Abstract
Psychosocial stress is a nontraditional risk factor for cardiovascular morbidity and mortality that may respond to behavioral or psychosocial interventions. To date, studies applying such interventions have reported a wide range of success rates in treatment or prevention of cardiovascular disease (CVD). The authors focus on a natural medicine approach that research indicates reduces both psychosocial and traditional risk factors for cardiovascular disease—the Transcendental Meditation (TM) program. Randomized controlled trials, meta-analyses, and other controlled studies indicate this meditation technique reduces risk factors and can slow or reverse the progression of pathophysiological changes underlying cardiovascular disease. Studies with this technique have revealed reductions in blood pressure, carotid artery intima-media thickness, myocardial ischemia, left ventricular hypertrophy, mortality, and other relevant outcomes. The magnitudes of these effects compare favorably with those of conventional interventions for secondary prevention.
Index Terms: cardiovascular disease, psychosocial stress, review, Transcendental Meditation
A growing body of research supports the proposal that psychosocial stress is an important risk factor for cardiovascular disease (CVD) as reviewed in Part 1 of this series1 and elsewhere.2–5 Psychosocial stress contributes not only to CVD risk factors (eg, high blood pressure, elevated cholesterol, insulin resistance/diabetes, high use of tobacco and alcohol, and stress reactivity of the cardiovascular system), but it is also implicated in the progression of CVD. All major stages along a chain of pathophysiological events that culminate in mortality appear to be affected, including clustering of traditional risk factors, endothelial function, atherosclerosis, myocardial ischemia, plaque rupture, thrombosis, and lethal arrhythmias.1
The Transcendental Meditation (TM) Program as an Intervention for Psychosocial Stress and CVD
Evidence for the multiple roles of psychosocial stress in CVD reviewed elsewhere6–9 indicates that interventions designed to address psychosocial factors might be expected to reduce recurrent CVD events. This appears to be the case. Trials of a variety of psychosocial interventions have found reductions in recurrent cardiac events, sometimes surpassing 50%. However, such large effects tend not to be replicated in the larger follow-up studies, and some results have been found to be short-lived.9–11
The cause of reported discrepancies in outcomes has not been directly demonstrated. However, quantitative meta-analyses of various approaches, including different types of meditation, suggest that the specific psychosocial intervention used may be a critical factor (see Orme-Johnson & Walton12 for review). Murphy13 reached a similar conclusion after examining a large body of research on stress management in work settings. A review of all meta-analyses on stress-reduction approaches available in 1997 (10 meta-analyses covering a total of 475 studies and 21 approaches) led us to conclude not only that different approaches have different effects, but also that those based on traditions spanning centuries (eg, the Vedic and Zen traditions) tended to prove more beneficial than their recent, clinically devised counterparts.12
Meditation techniques vary widely, as do other psychosocial interventions, in what takes place during the sessions and in their effectiveness at producing measured outcomes.12 According to Murphy and associates’14 updated bibliography of research on meditation, the Transcendental Meditation (TM) program has been investigated more extensively than any other method. This is especially true of research in the area of CVD. Because meta-analyses as well as direct comparisons have revealed that the TM technique is 2 to 3 times as effective as comparison approaches on most outcomes, we focus only on the TM program in this article.
Nature of the TM Program
The main component of the TM program is a systematic, psychophysiological procedure based in the ancient Vedic tradition.15 The technique, which is understood to be a comprehensive means of enhancing human health and awareness, is a principal component of the Maharishi Vedic Medicine program, a natural health-promotion technology that includes all 40 different approaches of the Vedic tradition.16–18 Five volumes of collected papers contain 430 of the more than 600 published studies on the TM program,19–21 and volumes 6 and 7 are in preparation. Many of these papers report research relevant to CVD. However, because of space limitations, we focus primarily on studies directly examining CVD risk factors and other CVD-related outcomes (a broader range of TM research literature can be found elsewhere15,22,23).
The TM program is taught by trained professionals through a standardized instruction procedure.24 Over the past 40 years, more than 6 million people around the world have been instructed in the program, which continues to be offered in larger cities in most countries. The technique is easy to learn and enjoyable to practice. Generally, compliance with the recommended practice of 15 to 20 minutes twice a day is high. Part 3 of this series, to be published in a future issue of Behavioral Medicine, will provide a detailed summary of characteristics of the TM program and describe how it is taught.
A Working Model of Psychosocial Stress and CVD
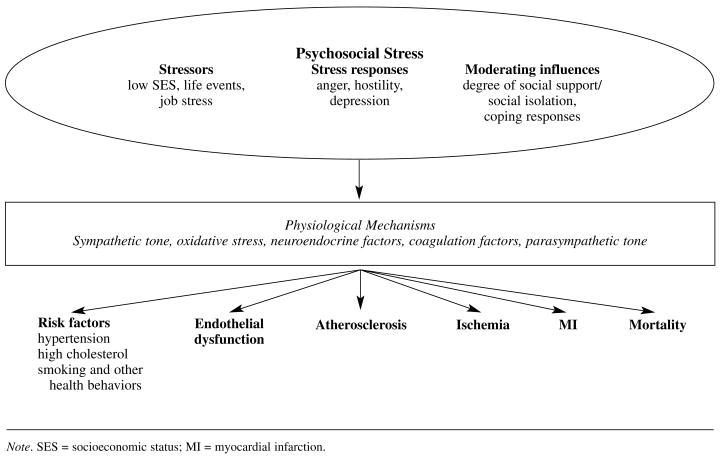
In this article, we elaborate on our model of the etiology and progression of CVD1 that we described in Part 1 of this series to illustrate some of the possible interactions and pathways involved in the effects of psychosocial interventions on CVD morbidity and mortality outcomes (see Figure 1). In brief, psychosocial stress associated with low socioeconomic status (ie, low levels of education, occupation, and income),25 adverse life events (eg, job loss, bereavement, and divorce),26 and high job strain27,28 may contribute to emotional and behavioral responses such as anger, hostility, depression, anxiety, and social isolation.
FIGURE 1.
Behavioral model of psychosocial stress and cardiovascular disease.
These maladaptive responses, in turn, have a negative impact on the cardiovascular system through physiologic mechanisms such as sympathetic hyperactivity, oxidative stress, and neuroendocrine imbalances.5 Each of these physiologic mechanisms may influence 1 or more of the traditional cardiovascular risk factors and increase cardiovascular morbidity and mortality. Psychosocial moderators such as social support and coping strategies can play an important role in modulating or preventing maladaptive behaviors.25 In this model, the TM program might best fit under the heading of moderating influences, altering the psychological effects of stressors, but evidence also suggests that it can have direct effects on physiological systems that mediate the stress response. Much research remains to be done, however, to elucidate the physiological and psychological mechanisms responsible for the beneficial effects of the TM program and the relationship of these effects to those of other moderating influences and other approaches to psychosocial intervention. (Part 3 of this series will provide a discussion of the mechanisms mediating the effects of this program.)
Review of TM Research on CVD Risk Factors, Morbidity, and Mortality
This review focuses on all controlled studies in the last 15 years, located by computer searches through May 2002. We conducted searches using PubMed (containing citations from Medline and several other sources), FirstSearch (containing citations from 59 different indexes), and Electronic Library. Because of the large number of controlled studies in the areas of substance abuse and psychological indicators of stress, we restricted our reviews of these areas to quantitative meta-analyses and randomized controlled trials.
The data in Table 1 summarize all references found on effects of the TM program on traditional and putative risk factors for CVD29 and provide the citation, field location, study design, sample size, control intervention(s), follow-up period, measures, and outcomes. We performed searches under each risk factor. The meta-analyses and randomized controlled trials of the effects of the TM program on the signs or consequences of psychosocial stress, including various categories of psychopathology and mental and psychological health, are listed in Table 2. The data in Table 3 summarize studies reflecting effects of the program on the mechanisms or physiological consequences of stress that are thought to contribute to CVD, and the data in Table 4 summarize studies on the effects of the program on CVD morbidity and mortality. Because of space limitations, we describe the collective outcomes and notable strengths or weaknesses of the studies in the text.
