Abstract
Objective
To examine how health aid is spent and channelled, including the distribution of resources across countries and between subsectors. Our aim was to complement the many qualitative critiques of health aid with a quantitative review and to provide insights on the level of development assistance available to recipient countries to address their health and health development needs.
Methods
We carried out a quantitative analysis of data from the Aggregate Aid Statistics and Creditor Reporting System databases of the Organisation for Economic Co-operation and Development, which are the most reliable sources of data on official development assistance (ODA) for health from all traditional bilateral and multilateral sources and from partnerships such as the Global Fund to Fight AIDS, Tuberculosis and Malaria.
Findings
The analysis shows that while health ODA is rising and capturing a larger share of total ODA, there are significant imbalances in the allocation of health aid which run counter to internationally recognized principles of “effective aid”. Countries with comparable levels of poverty and health need receive remarkably different levels of aid. Funding for Millennium Development Goal 6 (combat HIV/AIDS, malaria and other diseases) accounts for much of the recent increase in health ODA, while many other health priorities remain insufficiently funded. Aid is highly fragmented at country level, which entails high transaction costs, divergence from national policies and lack of coherence between development partners.
Conclusion
Although political momentum towards aid effectiveness is increasing at global level, some very real aid management challenges remain at country level. Continued monitoring is therefore necessary, and we recommend that a review of the type presented here be repeated every 3 years.
Résumé
Objectif
Étudier comment l’aide sanitaire est dépensée et distribuée, et notamment comment les ressources sont réparties entre les pays et les sous-secteurs. Nous avions pour objectif de compléter les nombreuses critiques qualitatives de l’aide sanitaire par un bilan quantitatif et de donner un aperçu du niveau d’assistance au développement dont bénéficient les pays destinataires pour répondre à leurs besoins en termes de santé et de développement sanitaire.
Méthodes
Nous avons analysé quantitativement des données provenant des bases de données des Statistiques agrégées de l’aide et du Système de notification des pays créanciers de l’OCDE (Organisation de coopération et de développement économiques), qui constituent les sources les plus fiables de renseignements sur l’aide au développement officielle (ADO) en faveur de la santé, apportée par l’ensembles des sources bilatérales et multilatérales traditionnelles et par des partenariats tels que le Fonds mondial de lutte contre le Sida, la tuberculose et le paludisme.
Résultats
Il ressort de cette analyse que, si l’ADO en faveur de la santé est en augmentation et représente une part grandissante de l’ADO totale, il existe néanmoins des déséquilibres importants dans l’affectation de l’aide sanitaire, qui sont contraires au principe internationalement reconnu «d’efficacité de l’aide». Des pays comparables par le niveau de pauvreté et les besoins sanitaires reçoivent des volumes d’assistance étonnamment différents. Le financement de l’Objectif du Millénaire pour le développement N° 6 (combattre le VIH/sida, le paludisme et d’autres maladies) représente une grande part de la récente augmentation de l’ADO sanitaire, alors que nombre d’autres priorités sanitaires restent sous-financées. L’aide est fortement fragmentée au niveau des pays, ce qui entraîne des coûts de transaction élevés, des écarts par rapport aux politiques nationales et un manque de cohérence entre les partenaires dans le développement.
Conclusion
Bien que l’impulsion politique en faveur d’une aide efficace s’amplifie à l’échelle mondiale, certaines difficultés de gestion bien réelles persistent au niveau des pays. Une surveillance continue s’impose donc et nous préconisons de refaire un bilan de ce type tous les 3 ans.
Resumen
Objetivo
Determinar cómo se gasta y canaliza la ayuda sanitaria, en particular cómo se distribuyen los recursos entre los países y entre subsectores. Nos propusimos complementar las numerosas críticas cualitativas de la ayuda sanitaria con un examen cuantitativo, y esclarecer el nivel de asistencia para el desarrollo de que disponen los países beneficiarios para afrontar sus necesidades sanitarias y de desarrollo sanitario.
Métodos
Realizamos un análisis cuantitativo de datos extraídos de las bases de datos de las Estadísticas Agregadas sobre la Ayuda y del Sistema de Notificación por parte de los Países Acreedores (CRS) de la Organización de Cooperación y Desarrollo Económicos, que son las fuentes más fiables de datos sobre la asistencia oficial para el desarrollo (AOD) destinada a la salud proporcionada por todas las fuentes bilaterales y multilaterales tradicionales y por alianzas como el Fondo Mundial de Lucha contra el SIDA, la Tuberculosis y la Malaria.
Resultados
El análisis muestra que si bien la AOD destinada a la salud está aumentando y captando una mayor proporción de la AOD total, la asistencia para la salud presenta desequilibrios importantes que son contrarios a los principios reconocidos internacionalmente como característicos de una «ayuda eficaz». Países con niveles comparables de pobreza y salud reciben niveles de ayuda considerablemente distintos. La financiación del sexto Objetivo de Desarrollo del Milenio (combatir el VIH/sida, la malaria y otras enfermedades) representa gran parte del aumento reciente de la AOD destinada a la salud, mientras que muchas otras prioridades sanitarias siguen sin contar con financiación suficiente. La ayuda está muy fragmentada a nivel de país, lo que entraña altos costos de transacción, divergencias respecto a las políticas nacionales y falta de coherencia entre los asociados para el desarrollo.
Conclusión
Aunque el impulso político para potenciar la eficacia de la ayuda está aumentando en el plano mundial, a nivel de país la gestión de la ayuda sigue tropezando con obstáculos muy reales. Se requiere en consecuencia una vigilancia permanente, por lo que recomendamos que cada tres años se vuelva a realizar un estudio como el aquí presentado.
