Abstract
African Americans with high blood pressure (BP) can benefit greatly from therapeutic lifestyle changes (TLC) such as diet modification, physical activity, and weight management. However, they and their health care providers face many barriers in modifying health behaviors. A multidisciplinary panel synthesized the scientific data on TLC in African Americans for efficacy in improving BP control, barriers to behavioral change, and strategies to overcome those barriers. Therapeutic lifestyle change interventions should emphasize patient self-management, supported by providers, family, and the community. Interventions should be tailored to an individual’s cultural heritage, beliefs, and behavioral norms. Simultaneously targeting multiple factors that impede BP control will maximize the likelihood of success. The panel cited limited progress with integrating the Dietary Approaches to Stop Hypertension (DASH) eating plan into the African American diet as an example of the need for more strategically developed interventions. Culturally sensitive instruments to assess impact will help guide improved provision of TLC in special populations. The challenge of improving BP control in African Americans and delivery of hypertension care requires changes at the health system and public policy levels. At the patient level, culturally sensitive interventions that apply the strategies described and optimize community involvement will advance TLC in African Americans with high BP.
Keywords: hypertension, African Americans, therapeutic lifestyle change, behavioral modification, cultural competence, diet
Introduction
Hypertension remains a leading cause of health disparity in African Americans. Based on National Health and Nutrition Examination Survey (NHANES) data from 2003 and 2004, blood pressure (BP) control (< 140/90 mm Hg for individuals without diabetes and < 130/80 mm Hg for those with diabetes) was achieved in only 29% of African Americans with hypertension.1 The low rate is difficult to explain considering the degree of hypertension awareness (66%) and treatment (55%) in African Americans and demonstrates a continued and urgent need for targeting effective antihypertensive therapy and patient adherence.
The International Society on Hypertension in Blacks (ISHIB) and Seventh Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure have recommended therapeutic lifestyle changes (TLC) to lower BP, enhance antihypertensive drug efficacy, and reduce cardiovascular risk.2,3 Therapeutic lifestyle changes include diet modification, physical activity, weight management, limiting alcohol consumption, and no tobacco use (Table 1).2,4–6 However, evidence suggests that patients experience difficulty with incorporating these changes in their daily lives.7 Health care providers also have reported difficulty prescribing TLC as an intervention to improve hypertension management.8 Recognizing the urgency of addressing these difficulties, the ISHIB developed an agenda to overcome them, with particular attention to special issues for African Americans.
Table 1.
Recommended Therapeutic Lifestyle Changes for Treatment of High Blood Pressure2
| Goal | Realistic Personal Plan to Achieve Goal |
|---|---|
| Normal weight for height |
|
| Dietary goals: |
|
| Low fat |
|
| Low sodium |
|
| High potassium |
|
| Adequate calcium |
|
| Limit alcohol |
|
| Physical fitness |
|
| No tobacco use |
|
The ISHIB convened a panel of clinicians and researchers on February 22 and 23, 2008, to develop recommendations for addressing hypertension-related health disparities by promoting better hypertension management in African Americans. The panel comprised individuals from academia, community groups, nursing, internal medicine, cardiology, and managed care. This multidisciplinary panel was asked to synthesize current scientific information regarding lifestyle changes in hypertension management and identify strategies to assist health care providers in incorporating TLC into the management plan of African Americans with high BP.
To address these goals, the panelists began by assembling and reviewing the evidence base regarding: 1) the efficacy of TLC interventions in published studies; 2) factors that impede adoption or maintenance of TLC; and 3) strategies to overcome such barriers. The panel then discussed the application of these strategies to the modification of diet, a TLC that is effective in African Americans with high BP. The panel considered the importance of assessing the impact of interventions to promote TLC, particularly in using culturally sensitive measures. Finally, the panel addressed translating research recommendations to clinical practice. This article summarizes panel findings regarding each of these topics.
Efficacy of TLC Interventions
To assess the likely efficacy of TLC for African Americans, the panel analyzed in greater detail the findings of a systematic review, focusing on interventions to improve cardiovascular care in ethnic communities. Conducted by Davis et al,9 the systematic review identified studies from 1995 to 2006 that: 1) either included a sample of at least 50% ethnic subjects or described subgroup data and 2) were connected with a health care organization. Studies involving collaboration with churches, schools, or other community organizations were excluded unless there was formal medical collaboration. The panel excluded studies without African American subjects and only included studies in which intervention focused on a modification in patient lifestyle. A total of 20 studies from the Davis et al compilation were relevant.10–31
These studies had many methodological differences, including the target sample, the type and length of intervention, personnel delivering the intervention, and target outcome. Some interventions targeted patients directly, whereas others targeted their health care providers. Sample sizes ranged from 26 to 2860 subjects.12,20 The type of intervention ranged from dietary/nutritional counseling to home- or community-based BP monitoring to physical exercise to stress reduction. Interventions in at least 9 studies targeted more than one type of lifestyle change (eg, diet plus exercise).11,13–18,28,29 At least 10 studies contained a dietary intervention.10,11,16–18,22,26–29 The length of the intervention ranged from 3 to 40 months.12,23 The study duration was ≤ 6 months in 7 studies11,12,,14,24,26,28,31 and ≤ 12 months in 15 studies.11–17,20–22,24–26,28,31 Some studies consisted of nurse-led interventions, whereas others involved pharmacists or community health workers.
Of the 20 studies, 19 specifically assessed the impact of TLC interventions on lowering BP or achieving BP targets (excluding Redder et al15). Ten of 14 studies reported BP reductions with TLC11,12,14,16,18,20,23–26 and 6 reported reductions in systolic BP values.11,12,14,16,18,23 Four of 6 studies reported improved BP control in patients carrying out TLC.10,13,20,23 of 10 studies with dietary interventions, 6 showed favorable BP outcomes.10,11,16,18,26,28
This evidence supports TLC—implemented in a variety of behavioral interventions—as an indispensable part of hypertension management. Both the ISHIB and Joint National Committee statements are being updated to reflect more recent data. Therapeutic lifestyle changes will continue to be recommended in the prevention of hypertension and as an adjunct to pharmacotherapy in patients at high cardiovascular risk. The panel noted that the same strategies for affecting TLC can be applied to improving medication adherence.
