Abstract
The objective of this study is to evaluate the sources of variability when using the metatarsal-phalangeal (MTP) semi-flexed radiographic technique to measure the tibiofemoral joint space width in the medial and lateral compartments of the knee using digital radiography.
Three independent digital MTP radiographs (X-RAYS) were taken of each knee of nine healthy volunteers. The joint space widths of both compartments of each knee were measured three times by two independent examiners using a computer program.
Intraclass correlation coefficients were high between repeated X-RAYS, between examiners, and within examiners (0.92–0.98). These three error components accounted for 9% and 14% of the total variance for the medial and lateral compartments respectively. The estimated standard deviations across radiographs for the medial and lateral compartments were 0.09mm and 0.16mm.
The digital radiographic technique based on the MTP view is a simple and reliable technique for measuring the joint space width that can be readily used to track longitudinal changes in cartilage thickness following knee joint surgery.
Introduction
Techniques that identify early osteoarthritis (OA) in the knee are necessary to identify risk factors for OA, and to determine if interventions are capable of slowing disease progression. The current standard for documenting OA progression in clinical trials are temporal measurements of tibiofemoral joint space width (JSW) from semi-flexed weight bearing x-rays1-4. Because articular cartilage is radiolucent, articular cartilage loss can theoretically be detected if the distance between the opposing bony surfaces decreases with time. Joint space narrowing (JSN) has been reported to occur at a rate of 0.1 to 0.2mm per year in patients with OA 9, 16. Semi-flexed x-rays have been shown to be the most sensitive radiographic means to detect disease progression and would be particularly useful to study the ACL injured knee13.
The weight-bearing metatarsal-phalangeal (MTP) semi-flexed view has been shown to provide reproducible patient positioning when used with fluoroscopy to ensure proper alignment of the medial tibial plateau with respect to the x-ray beam. However, fluoroscopy is time consuming and expensive. The MTP view using anatomical landmarks and a foot position map to reproducibly position the patient without fluoroscopy is more efficient and has been shown to be accurate for measuring the JSW of the medial compartment with traditional x-ray4, 6.
The objectives of this study were: 1) to evaluate the potential sources of variation (e.g. repeated x-ray examinations of the same patient, inter-examiner and intra-examiner variability of the same x-rays, and right-left knee variations), 2) to estimate the associated reliability of the technique to measure JSW in the medial and lateral compartments of the tibiofemoral joint, and 3) to evaluate the relationship between inter-rim distance of the medial compartment (the distance between the projection of the anterior and posterior edges of the tibial plateau on the radiograph, an indicator of joint position error) and the JSW measurements in the medial and lateral compartments when using digital x-ray in conjunction with a semi-automated computerized digitization algorithm in knees without disease.
Materials & Methods
Subjects
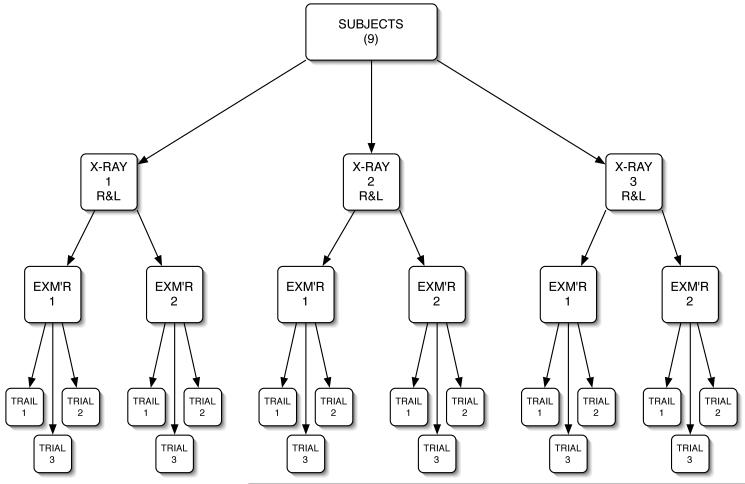
Nine healthy volunteers (5 males, 4 females; median age=26.5, range=22–44 years) were recruited from the Rhode Island Hospital campus. Subjects were excluded if they were pregnant, or had a history of arthritis, knee injury or knee surgery. The study was approved by the Institutional Review Board at Rhode Island Hospital, and informed consent was granted by all subjects prior to their participation. Both knees (right & left) of all nine subjects underwent three independent x-ray sessions (X-RAYS), which were independently analyzed three times (TRIALS) by two examiners (EXM’R) (Fig. 1).
