SYNOPSIS
Objective
We assessed health status and behavioral risks in American Indians (AIs) from rural, northern plains reservation communities.
Methods
AI interviewers from the communities administered the core and optional modules of the Behavioral Risk Factor Surveillance System (BRFSS) to 404 AI adults randomly selected from housing lists from four AI tribal communities located on the northern plains of the U.S. The BRFSS interview assessed several health functioning areas including medical conditions, preventive screenings, and behavioral risks. We measured health disparities by comparing the AI sample data with a northern plains statewide (North Dakota) sample and a U.S. national sample. We compared outcomes with BRFSS statewide (North Dakota) and U.S. national data from telephone-based interviews.
Results
AI participants showed a significantly greater prevalence of diabetes, coronary heart disease, myocardial infarction, smoking, obesity, and heavy alcohol use than either the regional or national samples. They also reported being less likely to engage in leisure-time physical activity and to have had age-appropriate preventive screenings for several diseases including colorectal cancer, prostate cancer, breast cancer, and cardiovascular disease.
Conclusions
Face-to-face interviews conducted by AI community members are an effective means of gathering health information about AIs living in rural, reservation communities. AIs living in these communities on the northern plains have a much higher prevalence of many health-risk behaviors and some medical conditions than are found in the general population. Improved health-care access, better preventive screenings, and culturally appropriate community-based health promotion programs and policies should be examined as possible ways to reduce health disparities.
Ethnic minority populations in the United States often experience disparities in health outcomes, access to health care, and quality of health-care services received.1,2 Reducing and eliminating health disparities are priority goals of U.S. health improvement initiatives such as Healthy People 2010;3 however, substantial health disparities remain. The existence of health disparities in ethnic subpopulations most certainly reflects the greater socioeconomic disparities for many ethnic minorities in the U.S., but are likely also due to complex interacting biological, social, psychological, and cultural factors that are often poorly understood and unique within different ethnic subpopulations.4
There are significant gaps in the identification, description, and understanding of health disparities among American Indians (AIs).5 National data do show that AIs have a lower life expectancy than other Americans.6 In fact, AIs die at higher rates than white Americans and most other ethnic minorities from cardiovascular disease (CVD), tuberculosis, alcoholism-related diseases, motor vehicle crashes, diabetes, unintentional injuries, homicide, and suicide.7–9 Moreover, there have been reports of higher rates of various diseases including asthma, diabetes, some cancers, CVD, and rheumatic diseases in at least some AI populations.10–15
Improving health outcomes and reducing health disparities necessitate addressing the major behavioral risk factors for chronic diseases: smoking, poor diet, physical inactivity, and excessive alcohol use.16,17 National data show that AIs have a higher prevalence of many risk behaviors including cigarette smoking, obesity, absence of leisure-time physical activity (LTPA), and binge alcohol use.18–22 Furthermore, research among specific AI populations indicated that these groups are more likely to have unhealthy diets characterized by high fat content and inadequate servings of fruit and vegetables.23–26 Reducing health disparities requires increasing access to, and use of, preventive health services. Data show that AIs are less likely than white and most other ethnic populations to have received a variety of preventive services including cervical pap smears, mammograms, and cholesterol screenings.18–20,27,28
Reliably identifying, understanding, and alleviating health disparities in AIs may be especially difficult to address because of their relatively small numbers and because of the diversity within their population. AIs and Alaska Natives, typically grouped together in national surveys, represent less than 1% of the U.S. population and are the smallest of the racial categories used in the U.S. Census. The relatively small number of people identifying as AI decreases the likelihood of representation in national population-based surveys, such as the Centers for Disease Control and Prevention's (CDC's) Behavioral Risk Factor Surveillance System (BRFSS). AI participants will, if described at all, be lumped into an “other” racial/ethnic category.29 Unfortunately, this methodology often results in the need to combine data over multiple survey years to estimate reliable prevalences in many national studies.
Despite the relatively small size of the U.S. AI population, they are a diverse ethnic minority representing 562 federally recognized tribes.30 Additionally, numerous tribes have not been recognized by the U.S. government.31 These multiple tribal groups often have different histories, unique languages, and varied cultural traditions and practices; reside in all geographic regions of the U.S.; and show various degrees of assimilation into society. This diversity can lead to inaccuracies when health data are reported in aggregate for AIs and Alaska Natives from different regions. For example, the prevalence of cigarette smoking in southwest tribes has been reported to be less than one-half the prevalence found in northern plains tribes.19
Northern plains AI populations have shown greater health disparities and behavioral risks in some previous studies; however, most of these studies have combined responses from several years and/or were obtained using telephone-based survey procedures.12,19 Telephone-based survey procedures may underestimate behavioral risk factors and health problems because of selection bias, especially among poorer, more rural, and/or ethnic minority samples.32–34
This study describes disparities in selected health problems, preventive health screening procedures, and behavioral risk factors among a sample of AIs residing in rural tribal communities on the northern plains of the U.S. Congruent with the aims of CDC's initiative, Racial and Ethnic Approaches to Community Health (REACH) 2010,35 this study represents AIs living in ethnic communities and tribal/reservation areas. Hence, partnerships with tribal governments were formed and tribal housing lists were used to randomly select households for face-to-face, rather than telephone, interviews.
METHODS
Participants and sampling procedures
All AI tribal communities located, at least in part, in the state of North Dakota (ND) were approached and invited to be partners in the present study. The councils of four tribes agreed to participate, and the study was then approved by the Institutional Review Board of the University of North Dakota and the -appropriate governing committees and councils of the four participating tribes. The estimated AI adult population of the area surveyed was 13,061,36,37 thus requiring a sample size of 400 to obtain parameter estimates with a 95% confidence interval (CI) and a 5% error rate with a power of 0.80.