ملخص
الغرض
هو فحص كيفية إنفاق المساعدات الصحية وقنوات هذا الإنفاق، بما في ذلك توزيع الموارد عبر البلدان وبين القطاعات الفرعية. لقد هدف الباحثون إلى إدماج العديد من الوسائل الانتقادية الكيفية للمساعدات الصحية مع المراجعة الكمّية لطرح رؤية واعية حول مستوى مساعدات التنمية المتاحة للبلدان المستقبلة للمساعدات لإيلاء الاهتمام بالصحة وباحتياجات التنمية الصحية لديها.
الطريقة
أجرى الباحثون تحليلاً كميّاً للبيانات الواردة من مجمل إحصائيات المساعدات، وقواعد بيانات نظام التسجيل الإتماني لمنظمة التعاون الاقتصادي والتنمية، وهي أكثر مصادر المعلومات ثقة حول مساعدات التنمية الرسمية الخاصة بالصحة من جميع مصادر التمويل التقليدية الثنائية الأطراف والمتعددة الأطراف ومن جهات الشراكة مثل الصندوق العالمي لمكافحة الإيدز والسل والملاريا.
الموجودات
أظهر التحليل أنه بالرغم من تزايد مساعدات التنمية الرسمية الخاصة بالصحة واستحواذها على النصيب الأكبر من إجمالي مساعدات التنمية، إلا أن هناك عدم توازن في تخصيص المساعدات الصحية والتي تسير عكس المبادئ الدولية المعترف بها “للمساعدات الفعّالة”. فالبلدان ذات المستويات المتشابهة من حيث احتياجات الفقر والصحة تتلقى مستويات شديدة التباين من المساعدات. ويشغل تمويل المرمى السادس من المرامي الإنمائية للألفية (محاربة الإيدز والعدوى بفيروسه، والملاريا، والأمراض الأخرى) حيزاً كبيراً من الزيادة التي تحققت في مساعدات التنمية الرسمية الخاصة بالصحة، بينما يظل تمويل كثير من الأولويات الصحية الأخرى غير كافٍ. ويجري على المستوى القطري تقسيم المساعدة تقسيماً شديد التجزؤ، مما يستنزف تكاليف باهظة في التحويلات النقدية، ويؤدي إلى الانحراف عن السياسات الوطنية، وانعدام الترابط بين الشركاء في التنمية.
الاستنتاج
بالرغم من تزايد قوة الدفع السياسي صوب فعالية المساعدات على الصعيد العالمي، مازال هناك بعض التحديات الحقيقية في إدارة المساعدات على المستوى القطري، ولذلك فمن الضروري استمرار الرصد، ويوصي الباحثون بمراجعة النمط المقدم في هذا البحث وتكراره كل ثلاث سنوات.
Introduction
Most assessments of the changes in international health aid over the past 10 years have focused on the fragmented nature of the new global health financing landscape and the health governance challenges created by growing numbers of aid channels and instruments.1–4
In the last decade, global health concerns and development priorities, including the health-related Millennium Development Goals (MDGs), have resulted in the mushrooming of new health initiatives targeting single diseases or programmes, many of them with substantial financing capabilities. As a result, concerns have been voiced that spending priorities are increasingly determined at global and regional levels rather than at the recipient country level. Concurrently, concerns about the efficiency of aid delivery have prompted the development community to promote the use of more efficient aid instruments, including general budget support and sector-wide approaches.
While global levels of health aid are clearly rising, it is less clear whether the amount of money available to countries to allocate flexibly, in accordance with their health priorities and health system development needs, is also increasing. With notable exceptions,5,6 few studies have looked in detail at any of the issues mentioned above or at what official development assistance (ODA) resources for health are being spent on, at which countries are benefiting or at the potential for new resources to contribute to health development and health systems strengthening. This study attempts to answer some of these complex questions using statistical data from the Development Assistance Committee of the Organisation for Economic Co-operation and Development (OECD/DAC).
It should be noted that much of the data reviewed here pre-dates the Paris Declaration on Aid Effectiveness,7 under which donors committed to provide their aid more coherently and in alignment with country priorities, systems and procedures.
Methods
This analysis focuses on ODA, i.e. grants or loans by governments to developing countries with promotion of economic development and welfare as the main objective. The data come from donor reports to the OECD/DAC. The OECD’s Aggregate Aid Statistics and Creditor Reporting System (CRS) are the most reliable sources of aid data. The CRS is the main source used in this analysis, although data series referring to years before 2000 are from the Aggregate Aid Statistics. Part of the analysis focuses on the least developed countries (LDCs), since they are at the centre of global health development efforts.
One limitation of OECD statistics, especially in recent years, is that they do not include funds provided by non-OECD governments such as China and India and by wealthy Middle-Eastern countries. Also excluded are funds provided by private entities such as the Bill & Melinda Gates Foundation. The real magnitude of health aid flows is therefore much higher: The World Bank reported, for example, that in 2006 total development assistance to health, including aid from private organizations, reached US$ 16.7 billion,8 whereas the CRS recorded only US$ 13.3 billion. In addition, although CRS statistics dating back to 1973 are available, reliable in-depth analysis can only be carried out from 2000 onwards because of the limited coverage of earlier data and changes in reporting guidelines.
The secretariat of the OECD/DAC continuously monitors the quality of aid activity data reported by donors, focusing on the completeness of reporting and its conformity with definitions. The quality of CRS data on commitments for the period 2002–2006, on which this analysis focuses, ranges from good to excellent.