Figure 1.
Outline of the experimental protocol. Three x-ray sessions (X-RAYS) were performed of both knees (R&L) for each subject. Once all of the imaging was completed, the X_RAYS were placed in a random order. Two independent examiners (EXM’RS) performed the JSW measurements of each film three times (TRIAL).
X-ray
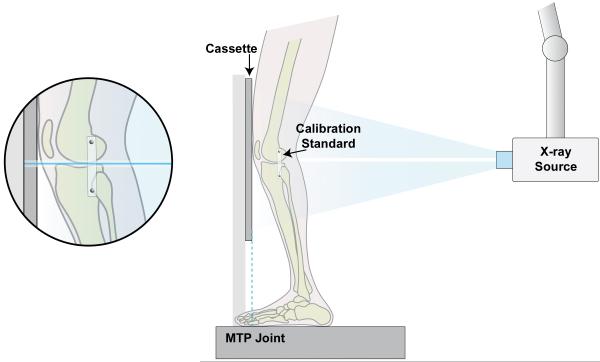
Three independent X-RAY examinations were performed of each knee of each subject using the weight-bearing semi-flexed MTP view (Fig. 2) 4. Subjects were asked to remove their shoes and were placed on an x-ray jacket on a custom platform facing the digital x-ray cassette with their feet 25 cm apart and their weight evenly distributed between them. The first MTP joint of each foot was aligned immediately below the front edge of the cassette. The subjects’ feet were then rotated externally by 15° while maintaining the correct orientation of the MTP joint relative to the cassette. With the subjects in the proper position for the first set of radiographs, outlines of the feet were drawn on the x-ray jacket to produce a map which was used to reposition the subject for subsequent X_RAYS. The subjects were instructed to flex their knees forward until their patellae contacted the cassettes which has been previously shown to place the knee between 9° and 18° of flexion (Fig. 2) 6. A calibration standard was taped to the knee at the level of the tibiofemoral joint space in a position superior and adjacent to the fibular head. The x-ray beam was directed orthogonally to the cassette in both vertical and horizontal planes. In the vertical plane, the beam was positioned over the center of the tibiofemoral joint space. In the horizontal plane, the beam was directed to the midpoint of the medial tibiofemoral compartment. It should be noted that the x-ray source was aligned relative to each knee independently. A MicroX-50HF (Fischer Imaging Corporation, Denver Colorado) source (60kVp/5mAs with a focus-to-focus distance of 102cm from the digital x-ray cassette) was used to take the X_RAYS for each knee (14 pixels/mm).
Figure 2.
Schematic of the platform used to position of the knee relative to the x-ray source and the cassette for the MTP view.
The subjects were then asked to leave the x-ray room and walk around for 5 minutes between each set of X-RAYS), while the x-ray source and subject platform were removed and repositioned between X-RAYS. All subjects were set up for each X-RAY by one person trained in this technique, though the X-RAYS were taken by any one of three technologists.
Joint Space Width
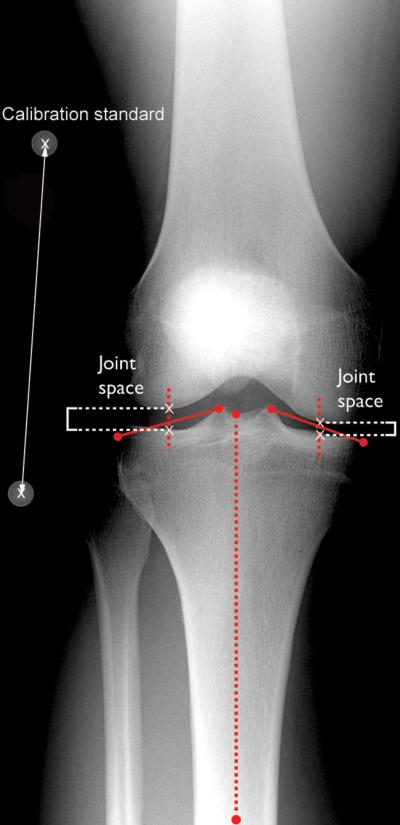
All six digital X-RAYS (3 on the right and left knees) were transferred to a PC computer. Trained examiners (EXM’R 1 & 2) utilized a custom designed software program (MATLAB; Natick MA) to independently measure the JSW of the medial and lateral compartments on each radiograph. The program utilized the “midpoint” technique, which was originally described and validated by Ravaud et al (Figure 3) 14.
