Abstract
The supply of oncologists is projected to increase by 14%, but the demand for oncology visits is projected to increase by 48% because of a growing aging population and an increase in the number of cancer survivors. Multiple strategies must be implemented to ensure continued access to quality cancer care, such as increasing the number of oncology training positions.
Introduction
In 2007, ASCO published a report concluding that the nation will face a severe shortage of physicians between now and 2020.1 Although the supply of oncologists is projected to increase by 14%, demand for oncology visits is projected to increase by 48%, in large part as a result of the growth and aging of the nation and the increase in the number of cancer survivors. The report concluded that no single solution could forestall the future shortages, and that multiple strategies must be implemented to ensure continued access to high-quality cancer care for America. One of the suggested strategies was to increase the number of oncology training positions.
Overall growth in graduate medical education (GME) stalled for the initial 5 years after the 1997 Balanced Budget Act, but during the past 5 years has grown 8%.2 The pipeline of internal medicine graduates, the prerequisite for applying to a medical oncology or hematology/oncology fellowship program, has remained fairly flat during the past decade, but has increased 4% during the past five years. There has also been a notable increase in the percentage of internal medicine residents who decide to pursue subspecialty training.2
In the 2005 Survey of Clinical Oncology Fellowship Program Directors, which was conducted as part of the background research for the workforce study, hematology/oncology and medical oncology program directors felt there was an insufficient number of clinical oncologists to meet the nation's needs, with 15% stating plans to increase enrollment by the 2010-11 academic year (AY). If those program directors who noted a “probable” or “definite” increase followed through, we would expect to see an 8% increase in new positions by AY2010-11.3
To assess if plans to increase the number of medical oncology and hematology/oncology training positions in the nation have changed since the 2005 survey, ASCO conducted a follow-up survey of program directors in 2007. The results of this survey and the potential implications are presented here.
Methods
In the fall of 2007, ASCO conducted a survey of medical oncology and hematology/oncology program directors to gain insight into their plans for new training positions during the next five years. To produce comparable results, many questions on the survey were similar or identical to those on the 2005 survey. The survey was administered to 159 program directors of medical oncology and hematology/oncology programs, using an email list maintained by ASCO. Three follow-up reminders were sent to nonrespondents. The survey received a 78% response rate (n = 124). The survey consisted of 26 questions that asked about plans to increase the number of training positions, how the new positions would be funded, the number and quality of recent applicants, barriers to expansion, initial employment setting for recent graduates, and respondent demographics. 81.5% of the respondents were hematology/oncology fellowship program directors, 15.3% were program directors of medical oncology fellowship programs, and 3.2% did not indicate a specialty affiliation.
Results
Increasing Training Slots
The survey contained several questions asking about future training program size. Respondents were asked to indicate how many first-year positions were available in AY2007 and to estimate the number of first-year positions for each subsequent year through AY2013. They were also asked a separate question about the likelihood of increasing the number of first-year positions between AY2007 and AY2013.
When comparing the responses for the number of first-year positions in AY2007 with the number estimated for AY2013, approximately one in four respondents (22.3%) indicated the number of first-year positions in their programs would be higher in AY2013, yielding an estimated 9.5% increase in positions for this group. The majority (89.3%) plan to increase by one position and the balance by two positions. None had plans to increase by more than two positions during the six-year period.
However, analysis of the additional question regarding the likelihood of enrollment introduces the possibility that the future plans could be higher than 9.5% or as low as 5.1%. 30% of the respondents said an increase in positions was “very likely” or “somewhat likely”. However, nearly half (47.5%) of those who said increases were “very or somewhat likely” did not report higher numbers of positions for AY2013 when compared with AY2007, raising the possibility of a larger increase in first-year positions than reflected in the estimates provided for AY2013. In contrast, only 67.9% of those with higher numbers of first-year positions in AY2013 indicated that an increase in positions was “very or somewhat likely,” and therefore a 9.5% increase could be an overestimate. When including only the programs where the increases were rated as “very or somewhat likely,” the estimated 9.5% growth in positions lowers to 5.1%.
