Abstract
Telephone continuing care (TCC) was compared to usual continuing care (UCC) on substance use and related problems among adults discharged from residential treatment. Participants were randomly assigned to receive either UCC or TCC. A tapered TCC protocol, initiated by paraprofessional staff and volunteers, was provided during the first three months following discharge. The TCC condition participants reported high satisfaction ratings with the procedure and were more than twice as likely to enter continuing care than UCC participants. At the three-month point, TCC patients reported significantly fewer past month substance problems than UCC patients. Among the subgroup of lower severity (LS) participants, the TCC-LS sample had both significantly more days abstinent and fewer past month substance problems at three months than the UCC-LS sample. The significant between-group differences in substance use outcomes were not maintained at the six-month follow-up. The high satisfaction ratings and early, favorable response among TCC patients suggest the procedure is promising. Further research with larger samples and over a longer period of time is necessary.
Keywords: Substance abuse, continuing care, aftercare, telephone, residential treatment
1. Introduction
The chronic, relapsing nature of substance use disorders and the complexity of addiction has been well-documented (McKay et al., 2004; McLellan, Lewis, O’Brien, & Kleber, 2000; Saitz, Larson, LaBelle, Richardson, & Samet, 2008; White, 1996, 2008). However, outcome studies typically have not reflected expected recovery trajectories, but instead usually evaluate acute care interventions without continuing care. Though acute, single care episodes may be successful with some individuals, there is evidence that over half of the patients entering publicly-funded addiction programs require longer-term care, consisting of three to four episodes of various kinds of treatment over several years to sustain recovery (Dennis, Foss, & Scott, 2007; Dennis & Scott, 2007). Researchers have drawn a parallel between addiction and chronic medical illnesses such as asthma, diabetes, and hypertension (Donovan, 1998; McLellan et al., 2000; O’Brien & McLellan, 1996), and have suggested treatment methods focused on continuing care for individuals with substance use disorders.
There has been a noticeable shift in the field toward focusing on the feasibility and efficacy of various continuing care models in addiction treatment. The American Society of Addiction Medicine (ASAM) urges that individuals receiving treatment for a substance disorder receive continuing care following the initial treatment, in order to maintain progress or to provide intensified treatment if necessary (ASAM, 2001). McKay (2005) found support for the effectiveness of extended continuing care interventions when delivered through face-to-face contact and at a distance via telephone. These finding held across all types of interventions that were examined (e.g., behavioral treatment; pharmacological, and monitoring). Although correlational in nature, the length of participation in continuing care has been cited as the best predictor of positive outcomes at one year post-treatment (Moos, Finney, Ouimette, & Suchinsky, 1999). At present, the most common type of formal continuing care is the 12-step group (Donovan, 1998; McKay, 2001). Though effective for many, McKay (2001) acknowledged that attendance rates tend to be low and drop off rapidly when treatment is complete. Donovan (1998) recommended that providers take a more proactive role to increase client attendance and compliance with continuing care, and Compton and colleagues (2003) proposed a model of continuing care to directly address persistent vulnerability to relapse, including proactive recovery management checkups (Dennis, Scott, & Funk, 2003).
Since cost and time burdens are concerns associated with long-term continuing care, recent efforts to increase compliance with continuing care have included discussion of telephone delivery of care as a possibility. Telephone contact has been used most extensively with smoking cessation; meta-analyses of telephone counseling outcomes have shown that proactive calls consistently produce better smoking outcomes than control conditions (Lichtenstein, Glasgow, Lando, Ossip-Klein, & Boles, 1996; Stead, Perera, & Lancaster, 2006). Telephone care has also proven useful in the monitoring and treatment of chronic mental and physical illnesses, such as depression (Osgood-Hynes et al., 1998; Simon, VonKorff, Rutter, & Wagner, 2000), obsessive-compulsive disorder (Greist et al., 2002; Taylor et al., 2003), hypertension (Bosworth et al., 2005), diabetes (Kim & Oh, 2003), and rheumatology problems (Pal, 1998).
Telephone-based continuing care for substance use disorders is a relatively new concept, yet several researchers have demonstrated the potential benefits of this method with adult (Cacciola et al., 2008; McKay et al., 2004, 2005) and adolescent (Kaminer & Napolitano, 2004) substance users. Telephone continuing care is often more attractive and less burdensome to patients than other forms of continuing care, and manual-based telephone interventions may be just as effective in maintaining treatment gains as in-person interventions (Kaminer, Burleson, & Burke, 2008); however, support for this approach is not unequivocal. Hubbard and colleagues (2007) found no clear evidence of the efficacy of telephone utilization to encourage compliance with continuing care plans, though they acknowledged those receiving calls had a greater likelihood of documented attendance to continuing care than those who were not called.
Given the need for additional research in telephone-based continuing care, the goals of this study are to examine the feasibility and outcomes of an assertive, outreach-oriented telephone continuing care protocol for adults discharged from residential treatment. The present study tests the hypotheses that telephone continuing care will reach more patients with greater frequency and improved clinical outcomes than usual continuing care.
2. Materials and Methods
2.1 Participants
Participants in this study were 104 adult patients who met criteria for and were admitted to Level III residential substance abuse treatment as defined by ASAM’s Patient Placement Criteria for the Treatment of Psychoactive Substance Use Disorders (PPC-2R; American Society of Addiction Medicine, 2001). Adults were eligible to participate in this study if they were at least 18 years of age, met Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV-TR; American Psychiatric Association, 2000) substance abuse and/or dependence criteria, and resided in the designated multi-county central Illinois area at the time of admission to treatment.
