Abstract
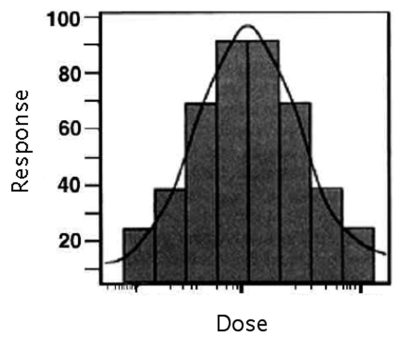
The use of low levels of visible or near infrared light for reducing pain, inflammation and edema, promoting healing of wounds, deeper tissues and nerves, and preventing cell death and tissue damage has been known for over forty years since the invention of lasers. Despite many reports of positive findings from experiments conducted in vitro, in animal models and in randomized controlled clinical trials, LLLT remains controversial in mainstream medicine. The biochemical mechanisms underlying the positive effects are incompletely understood, and the complexity of rationally choosing amongst a large number of illumination parameters such as wavelength, fluence, power density, pulse structure and treatment timing has led to the publication of a number of negative studies as well as many positive ones. A biphasic dose response has been frequently observed where low levels of light have a much better effect on stimulating and repairing tissues than higher levels of light. The so-called Arndt-Schulz curve is frequently used to describe this biphasic dose response. This review will cover the molecular and cellular mechanisms in LLLT, and describe some of our recent results in vitro and in vivo that provide scientific explanations for this biphasic dose response.
1. INTRODUCTION
1.1. Brief history
Low level laser therapy (LLLT) is the application of light (usually a low power laser or LED in the range of 1mW – 500mW) to a pathology to promote tissue regeneration, reduce inflammation and relieve pain. The light is typically of narrow spectral width in the red or near infrared (NIR) spectrum (600nm – 1000nm), with a power density (irradiance) between 1mw-5W/cm2. It is typically applied to the injury for a minute or so, a few times a week for several weeks. Unlike other medical laser procedures, LLLT is not an ablative or thermal mechanism, but rather a photochemical effect comparable to photosynthesis in plants whereby the light is absorbed and exerts a chemical change.
The phenomenon was first published by Endre Mester at Semmelweis University, Budapest, Hungary in 1967 a few years after the first working laser was invented (Mester et al. 1967). Mester conducted an experiment to test if laser radiation might cause cancer in mice. He shaved the hair off their backs, divided them into two groups and irradiated one group with a low powered ruby laser (694-nm). The treatment group did not get cancer and to his surprise, the hair grew back more quickly than the untreated group. He called this “Laser Biostimulation”.
1.2. Evidence for effectiveness of LLLT
Since 1967 over 100 phase III, randomized, double-blind, placebo-controlled, clinical trials (RCTs) have been published and supported by over 1,000 laboratory studies investigating the primary mechanisms and the cascade of secondary effects that contribute to a range of local tissue and systemic effects.
RCTs with positive outcomes have been published on pathologies as diverse as osteoarthritis (Bertolucci and Grey 1995; Ozdemir et al. 2001; Stelian et al. 1992), tendonopathies (Bjordal et al. 2006b; Stergioulas et al. 2008; Vasseljen et al. 1992), wounds (Caetano et al. 2009; Gupta et al. 1998; Ozcelik et al. 2008; Schubert et al. 2007), back pain (Basford et al. 1999), neck pain (Chow et al. 2006; Gur et al. 2004), muscle fatigue (Leal Junior et al. 2008a; Leal Junior et al. 2008b), peripheral nerve injuries (Rochkind et al. 2007) and strokes (Lampl et al. 2007; Zivin et al. 2009); nevertheless results have not always been positive. This failure in certain circumstances can be attributed to several factors including dosimetry (inadequate or too much energy delivered, inadequate or too much irradiance, inappropriate pulse structure, irradiation of insufficient area of the pathology), inappropriate anatomical treatment location and concurrent patient medication (such as steroidal and non-steroidal anti-inflammatories which can inhibit healing) (Aimbire et al. 2006; Goncalves et al. 2007).
1.3. The medicine and the dose
As with other forms of medication, LLLT has its active ingredients or “medicine” (irradiation parameters) and a “dose” (the irradiation time). Table 1 lists the key parameters that define the medicine and Table 2 defines the dose. It is beyond the scope of this paper to exhaustively list and discuss every conceivable aspect of laser radiation or other light sources however we believe we have captured the main elements with some comment on others.
TABLE 1.
Parameters involved in determining the LLLT “medicine”
| IRRADIATION PARAMETERS (The Medicine) | ||
|---|---|---|
| Irradiation Parameter | Unit of measurement | Comment |
| Wavelength | nm | Light is electromagnetic energy which travels in discrete packets that also have a wave-like property. Wavelength is measure in nanometres (nm) and is visible in the 400–700 nm range. |
| Irradiance | W/cm2 | Often called Intensity, or Power Density and is calculated as Irradiance = Power (W)/Area (cm2) |
| Pulse structure | Peak Power (W) Pulse freq (Hz) Pulse Width (s) Duty cycle (%) |
If the beam is pulsed then the Power should be the Average Power and calculated as follows: Average Power (W) = Peak Power (W) × pulse width (s) × pulse frequency (Hz) |
| Coherence | Coherence length depends on spectral bandwidth | Coherent light produces laser speckle, which has been postulated to play a role in the photobiomodulation interaction with cells and subcellular organelles. |
| Polarisation | Linear polarized or circular polarized | Polarized light may have different effects than otherwise identical non-polarized light (or even 90-degree rotated polarized light). However, it is known that polarized light is rapidly scrambled in highly scattering media such as tissue (probably in the first few hundred μm). |
TABLE 2.
Parameters involved in determining the LLLT “dose”
| IRRADIATION TIME OR ENERGY DELIVERED (The Dose) | ||
|---|---|---|
| Irradiation Parameter | Unit of measurement | Comment |
| Energy (Joules) | J | Calculated as: Energy (J) = Power (W) x time (s) This mixes medicine and dose into a single expression and ignores Irradiance. Using Joules as an expression of dose is potentially unreliable as it assumes reciprocity (the inverse relationship between power and time). |
| Energy Density | J/cm2 | Common expression of LLLT “dose” is Energy Density This expression of dose again mixes medicine and dose into a single expression and is potentially unreliable as it assumes a reciprocity relationship between irradiance and time. |
| Irradiation Time | s | In our view the safest way to record and prescribe LLLT is to define the four parameters of the medicine (see table 1.) and then define the irradiation time as “dose”. |
| Treatment interval | Hours, days or weeks | The effects of different treatment interval is underexplored at this time though there is sufficient evidence to suggest that this is an important parameter. |
Energy (J) or energy density (J/cm2) is often used as an important descriptor of LLLT dose, but this neglects the fact that energy has two components, power and time,
and it has been demonstrated that there is not necessarily reciprocity between them; in other words, if the power doubled and the time is halved then the same energy is delivered but a different biological response is often observed.
It is our view LLLT is best described as two separate sets of parameters;
The medicine (irradiation parameters)
The dose (time)
This paper will mainly focus on irradiance and time, as it is beyond the scope of this paper to report in detail on the response to all aspects laser radiation listed in the “medicine” table; however there is evidence to show that different wavelengths, pulses, coherence, polarization have some effect on the magnitude of biomodulation (see sections 3 and 4).
2. MECHANISMS OF LOW LEVEL LIGHT THERAPY
2.1. Cellular Chromophores and First Law of Photobiology
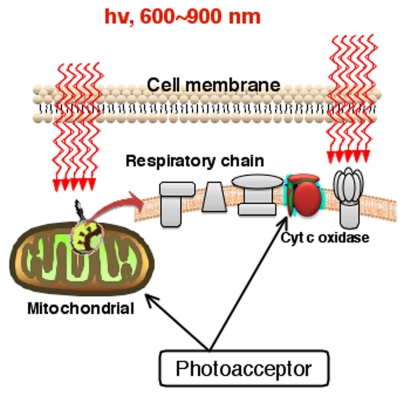
The first law of photobiology states that for low power visible light to have any effect on a living biological system, the photons must be absorbed by electronic absorption bands belonging to some molecular photoacceptors, or chromophores (Sutherland 2002). A chromophore is a molecule (or part of a molecule) which imparts some decided color to the compound of which it is an ingredient. Chromophores almost always occur in one of two forms: conjugated pi electron systems and metal complexes. Examples of such chromophores can be seen in chlorophyll (used by plants for photosynthesis), hemoglobin, cytochrome c oxidase (Cox), myoglobin, flavins, flavoproteins and porphyrins (Karu 1999). Figure 1 illustrates the general concept of LLLT.
FIGURE 1.
Schematic diagram showing the absorption of red and NIR light by specific cellular chromophores or photoacceptors localized in the mitochondrial respiratory chain
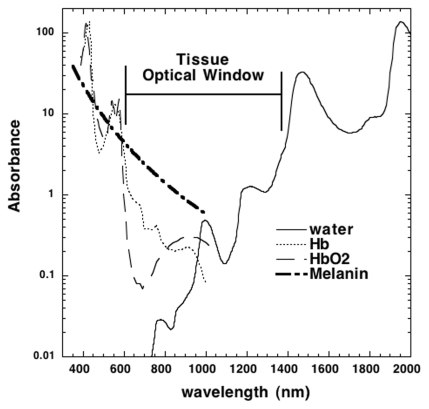
2.2. Action Spectrum and Tissue Optics
One important consideration should involve the optical properties of tissue. There is a so-called “optical window” in tissue, where the effective tissue penetration of light is maximized. This optical window runs approximately from 650 nm to 1200 nm. (Figure 2). The absorption and scattering of light in tissue are both much higher in the blue region of the spectrum than the red, because the principle tissue chromophores (hemoglobin and melanin) have high absorption bands at shorter wavelengths, tissue scattering of light is higher at shorter wavelengths, and furthermore water strongly absorbs infrared light at wavelengths greater than 1100-nm. Therefore the use of LLLT in animals and patients almost exclusively involves red and near-infrared light (600–1100-nm) (Karu and Afanas’eva 1995).
