Abstract
Purpose:
A large component of ambulatory oncology practice is management of telephone calls placed to and from the practice between outpatient appointments. However, scant information is available in the literature concerning oncology practice telephone calls. The specific aims of this study were to define telephone call volume and distribution in an active ambulatory oncology practice, describe the callers and reasons for the telephone calls, and examine any differences in call volume by practice characteristics.
Methods:
A descriptive retrospective design was used to analyze medical oncology and hematology telephone calls in a 4-month period. Two investigator-developed tools were validated and used to collect data on telephone call content and patient demographics.
Results:
The sample included 5,283 telephone calls to or from 1,486 different individuals. Individuals making and/or receiving more than one telephone call in the study period represented 56% of the telephone calls. For every 10 scheduled clinic appointments, seven telephone calls were received or made. The volume of telephone calls was significantly higher on Mondays and in the mornings. The reasons for high-volume telephone calls by diagnosis and frequency were identified, with 30% of telephone calls involving multiple reasons.
Conclusion:
The data demonstrate the impact of telephone calls on ambulatory oncology practice and highlight the complex and highly variable actions required to manage the telephone calls. The findings confirm and document specific practice patterns and identify subgroups that target repeat telephone calls as an area for improvement.
Short abstract
A large component of ambulatory oncology practice is management of telephone calls placed to and from the practice between outpatient appointments, but they are not a reimbursable service, they require staff resources, and they place an unpredictable demand on workload. In this study, telephone calls were examined at a private medical oncology practice to define telephone call volume and distribution in an active ambulatory oncology practice, describe the callers and reasons for calls, and examine any differences in call volume by practice characteristics.
Introduction
Oncology practitioners often report the demands on their practices created by telephone calls. Telephone calls placed to report toxicities of treatment and new or unresolved problems are desirable, and by conducting interventions by telephone, one can reinforce teaching, evaluate the effectiveness of treatments, monitor adverse effects, provide continuity, and increase patient satisfaction. With telephone calls, one can also prevent symptoms from becoming unmanageable and possibly help patients avoid unnecessary and costly visits to the clinic or emergency department. Telephone calls are not a reimbursable service. However, they require staff resources (ie, secretarial, nursing, and provider resources) and place an unpredictable demand on workload. Telephone calls also may indicate a failure to provide necessary or complete care or education during scheduled visits.
Surprisingly little evidence is available concerning the frequency or impact of telephone calls in oncology practice. However, some practice protocols have been developed and advocated for use in assessing symptom complaints reported by telephone.1–4 Despite the validation by Cox et al5 that telephone follow-up is “an acceptable and feasible form of patient contact” in the oncology setting, few descriptive studies have examined the volume and content of telephone calls in oncology practice. Only two studies reported in the literature have provided some descriptive data about telephone call management in the ambulatory oncology setting. In the first, Nail et al6 prospectively studied telephone calls in a 6-month period between 1987 and 1988. A total of 1,844 telephone calls were reviewed. Each telephone call lasted an average of 6.6 minutes, and the content of the telephone calls most often focused on information, comfort, or coping. In the nearly 20 years since that study, only one other small descriptive study has been reported in the literature. In this study, Lucia et al7 examined telephone calls at a private medical oncology practice. In 1 week, 337 telephone calls were made to or received from 26 patients. The majority of telephone calls (92%) were from patients, and 20% of the patients made multiple telephone calls.
Given the minimal information on telephone calls in oncology practice, the specific aims of our study were to define telephone call volume and distribution in an active ambulatory oncology practice, describe the callers and reasons for the telephone calls, and examine any differences in telephone call volume by practice characteristics.