Housing officials from each participating tribal group provided lists of tribal members' addresses within their respective geographical areas (i.e., reservations or, in one case, an Indian Health Service area). These lists are constantly updated and maintained by tribal governments to provide information that is as accurate as possible regarding current residences of tribal members. We used stratified random sampling to select 125 household addresses from each of the four tribal communities. Only one adult in each household was eligible for inclusion in this study. Therefore, in households with more than one adult (i.e., all people living in the household who were aged 18 years or older), the adult with the most recent birthday was invited to participate. Members from each of the four participating tribal communities were trained as interviewers by senior researchers, and interviewing was completed between February and December 2004.
Interviewers administered a computer-assisted personal interview to survey participants (n=404), and $30 gift cards were given to participating households upon survey completion. If a selected participant declined to participate (n=10) or was unavailable after three attempts (n=86), we considered that household nonresponsive. Using the conservative method recommended by the Council of American Survey Research Organizations, the response rate was 80.8%.37
Survey instrument
The BRFSS Questionnaire was established by CDC in 1984 as a state-based system to gather information about behavioral health risks, preventive practices, and chronic disease and injury. Updated annually, the BRFSS consists of core sections and optional modules. The current study used the 2003 version of the survey administered in its entirety.38 Questionnaire Programming Language (QPL) software version 4.139 was used to format the BRFSS survey as a computer-assisted personal interview, which was then installed on laptop computers used by the interviewers.
Data analysis
We used SPSS® version 16.040 complex samples procedure to calculate prevalence estimates and associated 95% CIs. Comparison data were obtained for ND and the U.S. samples from CDC's Web-based, interactive BRFSS database.41 To make comparisons between the current AI samples and the ND and U.S. samples, prevalence estimates were age- and sex-adjusted to the 2000 Census. We employed direct standardization with different weights for men and women by six age categories (18–24, 25–34, 35–44, 45–54, 55–64, and ≥65 years).42,43 We used Pearson's Chi-square analyses to determine if prevalence rates between participants in the AI sample differed from those in the ND and U.S. samples. We examined gender differences within the AI sample using Pearson's Chi-square tests conducted on unadjusted prevalence data (i.e., raw survey data), as a preliminary t-test [t(402)=0.58, p=0.57] showed no mean age difference between AI female (mean = 40.1, standard deviation [SD] = 16.5) and male (mean = 40.9, SD=15.3) respondents.
RESULTS
Demographics
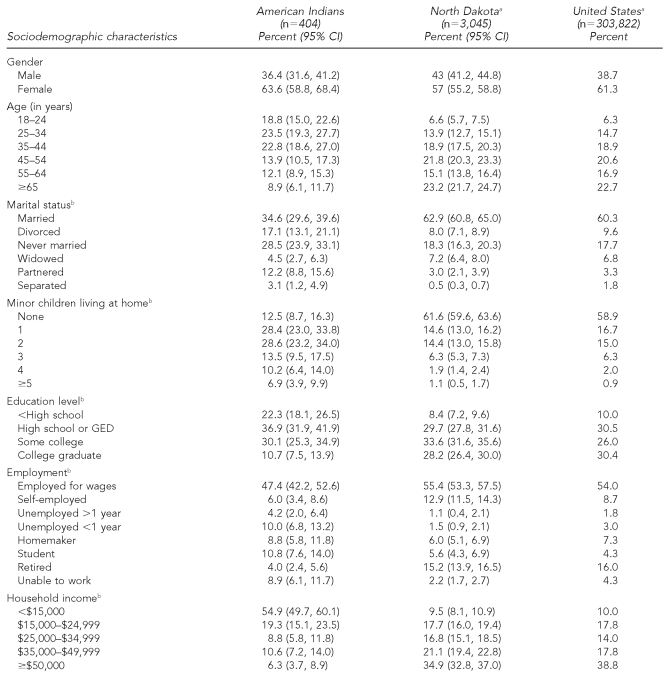
As shown in Table 1, 63.6% of the adults sampled were female, 65.4% were unmarried, 54.9% reported an annual income <$15,000, and 65.1% were aged 18–44 years. Most participants reported not having a college degree (89.3%) and most had children living in the home (87.5%). Approximately one-half of the participants were employed for wages or self-employed (53.4%). In contrast with the ND and U.S. samples, AI participants were more likely to be younger than 35 years of age (χ2=95.87, p<0.001, and χ2=110.50, p<0.001), unmarried (χ2=118.09, p<0.001, and χ2=110.82, p<0.001), unemployed (χ2=124.85, p<0.001, and χ2=76.33, p<0.001), living with minor children (χ2=350.61, p<0.001, and χ2=119.46, p<0.001), have not completed high school (χ2=76.03, p<0.001, and χ2=67.48, p<0.001), and have a household income <$15,000 (χ2=584.04, p<0.001, and χ2=901.02, p<0.001). In addition, women comprised a greater proportion of the AI sample than the ND sample (χ2=6.37, p<0.05) but not the U.S. sample (χ2=0.91, p=0.34).
Table 1.
Sociodemographic characteristics in a 2004 sample of American Indians compared with populations in North Dakota and the U.S.
aNorth Dakota and U.S. proportions presented are from weighted data available from the Centers for Disease Control and Prevention, with the exception of gender and age—which are from unweighted data—to be comparable with the same data from the American Indian sample.
bAmerican Indian sample data were adjusted for age and gender using direct standardization to the 2000 U.S. population.
