SYNOPSIS
Public health concerns such as multi- and extensive drug-resistant tuberculosis, bioterrorism, pandemic influenza, and severe acute respiratory syndrome have intensified efforts to prevent transmission of infections that are completely or partially airborne using environmental controls. One such control, ultraviolet germicidal irradiation (UVGI), has received renewed interest after decades of underutilization and neglect. With renewed interest, however, come renewed questions, especially regarding efficacy and safety. There is a long history of investigations concluding that, if used properly, UVGI can be safe and highly effective in disinfecting the air, thereby preventing transmission of a variety of airborne infections. Despite this long history, many infection control professionals are not familiar with the history of UVGI and how it has, and has not, been used safely and effectively. This article reviews that history of UVGI for air disinfection, starting with its biological basis, moving to its application in the real world, and ending with its current status.
Ultraviolet germicidal irradiation (UVGI) is an established means of disinfection and can be used to prevent the spread of certain infectious diseases. Low-pressure mercury (Hg) discharge lamps are commonly used in UVGI applications and emit shortwave ultraviolet-C (UV-C, 100–280 nanometer [nm]) radiation, primarily at 254 nm. UV-C radiation kills or inactivates microbes by damaging their deoxyribonucleic acid (DNA). The principal mode of inactivation occurs when the absorption of a photon forms pyrimidine dimers between adjacent thymine bases and renders the microbe incapable of replicating. UVGI can be used to disinfect air, water, and surfaces, although surface disinfection is limited by microshadows and absorptive protective layers. Water disinfection is currently the most advanced and accepted germicidal application. Air disinfection is accomplished via several methods: irradiating the upper-room air only, irradiating the full room (when the room is not occupied or protective clothing is worn), and irradiating air as it passes through enclosed air-circulation and heating, ventilation, and air-conditioning (HVAC) systems. UVGI is also used in self-contained room air disinfection units.
Upper-room UVGI is one of two primary applications of UVGI air disinfection. Designed for use in occupied rooms without using protective clothing, upper-room UVGI uses wall-mounted and ceiling-suspended, louvered/shielded UVGI fixtures to confine the germicidal radiation to the entire room area above people's heads and greatly minimizes exposure to occupants in the lower room. Effective air disinfection in the breathing zone then depends on good vertical air movement between the upper and lower room, which can be generated naturally by convection, the HVAC system, or low-velocity paddle fans where needed.
In-duct UVGI is the other primary application of UVGI air disinfection. Designed to disinfect air as it passes through the HVAC system and before it is recirculated or exhausted, in-duct UVGI irradiates the entire cross-section of a duct at high intensities not accessible to room occupants, and may include the use of highly UV-reflective materials to further increase irradiance levels. Effective room air disinfection depends on circulating maximal room air through the duct and the velocity at which it is circulated. Also, though not designed to disinfect the air in any direct way, UVGI is used to disinfect surfaces inside HVAC systems, such as cooling coils and drip pans. Disinfecting these surfaces may reduce the maintenance requirements for HVAC systems, and it has been suggested that it could also reduce nonspecific building-related illnesses.1,2
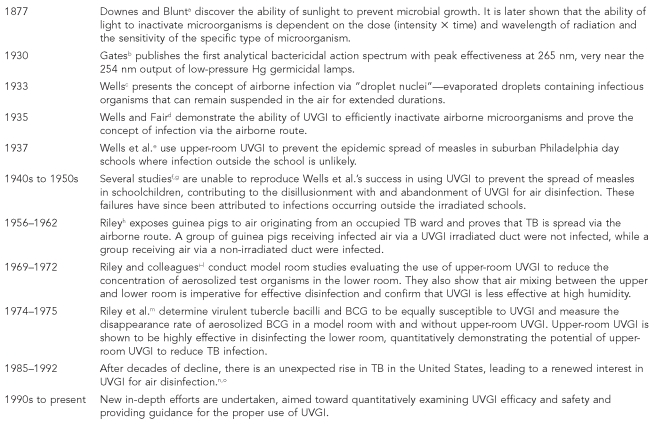
The history of UVGI air disinfection has been one of promise, disappointment, and rebirth. Investigations of the bactericidal effect of sunlight in the late 19th century planted the seed of air disinfection by UV radiation. First to nurture this seed was William F. Wells, who both discovered the spread of airborne infection by droplet nuclei and demonstrated the ability of UVGI to prevent such spread. Despite early successes in applying UVGI, its use would soon wane due to a variety of reasons that will be discussed in this article. However, with the enduring research of Riley and others, and an increase in tuberculosis (TB) during the 1980s, interest in UVGI was revitalized. With modern concerns regarding multi- and extensive drug-resistant TB, bioterrorism, influenza pandemics, and severe acute respiratory syndrome, interest in UVGI continues to grow. Research is ongoing, and there is much evidence on the efficacy of UVGI and the proper way to use it, though the technology has yet to fully mature. Figure 1 provides an overview of some of the key studies in the history of UVGI air disinfection.
Figure 1.
Overview of selected key events in the history of UVGI air disinfection
aDownes A, Blunt TP. The influence of light upon the development of bacteria. Nature 1877;16:218.
bGates FL. A study of the bactericidal action of ultra violet light: III. The absorption of ultra violet light by bacteria. J Gen Physiol 1930;14:31-42.
cWells WF. On air-borne infection: study II. Droplets and droplet nuclei. Am J Hyg 1934;20:611-8.
dWells WF, Fair MG. Viability of B. coli exposed to ultra-violet radiation in air. Science 1935;82:280-1.
eWells WF, Wells MW, Wilder TS. The environmental control of epidemic contagion I: an epidemiologic study of radiant disinfection of air in day schools. Am J Hyg 1942;35:97-121.
fPerkins JE, Bahlke AM, Silverman HF. Effect of ultra-violet irradiation of classrooms on spread of measles in large rural central schools: preliminary report. Am J Public Health Nations Health 1947;37:529-37.
gAir disinfection with ultra-violet irradiation: its effect on illness among school-children. Spec Rep Ser Med Res Counc (G B) 1954;283:1-88.
hRiley RL, Mills CC, O'Grady F, Sultan LU, Wittstadt F, Shivpuri DN. Infectiousness of air from a tuberculosis ward. Ultraviolet irradiation of infected air: comparative infectiousness of different patients. Am Rev Respir Dis 1962;85:511-25.
iRiley RL, Permutt S. Room air disinfection by ultraviolet irradiation of upper air: air mixing and germicidal effectiveness. Arch Environ Health 1971;22:208-19.
jRiley RL, Permutt S, Kaufman JE. Convection, air mixing, and ultraviolet air disinfection in rooms. Arch Environ Health 1971;22:200-7.
kRiley RL, Permutt S, Kaufman JE. Room air disinfection by ultraviolet irradiation of upper air: further analysis of convective air exchange. Arch Environ Health 1971;23:35-9.
lRiley RL, Kaufman JE. Effect of relative humidity on the inactivation of airborne Serratia marcescens by ultraviolet radiation. Appl Microbiol 1972;23:1113-20.
mRiley RL, Knight M, Middlebrook G. Ultraviolet susceptibility of BCG and virulent tubercle bacilli. Am Rev Respir Dis 1976;113:413-8.
nPorter JD, McAdam KP. The re-emergence of tuberculosis. Annu Rev Public Health 1994;15:303-23.
oNardell EA. Environmental control of tuberculosis. Med Clin North Am 1993;77:1315-34.
pEscombe AR, Moore DAJ, Gilman RH, Navincopa M, Ticona E, Mitchell B, et al. Upper-room ultraviolet light and negative air ionization to prevent tuberculosis transmission. PLoS Med 2009;6:e43.
qPersonal communication, Edward Nardell, Harvard School of Public Health, October 2008
UVGI = ultraviolet germicidal irradiation
nm = nanometer
Hg = mercury
TB = tuberculosis
BCG = Bacillus Calmette-Guérin
HIV = human immunodeficiency virus
This review highlights selected influential, critical, and representative events throughout the history of UVGI air disinfection.
DISCOVERY OF THE GERMICIDAL ACTION OF UV RADIATION AND ITS BIOLOGICAL BASIS
As early as 1845, it was known that microorganisms respond to light.3 A breakthrough came in 1877, when Downes and Blunt4–6 observed that exposing test tubes containing Pasteur's solution to sunlight prevented the growth of microorganisms inside the tube and, upon increased exposure durations, the test tubes remained bacteria-free for several months. In his 2002 article on the history of UV photobiology, Hockberger called this “one of the most influential discoveries in all of photobiology.”7 Downes and Blunt went on to demonstrate that the ability of sunlight to neutralize bacteria was dependent on intensity, duration, and wavelength, with the shorter wavelengths of the solar spectrum being the most effective. Tyndall later confirmed these results.8,9
These early investigations pointed toward some key factors (to be later investigated in-depth) that influence UVGI performance. Inactivation of a given fraction of organisms is dependent on the dose of radiation received. Dose (J●m−2) is the product of intensity (W●m−2) and exposure duration (s). Inactivation is also dependent on the wavelength of received radiation. Much of the work following these initial investigations was devoted to finding the wavelength dependence of the germicidal action of light, with investigations into the following wavelength ranges: UV-C (100–280 nm), UV-B (280–315 nm), UV-A (315–400 nm), visible (400–700 nm), and infrared (700–106 nm).