TABLE 1.
Controlled Research on Effects of the Transcendental Meditation (TM) Program on Risk Factors for CVD, 1987–2002
| Citation, field location, design | Participants | Intervention | Follow-up period | Measure | Result |
|---|---|---|---|---|---|
| High BP | |||||
| Alexander et al, 198932 Boston, MA RCT |
Residents of homes for the elderly, age M = 81 y (N = 73) 78% women |
TM (n = 20); MT (n = 21); MR (n = 21) no treatment control (n = 11, 22 for survival) |
3 mo for most variables 36 mo for survival |
SBP, survival, and other health-related variables; cognitive functioning, personality, and self-report measures, regularity of practice | TM reduced SBP more than did MT, MR, and C (contrast coefficients of 3, 1, −2, and −2, respectively, p < .01); similar results obtained with survival rates, mental health, paired associate learning, 2 measures of cognitive flexibility and ratings of behavioral flexibility, aging, and treatment efficacy |
| Schneider et al, 199530 Oakland, CA RCT |
Inner-city older African Americans with hypertension (N = 127) |
TM (n = 36); progressive muscle relaxation (PMR, n =37), health education controls (EC, n = 38) | 3 mo | BP changes from baseline to final follow-up, measured by blinded observers; secondary measures: linear BP trends, changes in home BP, intervention compliance | Compared with HE controls, TM reduced SBP by 11 mm Hg, and DBP by 6 mm Hg (p <.0003 and .00005, respectively); compared with PMR, TM reduced both SBP and DBP by 6 mm Hg (p < .02 & .03, respectively); linear trend analysis confirmed these patterns; compliance = 97% for TM and 81% for PMR |
| Alexander et al, 199631 Oakland, CA RCT |
Inner-city older African Americans with hypertension (N = 127) | TM (n = 22 women, 19 men) (PMR, n = 22 women, 20 men) HE controls (n = 30 women, 14 men) |
3 mo | Subgroup analysis of BP changes in Schneider et al, 1995, grouped by sex and by high and low risk on: psychosocial stress, obesity, alcohol use, physical inactivity, sodium-potassium ratio, and a composite measure | Compared with HE controls, TM reduced SBP in women (10 mm Hg, p < .01) and in men(13 mm Hg, p < .01) and DBP in women (6 mm Hg, p < .01) and men (8 mm Hg, p < .001); TM significantly reduced SBP and DBP in all risk subgroups compared with same risk sub-groups of HE controls |
| Wenneberg et al, 199733 Iowa City, IA RCT |
Young 18 y–34 y normotensive White American males (N = 39) |
TM (n = 20); Education control (n = 19) | 4 mo | Ambulatory BP from 1300 hours to 2200 hours on 1 day | Compared with controls, TM decreased ambulatory BP by 9 mm Hg in the high-compliance subgroup (p = .04) |
| Barnes et al, 200134 Augusta, GA RCT |
Adolescents with high normal BP (N =35; 34 African Americans and 1 White American) | TM (n = 17); Lifestyle education (n = 18) | 2 mo | Resting BP; pretest demographics; stress responsiveness (see below) | TM reduced resting SBP (7.5 mm Hg, p < .03) relative to controls and reduced the stress responsiveness (see below) |
| Lipids and Cholesterol | |||||
| De Armond, 199635 Kansas City, MO CS |
Managers and executives of a medical equipment developer and manufacturer (N = 76) | TM (n = 38) vs no-treatment controls matched for company rank (n = 38) | 3 mo | Fasting total cholesterol, BP, self-reported stress measures, observer-reported stress measures | TM significantly reduced total cholesterol relative to controls (p = .03) and improved self-reported and observer-reported stress measures (p < .002–.05) |
| Schneider et al, 199836 Fairfield, IA OS |
Older, normally healthy, community-dwelling volunteers, age range 56 to 74 y, M = 67 (N = 41) | Long-term (average age 16.5 y) practitioners of TM (n =18) vs age-, sex-, and education-matched nonpractitioner controls (n = 23) | NA | Lipid peroxides in serum; intakes of fat, vitamins, red meat; level of cigarette use | TM group was 15% lower in lipid peroxides (p = .026) and consumed less red meat (p <.001) |
| Calderon, 200037 Los Angeles, CA RCT |
African American adults with mild or medication-controlled hypertension (N = 66) | TM (n = 34) vs HE controls (n = 32); mean cholesterol was 213 mg/dL | 6 mo | Fasting cholesterol (total, LDL, HDL) and triglycerides; pretest demographics; diet, exercise, and physiologic measures | No significant effects of TM on any cholesterol or lipid variable when compared with controls by ANCOVA; controls improved significantly more on intake of total fat, cholesterol(trend), fiber, saturated fat, % calories from fat, % calories from sweets, total caloric intake |
| Tobacco and Other Substance Abuse | |||||
| Alexander et al, 199438 Various locations, USA & abroad QMA, controlling for strength of study design |
19 TM studies; adolescents, college students, working adults, elderly African Americans, criminal offenders, Vietnam veterans, and skid-row alcoholics (N = 4,524) | TM practice vs mixed controls, some no-treatment, some active treatment | 9.7 mo average | Use of alcohol, cigarettes, and illicit drugs | Compared with controls, TM effect sizes were alcohol use, .55 (p = .0008); cigarette use, .87 (p = .00003); illicit drug use, .83 (p = .000005) |
| High Reactivity or Shear Stress Sheer | |||||
| Wenneberg et al, 199733 Iowa City, IA RCT |
Young (ages 18–34 y) normotensive White American males (N =39) | TM (n = 20); Education control (n = 19) | 4 mo | Stress reactivity of BP and heart rate to 3 laboratory stressors and a simulated public speaking test | Compared with controls, TM did not affect BP or heart rate reactivity to mental arithmetic, mirror image tracing, or isometric handgrip, but increased SBP reactivity to public speaking stress in the high compliance participants (p = .06). |
| Barnes et al, 200134 Augusta, GA RCT |
Adolescents with high normal BP (N =35: 34 African Americans and 1 White American) | TM (n = 17); Lifestyle education (n = 18) | 2 mo | Stress responsiveness of BP, heart rate, cardiac output, and peripheral resistance; pretest demographics | Compared with controls, TM reduced the stress responsiveness of: SBP (9 mmHg, p <.03), cardiac output (p < .01), heart rate (p < .03), and DBP (p < .07) |
Note. RCT = randomized controlled trial; OS = observational study; QMA = quantitative meta-analysis; CS = controlled study; BP = blood pressure; SBP = systolic blood pressure; DBP = diastolic blood pressure; PMR = progressive muscle relaxation; HE = health education; MT = mindfulness training; MR = mental relaxation; C = control; LDL = low-density lipoprotein; HDL = high-density lipoprotein; NA = not applicable; OM = other meditation; OR = other relaxation; PR = progressive relaxation.
TABLE 2.