CI = confidence interval
GED = general educational development
Behavioral risks
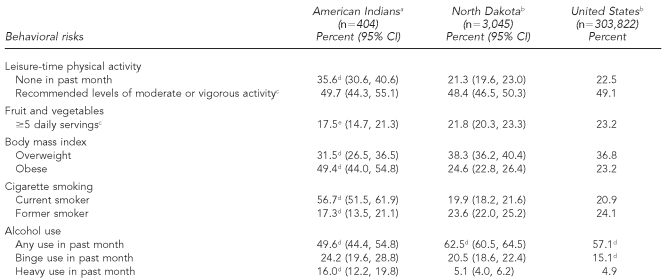
Participants in the AI sample were more likely than those in the ND or U.S. samples to be obese (χ2=110.95, p<0.001, and χ2=156.52, p<0.0001), smoke cigarettes (χ2=262.99, p<0.0001, and χ2=311.97, p<0.001), and not engage in LTPA (χ2=41.37, p<0.001, and χ2=39.95, p<0.001). However, they were less likely to be overweight (χ2=7.16, p<0.01, and χ2=4.99, p<0.05) and former smokers (χ2=7.00, p<0.01, and χ2=10.12, p<0.001). AI participants were less likely than those in the U.S. sample to eat five or more daily servings of fruit and vegetables (χ2=7.17, p<0.01), but the difference between AI and ND participants did not meet the p<0.05 level for statistical significance (χ2=3.81, p=0.051). Alcohol use was more complicated, as AI participants were less likely than those in the ND (χ2=25.30, p<0.001) or U.S. (χ2=9.50, p<0.01) samples to drink alcohol, but those who did were more likely to be heavy drinkers (i.e., at least three drinks/day for men and at least two drinks/day for women) (χ2=72.25, p<0.001, and χ2=108.10, p<0.001). The prevalence of binge drinking (i.e., consuming at least five drinks per occasion) was higher in the AI sample than in the U.S. sample (χ2=26.37, p<0.001), but was not different from that found in the ND sample (χ2=3.05, p=0.081). Table 2 provides details of these sample differences in behavioral risk factors.
Table 2.
Examining disparities in behavioral risks in a 2004 sample of American Indians compared with populations in North Dakota and the U.S.
aAmerican Indian sample data were adjusted for age and gender using direct standardization to the 2000 U.S. population.
bNorth Dakota and U.S. proportions presented are from the weighted data available from the Centers for Disease Control and Prevention.
cData from 2005 North Dakota (n=4,010) and U.S. (n=356,112) samples were substituted because data were not collected in 2004.
dProportions are significantly different from those in the same row (p<0.05) based on Chi-square analysis.
eThe American Indian sample proportion is significantly different (p<0.05) from the U.S. proportion, but not the North Dakota (ND) proportion (p>0.05), and the ND and U.S. proportions are not significantly different (p>0.05).
CI = confidence interval
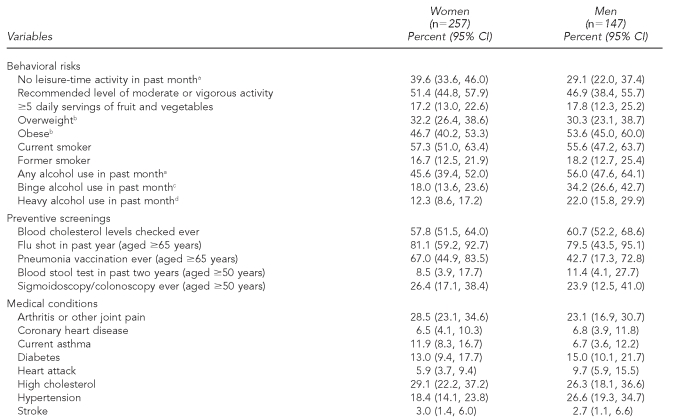
Chi-square analyses found significant gender differences within the AI sample for prevalence of LTPA (χ2=4.43, p<0.05), any alcohol use (χ2=3.94, p<0.05), binge drinking (χ2=13.41, p<0.001), and heavy drinking (χ2=7.34, p<0.01). As shown in Table 3, men were more likely than women to engage in all of these behaviors.
Table 3.
Examining disparities in behavioral risks, preventive screenings, and medical conditions between American Indian men and women, 2004
ap<0.05
bA body mass index (BMI) of 25.0–29.9 kilograms per meter squared (kg/m2) is considered overweight, and a BMI>30.0 kg/m2 is considered obese.
cp<0.001
dp<0.01
CI = confidence interval
Preventive screenings
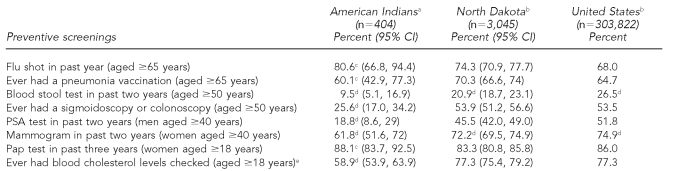
As shown in Table 4, comparisons among the AI, ND, and U.S. samples showed several significant differences in meeting age-appropriate screening recommendations. Participants aged 50 years and older in the AI sample were less likely to have taken a blood stool test in the past two years (χ2=7.77, p<0.01, and χ2=15.68, p<0.001) or ever to have had a sigmoidoscopy or colonoscopy than those in either the ND or U.S. samples (χ2=34.06, p<0.001, and χ2=35.64, p<0.001). Men aged 40 years and older in the AI sample were less likely than those in the ND (χ2=10.10, p<0.01) or U.S. (χ2=16.19, p<0.001) samples to have had a prostate-specific antigen (PSA) test. In addition, participants in the AI sample were less likely than those in the ND (χ2=64.64, p<0.001) or U.S. (χ2=77.69, p<0.001) samples to have ever had their blood cholesterol levels checked. Finally, fewer women aged 40 years and older in the AI sample than the ND (χ2=5.04, p<0.05) or U.S. (χ2=9.22, p<0.01) samples had a mammogram within the past two years. No significant gender differences for any of the preventive screening variables pertinent to both genders were found within the AI sample using Chi-square analyses (Table 3).
Table 4.
Examining disparities in preventive screenings in a 2004 sample of American Indians compared with North Dakota and U.S. data
aAmerican Indian sample data were adjusted for age and gender using direct standardization to the 2000 U.S. population.
bNorth Dakota and U.S. proportions presented are from the weighted data available from the Centers for Disease Control and Prevention.
cThe American Indian sample proportion was not significantly different (p>0.05) from either the North Dakota (ND) or U.S. proportions, but ND and U.S. proportions were significantly different (p<0.05).
dProportions are significantly different from those in the same row (p<0.05) based on Chi-square analysis.
eData from 2005 North Dakota (n=4,010) and U.S. (n=356,112) samples were substituted because data were not collected in 2004.
