Abstract
Objective. Inflammatory arthritis in childhood is variable in terms of both presentation and outcome. This analysis describes disease activity in children with juvenile idiopathic arthritis (JIA) during the first year following presentation to a paediatric rheumatologist and identifies predictors of moderate to severe disability [defined using a Childhood HAQ (CHAQ) score ⩾0.75] at 1 year.
Methods. The Childhood Arthritis Prospective Study recruits children <16 years with new inflammatory arthritis persisting for ⩾2 weeks from five UK tertiary referral centres. Demographics, disease features, joint count, CHAQ, physician's global assessment, parent's general evaluation of well-being (PGE), ESR and treatment, are collected at first presentation, 6 months and then yearly. Independent predictors of CHAQ ⩾0.75 at 1 year in children diagnosed with JIA were identified using multivariable logistic regression models.
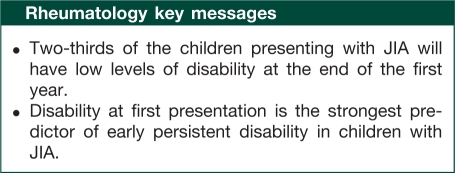
Results. Seven hundred and forty children with JIA were included; median age at presentation 7.6 years, 64% girls. During the first year, 85% received NSAIDs, 70% IA corticosteroids, 47% MTX and 27% systemic steroids (oral or i.v.). Median presenting CHAQ score was 0.63 and decreased to 0.25 at 1 year; 32% had CHAQ ⩾0.75 at 1 year. The strongest predictor of CHAQ ⩾0.75 at 1 year was CHAQ ⩾0.75 at presentation (odds ratio 3.92; 95% CI 2.17, 7.09). Additional predictors included female gender and higher PGE
Conclusion. Although CHAQ score improved in most children, the strongest predictor of persistent disability at 1 year was moderate to severe disability at first presentation. Follow-up beyond 1 year will assess whether CHAQ at presentation will continue to be a predictor of future poor outcome.
Keywords: Juvenile idiopathic arthritis, Disability, Outcomes, Disease activity
Introduction
Inflammatory arthritis is a chronic debilitating disease of childhood. It has been estimated that each year, ∼10/100 000 children will develop an inflammatory arthritis [1], with many subsequently being diagnosed with juvenile idiopathic arthritis (JIA). Although the disease course can be variable, with periods of activity followed by remission, previous studies have shown that up to 70% of children continue to report disability and limitation of their activities into adulthood [2–7]. However, comparison across studies has been difficult for many reasons, including variability in the classification of childhood arthritis [8–12], differences in study design and changes in treatments over time. In addition, most of these previous studies have based estimates of the chronicity and severity of this disease on retrospective medical record reviews, which may bias towards a more severe group of patients. As a result, many studies lack specific measures of disease activity at first presentation, making it difficult to predict later outcomes based on early presentation.
Finally, the change in the treatment of JIA towards earlier aggressive therapy is likely to have changed outcomes for many groups of patients, thus making previous estimates of outcomes less applicable to children today. Therefore, data concerning the early disease course in children presenting with inflammatory arthritis in this modern treatment era remains limited and there is a need to study prospective inception cohorts of children with inflammatory arthritis such that all aspects of the disease course can be captured, from the very mild to the most severe. Identifying early those children who are most likely to have a severe disease course may help to target therapies to those most likely to have poor outcomes and avoid over-treatment in those most likely to experience spontaneous remission.
The Childhood Arthritis Prospective Study (CAPS) is an ongoing prospective longitudinal inception cohort study, which aims to provide information on the long-term outcome of children with inflammatory arthritis following routine care in the UK. The aim of the current analysis was to describe the outcomes of children with JIA 1 year following first presentation to paediatric rheumatology and to identify factors that predicted moderate to severe disability at 1 year.
Methods
Study population
The CAPS study began recruitment in 2001. Details of this study have been described elsewhere [13]. In brief, children aged <16 years presenting to one of five paediatric rheumatology referral centres (Liverpool, Manchester, Glasgow, Newcastle-upon-Tyne and London) with a new diagnosis of inflammatory arthritis (in at least one joint) present for at least 2 weeks are approached to participate. Exclusion criteria are septic arthritis, haemarthrosis, arthritis caused by malignancy or trauma, connective tissue disorders such as SLE, MCTD or DM. Currently, the study continues to recruit new children. The study was approved by the UK Northwest Multicentre Research Ethics Committee. Written informed consent was obtained from the parent(s)/guardian for all participant children and children, if considered able, provided assent.