Barriers to Lifestyle Change
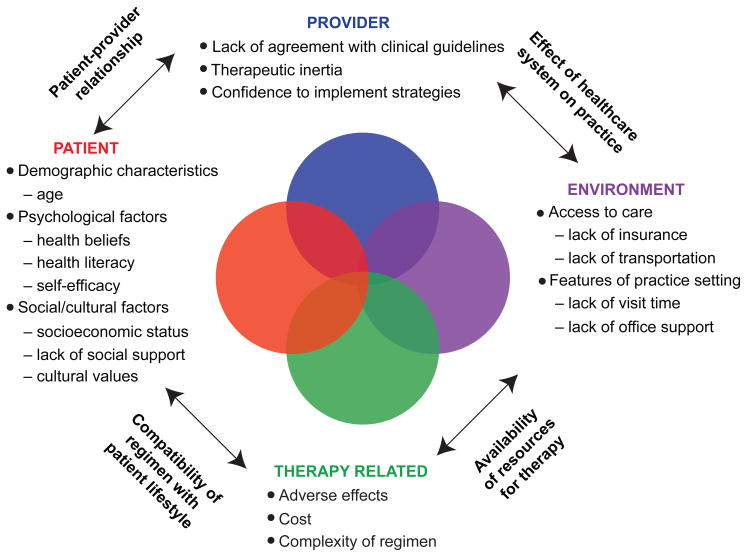
The panel considered a wide range of barriers to the adoption of TLC aimed at improving BP control.32,33 Factors were grouped into categories focusing on the patient, provider, therapy, medical/physical environment, and relationships between these categories (Figure 1).
Figure 1.
Barriers to behavior change.
Main Categories of Factors
Patient Factors
Various demographic, psychological, and social/cultural factors influence the extent to which patients incorporate TLC into their daily lives. For example, individuals can have perceptions of low self-efficacy, in which they lack confidence in their ability to carry out the behavior necessary to attain a desired goal.32 Cultural values and practices can impede lifestyle change (eg, not heeding nutritional recommendations that depart from traditional diets or require food preparation separate from that for other family members).34
Some African Americans may not trust the entire health care system and harbor suspicions of being a participant in an experiment.35,36 Patients may respond to health messages positively or negatively depending on how the message source (eg, government agency, medical center) is viewed.37,38
Provider Factors
Providers may lack awareness of some components of guidelines for hypertension management. They may also not agree with all guidelines. As a result, they may fail to initiate or intensify treatment appropriately when an abnormal parameter is recorded or the goal is unmet—a factor called “therapeutic inertia.”33,39
Confidence is as important for providers as for patients. In a survey of community health center-based providers, including registered nurses and physicians, TLC was considered more challenging to implement than adherence to a drug regimen, and few providers were confident of their own ability to change patient behavior.8 This lack of confidence is likely to impact providers’ treatment of hypertension.
Environmental Factors
Access to care can be limited by a person’s lack of insurance and by transportation problems in getting to the doctor’s office. Various features of the practice setting can reduce the likelihood of successful TLC, including insufficient lifestyle counseling during a physician visit or absence of appropriate office support to help with counseling.
Therapy-Related Factors
A complex drug regimen requiring multiple daily dosing can reduce adherence, particularly in the elderly. Similarly, the number and complexity of therapy-related factors associated with TLC (eg, extent of dietary change and addressing smoking, diet, and exercise simultaneously) can reduce adherence. Adverse effects such as sports injuries can limit adherence to an exercise regimen. Cost can clearly affect food choices.
Relationships Between Categories
Barriers can arise based on mismatches in the relationships between the categories listed previously. The relationship between patient and provider is particularly important.
Patient-Provider Relationship
How providers view their relationship with the patient will influence their approach to sharing information and responding to needs articulated by the patient.33 Obstacles may arise when patients are not involved in management decisions. When patients feel encouraged to ask questions and discuss their problems, which may have nothing to do with hypertension, positive outcomes, including BP lowering, have been reported.19,40
Respect—“the single most powerful ingredient in nourishing relationships”41—can mean the absence of condescension when someone does not speak standard English or the acknowledgment of different cultural norms. Patients may perceive (correctly or not) a lack of respect when a provider is not “actively” listening when they speak or appears dismissive of their customs or beliefs.36 When a provider does not communicate in a manner prescribed by a patient’s culture, the patient may not conform to social expectations.42
Providers should recognize that African Americans are a heterogeneous population. Many cultures are represented, such as those of many Caribbean nations, different African immigrant cultures, and regional cultures in the United States. Cultural differences also exist based on sociodemographic status. Not all African Americans eat the same foods or prepare them in the same way. Providers should elicit information to assess the specific barriers prevailing in each individual case.
The Health Care System and Provider Practices
The provider’s ability to provide care may be hindered or facilitated by the larger health care system. For example, inadequate reimbursement for patient counseling services limits time and resources for TLC. Newer electronic medical record and other informational support systems can help providers to quickly observe trends in patient progress, identify high-priority care activities for a particular visit, and produce copies of informational materials to support specified TLC recommendations.
Availability of Resources for Therapy
Recommendations for TLC often assume that patients have access to the relevant resources. However, patients cannot follow dietary recommendations if neighborhood stores do not offer fresh fruits and vegetables. Similarly, patients cannot heed advice to engage in physical exercise if there are no safe areas for exercise.
Compatibility of Therapy with Patient Lifestyle
A patient’s lifestyle can affect the ability or willingness to make TLC. Patients who have a busy schedule may eat often at fast-food restaurants where low-fat, balanced meals are less readily available. Preparing special meals for one member of the family can be more difficult and costly. Quitting smoking is more difficult when the people whom the patient spends time with are smokers.
Broader Relationships
The provision of care for hypertension must be redesigned. The decentralized US health care system is largely organized and financed using an acute care model that assumes providers are the primary managers of care and deliver care in episodes lasting a short period of time. This model produces many misalignments and barriers to care for chronic conditions such as hypertension. The provision of care for chronic conditions requires a rethinking of the training of health care personnel, responsibilities of office personnel, organization of office records, and adequate payment for services. More broadly, the organization of the larger health system for chronic care must be addressed, including affordable health insurance. These larger issues for African Americans with hypertension warrant further consideration but in another forum.