CI = confidence interval
PSA = prostate-specific antigen
Pap = Papanicolaou
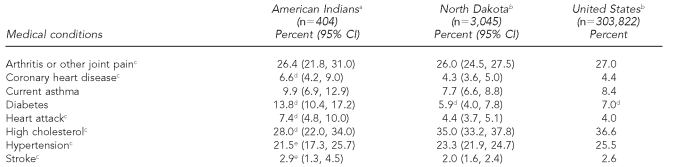
Medical conditions
Compared with participants in the ND and U.S. samples, AI participants were more likely to report being diagnosed with diabetes (χ2=35.37, p<0.001, and χ2=29.14, p<0.001), coronary heart disease (χ2=4.63, p<0.05, and χ2=5.00, p<0.05), and to have had a heart attack (χ2=7.21, p<0.01, and χ2=12.32, p<0.001). AI participants were also less likely to have been diagnosed with high cholesterol compared with the ND (χ2=7.85, p<0.01) and U.S. (χ2=7.80, p<0.01) samples. Table 5 provides prevalence data for these and other medical conditions for the AI, ND, and U.S. samples. Finally, no significant gender differences for any of the medical conditions were found within the AI sample using Chi-square analyses (Table 3).
Table 5.
Examining disparities in medical conditions in a 2004 sample of American Indians compared with North Dakota and U.S. data
aAmerican Indian sample data were adjusted for age and gender using direct standardization to the 2000 U.S. population.
bNorth Dakota and U.S. proportions presented are from the weighted data available from the Centers for Disease Control and Prevention.
cData from 2005 North Dakota (n=4,010) and U.S. (n=356,112) samples were substituted because data were not collected in 2004.
dProportions are significantly different from those in the same row (p<0.05) based on Chi-square analysis.
eThe American Indian sample proportion was not significantly different (p>0.05) from either the North Dakota (ND) or U.S. proportions, but ND and U.S. proportions were significantly different (p<0.05).
CI = confidence interval
DISCUSSION
This study is the first to use a face-to-face, personal interview conducted by AIs to gather information about the behavioral risks and health of AIs living in rural, reservation communities on the northern plains of the U.S. It adds to the growing literature emphasizing the persistence of health disparities in AIs.12,13,18 AI participants showed a significantly greater prevalence of diabetes, coronary heart disease, smoking, obesity, and heavy alcohol use than either regional (ND) or U.S. national samples. They also reported being less likely to engage in LTPA and to have had age-appropriate preventive screenings for several diseases, including colorectal cancer, prostate cancer, breast cancer, and CVD.
Limitations
These results must be considered in the context of certain limitations. First, the purpose of this study was to address health disparities in AIs residing in rural, northern plains, tribal communities and, as such, the results do not address health disparities among AIs living in non-reservation communities. Second, self-reported information can reflect various recall biases and a tendency toward socially acceptable/favorable answers; however, some studies have found self-report to be a reliable means of gathering data about the prevalence of some health concerns and behavioral risk factors assessed in this study (e.g., CVD, diabetes, hypertension, and cigarette smoking).44–46 In addition, gathering self-report information using face-to-face interviewing, such as used in this study, has been shown to be a more effective (i.e., higher response rate and perhaps a greater willingness to reveal negative information) method of interviewing rural, socioeconomically deprived participants and/or ethnic minority groups than telephone interviewing.32,47,48
Effective face-to-face interviewing, such as was conducted in this study, is not without limitations, including the costs and logistics associated with conducting in-person interviews. Other limitations include safety concerns related to motor vehicle travel and the necessity of approaching and potentially entering participants' homes. These concerns can often be mitigated and the costs can be managed in smaller studies when the circumstances clearly support the use of face-to-face interviews, but they can create insurmountable barriers to using face-to-face methods in larger-scale studies.
Behavioral risks
Tobacco use and obesity were dramatically higher in the AI sample than in the ND and U.S. samples. The high rate of smoking seen in the AI sample, contrasted with the much lower rates reported for AIs in the southwestern U.S.,18,21 illustrates the importance of considering regional variability when addressing behavioral risk and health disparities among AIs. Moreover, the prevalence of smoking in the AI sample was substantively higher than has been reported for AIs even in previous northern plains samples from South Dakota and Montana.21,49 This suggests that smoking persists among AIs living on the northern plains in stark contrast to the decreases observed in almost all demographic groups in all regions of the U.S. in the past 10 years. It appears that the preventive and cessation efforts that have been effective throughout the U.S. have shown little, if any, effect in at least some AI communities located on the northern plains. Several authors have suggested reducing smoking prevalence by using culturally appropriate efforts that include traditional AI concepts of wellness and address the historical role of tobacco in AI tribes;49–52 however, the effectiveness of such strategies has yet to be demonstrated.
Obesity prevalence, likened to an epidemic in the U.S.,53 was twice as prevalent in the AI sample as in either the ND or U.S. samples. Although previous research has often found greater rates of obesity among AIs than in the general population, the differences have not been as large as seen in this study, even in other northern plains samples.12,18,54,55 Our data suggest that the leveling off of the obesity epidemic recently noted in the general population56,57 may not have occurred in at least some rural AI communities. Obesity is an important risk factor in diabetes and CVD, two of the major causes of mortality in northern plains AIs. The high prevalence of obesity in northern plains AIs is not limited to adults but is also present in young children and has been implicated in the exponential increase in the type II diabetes rates of AI young people.58–60 Clearly, obesity prevention must become a top priority in attempts to reduce health disparities in rural, northern plains, AI communities.
