Abstract
We studied whether readiness to change predicts alcohol consumption (drinks per day) 3 months later in 267 medical inpatients with unhealthy alcohol use. We used 3 readiness to change measures: a 1 to 10 visual analog scale (VAS) and two factors of the Stages of Change Readiness and Treatment Eagerness Scale: Perception of Problems (PP) and Taking Action (TA). Subjects with the highest level of VAS-measured readiness consumed significantly fewer drinks 3 months later [Incidence rate ratio (IRR) and 95% confidence interval (CI): 0.57 (0.36, 0.91) highest vs. lowest tertile]. Greater PP was associated with more drinking [IRR (95%CI): 1.94 (1.02, 3.68) third vs. lowest quartile]. Greater TA scores were associated with less drinking [IRR (95%CI): 0.42 (0.23, 0.78) highest vs. lowest quartile]. Perception of Problems' association with more drinking may reflect severity rather than an aspect of readiness associated with ability to change; high levels of Taking Action appear to predict less drinking. Although assessing readiness to change may have clinical utility, assessing the patient's planned actions may have more predictive value for future improvement in alcohol consumption.
Keywords: unhealthy alcohol use, readiness to change, medical inpatients, Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES)
INTRODUCTION
Consequences resulting from excessive alcohol consumption are responsible for considerable disease burden (Rehm et al., 2003). Consequently, interventions aimed at reducing excessive alcohol consumption are viewed as beneficial from a public health point of view. In 2004, the US Services Preventive Task Force recommended the use of brief counseling intervention in primary care, where its efficacy has been confirmed; this practice is among the most effective and cost-effective of preventive care services (Bertholet, Daeppen, Wietlisbach, Fleming, & Burnand, 2005; Solberg, Maciosek, & Edwards, 2008). Assessing readiness to change is recommended as part of brief interventions to tailor advice and counseling, and physicians have been encouraged to see changes in readiness as short term goals on the path to behavior change (Samet, Rollnick, & Barnes, 1996).
The focus on readiness is based in large part on the assumption that there is a clear association between readiness and outcome (e.g., decreases in drinking). But stage-matched interventions may not be more effective than those that do not specifically address stage of change (Rollnick, 1998), and there is conflicting evidence regarding the relationship between readiness to change and outcome (Forsberg, Ekman, Halldin, & Ronnberg, 2004; Isenhart, 1997; Reed et al., 2005). This conflicting evidence may have a number of explanations. First, a family of concepts is included under the term “readiness,” and those concepts, especially importance of change or confidence in ability to change, could operate differently. In particular, confidence or self-efficacy seem to predict better outcomes (Maisto, Conigliaro et al., 1999). Action-related measures seem also to be predictive of better outcomes (Demmel, Beck, Richter, & Reker, 2004). Because recognition of a problem is intimately linked with its severity, readiness could also be interpreted as a measure of severity (Maisto, Conigliaro et al., 1999; Williams, Horton, Samet, & Saitz, 2007) but may also be related to self-efficacy (Demmel et al., 2004).
The differing associations between readiness measures and outcomes may also be explained by setting or circumstance, and by the assessment instrument, since various questionnaires have been used to assess readiness to change, stages of change, and motivation, some of which measure overlapping constructs.
The role of readiness to change is of particular interest in patients with unhealthy alcohol use (i.e., the spectrum from risky consumption to alcohol dependence) identified by screening in general health settings, such as hospitals. In this circumstance, patients are not necessarily help-seeking, unlike patients in specialty treatment. Since hospitalization and the presence of alcohol-related medical problems may provide a “teachable moment,” it is important to better understand the relationship between readiness and outcome in this setting.
Therefore we studied whether readiness to change predicts subsequent alcohol consumption in medical inpatients with unhealthy alcohol use. We studied this association using three different measures of readiness to change based on two instruments—a visual analog scale (VAS) for the simple question “how ready are you to change your drinking habits?” and two factors from the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES), level of perception of the drinking problem and taking action towards change / commitment to making a change. We hypothesized that a high level of taking action towards change / commitment to change would be associated with less drinking, and that greater problem perception would be associated with more drinking.