Potential participants were excluded from the study if they did not plan on returning to one of the target counties, displayed uncontrolled psychotic symptoms, were deemed a danger to themselves or others, or did not remain in residential treatment at least seven days. Out of 198 patients admitted to residential treatment, 61 (31%) did not meet eligibility criteria. The most common reasons for ineligibility were failure to re-enter one of the designated counties upon discharge (57%) and not remaining in treatment for at least seven days (36%). Remaining patients (7%) were excluded from the study because they were immediately incarcerated upon discharge from residential treatment (n=3) or were enrolled in another study (n=1). One hundred and four (76%) of the 137 eligible patients agreed to participate in the study. Ninety-four participants (90%) completed the three-month follow-up interview, three refused, one was located but unavailable, and six could not be located. Eighty participants (85%) completed their three-month follow-up interview within one week plus or minus their 90-day post-discharge target date. At six-months post-discharge, 88 participants (85%) completed the interview, four refused, and twelve could not be located. Seventy-six participants (86%) completed their six-month follow-up interviews within one week plus or minus their 90-day post-six-month follow-up date. This analysis utilized data from both three- and six-month follow-up intervals. There were no significant differences in follow-up rates by condition.
The participants in this study averaged 31.6 years of age (range 19–56), and the majority were Caucasian (76%), male (60%), not currently married (85%), and involved with the criminal justice system (65%). There were 11% that reported being in school/training in the 90 days prior to intake, and 32% were currently employed. In terms of clinical characteristics, 84% self-reported dependence on alcohol or other drug, with 53% reporting cocaine dependence, 49% alcohol dependence, 26% cannabis dependence, and 14% opioid dependence. Most (63%) started using drugs before the age of 15 and had at least one prior episode of substance abuse treatment (64%). Co-occurring mental disorders were common, as 78% reported criteria for one or more disorders. Approximately half reported prior mental health treatment (see Table 1 and Table 2).
Table 1.
Participant Demographics by Condition (Column Percents)
| Total | |||
|---|---|---|---|
| Control (n=53) | Telephone (n=51) | ||
| Female | 34% | 47% | |
| Race | African American | 21% | 12% |
| Caucasian | 72% | 80% | |
| Hispanic | 0% | 0% | |
| Other/Mixed | 8% | 8% | |
| Non-white | 28% | 20% | |
| Age | 18–20 Years Old | 4% | 18% |
| 21–29 Years Old | 36% | 41% | |
| 31–39 Years Old | 38% | 22% | |
| 41–49 Years Old | 17% | 14% | |
| 50+ Years Old | 6% | 6% | |
| Family | |||
| Married/Living with someone | 19% | 12% | |
| Divorced/Separated/Widowed | 40% | 29% | |
| Never married | 42% | 59% | |
| Employment | |||
| In school | 8% | 14% | |
| Employed | 34% | 29% | |
| Current CJ Involvement\1 | 64% | 67% | |
Table 2.
Clinical Characteristics by Condition (Column Percents)
| Total | |||
|---|---|---|---|
| Control (n=53) | Telephone (n=51) | ||
| Age of First Use Under 15 | 57% | 69% | |
| Drug Use | Weekly Any Alcohol or Drug Use\1 | 74% | 82% |
| Weekly Alcohol Use\1 | 49% | 54% | |
| Weekly Marijuana Use\1 | 29% | 33% | |
| Weekly Crack/Cocaine Use\1 | 23% | 28% | |
| Weekly Heroin/Opiod Use\1 | 9% | 16% | |
| Weekly Other Drug Use\1 | 9% | 6% | |
| Substance Severity\2 | |||
| No use | 0% | 0% | |
| Use | 0% | 8% | |
| Abuse | 19% | 6% | |
| Dependence | 2% | 2% | |
| Physiological Dependence | 79% | 84% | |
| Prior SA Treatment Episodes | |||
| None | 30% | 41% | |
| One | 21% | 20% | |
| 2+ episodes | 49% | 39% | |
| Mental Health | |||
| High Traumatic Distress | 51% | 57% | |
| ADHD | 51% | 49% | |
| Conduct Disorder | 49% | 49% | |
| Major Depressive Disorder | 68% | 73% | |
| Generalized Anxiety Disorder | 42% | 59% | |
| Prior MH Treatment Episodes | |||
| Any Prior Treatment | 51% | 49% | |
During the past 90 days
Based on self report
2.2 Procedures
Patients were approached about participating in the study within 24 hours of admission to residential treatment. The study was explained to each person as part of the informed consent process as approved and monitored by Chestnut Health Systems’ Institutional Review Board. All patients who met inclusion criteria, remained in residential treatment for at least seven days, and agreed to voluntarily participate in the study were randomized into one of two conditions by the research coordinator: Usual Continuing Care (UCC) or Telephone Support + Usual Continuing Care (TCC). Randomization resulted in 53 (51%) participants assigned to the UCC condition and 51 (49%) to the TCC condition. Participants were interviewed at admission to residential treatment and at three-and six-months post-discharge. For each completed post-discharge interview, participants were compensated $35 for time and transportation and earned an additional $10 for completing the interview within two weeks before or after the due date.