Strategies to Overcome Barriers
When considering African American patients, the panel identified 3 broad strategies toward overcoming barriers to TLC in hypertension management: 1) empowering patients, 2) enhancing cultural competence of providers, and 3) targeting multiple factors. The panel also identified other useful strategies.
Empowering Patients
A key requirement of TLC for chronic conditions such as hypertension is that patients must be empowered and motivated to take an active role in their care and ownership of patient-centered management plans. Two examples of models with comprehensive frameworks that address individual behavior change within a larger systems framework are the chronic care model and ecological model of health behavior. These models emphasize the role of patients with chronic conditions as being their own principal caregiver and the importance of provider, family, and community support in self-management (Table 2).43–46 The chronic care model is an integral part of patient-centered medical home models.47,48
Table 2.
Underlying Concepts in Chronic Care and Ecological Models
| Chronic Care Model | Ecological Model of Health Behavior |
|---|---|
|
|
Providers are experts about the disease and patients are experts about their lives.
Responsibility remains with the provider who must inform, activate, and assist patients in self-management of their condition.
For example, is someone showing the person appropriate health behaviors? Is someone providing health information? The most important setting, where individuals spend the most time and which exerts the most emotional influence, consists of family and social networks.
Settings or levels of influence where individuals typically do not spend time, including workplace or community mandates and federal, state, and local health laws and health policies.
The chronic care model can inform TLC strategies because hypertension is a chronic disease often requiring: 1) multiple encounters with the health care organization, 2) an effective patient-provider relationship, 3) a commitment to TLC on the part of the individual and the provider, and 4) adjustments in the treatment plan to achieve optimal care and appropriate hypertension management. The chronic care model proposes a patient-provider relationship based on collaborative care and self-management education.43,49 Collaborative care refers to shared decision making. Of particular relevance is the component of self-management support, which provides patients with problem-solving skills (ie, recognizing issues and generating a plan to forge a solution).47
A review of publications since 2000 that cited the chronic care model did not find consistent evidence of benefit across all medical conditions.47 However, studies in diabetes did report a reduction in cardiovascular risk and longer-term (3-year) improvements in health outcome.50,51
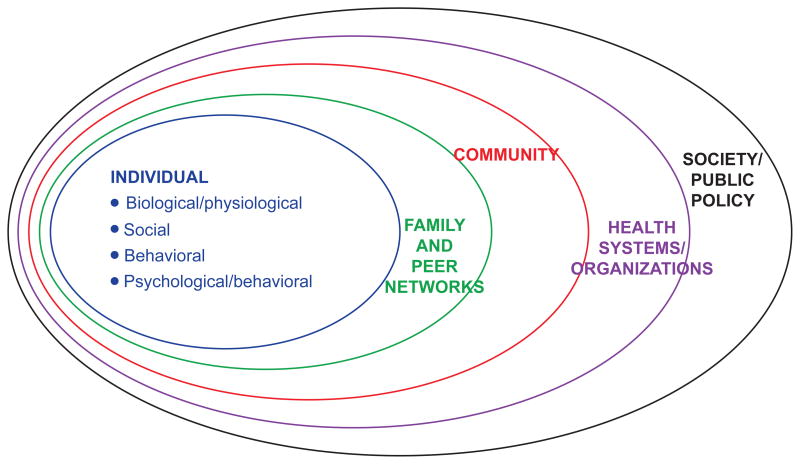
The ecological model, which has served as the basis for behavioral interventions such as the Well-Integrated Screening and Intervention for Women Across the Nation (WISEWOMAN) program,52 provides a framework for assessing the multiple factors that can influence TLC and hypertension management (Figure 2).44–46 The ecological model places the patient—the primary focus of TLC—in the center of the model and acknowledges that other factors (eg, family and peer networks, health systems/organizations, community, and social/public policy) have a compounding influence on the patient’s ability to successfully engage in TLC.
Figure 2.
Ecological model of health behavior in hypertension.
Therapeutic lifestyle change interventions should foster self-efficacy. In addition, by redirecting patients from an external to an internal locus of control, patients can empower themselves to rethink goals that can contribute to a healthier lifestyle, as can be exemplified by thoughts such as “It’s all in me,” “I have it in me to change who I am,” and “I will eat healthy and find the time to exercise.”
Cultural Competence of Providers
A patient’s health beliefs and health-related behaviors are grounded, at least in part, in his or her culture’s values and norms. Cultural competence is a dynamic, continuous process by which an individual provider, health care system, or health care agency finds meaningful and useful care delivery strategies based on knowledge of the cultural heritage, beliefs, attitudes, and behaviors of those receiving care.53 A culturally competent practitioner recognizes that the patient’s genetics/biology, behaviors, and environment interact synergistically.53
Many cultures are represented among the African American population. Therapeutic lifestyle change interventions to improve BP control are more likely to be accepted if the intervention can be adapted to the norms of the specific culture and community of which the patient is a part and the health decision-making in that culture. Competency can involve asking questions (to determine cultural beliefs or practices that may influence health behavior), listening closely, and using information about the patient to tailor an intervention to local context (Table 3).54
Table 3.
Suggestions for Enhancing Cultural Competency Among Health Care Providers
|
Adapted from Program for Multicultural Health, University of Michigan Health System. Suggested Content for Enhancing Cultural Competency Among Health Care Providers.54 Reprinted with permission from the University of Michigan Program for Multicultural Health.
Community input is invaluable toward overcoming many cultural barriers. Communication channels differ from locality to locality and cannot be predicted from outside the community.37 Community involvement can help dispel mistrust that many African Americans feel toward the health care system.36,37 A patient’s adherence to therapy, both pharmacologic and nonpharmacologic, may depend on the involvement of family members or community leaders. These individuals may serve as sources of health information and may support an individual’s decisions on health issues.42 Early community involvement can enhance patient acceptance and outcomes of an intervention. The broadening field of community participatory research offers insights on involving community partners and using community resources. Table 4 presents examples of culturally sensitive approaches toward promoting positive behavioral change.55
Table 4.
