SYNOPSIS
Objectives
We described young women in North Carolina (NC) who were pregnant at the time of diagnosis with human immunodeficiency virus (HIV) infection to identify an at-risk population that could be targeted for increased HIV screening. We investigated the combined effect of partner counseling and referral services (PCRS) and comprehensive prenatal HIV screening.
Methods
We conducted a retrospective review of PCRS charts on young women newly diagnosed with HIV in NC between 2002 and 2005. We determined the prevalence of pregnancy in the study sample and conducted bivariate analyses to assess predictors of pregnancy at the time of HIV diagnosis, calculating prevalence ratios (PRs) with 95% confidence intervals (CIs). We analyzed results of partner notification efforts, including timing and stage of diagnosis of HIV-positive partners.
Results
During the four-year period, 551 women aged 18–30 years were newly diagnosed with HIV; 30% were pregnant at the time of HIV diagnosis. Pregnant women were more likely to be Hispanic (PR=1.58, 95% CI 1.15, 2.17) and not report typical risk factors. Fourteen percent of pregnant women's partners had an undiagnosed infection compared with slightly more than 8% of nonpregnant women's partners (p<0.01).
Conclusions
Ethnic differences in co-diagnosis of pregnancy and HIV suggest that young Hispanic women may have differential access to and acceptance of routine HIV screening. Comprehensive prenatal screening combined with partner notification can be effective in reaching infected male partners who are undiagnosed.
Many women in the United States are not routinely tested for human immunodeficiency virus (HIV).1 Health-care providers may not offer HIV tests due to policies (e.g., inadequate reimbursement) or logistics (e.g., time constraints)2 and, prior to 2006, recommendations of risk-based screening.3 Women may not request and/or accept tests due to fear of testing positive or a low perception of risk,4,5 particularly women who are in relationships.6 Routine testing during prenatal care increases testing opportunities for women. In the 2006 National Health Interview Survey, more than 60% of women who were pregnant at the time of the interview reported an HIV test in the last year compared with less than 13% of all nonpregnant women.1 Women who are diagnosed with HIV during pregnancy represent a population that may have previously had decreased access to routine HIV testing and/or a low perception of risk. Routine screening during prenatal care reduces mother-to-child transmission7 and, when combined with a partner referral and notification program,8 may provide opportunities to reach disenfranchised partners and decrease delayed diagnoses.
Currently, the Centers for Disease Control and Prevention (CDC) provides separate guidance for HIV testing, counseling, and referral in the U.S., including testing of pregnant women9 and partner referral services.10 Previous research has examined routine testing of pregnant women11–15 and reported on partner notification programs,–19 but no studies have examined the combined efforts of both CDC recommendations. Using statewide HIV records on young women newly diagnosed with HIV in North Carolina (NC), we examined the combined effect of NC's testing and referral services programs on young women and their partners.
METHODS
As part of an ongoing investigation of HIV in young adults in NC,20–23 we conducted a retrospective review of available state HIV epidemiologic records on all women aged 18–30 years with newly diagnosed HIV infection in NC between 2002 and 2005. Data were abstracted from partner counseling and referral services (PCRS) records. PCRS counselors, also called disease intervention specialists (DISs), conduct voluntary, post-diagnosis interviews with all individuals with reported cases of HIV and syphilis (index cases).
During the interview, the PCRS counselor conducts a risk assessment, provides risk reduction information, and makes referrals for medical care and case management. Additionally, the PCRS counselor reviews communicable disease control measures that document the legal requirement to notify past partners. The PCRS counselor elicits names and locating information on all sex and needle-sharing partners (contacts), working with the index patient to conduct partner notification. All contacts to the index case are informed of possible exposure and offered both HIV and syphilis testing, either in a clinic or in the field. All information on both the index case and contacts is documented in STD*MIS, a CDC standardized electronic database, and in hard copy paper charts stored in secure locations across the state. Data recorded on the index case include demographics, risk behaviors, lab results, and testing history. The PCRS counselor follows up with all contacts and documents test uptake and results.