FIGURE 2.
Absorption spectra of the main chromophores in living tissue on a log scale showing the optical window where visible and NIR light can penetrate deepest into tissue.
Phototherapy is characterized by its ability to induce photobiological processes in cells. Exact action spectra are needed for determination of photoacceptors as well as for further investigations into cellular mechanisms of phototherapy. The action spectrum shows which specific wavelength of light is most effectively used in a specific chemical reaction (Karu and Kolyakov 2005). The fact that defined action spectra can be constructed for various cellular responses confirms the first law of photobiology described above (light absorption by specific molecular chromophores).
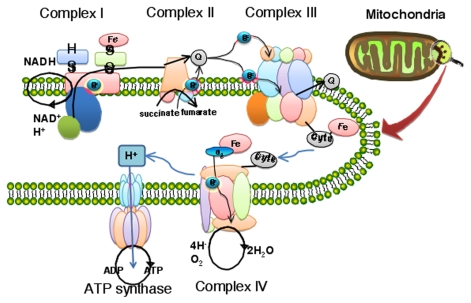
2.3. Mitochondrial Respiration and ATP
Current research about the mechanism of LLLT effects inevitably involves mitochondria. Mitochondria play an important role in energy generation and metabolism. Mitochondria are sometimes described as “cellular power plants”, because they convert food molecules into energy in the form of ATP via the process of oxidative phosphorylation (see Figure 3 for an illustartion of the mitochondrial respiratory chain).
FIGURE 3.
Mitochondrial respiratory chain consisting of contains five complexes of integral membrane proteins: NADH dehydrogenase (Complex I), succinate dehydrogenase (Complex II), cytochrome c reductase (Complex III), cytochrome c oxidase (Complex IV), and ATP synthase (ComplexV).
The mechanism of LLLT at the cellular level has been attributed to the absorption of monochromatic visible and NIR radiation by components of the cellular respiratory chain (Karu 1989). Several pieces of evidence suggest that mitochondria are responsible for the cellular response to red visible and NIR light. The effects of HeNe laser and other illumination on mitochondria isolated from rat liver, have included increased proton electrochemical potential, more ATP synthesis (Passarella et al. 1984), increased RNA and protein synthesis (Greco et al. 1989) and increases in oxygen consumption, membrane potential, and enhanced synthesis of NADH and ATP.
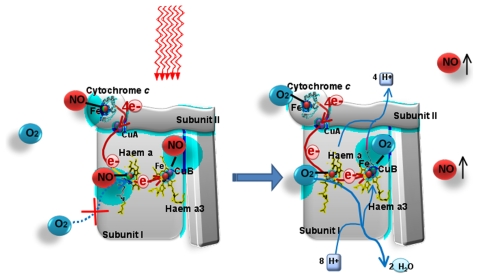
2.4. Cytochrome c oxidase and nitric oxide release
Absorption spectra obtained for cytochrome c oxidase (Cox) in different oxidation states were recorded and found to be very similar to the action spectra for biological responses to light (Karu and Kolyakov 2005). Therefore it was proposed that Cox is the primary photoacceptor for the red-NIR range in mammalian cells (Karu and Kolyakov 2005).
Nitric oxide produced in the mitochondria can inhibit respiration by binding to Cox and competitively displacing oxygen, especially in stressed or hypoxic cells (Brown 2001). Increased nitric oxide (NO) concentrations can sometimes be measured in cell culture or in animals after LLLT due to its photo release from the mitochondria and Cox. It has been proposed that LLLT might work by photodissociating NO from Cox, thereby reversing the mitochondrial inhibition of respiration due to excessive NO binding (Lane 2006). Figure 4 illustrates the photodissociation of NO from its binding sites on the heme iron and copper centers where it cometively inhibits oxygen binding and reduces necessary enzymic activity, thus allowing an immediate influx of oxygen and resumption of respiration and generation of reactive oxygen species.
FIGURE 4.
When NO is released from its binding to heme iron and copper centers in cytochrome c oxidase by the action of light, oxygen is allowed to rebind to these sites and respiration is restored to its former level leading to increased ATP synthesis.
2.5. NO signaling
In addition to NO being photodissociated from Cox as described, it may also be photo-released from other intracellular stores such as nitrosylated hemoglobin and nitrosylated myoglobin (Shiva and Gladwin 2009). Light mediated vasodilation was first described in 1968 by R F Furchgott, in his nitric oxide research that lead to his receipt of a Nobel Prize thirty years later in 1998 (Mitka 1998). Later studies conducted by other researchers confirmed and extended Furchgott’s early work and demonstrated the ability of light to influence the localized production or release of NO and stimulate vasodilation through the effect NO on cyclic guanine monophosphate (cGMP). This finding suggested that properly designed illumination devices may be effective, noninvasive therapeutic agents for patients who would benefit from increased localized NO availability
2.6. Reactive oxygen species and gene transcription
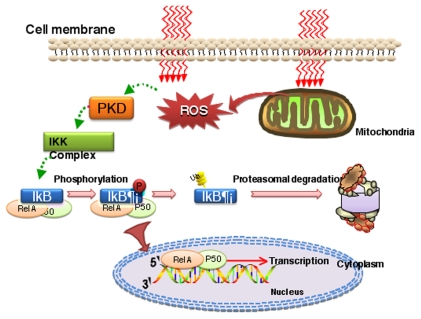
Reactive oxygen species (ROS) and reactive nitrogen species (RNS) are involved in the signaling pathways from mitochondria to nuclei. Reactive oxygen species (ROS) are very small molecules that include oxygen ions such as superoxide, free radicals such as hydroxyl radical, and hydrogen peroxide, and organic peroxides. They are highly with biological molecules such as proteins, nucleic acids and unsaturated lipids. ROS form as a natural by-product of the normal metabolism of oxygen and have important roles in cell signaling (Storz 2007), regulating nucleic acid synthesis, protein synthesis, enzyme activation and cell cycle progression (Brondon et al. 2005). LLLT was reported to produce a shift in overall cell redox potential in the direction of greater oxidation (Karu 1999) and increased ROS generation and cell redox activity have been demonstrated (Alexandratou et al. 2002; Chen et al. 2009b; Grossman et al. 1998; Lavi et al. 2003; Lubart et al. 2005; Pal et al. 2007; Zhang et al. 2008). These cytosolic responses may in turn induce transcriptional changes. Several transcription factors are regulated by changes in cellular redox state. But the most important one is nuclear factor B (NF-B). Figure 5 illustrates the effect of redox-sensitive transcription factor NF-κB activated after LLLT and is instrumental in causing transcription of protective and stimulatory gene products.
FIGURE 5.
Reactive oxygen species (ROS) formed as a result of LLLT effects in mitochondria may activate the redox-sensitive transcription factor NF-κB (relA-p50) via protein kinase D (PKD).
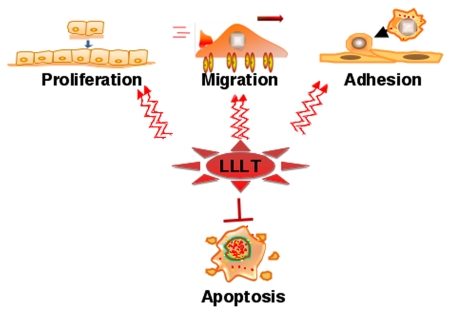
2.7. Downstream cellular response
Although the underlying mechanism of LLLT are still not completely understood, in vitro studies, animal experiments and clinical studies have all tended to indicate that LLLT delivered at low doses may produce a better result when compared to the same light delivered at high doses. LLLT can prevent cell apoptosis and improve cell proliferation, migration and adhesion at low levels of red/NIR light illumination (see Figure 6).
FIGURE 6.
The downstream cellular effects of LLLT signaling include increases in cell proliferation, migration and adhesion molecules. Cell survival is increased and cell death reduced by expression of proteins that inhibit apoptosis.
LLLT at low doses has been shown to enhance cell proliferation in vitro in several types of cells: fibroblasts (Lubart et al. 1992; Yu et al. 1994), keratinocytes (Grossman et al. 1998), endothelial cells (Moore et al. 2005), and lymphocytes (Agaiby et al. 2000; Stadler et al. 2000). The mechanism of proliferation was proposed to involve photostimulatory effects in mitochondria processes, which enhanced growth factor release, and ultimately led to cell proliferation (Bjordal et al. 2007). Kreisler et al showed (Kreisler et al. 2003) that the attachment and proliferation of human gingival fibroblasts were enhanced by LLLT in a dose-dependent manner. LLLT modulated matrix metalloproteinase activity and gene expression in porcine aortic smooth muscle cells (Gavish et al. 2006). Shefer at el. showed (Shefer et al. 2002) that LLLT could activate skeletal muscle satellite cells, enhancing their proliferation, inhibiting differentiation and regulating protein synthesis.
