Abstract
Background
There is inadequate recognition of alcohol misuse as a public health issue in India. Information on screening measures is critical for prevention and early intervention efforts. This study critically evaluated the full and shorter versions of the AUDIT and RAPS4-QF as screening measures for alcohol use disorders (AUDs) in a community sample of male drinkers in Goa, India.
Methods
Data from male drinking respondents in a population study on alcohol use patterns and sexual risk behaviors in randomly selected rural and urban areas of North Goa are reported. Overall, 39% (n=743) of the 1899 screened men, age 18 to 49, reported consuming alcohol in the last 12 months. These current drinkers were administered the screening measures as part of detailed interviews on drinking patterns and AUD symptoms. Receiver Operating Characteristic (ROC) analysis was conducted for each combination of screening measure and criterion (alcohol dependence or any AUD). Reliability and correlations among the 4 measures were also examined.
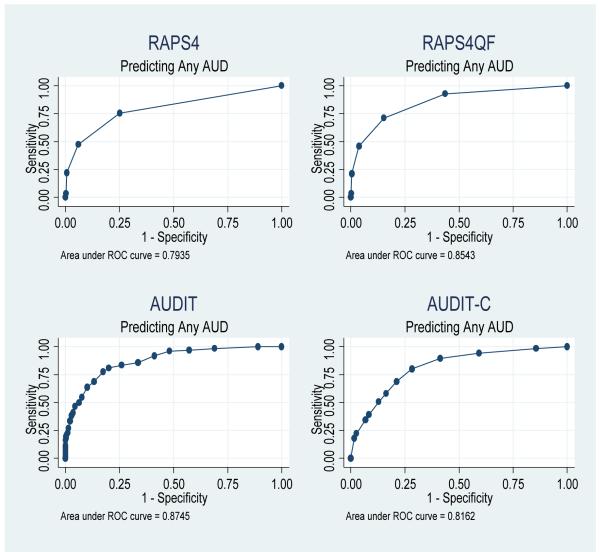
Results
All four measures performed well with area under the curves (AUCs) of at least .79. The full screeners that included both drinking patterns and problem items (the AUDIT and the RAP4-QF) performed better than their shorter versions (the AUDIT-C and the RAPS4) in detecting AUDs. Performance of the AUDIT and RAPS4-QF improved with lowered and raised thresholds, respectively, and alternate cut-off scores are suggested. Scores on the full measures were significantly correlated (.80). Reliability estimates for the AUDIT measures were higher than those for the RAPS4 measures.
Conclusions
All measures were efficient at detecting AUDs. When screening for alcohol-related problems among males in the general population in India, cut-off scores for screeners may need to be adjusted. Selecting an appropriate screening measure and cut-off score necessitates careful consideration of the screening context and resources available to confirm alcohol-related diagnoses.
Keywords: Alcohol-related problems, screening measures, ROC, India
INTRODUCTION
Rapid economic growth, including that of the alcohol industry combined with poor regulatory policies, multiple health risk factors, such as infectious diseases and malnutrition, and inadequate public health resources make alcohol-related problems especially significant in developing countries (Caetano and Laranjiera, 2006; Saxena, 2000). Alcohol production and consumption in India have shown increasing trends (Prasad, 2009). While overall abstention rates continue to be high, especially in women (Benegal et al., 2005), significant numbers of men drink and up to half meet criteria for heavy use. Despite being a public health crisis (Neufeld et al., 2005), alcohol misuse has not received adequate attention in India (Benegal, 2005; Gupta et al., 2003; Mohan et al., 2000).
Alcohol use is significant in Goa, one of India’s smallest states (Office of the Registrar General, 2001). Due to low excise duties on alcohol compared to that in other Indian states, thriving tourism, and local production of cashew-based spirits, alcohol is cheap and readily available. Hazardous alcohol use, assessed by the Alcohol Use and Disorders Identification test (AUDIT), is commonplace among drinkers in Goa. For instance, 31% and 56% of male drinkers respectively, among industrial workers and male primary care attendees, drank at levels likely to create physical and mental health problems (D’Costa et al., 2007; Silva et al., 2003).
Detecting alcohol use disorders (AUDs), specifically alcohol abuse and dependence, provides a critical opportunity for early intervention efforts to reduce adverse impacts of consumption. Studies in India have used alcohol screening measures, primarily the AUDIT (Babor et al., 1992), to examine hazardous alcohol use, defined as an alcohol consumption pattern that increases the risk of harmful consequences for the user and others (Babor et al., 2001), and to assess harmful drinking or alcohol abuse. Alcohol dependence has not been assessed in most of these studies. In general, the studies have used select and/or venue samples of industrial workers, primary care outpatients, psychiatric inpatients and substance use treatment and community outreach center attendees (Carey et al., 2003; D’Costa et al., 2007; Gaunekar et al., 2005; Pal et al., 2004) and indicate that the AUDIT is well suited for use in India. There is little or no data on screening for AUDs in community samples in India, however.
While studies in India using the AUDIT have used recommended cut-offs for hazardous drinking, Pal and colleagues (2004) found that a score of 24 provided a better balance of sensitivity and specificity, with improved specificity for alcohol dependence than the recommended cut-off of 20. They noted that higher cut-offs may be needed when using the AUDIT to screen for dependence among patients in substance use treatment in North India. This suggests the need for a critical evaluation of cut-off scores for the AUDIT and other screening measures of alcohol-related problems in India.
Research on alcohol use in Goa has not included new generation screening measures of alcohol use disorders that may outperform the AUDIT. Outside India, studies have evaluated various screening measures for AUDs, including short forms of the AUDIT and the RAPS4, CAGE and TWEAK, screeners named by mnemonics based on the first letter of key words for each item they measure (e.g.., remorse (R), amnesia (A), performance (P), and starter drinking behavior (S) for the RASP4) (Cherpitel et al., 2005b; Schafer and Cherpitel, 1998; Vinson et al., 2007). These studies have included population samples (Dawson et al., 2005; Rumpf et al., 2002; Woerle et al., 2007). An advantage of the RAPS4, where time is severely limited, is its brevity. RAPS4 items are dichotomous and any item affirmed screens positive for AUDs. The RAPS4 includes two AUDIT items, specifically drinking-related guilt/remorse and failure to do what is normally expected. The relative utility of the RAPS4 as a screening measure for AUDs has been compared across countries and findings indicate that it performs better in countries with a more detrimental drinking pattern (Cherpitel et al., 2005a). Thus, evaluating alternate screening measures of AUDs, including the RAPS4, in community samples in India may be useful.