Controlled Research on the Ability of the Transcendental Meditation (TM) Program to Change Psychologic Indicators or Consequences of Stress, 1987–2002
| Citation, field location, design | Participants | Intervention | Follow-up period | Measure | Result |
|---|---|---|---|---|---|
| Eppley et al, 198947 Various locations in USA & abroad QMA, controlling for strength of design, experimenter bias, pretest demographics, pretest anxiety |
All studies (146 independent outcomes) of meditation and relaxation on trait anxiety | TM (35 outcomes), other meditation (OM, 44 outcomes), progressive relaxation (PR, 30 outcomes), and other relaxation (OR, 37 outcomes) | Avg intervention (mo) TM =2.5, OM = 1.8, PR = 1.6, OR = 1.4 | Scores on standardized instruments measuring trait anxiety | Mean effect size for TM (.70) was larger than for OM (.28, p< .001), for PR (.38, p < .005), and for OR (.40, p < .005) |
| Gaylord et al, 198948 Pine Bluff, AR RCT |
African American volunteers, mostly college students (N = 83) | TM (n = 25), PMR (n = 29), cognitive-based self-improvement (CS, n = 29) | 1 y | Measures of mental health, anxiety, neuroticism, and electrophysiological variables, including habituation of the skin potential response to a noxious sound | TM (p = .02) and PMR (p = .04) each increased a general mental health factor, compared with CS, with state anxiety and neuroticism the most improved; TM shortened the time to habituation of skin potential response, compared with CS |
| Alexander et al, 199149 Various locations in USA & abroad QMA, controlling for duration of treatment and strength of experimental design |
All studies (42 treatment outcomes) on effects of TM on self-actualization, a measure of psychological health | TM (18 independent outcomes), assorted comparison groups (24 outcomes) | 5 wk–3.5 y | Scores on Shostrom’s Personal Orientation Inventory (14 studies) or alternate instruments (4 studies); factor analysis gave 3 factors: “affective maturity,” “integrative perspective on self and world,” and “resilient sense of self” | Effect size for TM was .78, which was 3 times the size for other forms of meditation (.26) and for relaxation techniques (.27) (p < .0002); individual factors also showed 3-fold greater change in the TM group (p < .0001, .005, .005, respectively) |
| Ferguson, 199150 Various locations in USA & abroad QMA, controlling for setting and strength of design |
51 studies with 404 independent outcomes (N = 9,470) | TM effects (160 outcomes) compared with effects of other meditation and relaxation techniques | 9.7 mo (avg) | All affective measures (eg, anxiety, self-concept, etc) were included | TM effect size (.62 or .70) was more than 2 times the size of comparison groups, regardless of experimental design used |
| Alexander et al, 199438 (see details under Tobacco and Other Substance Abuse, T-1) Various locations in USA & abroad QMA |
14 studies on abusers of alcohol or other substances that also examined the decrease of negative psychological outcomes; 10 studies on abusers that also examined increases in positive psychological outcomes | TM practice vs mixed controls (some no-treatment, some active treatment) | 10 mo (avg) | Decrease of negative psychological outcomes (eg, depression, anger, hostility, and anxiety); increase of positive psychological outcomes (eg, self- concept, internal locus of control) | TM reduced negative psychological outcomes relative to controls, with effect size of .64; TM increased positive psychological outcomes, with effect size of .51 (p = 2 ×10−6) |
Note. See note in Table 1 for abbreviations used in these studies.
TABLE 3.
Controlled Research on the Ability of the Transcendental Meditation (TM) Program to Change Physiologic Indicators or Consequences of Stress, 1987–2002
| Citation, field location, design | Participants | Intervention | Follow-up period | Measure | Result |
|---|---|---|---|---|---|
| Dillbeck & Orme-Johnson, 198752 Various locations in USA & abroad QMA |
31 studies, normal adult populations | Acute and longitudinal effects of TM vs eyes-closed rest: the meta-analysis for each variable had at least 5 studies on TM and at least 3 on eyes-closed rest | NA | Basal skin resistance, skin resistance responses, respiratory rate, heart rate, and plasma lactate levels | The TM session had larger effects on basal skin resistance (p < .05), respiratory rate (p < .05), and plasma lactate (p < .01); significant pretest differences on 4 of the 5 variables (p < .01 – p < .05) |
| Gaylord et al, 1989 (See previous listing, Table 2.) Mills et al, 199054 Fairfield, IA CS |
Normally healthy, nonobese volunteers (N = 20, age M = 31 y) | Long-term (9 y) male practitioners of TM (n = 10) and age-matched male controls (n = 10) who practiced no behavioral technique | NA | Beta-adrenergic receptors, binding affinity, plasma NE and E, Type A behavior, exercise, and family history of high BP | TM group higher on high-affinity beta-adrenergic receptors (p = .009), but groups did not differ on total beta receptors, binding affinity, plasma NE and E, Type A behavior, exercise, or family history of hypertension |
| Alexander et al, 199355 Midwest, USA CS |
Normally healthy workers at 2 separate sites in the automotive industry (N = 86) | TM group (n = 45), controls matched by worksite, job position, and demographic and pretest characteristics (n = 41) | 3 mo | Skin resistance, psychological indicators of stress, job tension, job satisfaction, employee effectiveness, work/personal relationships, cigarette and hard liquor use | Regular practice of TM significantly improved scores in all areas of measurement, compared with controls; irregular practice of TM produced changes intermediate between the regular practice group and controls |
| Walton et al, 199556 Fairfield & Cedar Falls, IA CS |
Normally healthy volunteers (N = 55, age M = 29 y) | Long-term (8.5 years) practitioners of TM (n = 22) and age-matched controls (n = 33) who practiced no stylized technique for stress reduction | NA | Self-report instruments and urinary indicators of chronic stress, specifically: POMS, STAI, and excretion rates of cortisol, aldosterone, 5HIAA, VMA, DHEAS, and the ions of Na, K, Ca, Mg, and Zn | TM group was lower on mood disturbance and anxiety (p < .01 and .05, respectively) and also on excretion of cortisol (p = .002), VMA (p < .001), aldosterone (p = .04), and electrolytes (except Mg, K; p < .001 to .02) and higher on excretion of 5HIAA (p < .01), and DHEAS (p < .01), all consistent with lower levels of stress |
| Levitsky, 199757 Iowa City, IA RCS |
Healthy male volunteers (N = 49, age range = 18–32 y) | Randomly assigned participants completing posttests (TM, n = 16; control, n = 19) | 4 mo | Changes in urinary indicators of chronic stress, specifically excretion rates of cortisol, aldosterone, 5HIAA, DHEAS, and the ions of Na, K, Ca, Mg, and Zn | TM significantly reduced cortisol excretion (p = .001, within-group) and electrolyte excretion (p < .05, between-group), and increased 5HIAA excretion (p = .03, within-group), consistent with a reversal of effects of chronic stress |
| MacLean et al, 199758 Iowa City, IA RCS |
Healthy male volunteers (N = 49, age range = 18–32 y) | Randomly assigned participants completing posttests (TM, n = 16; control, n = 13) | 4 mo | Plasma levels of cortisol, TSH, GH, and testosterone at baseline and during 3 laboratory stressors, all in the morning | TM reduced baseline cortisol (p = .04) and avg. cortisol (p = .04), increased cortisol response to stress (p = .02), and affected TSH, GH, and testosterone in a manner opposite to effects of stress. |
| Infante et al, 199859 Granada, Spain CS |
Healthy volunteers (TM group vs controls, N = 27) | Seasoned TM practitioners (n = 18) compared with nonpractitioner controls (n = 9) | NA | Plasma levels of cortisol, beta-endorphin, and ACTH at 0900 and 2000 h | TM group showed no diurnal rhythm in beta-endorphin and ACTH; a change in feedback sensitivity is suggested |
| Infante et al, 200160 Cordoba, Spain CS |
Healthy volunteers (TM group vs controls, N = 35) | Seasoned TM practitioners (n = 19) compared with nonpractitioner controls (n =16) | NA | Plasma levels of catecholamines (NE, E, and DA) at 0900 and 2000 h | Morning and evening NE and morning E were significantly lower in the TM group (morning NE, pg/mL: TM = 137, control = 237, p = .0001); (evening NE: TM = 120, control = 176, p = .009); (morning E: TM = 140, control 197, p = .02) |
| Hemodynamics | |||||
| Barnes et al, 199961 Augusta, GA CS |
Healthy, normotensive men and women (M age = 46 y, N = 32) | Long-term (22 y) practitioners of the TM program (n = 18), compared with nonpractitioner controls (n = 14) | NA | Hemodynamic variables were assessed before and during 2 periods: 20 min of eyes-open rest (both groups), 20 min of TM (TM group) or eyes-closed rest (control group) | During eyes-open rest and during TM or eyes-closed rest, the TM group significantly decreased SBP and total peripheral resistance and increased in cardiac output, relative to the control group (p < .004 to p < .04) |
Note. Abbreviations used are the same as those in Table 1, plus NE (norepinephrine), E (epinephrine), DA (dopamine), ACTH (adrenocorticotrophic hormone), TSH (thyroid stimulating hormone), GH (growth hormone), 5HIAA (5-hydroxyindoleacetic acid), VMA (vanillylmandelic acid), DHEAS (dehydroepiandrosterone sulfate).