In 1885, Duclaux reported differences in sensitivity to sunlight between different species of bacteria spores.10–12 This finding pointed to another key factor that influences UVGI performance—microbial sensitivity. Different microbes have different sensitivities to UVGI and require varying doses of radiation for the same fraction of inactivation. Many later studies would attempt to quantify the UVGI sensitivity for numerous types of microorganisms. In 1890, Koch demonstrated the lethal effect of sunlight on tubercle bacillus, portending the modern use of UVGI to combat TB infection.13 Two years later, using a prism, a heliostat, and quartz test tubes, Geisler showed that UV radiation from sunlight and electric lamps was more effective in killing bacteria than longer wavelength radiation; however, he also noted that the lethal effects of longer wavelength radiation were amplified at increased intensities.14 Buchner dismissed contributions from infrared radiation on the germicidal action of sunlight by passing sunlight through an infrared-absorbing water filter before it reached a bacterial sample.15 Ward improved upon these results between 1892 and 1894, demonstrating the violet-blue and UV-A portions of the solar spectrum to be the most deleterious to bacteria.16–18
Between 1901 and 1903, Bang reported different sensitivities of Bacillus prodigiosus to UV radiation, with UV-B and UV-C radiation more effective than UV-A radiation.19,20 Employing a prism and different arc lamps, a peak bactericidal effectiveness between 226.5 nm and 328.7 nm was confirmed by Barnard and Morgan.21 Hertel was the first to provide a thorough quantitative analysis of the effect of light on microorganisms. Between 1904 and 1905, Hertel used a prism and thermoelectric measurement technique to quantify the relative intensity of radiation emitted from arc lamps, varying as a function of wavelength. With these data, Hertel established the degree of germicidal effectiveness between the UV and visible spectral regions. The region of greatest effectiveness was found to be the UV-C, followed by UV-B, UV-A, and visible radiation, respectively, with the dose required for cell death increasing by orders of magnitude in the visible region.22,23
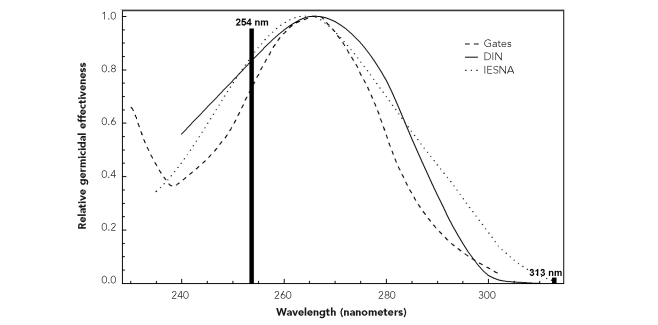
Henri and Henri were the first to show the mutagenic effects of UV radiation. In 1914, they observed modification of the metabolism of Bacillus anthracis upon exposure to sublethal doses of UV radiation.24 In 1929 and 1930, Gates published a series of articles providing the first analytical bactericidal action spectrum.25–27 Using an Hg arc lamp, Gates produced similarly shaped action spectra for Staphylococcus aureus and Bacillus coli (B. coli), both with peak effectiveness at 265 nm. These action spectra corresponded to the absorption spectrum of nucleic acids, and Gates hinted that his data “… point the way in a further search for the specific substance, or substances, involved in the lethal reaction,” suggesting that nucleic acids may be the genetic material and responsible for cell death—not proteins, as was a common belief28 at the time. In his article on UV action spectroscopy, Coohill expressed that Gates' bactericidal action spectrum was “… considered by some to be the most crucial action spectrum ever published.”29 Gates' findings were supported by Ehrismann and Noethling in 1932;30 in 1935, the Commission Internationale de l'Eclairage (CIE)31 examined early data and proposed an official bactericidal action spectrum. Gates' historical bactericidal action spectrum for B. coli is plotted in Figure 2, along with two modern germicidal action spectra and the relative output of a germicidal lamp.
Figure 2.
Gates' original bactericidal action spectrum for Bacterium coli,a modern germicidal action spectra,b and the relative output of a low-pressure Hg germicidal lampc,d
aAdapted from: Gates FL. A study of the bactericidal action of ultra violet light: III. The absorption of ultra violet light by bacteria. J Gen Physiol 1930;14:31-42.
bAdapted from: Commission Internationale de l'Eclairage. Technical report: ultraviolet air disinfection (CIE 155/2003). Vienna: CIE; 2003.
cAdapted from: Illuminating Engineering Society of North America. Lighting handbook: reference – application. 8th ed. New York: IESNA; 1993.
dThe modern action spectra are derived from the Deutsches Institut für Normung (represented with a solid line) and the Illuminating Engineering Society of North America (represented with a dotted line). The relative output of a low-pressure Hg germicidal lamp is overlaid on these action spectra to illustrate why the lamps are highly efficient in germicidal applications.
Hg = mercury
DIN = Deutsches Institut füur Normung
IESNA = Illuminating Engineering Society of North America
Hollaender and associates,32–34 among others, picked up where Gates left off, and by 1944, Hollaender and Oliphant claimed, “It is quite possible that the high sensitivity of many agents at about [260 nm] is based on the important function desoxyribose nucleic acid plays in biological activities.”35 Beukers and Berends36 exposed frozen solutions of thymine to UV-C radiation in 1960, resulting in the formation of thymine dimers. Shortly thereafter, the production of dimers from adjacent pyrimidines was demonstrated after exposure to UV radiation, accounting for “a large part of the effects of ultraviolet radiation on biological systems.”37 The biological foundation of UVGI had been laid. For a more extensive review on the history of the biological effects of UV radiation on microorganisms, see Hockberger7,38 and Coohill.29
The distinction should be made between the biological effect and the penetration depth of UV radiation, a key concept in UVGI safety. UV-C wavelengths are the most biologically active radiation and, ironically, much less dangerous to humans. This is because UV-C radiation is absorbed by the outer dead layer of human skin, while UV-B and UV-A radiation penetrate deeper.39 While attention to UVGI safety is important, because overexposure to 254 nm radiation can readily cause erythema (“sunburn”) to the skin and photokeratitis (“welder's flash”) to the eyes, the long-term health risks are considered to be negligible compared with common solar UV exposures.
THE EFFICACY AND APPLICATION OF UVGI AIR DISINFECTION
The beginning (1930s to 1950s): Wells, droplet nuclei, and the prevention of measles
William F. Wells pioneered both the concept of airborne infection by droplet nuclei and the use of UVGI to disinfect the air. In 1933, Wells presented the idea that various-sized droplets containing infectious organisms are expelled into the air and quickly dried by evaporation after an infectious person coughs or sneezes,40 expanding upon an early droplet theory put forth by Flüugge.41 These evaporated droplets, or droplet nuclei, can remain in the air for extended periods of time, and people can breathe them in. The idea of infection via droplet nuclei had been sparked by investigations into respiratory infections associated with dust-suppressive water sprays used in New England textile mills.
While the ability of UV radiation to inactivate microorganisms was known, previous studies had exposed microorganisms on solid media or in liquids, not in the air. In 1935, using aerosolized B. coli, 254 nm radiation, and carefully controlled conditions, Wells went on to demonstrate that airborne infectious organisms could be effectively killed in a short period of time.42 The use of UVGI not only inactivated the infectious organisms in the air, but proved the very concept that infections can be spread via the airborne route. Sharp was the first to confirm these results and documented an example of airstream disinfection, foreshadowing the use of UVGI in in-duct HVAC systems.43,44 These initial investigations would provide the framework and impetus for infection control by the irradiation of air.
