Narrative Abstract
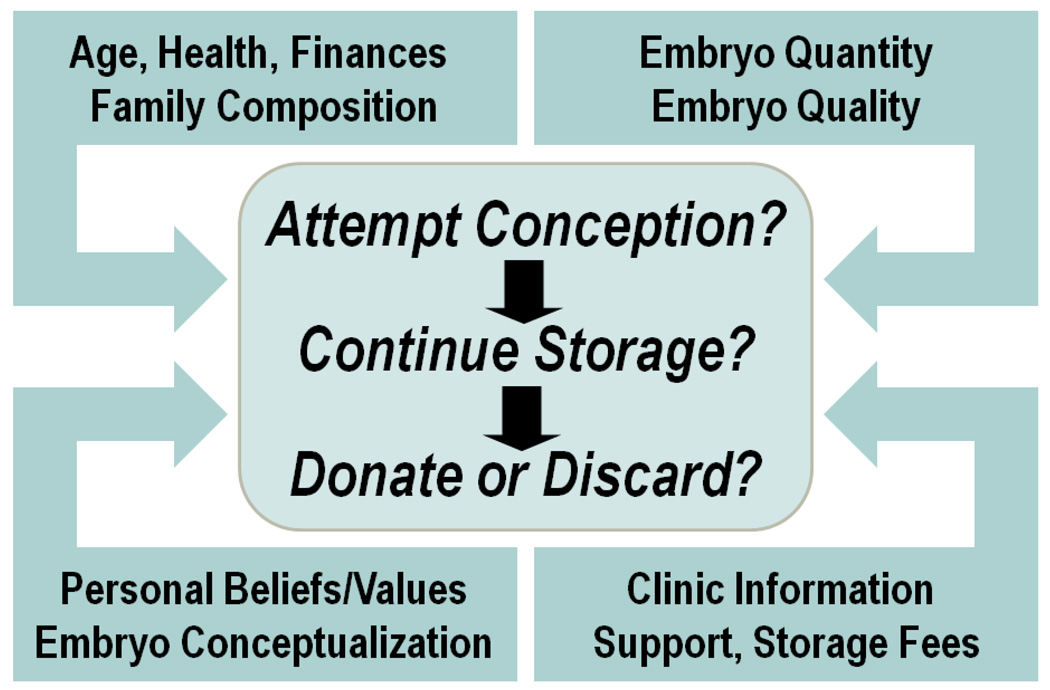
In a qualitative interview study of 77 families with stored frozen embryos, we found that while embryo disposition decision-making was influenced by individual life circumstances, embryo quantity/quality, personal values, embryo conceptualization, and clinic information, it was a stepwise process that could be represented as three sequential questions: (1) Additional conception attempts? (2) Continued storage? (3) Donation to science, to others, or destruction? While almost two-thirds (63%) of participants kept their embryos in storage after 5 years, either passively through disagreement or indecision or actively to maintain embryo “potential,” avert feelings of loss, or as psychological or genetic “insurance,” IVF clinic support and detailed information about options motivated families to make disposition decisions.
Previous research has found that the frozen embryo disposition decision-making process is often marked by ambivalence, discomfort, and uncertainty and may be influenced by factors which include how men and women conceptualize their embryos, practical and emotional investment in the “potential” of frozen embryos, conflicting attitudes about “genetic connectedness” and kinship, motivations to help others, and feelings of obligation or responsibility (1–10). The purpose of this correspondence is to use the experience of a large group of undecided embryo holders to provide a systematic description of the disposition-making process.
Participants were recruited from three large IVF practices in Northern California and the study protocol and consent form were approved by the Institutional Review Board of the University of California, San Francisco. Participants underwent three semi-structured interviews, each one to two hours long, at six-month intervals. Themes, ideas, and concepts that appeared in the interview transcripts were identified and code words defining and referencing these themes were developed. This report reflects an analysis of the interview data identified by the codes that referenced (a) any discussion of the process of or factors involved in making a decision about frozen embryo disposition or having more children or (b) any discussion of the value or worth of frozen embryos.