TABLE 4.
Controlled Research on the Effects of the Transcendental Meditation (TM) Program on CVD Morbidity and Mortality, 1987–2002
| Citation, field location, design | Participants | Intervention | Follow-up period | Measure | Result |
|---|---|---|---|---|---|
| Castillo-Richmond et al, 200063 Los Angeles, CA RCT |
African American adults with hypertension (avg age 54 y, N = 60) | TM (n = 31); health education control (n = 29) | 7.5 mo | Mean carotid IMT across 6 sites; secondary outcomes: BP, total, HDL-, and LDL-cholesterol, exercise, weight, smoking, and other variables | TM reduced carotid IMT by .15 mm (10%) relative to controls (p = .04); no significant differences between groups on other variables, although within-group decreases in BP were significant |
| Fields et al, 200264 Chicago, IL RCT |
Normally healthy older White Americans (avg age 74 y, N = 46) | TM (along with Vedic diet, exercises, herbal supplements; n = 20); modern diet (exercise, multivitamins; n = 9); usual care only (n = 14) | 12 mo | Mean carotid IMT across 6 sites; secondary outcomes: BP, cholesterol and lipids, serum glucose, weight, BMI, and other variables | TM (with other Vedic approaches) reduced carotid IMT in a higher fraction of participants than did the modern treatment and usual care combined (p < .05); in a high-risk subgroup, TM reduced IMT by .34 mm (20%, p = .009) compared with usual care |
| Kondwani, 199866 Oakland, CA RCT |
African American adults with hypertension (N = 42) | TM (n = 22); health education controls matched on medication, gender, BP range (n = 20) | 12 mo | LVMI, BP, vitality, affect, behavioral/emotional control, sleep dysfunction, anxiety, and depression | Both TM and HE reduced LVMI (> 10%, p < .01), but only TM produced significant improvements in DBP and in most other measures |
| Zamarra et al, 199667 Buffalo, NY RCT |
Patients with documented coronary artery disease (N = 21) | TM (n = 12) vs waitlisted controls (n = 9) | 7.6 mo | Symptom-limited exercise tolerance tests after an overnight fast | TM significantly reduced exercise-induced ischemia, and increased exercise tolerance, maximum workload, and delay of onset of ST segment depression, relative to controls |
| Alexander et al, 198932 Boston, MA RCT |
Residents of homes for elderly (M age =81, N = 84); 78% women | TM (n = 20); mindfulness training (MT, n = 21); mental relaxation (MR, n = 21); no treatment control (C, n = 22) | 36 mo | Survival (and other health-related variables; see Table 1 under High Blood Pressure) | TM group showed 100% survival, compared with 87% for MT, 65% for MR, 77% for C & 62.6% for all those in the same institutions who were not assigned to groups, p < .00025 |
Reductions in Risk Factors for CVD
High Blood Pressure
Five studies of the effects of the TM program on blood pressure (BP) have been published in the last 15 years (see Table 1). Significant reductions of blood pressure—up to 13 mm Hg in systolic blood pressure (SBP) and 8 mm Hg in diastolic (DBP) were reported in each study, which was consistent with results of earlier studies.30,31 Four of these studies were independent randomized clinical trials (RCTs). The fifth study, also randomized, was a subgroup analysis of data from 1 of the 4 trials and therefore was not independent. Two of the RCTs were performed among African American participants and 2 among White Americans.
The ages of participants varied from study to study but ranged from adolescence to old age. The pretreatment BP also varied, including individuals whose levels were normal, high normal, and hypertensive (> 139 SBP and > 89 DBP). Most studies used resting BP in the laboratory, but 1 study also used ambulatory measurements. The greatest shortcoming of the RCTs on blood pressure so far is the relatively short time of follow-up—the longest was only 4 months.
Strong points of these studies were (1) their demonstration that the TM program can be effectively implemented in widely different populations, from African American adolescents to older African Americans in lower socioeconomic, inner-city communities, to a higher socioeconomic group of White Americans in homes for the elderly; (2) a generally high compliance with the program, with participants in an inner-city, older African American sample showing 97% compliance with the recommended twice daily home practice of the TM program30; (3) the demonstration of significant BP reductions in participants of both sexes and at both ends of the spectrum of CVD risk31; and (4) that the TM program was twice as effective in reducing the BP of hypertensive older African Americans as was progressive muscle relaxation, which itself lowered BP significantly.30,31 The TM program’s effects on blood pressure were also clinically significant, as inferred from trials on antihypertensive drugs in which similar reductions in blood pressure produced substantial reductions in cardiovascular morbidity and mortality.39,40
Lipids and Cholesterol
An earlier prospective, controlled study showed a 10% decline in plasma total cholesterol in medication-free, hypercholesterolemic volunteers without heart, renal, or thyroid disorders after 11 months on the TM program, compared with matched controls.41 The latest studies examined individuals who were less hypercholesterolemic than the participants in the earlier study (ie, pretreatment means for the later studies were 213 and 193 mg/dL, compared with 257 for the earlier study). De Armond’s study35 of executives and managers reported a significantly lower cholesterol level after 3 months of TM, compared with controls, despite the low pretest cholesterol level (mean of 193 mg/dL). The failure of the Calderon study37 to find a significant cholesterol reduction in the TM group compared with controls may have been a result of significant differences in dietary improvements. The health education controls received dietary instruction that resulted in significantly greater improvements in factors related to cholesterol levels. Those patients’ diet questionnaires showed greater reductions than did the TM group in total fat, cholesterol (trend), fiber, saturated fat, percentage of calories from fat, percentage of calories from sweets, and total caloric intake.
Growing research evidence suggests that it is not cholesterol levels per se that contribute to atherosclerosis and heart disease but rather the level of oxidized cholesterol and oxidized lipids.42,43 Excessive free radicals of oxygen are recognized as the cause of oxidation of lipids and cholesterol and are now supported as a major contributor to the mechanisms underlying atherosclerotic CVD.44 In our literature search, we found 1 study on the effects of the TM program in reducing oxidative stress.36 This observational study of lipid peroxide levels in serum suggested that the TM program reduces oxidative stress, an effect that, if large enough, might account for some of the reduced atherosclerosis resulting from the program (see Table 4).
Tobacco and Other Substance Abuse
Because the quantitative meta-analysis38 shown in Table 1 included all TM studies on substance abuse published in the last 15 years (and earlier), only this meta-analysis was listed. This meta-analysis of 19 studies combined results from 4,524 participants—adolescents, college students, working adults, elderly African Americans, criminal offenders, Vietnam veterans, and skid-row alcoholics—and controlled for strength of study design. The effect sizes obtained were large and highly significant, especially the .87 effect size for cigarette use.