Immediately perceiving the potential of UVGI, Hart employed direct, high-intensity UVGI for the disinfection of hospital operating room air at the Duke University Hospital in 1936, after traditional methods had failed.45 The setup was designed to irradiate the entire room, with special emphasis on highly irradiating the volume around the surgical site and instrument/supply tables. Hart later reported the reduction in the postoperative wound infection rate in clean cases from 11.62% without the use of UVGI to 0.24% with the use of UVGI.46 Following Hart's lead, colleagues from Duke and other hospitals installed UVGI in their operating rooms and reported similar success.47–51
Following initial successes in the operating room, the application of UVGI in hospitals was soon extended to infant wards by implementing various configurations of cubicle-like UVGI “light curtains” designed to prevent respiratory cross-infections. As in the operating room, high-intensity, direct UVGI was used, assuming that human exposure would be transient in passing through. In 1936, Wells and colleagues designed such UVGI barriers for Charles McKhann at the Infants' and Children's Hospital in Boston. In 1941, Del Mundo and McKhann reported a difference in the infection rate of 12.5% in a control ward and 2.7% in a ward with UVGI barriers.52 Parallel studies evaluating UVGI barriers reported successes similar to that in Boston, including both the reduction of respiratory cross-infections and the reduction of cross-cubicle spread of aerosolized test organisms.53–58
Modifying the original experimental design, other studies of cross-infection in infant wards employed upper-room UVGI instead of light curtains. As discussed previously, upper-room UVGI confines the germicidal radiation to the entire room area above people's heads, and effective air disinfection in the lower room then depends on good vertical air movement between the upper and lower room. Robertson et al. reported nearly one-half the number of infections using only upper-room UVGI in rooms where natural ventilation was impeded; no additional effect from UVGI was found in rooms where doors and windows were left open.57 Several other investigators produced further positive results using upper-room UVGI to prevent cross-infections.58–60
Between 1937 and 1941, Wells successfully used upper-room UVGI to prevent the epidemic spread of measles among children in suburban Philadelphia day schools, where infection outside of school was unlikely—a classic experiment that has been difficult to reproduce. During this study, 53.6% of susceptibles in unirradiated schools were infected, while only 13.3% of susceptibles in irradiated schools were infected (excluding secondary infections from siblings), even with the irradiated schools having a greater percentage of susceptibles.61 These results were supported upon investigation of measles attack rates in other nearby unirradiated schools.62
In 1943, the Council on Physical Therapy accepted UVGI for disinfecting purposes.63 From 1941 to 1943, Lurie exposed two sets of rabbits to air originating from rabbits infected with TB. With sufficient germicidal intensity, none of the rabbits receiving irradiated air developed TB, while the majority of the rabbits receiving non-irradiated air did.64 Beginning in 1943, studies were undertaken to evaluate the ability of upper-room UVGI (the floor was later irradiated also) to prevent respiratory infections in the intermittent aggregations at naval training stations. These studies produced modest success, limited by less-than-ideal experimental designs.65–69
Early investigations by Whisler,70 Wells,71–74 and -others75 evaluated the effect of physical and environmental factors on UVGI efficacy, including humidity and air circulation—two important factors in the performance of UVGI. Microbes were found to be significantly more resistant to UVGI at higher humidity. Luckily, the humidity of most buildings is kept well below adverse levels to provide occupant comfort. Also, as discussed previously, good air circulation is requisite for effective upper-room UVGI. Infected lower-room air must circulate through the irradiated upper room, where inactivation depends on the received dose (the intensity of radiation in the upper room multiplied by how long the microbe remains in the irradiated zone). Air circulation is also an important factor in in-duct UVGI, which requires maximal room air circulation through the duct and is dependent on the velocity of air moving through the duct.
Throughout the 1940s, extensive work by Luckiesh and colleagues provided further evidence for the efficacy of UVGI, while also detailing early designs and guidelines for UVGI air disinfection systems and applications of UVGI.75 This work represented a high water mark in the technical knowledge and expertise of UVGI. The effectiveness of UVGI to disinfect exhaust air in infectious disease laboratories was also demonstrated, including the first use inside an air conditioner.76, 77
In 1955, Wells published the authoritative Air Contagion and Air Hygiene,62 deemed a “landmark monograph on air hygiene” by Edward Nardell.78 Six years later, Riley followed with his Airborne Infection: Transmission and Control.79 These two works may be consulted for greater detail in the early studies using UVGI and all other aspects of airborne infection.
Continued progress (1950s to 1970s): Riley, TB ward, and model rooms
Beginning in the 1930s as a Harvard medical student working in Wells' lab, Richard L. Riley became a disciple of and collaborator with Wells and his work on airborne infection and UVGI. In fact, Wells shared credit with Riley for the droplet nuclei concept. Riley and colleagues conducted two two-year experiments in a Veterans Hospital TB ward during the 1950s and early 1960s. In a preliminary study80 without patients, Escherrischia coli (E. coli) and bovine tubercle bacilli were separately aerosolized into the ward ventilation system with and without UVGI. UVGI effectively inactivated E. coli in the ward and prevented rabbits from developing TB. Conversely, exposed rabbits were infected with TB without the use of UVGI.
In subsequent studies, the TB ward was continually occupied with six infected patients and sealed from the rest of the hospital. The room air was exhausted through ventilation ducts to control chambers housing colonies of guinea pigs; one chamber received air from an irrFadiated duct and one received air from a non-irradiated duct. This method eliminated contagion via means other than through the exhausted air. The results of these studies confirmed both that TB could readily be spread through droplet nuclei and that UVGI could sufficiently inactivate the infected air (100% in the study).81,82 Riley also used the experiments to estimate the concentration of infectious droplet nuclei in the air and study the variability in the infectiousness of different patients. Around the same time, McLean prevented the spread of influenza in Veterans Hospital TB patients using upper-room UVGI during the 1957 pandemic, providing evidence for the airborne transmission of influenza. The infection rate was only 1.9% in an irradiated ward, while it was 18.9% in a non-irradiated ward.83
During the early 1970s, Riley and colleagues published a series of articles detailing the results of using upper-room UVGI in a model room aerosolized with Serratia marcescens. The effects on disinfection rates in the lower room from air mixing via convection and a ceiling fan were studied and mathematically modeled.84–86 It was shown that temperature gradients and ceiling fans could greatly affect air mixing in a room and, thus, the rate of disinfection in the lower room. By supplying air cooler than the lower-room air to the upper room and/or using a ceiling fan, the efficiency of UVGI in disinfecting the lower room was greatly increased. The ability to prevent the spread of infectious organisms throughout a building by placing UVGI in corridors was also demonstrated.87
Additionally, Riley et al. investigated the effect of relative humidity (RH) on the efficacy of UVGI, with a sharp decline found in the fraction of organisms killed at RH values higher than 60% to 70%.88 In 1972, Kethley and Branch conducted model room studies similar to Riley's and studied the effect of aerosol size and sampling location within a mechanically ventilated room. They found smaller particles to be more susceptible to UVGI, and discovered that different sampling locations produced different calculated disinfection rates. This led to the conclusion that lamp locations and air movement patterns within a room need to be considered for optimal disinfection.89
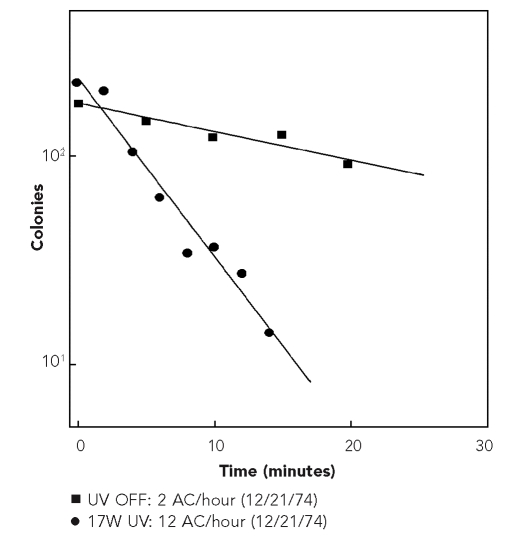
During 1975, Riley et al. found virulent tubercle bacilli and Bacillus Calmette-Guéerin (BCG) to be equally susceptible to UVGI. They then aerosolized BCG into an approximately 200-square-foot model room and measured its disappearance with and without upper-room UVGI, finding a sixfold increase in the disappearance rate using one 17-watt (electrical) fixture, and a ninefold increase using two fixtures of a combined 46 watts (electrical). It was inferred that the results using BCG were directly applicable to virulent tubercle bacilli.90 Riley also equated these results to the removal of contaminated air using ventilation, where one air change (AC) corresponds to a volume of fresh air entering (and contaminated air leaving) a room equal to the volume of the room. One AC equates to removing about 63% of contaminated air in a perfectly mixed room. Using this concept of air changes via ventilation, Riley expressed his results using UVGI in equivalent air changes (Eq AC). One Eq AC corresponds to inactivating about 63% of airborne microorganisms with UVGI in a perfectly mixed room. In his experiment, Riley calculated an increase of 10 and 25–33 AC/hour using the 17-watt and combined 46-watt upper-room UVGI fixtures, respectively. Figure 3 shows Riley's measured disappearance of BCG in the model room with and without the 17-watt upper-room UVGI fixture. This quantitatively illustrated the potential of upper-room UVGI to prevent TB transmission. For decades to follow, these results led to the following rule of thumb: 17 watts (electrical) input to UVGI lamps per 200 square feet of floor area. It was hoped that by following this guideline, similar air disinfection rates would be achieved.
Figure 3.
Disappearance rate of Bacillus Calmette-Guérin in a model room without upper-room UVGI and with a 17-watt upper-room UVGI lampa,b
aOne AC corresponds to adding a volume of fresh air to the room equal to the volume of the room and equates to a removal of about 63% of airborne organisms in a perfectly mixed room. One AC produced with UVGI represents an equivalent AC and equates to inactivating about 63% of airborne organisms with UVGI in a perfectly mixed room.
bAdapted from: Riley RL, Knight M, Middlebrook G. Ultraviolet susceptibility of BCG and virulent tubercle bacilli. Am Rev Respir Dis 1976;113:413-8.
UVGI = ultraviolet germicidal irradiation
UV = ultraviolet
AC = air change
W = WaH
Disillusionment, resurgence, and the current state of UVGI air disinfection
Despite the early successes in demonstrating the effectiveness of UVGI, the technology was largely abandoned and forgotten in the years following Wells' promising work.78,91 There are several reasons why this occurred. The inability to reproduce the success of Wells in preventing the spread of measles,92–95 along with other failures,96–100 engendered broad disillusionment with UVGI. Around the same time, antibiotics were developed to treat TB, and there was hope that common viral illnesses could be controlled by immunization. Additionally, there was concern regarding the health effects from UV-C exposure and the production of ozone by germicidal lamps. Concerns that UVGI required high maintenance, that UVGI would be ineffective at higher humidity, and that its germicidal efficacy was unproven also contributed to UVGI's second-class status among air disinfection strategies.