2.3 Residential Treatment
Length of stay in the residential treatment program was based on individual needs, with an average stay of 21 to 28 days. The average length of stay for this sample was 24 days (range of 9 to 44 days), and 86.5% were successfully discharged. The residential program followed a psychosocial abstinence model and community 12-step group participation. The treatment program included rotating group sessions on: (a) 12-step facilitation; (b) counseling; (c) spirituality; (d) assertiveness training; (e) relapse prevention; (f) coping styles based on the MMPI clinical scales; (g) stress management; (h) decision-making; (i) self-esteem; (j) recreation; (k) drug education; and (l) living and health skills. Family and parenting groups were also available one evening per week. All patients with planned discharges left the residential program with a continuing care plan. Plans typically included recommendations for outpatient substance abuse continuing care treatment and for attendance at 12-step groups in the community. As needed, additional referrals were made for other services, including: (a) psychiatric counseling; (b) criminal justice system monitoring; and (c) educational services.
2.4 Continuing Care Conditions
UCC protocol
Prior to discharge from residential treatment, all patients completed a continuing care plan, and counselors made referrals to other services according to the plan, including referral to an outpatient continuing care counselor. Typically, the first continuing care appointment was scheduled for one to three weeks from the date of discharge. Outpatient continuing care consisted of weekly group counseling for 1.5 hours in gender-specific groups. Group counseling topics were related to patients’ continuing care goals including relapse prevention and skill related topic areas, such as anger management, communication, and problem solving. Group leaders presented topics for discussion, and patients were encouraged to participate by drawing upon their recent life experiences to learn how they could better deal with stressors and triggers for substance use. Patients were also encouraged to discuss their progress and problems with early post-discharge recovery. Licensed master’s level clinicians provided group counseling.
TCC protocol
In addition to customary continuing care planning, participants in this condition were assigned to one of five telephone support workers for a 90-day period. Telephone support workers were paraprofessional staff or volunteers who had obtained a bachelor’s degree in a human service field, such as psychology, social work, etc., and had either work experience in prevention, treatment, or research programs for substance use disorders, or they had personal recovery experience including participation in treatment or 12-step meetings. They were recruited and trained to call participants once each week during the first month following residential discharge and approximately once every two weeks over the subsequent two months. During calls, telephone support workers followed a manual-guided protocol that asked participants about formal support involvement (e.g., aftercare counseling and/or 12-step meetings) and substance use status (i.e., usage and abstinence) and offered referrals for additional help if appropriate. Telephone support workers were trained to use a positive, supportive tone of voice, avoid confrontation, and look for opportunities to provide praise and encouragement for recovery-consistent behaviors described by participants. If participants were experiencing stress or described relapse situations, workers avoided judgment or lecturing; instead, they asked the participant to describe what steps they could follow to reduce stress, correct a relapse, or how they would seek help. When necessary, workers made additional suggestions and asked if they could provide assistance in linking them back to their counselor (e.g., make a direct call on their behalf to get an appointment time). Prior to completing a telephone session, workers sought to obtain agreement on specific recovery activities the participant would do prior to the next call. Telephone sessions were typically 20 minutes or less.
2.5 Telephone Support Protocol Fidelity
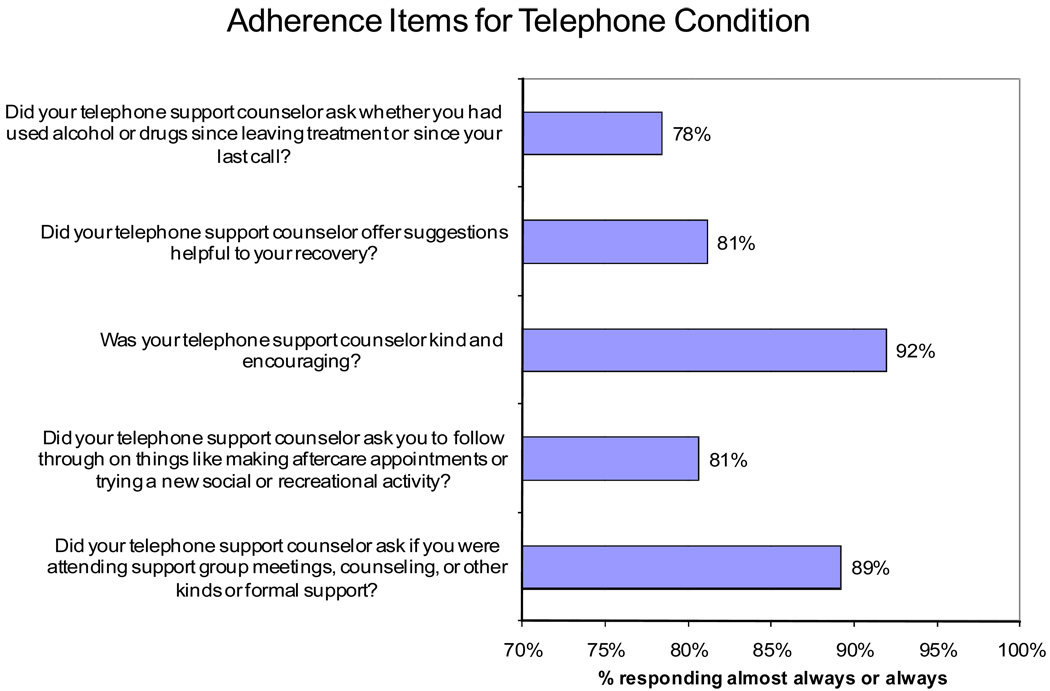
To ensure that workers adhered to the telephone support protocol, all telephone support sessions were audio taped with the participant’s permission, and a random sample was reviewed during weekly supervision meetings. During each call, workers completed a Telephone Support Documentation Form to record all contacts and conversations and to guide interactions with participants. These documentation forms were designed to both guide the worker through a call and help him/her follow the manual-guided protocol. A new form was completed for each contact, then turned in to and reviewed by the principal investigator. Both positive and corrective feedback was given to telephone support workers based on how well their documentation reflected the protocol in the manual. Adherence to the protocol was also measured from the participants’ perspective, and these findings are presented in Figure 1. Across five protocol adherence items, most participants reported that telephone support workers followed the protocol.