Examples of Culturally Sensitive Approach to Health Promotion
| Purpose | Process |
|---|---|
| To develop a computer-based nutrition education program for African American adults | Program content was based on a curriculum developed at 6 HBCUs. The program was designed to help families select and prepare meals consistent with their cultural traditions.55 |
| To implement the program | The developer (faculty and students at one of the HBCUs) presented the program at community churches, meeting “with ministers of selected churches to introduce themselves, explain the project, request permission to use the church as a test site, and recruit participants from the membership. Approval to use the targeted churches was granted by all 4 ministers. The team was then referred to individuals who held leadership positions or coordinated various church organizations. The designated individuals were contacted and their support and assistance was solicited.”55 |
| To identify where health messages need to be placed to reach African Americans in a specific locality | A media survey revealed the radio to be the primary source of information for African Americans in South Los Angeles, followed by ethnic newspapers and then local television and cable. The fourth most common source was magazines like Ebony, Essence, and Jet. For persons 18–25 years old, the primary sources were social media (eg, MySpace) and information received by cell phone.a |
Abbreviation: HBCUs, Historically Black Colleges and Universities.
Loretta Jones, oral communications, April 7, 2009, regarding narrowcasting media survey conducted from February to June 2007 in South Los Angeles by Voices Inc., Los Angeles, CA, and focus groups conducted from June to July 2008 on sources of voting information.
Adapted from Goodman and Blake.55
Increasing the cultural competence of providers should help to reduce health disparities among ethnic populations and lead to improved quality of care.56 Cultural competency training is mandated for medical licensure in New Jersey.57 Recommendations for culturally competent health care are available for many health care professionals, including nurses, diabetes educators, and pharmacists.41,58 Online cross-cultural training and resources are offered by government agencies and academic centers.54,59
Targeting Multiple Factors
Effective TLC interventions often consist of multiple components that target more than one factor with more than one approach.32,60 Barriers can differ from person to person. Multiple modalities may be needed to address a complex of interacting factors (Table 5).61 What constitutes an effective intervention may change over time. A “multilevel” approach also enables customization or tailoring of interventions to address the specific barriers present in any one individual.
Table 5.
Example of Interventions Addressing Multiple Behavioral Factors Related to Hypertension Control
| Health Behavior Issue | Specific Interventions |
|---|---|
| Hypertension knowledge/risk perception |
|
| Memory |
|
| Social/medical environment |
|
| Patient–provider relationship |
|
| Adverse effects of antihypertensive medication |
|
| Health behaviors |
|
| Diet |
|
| Exercise |
|
| Smoking |
|
| Alcohol |
|
| Stress reduction |
|
Abbreviation: DASH, Dietary Approaches to Stop Hypertension.
Above are topics of 11 tailored behavioral modules triggered by provider assessment of poor blood pressure control.
Adapted from Bosworth et al.61
Additional Important Strategies
The panel noted that evidence supports incorporating the following strategies in efforts to implement TLC:
More than information. Interventions must go beyond conveying information. Focusing solely on conveying information, either for patients or providers, is unlikely to improve BP control.60,62
Teams. The value of teams comprising physicians and allied health professionals in patient education and behavioral interventions is supported by the success of nurse- or pharmacist-led initiatives.9,62
Incremental steps. A start by encouraging relatively small changes will create a respectful and welcoming atmosphere when counseling modifications in lifestyle. This approach builds trust and fosters a productive patient-provider relationship.
Example of Applying Strategies to Interventions: Dietary Approaches to Stop Hypertension Eating Plan
The panel discussed how some strategies identified previously may strengthen an intervention or program targeting African Americans with high BP. On the strong evidence of Dietary Approaches to Stop Hypertension (DASH), DASH-Sodium, PREMIER, and other studies, dietary changes promoting the DASH eating plan are highly recommended in African Americans with high BP. The DASH plan combined with other TLC significantly lowered BP compared with usual care.63 To capture this powerful effect, TLC interventions in African Americans should always include dietary recommendations that incorporate or integrate principles of DASH into individual diets.64
Based on NHANES data, however, eating meals in accordance with DASH recommendations has declined among adults with high BP (19.4% from 1999–2004 compared with 26.7% from 1988–1994), with an even lower DASH accordance reported among African Americans.65 More strategically developed interventions are needed to promote DASH principles. Fundamental components of interventions designed to promote dietary change in patients with diabetes also apply in the hypertension setting and consist of assessment of patient readiness to make changes, setting of appropriate goals, instilling self-efficacy, training in problem solving, and encouraging family and community support.66,67 To understand the importance of an intervention and set goals appropriately, the individual must receive a direct, clear, concise explanation of what is to be done. It is just as important that the information provided be specific and practical; nutrition education should cover recipe modification, grocery shopping, and concrete recommendations regarding foods to eat and foods to avoid.
When cultural dietary habits include foods and forms of preparation that discourage adoption of nutritional recommendations, providers should find ways to assist the individual to not only cook and consume foods that they value in their culture, but also do so in a healthy, heart-smart way. For example, a staple among some African Americans, particularly in the South, is collard greens cooked with ham hocks. The problem to target is not the collard greens, but rather the manner in which they are prepared. This dish can be prepared with skinless turkey wings or necks and seasoned with spices (eg, apple cider vinegar) that have low or no sodium content. Another goal is the increased consumption of dairy products among African Americans. While lactose maldigestion has limited dairy food consumption, culturally determined food preferences and dietary practices learned early in life also have contributed to reduced intake.68 Individuals with lactose intolerance can be shown how to tolerate a dairy-rich diet that meets calcium intake recommendations without adverse effects.63,68
Some progress has been made in presenting DASH recommendations in the context of soul food and other traditional diets in African American communities.55,69,70 A means of facilitating access to local experiences merits consideration so that effective adaptations can be shared with other communities.
Long-term changes in eating behavior remain elusive. Two approaches should be considered: individual and family training in problem-solving skills to strengthen behavioral self-management and creation of community-based resources for ongoing support. Problem solving with regard to food choices, reading of food labels, grocery shopping, and food preparation can be instilled by trained individuals in the community.
The creation of community-based resources (community advocates from church groups, community health centers, or other community sources) should be considered prospectively. Levine et al23 have demonstrated the valuable work of indigenous (ie, from the community) health workers in sustaining BP lowering over a 40-month trial. These paraprofessionals were trained by nurses in BP management, monitoring, education and counseling, and social support mobilization. Hess et al71 reported on the value of community-based BP monitoring and peer-based health messaging in a 14-month study involving barbershops. A consensus has not yet been developed as to a structured approach for creating and maintaining community support. However, the value of such support is not questioned.