It is now known, through successes and failures, where and how UVGI can be effective.78 UVGI is most effective in preventing infections spread chiefly by droplet nuclei, not by direct contact or larger respiratory droplets, although some surface decontamination likely occurs. Also, the location(s) where UVGI is employed must also be the primary location(s) of disease transmission (i.e., there cannot be a high risk of acquiring the same infection outside the location where UVGI is used). From these criteria, the cause of previous UVGI failures can be deduced. The failure to prevent the spread of measles in schools can be explained by infections occurring outside the classroom (e.g., on school buses or through other extracurricular interaction).62,79 Wells successfully prevented the spread of measles in schools because infection occurring outside the school in a wealthy Philadelphia suburb was unlikely.
In the late 1980s, there was a renewed interest in UVGI due to the unexpected rise in TB in 1985 and the emergence of multiple drug-resistant strains, with specific concerns about the homeless, those infected with human immunodeficiency virus (HIV), and those who work with infected populations.101–103 It was then argued that UVGI, along with other measures, could be used to control the transmission of TB.104–109 Though the potential application of UVGI in locations such as hospitals and shelters was recognized, new challenges were also presented. Low ceiling heights and the lack of technical expertise, standards and regulations, and clinical trials all had to be addressed.
Since then, ongoing efforts toward meeting these new challenges have included: aerosol chamber and model room studies110–121 evaluating various environmental and physical factors on UVGI efficacy (e.g., air mixing and ventilation, humidity, microbial sensitivity, fixture irradiance and configuration, and photoreactivation); the mathematical modeling and predicting of UVGI fixture irradiances122–124 and room and duct disinfection/infection rates,123,125–133 including the use of computational fluid dynamics;134– 138 and applying UVGI in real-world studies.139–141 Other efforts have been directed toward establishing the maintenance requirements142 for UVGI fixtures, developing methods of accurate UVGI measurement,122,143–145 and evaluating the safety146,147 of UVGI installations, including the development of more modern “ozone-free” lamps. In 2003, the CIE148 published a technical report on UVGI air disinfection, summarizing the present state of knowledge. At press time, a CIE committee was preparing a report on the risk of photocarcinogenesis from UVGI lamps, including a comparison of the relative risk compared with typical UV-B and UV-A exposures from outdoor sunlight. Additional research has continued to evaluate the use of UVGI in the operating room to reduce postoperative infections.149,150
The Tuberculosis Ultraviolet Shelter Study (TUSS), the first real-world study on the use of UVGI to prevent TB, was conducted from 1997 to 2004.151 TUSS was a double-blind, placebo-controlled field trial that evaluated the use of upper-room UVGI at 14 homeless shelters in six U.S. cities. The results from TUSS were inconclusive due to insufficient numbers of documented TB skin test conversions (i.e., the rise in TB had already been checked); however, much practical experience and other data were gained from the study.147
Preliminary guidelines have also been -published,152–154 and, in 2005, the Centers for Disease Control and Prevention (CDC)155 expanded on its previous recommendation156 that UVGI be used as a supplement for TB infection control in health-care settings. In 2009, building upon initial guidelines and evaluating the influx of new research, CDC produced the first comprehensive guidance document for using upper-room UVGI to control TB in health-care settings.157
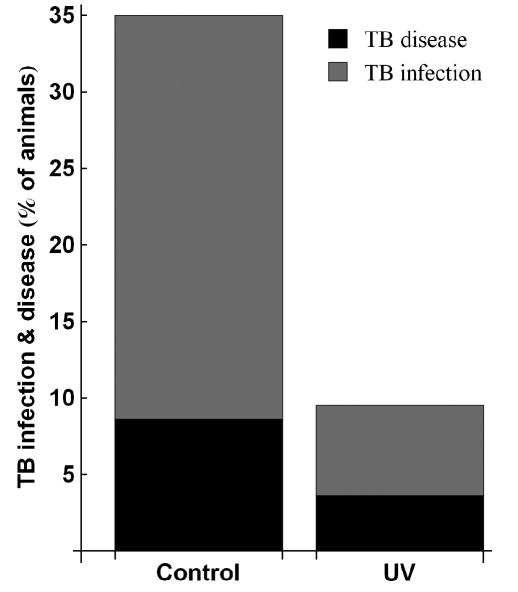
In 2009, Escombe and colleagues published the first clinical trial using upper-room UVGI to prevent TB transmission.158 Similar to Riley's classic studies in the 1950s, this study ventilated air from a continually occupied HIV-TB ward in Lima, Peru, to guinea pig colonies housed in rooftop chambers for 535 consecutive days. On alternating UV-on and -off days, one group of guinea pigs breathed air from the TB ward with upper-room UVGI and a mixing fan turned on, and a separate control group of guinea pigs breathed air from the TB ward with upper-room UVGI turned off. Further, air was drawn from the lower room without deliberately passing it through the UV field, simulating air breathed by occupants. Results showed a 34.9% infection rate in the control group and a reduced rate of 9.5% in the group with UVGI. TB disease was subsequently confirmed in 8.6% of the control group compared with 3.6% of the group with UVGI (Figure 4). It should also be noted that the mean RH during the study was about 77.0%, determined by previous studies to be above the maximum level for optimal UVGI efficacy.
Figure 4.
Escombe et al.'s results showing the proportion of TB ward-air exposed guinea pigs with evidence of TB infection or TB diseasea,b
aOne group was exposed when upper-room UVGI was turned on in the TB ward, and a control group was exposed when upper-room UVGI was turned off in the TB ward.
bAdapted from: Escombe AR, Moore DAJ, Gilman RH, Navincopa M, Ticona E, Mitchell B, et al. Upper-room ultraviolet light and negative air ionization to prevent tuberculosis transmission. PLoS Med 2009;6:e43.
TB = tuberculosis
UV = ultraviolet
UVGI = ultraviolet germicidal irradiation
At press time, Nardell and colleagues were completing a clinical trial using upper-room UVGI to prevent TB transmission similar to that of Escombe et al. (Personal communication, Edward Nardell, Harvard School of Public Health, October 2008). Also at the time of publication, Noakes and colleagues planned to develop a design tool and guidance documents to assist architects and engineers in designing effective and safe UVGI installations in real-world hospital environments (Personal communication, Catherine Noakes, Pathogen Control Engineering Research Group, School of Civil Engineering, University of Leeds, March 2009). Additionally, an interdisciplinary computer-assisted design lighting project promises to help engineers and architects design UVGI installations in a variety of settings (Personal communication, Edward Nardell, Harvard School of Public Health, October 2008). Together, these efforts will contribute even more valuable information, experience, and guidance for the use of upper-room UVGI to prevent airborne infection.
FUTURE DIRECTIONS
Research on UVGI air disinfection continues today. Although it is clear that UVGI can be effective in test chambers, engineering specifications for a given room application remain elusive and are currently based more on common sense and historical practice than on actual evidence. However, that evidence is accumulating, along with data on maintenance and safety in a wide variety of applications. It is now clearly understood, for example, that occupant motion and position within rooms greatly reduce the possibility of harmful overexposures to UV-C radiation in lower rooms.144 In practice, if upper-room UVGI systems are installed properly, UV radiation threshold limit values are rarely, if ever, approached, even using eye-level target values above those previously applied that assumed continuous eye exposure.
UVGI fixture designs are also evolving, becoming more efficient while remaining safe, but innovative designs are needed to further increase efficiency while keeping manufacturing costs low. Interest and investment by major lighting fixture companies is badly needed to stimulate further development; however, the cost of applying upper-room UVGI is an important factor—not in resource-rich countries, but in poor settings where UVGI is most critically needed to reduce transmission of TB, pandemic influenza, and other major airborne infectious threats. In these resource-limited settings, local manufacturers are needed to keep costs down. Finally, experts in the real-world application of UVGI are also needed, both in resource-rich and resource-limited settings. Once engineering specifications are better defined, however, interest by designers from the engineering, architecture, and lighting industries should follow.
Acknowledgments
The author thanks Edward Nardell for his inimitable insights into the history of ultraviolet germicidal irradiation for air disinfection and comments on this article; Stephen Rudnick for his invaluable comments on this article; and Claudia Coleman for finding many of the references.
Footnotes
This project was supported in part by an appointment to the Internship/Research Participation Program for the U.S. Army Center for Health Promotion and Preventive Medicine (USACHPPM) administered by the Oak Ridge Institute for Science and Education through an agreement between the U.S. Department of Energy and the USACHPPM.
The views expressed in this article are solely those of the author and do not necessarily reflect the official policy of the Department of the Army, the Department of Defense, or the U.S. government.