High Reactivity or Shear Stress
Elevated cardiovascular responses to stress are considered by some to reflect higher risk for hypertension and CVD.45,46 Two studies have examined the effects of the TM program on this variable. One, in African American adolescents with high normal BP,34 found that 2 months of the TM program significantly reduced the reactivity of SBP, cardiac output, and heart rate, with a trend toward reduced DBP. The other study, conducted among male college students, found a significantly increased SBP reactivity after 4 months of TM in the high-compliance TM participants, compared with the high-compliance educational control participants, but the researchers did not measure other indicators of hemodynamic functioning in that study.33
Changes in Psychologic Indicators and Consequences of Psychosocial Stress
The ability of the TM program to prevent or reverse psychologic indicators or effects of psychosocial stress has been the most active area of TM research. Because hundreds of studies in this area are available, we have chosen to present only the quantitative meta-analyses and RCTs. Individual studies have reported that the program reduces negative indicators of stress (eg, anger, hostility, anxiety, and depression) and elevates positive indicators of mental health (eg, self-concept, internal locus of control, and self-actualization). See Hawkins23 for citations of many of the individual studies. Findings from meta-analyses controlled for strength of design, length of time practicing, and sometimes for experimenter bias and pretest demographics have confirmed most of the positive effects.
The meta-analyses found that the TM program was 2 to 3 times as effective as comparison programs, a finding that was consistent with the meta-analyses on substance abuse mentioned earlier.38 This differential between TM and comparison interventions was independent of the strength of the research design. The order of increasing design strength generally consisted of (from lowest to highest) participants being used as their own controls, nonrandom assignment to groups, random assignment to groups, and random assignment with low attrition (less than 15%).
Effects on Physiologic Mechanisms: Physiologic Indicators or Consequences of Stress
In our working model (Figure 1), we propose a variety of physiologic systems to mediate the effects of psychosocial stress on cardiovascular health. Several studies indicate that the TM program has effects on these systems. In addition to the possible indirect effects arising from changes in psychological states such as anxiety and anger, there may be direct, acute effects of the program on physiologic systems involved in the stress response,51,52 a possibility to be discussed further in Part 3 of this series.
Research in the last 15 years can be grouped in 3 main areas, as were those in previous investigations of the effects of the TM programs on physical indicators and consequences of stress: (1) activity of neuronal systems, especially the sympathetic nervous system (SNS); (2) activity of the hypothalamic-pituitary-adrenocortical (HPA) axis or other hormonal systems; and (3) effects on skin resistance (thought to reflect SNS activity). Although some earlier studies (eg, Michaels and associates53) did not find effects of the TM program in some of these areas, those studies involved small numbers of participants and may have lacked the statistical power to detect changes. Or, as suggested in a later review,52 the research design of these studies reduced the likelihood of seeing significant effects.
In the studies shown in Table 3, significant differences apparently due to the TM program were found in each of the earlier-mentioned 3 categories, using various research designs. Most of the results of these studies can be interpreted as indications that the TM program reduces stress or reduces the signs of chronic stress. Thus, results of 5 controlled studies (2 with random assignment of participants48,55) suggested reductions of sympathetic activity or sympathetic tone; results of 3 studies (2 with random assignment57,58) indicated there was reduced or more normal activity of the HPA axis; the findings in 2 studies (1 randomized57) suggested an increase of serotonergic activity along with a reduction in HPA-axis activity; and 1 quantitative meta-analysis indicated that a single TM program session affected basal skin resistance, respiratory rate, and plasma lactate in a direction opposite from stress.52 This meta-analysis also found that TM practitioners showed signs of lower chronic stress (ie, their values before the meditation session were significantly lower than those of controls on spontaneous galvanic skin responses, respiratory rate, heart rate, and plasma lactate). Because many studies have found that the effects observed during individual sessions of the TM program become increasingly more noticeable outside the sessions over time, these baseline differences probably reflect the cumulative effects of the regular twice-daily practice of the TM technique. Alternatively, in studies in which random assignment to a group was not used, the results might reflect preexisting physiologic differences specific to the individuals who volunteered for the study because they were interested in learning TM. This explanation is not likely, however, because authors of other studies (eg, Alexander and associates62) did not find that volunteers interested in learning TM were different from those not interested.
Hemodynamic Function
One observational study that compared long-term practitioners of the TM program with nonpractitioner controls provided evidence that the TM program led to reduction of hemodynamic vasomotor dysfunction (vasomotor dysfunction is one of the earliest signs of CVD).1 In an eyes-open rest period prior to the practice of TM (or of eyes-closed rest in controls), SBP and total peripheral resistance both significantly decreased, and cardiac output significantly increased in the TM group, relative to controls. During the TM session, decreases in SBP and total peripheral resistance and an increase in cardiac output occurred, but the latter change did not reach the p = .05 level.
Reductions in CVD Morbidity and Mortality
Because of research indicating that the TM program reduces CVD risk factors and the possible physiologic mediators between stress and CVD, reductions in morbidity and mortality also would be expected. Several studies have investigated such outcomes, and so far the research findings support this conclusion (Table 4).
Regression of Atherosclerosis
Authors of 2 reports of studies in which the TM program was a main component of the intervention reported reductions in atherosclerosis (Table 4). The first study involved the TM program as the only intervention, beyond routine care by the patient’s usual physicians.63 The most recent study, a multimodality intervention, used the TM program along with 3 other components of the approach called Maharishi Vedic Medicine (MVM).64 Both trials reported significant reductions in atherosclerosis, as indicated by carotid artery intima-media thickness, that is both a direct measure of carotid artery atherosclerosis, and a surrogate measure of coronary atherosclerosis.65 Participants in the more recent study were normally healthy, older White Americans, and the earlier study participants were African American individuals with hypertension.
Although the numbers of volunteers in these trials were small, the effects found were not, especially in subjects with risk factors for CVD. The results are not only statistically significant, but in all probability clinically significant. Based on other studies,68 these 10% to 20% reductions in intima-media thickness are likely to reflect as much as 33% reduction in the risk of myocardial infarction or stroke.
Measures of blood pressure and other risk factors in these subjects before and after intervention did not show significant differences between groups. However, the within-group decreases in these risk factors were significant enough to suggest they may have contributed to the reduced intima-media thickness. Other factors that were not measured also may be involved; thus additional research is necessary to clarify the mechanisms of these apparent reductions in atherosclerosis.
Left-Ventricular Hypertrophy
Regression of left ventricular mass (LVM) in animal models and in humans with left ventricular hypertrophy has been associated with improvement in diastolic function, reduced arrhythmias, and the preservation of systolic function.69 A randomized, controlled study of mildly hypertensive African Americans (DBP = 90 to 104 mmHg) in West Oakland, California, found that both the TM program and a modern Health Education program significantly reduced LVM and LVM indexed to body mass.66,70 However, the TM group also showed a significant mean decrease in DBP (p < .01), whereas the Health Education group did not change significantly in either diastolic or systolic blood pressure.
The decrease of LVM with these psychosocial interventions is large enough to be clinically significant, comparing favorably with studies on antihypertensive medications where the reduction in mass index was 8%–12%. A review of the literature indicates that a 10% decrease would substantially reduce the occurrence of clinical CVD events.71–73
Reduction in Myocardial Ischemia
In a pilot RCT of effects of the TM program on myocardial ischemia, Zamarra, et al.67 found that exercise-induced myocardial ischemia in coronary heart disease patients was reduced in the TM group relative to a control cardiac care group. The TM group also showed significant increases in exercise tolerance, maximum workload, and delay of onset of ST segment depression compared with the control group.