The purpose of the present study was to compare an established screening measure, the AUDIT, with a promising rival, the RAPS4, using as the criteria more detailed measures of AUDs in a community sample of men in Northern Goa. The utility of these measures, including their shorter and full versions, in detecting alcohol-related problems was critically evaluated. ROC analyses examined and compared the accuracy of classification of cases and non cases for different cut-off scores across screeners against criterion measures of alcohol-related problems, specifically estimates of alcohol dependence and abuse. Classification indices compared included sensitivity or the proportion of all cases detected, specificity or the proportion of all non cases detected, positive predictive values (PPVs) or true cases among those screened positive and negative predictive values (NPVs) or true non cases among those screened negative by each screening measure. PPVs and NPVs indicate the likelihood of false positives and false negatives specific to each screening measure.
METHOD
Sample
Data come from male respondents in a population study on alcohol use patterns and sexual risk behaviors conducted in Northern Goa. Adults aged 18 to 49 years were randomly selected within rural and urban areas. These areas were selected purposively to represent the local Goan situation where urban areas are strongly influenced by economic liberalization and tourism, and rural areas have traditional village life dependent on agriculture and cashew-based (feni) alcohol production. Based on 2004 and 2007 electoral rolls, a two-staged probability sampling procedure was used to select households for participation. When no respondents were available at the randomly selected households or interviews could not be completed for other reasons, the household was replaced by approaching the first house on the right hand side of the house deemed unavailable.
Within each selected household, adults randomly selected on a probability basis participated in a screening interview. Screening interviews assessed for consumption of alcohol drinks with questions that included detailed beverage-specific drink size information (Nayak et al., 2008). A sub-sample, which included an over-sample of those who reported they drank at least one whole alcoholic drink in the past year, was invited to participate in a second more detailed main interview. Refusal rates for both interviews were very low (2% and <1%, respectively, for screening and main interviews).
A total of 1899 adult men completed screening interviews; 39% reported drinking alcohol in the past year. Past year drinking rates among women were extremely low (<5%); hence data from women are not included in this paper. Main interviews were completed by 1034 men, including 743 current drinkers. Roughly 69% (n=516) of all respondents were from randomly selected households, the remaining 31% (n=227) were from replacement households. No significant differences were found between respondents of randomly selected and replaced households in any study measures including demographics, alcohol use patterns and problems. Table 1 provides information on demographic characteristics of the male current drinkers and usual drinking frequency and quantity as well as frequency of heavy drinking as reported on the AUDIT (described below).
Table 1. Demographics and alcohol use* for Main Survey Male Drinkers (n=743, un-weighted data).
| Variable | Main survey male drinkers (n=743) |
|
|---|---|---|
| Area | Rural Urban |
53% (393) 47% (350) |
| Age | 18-20 21-29 30-39 40-49 |
5% (43) 31% (229) 39% (288) 26% (192) |
| Current Marital Status | Married & living with spouse Separated/divorced Widowed Never Married |
60% (444) 0.5% (6) 0.5% (4) 39% (289) |
| Religion | Hindu Muslim Christian |
80% (597) 5% (35) 15% (111) |
| Ethnicity | Goan Non-Goan |
81%(600) 19% (143) |
| Education | No education Primary & middle School Completed high School College or more Informal or other Education |
4% (27) 25% (185) 58% (430) 10% (77) 3% (24) |
| Employment | Employed (incl seasonal work) Not employed (incl. Full-time student of homemaker) |
91% (676) 9% (67) |
| Standard of Living Index (SLI) (Asset based wealth quintiles) |
Poor (lowest 40%) Middle (40%) Rich (highest 20%) |
36% (269) 41% (301) 23% (173) |
| Hunger in the last 3 months due to lack of money or money problems | Yes No |
5% (36) 95% (707) |
| Usual frequency of alcohol consumption | Monthly or Less than Monthly Two to Four times/Month Two to Three times/Week Four or more Times/Week |
35.9% (267) 28.3% (210) 14.7% (109) 21.1% (157) |
|
Usual quantity of alcohol consumption |
1 or 2 Drinks 3 or 4 Drinks 5 or 6 Drinks 7 or 8 Drinks 9 or more Drinks |
20.3% (151) 51.0% (379) 19.4% (144) 3.4% (25) 5.9% (44) |
|
Frequency of heavy drinking |
Never Less than Monthly Monthly Weekly Daily or almost Daily |
58.4% (434) 14.1% (105) 7.0% (52) 10.0% (74) 10.5% (78) |
Alcohol use information is as reported by drinkers on the AUDIT.
Measures
Current (past year) drinking
In the screening interview, respondents were asked if they had ever tasted alcohol or had a drink containing alcohol. Those responding ‘yes’ were also asked if they had a whole drink of any alcoholic beverage in the last 12 months. Only those responding ‘yes’ to the second question (current drinkers) completed the screening measures.
Screening measures
The Alcohol Use Disorders Identification Test (AUDIT) & AUDIT-C
The AUDIT is a 10-item questionnaire developed for international use by the World Health Organization that screens for hazardous alcohol use and AUDs, including harmful alcohol use and alcohol dependence (Babor et al., 2001; Saunders and Aasland, 1987). The AUDIT has been internationally validated on primary health care patients (Saunders et al., 1993) and used previously in Goa with industrial workers and primary care samples (D’Costa et al., 2007; Gaunekar et al., 2004; Gaunekar et al., 2005; Silva et al., 2003). The AUDIT-C comprises the first 3 consumption items of the AUDIT (Bush et al., 1998) and has been used in Western countries, including the U.S. and Germany but not in any published studies in India.
AUDIT items are coded 0 to 4. When summed, scores of 8, 16, and 20 or more indicate hazardous use, harmful use (alcohol abuse) and alcohol dependence, respectively (Babor et al., 2001). Studies indicate that scores of 4 or more and 5 or more on the AUDIT-C are optimal for screening for alcohol misuse and dependence in male drinkers, respectively, in U.S. and German population samples (Dawson et al., 2005; Rumpf et al., 2002). The AUDIT was administered in screening interviews and AUDIT-C scores derived from the first 3 items of the AUDIT.
The Rapid Alcohol Problems Screen (RAPS4) and RAPS4-QF
The RAPS4 was developed to assess for AUDs in emergency rooms in the U.S. (Cherpitel, 2000) using items initially from a number of short screening instruments. This 4-item screener has been found to outperform other screening instruments across gender and ethnic subgroups in the U.S. (Cherpitel and Bazargan, 2003); however sensitivity is better for alcohol dependence than harmful drinking or alcohol abuse. The RAPS4-QF combines RAPS4 information with that from two additional questions on usual consumption frequency and quantity, i.e. at least monthly drinking and any heavy drinking. The RAPS4-QF has been found to outperform other screening instruments for detecting harmful drinking or abuse in both the U.S. general population and in emergency rooms (Cherpitel, 2002).