Methods
Data were collected at an ambulatory medical oncology and hematologic-malignant diagnoses (hematology) adult oncology practice at the University of Rochester Medical Center, James P. Wilmot Cancer Center (Rochester, NY). Current telephone management practice at the site includes a dedicated telephone line answered by a secretary (or voice mail if the line is busy) solely assigned for incoming calls for symptom management or patient concerns. In addition, two RNs are assigned to manage telephone calls during normal business hours with a standard that all calls will be returned the same day. The nursing staff review the requests and prioritize call management on the basis of symptoms and acute needs when multiple calls are waiting for a response. The assignment of nursing staff to telephone calls is done on a rotational basis by the nurses who work in the clinics. A descriptive retrospective design was used. The study was approved by the university's human subject review board before data collection. All telephone calls documented in the center's ambulatory care telephone record in a 4-month timeframe were included in the sample. This timeframe was considered adequate for capturing repeat callers and generalizing for overall practice. To meet inclusion criteria, the telephone call had to have been completed in the 4-month study timeframe and documented by a registered nurse (RN) on the ambulatory care telephone record, and had to involve a medical oncology or hematology patient ≥ 18 years of age.
Two investigator-developed instruments were used in this study—a telephone call record instrument and a demographic and medical data instrument. The telephone call record instrument was based on an instrument used in previous research on telephone triage6 and revised to incorporate additional variables that were included on the medical record telephone form. The instrument was evaluated by the investigators in a pilot test, and four revisions were made to address missing response categories, make response categories mutually exclusive, and add response option items. Demographic and medical data were collected from the electronic medical record, and visit volume data were obtained for the same timeframe.
The original raw data were obtained from the ambulatory care telephone record. The data were alphabetized and organized by individual patient, so multiple telephone calls from the same person could be identified. Data were de-identified, and a unique subject code was assigned to each patient and each telephone record. A detailed code book was developed. Raw data were extracted from the medical record and coded on the data collection instrument. Data verification was conducted. SPSS16 statistical software (SPSS Inc, Chicago, IL) was used to generate descriptive and comparative analyses.
Results
Our sample included 5,283 telephone calls involving 1,486 individuals placed or received in a 4-month timeframe (86 workdays). Medical oncology telephone calls accounted for 57.3% of the sample (n = 3,028) and 58.5% of the individual patients (n = 869). The average age of patients was 61.1 years (range, 19 to 97; standard deviation [SD], 15.2), and 58.5% were women, which mirrored the regional population demographics; 91.5% of the patients in the sample were white. In the 4-month study period, 7,584 scheduled appointments were made at the medical oncology and hematology clinics (not including visits to the infusion center). For every 10 scheduled clinic appointments, seven telephone calls were made or received.
The number of telephone calls received on a single day ranged from 24 to 91 (mean, 61.4). Call distribution varied by day of the week, with mean number of calls ranging from 31 to 45. Testing with a one-way analysis of variance, the volume of telephone calls was significantly higher on Monday, compared with all other days (F[1,4] = 12.8; P < .01). The nursing staff returned the call on the same day 95% of the time. However, data were not collected on the more detailed time interval of minutes or hours between when the call was received and the time the call was returned by the nursing staff. The RN answering the telephone call had to consult with the oncology provider for 52.8% of the calls. Additional time data captured the amount of time required by the RN to manage each telephone call request. RN time required ranged from 1 to 105 minutes (mean, 12.13; SD, 10.43). These data convert to an average daily workload of 16.4 RN hours of time required for telephone call management; however, because of the wide range, the number of nursing care hours required for telephone management varied widely from day to day.
The majority of telephone calls were received from patients and family members (44.4% and 19.0%, respectively). The remaining 36.6% of telephone calls were received from nine additional categories of callers, including community health nurses (9.5%), pharmacists (5%), and radiology services, clinical laboratories, physical therapists, referring physicians, outside hospitals and nursing homes, employers, insurers, and funeral homes (< 5% each). The cancer center nursing staff initiated 7.8% of telephone calls.
