Abstract
Objective
To assess HIV/AIDS-related stigma and discrimination of people living with HIV/AIDS (PLWHA) in Kumasi, Ghana.
Methods
A cross-sectional survey of 104 adults from the four sub-districts in Kumasi was conducted.
Results
Four stigma constructs, employment-based discrimination, screening and identification of HIV positive people, revelation of HIV status and social contact stigma were determined based on reliability measures from responses to the questionnaire. Regression analysis showed that participants with higher educational attainment were more likely to favor policies denying employment to PLWHA (p<0.05), but disapproved of revealing HIV sero-status (p<0.05). Muslims were more likely than Christians to agree with identifying PLWHA (p<0.05) and more likely to advocate revealing HIV sero-status (p<0.05). Males were more likely to favor revealing HIV status (p<0.05). Employed persons were more likely to have social contact with PLWHA (p<0.05).
Conclusions
These findings are useful in guiding the design of interventions against HIV/AIDS-related stigma in Kumasi.
Keywords: HIV/AIDS, stigma, discrimination, community members, Ghana
Introduction
In 2005, an estimated 24.5 million people were living with HIV/AIDS in Sub-Saharan Africa (UNAIDS 2006), and 75% of all deaths since the beginning of the HIV/AIDS pandemic has occurred in this region. Currently, 320,000 Ghanaians are estimated to be living with HIV/AIDS (UNAIDS 2007) and 30,000 Ghanaians have died from AIDS (CIA 2005). The HIV prevalence rate in Ghana is 2.3% and HIV prevention and treatment programs have been established to combat the AIDS epidemic. However, reports from the United Nations Integrated Regional Information Networks (IRIN) on Africa indicate that the Ghanaian government’s AIDS program is in danger of failure due primarily to stigma and a failing health system (IRIN 2005). Identifying the predictors of stigma and designing effective interventions may be key to ensuring successful HIV/AIDS prevention and treatment programs, and thus, successful reversal of the AIDS epidemic. The purpose of our research was to determine the predictors of HIV/AIDS related stigma and discrimination, and to identify the perceptions of community members towards HIV/AIDS and persons living with HIV/AIDS (PLWHA) in Ghana. The paper provides insight on the factors influencing the perceptions of community members towards PLWHA.
Goffman (1963) defines stigma as a “mark” that links a person to undesirable characteristics (label) (Goffman 1963). HIV/AIDS related stigma has been a negative factor in the crusade to diminish the prevalence and effect of the HIV/AIDS pandemic. From the inception of AIDS, people have advocated extensive measures including quarantine of HIV infected people in order to protect the populace from the infection. Discrimination has often been rampant. Ostracism, isolation, and rejection have been common place in the lives of people identified to have AIDS (Carr and Gramling 2004). HIV/AIDS related stigma can range from a simple gossip to outright discrimination, resulting in job loss, house evictions, rejection, isolation and even killing of an HIV infected person. It can stem from legislative, and employment policies, hospital policies, cultural beliefs, or individual behaviors, thoughts, and attitudes (Standing 1992, Zwi 1993, Aggleton 1996). HIV/AIDS related stigma and discrimination have been linked to misconceptions about the disease, fear of the disease due to its manifestations and fatality, and to the association of HIV/AIDS with stigmatized/marginalized individuals in the community (Herek and Glunt 1988, Alonzo and Reynolds 1995, Boer and Emons 2004).
Since the beginning of the epidemic, much progress has been made in preventing new HIV infections and in delaying progression of the disease. However, very little has been done to halt the effect of stigma (Piot 2006). In 1988, a panel convened by the Institute of Medicine concluded that “the fear of discrimination is a major constraint to the wide acceptance of many potentially effective public health measures” (Herek and Glunt 1988). Now, twenty-five years after the start of the epidemic, the stigma of AIDS is still a hindrance in the fight against the disease. The stigma of AIDS, unswervingly hampers the effective AIDS response, deters people from knowing their HIV status, prevents high risk individuals from receiving needed services, prevents condom use, and creates non-compliance with breastfeeding recommendations for HIV positive mothers (WHO/UNAIDS 2004). Halting the epidemic will involve changing the perceptions of individuals in the community towards HIV and PLWHA.
In Ghana and many countries of sub-Saharan Africa, HIV transmission occurs primarily through heterosexual intercourse. In these countries, HIV/AIDS is widely viewed as a consequence of sexual immorality or immoral behaviors, thus, infected individuals are considered responsible for acquiring the disease. In some cases, the infection is perceived as a punishment given by God to perpetuators of sins like prostitution, promiscuity, drug use, or homosexuality (Kaldjian, et al. 1998, Ayranci 2005). Ghanaians are very religious and moral people and have a value system to which they adhere (Awusabo-Asare et al. 2004). They believe an individual should abstain from sex until marriage and that those who acquire HIV/AIDS through commercial sex work or promiscuity bring disgrace to their families. In Ghana, HIV/AIDS is believed to have emerged from individuals who engaged or solicited commercial sex workers (prostitutes) from Cote d’Ivoire (Yeboah-Afari 1988, Decosas 1995). HIV/AIDS is also blamed on foreigners, gay men and the Devil (Prince, 2004). Thus, people who have HIV/AIDS are blamed for the disease. The stigma related to sexual immorality due to cultural values against prostitution, promiscuity and homosexuality coupled with the fear of HIV/AIDS (due to misconception and fatality of AIDS) may be the source of HIV/AIDS stigma in Ghana (Ankomah 1998, Mill 2003, Prince, 2004). For example, commercial sex workers have been stigmatized and frequently harassed and humiliated by law enforcement agents (WiLDAF 2006).
Although there are homosexuals in Ghana (Known MSM Sites, 2008), the only form of sexual transmission of HIV that working documents of Ghana on HIV/AIDS recognize is heterosexual transmission (Republic of Ghana, 2000; Ghana AIDS Commission, 2000, National AIDS/STI Control Programme, 2001). International documents report nothing on HIV transmission by homosexual or bisexual groups in Ghana (UNAIDS, UNICEF, WHO 2002 Update; UNAIDS 2006). The Criminal Code of 1960 (Act 29) of Ghana, makes “sexual intercourse with a person in an unnatural manner” a crime (Attipoe, 2008). Although the act does not define what “Sexual intercourse in an unnatural manner” means, persons suspected of homosexuality are swiftly punished and incarcerated by law officials (Prince, 2004). Homosexuals (men who have sex with men; MSM) are also harassed, called evil, evicted from their homes and even beaten by members of the community (Prince, 2004). Drug use does not seem to play a major role among MSM in the Ghana Metropolis. Only 2% of MSM reported using methamphetamines or inhaling nitrates (Influencing Factors, 2008). Although a paper on HIV prevention among injecting drug users in developing and transitional countries list Ghana as one of these countries, no data was reported for Ghana and the source of the information was given as unpublished data from WHO, UNAIDS (Ball et al, 1998).