The CRS’s classification system, however, does not always perfectly fit some of the development benchmarks – such as the MDGs – against which health ODA resources are measured. We therefore aggregated the CRS categories (Table 1) where required to match health development goals or we used proxies. For example, data in the CRS category “Sexually-transmitted disease (STD) control including HIV/AIDS” are used as a proxy for HIV/AIDS funding. This is justified because the overwhelming majority of activities funded in this category, both in value and in number, relate to HIV/AIDS control.
Table 1. CRS categories under which health ODA is reported and definitions.
| Definition | ||
|---|---|---|
| 1. General health | ||
| Health policy and administrative management | Health sector policy, planning and programmes; aid to health ministries, public health administration; institution capacity-building and advice; medical insurance programmes; unspecified health activities | |
| Medical education/training | Medical education and training for tertiary-level services | |
| Medical research | General medical research (excluding basic health research) | |
| Medical services | Laboratories, specialized clinics and hospitals (including equipment and supplies); ambulances; dental services; mental health care; medical rehabilitation; control of non-infectious diseases; drug and substance abuse control (excluding narcotics traffic control) | |
| Basic health | ||
| Basic health care | Basic and primary health-care programmes; paramedical and nursing care programmes; supply of drugs, medicines and vaccines related to basic health care | |
| Basic health infrastructure | District-level hospitals, clinics and dispensaries and related medical equipment; excluding specialized hospitals and clinics | |
| Basic nutrition | Direct feeding programmes (maternal feeding, breastfeeding and weaning foods, child feeding, school feeding); determination of micro-nutrient deficiencies; provision of vitamin A, iodine, iron etc.; monitoring of nutritional status; nutrition and food hygiene education; household food security | |
| Infectious disease control | Immunization; prevention and control of malaria, tuberculosis, diarrhoeal diseases, vector-borne diseases (e.g. river blindness and guinea worm), etc. | |
| Health education | Information, education and training of the population for improving health knowledge and practices; public health and awareness campaigns | |
| Health personnel development | Training of health staff for basic health-care services | |
| 2. Population policies/programmes and reproductive health | ||
| Population policy and administrative management | Population/development policies; census work, vital registration; migration data; demographic research/analysis; reproductive health research; unspecified population activities | |
| Reproductive health care | Promotion of reproductive health; prenatal and postnatal care including delivery; prevention and treatment of infertility; prevention and management of consequences of abortion; safe motherhood activities | |
| Family planning | Family planning services including counselling; information, education and communication activities; delivery of contraceptives; capacity-building and training | |
| STD control including HIV/AIDS | All activities related to sexually transmitted diseases and HIV/AIDS control e.g. information, education and communication; testing; prevention; treatment, care | |
| Personnel development for population and reproductive health | Education and training of health staff for population and reproductive health-care services | |
CRS, Creditor Reporting System; ODA, official development assistance; STDs, sexually-transmitted disease. Source: Organisation for Economic Co-operation and Development.9
Activities aimed at improving the health of the population in ODA recipient countries are reported to the CRS under two broad categories – “Health, general” and “Population policies/programmes and reproductive health” – which are subdivided as shown in Table 1. The OECD/DAC’s CRS categories “Health” and “Population” are combined in this paper in a single category: “Health”.
Aid activities are categorized in the CRS according to type (Box 1). In recent years the OECD/DAC has requested that donors also report on the channel through which activities are implemented, i.e. whether aid is channelled through the public sector, nongovernment organizations (NGOs) and civil society organizations, public–private partnerships or multilateral organizations. This information is reported for only 20% of health activities, however, which limits the usefulness of such data.
Box 1. Types of aid reported in the CRS aid activity database.
Free-standing technical cooperation is defined as financing of activities whose primary purpose is to augment the level of knowledge, skills, technical know-how or productive aptitudes of the population of aid recipient countries, i.e. increasing their stock of human intellectual capital or their capacity for more effective use of their existing factor endowment. It includes the cost of personnel, training and research, as well as associated equipment and administrative costs.
Sector programme aid comprises contributions to carry out wide-ranging development plans in a defined sector such as agriculture, education, transportation, etc. Assistance is made available “in cash” or “in kind”, with or without restriction on the specific use of the funds, but on the condition that the recipient executes a development plan in favour of the sector concerned.
Investment projects comprise: (i) schemes to increase and/or improve the recipient’s stock of physical capital, and (ii) financing the supply of goods and services in support of such schemes.
Investment-related technical cooperation is defined as the financing of services by a donor country with the primary purpose of contributing to the design and/or implementation of a project or programme aiming to increase the physical capital stock of the recipient country. These services include consulting services, technical support, the provision of know-how linked to the execution of an investment project, and the contribution of the donor’s own personnel to the actual implementation of the project (managers, technicians, skilled labour etc.).
CRS, Creditor Reporting System.
Source: Organisation for Economic Co-operation and Development.9
Results
Trends in overall levels
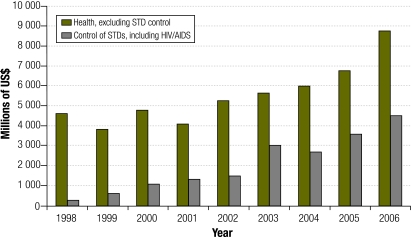
Analysis of the Development Assistance Committee’s aggregate development aid data from 1980 to 2006 reveals that total bilateral ODA commitments from OECD/DAC members have increased by more than 50% in real terms since 1980–1984, from an annual average of US$ 70.5 billion in the period 1980–1984 to US$ 108.7 billion in the period 2002–2006. (Five-year averages are used as many commitments entail expenditures for several years, so this produces a smoother trend.) Health is capturing an increasing share of all ODA. OECD/DAC members’ total bilateral aid commitments for health in 1980–1984 averaged US$ 2.8 billion per year (constant 2006 dollars), or 5.3% of all ODA. This figure remained virtually unchanged up to the end of the 1990s, increasing thereafter to an annual average of US$ 6.4 billion in 2002–2006, equivalent to 7.8% of total ODA. In 2006 alone, the CRS recorded bilateral and multilateral commitments for health from all members totalling US$ 13.3 billion – the highest level ever. The analysis also reveals that increased funding for HIV/AIDS activities accounts for a large share of the increases in health ODA in recent years. Funding for HIV/AIDS accounted for almost one third (32%) of total health ODA for the period 2002–2006 (Fig. 1).