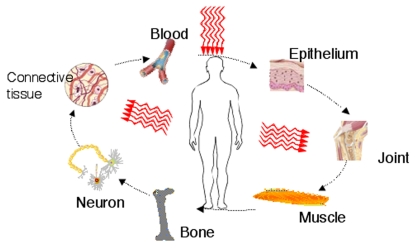
2.8. Downstream tissue response
There have been a large number of both animal model and clinical studies that demonstrated highly beneficial LLLT effects on a variety of diseases, injuries, and has been widely used in both chronic and acute conditions (see Figure 7). LLLT may enhance neovascularisation, promote angiogenesis and increase collagen synthesis to promote healing of acute (Hopkins et al. 2004) and chronic wounds (Yu et al. 1997). LLLT provided acceleration of cutaneous wound healing in rats with a biphasic dose response favoring lower doses (Corazza et al. 2007). LLLT can also stimulate healing of deeper structures such as nerves (Gigo-Benato et al. 2004), tendons (Fillipin et al. 2005), cartilage (Morrone et al. 2000), bones (Weber et al. 2006) and even internal organs (Shao et al. 2005). LLLT can reduce pain (Bjordal et al. 2006a), inflammation (Bjordal et al. 2006b) and swelling (Carati et al. 2003) caused by injuries, degenerative diseases or autoimmune diseases. Oron reported beneficial effect of LLLT on repair processes after injury or ischemia in skeletal and heart muscles in multiple animal models in vivo (Ad and Oron 2001; Oron et al. 2001a; Oron et al. 2001b; Yaakobi et al. 2001). LLLT has been used to mitigate damage after strokes (in both animals (Lapchak et al. 2008) and humans (Lampl et al. 2007)), after traumatic brain injury (Oron et al. 2007) and after spinal cord injury (Wu et al. 2009).
FIGURE 7.
Beneficial tissue effects of LLLT can include almost all the tissues and organs of the body.
3. REVIEW OF BIPHASIC DOSE RESPONSES IN LLLT
3.1. Dose dependence and dose rate effects—the biphasic curve
A biphasic response has been demonstrated many times in LLLT research (Lanzafame et al. 2007; Oron et al. 2001a) and the “Arndt-Schulz Law” is frequently quoted as a suitable model to describe dose dependent effects of LLLT (Chow et al. 2006; Hawkins and Abrahamse 2006a; Hawkins and Abrahamse 2006b; Lubart et al. 2006; Sommer et al. 2001). The concept of the Arndt-Schulz Law dates from the years around the end of the nineteenth century, when H. Schulz published a series of papers that examined the activity of various kinds of poisons (iodine, bromine, mercuric chloride, arsenious acid, etc.) on yeast, showing that almost all these agents have a slightly stimulatory effect on the yeast metabolism when given in low doses (Schulz 1877; Schulz 1888). He then came into contact with the psychiatrist R. Arndt and together they developed a principle that later became known as the ‘Arndt-Schulz law’, stating that weak stimuli slightly accelerate vital activity, stronger stimuli raise it further, but a peak is reached and even stronger stimuli suppress it, until a negative response is finally achieved (Martius 1923). In 1960 Townsend and Luckey surveyed the field of classic medical pharmacology and published a list of 100 substances known to be capable of causing an inhibition at high concentrations and stimulation at low concentrations and termed the phenomenon “hormoligosis” (Townsend and Luckey 1960). The modern term “hormesis” was first used by Stebbing in 1982 (Stebbing 1982) and has been thoroughly reviewed by Calabrese (Calabrese 2001b; Calabrese 2002; Calabrese 2004a; Calabrese 2004b; Calabrese 2005).
In the context of LLLT the increasing “stimulus” may be irradiation time or increased irradiance. This non-linear effect contradicts the Bunsen-Roscoe rule of reciprocity (which was originally formulated for visual detection of light by photoreceptors (Brindley 1952)), which predicts that if the products of exposure time in seconds and irradiance in mW/cm2 are equal, i.e. the energy density is the same, then the changes in biological endpoint will be equal. This inverse linear relationship between irradiance and time has frequently failed in LLLT research (Karu and Kolyakov 2005; Lubart et al. 2006).
A “biphasic” curve can be used to illustrate the expected dose response to light at a subcellular, cellular, tissue or clinical level. Simply put, it suggests that if insufficient energy is applied there will be no response (because the minimum threshold has not been met), if more energy is applied the then a threshold is crossed and biostimulation is achieved but when too much energy is applied then the stimulation disappears and is replaced by bioinhibition instead. An idealized illustration (Figure 8) similar to that suggested by Sommer (Sommer et al. 2001) helps understand the concept.
FIGURE 8.
Idealized biphasic dose response curve (often termed Arndt-Schulz curve) typically reported in LLLT studies.
3.2. Biphasic Response—irradiance
As early as 1978 Endre Mester observed a “threshold phenomenon” after laser irradiation of lymphocytes in vitro (Mester et al. 1978). Peter Bolton in 1991 irradiating macrophages with two different irradiances (W/cm2) but the same energy density (J/cm2) recorded different results (Bolton et al. 1991). Karu (Karu and Kolyakov 2005) found a dependence of stimulation of DNA synthesis rate on light intensity at a constant energy density 0.1 J/cm2 with a clear maximum at 0.8 mW/cm2. In another study (Karu et al. 1997) the same group found no less than seven maxima in the dose vs. biological effect curves using a pulsed 810-nm diode laser. Four different biological models were used: luminol-amplified chemiluminescence measured in nucleated cells of murine spleen (splenocytes), bone marrow (karyocytes), and murine blood and adhesion of HeLa cells cultivated in vitro. The peaks coincided for all four models. Anders conducted the widest ranging in-vitro study (on normal human neural progenitor cells) with four different energy density groups, each group tested across a range of six different irradiance parameters (Anders et al. 2007) Table 3.
TABLE 3.
Comparison of different irradiances and fluences of 810-nm laser on differentiation of normal human neural progenitor cells. Cells received light once a day for three days and neurite outgrowth was measured.
|
Anders et al. 2007 Average Summed Neurite Length Parameters | ||||||
|---|---|---|---|---|---|---|
| 1 mW/cm2 | 5 mW/cm2 | 15 mW/cm2 | 19 mW/cm2 | 25 mW/cm2 | 50 mW/cm2 | |
| 0.01 J/cm2 | NS | NS | — | NS | — | — |
| 0.05 J/cm2 | NS | NS | NS | S | S | NS |
| 0.2 J/cm2 | NS | NS | NS | S | S | S |
| 1 J/cm2 | NS | NS | NS | NS | NS | S |
NS: No statistical difference.
S: Groups significantly greater than Factors group.
(One way ANOVA *p<0.01, **p<0.001)
In 1979 Ginsbach found that laser stimulation of wound closure had “no reciprocity relation”. His controlled experiments on rats with He-Ne laser at an energy density of 4 J/cm2 found stimulation at an irradiance of 45 mW/cm2 but not at 12.4 mW/cm2 (Ginsbach 1979). Uri Oron (Oron et al. 2001a) showed different reductions of infarct size after induced heart attacks in rats. Keeping energy density constant and varying the irradiance he found that the beneficial effects were maximumal at 5 mW/cm2 and significantly less effect both at lower irradiances (2.5 mW/cm2) and also at higher irradiances (25 mW/cm2). Ray Lanzafame (Lanzafame et al. 2007) conducted a study varying irradiance and interval on laser-induced healing of pressure ulcers in mice. Energy density (5 J/cm2) was fixed but four different irradiance (0.7 – 40 mW/cm2) parameters were tested with a significant improvement only occurring for 8 mW/cm2
We know of only one human clinical trial which varied irradiance but this trial kept treatment time the same so energy density (J/cm2) did not remain the same. This RCT by Hashimoto on the treatment of the stellate ganglion to reduce pain in patients with post herpetic neuralgia of the facial type. This study compared the effects of 830-nm lasers delivering 60 mW, 150 mW and placebo, each applied for 3 minutes to the anterior aspect of the lateral process of the 7th cervical vertebrae. Each patient had three treatments (one treatment, three consecutive days), each treatment was with a different laser or placebo. The study was properly blinded and randomized. There was a significant difference in skin temperature of the forehead and in recorded pain scores. The greatest improvements were for the 150mW laser (Hashimoto et al. 1997).
There have been several systematic reviews and meta analyses of RCTs and these have revealed some irradiance dependant effects: Bjordal published a review of LLLT for chronic joint disorders and identified 14 RCTs of suitable methodological quality, 4 of which failed to report a significant effect because the irradiance was either too high or too low, and/or delivered insufficient energy, the remaining eight studies all produced positive effects (Bjordal et al. 2003). Tumilty reviewed 25 LLLT RCTs of tendinopathies,13 of which (55%) failed to produce a positive outcome, all of these negative/inconclusive studies that recorded irradiance (or could subsequently be established) had delivered an irradiance in excess of the guidelines set by the World Association for Laser Therapy (www.walt.nu) (Tumilty et al. 2009).
3.3. Biphasic Response—time or energy density
Again, Peter Bolton’s study mentioned in 3.2 above had an energy density aspect showing a different response for each of the irradiances used. For the 400mW/cm2 study he found increasing energy density from 2.4 J/cm2 to 7.2 J/cm2 increased fibroblast proliferation, in the 800 mW/cm2 group increasing energy density from 2.4 J/cm2 to 7.2 J/cm2 decreased fibroblast proliferation (Bolton et al. 1991). Anders’ study also mentioned in 3.2 above looked at four energy density groups, and for the irradiance parameters that produced significant results increasing energy density increased neurite length (Anders et al. 2007) Table 3. Yamaura and colleagues found a biphasic dose response in MTT activity in rheumatoid arthritis synoviocytes after 810-nm laser with a peak at 8 J/cm2 and less effect at lower and higher fluences (Yamaura et al. 2009). Loevschall measured human oral mucosal fibroblast cell proliferation by incorporation of tritiated thymidine after varying fluences of 812-nm laser delivered at 4.5 mW/cm2 and found a biphasic dose response with a distinct peak at 0.45 J/cm2 (Loevschall and Arenholt-Bindslev 1994). Another study (al-Watban and Andres 2001) looked at chinese hamster ovary and human fibroblast proliferation after various fluences of He-Ne laser delivered at a constant irradiance of 1.25 mW/cm2. Again they found a clear biphasic dose response with a peak at 0.18 J/cm2. Zhang et al (Zhang et al. 2003) found a biphasic dose response in human fibroblast cell numbers after treatment with varying fluences of 628-nm light, with a maximum increase of 30% after 0.88 J/cm2 and an actual reduction appearing at 9 J/cm2. Brondon and colleagues (Brondon et al. 2005) found that two treatments per day caused a bigger increase than 1 or 4 treatments per day measuring proliferation index in human HEP-2 and murine L-929 cell lines. They used a 670 nm light emitting diode device with an irradiance of 10 mW/cm2 and each single treatment was 5 J/cm2 and the course was stopped after 50 J/cm2 had been given (at 10, 5 or 2.5 days).