A total of 265 interviews were performed with 75 women and 55 men from 77 families with stored frozen embryos that had not made a disposition decision at the time of recruitment. The majority of participants were Caucasian, employed, married, college educated, identified as a member of a religious group, and reported median incomes of over $100,000. The median number of living children was two per family. One-third used donated gametes while two-thirds used only their own gametes to create embryos. The median number of stored embryos per family was seven and the average number of years they had been stored was five years at the time of the final interview. By the time of the final interview one year later, 26 families (34%) chose to deliberately store embryos indefinitely, 17 (22%) favored donation to science, 6 (8%) favored using embryos for further attempts as conception, 5 (6%) favored donation to others for family-building, and 1 (1%) favored embryo destruction. The remaining 22 families (29%) still had not made a disposition decision but continued to store their embryos.
While most couples reported having little or no discussion about embryo disposition throughout the year, except when the bill arrived, they also regarded the decision as an important one that should be made with adequate time and care. Our analysis suggests that the decision making process can be represented by three sequential questions: (1) Will the embryos be used for additional attempts at conception? If not, (2) Will the embryos remain in storage? And if not, (3) Will the embryos be donated to other people, to science, or will they be destroyed? Furthermore, at each stage of decision-making, one or more of the following four factors strongly influenced the response to these sequential questions: (a) personal beliefs, values, and embryo conceptualization; (b) individual life circumstances; (c) embryo parameters; and (d) clinic information and support. An overview of the decision making-process is represented schematically in Figure 1.
Figure 1.
Question (1) Will the embryos be used for additional attempts at conception?
This first question was the most difficult not only because it was at this point that most disagreements arose, but participants could not seriously consider other disposition options until this question was satisfactorily resolved. In most disagreeing couples, the gestational partner was the one most likely to want to make additional attempts at conception and pregnancy. While the existence of frozen embryos often fueled a yearning for more children, participants weighed this desire against their ability to parent and provide for an expanded family. As a result, the factors in participants’ individual life circumstances that dominated this stage of decision making included the couples ages, finances, the health and welfare of their children or themselves, the size and configuration of their immediate and extended family, and concerns about multiple gestation.
Participants considering additional attempts at conception also often considered the number and perceived “quality” or “viability” of the embryos. As a result, many who had few or “low grade” embryos questioned whether it would be worth the emotional investment and/or the financial expense to attempt additional frozen embryo transfers. Participants who had conceived children with frozen cycles were more likely to see frozen embryos as viable while those who had only conceived with “fresh” cycles tended to be more skeptical about the frozen embryos.
Question (2) Will the embryos remain in storage?
While many participants said that they would have preferred to avoid the issue of disposition by having used up all their embryos, most participants told us that without storage fees they would have very little motivation to make a disposition decision and would just keep the embryos in storage indefinitely. Despite a median annual storage fee of $500, almost two-thirds of participant families did indeed keep their embryos in storage. Of these families opting for continued storage, slightly more than half cited a variety of motivators, the most common of which was that indefinite storage represented an “insurance policy” (1) or “security blanket” (7) that allowed people to keep their reproductive options open while avoiding a variety of losses. These losses could include the loss of their emotional attachment to the embryos, the loss of embryo “potential” (11–13), and the loss of their identification as potentially fertile people (3). Ongoing storage also enabled people to avoid the unsettling prospect of relinquishing possession or control over the embryos and obviated the emotional challenge of reconceptualizing the stored embryos as something other than potential children (1, 3, 8). The other half of families choosing ongoing storage did so passively because they were unable or unwilling to make a disposition decision as a result of ambivalence, disagreement, or indecision.
Question (3) Will the embryos be donated to other people, to science, or be destroyed?
The idea of donating to others for family-building enabled participants to express the values of altruism (“helping others”) and/or reciprocity (“giving back”) and allowed the embryos to retain their original integrity and intention with which they were created. Yet for the most part, donating to others also meant not only relinquishing possession of embryos to which they felt a strong emotional attachment, but also required donors to reframe the embryos as potential children for people other than themselves (“like adopting out my own children”). This conceptualization created powerful concerns about the adequacy of others’ caretaking of these potential offspring as well as the possibilities for unintentional incest between “full siblings” or inadvertent disclosure of IVF or donated gametes. In the end these concerns were frequently at odds with the participant’s initial expressions of altruism and reciprocity and were found in families using both their own and donated gametes. Finally, citing a lack of information and a clear mechanism for donation, most participants felt that the potentially daunting financial, legal, and medical burdens of facilitating donation fell entirely on them. In a result that is congruent with other research (2, 5, 8, 14, 15), we found that only 6% of participating families favored donating their embryos to others.