Figure 1.
Adherence Items for Telephone Condition
2.6 Materials and Measures
Global Appraisal of Individual Needs (GAIN)
Baseline and follow-up data were gathered using the Global Appraisal of Individual Needs (GAIN; Dennis, 1991). The GAIN is a standardized clinical assessment that has been normed on both adults and adolescents (Dennis, Scott, Godley, & Funk, 1999; 2000). Item content is divided into the following eight main sections: Background, Substance use, Physical health, Risk behaviors, Mental health, Environment, Legal, and Vocational. It provides over 100 symptom, change score, and utilization indices and is designed to map onto ASAM’s Patient Placement Criteria for the Treatment of Psychoactive Substance Use Disorders (PPC-2R; American Society of Addiction Medicine, 2001), the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV-TR; American Psychiatric Association, 2000) diagnostic criteria, and several public data sets. Core indices have Cronbach alphas over .85 (most over .9). Diagnoses based on the GAIN have been shown to have good test-retest reliability for substance use disorders (kappa = .06; Dennis et al., 2002) and accurately predict independent and blind staff psychiatric diagnoses of co-occurring psychiatric disorders including ADHD (kappa = 1.00), Mood Disorders (kappa = 0.85), Conduct Disorder/Oppositional Defiant Disorder (kappa = .69), or the lack of non-substance use diagnoses (kappa = .91) (Shane, Jasiukaitus, & Green, 2003). The test-retest data were also generally very good (.7–.9) on both the scales and individual questions.
Percent of days abstinent
This measure was created from a single item, “how many days, in the past 90 days, did you go without using alcohol or other drugs,” asked at each time point. This answer was divided by 90 to obtain percent of days abstinent. Previous research on the GAIN 90-day substance use items was shown to be comparable with the time-line follow-back method (Dennis, Funk, Godley, Godley, & Waldron, 2004)
Substance problems
The Substance Problem Scale (SPS) was used to assess problems related to AOD use or AOD using behavior. It is based on recency ratings (i.e., past month, 2–12 months ago, more than 12 months ago, or never) on 16 symptoms: Seven corresponding to DSM-IV criteria for dependence, four for abuse, two for AOD-induced health and psychological problems, and three on lower severity symptoms of use (e.g., hiding use, people complaining about use, weekly use). On this sample, this scale showed good internal consistency with coefficient alpha=.93.
AccuSign© DOA 2 THC/COC
In order to assess the validity of self-reported substance use, participants were asked to provide a urine sample as part of the three-month follow-up. Samples were screened using the AccuSign© DOA 2 THC/COC (Princeton BioMeditech Corporation, Princeton, NJ) on-site, one step qualitative immunochromatographic assay. This test adopts the Substance Abuse and Mental Health Services Agency (SAMHSA) recommended cutoff detection levels for THC (50ng/mL) and cocaine (300ng/mL) metabolites. We obtained urine samples from 80% of participants. We could not obtain samples from all three-month interviews, as some interviews were completed by telephone or while the participant was in a controlled environment. If a participant reported no past month substance use but tested positive for an illicit substance, the self-report was considered to be a “false negative” (FN) response. The kappa for self-reported past-month marijuana use and a positive screen was 0.68, and the FN rate was 5.4% (58 participants reported no use and of those, 54 had marijuana-free urine samples). For past-month cocaine use, kappa was 0.57, with a FN rate of 6.8% (62 reported no use and of those, 57 had cocaine-free urine samples). For the combined past-month use of either drug versus positive screen for either, kappa was 0.69 with a 6.8% FN rate (51 reported no use and of those, 46 had marijuana and cocaine-free urine samples). The study-wide FN rate was relatively low and there were no significant differences by condition. Thus, outcome analyses were conducted on self-reported substance use data.
Satisfaction with telephone support survey
As an additional part of the three-month follow-up interview, TCC participants were asked about their experience with the telephone support intervention. Specifically, they were asked to report on a five-point Likert scale, their level of satisfaction with receiving support calls, their support worker, and the length and duration of the call.
Telephone support counselor log
Telephone support workers documented all call attempts to TCC participants on a standard form, including date and time of the call.
2.7 Data Analysis
All analyses were conducted with SPSS Version 16.0 (2007). An “intent to treat” model was utilized. Differences in intake characteristics by condition were examined by chi-square analysis, analysis for continuous variables was examined by independent sample t-test, and continuous outcomes were examined using one-way analysis of covariance (ANCOVA), where the factor was the two experimental conditions, and the covariate was the intake version of the outcome (used to control for initial severity). Missing data was minimal across the variables used in the analysis, ranging from 0–3% missing. Listwise deletion was used to handle missing data due to the small number of missing cases. Cohen’s effect size ‘d’ was calculated on differences in outcomes by experimental condition, with the difference between the two means being compared for the numerator, and the pooled standard deviation used for the denominator.
3. Results
3.1 Treatment Conditions at Intake
Participants in TCC and UCC were compared on demographic, diagnostic, and problem severity variables upon entry into residential treatment. No significant differences among the treatment conditions were found in the full sample on demographic variables; however, there was a significant difference in substance severity, with UCC participants reporting more abuse and TCC participants reporting more use and physiological dependence. No significant differences were found with planned residential discharge rates (TCC = 86.3%, UCC = 86.8%) or length of stay in residential treatment (TCC = 23.8 days, UCC = 24.3 days).