Lopes-Martins showed a biphasic response to LLLT on the number of mononuclear cells that accumulate in pleural cavity after carrageenan injection. The results showed neutrophil influx mice treated with three different laser fluencies at 1, 2.5 & 5 J/cm2) with 2.5 having the greatest effect (Lopes-Martins et al. 2005).
As stated in 3.2 above, Hashimoto reported on the laser treatment of the stellate ganglion to reduce pain in patients with post herpetic neuralgia of the facial type. The study compared the effects of 830-nm lasers delivering 60mW, 150mW and placebo, The greatest improvements were for the 150mW laser (Hashimoto et al. 1997). Again as stated in 3.2 above, there have been several systematic reviews and meta analyses of RCTs and these revealed some energy density dependant effects (Bjordal et al. 2003; Tumilty et al. 2009).
3.4. Beam measurement reporting errors
One notable aspect of the dose rate (W/cm2) studies is the wide variation of “optimal” irradiances in vitro studies as they range from 1–800 mW/cm2 in just the few papers referenced in this review. If the primary photo acceptor is cytochrome C oxidase as postulated here, then why would so many authors arrive at different conclusions for optimal parameters in vitro, should it not be the same for all of them?
Explanations may include, the slightly different wavelengths used or sensitivity due the redox state of mitochondia in the target cells (Tafur and Mills 2008), but we consider that the greater contributor may be laser beam measurement problems. It may be a surprise to non-physicists that diode laser beams are not inherently round, and even if circularizing lenses are used to correct this, then the beam intensity distribution is not homogeneous. Laser beams are brighter (higher irradiance) in the middle and weaker towards the edge. Cells in the centre of a culture well will be exposed to considerably higher irradiances than those on the periphery. Because the edge of a laser beam is hard to define and find this could mean that irradiance calculations are significantly different between research centers. Agreement on beam measurement and reporting of intensity distribution is needed to reduce these inconsistencies. This is important not only for in vitro studies but also in vivo and clinical trials as reporting of irradiance is just as important though we accept that tissue scattering diffuses the beam probably making non-homogenous sources less critical to clinical effectiveness.
4. BIPHASIC LLLT DOSE RESPONSE STUDIES IN OUR LABORATORY
4.1. In vitro activation of NF-κB
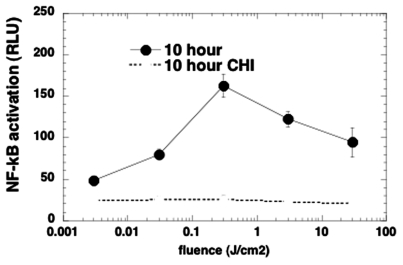
We developed the hypothesis (Chen et al. 2009a) that NIR light (810-nm laser) would activate the transcription factor NF-κB by generating reactive oxygen species from the mitochondria (see section 2.5). We tested this in mouse embryonic fibroblasts that had been genetically engineered to synthesize luciferase in response to NF-κB activation (Chen et al. 2009a). We used a wide range (four orders of magnitude) of delivered fluences by adjusting the laser power so that the illumination time was kept constant at 5 minutes. As shown in Figure 9 there was a biphasic dose dependent activation of NF-κB as measured by luciferase assay 10 hours after the illumination was completed. There was no significant increase at 0.003 J/cm2 compared to the dark control, a small increase at 0.03 J/cm2,, the maximum activation was observed at 0.3 J/cm2, while at 3 J/cm2 and even more so at 30 J/cm2 there was a decrease in NF-κB activation, but the level was still higher than that found at 0.03 J/cm2. The level of luciferase expression was also measured in the presence of cycloheximide (CHI) as a control. CHI is a protein synthesis inhibitor that removes even the background level of luciferase seen in dark control cells, as well as all the increases seen with the different fluences of 810-nm light.
FIGURE 9.
Biphasic dose response of NF-κB activation (measured by bioluminescence reporter assay) in mouse embryonic fibroblasts 10 hours after different fluences of 810-nm laser light. CHI is control where all protein synthesis has been inhibited.
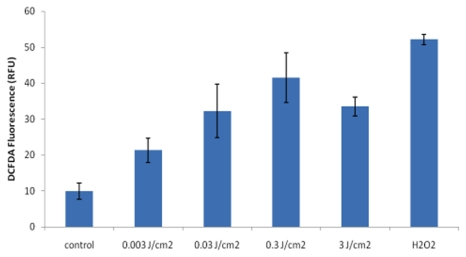
We tested the hypothesis that the activation of NF-κB by LLLT was mediated by generation of ROS because NF-κB is known to be a redox-sensitive transcription factor (Schreck et al. 1992) and moreover ROS have previously been shown to be generated during LLLT (Alexandratou et al. 2002; Lubart et al. 2005; Pal et al. 2007). We used dichlorodihydro-fluorescein diacetate (DCHF-DA) which is taken up into cells, hydrolyzed and oxidized to a fluorescent form by most species of ROS probably via lipid peroxides (Diaz et al. 2003). As can be seen in Figure 10 even the low fluence of 0.003 J/cm2 produced detectable levels of ROS, greater at 0.03 J/cm2 and maximum at 0.3 J/cm2 with a slight decrease observed at 3 J/cm2. The maximum level observed at 0.3 J/cm2 was only slightly less than that observed inside the cells after addition of hydrogen peroxide to the extracellular medium.
FIGURE 10.
Biphasic dose response in generation of ROS as detected by fluorescence probe under same conditions as Fig 9 but measured at 5 minutes post-irradiation.
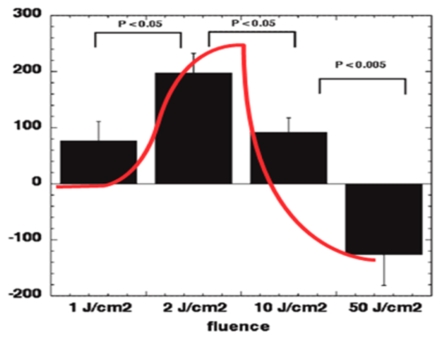
4.2. Mouse wound healing
In an in vivo study (Demidova-Rice et al. 2007) we used a set of fluences of 635-nm (+/−15-nm) light delivered from a filtered lamp. The model was a full thickness dorsal excisional wound in BALB/c mice treated with a single exposure to light 30 minutes after wounding. These fluences were 1, 2, 10 and 50 J/cm2 delivered at constant fluence rate of 100 mW/cm2 and taking 10, 20, 100 and 500 seconds respectively. In this model the untreated wound tends to expand for 2–3 days after it was made, but even a brief exposure to light soon after wounding, reduces or stops the expansion of the wound and the integrated time course of the wound size can therefore be significantly reduced. Our hypothesis is that fibroblasts in the edge of the wounded dermis can be transformed into myofibroblasts, and the contractile nature of these cells with their smooth muscle actin fibers prevents the wound expanding. It should be noted that the fibroblast-myofibroblast transition can be mediated by NF-κB activation (Watson et al. 2008). As shown in Figure 11 there was a biphasic dose response with positive effects (difference in integrated area under the curve of time course of wound size compared to no treatment control) seen in low doses with a clear maximum seen at 2 J/cm2, and the high dose of 50 J/cm2 actually gave a worsening of the wound healing time curve i.e. there was a greater expansion of the wound compared with non-treated controls.
FIGURE 11.
Biphasic dose response in measured difference in integrated area under the curve of time course of wound size compared to no treatment control, with a clear maximum seen at 2 J/cm2, and the high dose of 50 J/cm2 gave a worsening of the wound healing time curve.
4.3. Rat arthritis
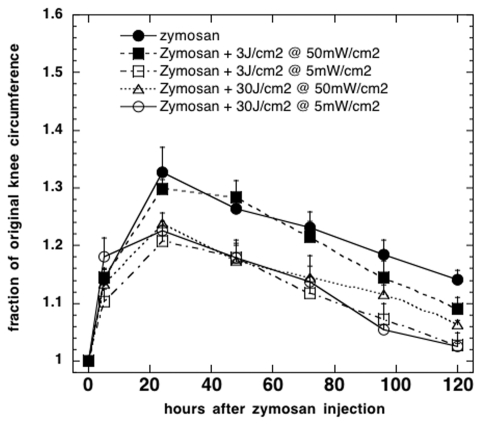
In another in vivo study (Castano et al. 2007) we investigated whether LLLT using an 810-nm laser could have a therapeutic effect in a rat model of inflammatory arthritis caused by zymosan injected into their knee joints. In this model the severity of the arthritis is quantified by measuring the diameter of the swollen joint every day and plotting a time course for each joint. We compared illumination regimens consisting of a high and low fluence (3 and 30 J/cm2), delivered at high and low irradiance (5 and 50 mW/cm2) using 810-nm laser light daily for 5 days, with the positive control of conventional corticosteroid (dexamethasone) therapy.