A review of NC's PCRS program in 2001 indicated that nearly 90% of all new cases of HIV were interviewed by a PCRS counselor. The proportion of patients not able to be located did not vary by age or race/ethnicity, although patients tested in a public clinic were more likely to be located. Approximately 87% of contacts identified were located, and 64% of those not already diagnosed with HIV were tested following notification.17
Using a case abstraction form, trained research assistants abstracted data from the standardized fields, as well as the narrative sections of the PCRS case reports. Data were entered into a Microsoft® Access database.24 Using unadjusted prevalence ratios (PRs) and 95% confidence intervals (CIs), we identified characteristics of women diagnosed while pregnant to determine an at-risk population that could be targeted for increased HIV screening. We examined women's demographics (e.g., age and race/ethnicity), testing history, stage at diagnosis, and risk behaviors for associations with a concurrent HIV diagnosis and pregnancy. We defined a recent/acute diagnosis as either (1) a reactive test with a documented negative test in the last six months or (2) a ribonucleic acid (RNA) positive test with a concurrent antibody negative test. We defined late diagnosis as an acquired immunodeficiency syndrome (AIDS) diagnosis at first HIV test. Risk factors included number of sex partners, sex partner characteristics, and drug use. We classified the latter as use of any recreational drug (not including alcohol use only) and injection drug use (IDU).
We described results of partner notification efforts including testing uptake by contacts and percent positivity of those testing. After linking contacts to the female index cases, we examined timing and stage of diagnosis of HIV-positive partners, testing to see if there were differences by pregnancy status of the female index case. To account for non-independence of male cases (nine men were named as positive partners to multiple women), we used clustered regression analysis when testing for statistical differences. We conducted data analyses using SAS® software version 9.1.25
This study was approved by the University of North Carolina at Chapel Hill Nursing-Public Health Institutional Review Board.
RESULTS
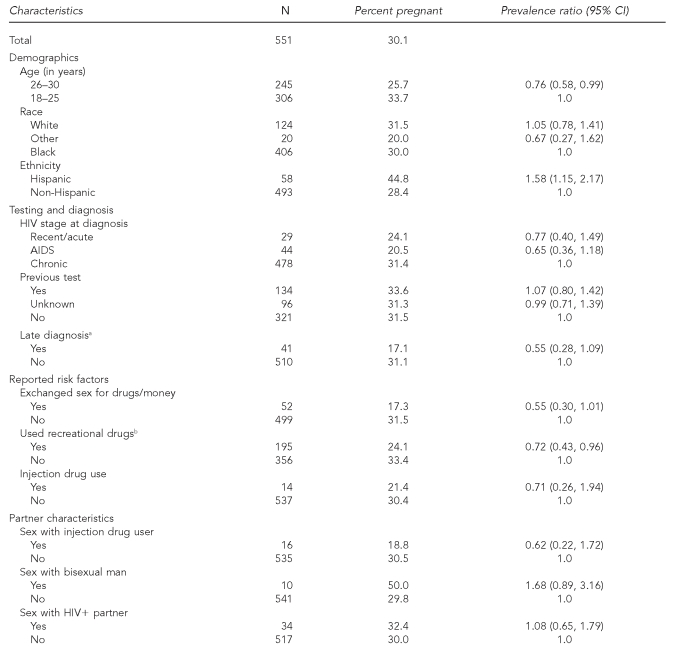
During the four-year period, 551 women aged 18 to 30 years with available PCRS records were newly diagnosed with HIV in NC; 166 (30.1%) were diagnosed while pregnant (Table 1). Women who reported exchanging sex for drugs/money (PR=0.55, 95% CI 0.30, 1.01) or using recreational drugs not including alcohol (PR=0.72, 95% CI 0.43, 0.96) were less likely to be pregnant at the time of HIV diagnosis. Women who were co-diagnosed with HIV and AIDS were less likely to also be pregnant at the time of diagnosis (PR=0.55, 95% CI 0.28, 1.09). Hispanic women were more likely to be diagnosed while pregnant (PR=1.58, 95% CI 1.15, 2.17). Only 11.5% of Hispanic pregnant women reported a previous HIV test compared with 30.0% of non-Hispanic pregnant women (p=0.05) (data not shown).
Table 1.