Reductions in Mortality
Arguably the most critical outcome measure for CVD is mortality. Mortality data on the TM program have been analyzed in several studies, but the results of only one study have yet appeared in a full-length article. Alexander et al. conducted a randomized controlled trial of ambulatory, non-institutionalized, elderly subjects in Massachusetts rest homes.32 Of these, 82% were women with high normal blood pressure and stage 1 hypertension. Mean age of the subjects at the outset was 81 years. Effects of the TM program were compared with effects of three other conditions: mindfulness training, a relaxation response-type technique, and usual medical care. Over a 3-year period, the survival rate in the TM group was 100%, compared with 87% for the mindfulness group, 77% for the usual care group, 65% for the relaxation-response group, and 62.5% for all others in the homes. The TM group also showed an improvement in SBP (−12 mm Hg) that was significantly larger than in the other groups, and improved most on multiple measures of cognitive and social functioning.
After 15 years, mortality data for the participants in this study were obtained from the National Death Index and analyzed using the Cox proportional hazards model for survival.74 Adjusting for age, gender, and pretest SBP, CVD mortality rate was significantly lower for the TM group than for the combined controls (p = 0.03, RR = 0.56). Risk for CVD mortality was 44% lower in the TM group. (Full-length publication of the follow-up study on this research was prevented by the untimely death of Dr Alexander, the principal investigator, in May 1998.)
Comment
The present summary of CVD-relevant research on the TM program provides important information for gauging this program’s effectiveness in treating and preventing CVD. The recent pilot randomized clinical trials showing reductions in atherosclerosis may represent the most significant evidence of the effectiveness of this program. Other results, indicating reduction of hemodynamics dysfunction, regression of left-ventricular mass, reduction of myocardial ischemia, decreased blood pressure, and reduced mortality, also support the ability of this program to positively affect the symptoms and progression of CVD.
All the randomized controlled trials and controlled studies listed here for CVD risk factors, morbidity, and mortality involved relatively small numbers of subjects and bear repetition. However, the research on factors representing psychosocial stress is more voluminous. The beneficial effects of the TM program on a wide spectrum of measures of psychosocial risk, such as anger and anger control, hostility, anxiety, depression, perceived health, and resistance resources, may help to explain significant effects of the TM program on CVD morbidity and mortality.
Part 3 of this series will include a discussion of issues important in further evaluating the practical use of this intervention in large-scale community settings. These include: (a) degree of standardization of instructional procedures, (b) availability of properly trained instructors, (c) degree of difficulty of the intervention—competency of patients to comply, (d) prior record of patient compliance with the intervention, (e) the cost of instruction, and (f) an empirically testable hypothesis or theory by which to understand the intervention and its effectiveness.
Summary and Synthesis
The importance of psychosocial stress as a contributor to CVD’s progression and prognosis is becoming widely recognized. Reductions in recurrent cardiac events and death have been reported for the most successful psychosocial approaches, and the magnitude of these reductions is similar to that of other proven therapies, such as lipid lowering, anti-platelet therapy, beta-blocker medication, and bypass surgery. The Transcendental Meditation program is a standardized behavioral intervention with holistic effects. The evidence summarized herein supports the ability of this program to reduce both psychosocial and traditional risk factors and to halt or reverse pathophysiological mechanisms underlying CVD progression and death. Other findings with regard to the community-wide application of this approach are covered in Part 3 of this series.
Acknowledgments
This review was partially funded by grants to Dr Schneider from the National Institutes of Health; National Center for Complementary and Alternative Medicine (Grant IP50AT00082-01); and the National Heart, Lung, and Blood Institute (Grants 2RO1-HL51519-05, RO1-HL48107, RO1-51519, and RO1-HL60703); as well as grants to Dr Bairey Merz from the National Heart, Lung, and Blood Institute (Grants 232HL07380 and HL49910).
Footnotes
Part 3 of this series will be published in a future issue of Behavioral Medicine.
References
- 1.Bairey Merz C, Dwyer J, Nordstrom C, Walton K, Salerno J, Schneider R. Psychosocial stress and cardiovascular disease: Pathophysiological links. Behav Med. 2002;27:141–146. doi: 10.1080/08964280209596039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tennant CC. Life stress and hypertension. J Cardiovasc Risk. 2001;8:51–56. doi: 10.1177/174182670100800107. [DOI] [PubMed] [Google Scholar]
- 3.Penninx BW, Beekman AT, Honig A, et al. Depression and cardiac mortality: Results from a community based longitudinal study. Arch Gen Psychiatry. 2001;58:221–227. doi: 10.1001/archpsyc.58.3.221. [DOI] [PubMed] [Google Scholar]
- 4.Tennant CC, Mclean L. Mood disturbances and coronary heart disease: Progress in the past decade. Med J Aust. 2000;172:151–152. doi: 10.5694/j.1326-5377.2000.tb125536.x. [DOI] [PubMed] [Google Scholar]
- 5.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 6.Bairey Merz C, Subramanian R. Efficacy of psychosocial interventions and stress management for reduction of coronary artery disease events. Preventive Cardiology. 1999;1:1–6. [Google Scholar]
- 7.Linden W, Stossel C, Maurice J. Psychosocial interventions for patients with coronary artery disease. Arch Intern Med. 1996;156:745–752. [PubMed] [Google Scholar]
- 8.Nunes E, Frank K, Kornfeld D. Psychologic treatment for Type A behavior pattern and for coronary artery disease: A meta-analysis of the literature. Psychosom Med. 1987;49:159–173. doi: 10.1097/00006842-198703000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Polk DM, Nordstrom CK, Dwyer J, Kop WJ, Krantz DS, Bairey Merz CN. Novel psychosocial factors and cardiovascular disease. In: Shah PK, editor. Risk Factors in Coronary Disease. New York: Marcel Dekker; 2003. [Google Scholar]
- 10.Frasure-Smith N, Lesperance F, Prince RH, et al. Randomized trial of home-based psychosocial nursing intervention for patients recovering from myocardial infarction. Lancet. 1997;350:473–479. doi: 10.1016/S0140-6736(97)02142-9. [DOI] [PubMed] [Google Scholar]
- 11.Jones DA, West RR. Psychological rehabilitation after myocardial infarction: Multicentre randomised controlled trial. BMJ. 1996;313:1517–1521. doi: 10.1136/bmj.313.7071.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Orme-Johnson DW, Walton KG. All approaches to preventing or reversing effects of stress are not the same. American Journal of Health Promotion. 1998;12:297–299. doi: 10.4278/0890-1171-12.5.297. [DOI] [PubMed] [Google Scholar]
- 13.Murphy LR. Stress management in work settings: A critical review of the health effects. American Journal of Health Promotion. 1996;11:112–135. doi: 10.4278/0890-1171-11.2.112. [DOI] [PubMed] [Google Scholar]