As shown in Figure 12 three of the illumination regimens were effective in reducing the mean integrated knee swelling almost as much as the positive control of the powerful steroid, dexamathasone; these were 3 J/cm2 delivered at 5 mW/cm2 and 30 J/cm2 delivered at 50 mW/cm2 both of which took 10 minutes, and 30 J/cm2 delivered at 5 mW/cm2 which took 100 minutes. The only ineffective dose regimen was 3 J/cm2 delivered at 50 mW/cm2 which took the comparatively short time of 1 minute to deliver. This observation led us to propose that the illumination time was an important parameter in some LLLT applications.
FIGURE 12.
Dose response of illumination time found in a study of 810-nm laser to treat zymosan-induced arthritis in rats. Integrated curves of knee circumference versus time were compared. Three LLLT regimens were equally successful where the illumination time was either 100 minutes or 10 minutes, but the ineffective regimen only had a 1 minute illumination time.
5. POSSIBLE EXPLANATIONS FOR BIPHASIC DOSE RESPONSE IN LLLT
The repeated observations that have been made of the biphasic dose response phenomenon in LLLT require some explanation. The natural assumption that is frequently made is, that if a small dose of red or near-infrared light produces a significant therapeutic effect, then a larger dose should produce an even more beneficial effect. This natural assumption is frequently not the case. We here propose three possible explanations for the existence of the biphasic dose response based upon mechanistic considerations outlined in section 2.
5.1. Excessive ROS
As discussed in 2.5 the light mediated generation of reactive oxygen species has been observed in many in vitro studies and has been proposed to account for the cellular changes observed after LLLT via activation of redox sensitive transcription factors (Chen et al. 2009a). The evidence of ROS mediated activation of NF-κB in MEF cells presented in 4.1 provides additional support for this hypothesis (Chen et al. 2009a). It is well-accepted that ROS can have both beneficial and harmful effects (Huang and Zheng 2006). Hydrogen peroxide is often used to kill cells in vitro (Imlay 2008). Other ROS such as singlet oxygen (Klotz et al. 2003) and hydroxyl radicals (Pryor et al. 2006) are thought to be harmful even at low concentrations. The concept of biphasic dose response in fact is well established in the field of oxidative stress (Day and Suzuki 2005). If the generation of ROS can be shown to be dose dependent on the delivered energy fluence this may provide an explanation for the stimulation and inhibition observed with low and high light fluences.
5.2. Excessive NO
The other mechanistic hypothesis that is put forward to explain the cellular effects of LLLT relates to the photolysis of nitrosylated proteins that releases free NO (see section 2.6). Again the literature has many papers that discuss the so-called two-faced or “Janus” molecule NO (Anggard 1994; Lane and Gross 1999). NO can be either protective or harmful depending on the dose and particularly on the cell or tissue type where it is generated (Calabrese 2001a).
5.3. Activation of a cytotoxic pathway
The third hypothesis to explain the biphasic dose response of LLLT is the idea that the protective and stimulatory effects of light occur at low doses, but there is an additional pathway that leads to damaging effects of light that only occurs at high doses, and effectively overwhelms the beneficial effects of low doses of light. Work from South China Normal University provides some support for this hypothesis. Low doses of LLLT were found to phosphorylate hepatocyte growth factor receptor (c-Met), and initiate signaling via cyclic AMP and Jun kinase and Src (Gao and Xing 2009). By contrast, high dose LLLT was found to induce apoptosis via a mitochondrial caspase-3 pathway and cytochrome c release was attributed to opening of the mitochondrial permeability transition pore caused by high-level intracellular reactive oxygen species (ROS) generation (Wu et al. 2009). A secondary signaling pathway through Bax activation was observed (Wu et al. 2009).
6. SUMMARY AND CONCLUSION
LLLT delivered at low doses tends to work better than the same wavelength delivered at high levels, which illustrates the basic concept of bipha-sic dose response or hormesis (Calabrese 2001b). In general, fluences of red or NIR as low as 3 or 5 J/cm2 will be beneficial in vivo, but a large dose like 50 or 100 J/cm2 will lose the beneficial effect and may even become detrimental. The molecular and cellular mechanisms LLLT suggest that photons are absorbed by the mitochondria; they stimulate more ATP production and low levels of ROS, which then activates transcription factors, such as NF-κB, to induce many gene transcript products responsible for the beneficial effects of LLLT. ROS are well known to stimulate cellular proliferation of low levels, but inhibit proliferation and kill cells at high levels. Nitric oxide is also involved in LLLT, and may be photo-released from its binding sites in the respiratory chain and elsewhere. It is possible that NO release in low amounts by low dose light may be beneficial, while high levels released by high dose LLLT may be damaging. The third possibility is that LLLT may activate transcription factors, upregulating protective proteins which are anti-apoptotic, and generally promote cell survival. In contrast, it is entirely possible that different transcription factors and cell-signaling pathways, that promote apoptosis, could be activated after higher light exposure. We believe that further advances in the mechanistic understanding of LLLT will continue to be made in the near future. These advances will lead to greater acceptance of LLLT in mainstream medicine and may lead to LLLT being used for serious diseases such as stroke, heart attack and degenerative brain diseases. Nevertheless the concept of biphasic dose response or LLLT hormesis (low levels of light are good for you, while high levels are bad for you) will remain.
ACKNOWLEDGMENTS
Research in the Hamblin laboratory is supported by the US NIH (grants R01CA/AI838801 and R01AI050875 to MRH).
REFERENCES
- Ad N, Oron U. Impact of low level laser irradiation on infarct size in the rat following myocardial infarction. Int J Cardiol. 2001;80:109–16. doi: 10.1016/s0167-5273(01)00503-4. [DOI] [PubMed] [Google Scholar]
- Agaiby AD, Ghali LR, Wilson R, Dyson M. Laser modulation of angiogenic factor production by T-lymphocytes. Lasers Surg Med. 2000;26:357–63. doi: 10.1002/(sici)1096-9101(2000)26:4<357::aid-lsm3>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Aimbire F, Albertini R, Pacheco MT, Castro-Faria-Neto HC, Leonardo PS, Iversen VV, Lopes-Martins RA, Bjordal JM. Low-level laser therapy induces dose-dependent reduction of TNFalpha levels in acute inflammation. Photomed Laser Surg. 2006;24:33–7. doi: 10.1089/pho.2006.24.33. [DOI] [PubMed] [Google Scholar]
- al-Watban FA, Andres BL. The effect of He-Ne laser (632.8 nm) and Solcoseryl in vitro. Lasers Med Sci. 2001;16:267–75. doi: 10.1007/pl00011363. [DOI] [PubMed] [Google Scholar]
- Alexandratou E, Yova D, Handris P, Kletsas D, Loukas S. Human fibroblast alterations induced by low power laser irradiation at the single cell level using confocal microscopy. Photochem Photobiol Sci. 2002;1:547–52. doi: 10.1039/b110213n. [DOI] [PubMed] [Google Scholar]
- Anders J, Romanczyk T, Moges H, Ilev I, Waynant R, Longo L. Light Interaction With Human Central Nervous System Progenitor Cells. NAALT conference proceedings; 2007. 2007. [Google Scholar]
- Anggard E. Nitric oxide: mediator, murderer, and medicine. Lancet. 1994;343:1199–206. doi: 10.1016/s0140-6736(94)92405-8. [DOI] [PubMed] [Google Scholar]
- Basford JR, Sheffield CG, Harmsen WS. Laser therapy: a randomized, controlled trial of the effects of low-intensity Nd:YAG laser irradiation on musculoskeletal back pain. Arch Phys Med Rehabil. 1999;80:647–52. doi: 10.1016/s0003-9993(99)90167-3. [DOI] [PubMed] [Google Scholar]
- Bertolucci LE, Grey T. Clinical analysis of mid-laser versus placebo treatment of arthralgic TMJ degenerative joints. Cranio. 1995;13:26–9. doi: 10.1080/08869634.1995.11678038. [DOI] [PubMed] [Google Scholar]
- Bjordal JM, Couppe C, Chow RT, Tuner J, Ljunggren EA. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother. 2003;49:107–16. doi: 10.1016/s0004-9514(14)60127-6. [DOI] [PubMed] [Google Scholar]