Funding
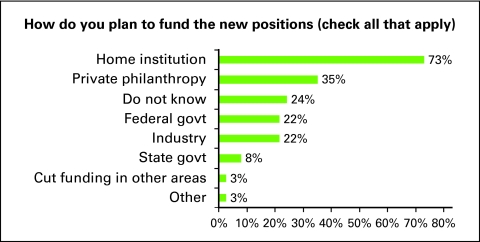
Program directors who indicated they were “very or somewhat likely” to increase positions were asked how they planned to fund the new positions by selecting all potential revenue sources that applied. The majority indicated they had one or more funding streams they would use. Three in four (73.0%) will use institutional funding to support some or all of the increased costs; 35.1% stated they will use private philanthropy; 21.6% reported plans to use industry; 21.6% planned to use funds from the federal government and 8.1% planned to use state government funding; 2.7% plan on cutting funds from other programs; and 2.7% replied “other” (Fig 1). However, one in four (24.3%) reported not knowing how they would fund the increase in positions. The majority of those who indicated they did not know where funding would come from (five of nine) did not indicate a higher number of positions for AY2013, despite saying plans to increase were “somewhat or very likely.” There was no statistically significant variation in results by program size or region.
Figure 1.
Funding for new positions. Govt, government.
Rationale for Increases
Program directors were asked if their planned increases were due to a perceived need or shortage at their institution, state/region, and/or the national level. Respondents were able to check as many answers as applied. Institutional needs were cited by the majority of program directors (68%). 45% cited national concerns, 32% state or regional concerns, and 13% indicated “other.” There was no statistically significant variation in results by program size or region.
Barriers to Expansion
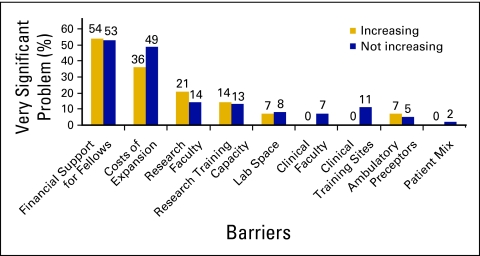
Program directors were also asked to evaluate if their laboratory and clinical space, faculty, number of patients, cost of expansion, or financial support for fellows would be a problem if the program increased the number of fellows. The two leading barriers were financial support for fellows and other costs of expansion (Fig 2). It is important to note that the cost of expansion, limited clinical faculty, and limited clinical sites were more likely to be rated as a “very significant problem” by those with no plans to increase the number of first-year positions in their program (P < .05).
Figure 2.
Barriers to expansion.
Number and Quality of Applicants
Respondents were also asked to indicate the number of applications received for AY2008, the number who came in for an interview, and the number accepted. Both the mean and median number of applications received was 206, though the number ranged from a low of nine to a high of 500. On average, programs interviewed 28 residents and accepted four. Smaller programs, with only one to two first-year positions available in AY2008, had a higher applicant-to-position ratio (93 per position) than those with three to five first-year positions or six or more first-year positions, which had 59 and 43 applications per position, respectively (P < .05).
More than 90% of program directors cited the qualifications of the AY2008 applicants as “excellent” (46%) or “good” (46%), with few (8%) marked as “acceptable,” and none rated their applicants as “poor” or “very poor.” When asked to compare the quality of the AY2008 applicants with those from 2 years ago, more than half of the program directors said they were better (50.0%) or “far better” (3.3%), 45.8% cited them as “about the same,” and only 0.8% reported them as “a little less qualified.”
Employment Settings
Program directors were asked to indicate the approximate number of recent graduates (completed training during the past 2 years) who found employment in the following areas: academic setting, private practice, government/military, industry, other, and unknown. Program directors noted 39.4% of recent graduates found employment in academic settings, 56.2% in private practice, 3.0% in government, 1.0% in industry, and 0.5% other or unknown. These results are nearly identical to those from the 2005 survey.3
Discussion
Limited Plans for Increasing Training Positions
Since the April 2007 report predicting shortages was published, there has not been a significant increase in the number of oncology training positions that will be offered between now and AY2013. Program directors' self-reported plans to increase fellowship positions are comparable to those expressed in the 2005 survey of oncology program directors.3 However, 18 respondents indicated they were likely to increase the number of positions available by 2013, though they did not include those positions in their future estimates. Perhaps some of the hesitancy to list higher first-year figures for FY2013, despite plans to increase, stems from questions regarding funding sources. Continued monitoring of the number of training positions, plans to increase, and availability of funds to support program growth will be required.