- 14.Murphy M, Donovan S, Taylor E. The Physical and Psychological Effects of Meditation: A Review of Contemporary Research with a Comprehensive Bibliography. Sausalito, California: Institute of Noetic Sciences; 1997. pp. 1931–1996. [Google Scholar]
- 15.Alexander CN, Davies JL, Dixon CA, et al. Growth of higher stages of consciousness: Maharishi’s Vedic psychology of human development. In: Alexander CN, Langer EJ, editors. Higher Stages of Human Development: Perspectives on Adult Growth. New York: Oxford University Press; 1990. pp. 286–341. [Google Scholar]
- 16.Schneider RH, Alexander CN, Salerno J, Robinson D, Fields J, Nidich S. Disease prevention and health promotion in the aging with a traditional system of natural medicine: Maharishi Vedic Medicine (MVM) The Journal of Aging and Health. 2002;14:57–78. doi: 10.1177/089826430201400104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nader T, Rothenberg S, Averbach R, Charles B, Fields J, Schneider R. Improvements in chronic diseases with a comprehensive natural medicine approach: A review and case studies. Behav Med. 2000;26:34–46. doi: 10.1080/08964280009595751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walton K, Pugh N. Stress, steroids, and “ojas”: Neuroendocrine mechanisms and current promise of ancient approaches to disease prevention. Indian J Physiol Pharmacol. 1995;39:3–36. [PubMed] [Google Scholar]
- 19.Orme-Johnson DW, Farrow J. Scientific Research on the Transcendental Meditation Program: Collected Papers. Vol. 1. Rheinweiler, West Germany: MERU Press; 1977. p. 722. [Google Scholar]
- 20.Chalmers R, Clements G, Schenkluhn H, Weinless M. Scientific Research on the Transcendental Meditation Program: Collected Papers. 2–4. Vlodrop, The Netherlands: MVU Press; 1990. [Google Scholar]
- 21.Wallace RK, Orme-Johnson DW, Dillbeck MC. Scientific Research on the Transcendental Meditation Program: Collected Papers. Vol. 5. Fairfield, Iowa: MIU Press; 1990. [Google Scholar]
- 22.Jevning R, Wallace RK, Biedebach M. The physiology of meditation: A review. A wakeful hypometabolic integrated response. Neurosci Biobehav Rev. 1992;16:415–424. doi: 10.1016/s0149-7634(05)80210-6. [DOI] [PubMed] [Google Scholar]
- 23.Hawkins MA. Effectiveness of the Transcendental Meditation program in criminal rehabilitation and substance abuse recovery: A review of the research. Journal of Offender Rehabilitation. 2002;36:47–65. [Google Scholar]
- 24.Roth R. Maharishi Mahesh Yogi’s Transcendental Meditation. Washington, DC: Primus; 1994. pp. 90–102. [Google Scholar]
- 25.Williams R, Barefoot J, Califf R. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. JAMA. 1992:267. [PubMed] [Google Scholar]
- 26.Julkunen J, Salonen R, Kaplan G, Chesney M, Salonen J. Hostility and the progression of carotid atherosclerosis. Psychosom Med. 1994;56:519–525. doi: 10.1097/00006842-199411000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Reed DM, LaCroix AZ, Karasek RA, Miller D, MacLean CA. Occupational strain and the incidence of coronary heart disease. Am J Epidemiol. 1989;129:495–502. doi: 10.1093/oxfordjournals.aje.a115160. [DOI] [PubMed] [Google Scholar]
- 28.Hlatky MA, Lam LC, Lee KL, et al. Job strain and the prevalence and outcome of coronary artery disease. Circulation. 1995;92:327–333. doi: 10.1161/01.cir.92.3.327. [DOI] [PubMed] [Google Scholar]
- 29.Grundy SM, Pasternak R, Greenland P, Smith SJ, Fuster V. AHA/ACC scientific statement: Assessment of cardiovascular risk by use of multiple-risk-factor assessment equations: A statement for healthcare professionals from the American Heart Association and the American College of Cardiology. J Am Coll Cardiol. 1999;34:1348–1359. doi: 10.1016/s0735-1097(99)00387-3. [DOI] [PubMed] [Google Scholar]
- 30.Schneider RH, Staggers F, Alexander C, et al. A randomized controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995;26:820–827. doi: 10.1161/01.hyp.26.5.820. [DOI] [PubMed] [Google Scholar]
- 31.Alexander C, Schneider R, Staggers F, et al. A trial of stress reduction for hypertension in older African Americans (Part II): Sex and risk factor subgroup analysis. Hypertension. 1996;28:228–237. doi: 10.1161/01.hyp.28.2.228. [DOI] [PubMed] [Google Scholar]
- 32.Alexander CN, Langer EJ, Newman RI, Chandler HM, Davies JL. Transcendental Meditation, mindfulness, and longevity: an experimental study with the elderly. J Person Soc Psychol. 1989;57:950–964. doi: 10.1037//0022-3514.57.6.950. [DOI] [PubMed] [Google Scholar]
- 33.Wenneberg S, Schneider R, Walton K, et al. A controlled study of the effects of the Transcendental Meditation program on cardiovascular reactivity and ambulatory blood pressure. Int J Neurosci. 1997;89:15–28. doi: 10.3109/00207459708988461. [DOI] [PubMed] [Google Scholar]
- 34.Barnes VA, Treiber FA, Davis H. Impact of Transcendental Meditation on cardiovascular function at rest and during acute stress in adolescents with high normal blood pressure. J Psychosom Res. 2001;51:597–605. doi: 10.1016/s0022-3999(01)00261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Armond DL. Effects of the Transcendental Meditation program on psychological, physiological, behavioral and organizational consequences of stress in managers and executives in management. Fairfield, Iowa: Maharishi University of Management; 1996. p. 161. [Google Scholar]
- 36.Schneider R, Nidich S, Salerno J, et al. Lower lipid peroxide levels in practitioners of the Transcendental Meditation program. Psychosom Med. 1998;60:38–41. doi: 10.1097/00006842-199801000-00008. [DOI] [PubMed] [Google Scholar]
- 37.Calderon R. Effects of Nonpharmacological Approaches on Cholesterol Levels in Mild Hypertensive African Americans: A Pilot Study of the Transcendental Meditation Program and a Health Education Program dissertation. Fairfield, Iowa: Maharishi University of Management; 2000. p. 122. [Google Scholar]
- 38.Alexander CN, Robinson P, Rainforth M. Treating and preventing alcohol, nicotine and drug abuse through Transcendental Meditation Technique: A review and statistical analysis. In: O’Connell DF, Alexander CN, editors. Self Recovery—Treating Addictions Using Transcendental Meditation and Maharishi Ayur-Veda. New York: Haworth Press; 1994. pp. 13–88. [Google Scholar]
- 39.Collins R, Petro R, MacMahone S, et al. Blood pressure, stroke, and coronary heart disease, part 2, Short-term reductions in blood pressure: Overview of randomized drug trials in their epidemiological context. Lancet. 1990;335:827–838. doi: 10.1016/0140-6736(90)90944-z. [DOI] [PubMed] [Google Scholar]
- 40.Collins P, Fox K. Pathophysiology of angina. Lancet. 1990;335:94–96. doi: 10.1016/0140-6736(90)90551-f. [DOI] [PubMed] [Google Scholar]
- 41.Cooper MJ, Aygen MM. Transcendental Meditation in the management of hypercholesterolemia. Journal of Human Stress. 1979;5:24–27. doi: 10.1080/0097840x.1979.10545991. [DOI] [PubMed] [Google Scholar]
- 42.Salonen JT, Yla-Herttuala S, Yamamoto R, et al. Autoantibody against oxidized LDL and progression of carotid atherosclerosis. Lancet. 1992;339:883–887. doi: 10.1016/0140-6736(92)90926-t. [DOI] [PubMed] [Google Scholar]
- 43.Naito C, Kawamura M, Yamamoto Y. Lipid peroxides as the initiating factor of atherosclerosis. Ann N Y Academ Sci. 1990:27–45. doi: 10.1111/j.1749-6632.1993.tb38723.x. [DOI] [PubMed] [Google Scholar]