- Bjordal JM, Johnson MI, Iversen V, Aimbire F, Lopes-Martins RA. Photoradiation in acute pain: a systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed Laser Surg. 2006a;24:158–68. doi: 10.1089/pho.2006.24.158. [DOI] [PubMed] [Google Scholar]
- Bjordal JM, Johnson MI, Lopes-Martins RA, Bogen B, Chow R, Ljunggren AE. Short-term efficacy of physical interventions in osteoarthritic knee pain. A systematic review and meta-analysis of randomised placebo-controlled trials BMC Musculoskelet Disord. 2007;8:51. doi: 10.1186/1471-2474-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjordal JM, Lopes-Martins RA, Iversen VV. A randomised, placebo controlled trial of low level laser therapy for activated Achilles tendinitis with microdialysis measurement of peritendinous prostaglandin E2 concentrations. Br J Sports Med. 2006b;40:76–80. doi: 10.1136/bjsm.2005.020842. discussion 76-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton P, Young S, Dyson M. Macrophage responsiveness to light therapy with varying power and energy densities. Laser Ther. 1991;3:6–9. doi: 10.1002/lsm.1900090513. [DOI] [PubMed] [Google Scholar]
- Brindley GS. The Bunsen-Roscoe law for the human eye at very short durations. J Physiol. 1952;118:135–139. doi: 10.1113/jphysiol.1952.sp004779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondon P, Stadler I, Lanzafame RJ. A study of the effects of phototherapy dose interval on photobiomodulation of cell cultures. Lasers Surg Med. 2005;36:409–13. doi: 10.1002/lsm.20183. [DOI] [PubMed] [Google Scholar]
- Brown GC. Regulation of mitochondrial respiration by nitric oxide inhibition of cytochrome c oxidase. Biochim Biophys Acta. 2001;1504:46–57. doi: 10.1016/s0005-2728(00)00238-3. [DOI] [PubMed] [Google Scholar]
- Caetano KS, Frade MA, Minatel DG, Santana LA, Enwemeka CS. Phototherapy Improves Healing of Chronic Venous Ulcers. Photomed Laser Surg. 2009 doi: 10.1089/pho.2008.2398. [DOI] [PubMed] [Google Scholar]
- Calabrese EJ. Nitric oxide: biphasic dose responses. Crit Rev Toxicol. 2001a;31:489–501. doi: 10.1080/20014091111776. [DOI] [PubMed] [Google Scholar]
- Calabrese EJ. The future of hormesis: where do we go from here? Crit Rev Toxicol. 2001b;31:637–48. doi: 10.1080/20014091111901. [DOI] [PubMed] [Google Scholar]
- Calabrese EJ. Hormesis: changing view of the dose-response, a personal account of the history and current status. Mutat Res. 2002;511:181–9. doi: 10.1016/s1383-5742(02)00013-3. [DOI] [PubMed] [Google Scholar]
- Calabrese EJ. Hormesis: a revolution in toxicology, risk assessment and medicine. EMBO Rep 5. 2004a;Spec No:S37–40. doi: 10.1038/sj.embor.7400222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrese EJ. Hormesis: from marginalization to mainstream: a case for hormesis as the default dose-response model in risk assessment. Toxicol Appl Pharmacol. 2004b;197:125–36. doi: 10.1016/j.taap.2004.02.007. [DOI] [PubMed] [Google Scholar]
- Calabrese EJ. Hormetic dose-response relationships in immunology: occurrence, quantitative features of the dose response, mechanistic foundations, and clinical implications. Crit Rev Toxicol. 2005;35:89–295. doi: 10.1080/10408440590917044. [DOI] [PubMed] [Google Scholar]
- Carati CJ, Anderson SN, Gannon BJ, Piller NB. Treatment of postmastectomy lymphedema with low-level laser therapy: a double blind, placebo-controlled trial. Cancer. 2003;98:1114–22. doi: 10.1002/cncr.11641. [DOI] [PubMed] [Google Scholar]
- Castano AP, Dai T, Yaroslavsky I, Cohen R, Apruzzese WA, Smotrich MH, Hamblin MR. Low-level laser therapy for zymosan-induced arthritis in rats: Importance of illumination time. Lasers Surg Med. 2007;39:543–50. doi: 10.1002/lsm.20516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen AC-H, Arany PR, Huang Y-Y, Tomkinson EM, Saleem T, Yull FE, Blackwell TS, Hamblin MR. Low level laser therapy activates NF-κB via generation of reactive oxygen species in mouse embryonic fibroblasts. In: Hamblin M.R., Anders J.J., Waynant R.W., editors. Mechanisms for Low-Light Therapy IV. Vol. 7165. The International Society for Optical Engineering, Bellingham, WA: San Jose; 2009a. pp doi: 101117/12809605. [Google Scholar]
- Chen AC-H, Arany PR, Huang YY, Tomkinson EM, Saleem T, Yull FE, Blackwell TS, Hamblin MR. Low level laser therapy activates NF-κB via generation of reactive oxygen species in mouse embryonic fibroblasts. Proc SPIE. 2009b doi: 10.1371/journal.pone.0022453. in press: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow RT, Heller GZ, Barnsley L. The effect of 300 mW, 830 nm laser on chronic neck pain: a double-blind, randomized, placebo-controlled study. Pain. 2006;124:201–10. doi: 10.1016/j.pain.2006.05.018. [DOI] [PubMed] [Google Scholar]
- Corazza AV, Jorge J, Kurachi C, Bagnato VS. Photobiomodulation on the angiogenesis of skin wounds in rats using different light sources. Photomed Laser Surg. 2007;25:102–6. doi: 10.1089/pho.2006.2011. [DOI] [PubMed] [Google Scholar]
- Day RM, Suzuki YJ. Cell proliferation, reactive oxygen and cellular glutathione. Dose Response. 2005;3:425–42. doi: 10.2203/dose-response.003.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demidova-Rice TN, Salomatina EV, Yaroslavsky AN, Herman IM, Hamblin MR. Low-level light stimulates excisional wound healing in mice. Lasers Surg Med. 2007;39:706–15. doi: 10.1002/lsm.20549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz G, Liu S, Isola R, Diana A, Falchi AM. Mitochondrial localization of reactive oxygen species by dihydrofluorescein probes. Histochem Cell Biol. 2003;120:319–25. doi: 10.1007/s00418-003-0566-8. [DOI] [PubMed] [Google Scholar]
- Fillipin LI, Mauriz JL, Vedovelli K, Moreira AJ, Zettler CG, Lech O, Marroni NP, Gonzalez-Gallego J. Low-level laser therapy (LLLT) prevents oxidative stress and reduces fibrosis in rat traumatized Achilles tendon. Lasers Surg Med. 2005;37:293–300. doi: 10.1002/lsm.20225. [DOI] [PubMed] [Google Scholar]
- Gao X, Xing D. Molecular mechanisms of cell proliferation induced by low power laser irradiation. J Biomed Sci. 2009;16:4. doi: 10.1186/1423-0127-16-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavish L, Perez L, Gertz SD. Low-level laser irradiation modulates matrix metalloproteinase activity and gene expression in porcine aortic smooth muscle cells. Lasers Surg Med. 2006;38:779–86. doi: 10.1002/lsm.20383. [DOI] [PubMed] [Google Scholar]
- Gigo-Benato D, Geuna S, de Castro Rodrigues A, Tos P, Fornaro M, Boux E, Battiston B, Giacobini-Robecchi MG. Low-power laser biostimulation enhances nerve repair after end-to-side neurorrhaphy: a double-blind randomized study in the rat median nerve model. Lasers Med Sci. 2004;19:57–65. doi: 10.1007/s10103-004-0300-3. [DOI] [PubMed] [Google Scholar]
- Ginsbach G. Laser induced stimulation of woundhealing in bad healing wounds. Proc Laser '79 Opto Elektronics Conf Munich; Guildford UK: IPC Science and Technology Press; 1979. p. 5. [Google Scholar]
- Goncalves WL, Souza FM, Conti CL, Cirqueira JP, Rocha WA, Pires JG, Barros LA, Moyses MR. Influence of He-Ne laser therapy on the dynamics of wound healing in mice treated with anti-inflammatory drugs. Braz J Med Biol Res. 2007;40:877–84. doi: 10.1590/s0100-879x2007000600018. [DOI] [PubMed] [Google Scholar]
- Greco M, Guida G, Perlino E, Marra E, Quagliariello E. Increase in RNA and protein synthesis by mitochondria irradiated with helium-neon laser. Biochem Biophys Res Commun. 1989;163:1428–34. doi: 10.1016/0006-291x(89)91138-8. [DOI] [PubMed] [Google Scholar]
- Grossman N, Schneid N, Reuveni H, Halevy S, Lubart R. 780 nm low power diode laser irradiation stimulates proliferation of keratinocyte cultures: involvement of reactive oxygen species. Lasers Surg Med. 1998;22:212–8. doi: 10.1002/(sici)1096-9101(1998)22:4<212::aid-lsm5>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Gupta AK, Filonenko N, Salansky N, Sauder DN. The use of low energy photon therapy (LEPT) in venous leg ulcers: a double-blind, placebo-controlled study. Dermatol Surg. 1998;24:1383–6. doi: 10.1111/j.1524-4725.1998.tb00019.x. [DOI] [PubMed] [Google Scholar]
- Gur A, Sarac AJ, Cevik R, Altindag O, Sarac S. Efficacy of 904 nm gallium arsenide low level laser therapy in the management of chronic myofascial pain in the neck: a double-blind and randomize-controlled trial. Lasers Surg Med. 2004;35:229–35. doi: 10.1002/lsm.20082. [DOI] [PubMed] [Google Scholar]