In Ghana, family members are considered ultimately responsible for the behavior of each household member and the family is blamed or praised for the behavior of its members (Hintz 1987). An individual is linked to a long chain of living and deceased members in his or her family and in his or her town or village (Hintz 1987). Thus, family members of a person who dies of or lives with HIV/AIDS are also stigmatized. Family members may encourage relatives with HIV/AIDS to remain silent about their HIV status to prevent gossip, social rejection and HIV related stigma. In some cases, family members isolate relatives with HIV to minimize social contact and/or prevent infection. Identifying the perception of family members towards HIV and family members with HIV/AIDS will be important in designing stigma averting interventions and educational programs for family members.
At the community level, the fear of stigma can lead to the refusal of voluntary counseling and testing (VCT) for HIV, increased gender-based violence, and marginalization of high risk individuals (Heyward, et al. 1993). Community members may not seek VCT because of the fear of discovering that they are HIV positive and fear of the resulting stigma and discrimination that may accompany their HIV/AIDS positive status. Thus, HIV/AIDS related stigma and discrimination may have a profound impact on the disclosure (revelation) of HIV status and the subsequent care, support, or treatment that HIV positive persons receive (Moneyham, et al. 1996, Muyinda, et al. 1997, Weiss and Ramakrishna 2001, Mill 2003, Carr and Gramling 2004, Reynolds, et al. 2004). In Ghana, HIV positive persons hide their HIV-seropositive status to reduce HIV/AIDS related stigma and discrimination and to retain the care and support of family members. Ironically, this secrecy hinders uptake of treatment and of support services that can be provided by family members (Mill 2003). People who feel stigmatized or discriminated against are more likely to have poor health outcomes, socio-psychological problems, and suicidal thoughts (Sowell, et al. 1996, Reynolds, et al. 2004, Bottonari, et al. 2005, Katz and Nevid 2005, Sledjeski, et al. 2005). Tackling HIV stigma will involve tackling perceptions and values towards sexuality and HIV/AIDS.
Few studies on AIDS stigma among family and community members have been conducted in Ghana. One study conducted by Mill (2003) explored the experience of HIV-seropositive women receiving care in Accra and Agomanya (Mill 2003). It reported that many HIV positive women felt the need to hide their HIV status due to the perceived shame and disgrace surrounding the HIV infection. HIV counselors also reinforced maintaining secrecy as a strategy to reduce stigma (Mill 2003). Another study was an in-depth interview with health care workers in the Cape Coast municipality in Ghana (Awusabo-Asare and Marfo 1997). It revealed that there was general fear of infection among health care workers that resulted from inadequate supply of basic protective items and insufficient information on the sero-status of some patients (Awusabo-Asare and Marfo 1997). Refusal to treat PLWHA, refusal to work in HIV/AIDS facilities, maltreatment of PLWHA, and inequality in treatment between HIV/AIDS infected and uninfected patients were forms of HIV/AIDS-related discrimination shown by health care professionals in health care facilities (Awusabo-Asare and Marfo 1997). A more recent study examined the effect of HIV stigma on caregivers of PLWHA in Accra. This study observed that caregivers also experienced widespread stigma and discrimination that were exhibited in negative attitudes from close neighbors, relatives, and health care workers (Mwinituo and Mill 2006). As a result, caregivers of PLWHA in the study, secretly offered care in order to minimize disrespect and isolation (Mwinituo and Mill 2006). In this study, we examined the predictors of stigma and the perception (knowledge, attitudes, and behaviors) of community members towards PLWHA.
Methods
Study setting
The study was conducted in Kumasi, the capital and cultural center of the Ashanti Region of Ghana. Kumasi is located in the south-central part of the country with a population of about 2.5 million. Sixty-three percent of the people are Christians; 16% are Muslims, and 21% practice indigenous beliefs (CIA 2005). While a majority of Ghanaians have heard about HIV/AIDS (Ghana Statistical Service (GSS) and ORC Macro 2004), available evidence (WHO/UNAIDS 2004) shows that very few have comprehensive knowledge of the disease. While the rich cultural and religious heritage of Kumasi makes it a prime candidate for AIDS-related stigma research, no previous studies have been conducted to elucidate the nature and correlates of AIDS stigma in the city.
Target population, informed consent and sample size calculation
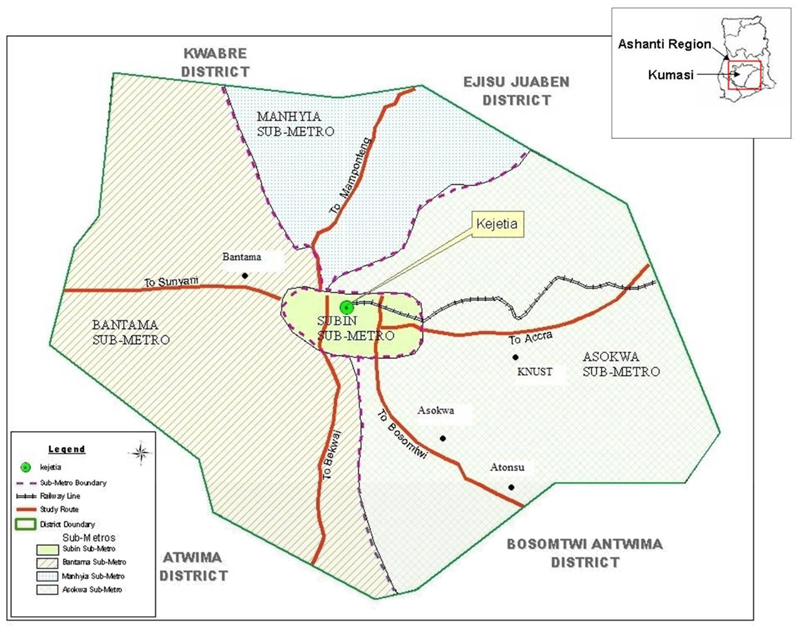
A random sample of adults was recruited from representative settings in the Kumasi Region. Participants were from the 4 sub-districts or sub-metros of the Kumasi Metropolitan Assembly (Subin, Asokwa, Bantama and Manhyia: Figure 1). During recruitment, the purpose of the study was explained to potential participants and their voluntary participation was sought. Potential participants were informed that if they chose not to participate, they would not lose any benefits from the Ministry of Health or their other local health providers, and they could withdraw from the study at any time if they chose to do so. Thus, participation in the study was voluntary and no incentives were provided. Participants were assured of confidentiality, and only study identification numbers were used on the questionnaires. Ethical approval for the study was obtained from the Institutional Review Board (IRB) of the University of Alabama at Birmingham, and the Ethics Committee of the Ghana Health Service. Based on previous research on stigma and discrimination against PLWHA in Africa (Wade, et al. 2006), we hypothesized that at least 50% of the adult population of Kumasi would express some form of stigmatization attitude against PLWHA and that at best this figure would be 40%. Thus, with an adult population of about 768,000 (Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat, 2005) and assuming a power of 80% at 95% confidence interval (CI), we determined the sample size for the study to be 83. We used EPI-Info 2000 (CDC, Atlanta, GA, USA) for this calculation. To account for non-responses, an additional 25% was added to the sample for a total sample size of 104.