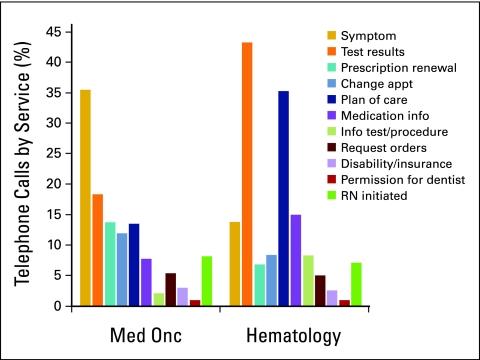
The majority of telephone calls (65%) included multiple requests or reasons for calling, which were coded into 11 categories. The most frequent reasons for calling were to request diagnostic or blood work results, report symptoms, and clarify questions about plan of care or treatment. Telephone calls to change appointments were included only if they required nursing intervention, not when they were handled by clerical staff. Telephone calls made to report symptoms included a range of one to eight different symptoms reported in a single telephone call. Reasons for placing calls varied between medical oncology and hematology patients, and are summarized in Table 1. Because many telephone calls involved multiple reasons, Table 1 lists the total number of requests rather than percentage (total number of reasons > 100% total call volume). Figure 1 shows the variation in reasons for telephone calls between clinical services.
Table 1.
Reasons for Telephone Calls
| Reason | Medical Oncology (n = 3,028) | Hematology (n = 2,255) |
|---|---|---|
| Report symptoms | 1,077 | 380 |
| Request test results, laboratory, x-ray, and so on | 414 | 1,074 |
| Plan of care questions/issues | 548 | 756 |
| Change/schedule appointment | 370 | 200 |
| Prescription renewal | 420 | 153 |
| Request medication information | 255 | 338 |
| Request information on test/procedure | 245 | 168 |
| Disability/insurance/record/referral questions | 92 | 59 |
| Permission for dentist/medication | 25 | 18 |
| Call originating with cancer center nurse | 251 | 476 |
Figure 1.
Reasons for telephone calls; percentage by clinical service. Med Onc, medical oncology; appt, appointment; RN, registered nurse.
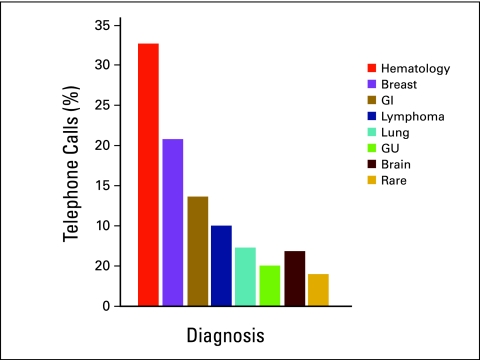
Telephone calls were placed by or for 1,486 different individuals; 869 (58.5%) were medical oncology patients, and 617 (41.5%) were hematology patients. The mode per person was one call, and the mean was 3.56 calls (SD, 4), with a range of one to 43 telephone calls per individual. Repeat callers accounted for 56% of telephone calls; 43.9% of callers made one telephone call only, 32.4% of callers made two to four telephone calls, and 15.7% of callers made five to nine telephone calls; 8% of callers were high-volume repeat callers who made 10 to 43 telephone calls each. Telephone call distribution was examined by diagnosis and is listed in Table 2. The largest volume of calls was received regarding hematology and breast cancer services, which was consistent with the number of visits scheduled for patients in these services. However, discrepancies between telephone call and visit volumes were noted in some services. For example, the neuro-oncology service, which accounts for only 1.3% of visits, accounted for 6.7% of telephone calls. Additional examination was conducted to determine high-volume callers by diagnosis. The mean percentage of calls by diagnosis is presented in Figure 2. Testing with an analysis of variance, significant differences were seen in the number of telephone calls placed by diagnosis, with individuals with brain cancer making significantly more telephone calls than made by individuals of any other group (F[1,7] = 75.6; P < .001).
Table 2.