Emergency room data from 13 countries, including India (Cherpitel et al., 2005a), indicates that the RAPS4 is a good screening measure for tolerance (a standard diagnostic criteria domain) as a proxy for alcohol dependence, and for heavy drinking (consuming 60g or more of ethanol on an occasion at least monthly) as a proxy for harmful drinking. Specifically, data from the Indian site in this study (Bangalore) found sensitivity and specificity of 77% and 90%, respectively for dependence (RAPS4) and 100% and 92%, respectively for abuse (RAPS4-QF). The RAPS4 was included in the main interviews. The RAPS4-QF was derived using RAPS4 data and that on usual frequency of consumption and frequency of heavy drinking assessed in the main interview by questions separate from those on the screening measures. All alcohol questions, including those in the screening measures used beverage-specific drink size information carefully assessed in the formative phases of the study (Nayak et al., 2008).
Criterion Measures
Alcohol Use Disorders (AUDs, Alcohol Abuse and Alcohol Dependence)
The DSM-IV (American Psychiatric Association, 2000) characterizes two distinct alcohol use disorders, i.e., abuse and dependence (Hasin, 2003). Alcohol abuse or harmful use is defined as involving significant alcohol-related consequences, specifically significant drinking-related failures to fulfill major obligations at work, school or home, interpersonal or legal problems and drinking involving hazardous situations. Alcohol dependence is defined as a maladaptive drinking pattern leading to clinically significant distress, marked by any three symptom clusters, e.g., withdrawal, tolerance, impaired control, continued use despite problems, co-occurring in the past 12 months. Measures of AUDs were administered in the main interviews
The alcohol abuse measure assessed relevant alcohol-related consequences using a 15-item scale (Appendix A) used extensively in prior U.S. national studies on alcohol (Greenfield et al., 2006; Midanik and Greenfield, 2000). The scale assesses five important alcohol-related problem areas: work problems, fights or arguments, family reactions, vehicular accidents and trouble with the law, and health problems. Prior research in the U.S. using this measure (Cherpitel, 2002; Midanik and Greenfield, 2000) used 2 or more consequences as indicative of alcohol abuse. Because the DSM-IV abuse criteria do not include alcohol-related health problems, we used 1 or more alcohol-related problems, other than those related to health, to indicate abuse.
The alcohol dependence measure was also adapted from U.S. national alcohol surveys and included 17 items (Appendix B) that reflect DSM-IV defined symptom domains (American Psychiatric Association, 2000) and 7 criteria for alcohol dependence (Caetano and Greenfield, 1997; Caetano and Tam, 1995). Respondents reporting at least one positive item from each of three or more symptom domains were identified as alcohol dependent. Since 12-month symptom occurrence is considered without the two week co-occurrence criterion needed for DSM-IV diagnosis of alcohol dependence (American Psychiatric Association, 2000), the measure, although standardized for surveys (Caetano and Tam, 1995), is not considered a formal diagnosis. A similar limitation applies to the alcohol abuse measure used since frequency of occurrence is not estimated. We used a combined measure of either estimated alcohol abuse or dependence to indicate alcohol-related problems.
While the DSM-IV diagnostic criteria stipulate that alcohol abuse cannot be diagnosed in the presence of dependence, research indicates that diagnosing alcohol abuse independently improves the reliability and validity of abuse as an AUD diagnosis (Hasin, 2003). More than half of the 88 respondents (59.1%, n=52) who met criteria for alcohol dependence did not report any alcohol-related consequences, suggesting a lack of significant overlap of abuse and dependence disorders in our sample. Conversely, few respondents reported alcohol-related consequences in the absence of dependence (n=34), providing insufficient statistical power to conduct ROC analyses with alcohol abuse as a residual diagnostic category. Thus, in keeping with rigorous diagnostic definitions, results on alcohol dependence (with or without problems indicative of abuse) and any AUD (alcohol abuse or dependence) are reported. Due to lack of power, results for alcohol abuse are not reported.
The adapted abuse and dependence scales had good internal consistency (Cronbach’s α=.75, α=.72, respectively), with no individual item removal resulting in a higher alpha. Following specifications for cross-cultural research in adapting measures for use in another culture (Bracken and Barona, 1991), all measures were translated and back-translated into Konkani, Goa’s official language, as well as other languages spoken in Goa, e.g., Marathi and Hindi. Most interviews were completed in Konkani (93.1%, n=692).
Procedure
Following informed consent procedures, screening and main interviews were completed, in private, in the homes of respondents. With the exception of one respondent, both interviews were completed on the same day. The study protocol, measures, and procedures were approved by the research ethics committees at Sangath in Goa and the Public Health Institute in the US. The study was also approved by the Indian Council of Medical Research.
Screening interviews took under 20 minutes to complete (mean=17.09, SD=7.01) with the main interviews taking just over an hour (mean=65.38, SD=26.76). To limit participant burden and reduce refusals or non-completion due to irrelevant questions, only current drinkers completed the screening measures and light drinkers were not administered the abuse and dependence (criterion) measures. Light drinkers were defined as those who met all 3 conditions: drinking less than once a month, a maximum consumption of less than 24 grams of pure ethanol, and a score of less than 8 on the AUDIT. A total 48 men who met all conditions for light drinking as defined, were skipped out of this section of the interview and coded as negative for AUDs. Thus, criterion measures (alcohol dependence and any AUD) were administered only to drinkers meeting any of the following criteria: a score 8 or more (hazardous drinking) on the AUDIT, drinking at least once a month, or maximum consumption of more than 24 grams of pure ethanol in a day.
Analysis
Distributions of demographic variables, screener variables, including the RAPS4, RAPS4-QF, Audit and Audit-C, and criterion variables were first examined. Internal consistencies of each of the four screening measures assessed with reliability analyses were moderate to good, with estimates for the AUDIT measures being higher than those for the RAPS4 measures (Cronbach’s α=.80, α=.82 for the AUDIT and AUDIT-C, respectively; KR20= .56, KR20=.61 for the RAPS4 and RAPS4-QF, respectively). Correlation of the RAPS4-QF with the AUDIT was high (.80). The shorter forms had relatively low correlations with each other (.44) and moderate correlations with the full form of the other measure (.68 for RAPS4 with AUDIT; .67 for RAPS4_QF with the AUDIT-C). As expected, short and full forms of each measure were highly correlated with each other (.86 for the AUDIT and AUDIT-C; .92 for the RAPS4 and RAPS4-QF).