Figure 1.
Map of the Kumasi Metropolitan area and sub-metros (Subin, Asokwa, Bantama and Manhyia) where the study was conducted.
Study instrument
The 43-item questionnaire was developed by UAB investigators based on a comprehensive literature review (Ehiri et al. 2005) and validated through a series of reviews by our Ghanaian collaborators at AIDS Ally and a network of other non-governmental organizations (NGOs) working with HIV patients in Kumasi. It was further tested by means of a small pilot of 10 randomly selected adults in Kumasi who were not included in the main study. The questionnaire included items related to demographic information (age, gender, educational level, and marital status), knowledge of HIV pathology, symptoms, prevention and care strategies, transmission of HIV and perceptions and behaviors regarding HIV/AIDS. A separate set of questions regarding perception, support, and revelation of HIV status was included for family members of PLWHA.
Data analysis
Analysis of quantitative data was conducted using SAS statistical program version 9.1. We generated descriptive statistics (frequencies and percentages) and tested for differences using Chi-square statistics. Descriptive statistics were used in presentation of the demographic characteristics in tabular form. Exploratory factor analysis was used to group questions related to perception and beliefs about HIV and PLWHA. The SCREE test with VARIMAX rotation was used to retain the meaningful factors using item loadings greater than 0.4 as the qualifying criterion for retention. Four constructs (factors) of stigma, namely, employment-based discrimination, screening and identification of HIV positive people, revelation of HIV status and social contact/interaction stigma were identified. Confirmatory factor analysis was used to confirm the various stigma factors using Cronbach alpha as a measure of reliability of the constructs. A Cronbach alpha of 0.70 is considered acceptable in the natural sciences (Nunnally, 1979) but Cronbach alphas of less than 0.60 have been noted in the social sciences (Hatcher, 1994). A p-value of at least 0.05 was used to indicate significant differences that were not due to chance. Structural equation modeling and ordinary least squares (OLS) regression were conducted to evaluate the factors influencing the stigma constructs.
Results
Sample characteristics
A summary of the socio-demographic characteristics of the participants is provided in Table 1. Majority of the participants were less than 30 years of age (61%), had less than a senior secondary school education (59%), and were Christians (80%). Only 13% of these participants had been tested for HIV/AIDS. Twelve percent (12%) of participants were family members and approximately 35% knew at least one person who was living with or who had died from HIV/AIDS.
Table 1.
Sociodemographic characteristics of the study population, Kumasi, Ghana.(N=104)
| Variable | Number* | Percent |
|---|---|---|
| Age | ||
| <30 years | 63 | (60.6) |
| >=30 years | 38 | (36.5) |
| Education | ||
| < Senior Secondary | 61 | (58.7) |
| ≥ Senior Secondary | 37 | (35.6) |
| Gender | ||
| Female | 49 | (47.1) |
| Male | 55 | (52.9) |
| Marital status | ||
| Single | 62 | (59.6) |
| Married | 42 | (40.4) |
| Religious affiliation | ||
| Christian | 83 | (79.8) |
| Muslim | 21 | (20.2) |
| Employment status | ||
| Not Employed | 51 | (49.0) |
| Employed | 50 | (48.1) |
| Income (in Cedis) | ||
| < 500,000 | 46 | (44.2) |
| ≥ 500,000 | 37 | (35.6) |
| Tested for HIV | ||
| Yes | 13 | (12.5) |
| No | 89 | (85.6) |
| Number HIV positive | ||
| persons known | ||
| 0 | 68 | (65.4) |
| 1–5 | 25 | (24.0) |
| >5 | 11 | (10.6) |
| Relationship to PLWHA | ||
| Family member | 12 | (11.5) |
| Community Member | 92 | (88.5) |
Numbers may not always add up to 104 because of missing responses
Knowledge of HIV/AIDS and PLWHA
Of the 104 respondents, 59% did not know why HIV makes people sick, and 67% could not correctly name or write two symptoms or opportunistic infections associated with HIV/AIDS (Table 2). Ninety-seven percent of participants had average to good knowledge of HIV transmission. However, only 39% had a good knowledge of care and support strategies for PLWHA.
Table 2.
Study participants knowledge of HIV pathology, symptoms, transmission, and care for PLWHA, Kumasi, Ghana, 2004
| Number | Percent | |
|---|---|---|
| Variable | (N =104) | (%) |
| Knowledge of HIV pathology | ||
| Good | 18 | (17.3) |
| Average | 22 | (21.2) |
| Poor | 61 | (58.7) |
| No response | 3 | (2.9) |
| Knowledge of HIV/AIDS symptoms or opportunistic infections | ||
| Good | 9 | (8.7) |
| Average | 21 | (20.2) |
| Poor | 70 | (67.3) |
| No response | 4 | (3.8) |
| Knowledge of HIV transmission | ||
| Good | 48 | (46.2) |
| Average | 50 | (48.1) |
| Poor | 3 | (2.9) |
| No response | 3 | (2.9) |
| Knowledge of HIV/AIDS care and support | ||
| Good | 40 | (38.5) |
| Poor | 47 | (45.2) |
| No response | 17 | (16.3) |
Good= >70% accurate responses; Average= 50–70% accurate responses; Poor: <50% accurate responses
Attitudes and behaviors of study participants towards PLWHA
A summary of the attitudes and behaviors of the study participants towards PLWHA is presented in Table 3. Majority of the respondents agreed that PLWHA must be treated fairly (89%), be provided with free healthcare or medications (87%), and be treated with compassion (92%). Regarding the treatment of children of PLWHA, 23% indicated that children of PLWHA should be treated differently from other children because they have HIV/AIDS in their family. Fourteen percent indicated that PLWHA should not be allowed to participate in team sports, and 36% indicated that they would not let their child(ren) play with a child with HIV. In addition, 59% of participants agreed that PLWHA should inform other people of their HIV/AIDS status, 28% agreed that PLWHA should be isolated in certain villages or towns. Twelve percent of participants indicated that they would request a job change if one of their coworkers, with whom they work closely, became HIV positive.