METHODS
We studied a prospective cohort of medical inpatients at an urban academic hospital who were drinking risky amounts (>14 drinks/wk or ≥5drinks/occasion for men, >11 drinks/wk or ≥4 drinks per occasion for women and persons aged 66 and over). Subjects were participants in a randomized trial of brief intervention to reduce alcohol use (Saitz et al., 2007) and were recruited from the inpatient medical service of an urban teaching hospital. Research associates approached all patients aged 18 or older whose physicians did not decline patient contact. Individuals fluent in English or Spanish who gave consent were asked to complete a screening interview. Eligibility criteria included the following: currently drinking risky amounts, 2 contacts to assist with follow up, no plans to move from the area for the next year, and a Mini-Mental State Examination score of ≥21 (Smith, Horton, Saitz, & Samet, 2006). Eligible subjects were randomized to receive usual care or a brief intervention to reduce alcohol use. The study population was used as a cohort in the present analyses. Assessments took place before group allocation.
Assessments
Demographics were assessed at study entry, as well as medical diagnoses by medical record review, and alcohol use disorder diagnosis based on the Diagnostic and Statistical Manual on Mental Disorders, 4th edition and determined by the Composite International Diagnostic Interview (CIDI) Alcohol Module (Robins et al., 1988; WHO, 1996). More details on assessment and enrollment were previously published (Saitz et al., 2007).
At study entry in the hospital and 3 months later, alcohol consumption was assessed using a validated calendar method (Timeline Followback) (Sobell & Sobell, 1995). Readiness to change was assessed with a 1-10 visual analog scale (VAS) and with the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). The VAS measure was a response to: “How ready are you to change your drinking habits?” The VAS has not been extensively validated but is attractive for clinical use in busy settings because of its brevity (LaBrie, Quinlan, Schiffman, & Earleywine, 2005; Williams et al., 2007). The SOCRATES is a 19 item questionnaire developed to assess readiness to change alcohol use (Miller & Tonnigan, 1996). Based on a factor analysis in this sample (Bertholet, Horton, & Saitz, 2007), we used a 2 factor structure for analyses on 16 items: 1-“Perception of Problems” (PP), and 2-“Taking Action” (TA). These two factors had good internal consistency (Cronbach's alpha 0.94 and 0.88, respectively). PP represents problem awareness and recognition of the need for additional help to address the drinking problem and TA denotes the concrete steps a person is taking or has already taken towards a decrease in drinking and commitment to change.
Analysis
The primary outcome was the average number of standard drinks per day (past 30 days) assessed at 3 months. The main predictors of interest were the three readiness to change measures (VAS readiness, SOCRATES PP and TA). To avoid assumptions of a linear relation between readiness to change measures and outcome, each independent variable was categorized into quartiles, with the exception of VAS where division into quartiles was not feasible due to the distribution of the data and tertiles were used instead. The distribution of drinks per day at 3 months, a count variable, was skewed, with a considerable number of zeros and a long tail, so the use of models assuming normality was not adeuqate. Therefore we used overdispersed Poisson regression models to assess the effect of readiness to change on subsequent drinking (Horton, Kim, & Saitz, 2007; McCullagh & Nelder, 1989). The Pearson chi-square correction was used to account for overdispersion in the data. Separate models were fit for VAS readiness and each of the two SOCRATES factors, and controlled for drinking at study entry (drinks per day, last 30 days), randomization group (despite the fact that there was no effect of intervention group in the parent trial on drinking outcome, both groups having reduced their drinking), age, gender, any heroin or cocaine use (last 30 days), marijuana use (last 30 days) and presence of an alcohol-related medical diagnosis at hospital admission. All analyses were conducted using two-sided tests and a significance level of 0.05. Analyses were performed using SAS software (version 9.1; SAS Institute, Cary, NC).