Assessment of Impact
The panel advocated the inclusion of a metrics component for all TLC interventions and emphasized the selection of assessment instruments that are culturally sensitive and validated in the population. Data obtained by recording indicators before and after implementation can not only measure effectiveness of the intervention but also provide feedback to help patients and providers understand the utility of the intervention and offer reinforcement of progress.
Assessment methods may be qualitative or quantitative and focus on processes or outcomes. Outcome indicators need to be selected and measured reliably and validly to determine impact. They must be appropriate and sensitive to the changes generated by the intervention. The outcomes selected can be those that the intervention was designed to change as well as unintended, negative outcomes.
Measurement approaches and tools should be compatible with the characteristics of the target population for which they are used. This is of particular importance in hypertension management because of the high proportion of patients who are from minority groups, are elderly, and have comorbidities. Strickland et al72 reported that a large proportion of psychometric tools used in nursing research had not been adequately designed and tested for use in ethnic and racial minorities (Table 6).
Table 6.
Laying the Groundwork for Effective Reporting of Metrics
|
Adapted from Strickland et al.72
Many questionnaires and scales are not designed for use in the elderly or persons who are not well educated. Long and burdensome measurement tools may be too time consuming or impractical for use in clinical settings or with individuals who are ill or frail.73–75 The reliability and validity of outcome assessments can be compromised when assessment approaches are used in a patient population or setting for which they are not compatible, and inappropriate conclusions can be drawn from the data about the effectiveness of hypertension programs. An example of an assessment instrument that has been to be shown to be reliable and valid in African Americans76 is the 12-item version of the Medical Outcomes Study 36-item Short Form Health Survey (SF-36).77 This instrument is also less cumbersome than the original version in assessing mental and physical health status.
Timing of measurement is crucial. Baseline measures of the selected outcome should be obtained. Follow-up assessments should be conducted at appropriate intervals so that change in the outcome due to the intervention can be documented. Therefore, assessment tools need to be highly sensitive to changes in outcome variables that measure the impact of interventions designed to control BP.
Assessment opportunities comprise: 1) patient attitudes and outcomes, 2) provider activities, and 3) aspects of the practice setting. Beyond the health center or clinic, assessments can be conducted across a community or within the larger health care system to which an individual belongs, such as an employer’s health system or managed care organization (MCO).
Some health systems are well organized in assessing the impact of interventions. In MCOs or Veterans Affairs medical centers, for example, data can be captured on clinical outcomes as well as resource use, physician and staff workflow, sustainability, and cost to the system and patient. Combined with the patient’s self-report of outcome and satisfaction, information from electronic health records and claims data can result in a comprehensive assessment of the relative cost and benefit of an intervention. In less-integrated settings, Health Insurance Portability and Accountability Act issues and irreconcilable databases can make the collection of such information impossible.
Translation to Clinical Practice
The panel members recognized the profound obstacles encountered in translating research findings into routine practice. Adaptation of clinical research results into practice often involves meaningful changes in individualized health decision-making, medical practice, and care delivery. Both public and private sector stakeholders must identify and implement changes in infrastructure, funding, and operation.78
One successful translational model focused on making large-scale improvements using a health care system-wide perspective.79 Centralized researchers work with local provider teams. The central researchers have access to greater resources for developing innovations. The centralized group recommends innovations to the local providers. The local providers adapt interventions, tailoring them to fit community-level resources and practices, organizing support mechanisms, and otherwise identifying how to install processes so that all patients receive the proposed intervention.
This translational process demonstrates the strategic importance of instilling a sense of local (community) ownership when working to improve TLC for BP control. Local stakeholders are best positioned to adapt recommendations to local culture based on ethnic values; to determine whether recommended behaviors are easy or difficult to comply with and modify recommendations accordingly; to provide ongoing support; and to evaluate performance.
Summary
A multidisciplinary panel was asked to synthesize the current scientific evidence regarding lifestyle changes in hypertension management and to identify strategies to assist health care providers with incorporating TLC into the management plan for African Americans with high BP.
Many types of interventions for TLC have scientific evidence demonstrating they can improve BP control. However, many factors may impede or facilitate the adoption or maintenance of TLC, including characteristics of and relationships between the patient, provider, recommended therapy, and environment.
Several strategies can be effective in overcoming barriers to patients making TLC. Empowering the patient involves patient-centered care emphasizing self-management supported by providers, family, and community. Increasing the cultural competence of providers and health care organizations enhances the use of strategies addressing the cultural heritage, beliefs, and behaviors of those receiving care. Likelihood of success is increased by simultaneously targeting multiple factors. At the patient level, assessing social and cultural factors (eg, socioeconomic status, health beliefs, health literacy, and health knowledge) may identify individual barriers and enhance TLC interventions. At the provider level, an effective relationship between the patient and provider is crucial to effective intervention. Changes across health systems and public policy decisions are needed to effect meaningful changes in the delivery of hypertension care. The application of multiple interventions for African Americans was illustrated.
Advances in improving TLC depend on the generation and application of scientific knowledge. Generating new knowledge requires the use of culturally sensitive metrics designed to identify barriers to hypertension management, measure the impact of the intervention, and assess the influence of the intervention on health outcomes. Translating research findings into practice requires local adaptation to address specific circumstances.
Clinical trials are under way that may further enrich our understanding of strategies conducive to sustained change. The ISHIB convened an expert panel meeting on TLC as part of a continuing campaign to update standards of hypertension care in African Americans. The next step for the ISHIB is to develop tools for both patients and providers that are informed by findings of the expert panel, communicate and reinforce management guidelines and TLC recommendations, and consolidate gains from both recent research and our experience in the community.
Acknowledgments
Editorial assistance for this article was provided by Inside Edge Consulting Group.
