Abstract
Objectives:
The primary objective was to compare a single, 6 ml, intra-articular injection of hylan G-F 20 with placebo in patients with symptomatic knee osteoarthritis. The safety of a repeat injection of hylan G-F 20 was also assessed.
Methods:
Patients with primary osteoarthritis knee pain were randomly assigned to arthrocentesis plus a 6 ml intra-articular injection of either hylan G-F 20 or placebo in a prospective, double-blind (one injector/one blinded observer) study. Results were evaluated at 4, 8, 12, 18 and 26 weeks post-injection. The primary outcome criterion was change from baseline over 26 weeks in Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index A pain. Secondary outcome measures included WOMAC A1 and C, patient global assessment (PGA) and clinical observer global assessment (COGA) and Outcome Measures in Rheumatology, Osteoarthritis Research Society International responder rates. A 4-week, open, repeat treatment phase evaluated safety only.
Results:
A total of 253 patients (Kellgren–Lawrence grade II or III) was randomly assigned. Patients receiving hylan G-F 20 experienced statistically significantly greater improvements in WOMAC A pain scores (−0.15, SE 0.076, p = 0.047), and several of the secondary outcome measures (WOMAC A1, PGA and COGA), than patients receiving placebo. There was no difference between the safety results of the two groups. No increased risk of local adverse events was observed in the open, repeat treatment phase.
Conclusions:
This placebo-controlled study demonstrated that, in patients with knee osteoarthritis, a single 6 ml intra-articular injection of hylan G-F 20 is safe and effective in providing statistically significant, clinically relevant pain relief over 26 weeks, with a modest difference versus placebo.
Trial registration number:
Osteoarthritis is the most common joint disease and one of the most frequent causes of physical impairment.1 Osteoarthritis of the knee has been associated with a decrease in the elasticity and viscosity of the synovial fluid,2 3 4 which may alter the transmission of mechanical forces to the cartilage, possibly increasing its susceptibility to mechanical damage, or wear and tear. Viscosupplementation addresses the degradation of hyaluronic acid (HA) in the synovial fluid of patients with knee osteoarthritis by the addition of exogenous HA, or its derivatives, by intra-articular injection and is cited for the treatment of knee osteoarthritis in the guidelines of several professional societies.5 6 7 8 9 10
Hylan G-F 20 (Synvisc) is a high molecular weight (average 6000 kDa) HA product consisting of two cross-linked components. Approved in several countries for the treatment of pain associated with knee osteoarthritis, the recommended treatment regimen for the treatment of knee osteoarthritis pain is one 2 ml intra-articular injection per week for three consecutive weeks.11 12
In order to reduce the number of intra-articular injections (and potential related side effects) a pilot study was conducted, and the results suggested that at 6 months post-injection, one 6 ml injection performed at least as well as three 2 ml injections.13 A single 6 ml injection may represent an attractive alternative to the current treatment regimen, reducing the number of intra-articular injections required and thereby offering potential comfort and safety benefits to patients.
The current study was designed to assess the efficacy and safety of one 6 ml injection of hylan G-F 20 in a 26-week, pivotal, prospective, multicentre, double-blind, randomised, placebo controlled clinical trial.
Methods
Ethics
The study was performed in accordance with the principles of good clinical practice guidelines. Ethics committee approvals and informed patient consents were obtained. The study was registered in the ClinicalTrials.gov National Institutes of Health trial register under the identification number NCT00131352.
Study design
At the screening visit patients gave their written, informed consent and a physical examination was performed on the knee to be treated (“target knee”). A radiographic assessment was also performed if no valid x ray had been taken within 3 months before screening was available. Demographic data and medical history information were collected.
Before commencing the study, a washout period of prohibited pain and osteoarthritis medications (analgesics and non-steroidal anti-inflammatory drugs with half lives of ⩾5 h and systemic corticosteroids) was required.
Patients were randomly assigned to receive arthrocentesis plus a 6 ml intra-articular injection of either hylan G-F 20 or buffered physiological sodium chloride solution (PBS) (placebo) on day 0.