RESULTS
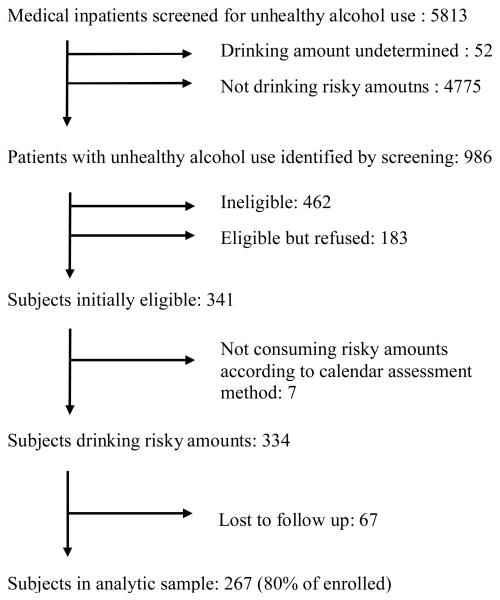
Of the 986 subjects with unhealthy alcohol use identified by screening, 462 were ineligible and 183 refused participation. Eligible subjects who enrolled more likely to be Black (45% vs 31%) and to drink greater amounts of alcohol (24 vs 18 drinks per week) compared to eligible subjects who refused participation. Of the 341 remaining eligible subjects, we excluded 7 because although they had unhealthy alcohol use according to the screening questions, results of the calendar assessment method were that they had not consumed risky amounts recently. An additional 67 of the 334 subjects (20.1%) were lost to follow-up and were excluded from the present analyses (Figure 1). Those analyzed were not different from those lost to follow up (p>0.05) with respect to alcohol consumption, readiness to change measures (VAS readiness, SOCRATES factors), age, gender, living with a partner, employment, homelessness, or drug use.
Figure 1.
Selection of subjects with unhealthy alcohol use for the prospective cohort study
Subject's median (25th and 75th percentiles) readiness to change drinking at study entry on a visual analog scale (VAS) that ranged from 1-10 was 8 (5, 10). Median (25th and 75th percentiles) SOCRATES Perception of Problems (PP) score was 39 (28, 44) on a scale from 10-50. Median (25th and 75th percentiles) SOCRATES Taking Action (TA) score was 22 (18, 26) on a scale from 6-30. Other subjects' characteristics are presented in Table 1.
Table 1.
Baseline Characteristics of the 267 medical inpatients with unhealthy alcohol use (n=267)
| Demographics | |
| Women, no. (%) | 81 (30.3) |
| Age, mean (SD) | 45.0 (10.5) |
| Race/Ethnicity: | |
| Black, no. (%) | 129 (48.3) |
| White, no. (%) | 96 (36.0) |
| Hispanic, no. (%) | 23 (8.6) |
| Other, no. (%) | 19 (7.1) |
| Alcohol related diagnosis at hospital admission, no. (%) | 129 (48.3) |
| Alcohol diagnosis (past year)† | |
| No diagnosis, no. (%) (risky drinking) | 46 (17.2) |
| Alcohol abuse, no. (%) | 13 (4.9) |
| Alcohol dependence, no. (%) | 208 (77.9) |
| Alcohol consumption (past 30 days) | |
| Drinks per day, mean (SD), median | 6.9 (9.0) 4.0 |
| # of days with binge drinking, no. (%), median | 12.8 (10.7) 9 |
| Drug use (last 30 days) | |
| Heroin or cocaine use, no. (%) | 68 (25.5) |
| Marijuana use, no. (%) | 81 (30.6) |
| Readiness to change measures | |
| Visual analog scale*, mean (SD), median (IQR) | 6.9 (3.5), 8(5, 10) |
| SOCRATES**: | |
| Perception of Problems, mean (SD), median (IQR) | 35.6 (10.8), 39 (28, 44) |
| Taking Action, mean (SD), median (IQR) | 21.2 (5.8), 22 (18, 26) |