Although studies performed in the 1990’s indicated little willingness to donate to science (16–18), our results are consistent with more recent research that finds donation to science to be an increasingly popular disposition option (3, 6, 19–22). This apparent shift in patient attitudes may reflect recent increased public awareness of stem cell research in the United States. For example, many participants cited media coverage of celebrities such as Michael J. Fox, as well as publicity about legislation supporting stem cell research in California. Some participants with few or “low quality” embryos considered donating to science because they believed the chances of conception resulting from their embryos was low. Furthermore, positive personal experiences with IVF clinic physicians or embryologists engendered trust and contributed to interest in donating embryos to science, although some expressed concerns about unscrupulous use of embryos in research. Finally, re-conceptualizing embryos as a socially beneficial, “valuable,” and “precious” resource allowed participants to both “close the chapter” on both their infertility and their associated emotional attachment to the embryos and satisfy altruistic personal values without having to confront entangling kinship ambiguities and responsibilities.
As in previous reports, destruction of embryos was an unpopular option that was widely construed as a “waste” that summarily precluded the opportunity to create children or provide benefit to others or society in general (2, 3, 5, 22). Although only one family in this study chose this option, it may prove to ultimately be a more popular option for the almost one-third of participants who are currently storing their embryos out of ambivalence or disagreement, as participants acknowledged that discarding provided a clear and definite outcome.
We believe that this analysis of the decision-making process may have useful implications for IVF practice and counseling as few IVF programs have established programs to deal with the long-term counseling needs of those with stored frozen embryos. Despite the appeal of having the option of indefinite storage, once confronted with the task of disposition decision-making, participants universally recognized that it was an “important” determination and voiced the desire to make a “responsible” choice and endorsed the values of altruism and reciprocity (1, 7). Because these altruistic ideals are frequently overcome by the perception of embryo donation as being personally and procedurally complicated, we suggest that embryo disposition in general and particularly embryo donation would likely be more strongly supported if IVF centers provided ongoing information, facilitation, and support (2, 15, 22–24).
Acknowledgments
Supported by NICHD Grant RO1 HD45429; R.D. Nachtigall, Principal Investigator; G. Becker, Co-investigator
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at the 64th Annual Meeting of the American Society for Reproductive Medicine, San Francisco, CA November 8–12, 2008.
Capsule
The frozen embryo disposition decision-making process can be represented as three sequential questions:(1) Additional conception attempts? (2) Continued storage? (3) Donation to science, to others, or destruction?
References
- 1.Nachtigall RD, Becker G, Friese C, Butler A, MacDougall K. Parents' conceptualization of their frozen embryos complicates the disposition decision. Fertil Steril. 2005;84:431–434. doi: 10.1016/j.fertnstert.2005.01.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lyerly AD, Steinhauser K, Voils C, Namey E, Alexander C, Bankowski B, et al. Fertility patients' views about frozen embryo disposition: results of a multi-institutional U.S. survey. Fertility and Sterility. doi: 10.1016/j.fertnstert.2008.10.015. In Press, Corrected Proof. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McMahon CA, Gibson FL, Leslie GI, Saunders DM, Porter KA, Tennant CC. Embryo donation for medical research: attitudes and concerns of potential donors. Hum Reprod. 2003;18:871–877. doi: 10.1093/humrep/deg167. [DOI] [PubMed] [Google Scholar]
- 4.de Lacey S. Patients' attitudes to their embryos and their destiny: social conditioning? Best Practice & Research Clinical Obstetrics & Gynaecology. 2007;21:101–112. doi: 10.1016/j.bpobgyn.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 5.de Lacey S. Decisions for the fate of frozen embryos: Fresh insights into patients' thinking and their rationales for donating or discarding embryos. Hum Reprod. 2007;22:1751–1758. doi: 10.1093/humrep/dem056. [DOI] [PubMed] [Google Scholar]
