The Mental Health Act 1983 provides legislation to ensure a consistent and comprehensive approach to the compulsory admission of psychiatric patients in England and Wales. Since the introduction of the act, the provision of service has changed: hospitals have closed and the care in the community programme has been introduced. Despite the reduction in the number of psychiatric beds available Department of Health data show a rise in the absolute number of compulsory admissions.1 We aimed to determine the proportion of all psychiatric admissions that these compulsory “formal” admissions represent.
Methods and results
The Department of Health collects data from health authorities on compulsory psychiatric admissions, and these data were used to determine the proportion of all psychiatric admissions that were compulsory. Between 1984 and 1986 these data were presented for each calendar year. Since 1987 they have been presented for each financial year. Data were available from the Mental Health Enquiry from 1984 to 1986 and from the hospital episodes statistics system from 1989 to 1996. This system holds details of inpatients in NHS hospitals in England. Using these sources we calculated the proportion of all admissions to psychiatric hospitals that occurred under the act. Data on the total number of psychiatric admissions were not available for 1987-9.
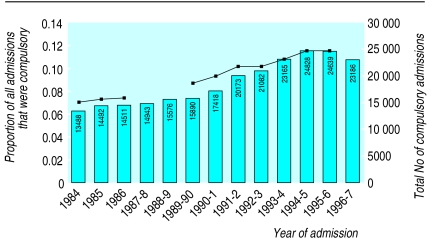
The total number of compulsory admissions has almost doubled, rising from 13 488 in 1984 to 24 639 in 1995-6. The number of all psychiatric admissions rose from 190 389 to 213 240 over the same period. Therefore, the proportion of psychiatric admissions made under the act has risen from 7% in 1984 to 12% in 1995-6 (figure).
Comment
There was a rise in the total number of admissions from 1984 to 1996, with increases in both the absolute number and the proportion of compulsory admissions. The quality of these data depends on accurate reporting by hospitals. There was discontinuity in the total number of admissions in 1986-9; in fact, they dropped slightly. We are unsure why this was so. It is possible that the data were collected in different ways and the change was artefactual. However, the number of compulsory admissions increased each year. Although the data that comprise the denominators were not ideal, as they came from two sources, the proportion of compulsory admissions increased steadily. For 1989-96, when only one source of data was used for the denominator, the trend remained constant.
What explanations are there for the increase in compulsory admissions? Firstly, these changes may be due to alterations in the presentation of patients with psychiatric disorders. For example, there is some evidence that a higher proportion of psychiatric patients misuse drugs and alcohol, and this may lead to more florid presentations of psychotic illness.2 Secondly, changes in the availability of beds during this period may have increased the threshold for admission and decreased the threshold for discharge. Between 1982 and 1992, approximately 43 000 fewer psychiatric hospital beds were available,3 and in inner city areas bed occupancy remains above 100% much of the time.4 The public’s fear of violence by mentally ill patients and pressures to keep patients in hospital until it is “safe” to discharge them put further strain on the availability of beds. Delays in admission and treatment caused by bed shortages may mean that patients’ illnesses are becoming more severe and that compulsory treatment is being initiated in cases in which informal admissions would previously have been possible.
These results have implications for resources in terms of costs and staffing. Compulsory admissions are more time consuming since they generally require that patients be assessed by two doctors and a social worker. Disturbed patients also require more intensive nursing and supervision. Patients admitted under the act have the right to appeal, and mental health tribunals are time consuming and costly. We suggest that the move to community care may have led to a paradoxical and unexpected increase in the use of coercion in the treatment of patients with mental illnesses.
Figure.
Bars represent the total number of compulsory psychiatric admissions to NHS facilities and the line represents the proportion of all admissions that were compulsory in England, 1984-96. Data on compulsory admissions not available for 1987-9
Footnotes
Funding: Department of Health. The views expressed in this paper are those of the authors and not necessarily those of the Department of Health.
Competing interests: None declared.
References
- 1.Department of Health. Inpatients formally detained in hospitals under the Mental Health Act 1983 and other legislation. London: DoH; 1998. [Google Scholar]
- 2.Cuffel B. Prevalence estimates of substance abuse in schizophrenia and their correlates. J Nerv Ment Dis. 1992;180:589–592. doi: 10.1097/00005053-199209000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Davidge M, Elias S, Jayes B, Wood K, Yates J. Survey of English mental illness hospitals. Birmingham, Health Services Management Centre, University of Birmingham; 1994. [Prepared for the Mental Health Task Force.] [Google Scholar]
- 4.Johnson S, Ramsay R, Thornicroft G, Brooks L, Lelliot P, Peck E, et al. London’s mental health: the report to the King’s Fund London Commission. Rev ed. London: King’s Fund; 1998. [Google Scholar]