In order to compare each screener variable against each criterion variable, a Receiver Operating Characteristic (ROC) analysis was performed (Green and Swets, 1966; Hosmer and Lemeshow, 2000). For each combination of candidate screener and criterion being used, ROC analyses provide a number of summary measures, including sensitivity, specificity, percent correctly classified, positive and negative predictive values. The area under the curve (AUC) is an important curve characteristic; higher areas indicate a more discriminating screening measure. Equality of AUC for each screening variable was carried out using STATA. Because prior research in Goa has employed standard cut-offs based on earlier cited research in developed countries for the AUDIT, ROC analyses results on the performance of these standard cut-off scores were first closely examined for each screening measure, separately for each criterion.
ROC analyses used un-weighted data from current drinkers only for several reasons. First, as stated previously in the description of the study procedures, non-drinkers were not administered the screening measures. Second, although non-drinkers are a legitimate part of the screening population, including them in the analyses would artificially inflate specificity of measures beyond that for the population at risk for AUDs, i.e., drinkers. Dawson and colleagues (2005) commented that decisions on appropriate cut-offs on the AUDIT-C for different outcomes are best made after exclusion of non-drinkers and other studies on screening measures for AUDs have also limited analyses to past year drinkers (Vinson et al., 2007). Finally, given that drinkers were over-sampled for our study main interviews in which the RAPS4 measures were administered, including non-drinkers in the analyses would necessitate weighting data back to population estimates, however ROC analyses do not accept case-weights (Stata Corp, 2007).
Because the AUDIT measures were administered in screening interviews for which drinkers and non-drinkers were selected on a probability basis, preliminary analyses included non-drinkers in ROC analyses on the AUDIT and the AUDIT-C measures. Additional sensitivity analyses, excluding the 48 light drinkers who were not administered the criterion measures and coded negative on AUDs, were also conducted for all the screening measures.
RESULTS
Table 2 shows that 12% of all (drinker) respondents were estimated to have alcohol dependence and 17% any AUD. Estimated prevalence rates for all North Goa men were 4.2% and 6.2% for alcohol dependence and any AUD, respectively. The most frequently endorsed items (by 62 to 68% of those with any AUD) on the AUDIT included the 3 items that comprise the AUDIT-C. The last item on whether someone had suggested they cut down their drinking was endorsed by 76.2% of the men positive for any AUD. Similarly, the consumption (monthly frequency and any heavy drinking) item of the RAPS-4 QF was endorsed by 86% of those with any AUD; a higher proportion than those that endorsed any of the RAPS4 items (ranging from 19.7% to 54%).
Table 2. Prevalence rates of positive scores on screening measures and of being positive on the criterion measures in Main Survey Male Drinkers (n=743, un-weighted data).
| Variable | % Positive on Measure |
Cronbach’s α | |
|---|---|---|---|
| RAPS4 | Score 1+ of 4 | 33.0% (248) | .56 |
| RAPS4-QF | Score 1+ of 5 | 51.7% (384) | .61 |
| AUDIT Low risk drinking Hazardous drinking Harmful use and dependence Dependence |
Score 7 or less Score 8 - 15 Score 16+ Score 20+ |
64.0% (480) 26.0%(191) 10.0% (72) 4.7% (35) |
.80 |
| AUDIT-C | Score 4+ Score 5+ |
49.1% (365) 36.7% (273) |
.82 |
| Past 12 month estimated Alcohol Dependence (3 of 7 symptom DSM criteria met) |
No Yes |
88.0% (641) 12.0% (88) |
.72 |
| Past 12 month estimated any AUD (Either 1+ Consequences or 3+ DSM) |
No Yes |
83.5% (616) 16.5% (122) |
.82 |
Post hoc analyses (not presented in the Tables) revealed that the majority of the 695 drinkers completing the AUD criterion measures reported drinking at least once a month (78.9%) or that their maximum consumption in the past year exceeded 24 grams of pure ethanol (95.7%). About a third were positive for hazardous drinking on the AUDIT (36.6%) and none met only the AUDIT 8+ criteria for being administered the AUD criterion measures. Hence, our procedure of skipping light drinkers out of the criterion measures did not result in only those “pre-screened” as hazardous drinkers on the AUDIT completing the criterion measures. Additional post hoc analyses on the 70 current drinkers who completed the criterion measures and had the lowest volumes of consumption (at or below the 10th percentile) revealed extremely low rates of AUD (n=1; 1.4%). This provided support for our decision to code the 48 light drinkers who were not assessed on the criterion measures as negative on AUDs for the ROC analyses.
ROC curves for each screening measure predicting AUD are shown in Figure 1. ROC curves predicting dependence appeared nearly identical and therefore are not shown. Table 3 presents AUCs for each screening measure evaluated and tests for significant differences between AUCs. An AUC of 1.0 indicates perfect sensitivity at all levels of specificity while that of 0.5 indicates that the measure’s performance does not predict any outcome better than that expected by chance. All four screening measures were associated with AUCs of .80 or higher, suggesting that they performed well as screening measures for AUDs. AUCs for the AUDIT and AUDIT-C (not reported in the table) were essentially unchanged when the 48 light drinkers not administered the criterion measures were excluded, but higher (.95 and .93 respectively) when non-drinkers were included (also not shown in the table). Overall, differences in AUCs suggested that the shorter measures did not perform as well as the full measures. Specifically, significant differences were found between the RAPS4 and RAPS4-QF and the AUDIT and AUDIT-C but differences between the RAPS4-QF and both forms of the AUDIT barely reached significance for the outcome of alcohol dependence (p<.10) and that between the RAPS4 and the AUDIT-C was not significant. The RAPS4_QF had better overall performance than the AUDIT-C for any AUD (p <.05).
Figure 1. ROC Curves Predicting any AUD.