3.2 Participation in Continuing Care
Usual continuing care was available to both sets of participants. The average number of outpatient sessions attended was 3.3 (SD = 5.3) for UCC and 2.1 (SD = 3.6) for TCC. Reporting averages for this skewed distribution obscures the fact that 63% of the UCC group received no continuing care outpatient services. Because of the skewed outpatient services distribution, we tested for significance with the nonparametric Mann-Whitney test for two independent samples. The test revealed no significant difference by condition for UCC outpatient session attendance. Patients in the telephone condition averaged three completed TCC calls out of eight planned calls. Thus, with the addition of TCC phone sessions, the average number of continuing care sessions received by TCC participants was 5 (SD = 5.0) and the median increased from 0 to 4 sessions, compared to 3.3 (SD=5.3) and a median of 0 for the UCC participants. The Mann-Whitney test was significant with ranked sessions attended higher for the TCC, condition U = 681.0, p < 0.01. The addition of TCC also lead to a significant difference in the percentage of individuals participating in continuing care with TCC participants initiating at a rate of 79% and UCC participants initiating at 37% (χ2(1) = 17.2, p<0.05).
3.3 Outcome Analyses
Percentage of days abstinent
Data on percentage of days abstinent for both TCC and UCC conditions are presented in Table 3. At baseline, participants were abstinent on 42% of the 90 days preceding their entry into residential treatment. The percentage increased to 91% during the three-month continuing care phase of the follow-up and then declined to 86% at the six-month follow-up point. Participants in the TCC condition did not differ significantly from those in the UCC condition at any time point.
Table 3.
Percentage of days abstinent from substances and substance problem severity
| Baseline |
1–3 months |
4–6 months |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Sample | M | SD | n | M | SD | n | M | SD | n |
| Percent of Days Abstinent | |||||||||
| TCC | 39.56 | 38.11 | 38 | 91.98 | 17.45 | 38 | 87.39 | 22.20 | 38 |
| UCC | 44.39 | 36.01 | 43 | 89.77 | 19.90 | 43 | 84.64 | 29.41 | 43 |
| Effect size | −0.13 | 0.12 | 0.11 | ||||||
| Substance Problem Scale (Past Month) | |||||||||
| TCC | 8.46 | 5.07 | 41 | 1.44 | 3.29 | 41 | 1.20 | 3.05 | 41 |
| UCC | 8.00 | 5.54 | 44 | 3.20 | 5.21 | 44 | 2.27 | 4.38 | 44 |
| Effect size | 0.09 | −0.40 * | −0.28 | ||||||
| Low Severity | |||||||||
| Percent of Days Abstinent | |||||||||
| TCC | 54.65 | 35.32 | 27 | 97.03 | 6.27 | 27 | 92.90 | 14.98 | 27 |
| UCC | 56.90 | 31.73 | 33 | 90.75 | 16.64 | 33 | 85.87 | 29.01 | 33 |
| Effect size | −0.07 | 0.47 * | 0.30 | ||||||
| Substance Problem Scale (Past Month) | |||||||||
| TCC | 8.17 | 5.44 | 29 | 0.69 | 2.38 | 29 | 0.69 | 2.63 | 29 |
| UCC | 7.12 | 5.61 | 34 | 3.29 | 5.15 | 34 | 2.26 | 4.30 | 34 |
| Effect size | 0.19 | −0.61 ** | −0.43 | ||||||
Note. TCC = Telephone condition; UCC = Control condition.
Effect size calculation: (TCC mean-UCC mean)/pooled standard deviation
p < .05
p < .01
Past month substance problems
Table 3 also contains data on past month substance problems for both conditions. At baseline, both conditions had similar rates of past month substance problems (UCC=8, TCC=8.5). With intake substance problems as the covariate, there is significance by condition at three months, with TCC reporting significantly fewer past month substance problems than UCC (F(1,91)=6.30, p<.05). At six months, there are no significant differences by condition.
Additional variables
We also compared the two conditions on days of inpatient and outpatient substance abuse treatment and 12-step attendance, and there was no significant difference by condition on these variables at three or six months. Days of mental health treatment at three or six months by condition were also not significant. There was a within condition significant improvement in employment for the TCC condition, but the between group comparison using logistic regression analysis was not significant.
Low severity subgroup analysis
Given findings from some prior research suggesting that TCC may be more effective for patients with lower severity substance use (McKay et al., 2005), we conducted additional analyses examining this subgroup specifically. The lower severity (LS) sample was comprised of participants in each condition with values on the AOD use variable below the 75th percentile at intake. We analyzed the LS sample data using ANCOVA with baseline values of the outcome variable as the covariate for the two main substance use outcomes. Significant differences at the three-month follow-up interval were found for percent of days abstinent, F(1,67) = 4.25, p < .05, d = .47, with TCC-LS having a higher average percent of days abstinent (M = 97%, SD = 0.06) than UCC-LS (M = 91%, SD = 0.17). We also found a significant increase in the effect for TCC on the substance problems scale at three months, with TCC-LS having an average of 0.7 (SD = 2.4) problems and UCC-LS reporting an average of 3.3 (SD = 5.1); F(1,67) = 9.86, p < .01, d = −0.61. There were no significant differences by condition at intake or at six months for this subgroup analysis (see Table 3).