Baseline data collection
At the first visit, the rheumatologist performs a rheumatological exam and completes a 100-mm physician's global assessment (PGA). They are asked to assign an International League Against Rheumatism (ILAR) subtype if the suspected diagnosis is JIA. The parent(s) and child are interviewed by a rheumatology research nurse and the medical records are reviewed to extract information on demographics, diagnosis, disease characteristics including disease duration at first presentation, past medical history, medications and relevant blood tests. Blood tests are only done as part of routine care and results are recorded when performed. The parent (or where appropriate the child) completes a Childhood HAQ (CHAQ) validated for use in the UK population [14], a 100-mm pain visual analogue scale (VAS) and a 100-mm parent general evaluation (PGE).
Follow-up data
Follow-up study visits are arranged at 6 months following first presentation and then yearly for a minimum of 5 years. At each follow-up, the child again undergoes a rheumatological examination, and the PGA, PGE, CHAQ and a pain VAS are completed. Again, details of medications taken since last follow-up are extracted from the medical record, as are results of any relevant blood tests. Children who are discharged from rheumatology care continue to be followed by the rheumatology research nurse for at least two additional years.
Analysis
This analysis was limited to children with a diagnosis of JIA (that is, arthritis persisting for ⩾6 weeks in one or more joint, of no other attributable cause) who had completed at least 1 year of follow-up. Demographic and disease characteristics including the JIA core outcome variables (active and limited joint count, PGA, PGE, CHAQ score and ESR) and pain measured at first presentation and at 1 year are presented for the entire cohort and by ILAR subtype. A joint was considered active if there was swelling due to active synovitis or in the absence of swelling, limited motion accompanied by heat, pain or tenderness [15]. A limited joint was a joint limited in motion. The ILAR subtype for this analysis was assigned at 6 months of symptom duration. If children had been symptomatic for >6 months at first paediatric rheumatology visit, the ILAR subtype was assigned at the first presentation. If the child had been symptomatic for <6 months, the subtype was assigned at the 6-month follow-up visit. The values of each disease characteristic at baseline and at 1 year were compared within the whole cohort and within each individual subtype using Wilcoxon matched-pairs test.
A CHAQ score ⩾0.75 was selected to indicate moderate to severe levels of disability. Previous studies which have attempted to correlate CHAQ scores with parent or child reports of the level of disability have found a value of 0.75 to be a good discriminant between none to mild and moderate to severe disability [16, 17]. Multivariable logistic regression models were developed to identify (i) factors associated with this high CHAQ at baseline and (ii) predictors (measured at first presentation) of a high CHAQ at 1 year. Co-variates in the models included age at first presentation, gender, study site, symptom duration at first presentation (defined using month of first reported symptom onset), active and limited joint count, ESR (per 10 mm/h increments), PGA (per 10 mm increments), PGE (per 10 mm increments) and pain score (per 10 mm increments). Missing data were imputed using multiple imputation (number of repeated imputations = 35) [18, 19]. The following variables were included in the imputation: age, gender, symptom duration, active joint count, ESR, PGA, PGE, CHAQ and pain scores. Regression models were run with both unimputed and imputed data and the results of both are presented. The results are presented as odds ratios (ORs) with 95% CIs. All analyses were performed in Stata version 9.2 (Statacorp 2003, College Station, TX, USA).
Results
Up to March 2009, CAPS had registered 917 cases with JIA. Of these, 740 had reached 1 year of follow-up. The study participants were primarily Caucasian (93%) with a median age at first presentation of 7.6 years [interquartile range (IQR) 3.6–11.5]; 64% were females (Table 1). The median symptom duration at first presentation was 5.2 months (IQR 2.5–10.4). The most common ILAR subtype was oligoarthritis (48%). At first presentation, the median active joint count was 2 (IQR 1–5). The median ESR was 20 mm/h (IQR 6–46), median pain score was 32 (IQR 9–57) and the median CHAQ was 0.63 (IQR 0.13–1.38) (Tables 2 and 3). For 91 children (19%), the presenting CHAQ score was 0.
Table 1.