Table 3.
Attitudes and behaviors of study participants towards PLWHA
| Variable | Number (N = 104) |
Percent |
|---|---|---|
| PLWHA should tell others they are HIV positive | ||
| Agree | 61 | (58.7) |
| Disagree | 32 | (30.8) |
| Not sure/No response | 11 | (10.6) |
| PLWHA should be isolated to certain town/village | ||
| Agree | 29 | (27.9) |
| Disagree | 68 | (65.4) |
| Not sure/ No response | 7 | (6.7) |
| PLWHA must be treated fairly | ||
| Agree | 92 | (88.5) |
| Disagree | 3 | (2.9) |
| Not sure/ No response | 9 | (8.7) |
| PLWHA should be provided free healthcare/medication | ||
| Agree | 90 | (86.5) |
| Disagree | 8 | (7.7) |
| Not sure/ No response | 6 | (5.7) |
| PLWHA should be treated with compassion | ||
| Agree | 96 | (92.3) |
| Disagree | 3 | (2.9) |
| Not sure/ No response | 5 | (4.8) |
| Children of PLWHA should be treated differently | ||
| Agree | 24 | (23.1) |
| Disagree | 76 | (73.1) |
| Not sure/no response | 4 | (3.9) |
| PLWHA and/or their children should be neglected/avoided | ||
| Agree | 2 | (1.9) |
| Disagree | 99 | (95.2) |
| Not sure/no response | 3 | (2.9) |
| PLWHA and/or their children should be verbally abused | ||
| Agree | 5 | (4.8) |
| Disagree | 97 | (93.3) |
| Not sure/no response | 2 | (1.9) |
| PLWHA and/or their children should be physically abused | ||
| Agree | 1 | (1.0) |
| Disagree | 101 | (97.1) |
| Not sure/no response | 2 | (1.9) |
| PLWHA should be allowed to participate in team sports | ||
| Agree | 88 | (84.6) |
| Disagree | 14 | (13.5) |
| Not sure/no response | 2 | (1.9) |
| Would you request a change of job if one of your coworkers became HIV positive? | ||
| Yes | 12 | (11.5) |
| No | 89 | (85.6) |
| Not sure/no response | 3 | (2.9) |
| Would you hug or touch a person with HIV? | ||
| Yes | 92 | (88.5) |
| No | 12 | (11.5) |
| Would you provide care for an HIV/AIDS positive person? | ||
| Yes | 100 | (96.1) |
| No | 4 | (3.9) |
| Would you let your child play with an HIV/AIDS positive child? | ||
| Yes | 30 | (28.9) |
| No | 17 | (16.3) |
| Not sure/ No response | 57 | (54.8) |
PLWHA – People living with HIV and AIDS
Sociodemographic characteristics of participants according to whether they knew someone living with or someone who died from HIV/AIDS
The Chi-square analysis of demographic characteristics of study participants who knew a PLWHA or someone who had died from HIV/AIDS is provided in table 4. Participants who did not know anyone living with or who had died from HIV/AIDS were more likely to be females (58%), younger than 30 years of age (77%), single (74%), and have less than a senior secondary education (73%) (p<0.05). On the contrary, participants who knew a person living with or who had died from HIV/AIDS were more likely to be males (70%), at least 30 years old (65%), married (35%), and with greater than a secondary school education (56%) (p>0.05). There was no association between knowing someone with HIV and having been tested for HIV.
Table 4.
Sociodemographic characteristics of participants according to whether they knew someone living with or someone who died from HIV/AIDS
| Characteristics | Know someone living with or who died from HIV/AIDS |
P- value1 |
|||
|---|---|---|---|---|---|
| Yes | No | ||||
| N | (%) | N | (%) | ||
| Gender | 0.006 | ||||
| Male | 26 | (70.3) | 28 | (42.4) | |
| Female | 11 | (29.7) | 38 | (57.6) | |
| Age (in years) | <0.0001 | ||||
| <30yrs | 12 | (35.3) | 51 | (77.3) | |
| ≥30yrs | 22 | (64.7) | 15 | (22.7) | |
| Marital status | <0.0001 | ||||
| Single2 | 13 | (22.7) | 49 | (74.2) | |
| Married3 | 24 | (35.1) | 17 | (25.8) | |
| Educational status | 0.005 | ||||
| <Senior Secondary | 15 | (44.1) | 46 | (73.0) | |
| ≥Senior Secondary | 19 | (55.9) | 17 | (27.0) | |
| Religious status | 0.067 | ||||
| Christian | 26 | (70.3) | 56 | (84.8) | |
| Muslim | 11 | (29.7) | 10 | (15.2) | |
| Occupation | 0.021 | ||||
| Student/Apprentice | 10 | (28.6) | 34 | (52.3) | |
| Employed/Self employed | 20 | (57.1) | 29 | (44.6) | |
| Unemployed/Retired/Homemaker | 5 | (14.3) | 2 | (3.1) | |
| Have taken HIV test | 0.31 | ||||
| Yes | 6 | (16.2) | 7 | (10.7) | |
| No | 31 | (83.8) | 58 | (89.2) | |
| Will get HIV test | 0.33 | ||||
| Yes | 21 | (63.6) | 43 | (78.2) | |
| No | 7 | (21.2) | 7 | (12.7) | |
| Not Sure | 5 | (15.2) | 5 | (9.1) | |
| Relationship with PLWHA | <0.0001 | ||||
| None | 2 | (5.4) | 66 | (100) | |
| Community member | 23 | (62.2) | 0 | (0.0) | |
| Family member | 12 | (32.4) | 0 | (0.0) | |
Reported p-values from Chi Square tests.