Characteristics of women aged 18 to 30 years with newly diagnosed HIV infection by pregnancy status at time of diagnosis, North Carolina, 2002–2005
aAIDS diagnosis at first HIV test
bNot including alcohol use only
HIV = human immunodeficiency virus
CI = confidence interval
AIDS = acquired immunodeficiency syndrome
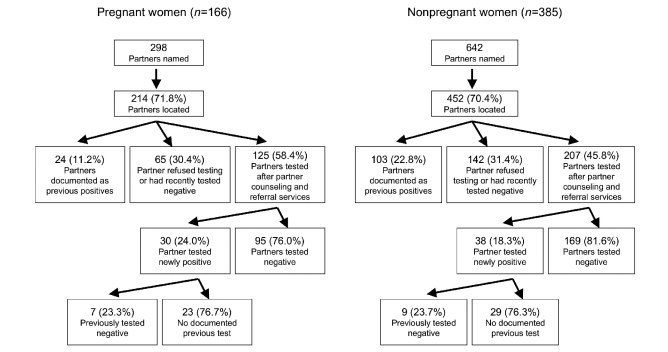
Nine hundred and forty sexual partners were named during PCRS counseling. On average, pregnant and nonpregnant women reported similar numbers of sexual contacts during partner notification (mean=1.8, standard deviation [SD] = 1.6; mean = 1.7, SD=1.6, respectively; p=0.4). Similarly, we found no statistical differences in the percentage of partners located by pregnancy status of the index case (Figure). We identified 196 HIV-positive male partners with either previously known infections or new diagnoses. Nine of the infected men (previously and newly diagnosed) were named as partners to multiple women. Six men were each contacts to two women, and three men were each contacts to three women for a total of 21 women involved (3.8% of the total population of women). Nine of the 21 women were pregnant (5.4% of the pregnant population). There were no differences in prevalence of infected partners found through contact tracing by pregnancy status; 32.5% of nonpregnant women (n=54) and 36.6% of pregnant women (n=141) had infected partners. However, pregnant women were more likely to have undiagnosed partners compared with nonpregnant women; 30 men newly diagnosed after contact tracing (14.0% of partners located) vs. 38 men (8.4% of partners located), respectively (p<0.01).
Figure.
Outcomes of partner notification services for 18- to 30-year-old female index cases newly diagnosed between 2002 and 2005 in North Carolina, stratified by pregnancy status at time of human immunodeficency virus diagnosis
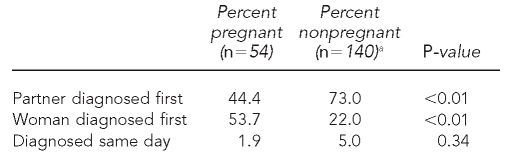
Comparing dates of diagnosis, more than half of pregnant women were diagnosed prior to their partner compared with 22.0% of nonpregnant women (p<0.01) (Table 2). When women were diagnosed first, HIV-positive contacts of pregnant women were subsequently diagnosed more quickly compared with nonpregnant women. Partners of pregnant women were diagnosed a mean of 63 days following the index female case's reactive test (interquartile range [IQR] 22, 98) vs. a mean of 122 days (IQR 23, 142) for partners of nonpregnant women (p=0.07). Among all women in the cohort, when men were diagnosed first, they had been notified of their infection a mean of 1,240 days (3.4 years) (IQR 60, 2,324) prior to the female's diagnosis. There was no difference in length of time before the women's diagnosis by pregnancy status.
Table 2.
Timing of diagnosis between women aged 18 to 30 years with newly diagnosed HIV infection and their positive partner, by pregnancy status at time of diagnosis, North Carolina, 2002–2005
aDate of diagnosis missing for one partner
Among all women in the cohort, when women were diagnosed first and their positive male partner was diagnosed through contact tracing, more than 75.0% of infected partners had never been tested and 13.3% already had progressed to an AIDS diagnosis. There were no statistical differences in partner's stage at diagnosis or testing history by pregnancy status of female index case.
DISCUSSION
We used statewide data abstracted from PCRS charts to examine characteristics of women newly diagnosed with HIV in NC, documenting differences in patient characteristics by pregnancy status at time of diagnosis. Women diagnosed with HIV during pregnancy did not report typical risk factors, such as drug use and high-risk sexual behavior. This finding suggests that there are few identifiable screening predictors, and lends support to universal HIV testing during prenatal care. Additionally, it underscores the need for testing at routine health-care visits prior to pregnancy care. Women who were diagnosed while pregnant were less likely to have progressed HIV disease (indicated by an AIDS diagnosis at the time of testing), suggesting that routine testing can help identify infections at an early stage.