LTPA was less prevalent in the AI sample (especially among women) than in either the ND or U.S. data. It also appears to be somewhat less prevalent than estimates from previous studies with AIs.19,50,61,62 However, most existing studies with AI samples have not focused on AIs from rural, northern plains communities, and barriers associated with rural areas, harsh winters, and poverty likely make the pursuit of LTPA more difficult. Nonetheless, the percentages of participants meeting recommended levels of physical activity were equivalent among the AI, ND, and U.S. samples. These data suggest a greater dichotomy in northern plains AIs, with individuals either meeting activity recommendations or being very sedentary with no LTPA at all. Therefore, health promotion efforts in northern plains, AI communities should focus on helping sedentary individuals develop more physically active lifestyles, perhaps by addressing personal and environmental barriers.
Compared with the ND and U.S. data, fewer AI participants reported eating the recommended number of daily servings of fruit and vegetables; however, the AI and ND samples were only marginally different (p=0.051), suggesting the importance of regional/geographical factors (e.g., fruit and vegetable availability). Although these data are generally consistent with previous studies of diet in AI communities,22–25 they go further by showing that inadequate consumption of fruit and vegetables is not limited to AIs but is also an issue in the general northern plains population. Increasing fruit and vegetable consumption in northern plains AIs should address barriers such as availability and cost that likely affect many northern plains communities.
Fewer people drank alcohol in the past month in the AI sample than in either the ND or U.S. samples. Although numerous studies have found that alcohol abuse is a prevalent behavioral risk factor in AI communities and that alcohol-related mortality is higher than in the general population,3,6,8,63–66 the present data suggest that at least some northern plains AI communities appear to have successfully reduced alcohol use among their members. However, those in the AI sample that did consume alcohol were more likely than those in the ND and U.S. samples to be heavy drinkers, and more likely than those in the U.S. sample to be binge drinkers. In addition, similar to general population surveys, men in the AI sample were more likely to drink heavily and to binge drink than women. These data are consistent with national data showing that excessive drinking, particularly binge drinking, is more prevalent in the northern plains than in any other region of the U.S.67 Programs addressing excessive drinking are clearly needed for the general population of the northern plains, and might be especially useful in AI communities where abstinence programs have shown some success but could be augmented by a focus on excessive alcohol use, rather than any alcohol use.
Preventive measures
Preventive screening procedures have shown to be an effective way to reduce morbidity and mortality.68,69 Unfortunately, ethnic minority groups including AIs often have lower rates for many preventive screening pro-cedures.19,27,69 Participants in the AI sample were less likely to have age-appropriate blood stool tests, colonoscopies or sigmoidoscopies, lipid panels or blood cholesterol tests, PSA tests, and mammograms. These data suggest glaring and troubling disparities in preventive health screenings between northern plains AIs and the general regional and national population. In the context of high, and in some cases increasing, rates of cancer and CVD in AIs,13,70 preventive screen-ing procedures are critical for earlier diagnoses of diseases among AIs in rural, northern plains, tribal communities. Increasing awareness of and access to preventive screening procedures for cancer and CVD is a critical means of reducing mortality and a necessary tool for eliminating health disparities.
Medical conditions
Past studies have reported several disparities in the prevalence and/or mortality associated with sev-eral diseases (e.g., cancers, CVD, diabetes, rheu-ma-toid arthritis, and asthma) in at least some AI pop-u-la-tions.10–15,18 Consistent with virtually all previous reports, a higher prevalence of diabetes was found in the AI sample compared with the ND and U.S. samples. CVD data were less clear. AI participants had a greater prevalence of coronary heart disease and heart attacks than in the ND and U.S. populations; however, they also reported a lower prevalence of high cholesterol and equivalent rates for strokes and hypertension. Relying on these prevalence estimates is complicated by the fact that, as discussed previously, age-appropriate preventive health screenings were lacking in the AI sample. For example, the lower prevalence of high cholesterol in the AI sample could be nothing more than a function of the fact that significantly fewer in the AI sample had ever had their cholesterol checked. The lower rate of hypertension in the AI sample might be similarly explained if we knew how many of the participants recently had their blood pressure measured. Finally, though higher rates of asthma and arthritis have been observed in some studies comparing AI groups with the general population,11,15 our data showed no differences among the AI, ND, and U.S. samples in the rates of either of these conditions.
Reducing health disparities in AIs
Clearly, diabetes and probably CVD reflect significant health disparities in northern plains AI communities. Furthermore, preventive screening procedures for various cancers and CVD are not being accessed and/or applied in accordance with age-appropriate guidelines in at least some rural, northern plains, AI communities. Remedies for these disparities may not be easy because of funding and provider staffing issues. For example, the Indian Health Service (IHS), the primary provider of health care to AI communities on the northern plains, has been estimated to operate with only 59% of what is needed to provide adequate care, and the federal government spends twice as much per capita on the health care of prisoners as it does on AIs and Alaska Natives.71 The availability of and access to appropriate health-care providers are also issues, as fewer than 90 physicians typically serve 100,000 AIs, compared with 229 per 100,000 people nationally.72 Additionally, IHS is experiencing critical shortages in many other health professions such as dentists, nurses, pharmacists, and optometrists.71
Our most striking finding was that all behavioral risks studied were higher in the AI sample, and some (e.g., current smoking and obesity) were markedly higher. These results indicate that public health prevention campaigns directed toward health promotion and disease prevention may not be effectively reaching AIs in rural, northern plains communities. Effectively changing behavioral risk factors in AI communities will likely require a community participatory approach that incorporates multiple intervention strategies, such as mass media and marketing, community and school programs, and policy/legal initiatives.
CONCLUSIONS
Health disparities in AI communities have persisted since Europeans arrived in the Americas more than 500 years ago.73 Current health disparities reflect an interaction of socioeconomic circumstances, physical and cultural community environments, personal -man-age-ment of health behaviors and medical concerns, and health-care financing and delivery.4 Efforts to reduce disparities in northern plains AI communities will likely continue to fail unless complex causal factors are addressed by integrated programs and policies. Comprehensively targeting the entire community via multiple methods—media campaigns, policies and legislation, school-based programs and curricula, health service provider education, and service delivery reform—will undoubtedly yield cost and health benefits for northern plains AI populations.