Single = Never married, divorced, or widowed
Married = Married or living as married
Confirmatory factor analysis
The four factors that were found to predict stigma among family and community members (employment based discrimination, screening and identification of HIV positive status, revelation of HIV status and social contact) are presented in Table 5. The first factor “employment based discrimination” was supported by 3 questions/items to which participants were asked to respond by circling one of three choices (A=Agree, D=Disagree, NS=Not sure). The items were: (1) employment of people known to have HIV/AIDS should be terminated; (2) employment of people believed to have HIV/AIDS should be terminated; and (3) employment should be denied to individuals who test positive for HIV. The correlations for these items were, 0.91, 0.90, and 0.66, respectively. The Cronbach alpha was 0.77.
Table 5.
Factors influencing stigma constructs, coefficients and reliability
| Factors | Coefficients | Cronbach Alpha |
|---|---|---|
| Policy construct | ||
| Employment-based discrimination | 0.77 | |
| Terminate employment those having HIV/AIDS | 0.91 | |
| Terminate employment if believed to have HIV | 0.90 | |
| Deny employment those having HIV/AIDS | 0.66 | |
| Screening and identification of HIV status | 0.44 | |
| Make HIV testing mandatory before employment | 0.63 | |
| Government develop strategies to combat discrimination | 0.59 | |
| Screen and test everyone for HIV/AIDS | 0.58 | |
| Government offer free health care services to PLWHA | 0.55 | |
| Prohibit PLWHA from working in certain occupations | 0.45 | |
| Revelation of HIV status | 0.71 | |
| Reveal HIV status of a coworker to everyone | 0.74 | |
| Reveal HIV status of the coworker to the employer and | 0.73 | |
| discourage the employer from keeping the person | ||
| Reveal HIV status of the coworker to the employer and let | 0.75 | |
| the employer decide the employee’s fate | ||
| Keep quiet about HIV status of coworker because its none | 0.69 | |
| of my business | ||
| Social contact | 0.68 | |
| Kiss an HIV positive individual on the cheek | 0.70 | |
| Share the same drinking cup or plate with an HIV/AIDS positive individual | 0.71 | |
| Be a confidential friend to someone positive for HIV/AIDS | 0.58 | |
| Have dinner with someone positive for HIV/AIDS | 0.89 | |
The second factor “screening and identification of persons positive for HIV” was supported by 5 questions/items to which participants were asked to respond by selecting one of three choices (A=Agree, D=Disagree, NS=Not sure). The items were: (1) there should be mandatory HIV testing prior to employment; (2) government and businesses should develop strategies to combat discrimination against PLWHA in the work place; (3) everyone should be screened and tested for HIV; (4) government or businesses should provide health benefits and free treatments for PLWHA; and (5) HIV/AIDS patients should be prohibited from working in certain occupations such as health and food preparation. The correlation coefficients were 0.63, 0.59, 0.58, 0.55 and 0.45, respectively. The Cronbach alpha was 0.44.
The third factor “revelation of HIV status” was supported by a question/item with 4 parts using a yes/no response. The question was “If you discovered that a person that you work with directly has HIV/AIDS would you (i) inform everyone of the co-worker’s HIV/AIDS status, (ii) tell your employer and discourage him/her from keeping the person, (iii) tell your employer and let him decide whether or not to keep the person, and (iv) keep quiet. The correlations were 0.74, 0.73, 0.75, and 0.69 respectively. The Cronbach alpha was 0.71.
The fourth factor “social contact or interaction” was determined by four questions/items using a yes/no scale. The questions were: (1) would you kiss an HIV positive individual on the cheek? (2) would you share the same drinking cup or plate with an HIV positive individual? (3) would you be a confidential friend to someone positive for HIV/AIDS? and (4) would you have dinner with someone positive for HIV/AIDS? The correlations were 0.70, 0.71, 0.58, and 0.82, respectively. The Cronbach alpha was 0.68.
Structural Equation Modeling
The analysis from structural equation modeling in which the latent variables (the constructs) were the dependent variables regressed on the sociodemographic observed variables showed that “Employment-based discrimination” was fairly and adequately described by the independent variables (Table 6). The Chi-square was 12.24 (p = 0.43, degrees of freedom (df) = 12,). The model had Normal Fit Index (NFl), Goodness of Fit Index (GFI), and Adjusted Goodness of Fit Index (AGFI) of 0.97, 0.97, and 0.89, respectively. Only education explained the variance in this construct. The model showed that educated people were likely to agree to deny or terminate employment of individuals with HIV. The variation in the explanatory variable explained 11% of the variation in this stigma construct.
Table 6.
Structural equation models using ordinary least squares
| Variables | Employment – based discrimination |
Screening and identification of HIV status |
Revelation of HIV status |
Social contact/interaction |
|---|---|---|---|---|
| Age | −0.56 (−0.75) | −0.10 (−0.76) | 0.17 (−1.60) | −0.14 (−1.74)** |
| Gender | −0.96 (−1.26) | −0.13 (−1.12) | 0.20 (2.11)* | −0.13 (−1.33) |
| Marital status | −0.13 (−1.14) | 0.018 (0.19) | ||
| Education | −0.15 (2.33)* | −0.18 (−1.83)** | −0.17 (−2.06)* | −0.13 (−1.67)** |
| Religion | 0.35 (3.25)* | 0.20 (2.26)* | −0.042 (−0.052) | |
| Occupation | 0.0097 (0.12) | −0.66 (−0.54) | −0.16 (−1.62) | - |
| Employment | 0.081 (1.05) | - | 0.007 (0.083) | 0.19(2.10)* |
| Income | 0.076 (0.097) | - | 0.070 (0.82) | |
| R2 | 0.11 | 0.34 | 0.33 | 0.17 |
| Error variance | 0.26 | 0.44 | 3.03 | 0.30 |
| NFI | 0.97 | 0.92 | 0.93 | 0.95 |
| GFI | 0.97 | 0.96 | 0.94 | 0.97 |
| AGFI | 0.89 | 0.90 | 0.83 | 0.92 |
Significant at the 5 percent level;
Significant at the 10 percent level
NFI = Normal Fit Index; GFI = Goodness Fit Index; AGFI = Adjusted Goodness Fit Index
The “Screening and Identification” construct was explained by religion and education. The Chi-square was 24.01 (p= 0.68, df = 28). The NFl, GFI, and AGFI of the model were 0.92, 0.96, and 0.90, respectively. The variation in the independent variable explained 34% of the variation of this stigma construct. Non-Christians (primarily Muslims) were more in favor of screening and identification of persons with HIV. Those who were more educated were marginally opposed to HIV screening and identification.