Ethnic differences in co-diagnosis of pregnancy and HIV and in previous testing history suggest young Hispanic women may not be routinely accessing testing outside of prenatal care. Barriers may include low-risk perception,26 perceived stigma, fatalistic beliefs,27 lack of knowledge about treatment availability,28 and difficulty accessing services.29 However, these barriers are likely context-specific and may depend on local clinic characteristics (e.g., availability of translators) and on the prevalence of local prevention and outreach testing programs. Formative research should be undertaken prior to intervention development. Qualitative methods, including focus groups and in-depth interviews, have been used to identify barriers to other HIV prevention efforts30–32 and may be useful in developing targeted testing programs.
By linking abstracted data on the female index cases to their sexual partners, we also examined the effects of the PCRS partner notification efforts. In this sample, contact tracing and notification identified undiagnosed infections in male partners, including many cases that reported no previous testing and were in the late stages of disease (i.e., AIDS). Although there were no differences in the stage of the partner's diagnosis, pregnant women were more likely to have undiagnosed, positive partners than nonpregnant women. This finding suggests that the combination of comprehensive prenatal screening with partner notification can be effective in reaching infected individuals who are undiagnosed. However, among all women, the majority of positive male partners were told of their infection prior to the woman's diagnosis. It is unclear if the prolonged time lag between diagnoses was a result of men's undisclosed status to female partners or their partner's acceptance of risk and/or decision not to test following initial partner notification. This finding highlights the need to understand both testing practices and post-diagnosis risk behaviors, as well as create opportunities for prevention with positives, such as clinic-based interventions,33 prevention case management,34 and group-level interventions.35
Limitations
We made efficient use of routinely collected statewide data on newly infected women; however, this analysis had several limitations. We included only charts of index patients who were able to be contacted and interviewed. Although close to 90% of new cases of HIV are located by PCRS counselors,17 it is likely that the cases not interviewed were not missing at random (e.g., may be more likely to be ill, to have left the state, or to have provided false contacting information). We were unable to assess this bias, but the low prevalence of cases that were not interviewed should have minimal impact on the analysis.
Additionally, approximately 30% of named sexual partners were unable to be located and interviewed by PCRS counselors. This percentage is higher than the prevalence reported in the 2001 review of the NC PCRS program. The difference may be due to our restriction to only females or our chart abstraction protocols. For our data, we included all named contacts, including those who were unlikely to be located (e.g., were residing out of the state or country or for whom no contacting information was provided). Still, 30% missing data could have substantial impact on our conclusions. However, there were no differences in the proportion of contacts interviewed by pregnancy status of the female index case, thereby minimizing bias in the statistical comparisons.
The majority of data abstracted from the PCRS charts were based on self-report, including risk behaviors and named sexual contacts. Pregnant women may differentially report risk behaviors, such as drug use and number of sexual partners, due to social desirability bias. Additionally, we did not have information on the type of sexual partnerships (e.g., husband, casual partner) for the named contacts. Because pregnant women may have a higher prevalence of steady partnerships, this may explain the shorter time lag between subsequent diagnoses of infected undiagnosed partners (e.g., they are easier to locate and/or more willing to accept testing). Additionally, for men who knew they were infected, partner type may have influenced whether they disclosed their status to the female case. Future research could investigate the role of partner type in outcomes of PCRS to better inform prevention efforts.
Finally, PCRS counselors were not able to identify an infected sex partner for more than 60% of the female cases in this sample. This lack of identification may be the result of missing data on partners unable to be located, partners declining testing, or women who may not have provided complete information on their sexual partners during PCRS counseling.
CONCLUSIONS
Our review of testing and PCRS for pregnant women documented the public health impact of the combined programs. Our findings suggest that comprehensive testing during prenatal care may increase early diagnosis of HIV among females and, combined with partner notification, can be effective in reaching infected male partners who are undiagnosed. At the community level, monitoring trends in co-diagnosis of pregnancy and HIV can aid public health practitioners in identifying groups to be targeted for increased screening efforts, as well as subpopulations that may have differential access to and acceptance of routine HIV screening. In this study sample, Hispanic women were disproportionately diagnosed while pregnant; however, other settings may have populations with different demographic or risk profiles.