Fig. 1.
HIV/AIDS control as a proportion of total health ODA commitments, in millions of US$ (constant 2005 dollars), 1998–2006
ODA, official development assistance; STD, sexually-transmitted disease; US$, United States dollars.
Statistics from the Development Assistance Committee of the Organisation for Economic Co-operation and Development.
Commitments vs disbursements
Ministries of health in recipient countries often complain about delays in disbursing funds for projects or activities already under way or for which a formal commitment already exists.10 Recent changes in CRS reporting practices mean that reliable data on disbursements, suitable for assessing the magnitude of this phenomenon at the aggregate level, are available only from 2002 onwards (Box 2).
Box 2. Commitments versus disbursements.
A commitment is a firm written obligation by a government or official agency, backed by the appropriation or availability of the necessary funds, to provide resources of a specified amount under specified financial terms and conditions and for specified purposes for the benefit of the recipient country.
A disbursement is the placement of resources at the disposal of a recipient country or agency, or in the case of internal development-related expenditures, the outlay of funds by the official sector.
Source: Organisation for Economic Co-operation and Development.9
It is difficult to evaluate disbursement rates for every health commitment reported to the CRS, as the time frame of disbursements for each commitment varies. We have therefore compared disbursements for each year during the period 2004–2006 with average commitments made 3 and 5 years earlier (3 to 5 years being the average period over which committed funds are disbursed). The results, though only indicative, reveal that disbursements of health ODA amount to more than 80% of average annual commitments over the previous 3 to 5 years. Disbursements in 2006 were equivalent to 98% of average annual commitments over the previous 5 years and 87% of commitments over the previous 3 years. These data suggest that the difference between commitments and disbursements is not great; however, the figures may hide within-year delays in programme implementation.
Unpacking health ODA
While delivering all committed aid is important, on its own it is not enough to secure progress in health. Equally important factors are how money is channelled and spent, who benefits, what purpose it serves and how much gets through to develop and strengthen the health system so that it is responsive to national health development needs and global health concerns.
Multi-country initiatives
In 2002–2006, global and regional multi-country initiatives accounted for 25% of all health ODA, including funds channelled through multilateral institutions (UN agencies, international NGOs and private entities) for activities that benefited several recipient countries. Examples include global immunization campaigns, HIV/AIDS prevention and control activities and support for basic health care. This category contrasts with funds sent directly to countries through agreements between donors and recipient governments. Although all sectors record multi-country regional activities, the volume in the health sector is unusually high. CRS data show that only 6.3% of education ODA and only 16.8% of total ODA is channelled through global and regional multi-country activities. The high levels in the health sector appear to be related to the way HIV/AIDS funding is channelled. In 2002–2006, HIV/AIDS accounted for 40.7% of support for global and regional multi-country health initiatives (44.2% in 2004–2006).
Global and regional multi-country initiatives are important mechanisms for targeting funding at global health challenges such as polio eradication and for sharing experiences across countries with similar needs. Such areas are priorities in most poor countries and need support. However, as the overarching operational and programming priorities of such initiatives are set at the regional or global level, they are often not fully aligned with national priorities. This can result in an uneven pattern of investment across the sector. In Uganda, for example, aid flows to HIV/AIDS have on average been higher than those going to all other health areas, which is perhaps justified given the high prevalence of HIV infection; however, other diseases, such as malaria, that are responsible for a significant share of the country’s burden of disease have not received as much attention from donors. Areas other than disease control, including human resources for health, rural health services, and family planning and reproductive health, also face relatively large funding gaps.11 Moreover, regional- and global-level funds often have their own budget cycles and reporting and monitoring procedures, which may impose an additional administrative burden on already overstretched recipient governments.
A substantial part of global and regional multi-country funding is likely to involve WHO, the United Nations Children’s Fund (UNICEF) and the United Nations Population Fund (UNFPA) and to support vertical initiatives such as Roll Back Malaria. International organizations have an important role to play in coordinating responses to global health challenges, which partly explains the high level of global and regional funding for health and also accounts for the rising levels of extra-budgetary (non-core) contributions to these organizations. As noted above, however, it is difficult to fully align such funding with national priorities.
Technical cooperation
A substantial part of health ODA is spent on technical cooperation, which the OECD defines as grants to nationals of aid recipient countries receiving education or training at home or abroad and payments to consultants, advisers and similar personnel as well as teachers and administrators serving in recipient countries (including the cost of associated equipment). Support of this kind, provided specifically to facilitate implementation of a capital project, is included indistinguishably among bilateral project and programme expenditures and is not separately identified as technical cooperation in statistics of aggregate aid flows.
In the period 2002–2006 more than 40% (41.7%) of all health ODA and 43.5% of all health aid activities (e.g. projects and programmes, training courses, research projects) were technical cooperation initiatives aimed at building human capital in recipient countries, which included, for example, salaries for local staff and international experts, consultants’ fees and training.
Technical cooperation accounted for the lion’s share of resources (58.6%) channelled through global or regional multi-country initiatives. In 2002–2006 technical cooperation funding committed directly to individual countries was a more modest 36.2%.