Footnotes
Conflict of Interest Statement
Margaret Scisney-Matlock, PhD, RN, FAAN; Hayden B. Bosworth, PhD; Joyce Newman Giger, EdD, RN, ARPN, BC, FAAN; Ora L. Strickland, PhD, DSc(Hon), RN, FAAN; R. Van Harrison, PhD; Dorothy Coverson, PhD, RN; Nirav R. Shah, MD, MPH; Cheryl R. Dennison, ANP, PhD; Jacqueline M. Dunbar-Jacob, PhD, RN, FAAN; Loretta Jones, MA; and Gbenga Ogedegbe, MD, MPH, MS disclose no conflicts of interest. Marian L. Batts-Turner, MSN, RN, CDE discloses conflicts of interest with Agamatrix, Inc., Eli Lilly, Inc., Amylin, and Delmarva Foundation. Kenneth A. Jamerson, MD discloses conflicts of interest with Daiichi-Sankyo, NHLBI, NIDDK, NIH, Merck, Novartis, and King Pharmaceuticals.
References
- 1.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49(1):69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 2.Douglas JG, Bakris GL, Epstein M, et al. Management of high blood pressure in African Americans: consensus statement of the Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks. Arch Intern Med. 2003;163(5):525–541. doi: 10.1001/archinte.163.5.525. [DOI] [PubMed] [Google Scholar]
- 3.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 4.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 5.American Heart Association. [Accessed March 9, 2009];Frequently asked questions about physical activity. Updated January 22, 2009. http://www.americanheart.org/presenter.jhtml?identifier=3048120.
- 6.Olsen RH, Krogh-Madsen R, Thomsen C, Booth FW, Pedersen BK. Metabolic responses to reduced daily steps in healthy nonexercising men. JAMA. 2008;299(11):1261–1263. doi: 10.1001/jama.299.11.1259. [DOI] [PubMed] [Google Scholar]
- 7.Douglas JG, Ferdinand KC, Bakris GL, Sowers JR. Barriers to blood pressure control in African Americans. Postgrad Med. 2002;112(4):51–70. doi: 10.3810/pgm.2002.10.1332. [DOI] [PubMed] [Google Scholar]
- 8.Cook S, Drum ML, Kirchhoff AC, et al. Providers’ assessment of barriers to effective management of hypertension and hyperlipidemia in community health centers. J Health Care Poor Underserved. 2006;17(1):70–85. doi: 10.1353/hpu.2006.0021. [DOI] [PubMed] [Google Scholar]
- 9.Davis AM, Vinci LM, Okwuosa TM, Chase AR, Huang ES. Cardiovascular health disparities: a systematic review of health care interventions. Med Care Res Rev. 2007;64(5 suppl):29S–100S. doi: 10.1177/1077558707305416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Appel LJ, Espeland MA, Easter L, Wilson AC, Folmar S, Lacy CR. Effects of reduced sodium intake on hypertension control in older individuals: results from the Trial of Nonpharmacologic Interventions in the Elderly (TONE) Arch Intern Med. 2001;161(5):685–693. doi: 10.1001/archinte.161.5.685. [DOI] [PubMed] [Google Scholar]
- 11.Ard JD, Rosati R, Oddone EZ. Culturally sensitive weight loss program produces significant reduction in weight, blood pressure, and cholesterol in eight weeks. J Natl Med Assoc. 2000;92(11):515–523. [PMC free article] [PubMed] [Google Scholar]
- 12.Artinian NT, Washington OG, Templin TN. Effects of home telemonitoring and community-based monitoring on blood pressure control in urban African Americans: a pilot study. Heart Lung. 2001;30(3):191–199. doi: 10.1067/mhl.2001.112684. [DOI] [PubMed] [Google Scholar]
- 13.Becker DM, Yanek LR, Johnson WR, Jr, et al. Impact of a community based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease. Circulation. 2005;111(10):1298–1304. doi: 10.1161/01.CIR.0000157734.97351.B2. [DOI] [PubMed] [Google Scholar]
- 14.Erickson SR, Slaughter R, Halapy H. Pharmacists’ ability to influence outcomes of hypertension therapy. Pharmacotherapy. 1997;17(1):140–147. [PubMed] [Google Scholar]
- 15.Fedder DO, Chang RJ, Curry S, Nichols G. The effectiveness of a community health worker outreach program on healthcare utilization of west Baltimore City Medicaid patients with diabetes, with or without hypertension. Ethn Dis. 2003;13(1):22–27. [PubMed] [Google Scholar]
- 16.Haskell WL, Berra K, Arias E, et al. Multifactor cardiovascular disease risk reduction in medically underserved, high-risk patients. Am J Cardiol. 2006;98(11):1472–1479. doi: 10.1016/j.amjcard.2006.06.049. [DOI] [PubMed] [Google Scholar]
- 17.Hill MN, Bone LR, Hilton SC, Roary MC, Kelen GD, Levine DM. A clinical trial to improve high blood pressure care in young urban black men: recruitment, follow-up, and outcomes. Am J Hypertens. 1999;12(6):548–554. doi: 10.1016/s0895-7061(99)00007-2. [DOI] [PubMed] [Google Scholar]
- 18.Hill MN, Han HR, Dennison CR, et al. Hypertension care and control in underserved urban African American men: behavioral and physiologic outcomes at 36 months. Am J Hypertens. 2003;16(11 pt 1):906–913. doi: 10.1016/s0895-7061(03)01034-3. [DOI] [PubMed] [Google Scholar]
- 19.Dennison CR, Post WS, Kim MT, et al. Underserved urban African American men: hypertension trial outcomes and mortality during 5 years. Am J Hypertens. 2007;20(2):164–171. doi: 10.1016/j.amjhyper.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 20.Jenkins RG, Ornstein SM, Nietert PJ, Klockars SJ, Thiedke C. Quality improvement for prevention of cardiovascular disease and stroke in an academic family medicine center: do racial differences in outcome exist? Ethn Dis. 2006;16(1):132–137. [PubMed] [Google Scholar]
- 21.Kokkinos PF, Narayan P, Colleran JA, et al. Effects of regular exercise on blood pressure and left ventricular hypertrophy in African-American men with severe hypertension. N Engl J Med. 1995;333(22):1462–1467. doi: 10.1056/NEJM199511303332204. [DOI] [PubMed] [Google Scholar]