Acknowledgments
The authors thank the following individuals for their contributions: Dr. Steven Helgerson, Francine McDonald, Dr. Patrick Kerr, Louise Diers, Twyla Baker-Demaray, Shacarah Gagnon-Kvale, Patty Lambert, Sandra Poitra, Melany Trowbridge, Dr. Jessica White Plume, and Sierra Abe.
Footnotes
This project was funded by a grant from the Health Resources and Services Administration, U.S. Department of Health and Human Services.
REFERENCES
- 1.Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: confronting racial and ethnic disparities in health care. Washington: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Health Policy Institute of Ohio. Understanding health disparities. Columbus (OH): Health Policy Institute of Ohio; 2004. [Google Scholar]
- 3.Department of Health and Human Services (US) Healthy People 2010: understanding and improving health and objectives for improving health. 2nd ed. 2 volumes. Washington: U.S. Government Printing Office; 2000. [Google Scholar]
- 4.Meyers KSH. Racial and ethnic health disparities: influences, actors, and policy opportunities. Oakland (CA): Kaiser Permanente Institute for Health Policy; 2007. [Google Scholar]
- 5.Moy E, Smith CR, Johansson P, Andrews R. Gaps in data for American Indians and Alaska Natives in the national healthcare disparities report. Am Indian Alsk Native Ment Health Res. 2006;13:52–69. doi: 10.5820/aian.1301.2006.52. [DOI] [PubMed] [Google Scholar]
- 6.Indian Health Service (US). Facts on Indian health disparities. Rockville (MD): Department of Health and Human Services (US); 2006. [Google Scholar]
- 7.Grim CW. Health of American Indians and Alaska Natives: health influence factors in common with other indigenous populations. BMJ. 2003;3:242. [Google Scholar]
- 8.Indian Health Service (US). Trends in Indian health, 1998–99. Rockville (MD): Department of Health and Human Services (US); 2000. [Google Scholar]
- 9.Young TK. Recent health trends in the Native American population. Popul Res Policy Rev. 1997;16:147–67. [Google Scholar]
- 10.Diabetes prevalence among American Indians and Alaska Natives and the overall population—United States, 1994–2002. MMWR Morb Mortal Wkly Rep. 2003;52(30):702–4. [PubMed] [Google Scholar]
- 11.Ferucci ED, Templin DW, Lanier AP. Rheumatoid arthritis in American Indians and Alaska Natives: a review of the literature. Semin Arthritis Rheum. 2004;34:662–7. doi: 10.1016/j.semarthrit.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Harwell TS, Gohdes D, Moore K, McDowall JM, Smilie JG, Helgerson SD. Cardiovascular disease and risk factors in Montana American Indians and non-Indians. Am J Prev Med. 2001;20:196–201. doi: 10.1016/s0749-3797(00)00312-3. [DOI] [PubMed] [Google Scholar]
- 13.Harwell TS, Miller SH, Lemons DL, Helgerson SD, Gohdes D. Cancer incidence in Montana: rates for American Indians exceed those for whites. Am J Prev Med. 2006;30:493–7. doi: 10.1016/j.amepre.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 14.Howard BV, Lee ET, Cowan LD, Devereux RB, Galloway JM, Go OT, et al. Rising tide of cardiovascular disease in American Indians. The Strong Heart Study. Circulation. 1999;99:2389–95. doi: 10.1161/01.cir.99.18.2389. [DOI] [PubMed] [Google Scholar]
- 15.Meng YY, Babey SH, Malcolm E, Brown ER, Chawla N. Asthma in California: findings from the 2001 California Health Interview Survey. Los Angeles: UCLA Center for Health Policy Research; 2003. [Google Scholar]
- 16.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–45. doi: 10.1001/jama.291.10.1238. published erratum appears in JAMA 2005;293:293-4, 298. [DOI] [PubMed] [Google Scholar]
- 17.Denny CH, Holtzman D. Health behaviors of American Indians and Alaska Natives: findings from the Behavioral Risk Factor Surveillance System, 1993–1996. Atlanta: Centers for Disease Control and Prevention (US); 1999. [PubMed] [Google Scholar]
- 18.Denny CH, Holtzman D, Cobb N. Surveillance for health behaviors of American Indians and Alaska Natives: findings from the Behavioral Risk Factor Surveillance System, 1997–2000. MMWR Surveill Summ. 2003;52(SS-7):1–13. [PubMed] [Google Scholar]
- 19.Denny CH, Taylor TL. American Indian and Alaska Native health behavior: findings from the Behavioral Risk Factor Surveillance System, 1992–1995. Ethn Dis. 1999;9:403–9. [PubMed] [Google Scholar]
- 20.Will JC, Denny C, Serdula M, Muneta B. Trends in body weight among American Indians: findings from a telephone survey, 1985 through 1996. Am J Public Health. 1999;89:395–8. doi: 10.2105/ajph.89.3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Welty TK, Lee ET, Yeh J, Cowan LD, Go O, Fabsitz RR, et al. Cardiovascular disease risk factors among American Indians. The Strong Heart Study. Am J Epidemiol. 1995;142:269–87. doi: 10.1093/oxfordjournals.aje.a117633. [DOI] [PubMed] [Google Scholar]
- 22.Harnack L, Sherwood N, Story M. Diet and physical activity patterns of urban American Indian women. Am J Health Promot. 1999;13:233–6. doi: 10.4278/0890-1171-13.4.233. [DOI] [PubMed] [Google Scholar]
- 23.Harnack L, Story M, Rock BH. Diet and physical activity patterns of Lakota Indian adults. J Am Diet Assoc. 1999;99:829–35. doi: 10.1016/S0002-8223(99)00197-2. [DOI] [PubMed] [Google Scholar]
- 24.deGonzague B, Receveur O, Wedll D, Kuhnlein HV. Dietary intake and body mass index of adults in 2 Ojibwe communities. J Am Diet Assoc. 1999;99:710–16. doi: 10.1016/S0002-8223(99)00170-4. [DOI] [PubMed] [Google Scholar]
- 25.Cole SM, Teufel-Shone NI, Ritenbaugh CK, Yzenbaard RA, Cockerham DL. Dietary intake and food patterns of Zuni adolescents. J Am Diet Assoc. 2001;101:802–6. doi: 10.1016/S0002-8223(01)00199-7. [DOI] [PubMed] [Google Scholar]
- 26.Liao Y, Tucker P, Okoro CA, Giles WH, Mokdad AH, Bales Harris V. Reach 2010 surveillance for health status in minority communities—United States, 2001–2002. MMWR Surveill Summ. 2004;53(SS-6):1–36. [PubMed] [Google Scholar]
- 27.Henry J, Kaiser Family Foundation . Key facts: race, ethnicity, and medical care: 2007 update. Menlo Park (CA): Henry J. Kaiser Family Foundation; 2007. [Google Scholar]
- 28.Centers for Disease Control and Prevention (US) Behavioral Risk Factor Surveillance System survey data. Atlanta: Department of Health and Human Services, CDC; 2008. [cited 2009 Sep 1]. Also available from: URL: http://www.cdc.gov/BRFSS. [Google Scholar]
- 29.Department of the Interior (US) Bureau of Indian Affairs. [cited 2009 Sep 1]. Available from: URL: http://www.doi.gov/bia.