REFERENCES
- 1.Persons tested for HIV—United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57(31):845–9. [PubMed] [Google Scholar]
- 2.Burke RC, Sepkowitz KA, Bernstein KT, Karpati AM, Myers JE, Tsoi BW, et al. Why don't physicians test for HIV? A review of the US literature. AIDS. 2007;21:1617–24. doi: 10.1097/QAD.0b013e32823f91ff. [DOI] [PubMed] [Google Scholar]
- 3.Revised guidelines for HIV counseling, testing, and referral. MMWR Recomm Rep. 2001;50(RR-19):1–58. [PubMed] [Google Scholar]
- 4.de Wit JB, Adam PC. To test or not to test: psychosocial barriers to HIV testing in high-income countries. HIV Med. 2008;9(Suppl 2):20–2. doi: 10.1111/j.1468-1293.2008.00586.x. [DOI] [PubMed] [Google Scholar]
- 5.Siegel K, Raveis VH, Gorey E. Barriers and pathways to testing among HIV-infected women. AIDS Educ Prev. 1998;10:114–27. [PubMed] [Google Scholar]
- 6.Carey MP, Gordon CM, Morrison-Beedy D, McLean DA. Low-income women and HIV risk reduction: elaborations from qualitative research. AIDS Behav. 1997;1:163–8. doi: 10.1023/b:aibe.0000002976.60851.8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Success in implementing Public Health Service guidelines to reduce perinatal transmission of HIV—Louisiana, Michigan, New Jersey and South Carolina, 1993, 1995, and 1996. MMWR Morb Mortal Wkly Rep. 1998;47(33):688–91. [PubMed] [Google Scholar]
- 8.Task Force on Community Preventive Services. Recommendations to increase testing and identification of HIV-positive individuals through partner counseling and referral services. Am J Prev Med. 2007;33(2) Suppl 1:S88. doi: 10.1016/j.amepre.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 9.Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (US) HIV partner counseling and referral services—guidance. Atlanta: CDC; 1998. [Google Scholar]
- 11.Anderson JE, Sansom S. HIV testing in a national sample of pregnant US women: who is not getting tested? AIDS Care. 2007;19:375–80. doi: 10.1080/09540120500521392. [DOI] [PubMed] [Google Scholar]
- 12.Anderson JE, Sansom S. HIV testing among U.S. women during prenatal care: findings from the 2002 National Survey of Family Growth. Matern Child Health J. 2006;10:413–7. doi: 10.1007/s10995-006-0120-0. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez MI, Wilson TE, Ethier KA, Walter EB, Gay CL, Moore J. Acceptance of HIV testing during prenatal care. Perinatal Guidelines Evaluation Project. Public Health Rep. 2000;115:460–8. doi: 10.1093/phr/115.5.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anderson JE, Koenig LJ, Lampe MA, Wright R, Leiss J, Saul J. Achieving universal HIV screening in prenatal care in the United States: provider persistence pays off. AIDS Patient Care STDS. 2005;19:247–52. doi: 10.1089/apc.2005.19.247. [DOI] [PubMed] [Google Scholar]
- 15.Patterson KB, Leone PA, Fiscus SA, Kuruc J, McCoy SI, Wolf L, et al. Frequent detection of acute HIV infection in pregnant women. AIDS. 2007;21:2303–8. doi: 10.1097/QAD.0b013e3282f155da. [DOI] [PubMed] [Google Scholar]
- 16.Landis SE, Schoenbach VJ, Weber DJ, Mittal M, Krishan B, Lewis K, et al. Results of a randomized trial of partner notification in cases of HIV infection in North Carolina. N Engl J Med. 1992;326:101–6. doi: 10.1056/NEJM199201093260205. [DOI] [PubMed] [Google Scholar]
- 17.Partner counseling and referral services to identify persons with undiagnosed HIV—North Carolina, 2001. MMWR Morb Mortal Wkly Rep. 2003;52(48):1181–4. [PubMed] [Google Scholar]
- 18.Hogben M, McNally T, McPheeters M, Hutchinson AB. The effectiveness of HIV partner counseling and referral services in increasing identification of HIV-positive individuals: a systematic review. Am J Prev Med. 2007;33(2) Suppl:S89–100. doi: 10.1016/j.amepre.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 19.Mackellar DA, Hou SI, Behel S, Boyett B, Miller D, Sey E, et al. Exposure to HIV partner counseling and referral services and notification of sexual partners among persons recently diagnosed with HIV. Sex Transm Dis. 2008;36:170–7. doi: 10.1097/OLQ.0b013e31818d6500. [DOI] [PubMed] [Google Scholar]
- 20.Hightow LB, MacDonald PD, Pilcher CD, Kaplan AH, Foust E, Nguyen TQ, et al. The unexpected movement of the HIV epidemic in the Southeastern United States: transmission among college students. J Acquir Immune Defic Syndr. 2005;38:531–7. doi: 10.1097/01.qai.0000155037.10628.cb. [DOI] [PubMed] [Google Scholar]
- 21.Hightow LB, Leone PA, Macdonald PDM, McCoy SI, Sampson LA, Kaplan AH. Men who have sex with men and women: a unique risk group for HIV transmission on North Carolina college campuses. Sex Transm Dis. 2006;33:585–93. doi: 10.1097/01.olq.0000216031.93089.68. [DOI] [PubMed] [Google Scholar]
- 22.Torrone EA, Thomas JC, Leone PA, Hightow-Weidman LB. Late diagnosis of HIV in young men in North Carolina. Sex Transm Dis. 2007;34:846–8. doi: 10.1097/OLQ.0b013e31809505f7. [DOI] [PubMed] [Google Scholar]
- 23.Sena AC, Torrone EA, Leone PA, Foust E, Hightow-Weidman L. Endemic early syphilis among young newly diagnosed HIV--positive men in a southeastern U.S. state. AIDS Patient Care STDS. 2008;22:955–63. doi: 10.1089/apc.2008.0077. [DOI] [PubMed] [Google Scholar]
- 24. Microsoft Corp. Microsoft® Access: Version 2003 for Windows. Redmond (WA): Microsoft Corp.; 2003.