Table 3. Comparison of Areas under the Curves (95% confidence intervals; current drinkers only).
| RAPS4 | RAPS4-QF | Audit | Audit-C | ||
|---|---|---|---|---|---|
| Alcohol Dependence | RAPS4 | .80 (.75, .85) | -- | -- | -- |
| RAPS4-QF | *** | .85 (.80, .89) | -- | -- | |
| Audit | *** | † | .88 (.84, .91) | -- | |
| Audit-C | ns | † | *** | .82 (.78, .87) | |
| Any AUD | RAPS4 | .79 (.75, .84) | -- | -- | -- |
| RAPS4-QF | *** | .85 (.82, .89) | -- | -- | |
| Audit | *** | † | .87 (.84, .91) | -- | |
| Audit-C | ns | * | *** | .82 (.78, .86) |
Indicate a significant difference in areas of .10, .05, .01, and .001
Indicate a significant difference in areas of .10, .05, .01, and .001
Indicate a significant difference in areas of .10, .05, .01, and .001
Indicate a significant difference in areas of .10, .05, .01, and .001
Note that tests of differences in the upper diagonal of tables are redundant with those in the lower diagonal and hence are not shown.
Table 4 reports information from ROC analyses when standard cut-offs (bolded and italicized) and alternative cut-off scores on each screening measure are applied. Pre-determined or recommended cut-off scores for abuse and dependence yielded lower sensitivity for the AUDIT compared to the other measures but much higher specificity. Excluding the 48 light drinkers coded as negative on AUDs (not shown in table) indicated no changes in specificity and very modest decreases in specificity for any AUDs (AUDIT: 96.46% to 96.30%; AUDIT-C: 58.78% to 55.46%; RAPS4: 74.88% to 73.59%; RAPS4-QF: 55.36% to 53.70%). In addition, as expected, including non-drinkers (also not in Table 4) did not alter sensitivity but increased specificity, particularly for the AUDIT-C, for the standard cut-off scores for both criterion standards (alcohol dependence: AUDIT - 98.75% to 99.39%; AUDIT-C - 68.80% to 88.46%: Any AUD: AUDIT - 96.46% to 98.59%; AUDIT-C - 58.78% to 84.67%).
Table 4. Performance of standard and alternate cut-off scores for the AUDIT, AUDIT-C, and RAPS4-QF with current drinkers.
| Standard Criterion | Screening Measure |
Cutpoint | Sensitivity | Specificity | % Correctly Classified |
NPV | PPV |
|---|---|---|---|---|---|---|---|
| Alcohol Dependence |
Audit | 8+ | 84.09 | 70.67 | 72.29 | 97.00 | 28.24 |
| 9+ | 81.82 | 76.60 | 77.23 | 96.84 | 32.43 | ||
| 10+ | 79.55 | 79.25 | 79.29 | 96.58 | 34.48 | ||
| 11+ | 72.73 | 84.24 | 82.85 | 95.74 | 38.79 | ||
| 20+ | 29.55 | 98.75 | 90.40 | 91.08 | 76.47 | ||
| Audit-C | 4+ | 89.77 | 55.54 | 59.67 | 97.53 | 21.70 | |
| 5+ | 81.82 | 68.80 | 70.37 | 96.50 | 26.47 | ||
| 6+ | 70.45 | 76.29 | 75.58 | 94.95 | 28.97 | ||
| 7+ | 62.50 | 81.90 | 79.56 | 94.09 | 32.16 | ||
| RAPS4 | 1+ | 79.55 | 72.39 | 73.25 | 96.27 | 28.34 | |
| RAPS4-QF | 1+ | 92.05 | 52.89 | 57.61 | 97.98 | 21.15 | |
| 2+ | 75.00 | 82.06 | 81.21 | 95.99 | 36.46 | ||
| 3+ | 47.73 | 94.38 | 88.75 | 92.93 | 53.85 | ||
| Any Alcohol Use Disorder |
Audit | 8+ | 83.61 | 74.07 | 75.64 | 95.83 | 38.78 |
| 9+ | 81.15 | 80.03 | 80.22 | 95.58 | 43.39 | ||
| 10+ | 77.87 | 82.45 | 81.70 | 94.99 | 46.57 | ||
| 11+ | 68.85 | 86.80 | 83.85 | 93.41 | 50.60 | ||
| 16+ | 40.98 | 96.46 | 87.35 | 89.27 | 69.44 | ||
| Audit-C | 4+ | 89.34 | 58.78 | 63.80 | 96.56 | 29.86 | |
| 5+ | 80.33 | 71.82 | 73.22 | 94.89 | 35.90 | ||
| 6+ | 68.85 | 78.90 | 77.25 | 92.80 | 39.07 | ||
| 7+ | 58.20 | 83.74 | 79.54 | 91.07 | 41.28 | ||
| RAPS4 | 1+ | 75.41 | 74.88 | 74.97 | 93.94 | 37.10 | |
| RAPS4-QF | 1+ | 92.67 | 55.36 | 62.31 | 97.49 | 29.43 | |
| 2+ | 71.31 | 84.70 | 82.50 | 93.76 | 47.80 | ||
| 3+ | 45.90 | 96.30 | 88.02 | 90.06 | 70.89 |
NPV=Negative predictive value; PPV=Positive Predictive Value
Standard Cut-off values for each of the AUDIT, AUDIT-C, RAPS4 and RAPS4-QF are shown in italics.
Bolded cut-off values are those found to perform the best among all possible cut-off choices
For some criterion-scale combinations (e.g., Dependence, Audit-C ), the standard and best-performing cut-off values coincided, in which case the rows are shown in bold-italics.
In order to be deemed acceptable, sensitivities and specificities associated with a cut-off score should be well above 50%. For current drinkers, either of these rates for at least one criterion measure was less than or close to 50% (Table 4) when pre-determined cut-off scores were used for the AUDIT, RAPS4-QF, and AUDIT-C. Therefore, information from the ROC curves for alternative cut-off points for these 3 measures is also provided in Table 4, with recommended cut-off scores highlighted. Cut-off scores of 9 or 10 and 5 or 6 for the AUDIT and AUDIT-C, respectively, were found to be associated with the best combinations of acceptable sensitivity and specificity. Similarly a score of 2 on the RAPS4-QF resulted in improved specificity and PPV for dependence compared to that of 1 or more.
DISCUSSION
To our knowledge, this study is the first to extend the use of the AUDIT to a large community sample in India and to compare multiple screening measures using a criterion measure of survey-assessed alcohol use disorders with drinkers in India. While the study findings re-affirm the usefulness of the AUDIT as a screening measure for use in Goa, the length of the AUDIT may preclude its use in settings where time is critical. Thus information on the alternative screening measures is useful.
When assessing problematic drinking within an early intervention paradigm, the identification of cases may be more important than minimizing the possibility of false positives. Screening, in essence, pre-supposes that additional detailed assessment will follow, at which point false positives can be identified as non-cases. Misidentification of cases as non-cases due to low sensitivity, however, clearly has undesirable public health implications. Thus, selecting an appropriate screening measure involves balancing concerns of over-diagnosing cases with that of missing true cases, and consideration of both the context in which the screening occurs (clinic versus non clinic) and time and other resources available to confirm the diagnosis and intervene.