Figure 3.
The midpoint technique described by Ravaud et al was adapted to this program to calculate the joint space width.
Each digital image was opened in the MATLAB program and the medial and lateral edges of each compartment of the tibial plateau were identified and digitized by the examiner using a mouse. Contrast and brightness were adjusted if necessary. The midpoints of the distal tibial shaft and the proximal intercondylar midpoint were identified and digitized. Lines were automatically drawn between two digitized points that represented the left and right edges of the medial and lateral compartments, respectively. A line was also automatically drawn between the proximal and distal tibial midpoints, establishing the long axis of the tibial shaft. Midpoint lines that bisected each of the respective tibial compartment lines were then drawn parallel to the long axis of the tibia.
The intersections of the femoral condyles and tibial compartments with the midpoint lines were then digitized for each compartment. If the superior and inferior edges of the tibial plateau were not perfectly aligned (i.e. the inter-rim distance not equal to zero), the anterior and posterior edges of the tibial plateau were digitized by the EXM’R to enable the computer to calculate the center of the inter-rim distance, which was then used as the tibial intersection for the midpoint line.
The distance between the femoral and tibial intersections with the bisecting midpoint line for each compartment were then calculated to determine the JSW of each compartment. The inter-rim distance along each bisecting midpoint line of the medial compartment was also computed. The computer algorithm automatically determined the location of the centers of the two spheres (Fig. 1 & 3), which were embedded a known distance apart within the calibration standard using an edge detection algorithm. The distance between the two centers was calculated to determine the magnification factor, which was used to account for parallax errors.
Statistical Methods
The three digital radiographs (X-RAY 1, 2, & 3) of each knee (right, left) were independently processed three times (TRIAL 1, 2, & 3) by two trained EXM’RS (Fig. 1). All radiographs were processed in a random order. A general linear model was used to estimate the variance components for the estimates of JSW in each compartment (medial, lateral) associated with each factor: across subjects, variation between knees (within-subject), between repeated X-RAYS (within knee), and between and within EXM’RS (within radiograph). Variance components were estimated using restricted maximum likelihood method (SAS, PROC VARCOMP). Pooled standard deviations were calculated by taking the square root of each of the estimated variance components. The intraclass correlation coefficients (ICCs) associated with each factor were calculated for each compartment to establish the reliability of the technique. The percentages of the total variability for each factor were also calculated for both the medial and lateral compartments. Lastly, the inter-rim distances were evaluated for each X-RAY to establish the reproducibly of patient positioning relative to the x-ray beam when using this protocol, and a variance component analysis was also performed to evaluate the effects of each factor (across subjects, within subjects, within knee, and within X-RAY) on the inter-rim distance of the medial compartment. The correlation coefficients between the medial inter-rim distance and the JSW in the medial and lateral compartments were also evaluated. All statistical analyses were performed using SAS version 8.2 (SAS Institute, Cary, NC).
Results
Joint Space Width
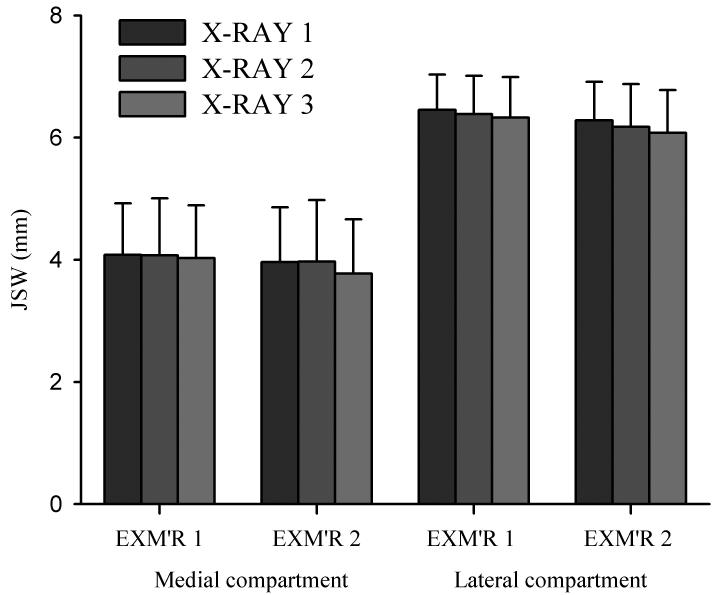
For the medial compartment, the mean deviations for the JSWs were 4.0 (SD 0.9) and 3.8 (SD 0.9) mm for the two EXM’RS. Mean JSWs for the three X-RAY sessions were 3.9 (SD 0.8), 3.9 (SD 0.9), and 3.8 (SD 0.9) mm (Fig. 4). For the lateral compartment, the mean values for the JSW were 6.3 (SD 0.6) and 6.1 (SD 0.7) mm for the two EXM’RS. Mean JSW for the three X-RAY sessions were 6.3 (SD 0.6), 6.2 (SD 0.7), and 6.2 (SD 0.7) mm (Fig. 4).