Patients completed the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index Likert and patient global assessment (PGA) questionnaires and a blinded evaluator completed the clinical observer global assessment (COGA).
Safety assessments (including physical examination findings), usage of concomitant medications and treatments and vital signs were recorded until study completion. It was left to the judgement of the clinical evaluator to decide whether each target knee adverse event (AE) was related to the study procedure (ie, expected with any intra-articular injection procedure) or to the study material.
Patients were followed up 1, 4, 8, 12, 18 and 26 weeks after injection.
To assess the safety of a repeat injection of 6 ml hylan G-F 20, patients from both groups were permitted to enter a 4-week open-label repeat treatment phase 26 weeks after their initial injection if they had no major safety concerns during the first course of treatment and an average WOMAC A score of at least 1.
Patient selection
Patients were required to meet the American College of Rheumatology criteria for osteoarthritis (knee pain for most days of the previous month and osteophyte(s) at the joint margin visible on x ray).14
Main inclusion criteria were: age 40 years or greater; diagnosis of primary osteoarthritis of the target knee; radiographic evidence of osteoarthritis in the medial and/or lateral tibiofemoral compartment (one or more osteophyte(s) and a measurable joint space on a standard radiograph taken within 3 months before screening); continued osteoarthritis pain in the target knee despite conservative treatments. Patients were required to have a score of 2 or 3 (0 to 4 scale) on question 1 of the WOMAC (Likert version 3.1) pain (A) subscale (pain while walking on a flat surface) as this is the most commonly reported symptom in clinical practice and the protocol was designed to weight this symptom more heavily. Included patients required a mean score of 1.5–3.5 on the WOMAC A (total pain) subscore.15
Main exclusion criteria were: secondary osteoarthritis in the target knee; grade IV radiographic stage osteoarthritis (Kellgren–Lawrence grading system);16 clinically apparent tense effusion of the target knee; significant valgus/varus deformities; viscosupplementation in any joint in the past 9 months; surgery in the knee within the past 6 months; symptomatic osteoarthritis of the contralateral knee or either hip unresponsive to paracetamol; systemic or intra-articular injection of corticosteroids in any joint within 3 months before screening.
Study treatments
Hylan G-F 20 (Synvisc-One, Genzyme Corporation, Ridgefield, New Jersey, USA), was supplied in 6 ml PBS. Placebo was 6 ml PBS. Both hylan G-F 20 and placebo were packaged identically in order to maintain the study blind.
The injection approach was left to the unblinded injector’s clinical discretion. Arthrocentesis was performed before injecting hylan or PBS.
Concomitant medications and treatments
Paracetamol (⩽4000 mg/day) was permitted as rescue medication for the target knee. Other permitted medications were analgesics/non-steroidal anti-inflammatory drugs with a half-life of 5 h or less for indications other than osteoarthritis pain (not to be taken for more than five consecutive days or >10 days/month) and aspirin (⩽325 mg/day). However, for 48 h before a study visit, patients were required to abstain from any paracetamol, pain or osteoarthritis medications.
Other permitted treatments may be reviewed in supplementary material 1 available online only.
Randomisation
Randomisation was performed by a centralised, interactive, voice-response system and was done by site in computer-generated blocks of four. Unblinded injectors were strictly forbidden from discussing treatment allocation with patients and clinical observers.
Power and sample size
The sample size estimation was based on the mean intergroup difference in the WOMAC A pain subscale change from baseline over 26 weeks. The following assumptions were made to compute the sample size: anticipated overall treatment difference of 0.297; common SD of 0.725; dropout rate of 25%; two-sided significance level of 5%. A resulting sample size of approximately 250 patients (125 patients per group) provided greater than 80% power to detect a difference between the hylan G-F 20 and placebo groups over 26 weeks.