- 30.Miller ME. Forgotten tribes: unrecognized Indians and the federal acknowledgment process. Lincoln (NE): University of Nebraska Press; 2006. [Google Scholar]
- 31.Pearson D, Cheadle A, Wagner E, Tonsberg R, Psaty BM. Differences in sociodemographic, health status, and lifestyle characteristics among American Indians by telephone coverage. Prev Med. 1994;23:461–4. doi: 10.1006/pmed.1994.1063. [DOI] [PubMed] [Google Scholar]
- 32.Donovan RJ, Holman CD, Corti B, Jalleh G. Face-to-face household interviews versus telephone interviews for health surveys. Aust N Z J Public Health. 1997;21:134–40. doi: 10.1111/j.1467-842x.1997.tb01672.x. [DOI] [PubMed] [Google Scholar]
- 33.Giulano A, Papenfuss M, Guerney De Zapien JG, Tilousi S, Nuvayestewa L. Prevalence of chronic disease risk and protective barriers among American Indian women living on the Hopi reservation. Ann Epidemiol. 1998;8:160–7. doi: 10.1016/s1047-2797(97)00200-7. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention (US) Racial and Ethnic Approaches to Community Health (REACH U.S.) [cited 2009 Sep 1]. Available from: URL: http://www.cdc.gov/reach.
- 35.ND Indian Affairs Commission. Statistics 2005. [cited 2009 Sep 1]. Available from: URL: http://www.nd.gov/indianaffairs/?id=37&page=Statistics+%26+Data.
- 36.Census Bureau (US) Census 2000 data for 539 tribes. [cited 2009 Sep 1]. Available from: URL: http://factfinder.census.gov/home/aian/sf_aian.html.
- 37.The American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 4th ed. Lenexa (KS): AAPOR; 2006. [Google Scholar]
- 38.Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System survey questionnaire. Atlanta: Department of Health and Human Services, CDC; 2004. [Google Scholar]
- 39.U.S. General Accounting Office. QPL data collection programs version 4.0. [cited 2009 Sep 1]. Available from: URL: http://www .gao.gov/qpl/col.pdf.
- 40.SPSS Inc. SPSS®: Version 16.0 for Windows. Chicago: SPSS Inc.; 2007. [Google Scholar]
- 41.Centers for Disease Control and Prevention (US) BRFSS Interactive Database. [cited 2009 Sept 1]. Available from: URL: http://apps.nccd.cdc.gov/BRFSS.
- 42.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People 2010 Statistical Notes, no. 20. Hyattsville (MD): National Center for Health Statistics (US); 2001. [PubMed] [Google Scholar]
- 43.Census Bureau (US) Race and Hispanic or Latino origin by age and sex for the United States: 2000. Pub. No. PHC-T-8. Washington: Department of Commerce (US); 2002. [Google Scholar]
- 44.Jackson C, Jatulis DE, Fortmann SP. The Behavioral Risk Factor Survey and the Stanford Five-City Project Survey: a comparison of cardiovascular risk behavior estimates. Am J Public Health. 1992;82:412–6. doi: 10.2105/ajph.82.3.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kehoe R, Wu SY, Leske MC, Chylack LT., Jr. Comparing self-reported and physician-reported medical history. Am J Epidemiol. 1994;139:813–8. doi: 10.1093/oxfordjournals.aje.a117078. [DOI] [PubMed] [Google Scholar]
- 46.Martin LM, Leff M, Calonge N, Garrett C, Nelson DE. Validation of self-reported chronic conditions and health services in a managed care population. Am J Prev Med. 2000;18:215–8. doi: 10.1016/s0749-3797(99)00158-0. [DOI] [PubMed] [Google Scholar]
- 47.Nebot M, Celentano DD, Burwell L, Davis A, Davis M, Polacsek M, et al. AIDS and behavioural risk factors in women in inner city Baltimore: a comparison of telephone and face to face surveys. J Epidemiol Community Health. 1994;48:412–8. doi: 10.1136/jech.48.4.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aquilino WS. Telephone versus face-to-face interviewing for house-hold drug use surveys. Int J Addict. 1992;27:71–91. doi: 10.3109/10826089109063463. [DOI] [PubMed] [Google Scholar]
- 49.Gohdes D, Harwell TS, Cummings S, Moore KR, Smilie JG, Helgerson SD. Smoking cessation and prevention: an urgent public health priority for American Indians in the Northern Plains. Public Health Rep. 2002;117:281–90. doi: 10.1016/S0033-3549(04)50162-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Doshi SR, Jiles R. Health behaviors among American Indian/Alaska Native women, 1998–2000 BRFSS. J Womens Health (Larchmt) 2006;15:919–27. doi: 10.1089/jwh.2006.15.919. [DOI] [PubMed] [Google Scholar]
- 51.Eichner JE, Cravatt K, Beebe LA, Blevins KS, Stoddart ML, Bursac Z, et al. Tobacco use in American Indians in Oklahoma: an epidemiologic view. Public Health Rep. 2005;120:192–9. doi: 10.1177/003335490512000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Struthers R, Hodge FS. Sacred tobacco use in Ojibwe communities. J Holist Nurs. 2004;22:209–25. doi: 10.1177/0898010104266735. [DOI] [PubMed] [Google Scholar]
- 53.Kumanyika SK, Obarzanek E, Stettler N, Bell R, Field AE, Fortmann SP, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention. Circulation. 2008;118:428–64. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]