The structural equation model for “Revelation of HIV Status” was significantly influenced by education and religion. The Chi-square was 34.23 (p = 0.62, df =23). The NFI, GFI and AGFI were 0.93, 0.94 and 0.83, respectively indicating that the model had a good fit. The independent variable explained 33 percent of the variation in the dependent variable. Those having secondary school or higher level of education were opposed to revealing HIV status while Muslims were positively inclined to favor revealing HIV status. Males were inclined to favor revelation of HIV status as opposed to females.
Only employment was significant and positive in explaining the “Social Contact/Interaction” stigma construct at the 5% level. The Chi-Square was 15.32 (p= 0.76, df = 20). The NFI, GFI and AGFI were 0.95, 0.97 and 0.92 respectively, which indicate that the model had a good fit. The independent variable explained 17% of the variation in the construct. Those who were educated and older were marginally opposed to social interaction.
Discussion
Work place discrimination remains a huge barrier for PLWHA. A study conducted by Brooks, et al. (2004), reported that 66% of unemployed PLWHA in the United States indicated that workplace discrimination along with the loss of health insurance and disability income benefits were significant barriers to returning to work (Brooks, et al. 2004). This study clearly indicates that work place discrimination exists; 12% of participants indicated that they would change jobs if someone they work with becomes positive for HIV. Unfortunately, this discriminatory behavior was more likely exhibited by people who attained a higher educational status. While this association has not been observed in other studies, we believe that the higher rate of discrimination among educated individuals may indicate that knowledge does not change behaviors.
People with lower education also exhibited some other forms of stigma. They were also more likely to favor mandatory screening and identification of HIV status, revelation of HIV status, and social distancing of people with HIV/AIDS. Non-Christians, predominately Muslims, were more likely to be in favor of mandatory screening, identification and revelation of HIV status. Policies that favor mandatory screening and testing for HIV/AIDS with the intent of identifying those positive can create avenues for further stigmatization and discrimination of PLWHA. In many cases, PLWHA perceive and/or experience further discrimination when their HIV serostatus is revealed. Yet, 59% of respondents agreed that PLWHA should tell others about their HIV seropositivity. Males were also more likely to be in favor of disclosure of HIV positive status than females. It was important to note that majority (85.6%) of respondents had not been tested for HIV/AIDS or knew their HIV serostatus, yet they supported the identification of persons with HIV with the intent to know and be safe from the virus. Many of these respondents admitted that the fear of HIV-related stigma and discrimination and fear of knowing their HIV status were the main reasons why they had not sought HIV voluntary counseling and testing.
The study also found that 29% of respondents agreed that people with HIV should be isolated in certain villages or towns. Social distancing of people with HIV/AIDS was more likely to be exhibited by people with lower educational status and those older than 30 years. Employed individuals were more likely to have social contact or interaction with people living with HIV/AIDS. It may be that employed people encountered HIV positive people on the job or during their travel to and from work. Studies have shown that men with access to resources, including those who are employed, may be more likely to have a greater number of female sexual partners and be at greater risk of HIV infection (Wilkins et al. 1991; Gregson et al. 2001). The coupling of high awareness of HIV/AIDS with low knowledge of HIV pathology, symptoms, care and support may be a huge contributing factor to the presence of HIV/AIDS stigma in the study population.
During the recruitment phase of the study, we experienced setbacks in recruiting family members of PLWHA. There was a general reluctance by PLWHA to recruit family members or to discuss their HIV/AIDS status with them. This reluctance stemmed from fear of the resulting stigma, discrimination, and loss of support from family and friends if HIV positive status is revealed. Data on family members were obtained primarily from community members who indicated that they had a family member who was living with or who had died from HIV/AIDS. Our study is limited by the small sample size that we recruited. A larger sample may have improved the reliability of two of the stigma constructs namely “Screening and Identification of HIV status” with Cronbach alpha of 0.44 and “Social Contact/Interaction” with Cronbach alpha of 0.68. Cronbach alpha measures how well a set of items (or variables) measures a single unidimensional latent construct, and is an important measure of the reliability or consistency of survey questions or psychometric instruments. In natural science, a Cronbach alpha of 0.70 is considered acceptable (Nunnally 1978), but in the social sciences, Cronbach alphas of less than 0.60 have been noted (Hatcher 1994). The Cronbach alpha of 0.68 for “Social Contact/Interaction” can be considered acceptable because with rounding off this would be 0.70, but the Cronbach alpha of 0.44 for “Screening and Identification of HIV Status” is marginal or low. The variables measuring the Screening and Identification construct all had factor loadings ranging form 0.45 to 0.63 which can be considered acceptable. However, since the Cronbach alpha is marginal we place less emphasis on this part of the results and suggest that future studies should be conducted to re-examine the questions that were asked.
The restriction of our data collection to Kumasi limits generalization of our results to this region of Ghana. Despite the limitations, this study identified constructs of HIV/AIDS stigma and characteristics of individuals more likely to demonstrate stigma. These findings add to the scientific body of literature focused on identifying the experience and effects of HIV/AIDS stigma on PLWHA, community members, caregivers and family members. Further research is needed to identify the effect of stigma reduction interventions in the workplace and community. Particular emphasis should be placed on careful identification of educational messages that will bring about change in cultural and religious attitudes and result in reduction of HIV/AIDS stigmatization in the work place and community. Our findings provide insightful information that can guide policy makers and researchers in the design and implementation of such interventions.
In the context of Ghana, educational interventions should be sensitive to the prevailing sociocultural, religious and economic environment, and should address areas such as, the harm of cultural and religious judgements of HIV positive persons, the benefits of testing and knowing one’s HIV status, inability to contract HIV by casual social contact, and the overall benefit to the individual and the economy when an HIV positive person is allowed to receive proper health care and treatment and to continue living as productive members of the community. HIV positive persons and their families also need to be provided with factual information about HIV/AIDS including information on home management and psychological aspects of the disease. They need training to help them improve their self-esteem and self-efficacy and positive coping skills. Educational intervention should seek to remove the belief among members of the community that they can be physically, socially and morally tainted by interacting with PLWHA. At the institutional level, health care workers and the legal system should be targeted in order to promote access to care and testing services and to protect the rights of PLWHA and their families. Since religion greatly influences daily life in Ghana, successful intervention with religious leaders (and other opinion leaders) regarding compassionate attitudes toward PLWHA should significantly impact and change societal attitudes toward PLWHA.