Efficacy analyses
The primary efficacy analysis was performed on the intent-to-treat (ITT) population (all randomly assigned patients), based on a repeated-measures analysis of covariance that was used to test for intergroup differences in the WOMAC A (pain) subscore over 26 weeks. The analysis of covariance model included terms for treatment, site, time and time-by-treatment interaction, as well as the baseline WOMAC A score as a covariate.
Secondary efficacy outcomes were analysed using generalised estimating equations for a proportional odds logistic regression. The generalised estimating equations model was fitted to the observed data and included terms for baseline measure, site, visit, treatment group and a visit-by-treatment group interaction. These analyses included the difference between the groups from baseline at week 26 in WOMAC A and the differences from baseline over and at 26 weeks in WOMAC A1, WOMAC subscale C, PGA, COGA, and the responders to treatment per the Outcome Measures in Rheumatology, Osteoarthritis Research Society International (OMERACT–OARSI) responder criteria.17
For the WOMAC A1 responder analysis, patients were classified at each post-baseline visit into a responder category (yes/no). Those patients with at least a one-point category improvement from baseline who did not withdraw due to lack of efficacy were considered responders.
Safety analyses
The safety analyses were performed on the safety population (all patients who received at least one injection of hylan G-F 20 or placebo).
Results
Disposition of patients, baseline data
Patients were enrolled at 21 sites in the UK, France, the Czech Republic, Germany, Belgium and The Netherlands. A total of 329 patients enrolled; 76 patients (23.1%) were screening failures; 253 patients (73 men, 180 women) were randomly assigned and analysed: 124 to receive hylan G-F 20 and 129 to receive placebo. All 253 randomly assigned patients were included in the safety population (hylan G-F 20 123 patients; placebo 130 patients). One patient was randomly assigned to the hylan G-F 20 group but received placebo in error and was therefore counted in the placebo group for safety and the hylan G-F 20 group for ITT efficacy.
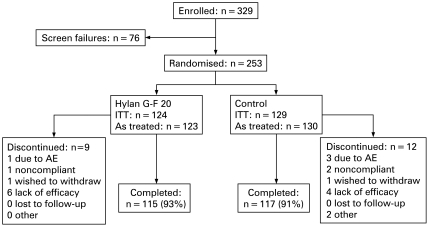
A total of 232 patients (91.7%) completed the study. Nine patients (7.3%) randomly assigned to hylan G-F 20 and 12 patients (9.2%) randomly assigned to placebo failed to complete the study schedule as planned (fig 1).
Figure 1.
Study flow chart. AE, adverse event; ITT, intent-to-treat.
There were no statistically significant, or clinically meaningful, differences between treatment groups in any baseline or demographic parameter (table 1).
Table 1.
Baseline characteristics for all randomly assigned patients (ITT population)
| Hylan G-F 20 (N = 124) | Placebo (N = 129) | |
| Mean age, years (SD) | 63.6 (9.64) | 62.5 (9.17) |
| Mean BMI, kg/m2 (SD) | 29.08 (4.81) | 29.77 (5.74) |
| Gender (M/F) | 32/92 | 41/88 |
| Tibiofemoral compartment with the most severe features of osteoarthritis, N* (%) | ||
| Medial | 93 (75.6) | 103 (79.2) |
| Lateral | 30 (24.4) | 27 (20.8) |
| Modified Kellgren–Lawrence grade in most severe tibiofemoral compartment, N* (%) | ||
| Grade II | 63 (51.2) | 51 (39.2) |
| Grade III | 60 (48.8) | 78 (60.0) |
| Grade IV | 0 | 1 (0.8) |
| Previous corticosteroids in the target knee, N* (%) | 40 (32) | 31 (24) |
| Previous arthroscopy in the target knee, N* (%) | 26 (21) | 28 (22) |
| Total WOMAC score (0–4), mean (SD) | 2.30 (0.44) | 2.28 (0.39) |
| WOMAC A score (0–4), mean (SD) | 2.30 (0.43) | 2.25 (0.41) |
| Symptomatic osteoarthritis that was responsive to paracetamol and did not require other therapy, N* (%) | ||
| In the contralateral knee | 68 (55.3) | 76 (58.5) |
| In either hip | 12 (9.8) | 18 (13.8) |
| Mean time since osteoarthritis diagnosis, months* (SD) (median, range) | 77.38 (76.44) (51.94, 3.1–350.9) | 70.01 (64.43) (47.34, 3.6–241.9) |
*Safety population. BMI, body mass index; ITT, intent-to-treat; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Treatment efficacy
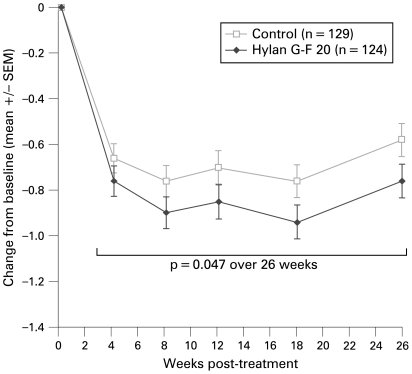
The treatment effect with hylan G-F 20 was statistically significantly superior to placebo for the primary endpoint, change in WOMAC A (pain) over 26 weeks (table 2 and fig 2).