REFERENCES
- 1.Levetin E, Shaughnessy R, Rogers CA, Scheir R. Effectiveness of germicidal UV radiation for reducing fungal contamination within air-handling units. Appl Environ Microbiol. 2001;67:3712–5. doi: 10.1128/AEM.67.8.3712-3715.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Menzies D, Popa J, Hanley JA, Rand T, Milton DK. Effect of ultraviolet germicidal lights installed in office ventilation systems on workers' health and wellbeing: double-blind multiple crossover trial. Lancet. 2003;362:1785–91. doi: 10.1016/S0140-6736(03)14897-0. [DOI] [PubMed] [Google Scholar]
- 3.Schmarda LK. Der Einfluss des Lichtes auf die Infusionsthierchen. Med Jahrbüucher des k. k. Österreichischen Staates. 1845;54:257–70. [Google Scholar]
- 4.Downes A, Blunt TP. The influence of light upon the development of bacteria. Nature. 1877;16:218. [Google Scholar]
- 5.Downes A, Blunt TP. Researches on the effect of light upon bacteria and other organisms. Proc R Soc Lond. 1877;26:488–500. [Google Scholar]
- 6.Downes A, Blunt TP. On the influence of light upon protoplasm. Proc R Soc Lond. 1878;28:199–212. [Google Scholar]
- 7.Hockberger PE. A history of ultraviolet photobiology for humans, animals and microorganisms. Photochem Photobiol. 2002;76:561–79. doi: 10.1562/0031-8655(2002)0760561AHOUPF2.0.CO2. [DOI] [PubMed] [Google Scholar]
- 8.Tyndall J. Note on the influence exercised by light on organic infusions. Proc R Soc Lond. 1878;28:212–3. [Google Scholar]
- 9.Tyndall J. On the arrestation of infusorial life. Science. 1881;2:478. doi: 10.1126/science.os-2.68.478. [DOI] [PubMed] [Google Scholar]
- 10.Duclaux E. Influence de la luminére du soleil sur la vitalité des germes des microbes. Compt Rendus Hebd des Seances de l'Academie des Sciences. 1885;100:119–21. [Google Scholar]
- 11.Duclaux E. Sur la durée de la vie chez les germes des microbes. Annales de Chimie et de Physique. 1885;6:5–59. [Google Scholar]
- 12.Duclaux E. Influence de la luminére du soliel sur la vitalité de micrococcus. Compt Rendus Hebd des Seances et Mémoires Soc et Biologies. 1885;37:508–10. [Google Scholar]
- 13.Koch R. Ueber bakteriologische Forschung. Berlin: Hirschwald; 1890. [Google Scholar]
- 14.Geisler T. Zur Frage über die Wirkung des Licht auf Bakterien. Centralblatt für Bakteriologie und Parasitenkunde. 1892;11:161–73. [Google Scholar]
- 15.Buchner H. Ueber den Einfluss des Lichtes auf Bakterien. Centralblatt für Bakteriologie und Parasitenkunde. 1892;11:781–3. [Google Scholar]
- 16.Ward HM. Experiments on the action of light on Bacillus anthracis. Proc R Soc Lond. 1892;52:393–400. [Google Scholar]
- 17.Ward HM. Further experiments on the action of light on Bacillus anthracis. Proc R Soc Lond. 1893;53:23–44. [Google Scholar]
- 18.Ward HM. The action of light on bacteria. III. Philos Trans R Soc Lond B. 1894;185:961–86. [Google Scholar]
- 19.Bang S. Die Wirkungen des Lichtes auf Mikrooganismen. Mitt Finsens Med Lysinst. 1901;2:1–107. [Google Scholar]
- 20.Bang S. Über die Wirkungen des Lichtes auf Mikroben. II. Eine verbesserte Untersuchungs methode. Mitt Finsens Med Lysinst. 1903;3:97–112. [Google Scholar]
- 21.Barnard JE, Morgan H. Upon the bactericidal action of some ultra-violet radiations as produced by the continuous-current arc. Proc R Soc Lond. 1903;72:126–8. [Google Scholar]
- 22.Hertel E. Ueber Beeinflussung des Organismus durch Licht, speziell durch die chemisch wirksamen Strahlen. Zeitschrift für Allgemeine Physiologie. 1904;4:1–43. [Google Scholar]
- 23.Hertel E. Ueber physiologische Wirkung von Strahlen verschiedener Wellenlänge. Zeitschrift für Allgemeine Physiologie. 1905;5:95–122. [Google Scholar]
- 24.Henri MmeV, Henri V. Variation du pouvoir abiotique des rayons ultraviolets avec leur longueur d'onde. C R Seances Soc Biol Fil. 1914;73:321–2. [Google Scholar]
- 25.Gates FL. A study of the bactericidal action of ultra violet light: I. The reaction to monochromatic radiations. J Gen Physiol. 1929;13:231–48. doi: 10.1085/jgp.13.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gates FL. A study of the bactericidal action of ultra violet light: II. The effect of various environmental factors and conditions. J Gen Physiol. 1929;13:249–60. doi: 10.1085/jgp.13.2.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gates FL. A study of the bactericidal action of ultra violet light: III. The absorption of ultra violet light by bacteria. J Gen Physiol. 1930;14:31–42. doi: 10.1085/jgp.14.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris FI, Hoyt HS. The possible origin of the toxicity of ultra-violet light. Science. 1917;46:318–20. doi: 10.1126/science.46.1187.318. [DOI] [PubMed] [Google Scholar]
- 29.Coohill TP. Historical aspects of ultraviolet action spectroscopy. Photochem Photobiol. 1997;65(Suppl 1):S123–8. [Google Scholar]
- 30.Ehrismann O, Noethling W. Uber die bactericide wirkung monochromatischen lichtes. Z Hyg Infektionskr. 1932;113:597–628. [Google Scholar]
- 31.Commission Internationale de l'Eclairage. Compte rendu. Berlin: Proceedings of the CIE Session; 1935. [Google Scholar]
- 32.Hollaender A, Claus WD. The bactericidal effect of ultraviolet radiation on Escherrischia coli in liquid suspensions. J Gen Physiol. 1936;19:753–65. doi: 10.1085/jgp.19.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hollaender A, Emmons CW. The action of ultraviolet radiation on dermatophytes: I. The fungicidal effect of monochromatic radiation on the spores of Trichophyton mentagrophytes. J Cell Comp Physiol. 1939;13:391–402. [Google Scholar]
- 34.Emmons CW, Hollaender A. The action of ultraviolet radiation on dermatophytes: II. Mutations induced in cultures of dermatophytes by exposure of spores to monochromatic radiation. Am J Bot. 1939;26:467–75. [Google Scholar]
- 35.Hollaender A, Oliphant JW. The inactivating effect of monochromatic ultraviolet radiation on influenza virus. J Bacteriol. 1944;48:447–54. doi: 10.1128/jb.48.4.447-454.1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beukers R, Berends W. Isolation and identification of the irradiation product of thymine. Biochim Biophys Acta. 1960;41:550–1. doi: 10.1016/0006-3002(60)90063-9. [DOI] [PubMed] [Google Scholar]
- 37.Setlow RB. Cyclobutane-type pyrimidine dimers in polynucleotides. Science. 1966;153:379–86. doi: 10.1126/science.153.3734.379. [DOI] [PubMed] [Google Scholar]
- 38.Hockberger PE. The discovery of the damaging effect of sunlight on bacteria. J Photochem Photobiol B. 2000;58:185–91. doi: 10.1016/s1011-1344(00)00121-4. [DOI] [PubMed] [Google Scholar]
- 39.Bruls WA, Slaper H, Van der Leun JC, Berrens L. Transmission of human epidermis and stratum corneum as a function of thickness in ultraviolet and visible wavelengths. Photochem Photobiol. 1984;40:485–94. doi: 10.1111/j.1751-1097.1984.tb04622.x. [DOI] [PubMed] [Google Scholar]
- 40.Wells WF. On air-borne infection: study II. Droplets and droplet nuclei. Am J Hyg. 1934;20:611–8. [Google Scholar]
- 41.Flüugge C. Ueber Luftinfektion. Z Hyg Infectionskr. 1897;25:179–224. [Google Scholar]
- 42.Wells WF, Fair MG. Viability of B. coli exposed to ultra-violet radiation in air. Science. 1935;82:280–1. doi: 10.1126/science.82.2125.280-a. [DOI] [PubMed] [Google Scholar]
- 43.Sharp DG. A quantitative method of determining the lethal effect of ultraviolet light on bacteria suspended in air. J Bacteriol. 1938;35:589–99. doi: 10.1128/jb.35.6.589-599.1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sharp DG. The effects of ultraviolet light on bacteria suspended in air. J Bacteriol. 1940;39:535–47. doi: 10.1128/jb.39.5.535-547.1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hart D. Sterilization of the air in the operating room by special bactericidal radiant energy: results of its use in extrapleural thoracoplasties. J Thorac Surg. 1936;6:45–81. [Google Scholar]
- 46.Hart D. Bactericidal ultraviolet radiation in the operating room: twenty-nine-year study for control of infections. JAMA. 1960;172:1019–28. doi: 10.1001/jama.1960.03020100027006. [DOI] [PubMed] [Google Scholar]
- 47.Overholt RH, Betts RH. A comparative report on infection of thoracoplasty wounds: experiences with ultraviolet irradiation of operating room air. J Thorac Surg. 1940;9:520–9. [Google Scholar]