Demographic characteristics at first presentation to a paediatric rheumatologist
| ILAR | n (% of total) | Age at symptom onset, median (IQR), years | Age at first presentation, median (IQR), years | Female, n (% within each subtype) |
|---|---|---|---|---|
| Whole cohort | 740 (100) | 6.6 (2.8, 10.7) | 7.6 (3.6, 11.5) | 476 (64) |
| Systemic arthritis | 42 (6) | 6.4 (3.4, 10) | 6.7 (3.6, 10.1) | 32 (76) |
| Persistent oligoarthritis | 353 (48) | 5.5 (2.4, 9.8) | 6.5 (3.1, 10.8) | 225 (64) |
| Extended oligoarthritis | 32 (4) | 4.3 (1.9, 8.4) | 5.3 (2.7, 9.4) | 23 (72) |
| RF(−) polyarthritis | 148 (20) | 5.8 (2.2, 9.4) | 7.5 (3.3, 10.6) | 110 (74) |
| RF(+) polyarthritis | 23 (3) | 11.4 (9.1, 13.4) | 12.2 (9.9, 14.8) | 21 (91) |
| ERA | 51 (7) | 11.8 (10.1, 13.1) | 13 (11.3, 13.9) | 6 (12) |
| PSA | 61 (8) | 9.8 (4.3, 11.6) | 11 (5.7, 13) | 40 (66) |
| Undifferentiated | 30 (4) | 7.1 (2.7, 9.8) | 8.9 (5.8, 10.9) | 19 (63) |
ERA: enthesitis related arthritis.
Table 2.
Disease activity at baseline and 1 year
| Active joint count |
Limited joint count |
ESR (mm/h) |
||||
|---|---|---|---|---|---|---|
| ILAR | Baseline | 1 year | Baseline | 1 year | Baseline | 1 year |
| Whole cohort | 2 (1–5) | 0 (0–1)* | 1 (1–3) | 0 (0–1)* | 20 (6–45) | 9 (4–20)* |
| Systemic arthritis | 3 (1–6) | 0 (0–1)* | 0 (0–4) | 0 (0–0)* | 85 (55–102) | 25 (5–43)* |
| Persistent oligoarthritis | 1 (1–2) | 0 (0–1)* | 1 (1–2) | 0 (0–1)* | 13 (5–30) | 8 (5–16)* |
| Extended oligoarthritis | 3 (1–6) | 0 (0–1)* | 2 (1–4) | 1 (0–1)* | 34 (13–53) | 15 (9–32) |
| RF(−) polyarthritis | 8 (4–14) | 0 (0–2)* | 5 (2–11) | 1 (0–3)* | 28 (8–56) | 8 (4–21)* |
| RF(+) polyarthritis | 7 (5–22) | 1 (0–5)* | 2 (1–16) | 1 (0–2) | 18 (10–46) | 12 (6–16)* |
| ERA | 2 (1–5) | 0 (0–1)* | 2 (1–4) | 0 (0–2)* | 16 (7–32) | 8 (3–14)* |
| PSA | 3 (2–5) | 0 (0–2)* | 2 (1–3) | 1 (0–2)* | 26 (8–43) | 8 (3–17)* |
| Undifferentiated | 1 (1–6) | 0 (0–1)* | 1 (1–5) | 0 (0–2)* | 14 (6–35) | 10 (5–48) |
| Physician global score |
PGE |
Pain score |
||||
|---|---|---|---|---|---|---|
| Baseline | 1 year | Baseline | 1 year | Baseline | 1 year | |
| Whole cohort | 31 (18–56) | 6 (1–18)* | 20 (5–46) | 6 (1–27)* | 32 (9–57) | 9 (1–32)* |
| Systemic arthritis | 57 (35–72) | 14 (3–31)* | 33 (7–53) | 9 (3–36)* | 42 (10–50) | 19 (7–50) |
| Persistent oligoarthritis | 24 (15–43) | 2 (0–17)* | 15 (3–39) | 4 (0–21)* | 24 (7–50) | 6 (0–30)* |
| Extended oligoarthritis | 36 (20–61) | 8 (4–21)* | 27 (7–48) | 9 (2–36) | 36 (7–50) | 14 (1–30) |
| RF(−) polyarthritis | 47 (30–67) | 9 (2–18)* | 32 (8–53) | 7 (2–26)* | 39 (12–70) | 8 (2–25)* |
| RF(+) polyarthritis | 39 (22–67) | 9 (4–27)* | 19 (15–32) | 42 (36–70) | 61 (21–65) | 41 (20–59)* |
| ERA | 31 (21–55) | 8 (0–15)* | 22 (12–50) | 5 (0–35)* | 49 (21–64) | 8 (0–51) |
| PSA | 30 (17–45) | 6 (1–18)* | 18 (3–33) | 8 (3–24) | 26 (9–55) | 9 (2–32)* |
| Undifferentiated | 22 (11–43) | 8 (1–24)* | 16 (2–28) | 8 (1–34) | 21 (1–66) | 10 (1–26)* |
Values are given as median (IQR). *Improvement at 1 year statistically significant at P < 0.05. ERA: enthesitis related arthritis.