Acknowledgements
This study was supported by the Minority Health International Research Training (MHIRT) grant # T37-MD001448 from the National Center on Minority Health and Health Disparities, National Institutes of Health, Bethesda, MD, USA, and the Ghana Health Service, Kumasi, Ghana. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. We thank St. Markus Hospital, Ghana, for providing office space for the project. We also acknowledge Mr. Toni Amoaten, Mr. Otchere Baffour, Mr. Daniel Kwabala, Mr. Alhaji Ali Salifu, Mr. Micheal Boamey, and Mr. Chibuike Ulasi for logistic and research support.
References
- Aggleton P. Global priorities for HIV/AIDS intervention research. International Journal of STD & AIDS. 1996;7 Suppl 2:13–16. doi: 10.1258/0956462961917726. [DOI] [PubMed] [Google Scholar]
- Alonzo AA, Reynolds NR. Stigma, HIV and AIDS: an exploration and elaboration of a stigma trajectory. Social Science & Medicine. 1995;41:303–315. doi: 10.1016/0277-9536(94)00384-6. [DOI] [PubMed] [Google Scholar]
- Ankomah A. Condom use in sexual exchange relationships among young single adults in Ghana. AIDS Education and Prevention. 1998;10:303–316. [PubMed] [Google Scholar]
- Attipoe D. [Accessed January 24, 2008];Literature Review: Looking at Ghana in view of AIDS epicenters elsewhere. The Gully online magazine. 2008 at http://www.thegully.com/essays/gaymundo/0403_gay-men_hiv_ghana/msm_ghana_lit_review.html.
- Awusabo-Asare K, Abane AM, Kumi-Kyereme A. [Accessed January 20, 2008];Adolescent sexual and reproductive health in Ghana: A Synthesis of Research Evidence. Occasional Report No. 13. 2004 from http://www.guttmacher.org/pubs/or_no13.pdf.
- Awusabo-Asare K, Marfo C. Attitudes to and management of HIV/AIDS among health workers in Ghana: the case of Cape Coast municipality. Health Transition Review. 1997;7 Suppl:271–280. [PubMed] [Google Scholar]
- Ayranci U. AIDS knowledge and attitudes in a Turkish population: an epidemiological study. BMC Public Health. 2005;5:95. doi: 10.1186/1471-2458-5-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball AL, Rana S, Dehne KL. HIV Prevention among Injecting Drug Users: Responses in Developing and Transitional Countries. Public Health Reports. 1998;113 Supp. 1:170–181. [PMC free article] [PubMed] [Google Scholar]
- Boer H, Emons PA. Accurate and inaccurate HIV transmission beliefs, stigmatizing and HIV protection motivation in northern Thailand. AIDS Care. 2004;16:167–176. doi: 10.1080/09540120410001641011. [DOI] [PubMed] [Google Scholar]
- Bottonari KA, Roberts JE, Ciesla JA, Hewitt RG. Life stress and adherence to antiretroviral therapy among HIV-positive individuals: a preliminary investigation. AIDS Patient Care and STDS. 2005;19:719–727. doi: 10.1089/apc.2005.19.719. [DOI] [PubMed] [Google Scholar]
- Brooks RA, Martin DJ, Ortiz DJ, Veniegas RC. Perceived barriers to employment among persons living with HIV/AIDS. AIDS Care. 2004;16:756–766. doi: 10.1080/09540120412331269594. [DOI] [PubMed] [Google Scholar]
- Carr RL, Gramling LF. Stigma: Health Barrier for Women with HIV/AIDS. The Journal of the Association of Nurses in AIDS Care. 2004;15:30–39. doi: 10.1177/1055329003261981. [DOI] [PubMed] [Google Scholar]
- CIA. The World Factbook. 2005 Available at: www.cia.gov/library/publications/the-world-factbook/index.html.
- Decosas J. Epidemic in Ghana: "a very distinct profile". AIDS Analysis Africa. 1995;5:12. [PubMed] [Google Scholar]
- Ehiri JE, Anyanwu EC, Amusu D, Sanu I, Jolly PE. AIDS-related stigma in sub-Saharan Africa: Its contexts and potential intervention strategies. AIDS & Public Policy Journal. 2005;20:25–39. [PubMed] [Google Scholar]
- Ghana AIDS Commission. Ghana HIV/AIDS Strategic Framework 2001–2005. 2000 [Google Scholar]
- Ghana Statistical Service (GSS), N.M.I.F.M.R.N., and ORC, and Macro. Ghana Demographic and Health Survey 2003. Calverton, Maryland: GSS, NMIMR, and ORC Macro; 2004. [Google Scholar]
- Goffman E. Stigma: Notes on the Management of Spoiled Identity. New York: Simon and Schuster; [Google Scholar]
- Gregson S, Mason PR, Garnett GP, Zhuwau T, Nyamukapa CA, Anderson RM, Chandiwana SK. A rural HIV epidemic in Zimbabwe? Findings from a population-based survey. Int J STD AIDS. 2001;12:189–196. doi: 10.1258/0956462011917009. [DOI] [PubMed] [Google Scholar]
- Hatcher L. A step-by-step approach to using the SAS System for Factor Analysis and Structural Equation Modeling. NC. USA: SAS Institute Inc.; 1994. [Google Scholar]
- Herek GM, Glunt EK. An epidemic of stigma. Public reactions to AIDS. The American Psychologist. 1988;43:886–891. doi: 10.1037//0003-066x.43.11.886. [DOI] [PubMed] [Google Scholar]
- Heyward WL, Batter VL, Malulu M, Mbuyi N, Mbu L, St Louis ME, Kamenga M, Ryder RW. Impact of HIV counseling and testing among child-bearing women in Kinshasa, Zaire. AIDS. 1993;7:1633–1637. doi: 10.1097/00002030-199312000-00014. [DOI] [PubMed] [Google Scholar]
- Hintz M. Living in the Tropics: A Cultural Geography. New York: Franklin Watts; 1987. 1987. [Google Scholar]
- Influencing Factors. [Accessed January 24, 2008];The Gully online magazine. 2008 http://www.thegully.com/essays/gaymundo/0403_gay-men_hiv_ghana/msm_ghana_findings3.html.