Negative predictive values (NPVs) indicate the efficiency of a measure to identify negative cases, with values that decrease as the threshold is raised. NPVs were found to be at least 90% for all the measures even with different cut-offs, suggesting a low likelihood of false negatives for any of the screening measures. In contrast, there was variability in the positive predictive values for the measures, with those associated with standard cut-offs for the AUDIT being the highest. PPVs represent true positives among those screened positive by the measure and increase with increasing thresholds.
Increasing the threshold or cut-off score, however, also reduces sensitivity of the screening measure. Sensitivity for standard cut-offs were the lowest for the AUDIT compared to the other screening measures, and increased over 2-fold without much loss in NPVs when cut-off scores were lowered from 16 to 9 or 10. Thus, lower cut-off scores may be necessary when the AUDIT is used to screen for AUDs outside clinical settings in Goa. Indeed, the AUDIT was developed for use in primary care settings where specified higher cut-offs scores are appropriate. Pal and colleagues (2004) reported that higher cut-offs may be needed when using the AUDIT to screen for dependence among patients in substance use treatment. Together, study findings suggest that when the AUDIT is used with drinkers in Goa, and potentially elsewhere in India, cut-off scores for the identification of possible AUDs may need to be adjusted.
Our findings suggest that the AUDIT-C performs in a similar way in Goa as that reported in western countries. Sensitivity rates for alcohol dependence with a cut-off score of 5 or more (81.82%) were similar to those reported for the U.S. and Germany (89.2% and 88.7%, respectively). Specificity rates (68.8%) with the same cut-off score, however, were lower than those reported for U.S. and German population samples (72.4% and 93%, respectively). Specificity is particularly important when prevalence of a disorder is low (<5%). Given that at least 15% of drinkers may be expected to have an AUD in Goa, the lower specificity does not appear to impede use of the AUDIT-C among Goan drinkers.
Prior research using U.S. national survey data found that the AUDIT-C falls short of sensitivities reported for the RAPS4 at high levels of specificity for dependence, (Cherpitel, 1999; Cherpitel, 2002). Our data also show that at similar specificity levels, the AUDIT-C had lower sensitivity for dependence compared to the RAPS4 (70% vs 79%). In their cross-nation analysis, Cherpitel and colleagues (2005a) noted that the RAPS4 and RAPS4-QF performed better in countries with a more detrimental drinking pattern, such as India. Given its brevity and ease of administration, the RAPS-QF may be a better choice than the AUDIT-C when screening for AUDs in Goa, particularly when time is limited. A cut-off score of 2 resulted in better specificity for the RAPS4-QF at roughly equivalent sensitivity, NPV and PPV as those found for the AUDIT with lowered cut-off scores, particularly for dependence.
Our findings indicate that shorter (3 and 4 item) alcohol screeners do not perform as well as their full versions in assessing alcohol use disorders. Limitations of shorter instruments are not specific to screening for AUDs alone. Patel and colleagues (2007) also reported poorer performance for shorter screeners for common mental disorders in a primary care sample of 598 adults in Goa. For the full measures in our study, among the most frequently endorsed were items related to consumption on either fuller measure. In addition, 3 of 4 men estimated to have any AUD endorsed AUDIT (problem) item 10, indicating that this item may be a particularly useful item for the sample studied. Additionally, the better performance of full measures may be due to their assessment of both drinking patterns and problems as opposed to either of these alone, as in their shorter forms. Current calls for including measures of consumption in the diagnosis of alcohol dependence are noteworthy in this direction (Li et al., 2007).
Overall, the RAPS4 and RAPSQF performed well but had lower internal consistencies (less than .70). This suggests the need for further evaluation of these measures in Goa. The fewer number of items, which make the RAPS4 measures highly efficient and easy to implement, likely reduced their internal consistency estimates. In addition, the disparate alcohol problems assessing on the RAPS4 measures may reduce internal consistency. Indeed, the AUDIT-C had a significantly higher reliability coefficient (.82) than the RAPS-QF, possibly due to all its items assessing the same domain of alcohol use, consumption.
The present study has several limitations. The screening measures were embedded in longer interviews with additional questions on alcohol use. This may have prompted better recall of drinking than when used alone. Hence, the study findings need to be replicated in contexts more similar to those in which alcohol screening measures are typically administered. Our criterion measures were not formal diagnostic interviews and represent, at best, a “silver”, rather than “gold”, standard for assessing alcohol use disorders. Ideally, the administration of screening measures should be randomized to reduce temporal order effects on performance. This could not be accomplished in our study as the AUDIT had to be administered in the screening interview to enable over-sampling of hazardous drinkers for the larger population study on alcohol use patterns and sexual risk behaviors. Thus, the RAPS4 measure, implemented in the subsequent main interview may have benefited from better recall of problem drinking. Administering both screeners in a contiguous interview, albeit separated in administration, could have also facilitated greater agreement between the two measures. Despite these limitations, the present study provides important information on the performance of four screening measures of AUDs in relation to more thorough AUD measures in a community sample in Goa. Study findings may facilitate decision making regarding screening for alcohol misuse in India and in developing countries with similar drinking patterns.
Acknowledgements
This work was supported by a R21 AA014773 grant from the National Institute on Alcohol Abuse and Alcoholism to the Alcohol Research Group. We thank staff at Sangath and community members of the selected areas of Goa for assistance with data collection.
APPENDIX A
APPENDIX A.
15-item alcohol-related consequence scale to assess for alcohol abuse and subscales
| Subscales | Items |
|---|---|
| Fight problem | I have gotten into a heated argument while drinking. |
| I have gotten into a fight while drinking | |
| Legal problem | A police officer, panchayat leader, community elder, NGO worker, priest, imam or pundit questioned or warned me because of my drinking. |
| I had trouble with the police, panchayat, NGO workers or community members (including religious leaders) about drinking when driving was not involved. | |
| I have been caught/threatened by the police or arrested for driving after drinking or riding. | |
| Hazardous use | My drinking contributed to getting involved in an accident in which someone else was hurt, or property, such as a bicycle, bike, scooter or car, was damaged. My drinking contributed to my getting hurt in an accident in a car, on a scooter, bike, bicycle or elsewhere |
| Health problem | I had an illness connected with drinking which kept me from working on my regular activities for a week or more. |
| I felt that my drinking was becoming a serious threat to my physical health. | |
| A doctor, vaid, hakim, compounder, health or NGO/CBO worker suggested I cut down on drinking. | |
| Work problem | have lost a job, or nearly lost one, because of drinking. |
| People at work indicated that I should cut down on drinking. | |
| Drinking may have hurt my chances for promotion, or salary increases or bonuses, or better jobs | |
| Other reactions | A spouse or someone I lived with got angry about my drinking or the way I behaved while drinking. |
| A spouse or someone I lived with threatened to leave me because of my drinking. |
Note: The health problem items were not included in estimated Alcohol Abuse as DSM-IV diagnostic criteria do not include health-related problems.