Barriers Remain
Program directors indicated that financial support for fellows is a major barrier to increasing the number of training positions. One in four programs that would like to increase positions did not know how they would fund the increase. Another 22% of the programs said they would use industry funds to support the new positions. However, there is increasing pressure for academic centers to reduce reliance on industry funding, so this potential source of funding could be eliminated.4,5 Programs that were not planning an increase were significantly more likely to say that the cost of expansion was a major barrier. Whereas the overall number of Accreditation Council for Graduate Medical Education (ACGME) –approved training positions has increased 8% since 1997, despite the cap in Medicare funding, it is unclear if this trend will continue or which specialties will grow. Oncology programs will likely be competing with other training programs for limited internal medicine resident graduates and limited GME funds—no matter what the source.
Other Ways Program Directors Can Help
Even if all 159 programs increase by one position between now and 2013, which would equate to a 31.2% increase, the nation would need to implement additional strategies for addressing projected oncologist shortages. The 2007 projection study concluded that even a 50% increase in training positions would only partially mitigate projected shortages. Because it would be difficult to make up the shortage with numbers of oncologists, another tactic would be to emphasize leadership skills and how to effectively manage collaborative care teams. The 2007 study found that 56% of oncologists who work with nurse practitioners or physician assistants report providing a higher number of visits than oncologists who do not.1 Education and training on collaborative care models could help improve not only the number of oncologists who practice with nurse practitioners or physician assistants, but also help meet demand for oncologist services.1
Applicant Pool Remains Strong
In the 2005 survey, program directors reported they would begin to have a concern about the potential quality of applicants at the level of a 30% expansion of fellowship programs. Though the number of applications has increased 30% since the 2005 survey, likely a result of oncology's recent participation in the Electronic Residency Application Service (ERAS), nearly all program directors indicated receiving better or the same level of quality applicants as in years past. Continuing excellence in an expansion effort seems to be manageable—assuming that other internal medicine subspecialties do not increase at the same rate and compete for the limited pipeline of internal medicine residents.
Limitations of the Study: Response Rate and Estimates
The results presented are self-reported data from a sample of the program directors in medical oncology and hematology/oncology. Although we were pleased to receive a 78% response rate, there is a potential for nonresponse bias. However, the sample does seem to reflect the size and specialty mix of the universe of training programs.
Program directors were asked to give their best estimates of future plans, but plans can change. To assess continuity of plans over time, responses from the 2005 survey were linked to the 2007 survey where possible, using the email domain name to match programs. Given that some respondents used Yahoo or Gmail accounts, which did not allow us to match responses across surveys; other respondents' institution domain names may have changed; some program directors were new to their position since 2005; and not all programs participated in both surveys, we were only able to match responses from 45 programs. Nonetheless, the majority (58%) of those with plans to increase in 2005 did still show plans to increase by 2010 on the follow-up survey – but not all. Similarly, 24% of those with tentative plans or no plans to increase in 2005 indicated a higher number of positions for AY2010 on the 2007 survey. As these are only estimates, and for many programs, funding for increases remains a challenge, plans will likely shift from year to year.
Conclusion
It is clear that we will not see a significant increase in the number of oncology training positions during the next 5 years. Although the overall quality of the applicant pool remains strong, there remain several barriers which could prevent additional increases. The most significant barriers seem to center on financial concerns, namely the availability of funding to support fellows and the cost of expansion. It will be important to continue to monitor plans to increase positions during the coming years so that the medical community can track the future supply of oncologists and the need for additional action to ensure continued access to oncology care for the nation.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
References
- 1.Erikson C, Salsberg E, Forte G, et al. Future supply and demand for oncologists: Challenges to assuring access to oncology services. J Oncol Pract. 2007;3:79–86. doi: 10.1200/JOP.0723601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salsberg E, Rockey PH, Rivers KL, et al. US residency training before and after the 1997 balanced budget act. JAMA. 2008;300:1174–1180. doi: 10.1001/jama.300.10.1174. [DOI] [PubMed] [Google Scholar]
- 3.Forecasting the supply of and demand for oncologists. A report to the American Society of Clinical Oncology (ASCO) from the AAMC Center for Workforce Studies. Washington, DC: Association of American Medical Colleges; 2007. [Google Scholar]
- 4.Industry Funding of Medical Education. Report of an AAMC Task Force. Washington, DC: Association of American Medical Colleges; 2008. [Google Scholar]
- 5.Brennan TA, Rothman DJ, Blank L, et al. Health industry practices that create conflicts of interest: A policy proposal for academic medical centers. JAMA. 2006;295:429–433. doi: 10.1001/jama.295.4.429. [DOI] [PubMed] [Google Scholar]