determined with the Composite International Diagnostic Interview (CIDI) Alcohol Module
“How ready are you to change your drinking habits?” 1to10
Perception of Problems, possible score: 10-50; Taking Action (commitment to change), possible score 6-30
IQR: interquartile range (25th,75th percentile)
Association between readiness and consumption
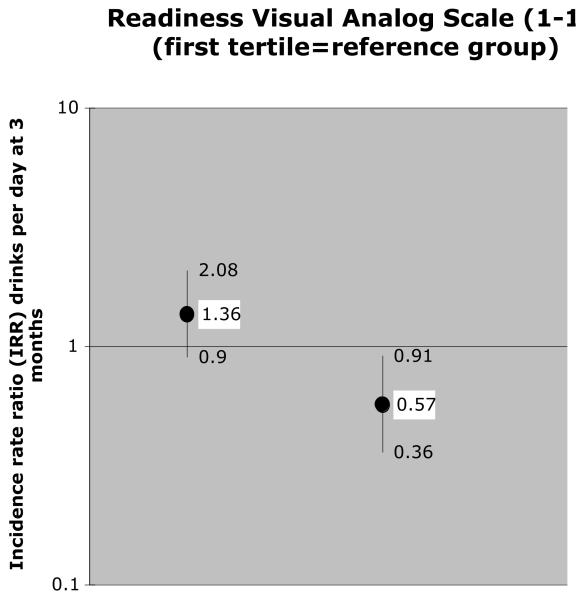
In adjusted analyses, subjects with VAS-measured readiness in the highest tertile at study entry, compared to those in the lowest tertile, drank significantly fewer drinks per day 3 months later (incidence rate ratio [IRR] 0.57, 95% confidence interval [CI] 0.36, 0.91); the middle tertile was not significantly associated with consumption (IRR [95%CI] 1.36 [0.90, 2.08]) (Figure 2).
Figure 2. Association between readiness to change (assessed with a visual analog scale) and drinks per day at 3 months†.
†: Controlled for drinking at study entry (drinks per day, last 30 days), randomization group, age, gender, heroin or cocaine use (last 30 days), marijuana use (last 30 days) and presence of an alcohol related medical diagnosis at hospital admission
Lines represent 95% confidence intervals
Tertiles were used instead of quartiles because of the distribution of data (see text)
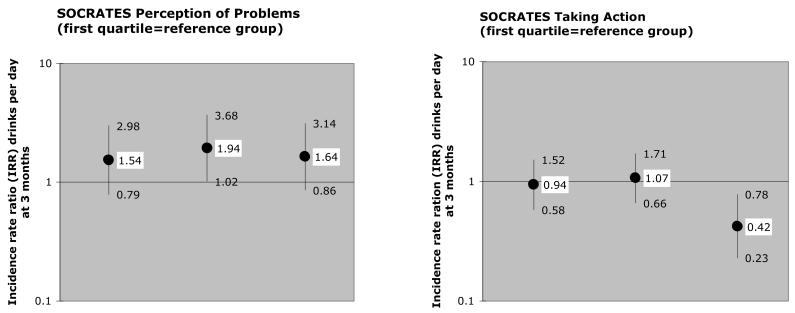
Subjects with Perception of Problems (PP) scores in the 3rd quartile, compared with those in the lowest quartile, drank significantly more at 3 months (IRR [95% CI] 1.94 [1.02, 3.68]); drinking was also higher but associations were not significant for the highest and second quartiles (IRRs [95% CIs] for 2nd quartile: 1.54 [0.79, 2.98], and for highest quartile: 1.64 [0.86, 3.14]) (Figure 3). Subjects with Taking Action (TA) scores in the highest quartile, compared with those in the lowest quartile, drank significantly less at 3 months (IRR [95% CI] 0.42 [0.23, 0.78]); associations were not significant for the second and third quartiles (IRRs [95% CIs] for 2nd quartile: 0.94 [0.58, 1.52], and for 3rd quartile: 1.07 [0.66, 1.71]) (Figure 3).
Figure 3. Associations between readiness to change (assessed with the SOCRATES factor 1: Perception of Problems and factor 2: Taking Action) and drinks per day at 3 months†.
†: Controlled for drinking at study entry (drinks per day, last 30 days), randomization group, age, gender, heroin or cocaine use (last 30 days), marijuana use (last 30 days) and presence of an alcohol related medical diagnosis at hospital admission
SOCRATES=Stages of Change Readiness and Treatment Eagerness Scale. Lines represent 95% confidence intervals.