Figure 4.
The means and standard deviations for each X-RAY of each EXM’R for both the medial and lateral compartments.
Variance Analysis - Medial Compartment
Most of the error variance for the medial compartment was due to EXM’R, which accounted for a total of 6.4% of the total variability in JSW (Table 1). More than half of this variance component, (3.9% of total variability) was due to the inability of EXM’RS to read radiographs in a parallel fashion (EXM’R X-RAY interaction) while 2.5% was attributed to systematic differences across EXM’R S (i.e. examiner bias). Repeated X-RAYS accounted for only 1.0% of the total variability, while multiple TRIALS within EXM’RS added an additional 1.4%. These three factors contributed less than 10% of the total variability in the measurement of JSW. Variability across knee within subject were considerable more homogeneous than were subjects, accounting for only 6.3% of the total variability, leaving the vast majority being inter-subject variability (85%). Intraclass correlation coefficients were high for EXM’RS (r=0.930), X-RAYS (r=0.989) and TRIALS (r=0.984) indicating these measurements had excellent reliability in the medial compartment.
Table 1.
The estimated variance components associated with each experimental factor for the measurements of JSW in the medial compartment. ICC = Intraclass Correlation Coefficient
| Medial Compartment JSW | |||||
|---|---|---|---|---|---|
| Variable | Estimated Variance |
% of Total Variance |
Estimated Standard Deviation |
Coefficient of Variation |
ICC |
| Subject | 0.741 | 85.0 | 0.861 | 22.177 | N/A |
| Knee | 0.055 | 6.3 | 0.234 | 6.035 | 0.931 |
| X-RAY | 0.009 | 1.0 | 0.093 | 2.389 | 0.989 |
| EXM’R | 0.056 | 6.4 | 0.236 | 6.093 | 0.930 |
| TRIAL | 0.012 | 1.4 | 0.109 | 2.801 | 0.984 |
Variance Analysis - Lateral Compartment
Results were similar for the lateral compartment (Table 2). EXM’R accounted for a total of 7.0% of the total variability of measurements in JSW. Slightly less than half of this variance component, (3.3% of total) was due to the inability of EXM’RS to read radiographs in a parallel fashion, while 3.7% of the total was attributable to systematic differences across EXM’RS. Repeated X-RAYS accounted for 4.6% of the total variability, and multiple TRIALS within EXM’RS added less than 2%. These factors represented approximately 14% of the total variability in measurement of JSW. Variability across knee within subject accounted for 7.6% of the total variability, leaving 79% to subject-to-subject variability. Intraclass correlation coefficients were high for EXM’RS (r=0.919), X-RAYS (r=0.945) and TRIALS (r=0.979) indicating these measurements had excellent reliability.
Table 2.
The estimated variance components associated with each experimental factor for the measurements of JSW in the lateral compartment. ICC = Intraclass Correlation Coefficient
| Lateral Compartment JSW | |||||
|---|---|---|---|---|---|
| Variable | Estimated Variance |
% of Total Variance |
Estimated Standard Deviation |
Coefficient of Variation |
ICC |
| Subject | 0.412 | 79.1 | 0.642 | 10.290 | N/A |
| Knee | 0.040 | 7.6 | 0.199 | 3.192 | 0.912 |
| X-RAY | 0.024 | 4.6 | 0.155 | 2.489 | 0.945 |
| EXM’R | 0.036 | 7.0 | 0.191 | 3.057 | 0.919 |
| TRIAL | 0.009 | 1.7 | 0.094 | 1.510 | 0.979 |
Inter-rim Distances
Medial inter-rim distance ranged from 0.0 to 4.8 mm (median=2.6 mm) and 1.0 to 5.0 mm (median=2.3 mm) for the two EXM’RS. Lateral inter-rim distance ranged from 0 to 2.9 mm (median=0 mm) and 0 to 2.4 mm (median=0 mm) for the two EXM’RS.