- 25. SAS Institute, Inc. SAS®: Version 9.1.3 for Windows. Cary (NC): SAS Institute, Inc.; 2004.
- 26.Lopez-Quintero C, Shtarkshall R, Neumark YD. Barriers to HIV-testing among Hispanics in the United States: analysis of the National Health Interview Survey, 2000. AIDS Patient Care STDS. 2005;19:672–83. doi: 10.1089/apc.2005.19.672. [DOI] [PubMed] [Google Scholar]
- 27.Parra EO, Doran TI, Ivy LM, Aranda JM, Hernandez C. Concerns of pregnant women about being tested for HIV: a study in a predominately Mexican-American population. AIDS Patient Care STDS. 2001;15:83–93. doi: 10.1089/108729101300003681. [DOI] [PubMed] [Google Scholar]
- 28.Ebrahim SH, Anderson JE, Weidle P, Purcell DW. Race/ethnic disparities in HIV testing and knowledge about treatment for HIV/AIDS: United States, 2001. AIDS Patient Care STDS. 2004;18:27–33. doi: 10.1089/108729104322740893. [DOI] [PubMed] [Google Scholar]
- 29.Tilson EC, Sanchez V, Ford CL, Smurzynski M, Leone PA, Fox KK, et al. Barriers to asymptomatic screening and other STD services for adolescents and young adults: focus group discussions. BMC Public Health. 2004;4:21. doi: 10.1186/1471-2458-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abreu S, Sala AC, Candelaria EM, Norman LR. Understanding the barriers that reduce the effectiveness of HIV/AIDS prevention strategies for Puerto Rican women living in low-income households in Ponce, PR: a qualitative study. J Immigr Minor Health. 2008 Aug 20; doi: 10.1007/s10903-008-9178-7. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rhodes SD, Hergenrather KC, Wilkin A, Alegria-Ortega J, Montano J. Preventing HIV infection among young immigrant Latino men: results from focus groups using community-based participatory research. J Natl Med Assoc. 2006;98:564–73. [PMC free article] [PubMed] [Google Scholar]
- 32.Choi KH, Roberts KJ, Gomez C, Grinstead O. Facilitators and barriers to use of the female condom: qualitative interviews with women of diverse ethnicity. Women Health. 1999;30:53–70. doi: 10.1300/j013v30n01_04. [DOI] [PubMed] [Google Scholar]
- 33.Richardson JL, Milam J, McCutchan A, Stoyanoff S, Bolan R, Weiss J, et al. Effect of brief safer-sex counseling by medical providers to HIV-1 seropositive patients: a multi-clinic assessment. AIDS. 2004;18:1179–86. doi: 10.1097/00002030-200405210-00011. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention, HIV/AIDS Prevention Research Synthesis Project (US) Compendium of HIV prevention interventions with evidence of effectiveness. Atlanta: CDC; [November 1999]. revised. [Google Scholar]
- 35.Kalichman SC, Rompa D, Cage M. Group intervention to reduce HIV transmission risk behavior among persons living with HIV/AIDS. Behav Mod. 2005;29:256–85. doi: 10.1177/0145445504272603. [DOI] [PubMed] [Google Scholar]