- 48.Kraissl CJ, Cimiotti JG, Meleney FL. Considerations in the use of ultraviolet radiation in operating rooms. Ann Surg. 1940;111:161–85. doi: 10.1097/00000658-194002000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Woodhall B, Neill RG, Dratz HM. Ultraviolet radiation as an adjunct in the control of postoperative neurosurgical infection. II clinical experience 1938–1948. Ann Surg. 1949;129:820–4. [PMC free article] [PubMed] [Google Scholar]
- 50.Goldner JL, Moggio M, Beissinger SF, McCollum DE. Ultraviolet light for the control of airborne bacteria in the operating room. Ann N Y Acad Sci. 1980;353:271–84. doi: 10.1111/j.1749-6632.1980.tb18930.x. [DOI] [PubMed] [Google Scholar]
- 51.Lowell JD, Kundsin RB, Schwartz CM, Pozin D. Ultraviolet radiation and reduction of deep wound infection following hip and knee arthroplasty. Ann N Y Acad Sci. 1980;353:285–93. doi: 10.1111/j.1749-6632.1980.tb18931.x. [DOI] [PubMed] [Google Scholar]
- 52.Del Mundo FD, McKhann CF. Effect of ultraviolet irradiation of air on incidence of infections in an infants' hospital. Am J Dis Child. 1941;61:213–25. [Google Scholar]
- 53.Robertson EC, Doyle ME, Tisdall FF, Koller LR, Ward FS. Air contamination and air sterilization. Am J Dis Child. 1939;58:1023–38. [Google Scholar]
- 54.Sommer HE, Stokes J., Jr. Studies on air-borne infection in a hospital ward: I. The effect of ultra-violet light on cross-infection in an infants' ward. J Pediatr. 1942;21:569–76. [Google Scholar]
- 55.Henle W, Sommer HE, Stokes J., Jr. Studies on air-borne infection in a hospital ward: II. Effects of ultraviolet irradiation and propylene glycol vaporization upon the prevention of experimental air-borne infection of mice by droplet nuclei. J Pediatr. 1942;21:577–90. [Google Scholar]
- 56.Sauer LW, Minsk LD, Rosenstern I. Control of cross infections of the respiratory tract in a nursery for young infants: a preliminary report. JAMA. 1942;118:1271–4. [Google Scholar]
- 57.Robertson EC, Doyle ME, Tisdall FF. Use of ultraviolet radiation in reduction of respiratory cross infections in a children's hospital: final report. JAMA. 1943;121:908–14. [Google Scholar]
- 58.Rosenstern I. Control of air-borne infections in a nursery for young infants. Am J Dis Child. 1948;75:193–202. doi: 10.1001/archpedi.1948.02030020204004. [DOI] [PubMed] [Google Scholar]
- 59.Barenberg LH, Greene D, Greenspan L, Greenberg B. Effect of irradiation of air in a ward on the incidence of infections of the respiratory tract: with a note on varicella. In: Moulton FR, editor. Aerobiology. Washington: Publication of the American Association for the Advancement of Science No. 17; 1942. pp. p. 233–6. American Association for the Advancement of Science. [Google Scholar]
- 60.Higgons RA, Hyde GM. Effect of ultraviolet air sterilization upon incidence of respiratory infections in a children's institution: a six-year study. N Y State J Med. 1947;47:707–10. [PubMed] [Google Scholar]
- 61.Wells WF, Wells MW, Wilder TS. The environmental control of epidemic contagion I: an epidemiologic study of radiant disinfection of air in day schools. Am J Hyg. 1942;35:97–121. [Google Scholar]
- 62.Wells WF. Airborne contagion and air hygiene: an ecological study of droplet infections. Cambridge (MA): Harvard University Press; 1955. [Google Scholar]
- 63.Council on Physical Therapy. Acceptance of ultraviolet lamps for disinfecting purposes. JAMA. 1943;122:503–5. [Google Scholar]
- 64.Lurie MB. Experimental epidemiology of tuberculosis: the prevention of natural air-borne contagion of tuberculosis in rabbits by ultraviolet irradiation. J Exp Med. 1944;79:559–72. doi: 10.1084/jem.79.6.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wheeler SM, Ingraham HS, Hollaender A, Lill ND, Gershon-Cohen J, Brown EW. Ultra-violet light control of air-borne infections in a naval training center: preliminary report. Am J Public Health Nations Health. 1945;35:457–68. doi: 10.2105/ajph.35.5.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Miller WR, Jarrett ET, Willmon TL, Hollaender A, Brown EW, Lewandowski T, et al. Evaluation of ultraviolet radiation and dust control measures in control of respiratory disease at a naval training center. J Infect Dis. 1948;82:86–100. doi: 10.1093/infdis/82.1.86. [DOI] [PubMed] [Google Scholar]
- 67.Willmon TL, Hollaender A, Langmuir AD. Studies of the control of acute respiratory diseases among naval recruits: I. A review of a four-year experience with ultraviolet irradiation and dust suppressive measures, 1943–1947. Am J Hyg. 1948;48:227–32. doi: 10.1093/oxfordjournals.aje.a119237. [DOI] [PubMed] [Google Scholar]
- 68.Jarrett ET, Zelle MR, Hollaender A. Studies of the control of acute reparatory disease among naval recruits: II. Limitations of ultraviolet irradiation in reducing air-borne bacteria in barracks with low ceilings. Am J Hyg. 1948;48:233–9. doi: 10.1093/oxfordjournals.aje.a119238. [DOI] [PubMed] [Google Scholar]
- 69.Langmuir AD, Jarrett ET, Hollaender A. Studies of the control of acute respiratory diseases among naval recruits: III. The epidemiological pattern and the effect of ultraviolet irradiation during the winter of 1946–1947. Am J Hyg. 1948;48:240–51. doi: 10.1093/oxfordjournals.aje.a119239. [DOI] [PubMed] [Google Scholar]
- 70.Whisler BA. The efficacy of ultra-violet light sources in killing bacteria suspended in air. Iowa State Coll J Sci. 1940;14:215–31. [Google Scholar]
- 71.Wells WF, Wells MW. Air-borne infection: sanitary control. JAMA. 1936;107:1805–9. [Google Scholar]
- 72.Wells WF. Bactericidal irradiation of air: part I. Physical factors. J Franklin Inst. 1940;229:347–72. doi: 10.1016/0016-0032(45)90534-5. [DOI] [PubMed] [Google Scholar]
- 73.Wells WF. Ray length in sanitary ventilation by bactericidal irradiation of air. J Franklin Inst. 1944;238:185–93. doi: 10.1016/0016-0032(45)90534-5. [DOI] [PubMed] [Google Scholar]
- 74.Wells WF. Circulation in sanitary ventilation by bactericidal irradiation of air. J Franklin Inst. 1945;240:379–95. doi: 10.1016/0016-0032(45)90534-5. [DOI] [PubMed] [Google Scholar]
- 75.Luckiesh M. Applications of germicidal, erythemal, and infrared energy. New York: D. Van Nostrand Company; 1946. [Google Scholar]
- 76.Harstad JB, Decker HM, Wedum AG. Use of ultraviolet irradiation in a room air conditioner for removal of bacteria. Appl Microbiol. 1954;2:148–51. doi: 10.1128/am.2.3.148-151.1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Miller OT, Schmitt RF, Phillips GB. Applications of germicidal ultraviolet in infectious disease laboratories: I. Sterilization of small volumes of air by ultraviolet irradiation. Am J Public Health Nations Health. 1955;45:1420–3. doi: 10.2105/ajph.45.11.1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nardell EA. Transmission and safety issues. In: Friedman LN, editor. Tuberculosis: current concepts and treatment. Boca Raton (FL): CRC Press; 1994. pp. p. 53–70. [Google Scholar]
- 79.Riley RL, O'Grady F. Airborne infection: transmission and control. New York: The Macmillan Company; 1961. [Google Scholar]
- 80.Riley RL, Wells WF, Mills CC, Nyka W, McLean RL. Air hygiene in tuberculosis: quantitative studies of infectivity and control in a pilot ward. Am Rev Tuberc. 1957;75:420–31. doi: 10.1164/artpd.1957.75.3.420. [DOI] [PubMed] [Google Scholar]
- 81.Riley RL, Mills CC, Nyka W, Weinstock N, Storey PB, Sultan LU, et al. Aerial dissemination of pulmonary tuberculosis: a two-year study of contagion in a tuberculosis ward. Am J Hyg. 1959;70:185–96. [Google Scholar]
- 82.Riley RL, Mills CC, O'Grady F, Sultan LU, Wittstadt F, Shivpuri DN. Infectiousness of air from a tuberculosis ward. Ultraviolet irradiation of infected air: comparative infectiousness of different patients. Am Rev Respir Dis. 1962;85:511–25. doi: 10.1164/arrd.1962.85.4.511. [DOI] [PubMed] [Google Scholar]
- 83.McLean RL. The mechanism of spread of Asian influenza: general discussion. Am Rev Respir Dis. 1961;83:36–8. doi: 10.1164/arrd.1961.83.2P2.29. (2 Pt 2) [DOI] [PubMed] [Google Scholar]
- 84.Riley RL, Permutt S. Room air disinfection by ultraviolet irradiation of upper air: air mixing and germicidal effectiveness. Arch Environ Health. 1971;22:208–19. doi: 10.1080/00039896.1971.10665834. [DOI] [PubMed] [Google Scholar]
- 85.Riley RL, Permutt S, Kaufman JE. Convection, air mixing, and ultraviolet air disinfection in rooms. Arch Environ Health. 1971;22:200–7. doi: 10.1080/00039896.1971.10665833. [DOI] [PubMed] [Google Scholar]