The subject to subject inter-rim variability was 84.4% of the total variability. EXM’R accounted for a total of 6.1% of the total variability, and multiple TRIALS within an EXM’R accounted for 1.6%. Repeated X-RAYS accounted for 3.4% of the total variability. Thus, EXM’R, repeated X-RAYS, and repeat TRIALS within an EXM’R when combined accounted for 11.1% of the variability in the inter-rim distance. Variability across knee within subject accounted for 4.6% of the total variability. Significant correlations were found between the inter-rim distances and the JSWs in the medial compartment (r=−0.60; p<0.01) and lateral compartments (r=0.27; p<0.01).
Discussion
This study was performed to determine the reliability of a digital radiographic method to measure knee JSW in normal knees without the need for fluoroscopic positioning. We chose knees without pathology because we are interested in early onset of knee osteoarthritis that results in joint space narrowing without other considerable changes. This technique is advantageous for measuring JSN in the tibiofemoral joint because it is relatively inexpensive and requires minimal time and resources compared to fluoroscopy-based techniques. The high ICCs between knees, repeated X-RAYS, EXM’RS and TRIALS within EXM’RS in the medial and lateral joint space and the variation component analyses for healthy volunteers indicate that the variability inherent to each of these factors is extremely small relative to the variability in JSW between subjects. These results demonstrate that these factors will have a negligible effect on estimates of JSW within a subject.
The estimated standard deviation of 0.09 and 0.16 mm (Tables 1&2) between repeated X-RAYS for the medial and lateral compartments, respectively, are comparable to those of previously published data using the MTP positioning technique with and without the use of fluoroscopy 2, 4, 6, 10, 12, 15. Dupuis et al. reported JSW reproducibility between x-rays without fluoroscopy of 0.11 mm (mean SD between repeated x-rays) using the midpoint technique while Buckland-Wright reported 0.08 mm (mean SD) at the perceived narrowest point 4, 6. JSW measurement at the narrowest point measured from the MTP view with the use of fluoroscopy have reported median standard deviations of 0.11 mm for the medial compartment in “normal” knees, 0.19 mm for the medial compartment of OA knees, 0.58 mm for the lateral compartment of “normal” knees, and 0.21 mm for the lateral compartment of OA knees 3. Three techniques have been employed to select the position within the condyle to measure the JSW: 1) at the location of the examiner perceived minimum, 2) at the location of the calculated minimum following digitization, and 3) at the midpoint of the compartment as defined in the present study 6. The calculated minimum was shown to be less accurate and more variable than the other two methods. Although the variability of the midpoint and examiner perceived minimum techniques are similar, the “midpoint” location was selected since this location would be less likely to change with the progression of disease 6.
In this study, the inter-rim distances ranged from 0.1–5.0 mm with a mean of 2.3 to 2.5 mm depending on the examiner. These ranges are similar to those reported by others, despite differences in measurement techniques and knee health status 4-6, 12. However, there has been debate whether the increased inter-rim distances affect the precision of measuring JSW. Our correlation data suggests study suggests that the inter-rim distance is related to the magnitude of the JSW. However, repeated X-RAYS within a subject did not introduce significant variability to the inter-rim distance (Table 3). Thus, a subject’s knee can be reproducibly positioned with respect to the x-ray source without changing the inter-rim distance and hence the relative changes in JSW within a subject.
Table 3.