Technical cooperation also accounted for much of new HIV/AIDS funding (53% of HIV/AIDS commitments in the period 2002–2006). Technical cooperation for HIV/AIDS activities represented almost half of all technical cooperation for health in 2005–2006.
Size matters
The size of projects matters. Large activities (in dollar terms) at the country level are more likely to attract political attention, receive significant technical input and, crucially, be of a scale that will have an impact on health and the health delivery system in recipient countries. This does not mean that smaller projects have no role to play. On the contrary, they are important for piloting new approaches, testing innovations, delivering benefits to individual communities and covering emerging or unplanned health system needs. Analysed in the light of the Paris Declaration, however, many small activities are likely to have high transaction costs for government, diverge from national policies and suffer from lack of coordination among development partners.12–14
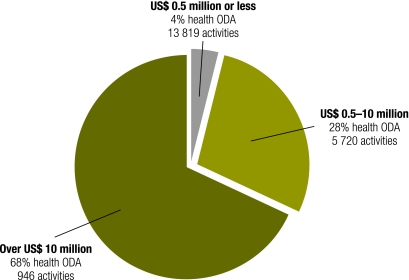
Over the period 2002–2006, the CRS recorded 20 485 health projects, only 946 of which were aid activities valued at more than US$ 10 million, such activities accounting for less than 5% (4.6%) of all aid activities reported to the OECD/DAC. They represented, however, more than two thirds (68.3%) of total health ODA commitments in the period.
Of the activities exceeding US$ 10 million, (i) more than 50% (51.4%) targeted tuberculosis, malaria, HIV/AIDS and other communicable diseases (a good proxy for MDG-6); and (ii) just 9.1% supported activities relating to reproductive health and family planning (a proxy for MDG-5).
The CRS recorded 5720 activities valued at between US$ 0.5 million and US$ 10 million. These represented 28.1% of total health ODA and 27.9% of all health aid activities. In addition, there were 13 819 commitments for activities valued at under US$ 0.5 million each, which made up 67.5% of all health aid activities in the period but accounted for only 3.6% of health ODA recorded by the CRS. Fig. 2 summarizes information on the scale of health activities.
Fig. 2.
Number and scale of health aid activities in US$ and as a proportion of total health ODA commitments, 2002–2006
ODA, official development assistance; US$, United States dollars.
Statistics from the Development Assistance Committee of the Organisation for Economic Co-operation and Development.
In general, a reported aid activity is a specific project or programme for which funds are allocated in a particular sector in a given recipient country. However, donors sometimes compile CRS reports at a more detailed level, in which case a reported activity may actually be a component of an activity. On the other hand, activities are sometimes aggregated, so a single reported activity may comprise several distinct activities. For many of these small reported activities, the normal project cycle will, however, have been followed: appraisal, possibly involving a mission; discussion of a project proposal with government officials and its subsequent submission to donors for approval; and production of a technical and financial report. This represents a substantial workload for recipients (and also donors). In the 5 years under examination, each LDC received, on average, a commitment of around US$ 30 000 every 2 to 3 weeks (1.7 projects/month).
Over the period 2002–2006, Ethiopia had commitments totalling US$ 1.1 billion, including 26 activities amounting to US$ 743 million (67% of total health ODA commitments) and 296 activities each valued at under US$ 0.5 million (US$ 123 000, on average, apiece), which represented 3.3% of its total health ODA. Similarly, in the United Republic of Tanzania, 2.6% of the US$ 1.35 billion in ODA committed to health was channelled via 279 projects, each with an average value of US$ 127 000. Just 30 reported activities accounted for 70% of all health ODA in the 5 years under examination. These figures relate only to activities targeting recipient countries directly; they do not include activities channelled through global and regional multi-country projects.
We are not suggesting that smaller amounts are not important for health development or that they will not improve specific health outcomes among specific populations for discrete periods of time. There does, however, appear to be an excessively large number of small donor projects in the health sector, which would appear to indicate a high level of fragmentation in health aid.
How much aid remains?
The dramatic but welcome and overdue increase in funding for HIV/AIDS control activities and the prominence of technical cooperation in health ODA beg the question: How much aid remains for other health activities?
Data from the CRS are troubling. Out of all health ODA provided directly to LDCs in 2002–2006, commitments towards the achievement of MDG-6 (combat HIV/AIDS, malaria and other diseases) accounted for 46.8%. That left the equivalent of US$ 2.25 per capita per year for the strengthening of health systems and service delivery needed to achieve MDGs 4 and 5 (reduce child mortality and improve maternal health, respectively). However, in 2006, WHO reported that training the numbers of health workers necessary to strengthen health systems would require an increase in health expenditure of US$ 2.80 per capita, while the additional cost of paying salaries of new doctors, nurses and midwives would mean a minimum increase of US$ 7.50 per person per year on average.15
Subtracting that part of health ODA aimed at building human capacity (i.e. technical cooperation) leaves just US$ 0.53 per capita a year for health activities not related to the achievement of MDG-6. This is clearly insufficient to provide meaningful support for the scaling up of health services in poor countries with low capacity and resource shortages.