Table 3.
Disability (measured using CHAQ score) at first presentation and at 1 year in children with JIA
| CHAQ at first presentation |
CHAQ at 1 year |
|||
|---|---|---|---|---|
| JIA ILAR subtype | Median (IQR) | Percentage with CHAQ ⩾0.75 | Median (IQR) | Percentage with CHAQ ⩾0.75 |
| Whole cohort | 0.63 (0.13–1.38) | 50 | 0.25 (0–1.0)* | 32 |
| Systemic arthritis | 0.94 (0.25–2.0) | 54 | 0.5 (0.06–1.5) | 47 |
| Persistent oligoarthritis | 0.63 (0.13–1.13) | 46 | 0.13 (0–0.75)* | 27 |
| Extended oligoarthritis | 0.56 (0.38–1.5) | 45 | 0.56 (0.06–1.19) | 42 |
| RF(−) polyarthritis | 1.25 (0.38–1.88) | 65 | 0.38 (0.13–1.5)* | 40 |
| RF(+) polyarthritis | 1.13 (0.5–1.5) | 64 | 0.56 (0.13–1.13)* | 40 |
| ERA | 0.5 (0.06–1.19) | 44 | 0.13 (0–0.5)* | 24 |
| PSA | 0.38 (0.13–1.0) | 40 | 0.13 (0–1.0) | 30 |
| Undifferentiated | 0.38 (0–1.13) | 36 | 0.19 (0–1.19) | 35 |
*Improvement at 1 year statistically significant at P < 0.05. ERA: enthesitis related arthritis.
After 1 year of follow-up, all subtypes of JIA had experienced improvements in scores (Tables 2 and 3). The median active and limited joint count at 1 year was 0 (IQR 0–1). The median ESR had fallen to 9 (IQR 4–20) and the median pain score had decreased to 9 (IQR 1–32). CHAQ scores had also improved with a median CHAQ score of 0.25 (IQR 0.00–1.00) at 1 year. Twenty-six per cent had a CHAQ score of 0 at 1 year. The one exception was a deterioration in the PGE in children with RF(+) polyarthritis, although this did not reach statistical significance. Of those presenting with oligoarthritis in the first 6 months (n = 353), 16 (5%) children had evolved to the extended subtype at 1 year. Although small numbers prevent robust estimates, there were no significant differences in age, gender, active or limited joint counts or ESR at first presentation between those children with persistent oligoarthritis and those who extended.
Over the course of the first year following presentation, 85% of children received treatment with NSAIDs (Table 4), 70% of children had received an IA steroid injection, with a median of one injected joints/child (range 1–35) and 47% had started on MTX. Approximately half of the children had received their first dose of MTX within 6 months of disease onset [n = 169 (48%)]. Eighty-seven per cent of children had received their first dose of MTX within 6 months of first presentation to a paediatric rheumatologist and 57% within the first month following presentation. Seven per cent of children had already received biologic therapy before the end of the first year.
Table 4.
Details of anti-rheumatic therapies received in first year following presentation
| ILAR | NSAID | Systemic steroidsa | IA steroids | MTX | Biologics |
|---|---|---|---|---|---|
| Whole cohort | 632 (85) | 197 (27) | 515 (70) | 350 (47) | 55 (7) |
| Systemic arthritis | 35 (83) | 37 (88) | 11 (26) | 33 (79) | 7 (17) |
| Persistent oligoarthritis | 300 (85) | 41 (12) | 261 (74) | 65 (18) | 3 (1) |
| Extended oligoarthritis | 29 (91) | 8 (25) | 28 (88) | 24 (75) | 3 (9) |
| RF(−) polyarthritis | 128 (86) | 73 (49) | 107 (72) | 135 (91) | 23 (16) |
| RF(+) polyarthritis | 20 (87) | 12 (52) | 10 (43) | 21 (91) | 5 (22) |
| ERA | 45 (88) | 13 (25) | 32 (63) | 22 (43) | 7 (14) |
| PSA | 50 (82) | 8 (13) | 44 (72) | 38 (62) | 5 (8) |
| Undifferentiated | 25 (83) | 5 (17) | 22 (73) | 12 (40) | 2 (7) |
Values are given as n (%). aIncluded either oral or systemic steroids. ERA: enthesitis related arthritis.