Continuing care initiation rates for the lower severity sample were similar to those reported for the full sample. TCC-LS participants initiated at a rate of 74%, and UCC-LS participants initiated at 33% (χ2(1) = 11.3, p<0.01). The average number of UCC sessions attended was 3.5 (SD = 5.6) for UCC and 2.4 (SD = 3.9) for TCC. Testing for significance with the nonparametric Mann-Whitney test revealed no significant difference by condition. With the addition of TCC sessions, the mean number of continuing care sessions received by TCC participants was 5.4 (SD = 5.4) compared to 3.5 (SD = 5.6) for the UCC participants. The Mann-Whitney test was significant with ranked sessions attended higher for TCC, condition U = 398.5, p < 0.05.
3.4 Participant Satisfaction
The majority of TCC participants reported that they liked (“sometimes” or “always”) receiving calls from their telephone support counselor (89%) and would recommend that calls continue beyond three months post-treatment (72%). They also reported that their telephone support counselor was “never” (95%) demanding or expecting too much, that they were able to speak with their telephone support counselor for the “right amount of time” (85%), and that the length of the telephone calls was “just right” (91%).
4. Discussion
Recent evidence suggests that telephone continuing care may be a cost-effective, and for many patients, a more acceptable, alternative to individual or group counseling (McKay et al., 2005). Three separate lines of evidence from the present study provide support for this emerging approach to continuing care. First, the TCC group was significantly more likely to receive continuing care sessions than the UCC group. Second, the clinical outcome findings for the full sample were mixed, with a significant decrease in abuse/dependence symptoms for the TCC group but no significant difference noted in percentage of days abstinent from AOD. However, both clinical outcomes resulted in significant findings for the low-severity TCC sample relative to the low-severity UCC sample at the initial follow-up interval. Third, despite the fact that it was challenging to reach TCC participants for their TCC sessions, nearly a 3:1 margin indicated they liked receiving the calls and thought they should continue beyond the study period. Interestingly, the clinical outcome data lends support for extending calls six months or longer since the significant effects favoring TCC for both clinical outcomes were reduced to statistical trends at the six-month follow-up. Though several investigators (Donovan, 1998; McKay, 2005; White, 2008) provide evidence of the feasibility and effectiveness of extended interventions, there continue to be questions related to how “extended” an extended intervention should be, how to appropriately adapt level of care when needed, and how much onus to place on the individual to comply with monitoring. The present study suggests the feasibility of a three-month paraprofessional-initiated telephone monitoring and support approach, but also suggests the need to go beyond that. Further research is needed to test whether an assertive, outreach approach such as this can be sustained over longer periods of time and whether it can result in stepped-up care (if needed) or improved attendance at mutual aid meetings. Prior research points to this possibility (Mensinger, Lynch, TenHave, & McKay, 2007), but telephone continuing care in the present study did not lead to improved 12-step meeting attendance or greater participation in UCC sessions.
While there were no formal economic analyses associated with this investigation, the fact that TCC sessions were brief (<20 minutes) and were delivered by paraprofessional staff and volunteers is likely to prove cost-efficient. However, employing paraprofessionals or relying on volunteers does raise the question of whether it is clinically appropriate. Within many treatment systems, paraprofessionals or volunteers are used to augment clinical duties by providing recreation, transportation to 12-step meetings, or other supportive duties, and it is within this framework that our TCC paraprofessionals served by following a prescribed written telephone protocol. By conducting protocol training, monitoring adherence, and regular TCC tape-reviews during supervision meetings, it was feasible for paraprofessionals to deliver telephone continuing care to monitor and support patients after discharge from residential treatment. Whether TCC might be more effective if delivered by professional therapists using a more active counseling approach (e.g., motivational enhancement training and cognitive behavior therapy) or a supportive approach has been evaluated with smoking cessation. Mermelstein and her colleagues (2003) found no significant difference in smoking abstinence rates between basic support calls with no counselor-initiated goal setting and “enhanced” telephone counseling that provided specific focus on an individual’s problem areas. Future continuing care research in alcohol and drug treatment should study the effectiveness and cost-effectiveness of these different forms of telephone continuing care.
4.1 Strengths and Limitations
This study has several strengths, including random assignment, good recruitment and follow-up rates, the use of biological drug tests, assessment of protocol adherence, and acceptability to patients. An additional strength is that, unlike many previous studies, we included individuals who failed to complete treatment. Whether this subgroup can benefit from telephone continuing care is unclear and should be researched in larger scale studies. Limitations include the brief follow-up period and small sample size. The small sample size limits the generalizability of findings and the follow-up period should be extended to better understand the long-term effectiveness of this continuing care intervention. Another limitation was that the completion of the planned telephone sessions was less than designed. In the present study, paraprofessionals initiated approximately six call attempts for every completed telephone session. This was in part due to several participants having temporary living arrangements and moving one or more times within the first three months after residential discharge. Future research to determine more effective ways to reach patients by telephone is needed. Finally, the method of selecting lower severity patients for subgroup analysis should be replicated in future studies with a larger sample size to further determine whether telephone continuing care is more effective and cost-effective with this subgroup.
4.2 Implications
Telephone follow-up after surgery or to monitor chronic medical conditions is increasingly common, and most people have a positive reaction to this type of outreach checkup. With increasing frequency, telephone continuing care is being tested in the long-term management of medical, mental, and substance use disorders. It allows for flexible scheduling, easy accessibility, and patient satisfaction is generally high. Results of this study indicate a similar reaction, although it is possible that may diminish somewhat the further out in time calls are extended. Moreover, it typically required several call attempts to complete a single call with patients from a publicly subsidized treatment program. Operating a telephone continuing care service by using procedures similar to those developed for longitudinal tracking and interviewing of research participants (Scott, 2004) should improve the efficiency of successfully reaching patients. Following the recovery monitoring and re-intervention logic in the work of Dennis et al. (2002) and McKay (2006), larger scale randomized trials of TCC are needed and should be tested over an extended post-discharge period. Continued attention should be focused on studying whether lower severity patients might respond best to such interventions, while making face-to-face, stepped-up interventions available to higher severity patients as well as others who experience relapse.