- 22.Kumanyika SK, Adams-Campbell L, Van Horn B, et al. Outcomes of a cardiovascular nutrition counseling program in African-Americans with elevated blood pressure or cholesterol level. J Am Diet Assoc. 1999;99(11):1380–1391. doi: 10.1016/S0002-8223(99)00336-3. [DOI] [PubMed] [Google Scholar]
- 23.Levine DM, Bone LR, Hill MN, et al. The effectiveness of a community/academic health center partnership in decreasing the level of blood pressure in an urban African-American population. Ethn Dis. 2003;13(3):354–361. [PubMed] [Google Scholar]
- 24.Rogers MA, Small D, Buchan DA, et al. Home monitoring service improves mean arterial pressure in patients with essential hypertension: a randomized, controlled trial. Ann Intern Med. 2001;134(11):1024–1032. doi: 10.7326/0003-4819-134-11-200106050-00008. [DOI] [PubMed] [Google Scholar]
- 25.Schneider RH, Staggers F, Alexander CN, et al. A randomised controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995;26(5):820–827. doi: 10.1161/01.hyp.26.5.820. [DOI] [PubMed] [Google Scholar]
- 26.Svetkey LP, Simons-Morton D, Vollmer WM, et al. Effects of dietary patterns on blood pressure: subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159(3):285–293. doi: 10.1001/archinte.159.3.285. [DOI] [PubMed] [Google Scholar]
- 27.Svetkey LP, Erlinger TP, Vollmer WM, et al. Effect of lifestyle modifications on blood pressure by race, sex, hypertension status, and age. J Hum Hypertens. 2005;19(1):21–31. doi: 10.1038/sj.jhh.1001770. [DOI] [PubMed] [Google Scholar]
- 28.Tao LS, Hart P, Edwards E, Evans AT, Whitaker E, Smith P. Treatment of difficult to control blood pressure in a multidisciplinary clinic at a public hospital. J Natl Med Assoc. 2003;95(4):263–269. [PMC free article] [PubMed] [Google Scholar]
- 29.The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels: results of the Trials of Hypertension Prevention, Phase I. JAMA. 1992;267(9):1213–1220. doi: 10.1001/jama.1992.03480090061028. [DOI] [PubMed] [Google Scholar]
- 30.Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. The Trials of Hypertension Prevention Collaborative Research Group. Arch Intern Med. 1997;157(6):657–667. [PubMed] [Google Scholar]
- 31.Walker CC. An educational intervention for hypertension management in older African Americans. Ethn Dis. 2000;10(2):165–174. [PubMed] [Google Scholar]
- 32.Bosworth HB, Oddone EZ. A model of psychosocial and cultural antecedents of blood pressure control. J Natl Med Assoc. 2002;94(4):236–248. [PMC free article] [PubMed] [Google Scholar]
- 33.Borzecki AM, Oliveria SA, Berlowitz DR. Barriers to hypertension control. Am Heart J. 2005;149(5):785–794. doi: 10.1016/j.ahj.2005.01.047. [DOI] [PubMed] [Google Scholar]
- 34.Horowitz CR, Tuzzio L, Rojas M, Monteith SA, Sisk JE. How do urban African Americans and Latinos view the influence of diet on hyper tension? J Health Care Poor Underserved. 2004;15(4):631–644. doi: 10.1353/hpu.2004.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lukoschek P. African Americans’ beliefs and attitudes regarding hypertension and its treatment: a qualitative study. J Health Care Poor Underserved. 2003;14(4):566–587. doi: 10.1353/hpu.2010.0690. [DOI] [PubMed] [Google Scholar]
- 36.Robert Wood Johnson Foundation. [Accessed January 21, 2009];Opening doors: a program to reduce sociocultural barriers to health care. 1998 December 1; http://www.rwjf.org/reports/npreports/opendoorse.htm.
- 37.Anderson NB. Appealing to diverse audiences: reaching the African-American community. J Natl Med Assoc. 1995;87(8 suppl):647–649. [PMC free article] [PubMed] [Google Scholar]
- 38.Speaking of Health: Assessing Health Communication Strategies for Diverse Populations. Washington, DC: National Academies Press; 2002. Institute of Medicine Committee on Communication for Behavior Change in the 21st Century. [PubMed] [Google Scholar]
- 39.Okonofua EC, Simpson KN, Jesri A, Rehman SU, Durkalski VL, Egan BM. Therapeutic inertia is an impediment to achieving the Healthy People 2010 blood pressure control goals. Hypertension. 2006;47(3):345–351. doi: 10.1161/01.HYP.0000200702.76436.4b. [DOI] [PubMed] [Google Scholar]
- 40.Stewart MA. Effective physician-patient communications and health outcomes: a review. CMAJ. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 41.American Association of Diabetes Educators. AADE position statement. Cultural sensitivity and diabetes education: recommendations for diabetes educators. Diabetes Educ. 2007;33(1):41–44. doi: 10.1177/0145721706298202. [DOI] [PubMed] [Google Scholar]
- 42.Cherry B, Giger JN. African Americans. In: Giger JN, Davidhizar RE, editors. Transcultural Nursing. 5. St Louis, MO: Mosby Elsevier; 2008. pp. 190–196. [Google Scholar]
- 43.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 44.Bronfenbrenner U. The Ecology of Human Development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 45.Bronfenbrenner U, Morris PA. The ecology of developmental processes. In: Lerner RM, editor. Handbook of Child Psychology: Theoretical Models of Human Development. 5. Vol. 1. New York, NY: John Wiley and Sons Inc; 1998. pp. 993–1028. [Google Scholar]
- 46.Bronfenbrenner U. Making Human Beings Human: Bioecological Perspectives on Human Development. Thousand Oaks, CA: Sage Publications, Inc; 2004. [Google Scholar]
- 47.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Aff (Millwood) 2009;28(1):75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Physician Practice Connections®–Patient-Centered Medical Home™. [Accessed January 24, 2009]; http://ncqa.org/tabid/631/default.aspx.