CHAQ score ⩾0.75 at first presentation was significantly associated with active joint count, ESR, PGE and pain scores (Table 5). At 1 year, the proportion of children with a CHAQ score ⩾0.75 had fallen from 50 to 32%. The highest scores were again seen in children with systemic arthritis, polyarthritis [RF(+) and RF(−)] and extended oligoarthritis. The majority of children with a CHAQ score <0.75 at first presentation continued to have a CHAQ <0.75 at 1 year although 14% of children with an initial low CHAQ had a 1 year CHAQ ⩾0.75. The strongest predictor of a CHAQ score ⩾0.75 at 1 year was a CHAQ score ⩾0.75 at first presentation (OR 3.92; 95% CI 2.17, 7.09). In addition, higher CHAQ scores at 1 year were less common in boys (OR 0.62; 95% CI 0.37, 1.03) and more common in those with higher PGE at baseline (OR 1.16 per 10-mm VAS; 95% CI 1.01, 1.32). Other factors, including symptom duration at first presentation, ESR, pain scores and PGA were not independently associated with CHAQ ⩾0.75 at 1 year.
Table 5.
Predictors of CHAQ score ≥0.75 at presentation and at 1 yeara
| Factors associated with CHAQ ≥0.75 at first presentation |
Factors associated with CHAQ ≥0.75 at 1 year |
|||||
|---|---|---|---|---|---|---|
| Measure at first presentation | Univariate analysis OR (95% CI) | Multivariate analysis OR (95% CI) | Multivariate analysis OR (95% CI) (imputed data) | Univariate analysis OR (95% CI) | Multivariate analysis OR (95% CI) | Multivariate analysis OR (95% CI) (imputed data) |
| Age at presentation (per year) | 0.98 (0.94, 1.02) | 0.92 (0.86, 0.99) | 0.92 (0.87, 0.98) | 0.99 (0.95, 1.04) | 1.02 (0.94, 1.10) | 1.00 (0.95, 1.05) |
| Male | 1.00 (0.69, 1.45) | 1.29 (0.67, 2.47) | 1.03 (0.64, 1.63) | 0.74 (0.5, 1.09) | 0.59 (0.30, 1.18) | 0.62 (0.37, 1.03) |
| Delay to presentation (per month) | 1.00 (0.99, 1.01) | 1.00 (0.98, 1.02) | 0.99 (0.98, 1.01) | 1.01 (0.99, 1.02) | 1.00 (0.99, 1.02) | 1.01 (0.99, 1.02) |
| Active joint count (per joint) | 1.08 (1.04, 1.12) | 1.09 (1.03, 1.14) | 1.08 (1.04, 1.12) | 1.03 (1.01, 1.05) | 1.02 (0.98, 1.05) | 1.00 (0.97, 1.02) |
| CHAQ ≥0.75 | 5.61 (3.41, 9.23) | 4.81 (2.09, 11.07) | 3.92 (2.17, 7.09) | |||
| ESR (per 10 mm/h) | 1.18 (1.09, 1.27) | 1.14 (1.02, 1.27) | 1.09 (0.99, 1.21) | 1.08 (1.01,1.16) | 1.03 (0.93, 1.14) | 1.01 (0.93, 1.10) |
| PGA (per 10 mm) | 1.17 (1.08, 1.27) | 0.98 (0.85, 1.12) | 0.97 (0.87, 1.09) | 1.16 (1.06,1.26) | 0.93 (0.80, 1.08) | 1.06 (0.95, 1.18) |
| PGE (per 10 mm) | 1.73 (1.55, 1.93) | 1.46 (1.24, 1.72) | 1.38 (1.21, 1.56) | 1.32 (1.21, 1.45) | 1.14 (0.97,1.34) | 1.16 (1.01, 1.32) |
| Pain score (per 10 mm) | 1.60 (1.46, 1.74) | 1.40 (1.22, 1.60) | 1.40 (1.25, 1.56) | 1.25 (1.15, 1.35) | 1.01 (0.86,1.17) | 1.00 (0.90, 1.12) |
aResults in bold indicate statistically significant results at P < 0.05.