Acknowledgments
The development of this paper was supported in part by RO1 AA 010368. The authors thank Glenn Covert and Tammy Rodgers for their support of this study and Anna Carlson, Amanda Collins, Jennifer Long, and Jessica Stiffler for their assistance. The authors also wish to acknowledge Stephanie Merkle and Kelli Wright for their assistance in preparing this manuscript. The opinions are those of the authors and do not reflect official positions of the government. Please direct correspondence to M.Godley, Chestnut Health Systems, 448 Wylie Drive, Normal, IL 61761; E-mail: mgodley@chestnut.org; Phone: 309-451-7800.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mark D. Godley, Director, Research and Development, Chestnut Health Systems, 448 Wylie Dr., Normal, IL 61761, Telephone: 309-451-7800, Fax: 309-451-7761. mgodley@chestnut.org
Victoria H. Coleman-Cowger, Research Scientist, Chestnut Health Systems, 448 Wylie Dr., Normal, IL 61761.
Janet C Titus, Research Psychologist, Chestnut Health Systems, 448 Wylie Dr., Normal, IL 61761.
Rodney R Funk, Research Associate, Chestnut Health Systems, 448 Wylie Dr., Normal, IL 61761.
Matthew G. Orndorff, Project Manager, Chestnut Health Systems, 448 Wylie Dr., Normal, IL 61761.
References
- American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: 2000. Text Revision, DSM-IV-TR)Author. [Google Scholar]
- American Society of Addiction Medicine (ASAM) ASAM patient placement criteria for the treatment of substance-related disorders. 2nd ed. Chevy Chase, MD: 2001. Revised, ASAM PPC-2R)Author. [Google Scholar]
- Bosworth HB, Olsen MK, Gentry P, Orr M, Dudley T, McCant F, et al. Nurse administered telephone intervention for blood pressure control: A patient-tailored multifactorial intervention. Patient Education and Counseling. 2005;57:5–14. doi: 10.1016/j.pec.2004.03.011. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Camilleri AC, Carise D, Rikoon SH, McKay JR, McLellan AT, et al. Extending residential care through telephone counseling: Initial results from the Betty Ford Center Focused Continuing Care protocol. Addictive Behaviors. 2008;33:1208–1216. doi: 10.1016/j.addbeh.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Glantz M, Delany P. Addiction as a chronic illness: Putting the concept into action. Evaluation and Program Planning. 2003;26:353–354. [Google Scholar]
- Dennis ML. Global Appraisal of Individual Needs (GAIN) Bloomington, IL: Chestnut Health Systems; 1991. [Google Scholar]
- Dennis ML, Foss MA, Scott CK. An eight-year perspective on the relationship between the duration of abstinence and other aspects of recovery. Evaluation Review. 2007;31:585–612. doi: 10.1177/0193841X07307771. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Funk RR, Godley SH, Godley MD, Waldron H. Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction. 2004;99:120–128. doi: 10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Scott CK. Managing addiction as a chronic condition. Addiction Science and Clinical Practice. 2007;4:45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Scott CK, Funk RR. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Evaluation and Program Planning. 2003;26:339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Scott CK, Godley MD, Funk RR. Bloomington, IL: Chestnut Health Systems; 1999. Comparisons of adolescents and adults by ASAM profile using GAIN data from the Drug Outcome Monitoring Study (DOMS): Preliminary data tables. Retrieved from http://www.chestnut.org/li/posters/asamprof.pdf. [Google Scholar]
- Dennis ML, Scott CK, Godley MD, Funk RR. Predicting outcomes in adult and adolescent treatment with case mix vs. level of care: Findings from the Drug Outcome Monitoring Study. Drug and Alcohol Dependence. 2000;60 Suppl 1:S51. [Google Scholar]
- Dennis ML, Titus JC, White MK, Unsicker J, Hodgkins D. Global Appraisal of Individual Needs (GAIN): Administration guide for the GAIN and related measures. Bloomington, IL: 2002. Retrieved from http://www.chestnut.org/li/gain. [Google Scholar]
- Donovan DM. Continuing care: Promoting the maintenance of change. In: Miller WR, Heather N, editors. Treating addictive behaviors. 2nd ed. New York: Plenum; 1998. pp. 317–336. [Google Scholar]
- Greist JH, Marks IM, Baer L, Kobak KA, Wenzel KW, Hirsch MJ, et al. Behavior therapy for obsessive-compulsive disorder guided by a computer or by a clinician compared with relaxation as a control. Journal of Clinical Psychiatry. 2002;63:138–145. doi: 10.4088/jcp.v63n0209. [DOI] [PubMed] [Google Scholar]
- Hubbard RL, Leimberger JD, Haynes L, Patkar AA, Holter J, Liepman MR, et al. Telephone enhancement of long-term engagement (TELE) in continuing care for substance abuse treatment: A NIDA clinical trials network (CTN) study. American Journal on Addictions. 2007;16:495–502. doi: 10.1080/10550490701641678. [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Burleson JA, Burke RH. Efficacy of outpatient aftercare for adolescents with alcohol use disorders: A randomized controlled study. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:1405–1412. doi: 10.1097/CHI.0b013e318189147c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminer Y, Napolitano C. Dial for therapy: Aftercare for adolescent substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:1171–1174. doi: 10.1097/01.chi.0000133260.98666.bf. [DOI] [PubMed] [Google Scholar]