Table 2.
Primary efficacy endpoint—WOMAC A (pain) change over 26 weeks (ITT population)
| Baseline mean (SE) | 26-Week mean (SE) | Estimated change (SE) | Estimated difference between groups (SE) | p Value | |
| Hylan G-F 20 (n = 124) | 2.30 (0.038) | 1.43 (0.060) | −0.84 (0.060) | −0.15 (0.076) | 0.047 |
| Placebo (n = 129) | 2.25 (0.036) | 1.59 (0.058) | −0.69 (0.058) |
ITT, intent-to-treat; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Figure 2.
Mean change from baseline in the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index A (pain), intent-to-treat population.
Hylan G-F 20 demonstrated an estimated change (absolute change, adjusted for values, time and treatment) from baseline over 26 weeks of −0.84, a mean percentage change in pain from baseline of 36%. Patients in the placebo group had an estimated change from baseline over 26 weeks of −0.69, a mean percentage change in pain from baseline of 29%. The estimated treatment difference between the two treatment groups over the 26-week study was statistically significant (p = 0.047).
Some, but not all, of the secondary endpoints, including WOMAC A1 (walking pain), PGA and COGA, showed statistically significant differences between the two groups favouring hylan G-F 20 treatment (tables 3 and 4).
Table 3.
Secondary efficacy endpoints (ITT population): estimated between-group differences
| Baseline mean (SE) | Week 26 mean/overall mean (SE) | Estimated change (SE) | Estimated between-group difference | p Value | |
| WOMAC A (pain) change from baseline at 26 weeks* | |||||
| Hylan G-F 20 | 2.30 (0.04) | 1.51 (0.074) | −0.76 (0.07) | −0.18 (0.097) | 0.064 |
| Placebo | 2.25 (0.04) | 1.69 (0.073) | −0.58 (0.07) | ||
| WOMAC C (function) change from baseline over 26 weeks† | |||||
| Hylan G-F 20 | 2.29 (0.04) | 1.62 (0.061) | −0.66 (0.061) | −0.03 (0.077) | 0.679 |
| Placebo | 2.28 (0.04) | 1.66 (0.059) | −0.63 (0.059) | ||
| WOMAC C (function) change from baseline at 26 weeks† | |||||
| Hylan G-F 20 | 2.29 (0.04) | 1.69 (0.076) | −0.59 (0.076) | −0.11 (0.100) | 0.266 |
| Placebo | 2.28 (0.04) | 1.80 (0.074) | −0.48 (0.074) |
*Week 26 mean in column 3; †overall mean in column 3. ITT, intent-to-treat; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Table 4.