- 86.Riley RL, Permutt S, Kaufman JE. Room air disinfection by ultraviolet irradiation of upper air: further analysis of convective air exchange. Arch Environ Health. 1971;23:35–9. doi: 10.1080/00039896.1971.10665951. [DOI] [PubMed] [Google Scholar]
- 87.Riley RL, Kaufman JE. Air disinfection in corridors by upper air irradiation with ultraviolet. Arch Environ Health. 1971;22:551–3. doi: 10.1080/00039896.1971.10665899. [DOI] [PubMed] [Google Scholar]
- 88.Riley RL, Kaufman JE. Effect of relative humidity on the inactivation of airborne Serratia marcescens by ultraviolet radiation. Appl Microbiol. 1972;23:1113–20. doi: 10.1128/am.23.6.1113-1120.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kethley TW, Branch K. Ultraviolet lamps for room air disinfection: effect of sampling location and particle size of bacterial aerosol. Arch Environ Health. 1972;25:205–14. doi: 10.1080/00039896.1972.10666162. [DOI] [PubMed] [Google Scholar]
- 90.Riley RL, Knight M, Middlebrook G. Ultraviolet susceptibility of BCG and virulent tubercle bacilli. Am Rev Respir Dis. 1976;113:413–8. doi: 10.1164/arrd.1976.113.4.413. [DOI] [PubMed] [Google Scholar]
- 91.Riley RL, Nardell EA. Clearing the air: the theory and application of ultraviolet air disinfection. Am Rev Repir Dis. 1989;139:1286–94. doi: 10.1164/ajrccm/139.5.1286. [DOI] [PubMed] [Google Scholar]
- 92.Wells MW. Ventilation in the spread of chickenpox and measles within school rooms. JAMA. 1945;129:197–200. [Google Scholar]
- 93.Perkins JE, Bahlke AM, Silverman HF. Effect of ultra-violet irradiation of classrooms on spread of measles in large rural central schools: preliminary report. Am J Public Health Nations Health. 1947;37:529–37. [PMC free article] [PubMed] [Google Scholar]
- 94.Wells MW, Holla WA. Ventilation in the flow of measles and chickenpox through a community: progress report, Jan. 1, 1946 to June 15, 1949, Airborne Infection Study, Westchester County Department of Health. JAMA. 1950;142:1337–44. doi: 10.1001/jama.1950.02910350007004. [DOI] [PubMed] [Google Scholar]
- 95.Air disinfection with ultra-violet irradiation: its effect on illness among school-children. Spec Rep Ser Med Res Counc (G B) 1954;283:1–88. [PubMed] [Google Scholar]
- 96.Brooks GL, Wilson U, Blackfan KD. Studies of cross-infection in the infants' hospital in Boston. In: Moulton FR, editor. Aerobiology. Washington: AAAS; 1942. pp. p. 228–32. Publication of the American Association for the Advancement of Science, No. 17. [Google Scholar]
- 97.Schneiter R, Hollaender A, Caminita BH, Kolb RW, Fraser HF, duBuy HG, et al. Effectiveness of ultraviolet irradiation of upper air for the control of bacterial air contamination in sleeping quarters. Preliminary report. Am J Hyg. 1944;40:136–53. [Google Scholar]
- 98.duBuy HG, Dunn JE, Brackett FS, Dreessen WC, Neal PA, Posner I. An evaluation of ultraviolet radiation of sleeping quarters as supplement of accepted methods of disease control. Am J Hyg. 1948;48:207–26. doi: 10.1093/oxfordjournals.aje.a119236. [DOI] [PubMed] [Google Scholar]
- 99.Bahlke AM, Silverman HF, Ingraham HS. Effect of ultra-violet irradiation of classrooms on spread of mumps and chickenpox in large rural central schools: progress report. Am J Public Health Nations Health. 1949;39:1321–30. doi: 10.2105/ajph.39.10.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kingston D, Lidwell OM, Williams RE. The epidemiology of the common cold: III. The effect of ventilation, air disinfection and room size. J Hyg (Lond) 1962;60:341–52. doi: 10.1017/s0022172400020453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.McAdam JM, Brickner PW, Scharer LL, Crocco JA, Duff AE. The spectrum of tuberculosis in a New York City men's shelter clinic (1982–1988) Chest. 1990;97:798–805. doi: 10.1378/chest.97.4.798. [DOI] [PubMed] [Google Scholar]
- 102.Porter JD, McAdam KP. The re-emergence of tuberculosis. Annu Rev Public Health. 1994;15:303–23. doi: 10.1146/annurev.pu.15.050194.001511. [DOI] [PubMed] [Google Scholar]
- 103.Vincent RL. Airborne disease control: measurement of ultraviolet germicidal irradiation (UVR) in high-risk environments. In: Matthes R, Sliney D, editors. Measurements of optical radiation hazards (ICNIRP 6/98; CIE x016-1998) München: Märkl-Druck; 1998. pp. p. 369–86. [Google Scholar]
- 104.Nardell EA. Ultraviolet air disinfection to control tuberculosis in a shelter for the homeless. In: Kundsin RB, editor. Architectural design and indoor microbial pollution. New York: Oxford University Press; 1988. pp. p. 296–308. [Google Scholar]
- 105.Iseman MD. A leap of faith: what can we do to curtail intrainstitutional transmission of tuberculosis? Ann Intern Med. 1992;117:251–3. doi: 10.7326/0003-4819-117-3-251. [DOI] [PubMed] [Google Scholar]
- 106.Nardell EA. Environmental control of tuberculosis. Med Clin North Am. 1993;77:1315–34. doi: 10.1016/s0025-7125(16)30196-1. [DOI] [PubMed] [Google Scholar]
- 107.Riley RL, Nardell EA. Plant, technology & safety management series: controlling occupational exposures to tuberculosis. Oakbrook Terrace (IL): The Joint Commission; 1993. Controlling transmission of tuberculosis in health care facilities: ventilation, filtration, and ultraviolet air disinfection; pp. p. 25–31. [Google Scholar]
- 108.Nardell EA. Interrupting transmission from patients with unsuspected tuberculosis: a unique role for upper-room ultraviolet air disinfection. Am J Infect Control. 1995;23:156–64. doi: 10.1016/0196-6553(95)90261-9. [DOI] [PubMed] [Google Scholar]
- 109.Stead WW, Yeung C, Hartnett C. Probable role of ultraviolet irradiation in preventing transmission of tuberculosis: a case study. Infect Control Hosp Epidemiol. 1996;17:11–3. doi: 10.1086/647182. [DOI] [PubMed] [Google Scholar]
- 110.Ko G, First MW, Burge HA. Influence of relative humidity on particle size and UV sensitivity of Serratia marcescens and Mycobacterium bovis BCG aerosols. Tuber Lung Dis. 2000;80:217–28. doi: 10.1054/tuld.2000.0249. [DOI] [PubMed] [Google Scholar]
- 111.Miller SL, Macher JM. Evaluation of a methodology for quantifying the effect of room air ultraviolet germicidal irradiation on airborne bacteria. Aerosol Sci Technol. 2000;33:274–95. [Google Scholar]
- 112.Peccia J, Werth HM, Miller S, Hernandez M. Effects of relative humidity on the ultraviolet induced inactivation of airborne bacteria. Aerosol Sci Technol. 2001;35:728–40. [Google Scholar]
- 113.Peccia J, Hernandez M. Photoreactivation in airborne Mycobacterium parafortuitum. Appl Environ Microbiol. 2001;67:4225–32. doi: 10.1128/AEM.67.9.4225-4232.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ko G, First MW, Burge HA. The characterization of upper-room ultraviolet germicidal irradiation in inactivating airborne microorganisms. Environ Health Perspec. 2002;110:95–101. doi: 10.1289/ehp.0211095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Miller SL, Hernandez M, Fennelly K, Martyny J, Macher J, Kujundzic E, et al. Efficacy of ultraviolet irradiation in controlling the spread of tuberculosis. Atlanta: Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health (US); 2002. NIOSH Contract No.: 200-97-2602. [Google Scholar]
- 116.Xu P, Peccia J, Fabian P, Martyny JW, Fennelly KP, Hernandez M, et al. Efficacy of ultraviolet germicidal irradiation of upper-room air in inactivating airborne bacterial spores and mycobacteria in full-scale studies. Atmos Environ. 2003;37:405–19. [Google Scholar]
- 117.Lai KM, Burge HA, First MW. Size and UV germicidal irradiation susceptibility of Serratia marcescens when aerosolized from different suspending media. Appl Environ Microbiol. 2004;70:2021–7. doi: 10.1128/AEM.70.4.2021-2027.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Xu P, Kujundzic E, Peccia J, Schafer MP, Moss G, Hernandez M, et al. Impact of environmental factors on efficacy of upper-room air ultraviolet germicidal irradiation for inactivating airborne mycobacteria. Environ Sci Technol. 2005;39:9656–64. doi: 10.1021/es0504892. [DOI] [PubMed] [Google Scholar]
- 119.Kujundzic E, Hernandez M, Miller SL. Ultraviolet germicidal irradiation inactivation of airborne fungal spores and bacteria in upper-room air and HVAC in-duct configurations. J Environ Eng Sci. 2007;6:1–9. [Google Scholar]