- Hashimoto K, Kemmotsu O, Otsuka H, Numazawa R, Ohta Y. Efficacy of laser irradiation on the area near the stellate ganglion is dose-dependent: a double-blind crossover placebo-controlled study. Laser Therapy. 1997;7:5. [Google Scholar]
- Hawkins D, Abrahamse H. Effect of multiple exposures of low-level laser therapy on the cellular responses of wounded human skin fibroblasts. Photomed Laser Surg. 2006a;24:705–14. doi: 10.1089/pho.2006.24.705. [DOI] [PubMed] [Google Scholar]
- Hawkins DH, Abrahamse H. The role of laser fluence in cell viability, proliferation, and membrane integrity of wounded human skin fibroblasts following helium-neon laser irradiation. Lasers Surg Med. 2006b;38:74–83. doi: 10.1002/lsm.20271. [DOI] [PubMed] [Google Scholar]
- Hopkins JT, McLoda TA, Seegmiller JG, David Baxter G. Low-level laser therapy facilitates superficial wound healing in humans: a triple-blind, sham-controlled study. J Athl Train. 2004;39:223–229. [PMC free article] [PubMed] [Google Scholar]
- Huang SS, Zheng RL. Biphasic regulation of angiogenesis by reactive oxygen species. Pharmazie. 2006;61:223–9. [PubMed] [Google Scholar]
- Imlay JA. Cellular defenses against superoxide and hydrogen peroxide. Annu Rev Biochem. 2008;77:755–76. doi: 10.1146/annurev.biochem.77.061606.161055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karu T. Laser biostimulation: a photobiological phenomenon. J Photochem Photobiol B. 1989;3:638–40. doi: 10.1016/1011-1344(89)80088-0. [DOI] [PubMed] [Google Scholar]
- Karu T. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B. 1999;49:1–17. doi: 10.1016/S1011-1344(98)00219-X. [DOI] [PubMed] [Google Scholar]
- Karu TI, Afanas'eva NI. Cytochrome c oxidase as the primary photoacceptor upon laser exposure of cultured cells to visible and near IR-range light. Dokl Akad Nauk. 1995;342:693–5. [PubMed] [Google Scholar]
- Karu TI, Kolyakov SF. Exact action spectra for cellular responses relevant to phototherapy. Photomed Laser Surg. 2005;23:355–61. doi: 10.1089/pho.2005.23.355. [DOI] [PubMed] [Google Scholar]
- Karu TI, Pyatibrat LV, Ryabykh TP. Nonmonotonic behavior of the dose dependence of the radiation effect on cells in vitro exposed to pulsed laser radiation at lambda = 820 nm. Lasers Surg Med. 1997;21:485–92. doi: 10.1002/(sici)1096-9101(1997)21:5<485::aid-lsm11>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- Klotz LO, Kroncke KD, Sies H. Singlet oxygen-induced signaling effects in mammalian cells. Photochem Photobiol Sci. 2003;2:88–94. doi: 10.1039/b210750c. [DOI] [PubMed] [Google Scholar]
- Kreisler M, Christoffers AB, Willershausen B, d'Hoedt B. Effect of low-level GaAlAs laser irradiation on the proliferation rate of human periodontal ligament fibroblasts: an in vitro study. J Clin Periodontol. 2003;30:353–8. doi: 10.1034/j.1600-051x.2003.00001.x. [DOI] [PubMed] [Google Scholar]
- Lampl Y, Zivin JA, Fisher M, Lew R, Welin L, Dahlof B, Borenstein P, Andersson B, Perez J, Caparo C, Ilic S, Oron U. Infrared Laser Therapy for Ischemic Stroke: A New Treatment Strategy. Results of the NeuroThera Effectiveness and Safety Trial-1 (NEST-1) Stroke. 2007 doi: 10.1161/STROKEAHA.106.478230. [DOI] [PubMed] [Google Scholar]
- Lane N. Cell biology: power games. Nature. 2006;443:901–3. doi: 10.1038/443901a. [DOI] [PubMed] [Google Scholar]
- Lane P, Gross SS. Cell signaling by nitric oxide. Semin Nephrol. 1999;19:215–29. [PubMed] [Google Scholar]
- Lanzafame RJ, Stadler I, Kurtz AF, Connelly R, Peter TA, Sr, Brondon P, Olson D. Reciprocity of exposure time and irradiance on energy density during photoradiation on wound healing in a murine pressure ulcer model. Lasers Surg Med. 2007;39:534–42. doi: 10.1002/lsm.20519. [DOI] [PubMed] [Google Scholar]
- Lapchak PA, Han MK, Salgado KF, Streeter J, Zivin JA. Safety profile of transcranial near-infrared laser therapy administered in combination with thrombolytic therapy to embolized rabbits. Stroke. 2008;39:3073–8. doi: 10.1161/STROKEAHA.108.516393. [DOI] [PubMed] [Google Scholar]
- Lavi R, Shainberg A, Friedmann H, Shneyvays V, Rickover O, Eichler M, Kaplan D, Lubart R. Low energy visible light induces reactive oxygen species generation and stimulates an increase of intracellular calcium concentration in cardiac cells. J Biol Chem. 2003;278:40917–22. doi: 10.1074/jbc.M303034200. [DOI] [PubMed] [Google Scholar]
- Leal Junior EC, Lopes-Martins RA, Baroni BM, De Marchi T, Taufer D, Manfro DS, Rech M, Danna V, Grosselli D, Generosi RA, Marcos RL, Ramos L, Bjordal JM. Effect of 830 nm low-level laser therapy applied before high-intensity exercises on skeletal muscle recovery in athletes. Lasers Med Sci. 2008a doi: 10.1007/s10103-008-0633-4. [DOI] [PubMed] [Google Scholar]
- Leal Junior EC, Lopes-Martins RA, Vanin AA, Baroni BM, Grosselli D, De Marchi T, Iversen VV, Bjordal JM. Effect of 830 nm low-level laser therapy in exercise-induced skeletal muscle fatigue in humans. Lasers Med Sci. 2008b doi: 10.1007/s10103-008-0592-9. [DOI] [PubMed] [Google Scholar]
- Loevschall H, Arenholt-Bindslev D. Effect of low level diode laser irradiation of human oral mucosa fibroblasts in vitro. Lasers Surg Med. 1994;14:347–54. doi: 10.1002/lsm.1900140407. [DOI] [PubMed] [Google Scholar]
- Lopes-Martins RA, Albertini R, Martins PS, Bjordal JM, Faria Neto HC. Spontaneous effects of low-level laser therapy (650 nm) in acute inflammatory mouse pleurisy induced by Carrageenan. Photomed Laser Surg. 2005;23:377–81. doi: 10.1089/pho.2005.23.377. [DOI] [PubMed] [Google Scholar]
- Lubart R, Eichler M, Lavi R, Friedman H, Shainberg A. Low-energy laser irradiation promotes cellular redox activity. Photomed Laser Surg. 2005;23:3–9. doi: 10.1089/pho.2005.23.3. [DOI] [PubMed] [Google Scholar]
- Lubart R, Lavi R, Friedmann H, Rochkind S. Photochemistry and photobiology of light absorption by living cells. Photomed Laser Surg. 2006;24:179–85. doi: 10.1089/pho.2006.24.179. [DOI] [PubMed] [Google Scholar]
- Lubart R, Wollman Y, Friedmann H, Rochkind S, Laulicht I. Effects of visible and near-infrared lasers on cell cultures. J Photochem Photobiol B. 1992;12:305–10. doi: 10.1016/1011-1344(92)85032-p. [DOI] [PubMed] [Google Scholar]
- Martius F. Das Amdt-Schulz Grandgesetz. Munch Med Wschr. 1923;70:1005–1006. [Google Scholar]
- Mester E, Nagylucskay S, Waidelich W, Tisza S, Greguss P, Haina D, Mester A. Effects of direct laser radiation on human lymphocytes. Arch Dermatol Res. 1978;263:241–5. doi: 10.1007/BF00446940. [DOI] [PubMed] [Google Scholar]
- Mester E, Szende B, Tota J.G. Effect of laser on hair growth of mice. Kiserl Orvostud. 1967;19:628–631. [Google Scholar]
- Mitka M. 1998 NObel Prize winners are announced: three discoverers of nitric oxide activity. Jama. 1998;280:1648. [PubMed] [Google Scholar]
- Moore P, Ridgway TD, Higbee RG, Howard EW, Lucroy MD. Effect of wavelength on low-intensity laser irradiation-stimulated cell proliferation in vitro. Lasers Surg Med. 2005;36:8–12. doi: 10.1002/lsm.20117. [DOI] [PubMed] [Google Scholar]
- Morrone G, Guzzardella GA, Torricelli P, Rocca M, Tigani D, Brodano GB, Fini M, Giardino R. Osteochondral lesion repair of the knee in the rabbit after low-power diode Ga-Al-As laser biostimulation: an experimental study. Artif Cells Blood Substit Immobil Biotechnol. 2000;28:321–36. doi: 10.3109/10731190009119362. [DOI] [PubMed] [Google Scholar]
- Oron A, Oron U, Streeter J, de Taboada L, Alexandrovich A, Trembovler V, Shohami E. low-level laser therapy applied transcranially to mice following traumatic brain injury significantly reduces long-term neurological deficits. J Neurotrauma. 2007;24:651–6. doi: 10.1089/neu.2006.0198. [DOI] [PubMed] [Google Scholar]
- Oron U, Yaakobi T, Oron A, Hayam G, Gepstein L, Rubin O, Wolf T, Ben Haim S. Attenuation of infarct size in rats and dogs after myocardial infarction by low-energy laser irradiation. Lasers Surg Med. 2001a;28:204–11. doi: 10.1002/lsm.1039. [DOI] [PubMed] [Google Scholar]
- Oron U, Yaakobi T, Oron A, Mordechovitz D, Shofti R, Hayam G, Dror U, Gepstein L, Wolf T, Haudenschild C, Haim SB. Low-energy laser irradiation reduces formation of scar tissue after myocardial infarction in rats and dogs. Circulation. 2001b;103:296–301. doi: 10.1161/01.cir.103.2.296. [DOI] [PubMed] [Google Scholar]