Secondary efficacy endpoints (ITT population): estimates of odds ratios
| Week 26 subscore | Estimate of OR (placebo/hylan G-F 20) (95% CI) | |||
| Hylan G-F 20 n (%) | Placebo n (%) | At week 26 | Over 26 weeks | |
| WOMAC A1 (walking pain) subscore | ||||
| None | 17 (13.7) | 13 (10.1) | 0.56 (0.35 to 0.92) p = 0.022 | 0.64 (0.45 to 0.91) p = 0.013 |
| Mild | 45 (36.3) | 39 (30.2) | ||
| Moderate | 41 (33.1) | 42 (32.6) | ||
| Severe | 11 (8.9) | 19 (14.7) | ||
| Extreme | 1 (0.8) | 4 (3.1) | ||
| Patient global assessment | ||||
| Very well | 9 (7.3) | 2 (1.6) | 0.51 (0.31 to 0.82) p = 0.005 | 0.69 (0.50 to 0.96) p = 0.029 |
| Well | 33 (26.6) | 27 (20.9) | ||
| Fair | 50 (40.3) | 54 (41.9) | ||
| Poor | 21 (16.9) | 31 (24.0) | ||
| Very poor | 2 (1.6) | 3 (2.3) | ||
| Clinician observer global assessment | ||||
| Very well | 13 (10.5) | 8 (6.2) | 0.56 (0.34 to 0.93) p = 0.025 | 0.71 (0.50 to 0.99) p = 0.041 |
| Well | 37 (29.8) | 31 (24.0) | ||
| Fair | 38 (30.6) | 38 (29.5) | ||
| Poor | 22 (17.7) | 34 (26.4) | ||
| Very poor | 5 (4.0) | 6 (4.7) | ||
| OMERACT–OARSI responders | ||||
| Responder | 73 (58.9) | 66 (51.2) | 0.69 (0.41 to 1.16) p = 0.156 | 0.66 (0.44 to 1.02) p = 0.059 |
| Non-responder | 50 (40.3) | 63 (48.8) | ||
| Based on OMERACT–OARSI responder criteria | 43 (34.7) | 52 (40.3) | ||
| Due to withdrawal before study completion | 7 (5.6) | 11 (8.5) | ||
ITT, intent-to-treat; OMERACT–OARSI, Outcome Measures in Rheumatology, Osteoarthritis Research Society International; OR, odds ratio; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Seventy-one per cent (88/124) of the patients were WOMAC A1 (walking pain) responders at week 18 in the hylan G-F 20 group compared with 53% (69/129) in the placebo group (p = 0.003). At week 26, 64% (79/124) of patients in the hylan G-F 20 group were WOMAC A1 responders compared with 50% (64/129) in the placebo group (p = 0.028).
The change in WOMAC C (function) scores did not reach statistical significance. Further exploratory analyses of predefined covariates were carried out to understand better the lack of effect of hylan G-F 20 on the WOMAC C endpoint. In patients without any other lower limb osteoarthritis (defined as hip or contralateral knee involvement), those treated with Synvisc experienced a greater change in WOMAC C than those treated with placebo (−0.71 and −0.55, respectively).
The OMERACT–-OARSI responder analysis over 26 weeks approached statistical significance (p = 0.059). At week 26, 73 patients (59%) in the hylan G-F 20 group and 66 patients (51%) in the placebo group were responders.
Overall, patients consumed a mean daily dose of 0.26 g (SD 0.654 g) of paracetamol in the hylan G-F 20 group, and 0.28 g (SD 0.570 g) in the placebo group. Throughout the study there was no statistically significant difference in paracetamol consumption between the two groups (p = 0.370).
AE and safety
There were no target knee serious AE and no serious AE that were related to the study treatment or the study procedure. The overall frequency of AE was comparable between the two treatment groups (hylan G-F 20, n = 70, 56.9%; placebo, n = 79, 60.8%).
The most commonly reported AE were pain in the target knee (coded as “arthralgia”), joint stiffness, joint effusion and joint swelling. The incidence of AE was slightly higher in the hylan G-F 20 group (n = 7, 5.7%) than in the placebo group (n = 4, 3.1%) but this was not statistically significant (p = 0.366) (table 5). In addition, there were no statistically significant differences between the groups in treatment-related (p = 0.203) or procedure-related (p = 0.531) target knee AE, all of which were of mild or moderate severity.