DISCUSSION
We explored whether readiness to change predicts subsequent alcohol consumption three months after a medical hospitalization among adults with unhealthy alcohol use. The predictive value of readiness to change appears to depend on the measures used, and on the various concepts included under the rubric of “readiness.” Components of readiness to change measured by the SOCRATES questionnaire (“Perception of Problems” and “Taking Action” or commitment to change) appear to operate differently. Higher levels of Perception of Problems appeared to be associated with more, not less, drinking 3 months later. These results suggest that this measure may capture severity rather than an aspect of readiness associated with the ability to change in the future (Maisto, Conigliaro et al., 1999). In contrast, the highest level of Taking Action was associated with less drinking. Results suggested a threshold level for Taking Action; only the highest level was associated with a decrease in drinking. The highest level of Taking Action was the strongest predictor of decrease in drinking 3 months later of all the measures examined.
The implications of our results for the SOCRATES are that greater Perception of Problems is not a predictor of decreased drinking since it may be a measure of severity. In contrast to the denial stereotype, patients in this sample of mainly non-treatment seeking alcohol dependent adults appeared to recognize that their drinking patterns were problematic, which is consistent with other studies where higher readiness to change was associated with more consequences (Williams et al., 2006). Our results also underscore the importance of commitment to change, and change-related actions (i.e. concrete steps a person takes towards a decrease in drinking); a high level of Taking Action was predictive of less drinking, consistent with studies that have emphasized the impact of commitment to change on behavior change (Amrhein, Miller, Yahne, Palmer, & Fulcher, 2003).
The second measure used, the visual analog scale, was associated with less drinking at the highest level. Of note, the middle tertile appeared to be associated with more drinking, although the results were not statistically significant. It is possible that different concepts (e.g. severity, and commitment) may be captured with this single scale, or that there may be simply threshold effects. Thus, outside its clinical utility to elicit discussion about alcohol use during a patient-physician interaction, the VAS should probably be used with caution as a predictive tool.
We are unaware of similar studies of the predictive value of readiness measures in medical inpatients with unhealthy alcohol use. Nonetheless, these results are comparable to those observed in other populations regarding the importance of commitment to change and planned action. Readiness is predictive of change when related to action in people with alcohol dependence recruited in psychiatric hospitals (Demmel et al., 2004). As such, counseling that supports self-efficacy and action plans may be particularly useful for medical inpatients with unhealthy alcohol use (Maisto, Carey, & Bradizza, 1999). Our results also add to the evidence linking problem recognition to severity. Individuals with more severe problems related to their alcohol consumption are more likely to have high level of recognition (Williams et al., 2007; Williams et al., 2006).
These findings should be considered in the context of limitations of the present study. First, our subjects agreed to participate in a study in which they could receive alcohol counseling. This sample could have been predisposed to change. In addition, participants drank more than those who refused to enroll in the study. However, enrolled subjects and refusers did not differ on VAS-measured readiness to change. Given the approach to recruitment in this study, these results are likely generalizable to individuals who agree to talk about their alcohol consumption after screening. Second, although recommended for use based on its face validity, the visual analog scale for readiness has not been extensively validated.
Secondary analysis of randomized trial data can raise methodological challenges. But unlike secondary analyses in other cohorts, an intervention is well-specified and its receipt and effects are known. In our study, the intervention delivered was not effective: both groups (intervention and usual care) reduced their drinking without statistically significant differences between groups (Saitz et al., 2007). In addition we controlled all analyses for randomization group. Furthermore, the follow-up rate was high and did not differ by group. Finally, prospective data collection and follow-up in this randomized trial is a strength because of high quality assessments and a detailed description of the study population.
Our study also had notable strengths. We used a large sample of mostly dependent medical inpatients, a population that is of great interest since they are at higher risk of morbidity and mortality, represent the vast majority of medical inpatients with unhealthy alcohol use (Freyer-Adam et al., 2008; Saitz, Freedner, Palfai, Horton, & Samet, 2006), and are generally not seeking alcohol treatment despite experiencing alcohol consequences. Data collection was prospective and loss to follow-up was small. We used a factor structure for the SOCRATES questionnaire that was determined in medical inpatients. Since this questionnaire has been shown to have different factor structure across settings, it was a strength to use a structure determined for this sample (Demmel et al., 2004; Figlie, Dunn, & Laranjeira, 2004; Maisto, Chung, Cornelius, & Martin, 2003; Maisto, Conigliaro et al., 1999; Miller & Tonnigan, 1996). By using various measures of readiness to change, we were able to test different aspects of readiness. Also, by avoiding the assumption of a linear relation between readiness to change measures and drinking outcome in our analyses, we were able to identify a more refined relation between readiness and outcome.