- Kim H, Oh J. Adherence to diabetes control recommendations: Impact of nurse telephone calls. Journal of Advanced Nursing. 2003;44:256–261. doi: 10.1046/j.1365-2648.2003.02800.x. [DOI] [PubMed] [Google Scholar]
- Lichtenstein E, Glasgow RE, Lando HA, Ossip-Klein DJ, Boles SM. Telephone counseling for smoking cessation: Rationales and meta-analytic review of evidence. Health Education Research. 1996;11:243–257. doi: 10.1093/her/11.2.243. [DOI] [PubMed] [Google Scholar]
- McKay JR. Recent developments in alcoholism: The role of continuing care in outpatient alcohol treatment programs. In: Galanter M, editor. Services research in the era of managed care. Vol. 15. New York: Plenum; 2001. pp. 357–372. [DOI] [PubMed] [Google Scholar]
- McKay JR. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100:1594–1610. doi: 10.1111/j.1360-0443.2005.01208.x. [DOI] [PubMed] [Google Scholar]
- McKay JR. Continuing care in the treatment of addictive disorders. Current Psychiatry Reports. 2006;8:355–362. doi: 10.1007/s11920-006-0036-9. [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Pettinati HM. The effectiveness of telephone-based continuing care for alcohol and cocaine dependence: 24-month outcomes. Archives of General Psychiatry. 2005;62:199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Ratichek S, Morrison R, Koppenhaver J, Pettinato HM. The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12-month outcomes. Journal of Consulting and Clinical Psychology. 2004;72:967–979. doi: 10.1037/0022-006X.72.6.967. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. Journal of the American Medical Association. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- Mensinger JL, Lynch KG, TenHave TR, McKay JR. Mediators of telephone-based continuing care for alcohol and cocaine abuse. Journal of Consulting and Clinical Psychology. 2007;75:775–784. doi: 10.1037/0022-006X.75.5.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mermelstein R, Hedeker D, Wong SC. Extended telephone counseling for smoking cessation: Does content matter? Journal of Counseling and Clinical Psychology. 2003;71:565–574. doi: 10.1037/0022-006x.71.3.565. [DOI] [PubMed] [Google Scholar]
- Moos RH, Finney J, Ouimette PC, Suchinsky RT. A comparative evaluation of substance abuse treatment: I Treatment orientation, amount of care, and one-year outcomes. Alcoholism: Clinical and Experimental Research. 1999;23:529–536. [PubMed] [Google Scholar]
- O’Brien CP, McLellan AT. Myths about the treatment of addiction. Lancet. 1996;347:237–240. doi: 10.1016/s0140-6736(96)90409-2. [DOI] [PubMed] [Google Scholar]
- Osgood-Hynes DJ, Greist JH, Marks IM, Baer L, Henerman SW, Wensel KW, et al. Self-administered psychotherapy for depression using a telephone-accessed computer system plus booklets: An open U.S.-U.K. study. Journal of Clinical Psychiatry. 1998;59:358–365. doi: 10.4088/jcp.v59n0704. [DOI] [PubMed] [Google Scholar]
- Pal B. Following up outpatients by telephone: Pilot study. British Medical Journal. 1998;316:1647–1650. doi: 10.1136/bmj.316.7145.1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Larson MJ, LaBelle C, Richardson J, Samet JH. The case for chronic disease management for addiction. Journal of Addiction Medicine. 2008;2:1–11. doi: 10.1097/ADM.0b013e318166af74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott CK. A replicable model for achieving over 90% follow-up rates in longitudinal studies of substance abusers. Drug and Alcohol Dependence. 2004;74(1):21–36. doi: 10.1016/j.drugalcdep.2003.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shane P, Jasiukaitis P, Green RS. Treatment outcomes among adolescents with substance abuse problems: The relationship between comorbidities and post-treatment substance involvement. Evaluation and Program Planning. 2003;26:393–402. [Google Scholar]
- Simon GE, VonKorff M, Rutter C, Wagner E. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. British Medical Journal. 2000;320:550–554. doi: 10.1136/bmj.320.7234.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SPSS. Statistical Program for the Social Sciences. Chicago, IL: SPSS, Inc; 2007. Version 16.0. [Google Scholar]
- Stead LF, Perera R, Lancaster T. Telephone counseling for smoking cessation. Cochrane Database of Systematic Reviews. 2006;3:CD002850. doi: 10.1002/14651858.CD002850.pub2. [DOI] [PubMed] [Google Scholar]
- Taylor S, Thordarson DS, Spring T, Yeh AH, Corcoran KM, Eugster K, et al. Telephone-administered cognitive behavior therapy for obsessive-compulsive disorder. Cognitive Behavior Therapy. 2003;32:13–25. doi: 10.1080/16506070310003639. [DOI] [PubMed] [Google Scholar]
- White WL. Pathways from the culture of addiction to the culture of recovery: A travel guide for addiction professionals. 2nd ed. Center City, MN: Hazelden; 1996. [Google Scholar]
- White WL. Pittsburgh, PA: Northeast Addiction Technology Transfer Center, Great Lakes Addiction Technology Transfer Center, Philadelphia Department of Behavioral Health and Mental Retardation Services; 2008. Recovery management and recovery-oriented systems of care: Scientific rationale and promising practices. [Google Scholar]