Discussion
This study represents the largest prospective report of early outcomes in a modern inception cohort of children presenting to paediatric rheumatology with inflammatory arthritis. In addition, the results are not limited to a single centre or rheumatologist, but represent the current outcomes at five of the largest paediatric rheumatology centres in the UK, which practise within the guidelines as set out by the British Society for Paediatric and Adolescent Rheumatology (BSPAR) consensus document on the standards of care for children and young people with JIA (http://www.bspar.org.uk/downloads/clinical_guidelines/Standards_of_Care.pdf).
Over 50% of children presented with oligoarthritis and a significant proportion of children were found to have no active or limited joints at the 1 year assessment. However, even in this era of modern therapies, there still remained a subgroup of children with persistently active disease. Not surprisingly, the strongest predictor of disability at 1 year was the level of disability at the first presentation, which likely encompasses many other features of the disease, including active joint counts and pain. High levels of disability at first presentation have also been shown to be a strong predictor of future disability in studies of adults with RA [20].
In our study, we found an association between higher levels of disability among girls at 1 year, which is consistent with earlier reports [21, 22]. Oen et al. [23] specifically looked at predictors of CHAQ score ⩾0.75 after a mean of 12 years of disease in her retrospective cohort of children with JRA. Although specific details of disease activity at disease presentation were not available, there was also a trend towards less disability, albeit at a much later time point in disease, in males. The reasons why females should do worse than males is not clear. However, an over-representation of females in certain subgroups, particularly RF(+) polyarthritis, which often has a more severe course, may explain part of the association.
Few previous studies have specifically looked at the early course of the disease in children with inflammatory arthritis and fewer still have specifically classified children according to the ILAR JIA subtypes, making direct comparisons of our results difficult. A retrospective study by Bowyer et al. [24] described outcomes at 1 and 5 years in children with JRA presenting between 1992 and 1997 and found that the vast majority had milder levels of disability at the end of the first year (defined as Steinbrocker Class I or II). However, children with SpAs and/or psoriasis were specifically excluded. In our study, 24% of the children with enthesitis related arthritis (ERA) and 30% of the children with PSA had significant disability (CHAQ ⩾0.75) at 1 year.
The results of our study are similar to those found in a single-centre inception cohort of 197 children with JRA or juvenile SpA in Norway [25], which also found that CHAQ score in the first 6 months of the disease was the strongest predictor of disability, measured using CHAQ, at 3 years. Similarly, they also found that the parent's global assessment of the child's well-being was a predictor of CHAQ at 3 years, suggesting there are other important aspects of the child's arthritis observed by the parent but independent of the physician, which are important in determining functional outcome.
It is difficult to know at this time point specifically what role the DMARDs and other anti-rheumatic therapies played in the improvement of CHAQ scores in these children and how much was the natural variability within the disease. An Italian study of 227 children with JIA found that patterns of disability fluctuated between states of mild, moderate and severe disability in 40% of the children measured over a median of 3 years [26]. One-quarter of the children demonstrated a continuous improvement in disability over this same period and a further one-quarter demonstrated persistently stable low disability levels. Further analyses of the CAPS cohort will also confirm whether or not early treatment with DMARDs significantly improves longer term outcome. In this study, the biggest determinant in how long after the disease onset MTX was started was the time taken to first paediatric rheumatology assessment, as the majority of children who did start MTX did so soon after this first appointment. However, at this stage, delay to first presentation was not found to be a predictor of high CHAQ at 1 year. Continued follow-up will determine whether delay to presentation influences longer term outcomes.
A possible limitation to our study may have been the impact of missing data. In our study, the two variables with the most missing data at baseline included the ESR (23% missing) and the CHAQ score (30% missing). As per ethical approval, blood tests could only be taken as part of routine clinical practice and therefore, if an ESR had not been performed, this value would not be available. Although most centres now collect CHAQ as part of routine clinical care, this was not always the case over the study period. In addition, for some families, due to circumstances at the time of first presentation, parents may have been unable to complete these forms at the first visit. However, despite this missing data, all children had available information for multiple imputations. To confirm the validity of our multiple imputations, we also ran regression models in those with complete data only. This analysis also confirmed the significant association with CHAQ ⩾0.75 at baseline and calculated similar point estimates for PGE and gender, albeit with wider CIs, likely due to the smaller sample size.