In conclusion, readiness to change does predict subsequent alcohol consumption in medical inpatients with unhealthy alcohol use, however, readiness appears to be less useful as a monolithic construct. Readiness appears to be comprised of a number of more specific constructs. These findings may explain, at least in part, inconsistencies in the literature regarding the predictive ability of “readiness” and the role and importance of “readiness” for behavior change. In medical inpatients, the readiness construct “Perception of Problems” (or problem recognition) should be viewed more as a measure of severity than as a predictor of change. Nevertheless, it may still be useful to assess problem recognition as a first step to set goals and to plan actions to reduce drinking or to attend specialty treatment. Visual analog scale measures of readiness have some ability to predict behavior change however this ability may operate only after some threshold. Since a high level of taking action / commitment to change appeared to predict less drinking, physicians should be encouraged to enhance their patient's self-efficacy and help them set goals and action plans. For greatest clinical and predictive utility, the component concepts of readiness should be separated when they are measured and used in research and practice. Additional studies of these separate constructs may help determine their optimal use.
REFERENCES
- Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. J Consult Clin Psychol. 2003;71(5):862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165(9):986–995. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- Bertholet N, Horton NJ, Saitz R. Factor Structure Of The Socrates Questionnaire In Hospitalized Medical Patients. Alcoholism Clin Exp Res. 2007;31(suppl):43A. doi: 10.1016/j.addbeh.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demmel R, Beck B, Richter D, Reker T. Readiness to change in a clinical sample of problem drinkers: relation to alcohol use, self-efficacy, and treatment outcome. Eur Addict Res. 2004;10(3):133–138. doi: 10.1159/000077702. [DOI] [PubMed] [Google Scholar]
- Figlie NB, Dunn J, Laranjeira R. Factor structure of the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) in alcohol dependent outpatients. Rev Bras Psiquiatr. 2004;26(2):91–99. doi: 10.1590/s1516-44462004000200005. [DOI] [PubMed] [Google Scholar]
- Forsberg L, Ekman S, Halldin J, Ronnberg S. The readiness to change questionnaire: reliability and validity of a Swedish version and a comparison of scoring methods. Br J Health Psychol. 2004;9(Pt 3):335–346. doi: 10.1348/1359107041557084. [DOI] [PubMed] [Google Scholar]
- Freyer-Adam J, Coder B, Baumeister SE, Bischof G, Riedel J, Paatsch K, et al. Brief alcohol intervention for general hospital inpatients: A randomized controlled trial. Drug Alcohol Depend. 2008;93(3):233–243. doi: 10.1016/j.drugalcdep.2007.09.016. [DOI] [PubMed] [Google Scholar]
- Horton NJ, Kim E, Saitz R. A cautionary note regarding count models of alcohol consumption in randomized controlled trials. BMC Med Res Methodol. 2007;7:9. doi: 10.1186/1471-2288-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isenhart CE. Pretreatment readiness for change in male alcohol dependent subjects: predictors of one-year follow-up status. J Stud Alcohol. 1997;58(4):351–357. doi: 10.15288/jsa.1997.58.351. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Quinlan T, Schiffman JE, Earleywine ME. Performance of alcohol and safer sex change rulers compared with readiness to change questionnaires. Psychol Addict Behav. 2005;19(1):112–115. doi: 10.1037/0893-164X.19.1.112. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Carey KB, Bradizza CM. Social learning theory. In: Leonard KE, Blane HT, editors. Psychological Theories of Drinking and Alcoholism. Guilford Press; New York: 1999. pp. 106–163. [Google Scholar]