Appendix B
Appendix B. Domains and Items comprising DSM-IV dependence symptoms.
| DSM-IV criteria for substance dependence | Main Interview Item |
|---|---|
| Criteria # 3. The substance is often taken in larger amounts over a longer period than was intended. | Once I started drinking it was difficult for me to stop before I became completely intoxicated. I sometimes kept on drinking after I had promised myself not to. |
| Criteria #: 4: There is persistent desire or unsuccessful efforts to cut down or control substance use. | I deliberately tried to cut down or quit drinking, but I was unable to do so. I wanted to cut down or quit drinking. |
| Criteria #: 5: A great deal of time is spent in activities necessary to obtain the substance (e.g. visiting multiple doctors or driving long distances) use the substance, or recover from its effects | I spent a lot of my time on drinking or getting over the effects of drinking or doing things to get alcohol. |
| Criteria # 6. Important social, occupational, or recreational activities are given up or reduced because of substance use | My drinking has interfered with my spare time activities or hobbies leisure or family activities and interests. I have given up or reduced important work or social activities for my drinking. |
| Criteria # 7. The substance use is continued despite knowledge of having a persistent or recurrent problems | I kept on drinking although I knew that I had a health problem caused by or made worse by my drinking. I kept on drinking although I felt that my drinking was giving me psychological or emotional problems |
Criteria # :1. Tolerance as defined by either of the following
|
I needed more alcohol than I used to, to get the same effect as before. I found that the same amount of drinking had much less effect than it used to. |
Criteria#: 2. Withdrawal as manifested by either of the following:
|
My hands shook a lot the morning after drinking; Sometimes I have awakened during the night or early morning sweating all over because of drinking; I found that I needed a drink to keep from getting the shakes or becoming sick. I was sick or vomited after drinking or the morning after drinking; I was depressed, irritable or nervous after drinking or the morning after drinking. I have taken a strong drink in the morning to get over the effects of last night’s drinking. |
REFERENCES
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Text Revision [DSM-IV-TR] 4th ed. American Psychiatric Association; Washington, D.C.: 2000. [Google Scholar]
- Babor TF, de la Fuente JR, Saunders JB, Grant M. AUDIT: The Alcohol Use Disorders Identification Test. World Health Organization Programme on Substance Abuse; Geneva, Switzerland: 1992. Update of No. WHO/MNH/DAT/89.4. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT. The Alcohol Use Disorders Indentification Test. Guidelines for use in primary care [WHO/MSD/MSB/01.6a] 2nd ed. Department of Mental Health and Substance Dependence, World Health Organization; Geneva, Switzerland: 2001. [Google Scholar]
- Benegal V. India: alcohol and public health. Addiction. 2005;100(8):1051–1056. doi: 10.1111/j.1360-0443.2005.01176.x. [DOI] [PubMed] [Google Scholar]
- Benegal V, Nayak MB, Murthy P, Chandra PS, Gururaj G. Women and alcohol in India. In: Obot I, Room R, editors. Alcohol, Gender and Drinking Problems. Perspectives from low and middle income countries. World Health Organization; Geneva, Switzerland: 2005. pp. 89–123. [Google Scholar]
- Bracken BA, Barona A. State of the art procedures in translating, validating and using psychoeducational tests in cross-cultural assessment. School Psychology International. 1991;12:119–132. [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alchol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Caetano R, Greenfield TK. Trends in DSM-IV alcohol dependence: 1990 and 1995 U.S. national alcohol surveys. Alcohol Research Group, Public Health Institute; Berkeley, CA: 1997. [Google Scholar]
- Caetano R, Laranjiera R. A ‘perfect storm’ in developing countries: economic growth and the alcohol industry. Addiction. 2006;101(2):149–152. doi: 10.1111/j.1360-0443.2006.01334.x. [DOI] [PubMed] [Google Scholar]
- Caetano R, Tam TW. Prevalence and correlates of DSM-IV and ICD-10 alcohol dependence: 1990 U.S. National Alcohol Survey. Alcohol Alcohol. 1995;30(2):177–186. [PubMed] [Google Scholar]
- Carey KB, Carey MP, Chandra PS. Psychometric evaluation of the alcohol use disorders identification test and short drug abuse screening test with psychiatric patients in India. J Clin Psychiatry. 2003;64(7):767–774. doi: 10.4088/jcp.v64n0705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ. Screening for alcohol problems in the U.S. general population: a comparison of the CAGE and TWEAK by gender, ethnicity and service utilization. J Stud Alcohol. 1999;60:705–711. doi: 10.15288/jsa.1999.60.705. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. A brief screening instrument for problem drinking in the emergency room: the RAPS4. J Stud Alcohol. 2000;61:447–449. doi: 10.15288/jsa.2000.61.447. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. Screening for alcohol problems in the U.S. general population: comparison of the CAGE, and RAPS4, and RAPS4-QF by gender, ethnicity, and services utilization. Alcohol Clin Exp Res. 2002;26(11):1686–1691. doi: 10.1097/01.ALC.0000036300.26619.78. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Bazargan S. Screening for alcohol problems: comparison of the AUDIT, RAPS4, and RAPS4-QF among African American and Hispanic patients in an inner city emergency department. Drug Alcohol Depend. 2003;71(3):275–280. doi: 10.1016/s0376-8716(03)00140-6. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y, Bond J, Borges G, Cremonte M, Marais S, Poznyak V, Sovinova H, Moskalewicz J, Swiatkiewicz G. Cross-national performance of the RAPS4/RAPS4-OF for tolerance and heavy drinking: data from 13 countries. A research report from the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) and the WHO Collaborative Study on Alcohol and Injuries. J Stud Alcohol. 2005a;66:428–432. doi: 10.15288/jsa.2005.66.428. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y, Moskalewicz J, Swiatkiewicz G. Screening for alcohol problems in two emergency service samples in Poland: comparison of the RAPS4, CAGE, and AUDIT. Drug Alcohol Depend. 2005b;80(2):201–207. doi: 10.1016/j.drugalcdep.2005.03.025. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin Exp Res. 2005;29(5):844–854. doi: 10.1097/01.alc.0000164374.32229.a2. [DOI] [PubMed] [Google Scholar]