The estimated variance components associated with each experimental factor for the inter-rim distances of the medial compartment. ICC = Intraclass Correlation Coefficient
| Medial Inter-rim Distances | |||||
|---|---|---|---|---|---|
| Variable | Estimated Variance |
% of Total Variance |
Estimated Standard Deviation |
Coefficient of Variation |
ICC |
| Subject | 1.346 | 84.3 | 1.160 | 43.698 | N/A |
| Knee | 0.073 | 4.6 | 0.270 | 10.163 | 0.949 |
| X-RAY | 0.054 | 3.4 | 0.233 | 8.761 | 0.961 |
| EXM’R | 0.098 | 6.1 | 0.313 | 11.786 | 0.932 |
| TRIAL | 0.026 | 1.6 | 0.160 | 6.022 | 0.981 |
When performing repeated x-rays on the same day, Mazzuca et al reported that the reproducibility of the semiflexed MTP view approaches that of the fluoroscopically assisted views 12. However, they also found that the inter-rim distances were accurately reproduced in patients with OA at baseline in 88% ofx-rays, but only in 54% of the x-rays at 14-month follow up 11. The mean JSW increased in the MTP x-rays after 14 months, although this was not significantly different from zero. The same knees also showed a narrowing of JSW in fluoroscopically assisted semiflexed AP examinations, but again this was not significantly different from zero.
Le Graverand et al. evaluated the effects of knee position on JSW in 80 subjects randomly selected from three studies of the x-ray progression of knee OA 8. They reported that 73% of MTP PA x-rays reproduced alignment at 12 month follow-up and 80% of semiflexed AP x-rays using fluoroscopy reproduced alignment after 16 months (±1.4 mm) 8. In x-rays that reproduced alignment at the midpoint of the medial tibia, (<0.5 mm) JSN was 0.19 (SD 0.274) mm. In x-rays with alignment between 0.5 and 1.4 mm, JSN was 0.16 (SD 0.308) mm, and when alignment was greater than or equal to 1.5 mm, JSN was 0.130 (SD 0.321) mm. Based on this data they stated that parallel alignment improves the measurement accuracy of JSN. However, there are limitations to their study in that comparisons were made ad-hoc between three different studies, which differed in: age groups, x-ray protocols, follow-up time points and levels of OA. The majority of subjects with skewed alignment came from a study where many of the subjects did not have OA and the majority of subjects with perfect alignment came from a study where 100% of subjects had OA at baseline. This could explain why the group with better tibial alignment showed a faster rate of JSN.
It should be noted that in our study the lateral compartment mean JSW [6.2 (SD 0.66) mm] was greater than the medial compartment mean JSW [3.9 (SD 0.88) mm], and that these values correspond with those measured with weight-bearing MRI 7. It has been reported that the medial compartment is more effective in documenting the progression of OA in patients with disease and that the lateral compartment is less sensitive to change 15. The lower sensitivity of JSN of the lateral compartment with disease progression is most likely due to the lower proportion of the compressive force supported by the lateral compartment as compared to the medial compartment. The data presented here suggests that the lateral compartment is more variable.
Limitations of this study were that the X-RAYS were performed only on healthy volunteers with no knee pathology. The reliability of the technique may change when used with OA knees due to changes in joint positioning and the presence of osteophytes. Another limitation was that the X-RAYS did not include the entire length of the tibia. This limitation may have resulted in decreased accuracy of determining the tibial shaft and thus determining the midpoint of each compartment relative to the tibial shaft. Finally, repeat X-RAYS were performed on the same day, so we only assumed that the technique would be as reliable if no change occurred over time.
Conclusions
In conclusion, the digital x-ray technique based on the MTP view without fluoroscopy is a simple and reliable technique for measuring the JSW in the normal knee. The greatest source of variation was due to the subject. Furthermore, the measurements of JSW across repeated radiographs (X-RAYS) were highly repeatable indicating that this technique may be effective in documenting longitudinal changes in JSW in patients who may be at risk for OA. Further studies need to be performed looking at documenting longitudinal changes in JSW in a population at risk for osteoarthritis.
Acknowledgement
This study was funded by the National Institutes of Health (AR047910; AR047910S1). These data were presented at the Annual Meeting of the Orthopaedic Research Society, Chicago, Illinois, 2006.
Footnotes
Conflicts of Interest
None of the authors have any personal or financial relationships that could bias this work.