Table 5.
Target knee adverse events: safety population
| Hylan G-F 20 | Placebo | |
| N = 123 | N = 130 | |
| Preferred term | n (% of patients) | n (% of patients) |
| Any treatment-emergent target knee AE | 44 (35.8) | 44 (33.8) |
| Any treatment and/or procedure-related target knee AE | 7 (5.7) | 4 (3.1) |
| Arthralgia | 2 (1.6) | 3 (2.3) |
| Joint effusion | 2 (1.6) | 0 (0) |
| Arthritis | 1* (0.8) | 0 (0) |
| Arthropathy | 1 (0.8) | 0 (0) |
| Injection site pain | 1 (0.8) | 1 (0.8) |
| Any treatment-related target knee AE | 4 (3.3) | 1 (0.8) |
| Any procedure-related target knee AE | 6 (4.9) | 4 (3.1) |
Related to treatment refers to unknown relationship to, or possibly, probably, or definitely related to treatment. Patients are counted once for each unique adverse event (AE) and may have had more than one unique AE. If a patient had more than one occurrence of the same AE, the strongest relationship to study treatment or injection procedure was included. Treatment groups reflect the actual treatment received, not the randomised treatment. Patients may be counted in more than one category. *Patient withdrew from the study due to target knee arthritis of moderate severity.
Repeat treatment phase
A total of 160 patients was treated in the open, repeat treatment phase, of which 77 received a second injection of hylan G-F 20 and 83 received a first injection of hylan G-F 20, having received placebo during the initial treatment phase. There were no target knee serious AE. In the group receiving a second injection of hylan G-F 20 one patient (1.3%) experienced target knee AE related to the study treatment and four patients (5.2%) experienced target knee AE related to the study procedure.
Patients who developed target knee AE during the initial phase of the study, and who subsequently received repeat treatment, did not experience target knee AE on repeat exposure to hylan G-F 20. All treatment-related and procedure-related target knee AE were of mild or moderate severity.
Discussion
This study demonstrates that a single intra-articular injection of hylan G-F 20 is safe and effective in providing statistically significant, clinically relevant pain relief, as measured by WOMAC A1 (walking pain) over 26 weeks, with a modest difference compared with placebo. Several secondary efficacy results also show the superiority of hylan G-F 20 over placebo. Pain while walking is particularly medically relevant for the assessment of symptomatic relief and has been selected as the primary efficacy measure in other studies of hylan G-F 20 or other hyaluronans.18 19 20 The OMERACT–OARSI responder analysis also favoured hylan G-F 20 although statistical significance was not reached (p = 0.059).
This trial had a large placebo effect (−0.69 change in mean WOMAC A score over 26 weeks), which may explain why the observed overall treatment difference (0.15) was weaker than anticipated (0.297). The placebo effect in osteoarthritis treatment has been re-evaluated in a recent meta-analysis showing that it induces significant pain relief, especially in trials involving intra-articular injections.21 Furthermore, because the actual therapeutic effect of arthrocentesis (with synovial fluid aspiration if needed) has never been assessed, it is possible that this contributed to the robust response in patients receiving placebo. However, hylan G-F 20 was still significantly superior to placebo in the primary and several of the secondary endpoints.
Effect size is a way to measure effectiveness and to compare clinical interventions.22 The effect size of hylan G-F 20 versus control in this study was −0.23 for WOMAC A at week 26. In chronic pain conditions such as osteoarthritis, this modest effect size should be interpreted as clinically relevant on an individual patient basis as recommended by the IMMPACT consensus.23 24
In addition, the accepted threshold for a minimum clinically important improvement in osteoarthritis (12–18% improvement in WOMAC A from baseline)25 was exceeded in this study. Patients treated with one 6 ml injection of hylan G-F 20 experienced a 31.3% improvement in WOMAC A from baseline (p<0.001) at week 26.