It is important to remember that resources other than those mentioned above are made available to countries through multi-country activities, and the CRS’s broad classification system may hide a more complex reality. For example, both the GAVI Alliance and the Global Fund to Fight AIDS, Tuberculosis and Malaria now provide support for health systems development and capacity-building in recipient countries. However, the extent to which countries should rely for health systems financing on funding mechanisms that were established primarily to address specific diseases – as compared to other sources, such as low-interest loans from The World Bank – is a subject of ongoing debate.6,16,17
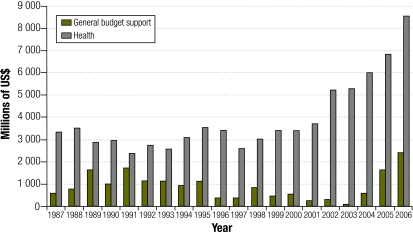
General budget and sector support
General budget support, wherein donors channel their aid directly into the budget of a recipient country, is arguably one of the most efficient aid modalities: it avoids many of the costs and inefficiencies associated with projects; it is easier to align with the recipient’s priorities; and it opens the way to a broader, strategic dialogue on economy-wide issues.18 If accountability and governance are poor, however, as they often are in developing countries, these resources may well be misspent. Overall, general budget support commitments account for a small part of all ODA: for example, in 2002–2006 they were equivalent to 6.4% of total ODA (excluding debt relief). Since domestic allocations to health tend to be low, particularly in poor countries, the level of resources reaching the health sector via this modality is likely to be relatively small.
Nevertheless, whatever its pros and cons, budget support has increasingly come to be seen as “effective aid”, championed by those donors who are also champions of the Paris Declaration.19 It is therefore surprising that ODA commitment to general budget support has only in the last few years returned to the same levels as in the late 1980s (Fig. 3).
Fig. 3.
General budget support and health: official bilateral commitments, in millions of US$ (constant 2006 dollars), 1987–2006
US$, United States dollars.
Statistics from the Development Assistance Committee of the Organisation for Economic Co-operation and Development.
Similar arguments can be advanced in favour of sector programmes: they reduce transaction costs for government, allow alignment with national priorities and help to develop a strategic, sector-wide vision. The CRS reveals, however, that the proportion of health aid spent on sector programmes is relatively minor: 7.7% of all health ODA in 2002–2006, and even that is likely to be an overestimate. Our review of data reported to the OECD/DAC in this category suggests that, notwithstanding substantial data quality improvements in recent years, the “sector programme” category still includes funding for activities which do not appear to meet the OECD/DAC’s own definition of “sector support”.
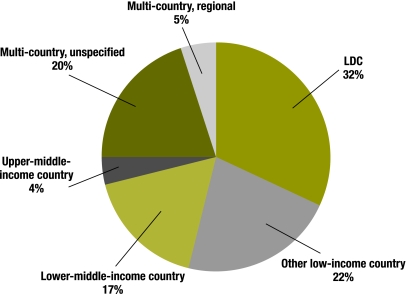
Distribution across countries
Fig. 4 shows the distribution of health ODA by country income group. LDCs receive the most health aid – close to the share received by other low-income countries and lower-middle income countries together. They also receive a substantially larger amount per capita: over US$ 4.50, compared to just over US$ 1.00 for other low-income countries and only US$ 0.50 for lower-middle-income countries.
Fig. 4.
Distribution of health ODA by country income group, 2002–2006
ODA, official development assistance; LDC, least developed country.
Statistics from the Development Assistance Committee of the Organisation for Economic Co-operation and Development.
Least developed countries
The LDCs are the focus of major development efforts and the direct recipients of one third of all health ODA. This group includes many countries immersed in or emerging from conflict. These countries also have the worst health outcomes and are the least likely to meet the health-related MDGs.20 It is therefore important to understand how aid is distributed in support of health development efforts and service delivery in these countries.
Table 2 summarizes the main features and focus of health ODA in LDCs with a population of over 1 million. Countries are ranked in descending order according to per capita health ODA. The table shows that there are huge geographical variations in health ODA per capita in the LDC group: from almost US$ 20 per capita a year for Zambia to US$ 1.59 for Chad.
Table 2. Health ODA in selected least developed countries, 2002–2006.
| LDC recipient | Average population (thousands) 2002–2006 | Under-5 mortality rate 2004 | Life expectancy at birth 2004 | Health ODA per capita 2002–2006 | MDG-6% health ODA | HIV/AIDS prevalence (15–49) – Est. 2005 | MDG-5% health ODA | Technical cooperation % health ODA | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Zambia | 11 277 | 182 | 40 | 19.97 | 58.5 | 17 | 0.6 | 36.2 | ||||||||
| Timor-Leste | 1 009 | NA | NA | 14.94 | 18.9 | NA | 0.8 | 20.4 | ||||||||
| Malawi | 12 905 | 175 | 41 | 13.44 | 49.9 | 14.1 | 1.5 | 22.4 | ||||||||
| Lesotho | 1 965 | 82 | 41 | 12.7 | 72.1 | 23.2 | 0.7 | 19.3 | ||||||||