- Ozcelik O, Cenk Haytac M, Kunin A, Seydaoglu G. Improved wound healing by low-level laser irradiation after gingivectomy operations: a controlled clinical pilot study. J Clin Periodontol. 2008;35:250–4. doi: 10.1111/j.1600-051X.2007.01194.x. [DOI] [PubMed] [Google Scholar]
- Ozdemir F, Birtane M, Kokino S. The clinical efficacy of low-power laser therapy on pain and function in cervical osteoarthritis. Clin Rheumatol. 2001;20:181–4. doi: 10.1007/s100670170061. [DOI] [PubMed] [Google Scholar]
- Pal G, Dutta A, Mitra K, Grace MS, Romanczyk TB, Wu X, Chakrabarti K, Anders J, Gorman E, Waynant RW, Tata DB. Effect of low intensity laser interaction with human skin fibroblast cells using fiber-optic nano-probes. J Photochem Photobiol B. 2007;86:252–61. doi: 10.1016/j.jphotobiol.2006.12.001. [DOI] [PubMed] [Google Scholar]
- Passarella S, Casamassima E, Molinari S, Pastore D, Quagliariello E, Catalano IM, Cingolani A. Increase of proton electrochemical potential and ATP synthesis in rat liver mitochondria irradiated in vitro by helium-neon laser. FEBS Lett. 1984;175:95–9. doi: 10.1016/0014-5793(84)80577-3. [DOI] [PubMed] [Google Scholar]
- Pryor WA, Houk KN, Foote CS, Fukuto JM, Ignarro LJ, Squadrito GL, Davies KJ. Free radical biology and medicine: it's a gas, man! Am J Physiol Regul Integr Comp Physiol. 2006;291:R491–511. doi: 10.1152/ajpregu.00614.2005. [DOI] [PubMed] [Google Scholar]
- Rochkind S, Leider-Trejo L, Nissan M, Shamir MH, Kharenko O, Alon M. Efficacy of 780-nm laser phototherapy on peripheral nerve regeneration after neurotube reconstruction procedure (double-blind randomized study) Photomed Laser Surg. 2007;25:137–43. doi: 10.1089/pho.2007.2076. [DOI] [PubMed] [Google Scholar]
- Schreck R, Albermann K, Baeuerle PA. Nuclear factor kappa B: an oxidative stress-responsive transcription factor of eukaryotic cells (a review) Free Radic Res Commun. 1992;17:221–37. doi: 10.3109/10715769209079515. [DOI] [PubMed] [Google Scholar]
- Schubert MM, Eduardo FP, Guthrie KA, Franquin JC, Bensadoun RJ, Migliorati CA, Lloid CM, Eduardo CP, Walter NF, Marques MM, Hamdi M. A phase III randomized double-blind placebo-controlled clinical trial to determine the efficacy of low level laser therapy for the prevention of oral mucositis in patients undergoing hematopoietic cell transplantation. Support Care Cancer. 2007;15:1145–54. doi: 10.1007/s00520-007-0238-7. [DOI] [PubMed] [Google Scholar]
- Schulz H. Uber die Theorie der Arzneimittelwirkung. Virchows Archiv. 1877;108:423–434. [Google Scholar]
- Schulz H. Uber Hefegiste. Pflügers Archiv Gesammte Physiologie. 1888;42:517–541. [Google Scholar]
- Shao XH, Yang YP, Dai J, Wu JF, Bo AH. Effects of He-Ne laser irradiation on chronic atrophic gastritis in rats. World J Gastroenterol. 2005;11:3958–61. doi: 10.3748/wjg.v11.i25.3958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shefer G, Partridge TA, Heslop L, Gross JG, Oron U, Halevy O. Low-energy laser irradiation promotes the survival and cell cycle entry of skeletal muscle satellite cells. J Cell Sci. 2002;115:1461–9. doi: 10.1242/jcs.115.7.1461. [DOI] [PubMed] [Google Scholar]
- Shiva S, Gladwin MT. Shining a light on tissue NO stores: near infrared release of NO from nitrite and nitrosylated hemes. J Mol Cell Cardiol. 2009;46:1–3. doi: 10.1016/j.yjmcc.2008.10.005. [DOI] [PubMed] [Google Scholar]
- Sommer AP, Pinheiro AL, Mester AR, Franke RP, Whelan HT. Biostimulatory windows in low-intensity laser activation: lasers, scanners, and NASA's light-emitting diode array system. J Clin Laser Med Surg. 2001;19:29–33. doi: 10.1089/104454701750066910. [DOI] [PubMed] [Google Scholar]
- Stadler I, Evans R, Kolb B, Naim JO, Narayan V, Buehner N, Lanzafame RJ. In vitro effects of low-level laser irradiation at 660 nm on peripheral blood lymphocytes. Lasers Surg Med. 2000;27:255–61. doi: 10.1002/1096-9101(2000)27:3<255::aid-lsm7>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Stebbing AR. Hormesis; the stimulation of growth by low levels of inhibitors. Sci Tot Environ. 1982;22:213–234. doi: 10.1016/0048-9697(82)90066-3. [DOI] [PubMed] [Google Scholar]
- Stelian J, Gil I, Habot B, Rosenthal M, Abramovici I, Kutok N, Khahil A. Improvement of pain and disability in elderly patients with degenerative osteoarthritis of the knee treated with narrow-band light therapy. J Am Geriatr Soc. 1992;40:23–6. doi: 10.1111/j.1532-5415.1992.tb01824.x. [DOI] [PubMed] [Google Scholar]
- Stergioulas A, Stergioula M, Aarskog R, Lopes-Martins RA, Bjordal JM. Effects of low-level laser therapy and eccentric exercises in the treatment of recreational athletes with chronic achilles tendinopathy. Am J Sports Med. 2008;36:881–7. doi: 10.1177/0363546507312165. [DOI] [PubMed] [Google Scholar]
- Storz P. Mitochondrial ROS--radical detoxification, mediated by protein kinase D. Trends Cell Biol. 2007;17:13–8. doi: 10.1016/j.tcb.2006.11.003. [DOI] [PubMed] [Google Scholar]
- Sutherland JC. Biological effects of polychromatic light. Photochem Photobiol. 2002;76:164–70. doi: 10.1562/0031-8655(2002)076<0164:beopl>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Tafur J, Mills PJ. Low-intensity light therapy: exploring the role of redox mechanisms. Photomed Laser Surg. 2008;26:323–8. doi: 10.1089/pho.2007.2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend JF, Luckey TD. Hormoligosis in pharmacology. J Am Med Assoc. 1960;173:44–48. doi: 10.1001/jama.1960.73020190007010. [DOI] [PubMed] [Google Scholar]
- Tumilty S, Munn J, McDonough S, Hurley DA, Basford JR, Baxter GD. Low Level Laser Treatment of Tendinopathy: A Systematic Review with Meta-analysis. Photomed Laser Surg. 2009 doi: 10.1089/pho.2008.2470. Ahead of print. [DOI] [PubMed] [Google Scholar]
- Vasseljen O, Jr, Hoeg N, Kjeldstad B, Johnsson A, Larsen S. Low level laser versus placebo in the treatment of tennis elbow. Scand J Rehabil Med. 1992;24:37–42. [PubMed] [Google Scholar]
- Watson MR, Wallace K, Gieling RG, Manas DM, Jaffray E, Hay RT, Mann DA, Oakley F. NF-kappaB is a critical regulator of the survival of rodent and human hepatic myofibroblasts. J Hepatol. 2008;48:589–97. doi: 10.1016/j.jhep.2007.12.019. [DOI] [PubMed] [Google Scholar]
- Weber JB, Pinheiro AL, de Oliveira MG, Oliveira FA, Ramalho LM. Laser therapy improves healing of bone defects submitted to autologous bone graft. Photomed Laser Surg. 2006;24:38–44. doi: 10.1089/pho.2006.24.38. [DOI] [PubMed] [Google Scholar]
- Wu S, Xing D, Gao X, Chen WR. High fluence low-power laser irradiation induces mitochondrial permeability transition mediated by reactive oxygen species. J Cell Physiol. 2009;218:603–11. doi: 10.1002/jcp.21636. [DOI] [PubMed] [Google Scholar]
- Yaakobi T, Shoshany Y, Levkovitz S, Rubin O, Ben Haim SA, Oron U. Long-term effect of low energy laser irradiation on infarction and reperfusion injury in the rat heart. J Appl Physiol. 2001;90:2411–9. doi: 10.1152/jappl.2001.90.6.2411. [DOI] [PubMed] [Google Scholar]
- Yamaura M, Yao M, Yaroslavsky I, Cohen R, Smotrich M, Kochevar IE. Low level light effects on inflammatory cytokine production by rheumatoid arthritis synoviocytes. Lasers Surg Med. 2009;41:282–90. doi: 10.1002/lsm.20766. [DOI] [PubMed] [Google Scholar]
- Yu W, Naim JO, Lanzafame RJ. The effect of laser irradiation on the release of bFGF from 3T3 fibroblasts. Photochem Photobiol. 1994;59:167–70. doi: 10.1111/j.1751-1097.1994.tb05017.x. [DOI] [PubMed] [Google Scholar]
- Yu W, Naim JO, Lanzafame RJ. Effects of photostimulation on wound healing in diabetic mice. Lasers Surg Med. 1997;20:56–63. doi: 10.1002/(sici)1096-9101(1997)20:1<56::aid-lsm9>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Zhang J, Xing D, Gao X. Low-power laser irradiation activates Src tyrosine kinase through reactive oxygen species-mediated signaling pathway. J Cell Physiol. 2008;217:518–28. doi: 10.1002/jcp.21529. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Song S, Fong CC, Tsang CH, Yang Z, Yang M. cDNA microarray analysis of gene expression profiles in human fibroblast cells irradiated with red light. J Invest Dermatol. 2003;120:849–57. doi: 10.1046/j.1523-1747.2003.12133.x. [DOI] [PubMed] [Google Scholar]
- Zivin JA, Albers GW, Bornstein N, Chippendale T, Dahlof B, Devlin T, Fisher M, Hacke W, Holt W, Ilic S, Kasner S, Lew R, Nash M, Perez J, Rymer M, Schellinger P, Schneider D, Schwab S, Veltkamp R, Walker M, Streeter J. Effectiveness and safety of transcranial laser therapy for acute ischemic stroke. Stroke. 2009;40:1359–64. doi: 10.1161/STROKEAHA.109.547547. [DOI] [PubMed] [Google Scholar]