- 6.Parry S. (Re)constructing embryos in stem cell research: Exploring the meaning of embryos for people involved in fertility treatments. Social Science & Medicine. 2006;62:2349–2359. doi: 10.1016/j.socscimed.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 7.Lyerly AD, Steinhauser K, Namey E, Tulsky JA, Cook-Deegan R, Sugarman J, et al. Factors that affect infertility patients' decisions about disposition of frozen embryos. Fertil Steril. 2006;85:1623–1630. doi: 10.1016/j.fertnstert.2005.11.056. [DOI] [PubMed] [Google Scholar]
- 8.McMahon CA, Saunders DM. Attitudes of couples with stored frozen embryos toward conditional embryo donation. Fertility and Sterility. 2009;91:140–147. doi: 10.1016/j.fertnstert.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 9.de Lacey S. Parent identity and 'virtual' children: why patients discard rather than donate unused embryos. Hum Reprod. 2005;20:1661–1669. doi: 10.1093/humrep/deh831. [DOI] [PubMed] [Google Scholar]
- 10.Klock SC, Sheinin S, Kazer R. Couples' attitudes regarding embryo disposition after in vitro fertilization (IVF) Fertility and Sterility. 2001;76:S25. [Google Scholar]
- 11.Tversky A, Kahneman D. Loss Aversion in Riskless Choice: A Reference-Dependent Model. The Quarterly Journal of Economics. 1991;106:1039–1061. [Google Scholar]
- 12.Shin J, Ariely D. Keeping Doors Open: The Effect of Unavailability on Incentives to Keep Options Viable. Management Science. 2004;50:575–586. [Google Scholar]
- 13.Irons B, Hepburn C. Regret Theory and the Tyranny of Choice*. Economic Record. 2007;83:191–203. [Google Scholar]
- 14.Kingsberg SA, Applegarth LD, Janata JW. Embryo donation programs and policies in North America: survey results and implications for health and mental health professionals. Fertil Steril. 2000;73:215–220. doi: 10.1016/s0015-0282(99)00506-3. [DOI] [PubMed] [Google Scholar]
- 15.Zweifel JE, Rathert MA, Klock SC, Walaski HP, Pritts EA, Olive DL, et al. Comparative assessment of pre- and post-donation attitudes towards potential oocyte and embryo disposition and management among ovum donors in an oocyte donation programme. Hum Reprod. 2006 doi: 10.1093/humrep/dei468. [DOI] [PubMed] [Google Scholar]
- 16.Laruelle C, Englert Y. Psychological study of in vitro fertilization-embryo transfer participants' attitudes toward the destiny of their supernumerary embryos. Fertil Steril. 1995;63:1047–1050. doi: 10.1016/s0015-0282(16)57546-3. [DOI] [PubMed] [Google Scholar]
- 17.Darlington N, Matson P. The fate of cryopreserved human embryos approaching their legal limit of storage within a West Australian in-vitro fertilization clinic. Hum Reprod. 1999;14:2343–2344. doi: 10.1093/humrep/14.9.2343. [DOI] [PubMed] [Google Scholar]
- 18.Van Voorhis BJ, Grinstead DM, Sparks AE, Gerard JL, Weir RF. Establishment of a successful donor embryo program: medical, ethical, and policy issues. Fertil Steril. 1999;71:604–608. doi: 10.1016/s0015-0282(98)00545-7. [DOI] [PubMed] [Google Scholar]
- 19.Lyerly AD, Faden RR. Embryonic Stem Cells: Willingness to Donate Frozen Embryos for Stem Cell Research. Science. 2007;317:46–47. doi: 10.1126/science.1145067. [DOI] [PubMed] [Google Scholar]
- 20.Bangsboll S, Pinborg A, Yding Andersen C, Nyboe Andersen A. Patients' attitudes towards donation of surplus cryopreserved embryos for treatment or research. Hum Reprod. 2004;19:2415–2419. doi: 10.1093/humrep/deh441. [DOI] [PubMed] [Google Scholar]
- 21.Burton P, Sanders K. Patient attitudes to donation of embryos for research in Western Australia. Medical journal of Australia. 2004;180:559–561. doi: 10.5694/j.1326-5377.2004.tb06091.x. [DOI] [PubMed] [Google Scholar]
- 22.Hammarberg K, Tinney L. Deciding the fate of supernumerary frozen embryos: a survey of couples' decisions and the factors influencing their choice. Fertil Steril. 2006;86:86–91. doi: 10.1016/j.fertnstert.2005.11.071. [DOI] [PubMed] [Google Scholar]
- 23.Fuscaldo G, Russell S, Gillam L. How to facilitate decisions about surplus embryos: patients' views. Hum Reprod. 2007;22:3129–3138. doi: 10.1093/humrep/dem325. [DOI] [PubMed] [Google Scholar]
- 24.Newton CR, McDermid A, Tekpetey F, Tummon IS. Embryo donation: attitudes toward donation procedures and factors predicting willingness to donate. Hum Reprod. 2003;18:878–884. doi: 10.1093/humrep/deg169. [DOI] [PubMed] [Google Scholar]