References
- 1.Buckland-Wright JC. Radiographic assessment of osteoarthritis: Comparison between existing methodologies. Osteoarthritis Cartilage. 1999;7:430–433. doi: 10.1053/joca.1998.0234. [DOI] [PubMed] [Google Scholar]
- 2.Buckland-Wright JC, Macfarlane DG, Lynch JA, Jasani MK, Bradshaw CR. Joint space width measures cartilage thickness in osteoarthritis of the knee: high resolution plain film and double contrast macroradiographic investigation. Ann Rheum Dis. 1995;54:263–268. doi: 10.1136/ard.54.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buckland-Wright JC, Macfarlane DG, Williams SA, Ward RJ. Accuracy and precision of joint space width measurements in standard and macroradiographs of osteoarthritic knees. Ann Rheum Dis. 1995;54:872–880. doi: 10.1136/ard.54.11.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buckland-Wright JC, Wolfe F, Ward RJ. Substantial superiority of semiflexed (MTP) views in knee osteoarthritis: a comparative radiographic study, without fluoroscopy, of standing extended, semiflexed (MTP), and schuss views. J Rheumatol. 1999;26:2664–2674. [PubMed] [Google Scholar]
- 5.Cline GA, Meyer JM, Stevens R, Buckland-Wright C, Peterfy C, Beary JF. Comparison of fixed flexion, fluoroscopic semi-flexed and MTP radiographic methods for obtaining the minimum medial joint space width of the knee in longitudinal osteoarthritis trials. Osteoarthritis Cartilage. 2006;14:A32–A36. doi: 10.1016/j.joca.2006.02.023. [DOI] [PubMed] [Google Scholar]
- 6.Dupuis DE, Beynnon BD, Richard MJ, Novotny JE, Skelly JM, Cooper SM. Precision and accuracy of joint space width measurements of the medial compartment of the knee using standardized MTP semi-flexed radiographs. Osteoarthritis Cartilage. 2003;11:716–724. doi: 10.1016/s1063-4584(03)00158-4. [DOI] [PubMed] [Google Scholar]
- 7.Koo S, Gold GE, Andriacchi TP. Considerations in measuring cartilage thickness using MRI: factors influencing reproducibility and accuracy. Osteoarthritis Cartilage. 2005;13:782–789. doi: 10.1016/j.joca.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 8.Le Graverand M-PH, Mazzuca S, Lassere M, Guermazi A, Pickering E, Brandt K, et al. Assessment of the radioanatomic positioning of the osteoarthritic knee in serial radiographs: comparison of three acquisition techniques. Osteoarthritis Cartilage. 2006;14:A37–A43. doi: 10.1016/j.joca.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 9.Lequesne M. Osteoarthritic Disorders. 1st ed. American Academy of Orthopaedic Surgeons; Illinois: 1995. Quantitative measurements of joint space during progression of osteoarthritis: “Chondrometry”; p. 427. [Google Scholar]
- 10.Mazzuca SA, Brandt KD. Field test of the reproducibility of automated measurements of medial tibial femoral joint space width derived from standardized knee radiographs. J Rheumatol. 1999;26:1359–1365. [PubMed] [Google Scholar]
- 11.Mazzuca SA, Brandt KD, Buckwalter KA. Detection of radiographic joint space narrowing in subjects with knee osteoarthritis: longitudinal comparison of the metatarsophalangeal and semiflexed anteroposterior views. Arthritis Rheum. 2003;48:385–390. doi: 10.1002/art.10765. [DOI] [PubMed] [Google Scholar]
- 12.Mazzuca SA, Brandt KD, Buckwalter KA, Lane KA, Katz BP. Field test of the reproducibility of the semiflexed metatarsophalangeal view in repeated radiographic examinations of subjects with osteoarthritis of the knee. Arthritis Rheum. 2002;46:109–113. doi: 10.1002/1529-0131(200201)46:1<109::aid-art10040>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 13.Piperno M, Hellio Le Graverand MP, Conrozier T, Bochu M, Mathieu P, Vignon E. Quantitative evaluation of joint space width in femorotibial osteoarthritis: comparison of three radiographic views. Osteoarthritis Cartilage. 1998;6:252–259. doi: 10.1053/joca.1998.0118. [DOI] [PubMed] [Google Scholar]
- 14.Ravaud P, Chastang C, Auleley GR, Giraudeau B, Royant V, Amor B, et al. Assessment of joint space width in patients with osteoarthritis of the knee: a comparison of 4 measuring instruments. J Rheumatol. 1996;23:1749–1755. [PubMed] [Google Scholar]
- 15.Ravaud P, Graudeau B, Auleley GR, Chastang C, Poiraudeau S, Ayral X, et al. Radiographic assessment of knee osteoarthritis: reproducibility and sensitivity to change. J Rheumatol. 1996;23:1756–1764. [PubMed] [Google Scholar]
- 16.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh MS, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]