- 49.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 50.Vargas RB, Mangione CM, Asch S, et al. Can a chronic care model collaborative reduce heart disease risk in patients with diabetes? J Gen Intern Med. 2007;22(2):215–222. doi: 10.1007/s11606-006-0072-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chin MH, Drum ML, Guillen M, et al. Improving and sustaining diabetes care in community health centers with the health disparities collaboratives. Med Care. 2007;45(12):1135–1143. doi: 10.1097/MLR.0b013e31812da80e. [DOI] [PubMed] [Google Scholar]
- 52.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 53.Giger JN, Davidhizar RE, editors. Transcultural Nursing. 5. St Louis, MO: Mosby Elsevier; 2008. pp. 1–36. [Google Scholar]
- 54.Program for Multicultural Health, University of Michigan Health System. Suggested content for enhancing cultural competency among health care providers; terms and concepts for cross-cultural competence. [Accessed January 14, 2009]; http://www.med.umich.edu/multicultural/ccp/tools.htm.
- 55.Goodman J, Blake J. Nutrition education: a computer-based education program. J Health Care Poor Underserved. 2005;16(4 suppl A):118–127. doi: 10.1353/hpu.2005.0123. [DOI] [PubMed] [Google Scholar]
- 56.Smedley BD, Stith AY, Nelson AR, editors. Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Board on Health Sciences Policy, Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 57.Office of the Attorney General, Department of Law and Public Safety. Cultural competency training. [Accessed January 14, 2009];New Jersey Register. http://www.nj.gov/lps/ca/adoption/bmeado47.htm.
- 58.Halbur KV, Halbur DA, editors. Essentials of Cultural Competence in Pharmacy Practice. Washington, DC: American Pharmacists Association; 2008. [Google Scholar]
- 59.United States Department of Health and Human Services, Office of Minority Health. [Accessed January 14, 2009];Think Cultural Health. http://www.thinkculturalhealth.org/
- 60.World Health Organization. Adherence to Long-Term Strategies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- 61.Bosworth HB, Olsen MK, McCant F, et al. Hypertension Intervention Nurse Telemedicine Study (HINTS): testing a multifactorial tailored behavioral/educational and a medication management intervention for blood pressure control. Am Heart J. 2007;153(6):918–924. doi: 10.1016/j.ahj.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 62.Fahey T, Schroeder K, Ebrahim S. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database of Syst Rev. 2006;(4):CD005182. doi: 10.1002/14651858.CD005182.pub2. [DOI] [PubMed] [Google Scholar]
- 63.Reusser ME, McCarron DA. Reducing hypertensive cardiovascular disease risk of African Americans with diet: focus on the facts. J Nutr. 2006;136(4):1099–1102. doi: 10.1093/jn/136.4.1099. [DOI] [PubMed] [Google Scholar]
- 64.Scisney-Matlock M, Glazewski L, McClerking C, Kachorek L. Development and evaluation of DASH diet tailored messages for hypertension treatment. Appl Nurs Res. 2006;19:78–87. doi: 10.1016/j.apnr.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 65.Mellen PB, Gao SK, Vitolins MZ, Goff DC., Jr Deteriorating dietary habits among adults with hypertension: DASH dietary accordance, NHANES 1988–1994 and 1999–2004. Arch Intern Med. 2008;168(3):308–314. doi: 10.1001/archinternmed.2007.119. [DOI] [PubMed] [Google Scholar]
- 66.McCann BS, Bovbjerg VE. Promoting dietary change. In: Shumaker SA, Ockene JK, Schron EB, McBee WL, editors. Handbook of Health Behavior Change. 2. chap 7 New York, NY: Springer Publishing Co; 1998. [Google Scholar]
- 67.Dunbar-Jacob J. Models for changing patient behavior. Am J Nurs. 2007;107(6 suppl):20–25. doi: 10.1097/01.NAJ.0000277821.67053.f7. [DOI] [PubMed] [Google Scholar]
- 68.Jarvis JK, Miller GD. Overcoming the barrier of lactose intolerance to reduce health disparities. J Natl Med Assoc. 2002;94(2):55–66. [PMC free article] [PubMed] [Google Scholar]
- 69.National Institutes of Health. Heart-Healthy Home Cooking: African American Style. Bethesda, MD: National Heart, Lung, and Blood Institute, Office of Research on Minority Health; 1997. [Accessed April 7, 2009]. (revised May 2008). NIH publication 08-3792. http://www.nhlbi.nih.gov/health/public/heart/other/chdblack/cooking.htm. [Google Scholar]
- 70.Rankins J, Wortham J, Brown LL. Modifying soul food for the Dietary Approaches to Stop Hypertension diet (DASH) plan: implications for metabolic syndrome (DASH of Soul) Ethn Dis. 2007;17(3 suppl 4):S4–7. 12. [PubMed] [Google Scholar]
- 71.Hess PL, Reingold JS, Jones J, et al. Barbershops as hypertension detection, referral, and follow-up centers for black men. Hypertension. 2007;49(5):1040–1046. doi: 10.1161/HYPERTENSIONAHA.106.080432. [DOI] [PubMed] [Google Scholar]
- 72.Strickland OL, DiIorio C, Coverson D, Nelson M. Advancing nursing science in vulnerable populations: measurement issues. Annu Rev Nurs Res. 2007;25:27–48. [PubMed] [Google Scholar]
- 73.Strickland OL. Challenges in measuring nursing outcomes. Nurs Clin North Am. 1997;32(3):495–512. [PubMed] [Google Scholar]
- 74.Strickland OL. Practical measurement, editorial. J Nurs Measurement. 1998;6(2):107–109. [PubMed] [Google Scholar]
- 75.Strickland OL. The practical side of measurement. Behavioral Measurement Letter. 1999;6(1):9–11. [Google Scholar]
- 76.Larson CO, Schlundt D, Patel K, Beard K, Hargreaves M. Validity of the SF-12 for use in a low-income African American community-based research initiative (REACH 2010) Prev Chronic Dis. 2008;5(2):A44. [PMC free article] [PubMed] [Google Scholar]
- 77.Ware J, Jr, Kosinski M, Keller SD. A 12-item Short Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 78.Sung NS, Crowley WF, Jr, Genel M, et al. Central challenges facing the national clinical research enterprise. JAMA. 2003;289(10):1278–1287. doi: 10.1001/jama.289.10.1278. [DOI] [PubMed] [Google Scholar]
- 79.Pronovost P, Berenholtz S, Needham D. Translating evidence into practice: a model for large scale knowledge translation. BMJ. 2008;337:a1714. doi: 10.1136/bmj.a1714. [DOI] [PubMed] [Google Scholar]