The WOMAC C (function) subscale findings in the current study are inconsistent with those from previous controlled studies of hylan G-F 20.18 26 However, our post-hoc analysis showed that WOMAC C scores were improved in a subgroup of patients without any other lower limb joint involvement, suggesting that osteoarthritis occurring in other lower limbs may contribute to substantial functional impairment, and may confound the patient’s ability to detect improvement in the target knee in a clinical trial setting.
Evaluation of the safety profile for the higher injected volume (6 ml) of hylan G-F 20 was also a major objective of this study. The similarity in the safety profiles of hylan G-F 20 and placebo (PBS) is reassuring. No new, unrecognised AE were identified during this study. The safety profile of hylan G-F 20 was confirmed during the repeat treatment phase of the study, indicating no increase in the risk of AE in the patients receiving a second injection of hylan G-F 20. This finding contrasts with previous reports of post-marketing studies, which suggest an approximate threefold increased risk of local target knee AE with a repeat course of hylan G-F 20.19 The excellent safety profile of the increased 6 ml dose translates to an improved benefit-to-risk ratio for the patient.
Conclusions
This placebo-controlled study demonstrated that, in patients with knee osteoarthritis, a single 6 ml intra-articular injection of hylan G-F 20 is safe and effective in providing statistically significant, clinically relevant pain relief over 26 weeks, with a modest difference compared with placebo.
In daily practice the favourable benefit/risk profile of a single injection of 6 ml hylan G-F 20 has the major advantage of decreasing the number of injections from three to five to only one.
Acknowledgments
The authors would like to thank all the investigators and study nurses (listed in supplementary material 2 available online only) for helping to recruit the patients and collect and verify the data. From Genzyme, the authors also thank Joël Guidoux for project coordination and Clare Elkins for the statistical analysis, and they are also grateful to Christopher Murray of Genzyme and Anna Porter for their help in the development and preparation of the manuscript.
Footnotes
Funding: This manuscript is based upon clinical trial results from a study sponsored by Genzyme Biosurgery.
Competing interests: Declared. XC, JJ and PG have been reimbursed by Genzyme Biosurgery, the manufacturer of hylan G-F 20, for attending symposia and have also received speaker fees. JJ has received research funds from Genzyme Biosurgery. FB is an employee of Genzyme Biosurgery working in the Clinical Research and Medical Affairs Departments. NvD, FPL, DLS and KP have no conflicts of interest. All authors actively participated in the conduct of this trial and in its analysis and interpretation.
Ethics approval: Ethics committee approvals were obtained.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
REFERENCES
- 1.Buckwalter JA, Saltzman C, Brown T. The impact of osteoarthritis: implications for research. Clin Orthop Relat Res 2004;427(Suppl):S6–15 [DOI] [PubMed] [Google Scholar]
- 2.Schurz J, Ribitsch V. Rheology of synovial fluid. Biorheology 1987;24:385–99 [DOI] [PubMed] [Google Scholar]
- 3.Mazzucco D, McKinley G, Scott RD, et al. Rheology of joint fluid in total knee arthroplasty patients. J Orthop Res 2002;20:1157–63 [DOI] [PubMed] [Google Scholar]
- 4.Fam H, Bryant JT, Kontopoulou M. Rheological properties of synovial fluids. Biorheology 2007;44:59–74 [PubMed] [Google Scholar]
- 5.Bellamy N, Campbell J, Robinson V, et al. Viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst Rev 2006;19(2):CD005321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Divine JG, Zazulak BT, Hewett TE. Viscosupplementation for knee osteoarthritis: a systematic review. Clin Orthop Relat Res 2007;455:113–22 [DOI] [PubMed] [Google Scholar]