We specifically chose not to include the JIA subtype as a predictor of disability at 1 year in our multivariable model. Although it was clear from looking at crude results that certain subtypes had a more severe course over the first year, there is likely to be much variability within each subgroup. The common factor that linked all of these subgroups to outcome was disease severity at first presentation. As many children may present with persistent inflammatory arthritis and not fit into a specific ILAR category, instead being classified as ‘Undifferentiated’, we felt it important to include other easily measurable factors, such as joint counts, pain score, disability and ESR that are common to all children presenting with inflammatory arthritis. With time, it may be more sensible to include these subtypes into further predictive models. In addition, there may be certain characteristics within each subtype which may predict a worse disease course, such as ANA or HLA-B27 status. For example, 33 of the 51 children with ERA had HLA-B27 test results, of which 64% were positive.
Conclusions
This analysis has shown that even within a short 1-year period following presentation with inflammatory arthritis, the majority of children will have a significant improvement in pain, joint inflammation and disability, with many children having no active or limited joints. However, after 1 year, one-third of the children continued to have moderate to severe levels of disability, despite treatment with IA steroid injections or DMARDs. These higher levels of disability were predicted by higher levels of CHAQ at baseline, higher PGEs and female gender. Further follow-up of this cohort will continue to explore the longer term outcomes in these children and confirm whether these same predictors (measured at first presentation) or other factors, such as any delay to treatment, will predict outcome of disability at later stages of the disease.
Acknowledgements
The authors would like to thank the CAPS specialist rheumatology nurses (Carol Lydon, Sharon Bradshaw, Joanne Buckley, Julie Jones, Jane Sims, Alexandra Meijer, Vicki Price and Mick Eltringham) who collected the data; Peter Ward for coordinating the study; Mark Lay for running the database; and Prof. Alan Silman, Medical Director of the ARC, for his help in establishing the study.
Funding: This work was supported by an Arthritis Research Campaign programme grant, #17552. Funding to pay the Open Access publication charges for this article was provided by the ARC.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1.Symmons DP, Jones M, Osborne J, Sills J, Southwood TR, Woo P. Pediatric rheumatology in the United Kingdom: data from the British Pediatric Rheumatology Group National Diagnostic Register. J Rheumatol. 1996;23:1975–80. [PubMed] [Google Scholar]
- 2.Oen K, Malleson PN, Cabral DA, Rosenberg AM, Petty RE, Cheang M. Disease course and outcome of juvenile rheumatoid arthritis in a multicenter cohort. J Rheumatol. 2002;29:1989–99. [PubMed] [Google Scholar]
- 3.Hashkes PJ, Laxer RM. Medical treatment of juvenile idiopathic arthritis. J Am Med Assoc. 2005;294:1671–84. doi: 10.1001/jama.294.13.1671. [DOI] [PubMed] [Google Scholar]
- 4.Foster HE, Marshall N, Myers A, Dunkley P, Griffiths ID. Outcome in adults with juvenile idiopathic arthritis: a quality of life study. Arthritis Rheum. 2003;48:767–75. doi: 10.1002/art.10863. [DOI] [PubMed] [Google Scholar]
- 5.Packham JC, Hall MA. Long-term follow-up of 246 adults with juvenile idiopathic arthritis: functional outcome. Rheumatology. 2002;41:1428–35. doi: 10.1093/rheumatology/41.12.1428. [DOI] [PubMed] [Google Scholar]
- 6.Packham JC, Hall MA. Long-term follow-up of 246 adults with juvenile idiopathic arthritis: education and employment. Rheumatology. 2002;41:1436–9. doi: 10.1093/rheumatology/41.12.1436. [DOI] [PubMed] [Google Scholar]
- 7.Packham JC, Hall MA. Long-term follow-up of 246 adults with juvenile idiopathic arthritis: social function, relationships and sexual activity. Rheumatology. 2002;41:1440–3. doi: 10.1093/rheumatology/41.12.1440. [DOI] [PubMed] [Google Scholar]