- 120.First M, Rudnick SN, Banahan KF, Vincent RL, Brickner PW. Fundamental factors affecting upper-room ultraviolet germicidal irradiation—part I. Experimental. J Occup Environ Hyg. 2007;4:321–31. doi: 10.1080/15459620701271693. [DOI] [PubMed] [Google Scholar]
- 121.McDevitt JJ, Milton DK, Rudnick SN, First MW. Inactivation of poxviruses by upper-room UVC light in a simulated hospital room environment. PLoS One. 2008;3:e3186. doi: 10.1371/journal.pone.0003186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Dumyahn T, First M. Characterization of ultraviolet upper room air disinfection devices. Am Ind Hyg Assoc J. 1999;60:219–27. [Google Scholar]
- 123.Kowalski WJ, Bahnfleth WP, Witham DL, Severin BF, Whittam TS. Mathematical modeling of ultraviolet germicidal irradiation for air disinfection. Quant Microbiol. 2000;2:249–70. [Google Scholar]
- 124.Rudnick SN. Predicting the ultraviolet radiation distribution in a room with multilouvered germicidal fixtures. AIHAJ. 2001;62:434–45. doi: 10.1080/15298660108984645. [DOI] [PubMed] [Google Scholar]
- 125.Gammaitoni L, Nucci MC. Using a mathematical model to evaluate the efficacy of TB control measures. Emerg Infect Dis. 1997;3:335–42. doi: 10.3201/eid0303.970310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Nicas M, Miller SL. A multi-zone model evaluation of the efficacy of upper-room air ultraviolet germicidal irradiation. Appl Occup Environ Hyg. 1999;14:317–28. doi: 10.1080/104732299302909. [DOI] [PubMed] [Google Scholar]
- 127.Kowalski WJ, Bahnfleth WP. Effective UVGI system design through improved modeling. ASHRAE Trans. 2000;106(Pt 2):1–10. [Google Scholar]
- 128.Ko G, Burge HA, Nardell EA, Thompson KM. Estimation of tuberculosis risk and incidence under upper room ultraviolet germicidal irradiation in a waiting room in a hypothetical scenario. Risk Anal. 2001;21:657–73. doi: 10.1111/0272-4332.214142. [DOI] [PubMed] [Google Scholar]
- 129.Beggs CB, Sleigh PA. A quantitative method for evaluating the germicidal effect of upper room UV fields. J Aerosol Sci. 2002;33:1681–99. [Google Scholar]
- 130.Kowalski WJ, Bahnfleth WP, Rosenberger JL. Dimensional analysis of UVGI air disinfection systems. HVAC&R Res. 2003;9:347–63. [Google Scholar]
- 131.Beggs CB, Noakes CJ, Sleigh PA, Fletcher LA, Kerr KG. Methodology for determining the susceptibility of airborne microorganisms to irradiation by an upper-room UVGI system. J Aerosol Sci. 2006;37:885–902. [Google Scholar]
- 132.Rudnick SN, First MW. Fundamental factors affecting upper-room ultraviolet germicidal irradiation—part II. Predicting effectiveness. J Occup Environ Hyg. 2007;4:352–62. doi: 10.1080/15459620701298167. [DOI] [PubMed] [Google Scholar]
- 133.Chang D, Young C. Effect of turbulence on ultraviolet germicidal irradiation. J Archit Eng. 2007;13:152–61. [Google Scholar]
- 134.Memarzedeh F. Assessing the efficacy of ultraviolet germicidal irradiation and ventilation in removing Mycobacterium tuberculosis. Bethesda: National Institutes of Health; 2000. [Google Scholar]
- 135.Alani A, Barton IE, Seymour MJ, Wrobel LC. Application of Lagrangian particle transport model to tuberculosis (TB) bacteria UV dosing in a ventilated room. Int J Environ Health Res. 2001;11:219–28. doi: 10.1080/09603120020047000. [DOI] [PubMed] [Google Scholar]
- 136.Noakes CJ, Fletcher LA, Beggs CB, Sleigh PA, Kerr KG. Development of a numerical model to simulate the biological inactivation of airborne microorganisms in the presence of ultraviolet light. J Aerosol Sci. 2004;35:489–507. [Google Scholar]
- 137.Noakes CJ, Beggs CB, Sleigh PA. Modelling the performance of upper room ultraviolet germicidal irradiation devices in ventilated rooms: comparison of analytical and CFD methods. Indoor Built Environ. 2004;13:477–88. [Google Scholar]
- 138.Noakes CJ, Sleigh PA, Fletcher LA, Beggs CB. Use of CFD modeling to optimize the design of upper-room UVGI disinfection systems for ventilated rooms. Indoor Built Environ. 2006;15:347–56. [Google Scholar]
- 139.Macher JM, Alevantis LE, Chang Y-L, Liu K-S. Effect of ultraviolet germicidal lamps on airborne microorganisms in an outpatient waiting room. Appl Occup Environ Hyg. 1992;7:505–13. [Google Scholar]
- 140.Macher JM, Alevantis LE, Chang Y-L, Liu K-S. Effect of ultraviolet germicidal lamps on airborne microorganisms in an outpatient waiting room [letter] Appl Occup Environ Hyg. 1994;9:462. [Google Scholar]
- 141.Bernstein JA, Bobbitt RC, Levin L, Floyd R, Crandall MS, Shalwitz RA, et al. Health effects of ultraviolet irradiation in asthmatic children's homes. J Asthma. 2006;43:255–62. doi: 10.1080/02770900600616887. [DOI] [PubMed] [Google Scholar]
- 142.First MW, Banahan KF, Dumyahn TS. Performance of ultraviolet germicidal irradiation lamps and luminaires in long-term service. LEUKOS. 2007;3:181–8. [Google Scholar]
- 143.Rahn RO, Xu P, Miller SL. Dosimetry of room-air germicidal (254 nm) radiation using spherical actinometry. Photochem Photobiol. 1999;70:314–8. [PubMed] [Google Scholar]
- 144.Schafer MP, Kujundzic E, Moss CE, Miller SL. Method for estimating ultraviolet germicidal fluence rates in a hospital room. Infect Control Hosp Epidemiol. 2008;29:1042–7. doi: 10.1086/591856. [DOI] [PubMed] [Google Scholar]
- 145.Reed NG, Wengraitis S, Sliney DH. Intercomparison of instruments used for safety and performance measurements of ultraviolet germicidal irradiation lamps. J Occup Environ Hyg. 2009;6:289–97. doi: 10.1080/15459620902801041. [DOI] [PubMed] [Google Scholar]
- 146.First MW, Weker RA, Yasui S, Nardell EA. Monitoring human exposures to upper-room germicidal ultraviolet irradiation. J Occup Environ Hyg. 2005;2:285–92. doi: 10.1080/15459620590952224. [DOI] [PubMed] [Google Scholar]
- 147.Nardell EA, Bucher SJ, Brickner PW, Wang C, Vincent RL, Becan-McBride K, et al. Safety of upper-room ultraviolet germicidal air disinfection for room occupants: results from the Tuberculosis Ultraviolet Shelter Study. Public Health Rep. 2008;123:52–60. doi: 10.1177/003335490812300108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Commission Internationale de l'Eclairage. Technical report: ultraviolet air disinfection. Vienna: CIE; 2003. CIE 155/2003. [Google Scholar]
- 149.Lidwell OM. Ultraviolet radiation and the control of airborne contamination in the operating room. J Hosp Infect. 1994;28:245–8. doi: 10.1016/0195-6701(94)90088-4. [DOI] [PubMed] [Google Scholar]
- 150.Ritter MA, Olberding EM, Malinzak RA. Ultraviolet lighting during orthopaedic surgery and the rate of infection. J Bone Joint Surg Am. 2007;89:1935–40. doi: 10.2106/JBJS.F.01037. [DOI] [PubMed] [Google Scholar]
- 151.Brickner PW, Vincent RL, Nardell EA, Pilek C, Chaisson WT, First M, et al. Ultraviolet upper room air disinfection for tuberculosis control: an epidemiological trial. J Healthcare Saf Compliance Infect Control. 2000;4:123–31. [Google Scholar]
- 152.First MW, Nardell NA, Chaisson W, Riley R. Guidelines for the application of upper-room ultraviolet germicidal irradiation for preventing transmission of airborne contagion—part I: basic principles. ASHRAE Transactions. 1999;105:869–76. [Google Scholar]
- 153.First MW, Nardell NA, Chaisson W, Riley R. Guidelines for the application of upper-room ultraviolet germicidal irradiation for preventing transmission of airborne contagion—part II: design and operation guidance. ASHRAE Transactions. 1999;105:877–87. [Google Scholar]
- 154.Kowalski WJ, Bahnfleth WP. Proposed standards and guidelines for UVGI air disinfection. IUVA News. 2004;6:20–5. [Google Scholar]
- 155.Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. MMWR Recomm Rep. 2005;54(RR-17):1–141. [PubMed] [Google Scholar]
- 156.Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care facilities, 1994. MMWR Recomm Rep. 1994;43(RR-13):1–132. [PubMed] [Google Scholar]
- 157.Centers for Disease Control and Prevention (US) Environmental control for tuberculosis: basic upper-room ultraviolet germicidal irradiation guidelines for healthcare settings. Atlanta: CDC, National Institute for Occupational Safety and Health (US); 2009. DHHS (NIOSH) Publication No. 2009-105. [Google Scholar]
- 158.Escombe AR, Moore DAJ, Gilman RH, Navincopa M, Ticona E, Mitchell B, et al. Upper-room ultraviolet light and negative air ionization to prevent tuberculosis transmission. PLoS Med. 2009;6:e43. doi: 10.1371/journal.pmed.1000043. [DOI] [PMC free article] [PubMed] [Google Scholar]