- D’Costa G, Nazareth I, Naik D, Vaidya R, Levy G, Patel V, King M. Harmful alcohol use in Goa, India, and its associations with violence: a study in primary care. Alcohol Alcohol. 2007;42(MarApr):131–137. doi: 10.1093/alcalc/agl103. [DOI] [PubMed] [Google Scholar]
- Gaunekar G, Patel V, Jacob KS, et al. Drinking patterns of hazardous drinkers: a multicenter study in India. In: A H, Simpson R, editors. Moonshine Markets. Brunner-Routledge; New York: 2004. pp. 125–144. [Google Scholar]
- Gaunekar G, Patel V, Rane A. The impact and patterns of hazardous drinking amongst male industrial workers in Goa, India. Social Psychiatry and Psychiatric Epidemiology. 2005;40:267–275. doi: 10.1007/s00127-005-0886-1. [DOI] [PubMed] [Google Scholar]
- Green DM, Swets JM. Signal detection theory and psychophysics. John Wiley and Sons Inc.; New York: 1966. [Google Scholar]
- Greenfield TK, Nayak MB, Bond J, Ye Y, Midanik LT. Maximum quantity consumed and alcohol-related problems: assessing the most alcohol drunk with two measures. Alcohol Clin Exp Res. 2006;30(9):1576–1582. doi: 10.1111/j.1530-0277.2006.00189.x. [DOI] [PubMed] [Google Scholar]
- Gupta PC, Saxena S, Pednekar M, Maulik P. Alcohol consumption among middle-aged and elderly men: a community study from Western India. Alcohol Alcohol. 2003;38(4):327–331. doi: 10.1093/alcalc/agg077. [DOI] [PubMed] [Google Scholar]
- Hasin DS. Classification of alcohol use disorders. Alcohol Res Hlth. 2003;27(1):5–17. [PMC free article] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. John Wiley & Sons; New York, NY: 2000. [Google Scholar]
- Li T-K, Hewitt BG, Grant BF. Is there a future for quantifying drinking in the diagnosis, treatment, and prevention of alcohol use disorders? Alcohol Alcohol. 2007;41(4):57–63. doi: 10.1093/alcalc/agl125. [DOI] [PubMed] [Google Scholar]
- Midanik L, Greenfield TK. Trends in social consequences and dependence symptoms in the United States: the National Alcohol Surveys, 1984-1995. Am J Public Health. 2000;90(1):53–56. doi: 10.2105/ajph.90.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohan D, Chopra A, Ray R, Sethi H. India. In: Demers A, Room R, Bourgault C, editors. Surveys of Drinking Patterns and Problems in Seven Developing Countries. Department of Mental Health and Substance Dependence, World Health Organization; Geneva, Switzerland: 2000. pp. 103–114. [Google Scholar]
- Nayak MB, Kerr WC, Greenfield TK, Pillai A. Not all drinks are created equal: Implications for alcohol assessment in India; Joint Scientific Meeting of the Research Society on Alcoholism and the International Society for Biomedical Research on Alcoholism; Washington, D.C.. 2008; Jun 27 2, Jul 27 2, p. 293A. Alcoholism: Clinical and Experimental Research. [Google Scholar]
- Neufeld KJ, Peters DH, Rani M, Bonu S, Brooner RK. Regular use of alcohol and tobacco in India and its association with age, gender, and poverty. Drug Alcohol Depend. 2005;77(3):283–291. doi: 10.1016/j.drugalcdep.2004.08.022. [DOI] [PubMed] [Google Scholar]
- Office of the Registrar General I. Census of India . Provisional population totals, Census of India 2001. Ministry of Home Affairs, Government of India; New Delhi, India: [accessed 4/14/03]. 2001. Part 1. www.censusindia.net/results/provindia1.html. [Google Scholar]
- Pal HR, Jena R, Yadav D. Validation of the alcohol use disorders identification test (AUDIT) in urban community outreach and de-addiction center samples in North India. J Stud Alcohol. 2004;65:794–800. doi: 10.15288/jsa.2004.65.794. [DOI] [PubMed] [Google Scholar]
- Patel V, Araya R, Chowdhary N, King M, Kirkwood B, Nayak S, Simon G, Weiss HA. Detecting common mental disorders in primary care in India: a comparison of five screening questionnaires. Psychol Med. 2007;38(18) doi: 10.1017/S0033291707002334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad R. Alcohol use on the rise in India. The Lancet. 2009;373(9657):17–18. doi: 10.1016/s0140-6736(08)61939-x. [DOI] [PubMed] [Google Scholar]
- Rumpf HJ, Hapke U, Meyer C, John U. Screening for alcohol disorders and at-risk drinking in the general population: psychometric performance of three questionnaires. Alcohol Alcohol. 2002;37(3):261–268. doi: 10.1093/alcalc/37.3.261. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG. WHO collaborative project on identification and treatment of persons with harmful alcohol consumption: report on phase I development of a screening instrument. World Health Organization, Division of Mental Health; 1987. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption -- II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Saxena S. Alcohol problems and responses: challenges for India. J Subst Abuse. 2000;5:62–70. [Google Scholar]
- Schafer J, Cherpitel CJ. Differential functioning of the CAGE, TWEAK, BMAST and AUDIT by gender and ethnicity. Contemp Drug Prob. 1998;25(2):399–409. [Google Scholar]
- Silva MC, Gaunekar G, Patel V, Kukalekar DS, Fernandes J. The prevalence and correlates of hazardous drinking in industrial workers: a study from Goa, India. Alcohol Alcohol. 2003;38(1):79–83. doi: 10.1093/alcalc/agg016. [DOI] [PubMed] [Google Scholar]
- Stata Corp . Stata Statistical Software: Release 10.0. Stata Corporation; College Station, TX: 2007. [Google Scholar]
- Vinson DC, Kruse RL, Seale JP. Simplifying alcohol assessment: two questions to identify alcohol use disorders. Alcohol Clin Exp Res. 2007;31(8):1392–1398. doi: 10.1111/j.1530-0277.2007.00440.x. [DOI] [PubMed] [Google Scholar]
- Woerle S, Roeber J, Landen MG. Prevalence of alcohol dependence among excessive drinkers in New Mexico. Alcohol Clin Exp Res. 2007;31(2):293–298. doi: 10.1111/j.1530-0277.2007.00305.x. [DOI] [PubMed] [Google Scholar]