- Maisto SA, Chung TA, Cornelius JR, Martin CS. Factor structure of the SOCRATES in a clinical sample of adolescents. Psychol Addict Behav. 2003;17(2):98–107. doi: 10.1037/0893-164x.17.2.98. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Conigliaro J, McNeil M, Kraemer K, O'Connor M, Kelley ME. Factor structure of the SOCRATES in a sample of primary care patients. Addict Behav. 1999;24(6):879–892. doi: 10.1016/s0306-4603(99)00047-7. [DOI] [PubMed] [Google Scholar]
- McCullagh P, Nelder JA. Generalized Linear Models. 2nd ed. Chapman and Hall; London, England: 1989. [Google Scholar]
- Miller WR, Tonnigan JS. Assessing drinker's motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) Psychol Addict Behav. 1996;10:81–89. [Google Scholar]
- Reed DN, Jr., Wolf B, Barber KR, Kotlowski R, Montanez M, Saxe A, et al. The stages of change questionnaire as a predictor of trauma patients most likely to decrease alcohol use. J Am Coll Surg. 2005;200(2):179–185. doi: 10.1016/j.jamcollsurg.2004.10.020. [DOI] [PubMed] [Google Scholar]
- Rehm J, Room R, Monteiro M, Gmel G, Graham K, Rehn N, et al. Alcohol as a risk factor for global burden of disease. Eur Addict Res. 2003;9(4):157–164. doi: 10.1159/000072222. [DOI] [PubMed] [Google Scholar]
- Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry. 1988;45(12):1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- Rollnick S. Readiness, importance and confidence: critical conditions of change in treatment. In: Miller WR, Heather N, editors. Treating Addictive Behaviour. 2nd ed. Plenum; New York: 1998. [Google Scholar]
- Saitz R, Freedner N, Palfai TP, Horton NJ, Samet JH. The severity of unhealthy alcohol use in hospitalized medical patients. The spectrum is narrow. J Gen Intern Med. 2006;21(4):381–385. doi: 10.1111/j.1525-1497.2006.00405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Palfai TP, Cheng DM, Horton NJ, Freedner N, Dukes K, et al. Brief intervention for medical inpatients with unhealthy alcohol use: a randomized, controlled trial. Ann Intern Med. 2007;146(3):167–176. doi: 10.7326/0003-4819-146-3-200702060-00005. [DOI] [PubMed] [Google Scholar]
- Samet JH, Rollnick S, Barnes H. Beyond CAGE. A brief clinical approach after detection of substance abuse. Arch Intern Med. 1996;156(20):2287–2293. doi: 10.1001/archinte.156.20.2287. [DOI] [PubMed] [Google Scholar]
- Smith KL, Horton NJ, Saitz R, Samet JH. Use of mini-mental state examination in recruitment for substance abuse research studies. Drug Alc Depend. 2006;(82):231–237. doi: 10.1016/j.drugalcdep.2005.09.012. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol Timeline Followback (TLFB) Users' Manual. Addiction Research Foundation; Toronto, Canada: 1995. [Google Scholar]
- Solberg LI, Maciosek MV, Edwards NM. Primary care intervention to reduce alcohol misuse ranking its health impact and cost effectiveness. Am J Prev Med. 2008;34(2):143–152. doi: 10.1016/j.amepre.2007.09.035. [DOI] [PubMed] [Google Scholar]
- WHO. Composite International Diagnostic Interview (CIDI)(Core Version 2.0) World Health Organization; Geneva, Swtizerland: 1996. [Google Scholar]
- Williams EC, Horton NJ, Samet JH, Saitz R. Do brief measures of readiness to change predict alcohol consumption and consequences in primary care patients with unhealthy alcohol use? Alcohol Clin Exp Res. 2007;31(3):428–435. doi: 10.1111/j.1530-0277.2006.00324.x. [DOI] [PubMed] [Google Scholar]
- Williams EC, Kivlahan DR, Saitz R, Merrill JO, Achtmeyer CE, McCormick KA, et al. Readiness to change in primary care patients who screened positive for alcohol misuse. Ann Fam Med. 2006;4(3):213–220. doi: 10.1370/afm.542. [DOI] [PMC free article] [PubMed] [Google Scholar]