- 8.Cassidy JT, Levinson JE, Bass JC, et al. A study of classification criteria for a diagnosis of juvenile rheumatoid arthritis. Arthritis Rheum. 1986;29:274–81. doi: 10.1002/art.1780290216. [DOI] [PubMed] [Google Scholar]
- 9.European League Against Rheumatism. EULAR Bulletin No. 4: nomenclature and classification of arthritis in children. Basel: National Zeitung AG; 1977. [Google Scholar]
- 10.Fink CW. Proposal for the development of classification criteria for idiopathic arthritides of childhood. J Rheumatol. 1995;22:1566–9. [PubMed] [Google Scholar]
- 11.Petty RE, Southwood TR, Baum J, et al. Revision of the proposed classification criteria for juvenile idiopathic arthritis: Durban, 1997. J Rheumatol. 1998;25:1991–4. [PubMed] [Google Scholar]
- 12.Petty RE, Southwood TR, Manners P, et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31:390–2. [PubMed] [Google Scholar]
- 13.Adib N, Hyrich K, Thornton J, et al. Association between duration of symptoms and severity of disease at first presentation to paediatric rheumatology: results from the Childhood Arthritis Prospective Study. Rheumatology. 2008;47:991–5. doi: 10.1093/rheumatology/ken085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nugent J, Ruperto N, Grainger J, et al. The British version of the Childhood Health Assessment Questionnaire (CHAQ) and the Child Health Questionnaire (CHQ) Clin Exp Rheumatol. 2001;19(Suppl. 23):S163–7. [PubMed] [Google Scholar]
- 15.Giannini EH, Ruperto N, Ravelli A, Lovell DJ, Felson DT, Martini A. Preliminary definition of improvement in juvenile arthritis. Arthritis Rheum. 1997;40:1202–9. doi: 10.1002/1529-0131(199707)40:7<1202::AID-ART3>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 16.Dempster H, Porepa M, Young N, Feldman BM. The clinical meaning of functional outcome scores in children with juvenile arthritis. Arthritis Rheum. 2001;44:1768–74. doi: 10.1002/1529-0131(200108)44:8<1768::AID-ART312>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 17.Spiegel LR, Schneider R, Lang BA, et al. Early predictors of poor functional outcome in systemic-onset juvenile rheumatoid arthritis: a multicenter cohort study. Arthritis Rheum. 2000;43:2402–9. doi: 10.1002/1529-0131(200011)43:11<2402::AID-ANR5>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 18.van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18:681–94. doi: 10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 19.Royston P. Multiple imputation of missing values: update. Stata J. 2005;5:188–201. [Google Scholar]
- 20.Wiles NJ, Dunn G, Barrett EM, Harrison BJ, Silman AJ, Symmons DP. One year follow up variables predict disability 5 years after presentation with inflammatory polyarthritis with greater accuracy than at baseline. J Rheumatol. 2000;27:2360–6. [PubMed] [Google Scholar]
- 21.Gare BA, Fasth A. The natural history of juvenile chronic arthritis: a population based cohort study. II. Outcome. J Rheumatol. 1995;22:308–19. [PubMed] [Google Scholar]
- 22.Flato B, Lien G, Smerdel A, et al. Prognostic factors in juvenile rheumatoid arthritis: a case-control study revealing early predictors and outcome after 14.9 years. J Rheumatol. 2003;30:386–93. [PubMed] [Google Scholar]
- 23.Oen K, Malleson PN, Cabral DA, et al. Early predictors of longterm outcome in patients with juvenile rheumatoid arthritis: subset-specific correlations. J Rheumatol. 2003;30:585–93. [PubMed] [Google Scholar]
- 24.Bowyer SL, Roettcher PA, Higgins GC, et al. Health status of patients with juvenile rheumatoid arthritis at 1 and 5 years after diagnosis. J Rheumatol. 2003;30:394–400. [PubMed] [Google Scholar]
- 25.Selvaag AM, Lien G, Sorskaar D, Vinje O, Forre O, Flato B. Early disease course and predictors of disability in juvenile rheumatoid arthritis and juvenile spondyloarthropathy: a 3 year prospective study. J Rheumatol. 2005;32:1122–30. [PubMed] [Google Scholar]
- 26.Magni-Manzoni S, Pistorio A, Labo E, et al. A longitudinal analysis of physical functional disability over the course of juvenile idiopathic arthritis. Ann Rheum Dis. 2008;67:1159–64. doi: 10.1136/ard.2007.078121. [DOI] [PubMed] [Google Scholar]