- 54.Welty TK, Rhoades DA, Yeh F, Lee ET, Cowan LD, Fabsitz RR, et al. Changes in cardiovascular disease risk factors among American Indians. The Strong Heart Study. Am J Epidemiol. 2002;12:97–106. doi: 10.1016/s1047-2797(01)00270-8. [DOI] [PubMed] [Google Scholar]
- 55.Oser CS, Harwell TS, Strasheim C, Fogle C, Blades LL, Dennis TD, et al. Increasing prevalence of cardiovascular risk factors among American Indians in Montana. Am J Prev Med. 2005;28:295–7. doi: 10.1016/j.amepre.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 56.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–5. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 57.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 58.Islam-Zwart K, Cawston A. Investigation of factors contributing to diabetes risk in American Indian/Alaska Native youth. Am Indian Alsk Native Ment Health Res. 2008;14:49–58. doi: 10.5820/aian.1403.2007.49. [DOI] [PubMed] [Google Scholar]
- 59.Zephier E, Himes JH, Story M, Zhou X. Increasing prevalences of overweight and obesity in Northern Plains American Indian children. Arch Pediatr Adolesc Med. 2006;160:34–9. doi: 10.1001/archpedi.160.1.34. [DOI] [PubMed] [Google Scholar]
- 60.Jollie-Trottier T, Holm JE, McDonald, JD Correlates of overweight and obesity in American Indian children. J Pediatr Psychol. 2009;34:245–53. doi: 10.1093/jpepsy/jsn047. [DOI] [PubMed] [Google Scholar]
- 61.Coble JD, Rhodes RE. Physical activity and Native Americans: a review. Am J Prev Med. 2006;31:36–46. doi: 10.1016/j.amepre.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 62.Fischer ID, Brown DR, Blanton CJ, Casper ML, Croft JB, Brownson RC. Physical activity patterns of Chippewa and Menominee Indians: the Inter-Tribal Heart Project. Am J Prev Med. 1999;17:189–97. doi: 10.1016/s0749-3797(99)00073-2. [DOI] [PubMed] [Google Scholar]
- 63.May PA, Gossage JP. New data on the epidemiology of adult drinking and substance use among American Indians of the northern states: male and female data on prevalence, patterns, and consequences. Am Indian Alsk Native Ment Health Res. 2001;10:1–26. doi: 10.5820/aian.1002.2001.1. [DOI] [PubMed] [Google Scholar]
- 64.O'Connell JM, Novins DK, Beals J, Spicer P, AI-SUPERPFP Team Disparities in patterns of alcohol use among reservation-based and geographically dispersed American Indian populations. Alcohol Clin Exp Res. 2005;29:107–16. doi: 10.1097/01.alc.0000153789.59228.fc. [DOI] [PubMed] [Google Scholar]
- 65.Spicer P, Beals J, Mitchell CM, Novins DK, Croy CD, Manson SM, AI-SUPERPFP Team The prevalence of alcohol dependence in two American Indian reservation populations. Alcohol Clin Exp Res. 2003;27:1785–97. doi: 10.1097/01.ALC.0000095864.45755.53. [DOI] [PubMed] [Google Scholar]
- 66.Welty TK. The epidemiology of alcohol use and alcohol-related health problems among American Indians and Alaska Natives. In: Mail PD, Heurtin-Roberts S, Martin SE, Howard J, editors. Alcohol use among American Indians and Alaska Natives: multiple perspectives on a complex problem. Bethesda (MD): Department of Health and Human Services (US); 2002. pp. p. 49–70. [Google Scholar]
- 67.Hughes A, Sathe N, Spagnola K. State estimates of substance use from the 2005–2006 National Surveys on Drug Use and Health (DHHS Publication No. SMA 08-4311, NSDUH Series H-33) Rockville (MD): Substance Abuse and Mental Health Services Administration, Office of Applied Studies (US); 2008. [Google Scholar]
- 68.Rasmussen SR, Thomsen JL, Kilsmark J, Hvenegaard A, Engberg M, Lauritzen T, et al. Preventive health screenings and health consultations in primary care increase life expectancy without increasing costs. Scand J Public Health. 2007;35:365–72. doi: 10.1080/14034940701219642. [DOI] [PubMed] [Google Scholar]
- 69.Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Goodman MJ, Solberg LI. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31:52–61. doi: 10.1016/j.amepre.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 70.Harwell TS, Oser CS, Okon NJ, Fogle CC, Helgerson SD, Gohdes D. Defining disparities in cardiovascular disease for American Indians. Circulation. 2005;112:2263–7. doi: 10.1161/CIRCULATIONAHA.105.560607. [DOI] [PubMed] [Google Scholar]
- 71.Commission on Civil Rights (US) A quiet crisis: federal funding and unmet needs in Indian country. Washington: Commission on Civil Rights; 2003. [Google Scholar]
- 72.Intercultural Cancer Council. American Indians/Alaska Natives and cancer. [cited 2009 Sep 1]. Available from: URL: http://iccnetwork.org/cancerfacts/ICC-CFS2.pdf.
- 73.Jones DS. The persistence of American Indian health disparities. Am J Public Health. 2006;96:2122–34. doi: 10.2105/AJPH.2004.054262. [DOI] [PMC free article] [PubMed] [Google Scholar]