- Integrated Regional Information Networks (IRIN), Africa. GHANA: New malaria drugs and expansion of ARV treatment push up government drugs bill: UN Office for the Coordination of Humanitarian Affairs. IRIN. 2005 January; News.org.
- Kaldjian LC, Jekel JF, Friedland G. End-of-life decisions in HIV-positive patients: the role of spiritual belief. AIDS. 1998;12:103–107. doi: 10.1097/00002030-199801000-00012. [DOI] [PubMed] [Google Scholar]
- Katz S, Nevid JS. Risk factors associated with posttraumatic stress disorder symptomatology in HIV-infected women. AIDS Patient Care and STDS. 2005;19:110–120. doi: 10.1089/apc.2005.19.110. [DOI] [PubMed] [Google Scholar]
- Known MSM Sites. [Accessed January 24, 2008];The Gully online magazine. 2008 at http://www.thegully.com/essays/gaymundo/0403_gay-men_hiv_ghana/msm_ghana_findings3.html.
- Mill J. Shrouded in Secrecy: Breaking the News of HIV Infection to Ghanaian Women. Journal of Transcultural Nursing. 2003;14:6–16. doi: 10.1177/1043659602238345. [DOI] [PubMed] [Google Scholar]
- Moneyham L, Seals B, Demi A, Sowell R, Cohen L, Guillory J. Experiences of disclosure in women infected with HIV. Health Care for Women International. 1996;17:209–221. doi: 10.1080/07399339609516236. [DOI] [PubMed] [Google Scholar]
- Muyinda H, Seeley J, Pickering H, Barton T. Social aspects of AIDS-related stigma in rural Uganda. Health & Place. 1997;3:143–147. doi: 10.1016/s1353-8292(97)00010-5. [DOI] [PubMed] [Google Scholar]
- Mwinituo PP, Mill JE. Stigma Associated With Ghanaian Caregivers of AIDS Patients. Western Journal of Nursing Research. 2006;28:369–382. doi: 10.1177/0193945906286602. [DOI] [PubMed] [Google Scholar]
- HIV/AIDS in Ghana (Background, Projections, Impacts, Interventions and Policy) 3rd Edition 2001. Dec, National AIDS/STI Control Programme, Disease Control Unit, Ministry of Health. [Google Scholar]
- Nunally J. Psychometric theory. New York: McGraw-Hill; 1978. [Google Scholar]
- Piot P. AIDS: from crisis management to sustained strategic response. Lancet. 2006;368:526–530. doi: 10.1016/S0140-6736(06)69161-7. [DOI] [PubMed] [Google Scholar]
- Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat. World Population Prospects: The 2004 Revision and World Urbanization Prospects. 2005 Available: http://esa.un.org/unup.
- Prince. Gay in Ghana. [Accessed January 24, 2008];The Gully online magazine. 2004 at http://www.thegully.com/essays/gaymundo/040623_gay_life_ghana.html.
- Reynolds NR, Testa MA, Marc LG, Chesney MA, Neidig JL, Smith SR, Vella S, Robbins GK. Factors influencing medication adherence beliefs and self-efficacy in persons naive to antiretroviral therapy: a multicenter, cross-sectional study. AIDS and Behavior. 2004;8:141–150. doi: 10.1023/B:AIBE.0000030245.52406.bb. [DOI] [PubMed] [Google Scholar]
- Republic of Ghana. Ghana HIV/AIDS Response Analysis. 2000 [Google Scholar]
- Sledjeski EM, Delahanty DL, Bogart LM. Incidence and impact of posttraumatic stress disorder and comorbid depression on adherence to HAART and CD4+ counts in people living with HIV. AIDS Patient Care and STDS. 2005;19:728–736. doi: 10.1089/apc.2005.19.728. [DOI] [PubMed] [Google Scholar]
- Sowell RL, Seals B, Moneyham L, Guillory J, Demi A, Cohen L. Barriers to health-seeking behaviors for women infected with HIV. NursingConnections. 1996;9:5–17. [PubMed] [Google Scholar]
- Standing H. AIDS: conceptual and methodological issues in researching sexual behaviour in sub-Saharan Africa. Social Science & Medicine. 1992;34:475–483. doi: 10.1016/0277-9536(92)90202-2. [DOI] [PubMed] [Google Scholar]
- UNAIDS. Report on the global AIDS epidemic. Geneva: World Health Organization; 2006. Available at website: www.unaids.org/en/Regions_Countries/Countries/ghana.asp. [Google Scholar]
- UNAIDS. Geneva: World Health Organization (WHO); Joint United Nations Programme on HIV/AIDS (UNAIDS) 2006; Uniting the world against AIDS. 2007 Accessed.
- UNAIDS, UNICEF, WHO. Epidemiological Fact Sheets on HIV/AIDS and Sexually Transmitted Infections - Ghana. 2002 Update.
- Wade AS, Enel C, Lagarde E. Qualitative changes in AIDS preventive attitudes in a rural Senegalese population. AIDS Care. 2006;18:514–519. doi: 10.1080/09540120600569465. [DOI] [PubMed] [Google Scholar]
- Weiss MG, Ramakrishna J. Conference examines need for more study of AIDS stigma. AIDS Policy & Law. 2001;16:4. [PubMed] [Google Scholar]
- WHO/UNAIDS. Geneva: World Health Organization (WHO), Joint United Nations Programme on HIV/AIDS (UNAIDS) 2004; Report on the Global AIDS Epidemic. 2004
- WiLDAF-Ghana. [Accessed January 21, 2008];Shadow Report to Ghana’s Third, Fourth & Fifth Reports on the Implementation of the CEDAW in Ghana. 2006 from http://www.iwraw-ap.org/resources/pdf/Ghana_SR.pdf.
- Wilkins A, Hayes R, Alonso P, Baldeh S, Berry N, Cham K, Hughes A, Jaiteh K, Oelman B, Tedder R, et al. Risk factors for HIV-2 infection in The Gambia. AIDS. 1991;5:1127–1132. doi: 10.1097/00002030-199109000-00012. [DOI] [PubMed] [Google Scholar]
- Yeboah-Afari A. Helping prostitutes in Accra. AIDS Watch. 1988;4:4–5. [PubMed] [Google Scholar]
- Zwi AB. Reassessing priorities: identifying the determinants of HIV transmission. Social Science & Medicine. 1993;36:iii–viii. doi: 10.1016/0277-9536(93)90054-8. [DOI] [PubMed] [Google Scholar]