- 44.Berliner J, Navab M, Fogelman A, et al. Atherosclerosis: Basic mechanisms. Oxidation, inflammation and genetics. Circulation. 1995;91:2488–2496. doi: 10.1161/01.cir.91.9.2488. [DOI] [PubMed] [Google Scholar]
- 45.Matthews KA, Woodall KL, Allen MT. Cardiovascular reactivity to stress predicts future blood pressure status. Hypertension. 1993;22:479–485. doi: 10.1161/01.hyp.22.4.479. [DOI] [PubMed] [Google Scholar]
- 46.Kamarck TW, Jennings JR, Pogue-Geile M, Manuck SB. A multidimensional measurement model for cardiovascular reactivity: Stability and cross-validation in two adult samples. Health Psychol. 1994;13:471–478. doi: 10.1037//0278-6133.13.6.471. [DOI] [PubMed] [Google Scholar]
- 47.Eppley K, Abrams AI, Shear J. Differential effects of relaxation techniques on trait anxiety: A meta-analysis. J Clin Psychol. 1989;45:957–974. doi: 10.1002/1097-4679(198911)45:6<957::aid-jclp2270450622>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 48.Gaylord C, Orme-Johnson D, Travis F. The effects of the Transcendental Meditation technique and progressive muscle relaxation on EEG coherence, stress reactivity, and mental health in black adults. Intern J Neurosci. 1989;46:77–86. doi: 10.3109/00207458908991618. [DOI] [PubMed] [Google Scholar]
- 49.Alexander CN, Rainforth MV, Gelderloos P. Transcendental Meditation, self actualization, and psychological health: A conceptual overview and statistical meta-analysis. Journal of Social Behavior and Personality. 1991;6:189–247. [Google Scholar]
- 50.Ferguson PC. An integrative meta-analysis of psychological studies investigating the treatment outcomes of meditation techniques. In: Chalmers R, Clements G, Schenkluhn H, Weinless M, editors. Scientific Research on Maharishi’s Transcendental Meditation and TM-Sidhi Programme: Collected Papers. Vol. 4. Vlodrop, Holland: Maharishi European Research University, MVU Press; 1991. pp. 2039–2048. [Google Scholar]
- 51.Jevning R, Wilson AF, Smith WR. Adrenocortical activity during meditation. Hormones and Behavior. 1978;10:54–60. doi: 10.1016/0018-506x(78)90024-7. [DOI] [PubMed] [Google Scholar]
- 52.Dillbeck MC, Orme-Johnson DW. Physiological differences between Transcendental Meditation and rest. American Psychologist. 1987;42:879–881. [Google Scholar]
- 53.Michaels RR, Huber MJ, McCann DS. Evaluation of Transcendental Meditation as a method of reducing stress. Science. 1976;192:1242–1244. doi: 10.1126/science.775639. [DOI] [PubMed] [Google Scholar]
- 54.Mills PJ, Schneider RH, Hill D, Walton KG, Wallace RK. Beta-adrenergic receptor sensitivity in subjects practicing transcendental meditation. J Psychosom Res. 1990;34:29–33. doi: 10.1016/0022-3999(90)90005-o. [DOI] [PubMed] [Google Scholar]
- 55.Alexander CN, Swanson GC, Rainforth MV, Carlisle TW, Todd CC, Oates RM. Effects of the Transcendental Meditation program on stress reduction, health, and employee development: A prospective study in two occupational settings. Anxiety, Stress and Coping: An International Journal. 1993;6:245–262. [Google Scholar]
- 56.Walton KG, Pugh N, Gelderloos P, Macrae P. Stress reduction and preventing hypertension: Preliminary support for a psychoneuroendocrine mechanism. Journal of Alternative and Complementary Medicine. 1995;1:263–283. doi: 10.1089/acm.1995.1.263. [DOI] [PubMed] [Google Scholar]
- 57.Levitsky DK. Effects of the Transcendental Meditation program on neuroendocrine indicators of chronic stress dissertation. Fairfield, Iowa: Maharishi University of Management; 1997. p. 298. [Google Scholar]
- 58.MacLean C, Walton K, Wenneberg S, et al. Effects of the Transcendental Meditation program on adaptive mechanisms: Changes in hormone levels and responses to stress after 4 months of practice. Psychoneuroendocrinology. 1997;22:277–295. doi: 10.1016/s0306-4530(97)00003-6. [DOI] [PubMed] [Google Scholar]
- 59.Infante JR, Peran F, Martinez M, et al. ACTH and beta-endorphin in Transcendental Meditation. Physiol Behav. 1998;64:311–315. doi: 10.1016/s0031-9384(98)00071-7. [DOI] [PubMed] [Google Scholar]
- 60.Infante JR, Torres-Avisbal M, Pinel P, et al. Catecholamines in practitioners of the Transcendental Meditation technique. Physio Behav. 2001;72:141–146. doi: 10.1016/s0031-9384(00)00386-3. [DOI] [PubMed] [Google Scholar]
- 61.Barnes VA, Treiber FA, Turner JR, Davis H, Strong WB. Acute effects of Transcendental Meditation on hemodynamic functioning in middle-aged adults. Psychosom Med. 1999;61:525–531. doi: 10.1097/00006842-199907000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Alexander C, Walton K, Goodman R. Walpole study of the TM program in maximum security prisoners I: Cross-sectional differences in development and psychopathology. Journal of Offender Rehabilitation. 2002;36:97–125. [Google Scholar]
- 63.Castillo-Richmond A, Schneider R, Alexander C, et al. Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke. 2000;31:568–573. doi: 10.1161/01.str.31.3.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fields JZ, Walton KG, Schneider RH, et al. Effect of a multimodality natural medicine program on carotid atherosclerosis in older subjects: A pilot trial of Maharishi Vedic Medicine. Am J Cardiol. 2002;89:952–958. doi: 10.1016/s0002-9149(02)02245-2. [DOI] [PubMed] [Google Scholar]
- 65.Blankenhorn DH, Hodis HN. Arterial imaging and atherosclerosis reversal. George Lyman Duff Memorial Lecture. Arteriosclerosis & Thrombosis. 1994;14:177–192. doi: 10.1161/01.atv.14.2.177. [DOI] [PubMed] [Google Scholar]
- 66.Kondwani KA. Psychology. Fairfield, Iowa: Maharishi University of Management; 1998. Nonpharmacologic treatment of hypertension and hypertensive heart disease in African Americans: A trial of the Transcendental Meditation program and a health education program; p. 130. [Google Scholar]
- 67.Zamarra JW, Schneider RH, Besseghini I, Robinson DK, Salerno JW. Usefulness of the Transcendental Meditation program in the treatment of patients with coronary artery disease. Am J Cardio. 1996;78:77–80. doi: 10.1016/S0002-9149(97)89184-9. [DOI] [PubMed] [Google Scholar]
- 68.Salonen JT, Salonen R. Ultrasound B-mode imaging in observational studies of atherosclerotic progression. Circulation. 1993;87(Suppl 2):56–65. [PubMed] [Google Scholar]
- 69.Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med. 1991;114:345–352. doi: 10.7326/0003-4819-114-5-345. [DOI] [PubMed] [Google Scholar]
- 70.Kondwani K, Schneider RH, Alexander CN, et al. Left ventricular mass regression with the Transcendental Meditation technique and a health education program in hypertensive African Americans. Journal of Social Behavior and Personality. In press. [Google Scholar]
- 71.Devereux RB, Okin PM, Roman MJ. Pre-clinical cardiovascular disease and surrogate end-points in hypertension: Does race influence target organ damage independent of blood pressure? Ethnicity and Disease. 1998;8:138–148. [PubMed] [Google Scholar]
- 72.Devereux RB, Roman MJ, Ganau A, de Simone G, Okin PM, Kligfield P. Cardiac and arterial hypertrophy and atherosclerosis in hypertension. Hypertension. 1994;23:802–809. doi: 10.1161/01.hyp.23.6.802. [DOI] [PubMed] [Google Scholar]
- 73.Devereux R, Roman M. Hypertensive left ventricular hypertrophy: Pathogenesis, prognostic importance and treatment. CVR & R. 1992 August;:24–33. [Google Scholar]
- 74.Alexander CN, Barnes VA, Schneider RH, et al. A randomized controlled trial of stress reduction on cardiovascular and all-cause mortality in the elderly: Results of 8 and 15 year follow-ups. Circulation. 1996;93:629. [abstract] [Google Scholar]