- 7.Jordan KM, Arden NK, Doherty M, et al. EULAR recommendations 2003: an evidence based approach to the management of knee osteoarthritis: report of a task force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 2003;62:1145–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum 2000;43:1905–15 [DOI] [PubMed] [Google Scholar]
- 9.Simon L, Lipman AG, Jacox AK, et al. Guidelines for the management of pain in osteoarthritis, rheumatoid arthritis, and juvenile chronic arthritis. In: APS Clinical Practice Guidelines Series, 2nd edn. Glenview, IL: American Pain Society, 2002 [Google Scholar]
- 10.Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008;16:137–62 [DOI] [PubMed] [Google Scholar]
- 11.Synvisc (hylan G-F 20) package insert Ridgefield, NJ: Genzyme Corporation, 2006 [Google Scholar]
- 12.Synvisc (hylan G-F 20) package insert Naarden, The Netherlands: Genzyme Europe, BV, 2007 [Google Scholar]
- 13.Conrozier T, Jerosch J, Beks P, et al. Prospective, multi-centre, randomised evaluation of the safety and efficacy of five dosing regimens of viscosupplementation with hylan G-F 20 in patients with symptomatic tibio-femoral osteoarthritis: a pilot study. Arch Orthop Trauma Surg 2009;129:417–23 [DOI] [PubMed] [Google Scholar]
- 14.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Arthritis Rheum 1986;29:1039–49 [DOI] [PubMed] [Google Scholar]
- 15.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to anti-rheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833–40 [PubMed] [Google Scholar]
- 16.Kellgren JH, Lawrence JS. Radiographic assessment of osteoarthritis. Ann Rheum Dis 1957;16:494–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pham T, van der Heijde D, Altman RD, et al. OMERACT–OARSI initiative: Osteoarthritis Research Society International set of responder criteria for osteoarthritis clinical trials revisited. Osteoarthritis Cartilage 2004;12:389–99 [DOI] [PubMed] [Google Scholar]
- 18.Caborn D, Rush J, Lanzer W, et al. A randomized, single-blind comparison of the efficacy and tolerability of hylan G-F 20 and triamcinolone hexacetonide in patients with osteoarthritis of the knee. J Rheumatol 2004;31:333–43 [PubMed] [Google Scholar]
- 19.Waddell DD, Cefalu CA, Bricker DC. An open-label study of a second course of hylan G-F 20 for the treatment of pain associated with knee osteoarthritis. Curr Med Res Opin 2003;19:499–507 [DOI] [PubMed] [Google Scholar]
- 20.Altman R, Moskowitz R, the Hyalgan study group Intraarticular sodium hyaluronate (Hyalgan) in the treatment of patients with osteoarthritis of the knee: a randomized clinical trial. J Rheumatol 1998;25:2203–12 [PubMed] [Google Scholar]
- 21.Zhang W, Robertson J, Jones AC, et al. The placebo effect and its determinants in osteoarthritis: meta-analysis of randomised controlled trials. Ann Rheum Dis 2008;67:1716–23 [DOI] [PubMed] [Google Scholar]
- 22.Jüni P, Reichenbach S, Dieppe P. Osteoarthritis: rational approach to treating the individual. Best Pract Res Clin Rheumatol 2006;20:721–40 [DOI] [PubMed] [Google Scholar]
- 23.Bjordal JM, Klovning A, Ljunggren AE, et al. Short-term efficacy of pharmacotherapeutic interventions in osteoarthritic knee pain: a meta-analysis of randomized placebo-controlled trials. Eur J Pain 2007;11:125–38 [DOI] [PubMed] [Google Scholar]
- 24.Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain 2008;9:105–21 [DOI] [PubMed] [Google Scholar]
- 25.Angst F, Aeschlimann A, Michel BA, et al. Minimal clinically important rehabilitation effects in patients with osteoarthritis of the lower extremities. J Rheumatol 2002;29:131–8 [PubMed] [Google Scholar]
- 26.Raynauld JP, Torrance GW, Band PA, et al. A prospective, randomized, pragmatic, health outcomes trial evaluating the incorporation of hylan G-F 20 into the treatment paradigm for patients with knee osteoarthritis (part 1 of 2): clinical results. Osteoarthritis Cartilage 2002;10:506–17 [DOI] [PubMed] [Google Scholar]