| Rwanda | 9 085 | 203 | 46 | 10.75 | 73.9 | 3.1 | 2.1 | 53.8 | ||||||||
| Haiti | 9 151 | 117 | 55 | 10.07 | 63.1 | 3.8 | 15.2 | 57.3 | ||||||||
| Mozambique | 20 065 | 152 | 45 | 9.92 | 47 | 16.1 | 4.5 | 34.9 | ||||||||
| Cambodia | 13 724 | 141 | 54 | 7.68 | 54.9 | 1.6 | 5.4 | 44 | ||||||||
| Uganda | 28 059 | 138 | 49 | 7.63 | 69 | 6.7 | 1.3 | 47.1 | ||||||||
| Senegal | 11 477 | 137 | 55 | 7.44 | 28.9 | 0.9 | 1.5 | 45.7 | ||||||||
| United Republic of Tanzania | 37 522 | 126 | 48 | 7.23 | 57.1 | 6.5 | 5.5 | 32.2 | ||||||||
| Benin | 8 228 | 152 | 53 | 6.61 | 46.4 | 1.8 | 2.9 | 27.1 | ||||||||
| Afghanistan | 24 112 | 257 | 42 | 6.39 | 7.3 | 0.1 | 1.9 | 46.1 | ||||||||
| Sierra Leone | 5 361 | 283 | 39 | 5.61 | 40.9 | 1.6 | 1.3 | 8.1 | ||||||||
| Mali | 11 276 | 219 | 46 | 5.46 | 39.8 | 1.7 | 6.4 | 33.9 | ||||||||
| Guinea-Bissau | 1 550 | 203 | 47 | 5.1 | 34.4 | 3.8 | 5.2 | 24.6 | ||||||||
| Gambia | 1 570 | 122 | 57 | 5.04 | 79.2 | 2.4 | 1.9 | 3.1 | ||||||||
| Eritrea | 4 349 | 82 | 60 | 4.93 | 45.1 | 2.4 | 26.3 | 18.6 | ||||||||
| Lao People’s Democratic Republic | 5 577 | 83 | 59 | 4.83 | 29 | 0.1 | 3.2 | 25.7 | ||||||||
| Burkina Faso | 13 509 | 192 | 48 | 4.73 | 46.3 | 2 | 7 | 19.5 | ||||||||
| Mauritania | 2 882 | 125 | 58 | 4.53 | 60 | 0.7 | 8.1 | 9.2 | ||||||||
| Burundi | 7 588 | 190 | 45 | 4.4 | 67.6 | 3.3 | 9 | 18.9 | ||||||||
| Liberia | 3 382 | 235 | 42 | 4.14 | 55.8 | 3.5 | 3.8 | 33.5 | ||||||||
| Central African Republic | 4 127 | 193 | 41 | 3.9 | 65.4 | 10.7 | 2 | 9.6 | ||||||||
| Angola | 15 641 | 260 | 40 | 3.8 | 54.1 | 3.7 | 2.5 | 29.6 | ||||||||
| Guinea | 8 840 | 155 | 53 | 3.52 | 52 | 1.5 | 9.5 | 35.1 | ||||||||
| Niger | 12 823 | 259 | 41 | 3.41 | 44.1 | 1.1 | 3.4 | 23.1 | ||||||||
| Democratic Republic of the Congo | 57 003 | 205 | 44 | 3.19 | 39.1 | 3.2 | 0.5 | 31.1 | ||||||||
| Nepal | 26 560 | 76 | 61 | 2.99 | 25 | 0.5 | 19.8 | 41.3 | ||||||||
| Ethiopia | 77 036 | 166 | 50 | 2.9 | 68.3 | 2.2 | 5.8 | 35.8 | ||||||||
| Madagascar | 18 143 | 123 | 57 | 2.77 | 41.9 | 0.5 | 3.6 | 30.2 | ||||||||
| Togo | 6 074 | 140 | 54 | 2.35 | 65 | 3.2 | 2.2 | 10.8 | ||||||||
| Somalia | 7 962 | NA | NA | 2.14 | 64.4 | NA | 2.5 | 20.8 | ||||||||
| Yemen | 20 496 | 111 | 59 | 1.88 | 17.8 | 0.1 | 35.2 | 22.8 | ||||||||
| Bangladesh | 150 497 | 77 | 62 | 1.71 | 9.9 | 0.1 | 18.4 | 34.2 | ||||||||
| Sudan | 36 188 | 91 | 58 | 1.71 | 60.1 | 1.6 | 1.2 | 43.2 | ||||||||
| Chad | 9 802 | 200 | 46 | 1.59 | 39.7 | 3.5 | 4.6 | 36.9 | ||||||||
| Myanmar | 47 570 | NA | NA | 0.64 | 53.6 | NA | 3.6 | 24.6 | ||||||||
LDC, least developed country; MDG, Millennium Development Goal; NA, not available; ODA, official development assistance. Statistics from the Development Assistance Committee of the Organisation for Economic Co-operation and Development.
The first 10 countries in Table 2 capture almost half (49.1%) of total health ODA for LDCs, although they account for only one fifth of the population (21%). In 20 (out of the 50) LDCs, more than 50% of health ODA is targeted to MDG-6. Health ODA for MDG-5 amounts to 10% or more of all health ODA in just 7 countries.Twenty countries receive more than 33% of their health ODA as technical cooperation.
A major predictor of aid per capita in LDCs is HIV/AIDS prevalence. In countries such as Rwanda there is evidence that these resources have a positive effect on the health system as a whole.11 Countries with low HIV/AIDS prevalence (but high levels of morbidity and mortality from other causes) receive much less aid and thus remain at a disadvantage.
Discussion
The analysis presented in this paper relies primarily on figures reported to the OECD by official donors. The major limitation of these data is that the categories into which health ODA is classified are broad, making detailed analysis difficult. Nevertheless, we believe that our analysis highlights significant imbalances and distortions in the provision of health aid. We have deliberately avoided speculating on the causes of these imbalances. Rather, our aim has been to make the figures available with a view to stimulating debate.
Health ODA is increasing, and health is capturing a bigger share of all ODA. While this is encouraging, there are some marked imbalances in the allocation of health aid which run counter to the commitments of the Paris Declaration. Countries with comparable levels of poverty and health-related needs receive remarkably different levels of aid. Funding for MDG-6 accounts for much of the recent increase in health ODA. Many other health and health-related priorities remain insufficiently funded. In particular, “systems issues”, such as management, logistics, procurement, infrastructure and workforce development, are often neglected. These areas may not appeal to donors, but they will have to be tackled if current progress in disease control is to continue and if the quality and coverage of health services are to improve. Given that HIV/AIDS control already benefits from comparatively high levels of support, but at the same time still faces a funding gap, raising the additional resources needed to strengthen health systems – and thereby address MDGs 4 and 5 – will be a challenge.
