stampfer MJ, Colditz GA, et al. Physical activity and risk of stroke in women. JAMA 2000;283:2961–2967. [DOI] [PubMed] [Google Scholar]
- 26.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med 2002;347:716–725. [DOI] [PubMed] [Google Scholar]
- 27.Woo J, Ho SC, Yuen YK, Yu LM, Lau J. Cardiovascular risk factors and 18-month mortality and morbidity in an elderly Chinese population aged 70 years and over. Gerontology 1998;44:51–55. [DOI] [PubMed] [Google Scholar]
- 28.Agnarsson U, Thorgeirsson G, Sigvaldason H, Sigfusson N. Effects of leisure-time physical activity and ventilatory function on risk for stroke in men: the Reykjavik Study. Ann Intern Med 1999;130:987–990. [DOI] [PubMed] [Google Scholar]
- 29.Kurl S, Laukkanen JA, Rauramaa R, Lakka TA, Sivenius J, Salonen JT. Cardiorespiratory fitness and the risk for stroke in men. Arch Intern Med 2003;163:1682–1688. [DOI] [PubMed] [Google Scholar]
- 30.Hooker SP, Sui X, Colabianchi N, et al. Cardiorespiratory fitness as a predictor of fatal and nonfatal stroke in asymptomatic women and men. Stroke 2008;39:2950–2957. [DOI] [PubMed] [Google Scholar]
- 31.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–M156. [DOI] [PubMed] [Google Scholar]
- 32.Masaki KH, Schatz IJ, Burchfiel CM, et al. Orthostatic hypotension predicts mortality in elderly men: the Honolulu Heart Program. Circulation 1998;98:2290–2295. [DOI] [PubMed] [Google Scholar]
- 33.McGinn AP, Kaplan RC, Verghese J, et al. Walking speed and risk of incident ischemic stroke among postmenopausal women. Stroke 2008;39:1233–1239. [DOI] [PubMed] [Google Scholar]
- 34.Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 2004;59:255–263. [DOI] [PubMed] [Google Scholar]
- 35.Blair SN, Haskell WL. Objectively measured physical activity and mortality in older adults. JAMA 2006;296:216–218. [DOI] [PubMed] [Google Scholar]