In comparison to other sectors, a large proportion of aid in the health sector is channelled through multi-country projects or spent on technical cooperation. The latter plays an important role in transferring knowledge and skills to build capacity in developing countries. However, spending such large proportions of aid resources on technical cooperation seems difficult to justify, particularly in settings where national resources for health are meagre and large segments of the population have no access to drugs or basic health-care services. Further analysis – for example, to distinguish between funding amounts for long- and short-term technical cooperation and between technical cooperation funds spent on international versus local personnel – would be useful.
Finally, our findings suggest that control over spending decisions at the country level is limited, as global and regional priorities dominate aid allocation. Indeed, the amount of aid channelled through sector- and budget-support programmes remains low, despite recognition that this is one of the most efficient forms of aid.
The imbalances identified by our analysis predate the Paris Declaration. The data currently available are insufficient to assess whether that agreement has had an impact on health aid flows. Much of the debate on how to make health aid more effective has focused on institutional fragmentation in global health and on the need to reform the health aid architecture. However, our findings show that many other issues also need to be addressed. Continued close monitoring of financial flows is needed to fully understand the challenges and to inform the debate on how health aid can be made more effective. We recommend that a review of the type presented here be repeated every 3 years. ■
Acknowledgements
We are grateful to Shambhu Acharya, Andrew Cassels and Iqbal Shah at WHO Headquarters for their comments and input on this paper. Special thanks to the OECD Development Assistance Committee staff for their valuable assistance. Rebecca Dodd is also a PhD student at the School of Population Health, University of Queensland, Australia.
Footnotes
Competing interests: None declared.
References
- 1.Caines K. Key evidence from major studies of selected global health partnerships:background paper prepared for the High-Level Forum on the Health MDGs London: Department for International Development Health Resource Centre; 2005. [Google Scholar]
- 2.Cohen J. The New World of Global Health. Science. 2006;311:162–7. doi: 10.1126/science.311.5758.162. [DOI] [PubMed] [Google Scholar]
- 3.Fidler D. Architecture amidst anarchy: global health’s quest for governance. Global Health Governance 2007;1. Available from: http://ghgj.org/Fidler_1.1_Architecture.htm [accessed on 27 July 2009].
- 4.Kickbusch I. The development of international health policies – accountability intact? Soc Sci Med. 2000;51:979–89. doi: 10.1016/S0277-9536(00)00076-9. [DOI] [PubMed] [Google Scholar]
- 5.Shiffman J. Has donor prioritization of HIV/AIDS displaced aid for other health issues? Health Policy Plan. 2008;23:95–100. doi: 10.1093/heapol/czm045. [DOI] [PubMed] [Google Scholar]
- 6.Lane C, Glassman A. Bigger and better? Scaling up and innovation in health aid. Health Aff. 2007;26:935–48. doi: 10.1377/hlthaff.26.4.935. [DOI] [PubMed] [Google Scholar]
- 7.Paris Declaration on Aid Effectiveness. Adopted at the: Paris High-Level Forum, Paris, 28February–2March2005 Available from: http://www.oecd.org/dataoecd/11/41/34428351.pdf [accessed on 27 July 2009].
- 8.Global monitoring report 2008 Washington, DC: The World Bank; 2008. [Google Scholar]
- 9.Organisation for Economic Co-operation and Development. Reporting directives for the Creditor Reporting System. Paris: OECD; 2007 (DCD/DAC(2007)39/FINAL). [Google Scholar]
- 10.Williams G. Fiscal space and sustainability from the perspective of the health sector. In: High-Level Forum on the Health Millennium Development Goal: selected papers, 2003–2005 Geneva: World Health Organization; 2006. [Google Scholar]
- 11.Effective Aid – Better Health. Report prepared for the: Third High-Level Forum on Aid Effectiveness, Accra (Ghana), 2–4 September 2008 Geneva: World Health Organization; 2008. [Google Scholar]
- 12.Buse K, Walt G. An unruly melange? Coordinating external resources to the health sector: a review. Soc Sci Med. 1997;45:449–63. doi: 10.1016/S0277-9536(96)00365-6. [DOI] [PubMed] [Google Scholar]
- 13.Cassels A. Health sector reform: key issues in less developed countries. J Int Dev. 1995;7:329–47. doi: 10.1002/jid.3380070303. [DOI] [PubMed] [Google Scholar]
- 14.Walt G, Buse K. Partnership and fragmentation in international health: threat or opportunity? Trop Med Int Health. 2000;5:467–71. doi: 10.1046/j.1365-3156.2000.00596.x. [DOI] [PubMed] [Google Scholar]
- 15.World health report 2006: working together for health Geneva: World Health Organization; 2006. [Google Scholar]
- 16.Global health initiatives and health systems strengthening: the challenge of providing technical support (technical approach paper). London: HLSP Institute; 2008.Available from: http://www.hlspinstitute.org/files/project/216258/TS_for_HSS_June08.pdf [accessed on 27 July 2009].
- 17.Shiffman J. Donor funding priorities for communicable disease control in the developing world. Health Policy Plan. 2006;21:411–20. doi: 10.1093/heapol/czl028. [DOI] [PubMed] [Google Scholar]
- 18.Killick T, Lawson A. Budget support to Ghana: a risk worth taking? (briefing paper 24). London: Overseas Development Institute; 2007. [Google Scholar]
- 19.Lister S, Carter R. Evaluation of general budget support: synthesis report: executive summary London: Department for International Development; 2006. [Google Scholar]
- 20.Why we need to work more effectively in fragile states London: Department for International Development; 2005.