Telephone Call Distribution by Diagnosis
| Diagnosis | Telephone Calls (%) | Visits (%) | Callers (%) |
|---|---|---|---|
| Hematology | 32.7 | 31.3 | 27.2 |
| Breast cancer | 20.8 | 22.9 | 26.9 |
| GI cancer | 13.6 | 14.9 | 10.5 |
| Lymphoma | 10 | 11.6 | 14.3 |
| Thoracic cancer | 7.3 | 6.8 | 6.3 |
| Genitourinary cancer | 5 | 8.7 | 7.9 |
| Brain cancer | 6.7 | 1.3 | 3.1 |
| Rare cancer | 4 | 2.5 | 3.9 |
Figure 2.
Percentage of telephone calls by diagnosis. GU, genitourinary.
Additional data were collected to confirm the volume of telephone calls received compared with scheduled visits. In a 2-week period (10 business days) in June 2007, a total of 820 telephone calls were received. During this same period, there were 740 visits, equating to 11 telephone calls for every 10 visits. In a 4-week follow-up period (21 business days) in June 2008, there were 1,628 telephone calls and 1,588 visits with providers, equating to 10 telephone calls for every 10 visits.
Discussion
In our study, 5,283 telephone calls were made in 86 workdays, with a mean of 61.4 telephone calls per day, and seven telephone calls for every 10 visits. These data support the widely accepted belief that telephone calls are a large component of ambulatory oncology practice. The telephone call volume was lower than that described by Lucia et al,7 who reported 337 telephone calls in a 1-week period (average, 67 telephone calls per day). However, no data were provided on visit volume in that study. Data for the same setting, collected prospectively and reported by Nail et al6 18 years earlier, showed four telephone calls for every 10 visits; results of the two studies indicate a clear increase in the setting's telephone call volume in an 18-year period. The assumption that telephone call volume has increased historically is clinically accepted, but rarely has this assumption been made on the basis of evidence. Updated data collected at two time points confirm that telephone calls represent a large component of ambulatory practice. Possible explanations for the large volume of telephone calls could include the increased complexity of oral chemotherapy management, an increased willingness among patients to report issues, and an overall increase in the complexity of and trend toward ambulatory management of cancer.
In addition to confirming that telephone calls represent a large component of practice, our data also confirm the unpredictability of telephone call volume, which varies by day of week and time of day. In our study, telephone call distribution ranged widely by day and was significantly higher on Mondays, which supports findings by Lucia et al7 and Nail et al,6 although call patterns in their studies were different from those in ours. The variability in telephone call patterns and distribution has been a consistent finding. The mean time it took RNs to answer telephone calls was 12 minutes, which was much higher than the 6 minutes previously reported in the literature.6 The wide range of time required to manage individual telephone calls also confirms the highly variable nature of the workload of responding RNs.
Although 12 categories of callers were identified, patients (44%) and family members (19%) accounted for the majority (63%) of calls. This differs from the findings of Lucia et al,7 who reported that 98% of calls were from patients and 6% were from family members. There are several possible explanations for this difference. For example, the different findings regarding who places calls to an oncology office may reflect geographic variance or patient or practice characteristics, or may be a measurement artifact that only patient-generated calls were included in the prior sample. The range and percentage of calls received from various individuals require additional descriptive research to verify the findings. Interestingly, only a small percentage of telephone calls were initiated prospectively as outgoing calls by nursing staff. In our sample, 56% of telephone calls were repeat calls concerning the same individual. This was a much higher percentage than the percentage of repeat calls (20%) in the Lucia et al sample. However, their data were collected in a 1-week period, which could account for the difference. The large volume of telephone calls received from repeat callers in the 4-month study period indicates that telephone call management is a mechanism for providing continuity of care, not just triage of urgent needs.
The findings in our examination of telephone call volume and reasons for calling demonstrate variation by oncology services. The categories for reasons for calling were established by a content analysis. Our findings reflect the varying diagnostic needs of different oncology practices. The subgroup of callers who made repeat calls represents a group of patients whose multiple needs are not being met during visits and/or at home. In the Lucia et al7 study, 13% of telephone calls were placed for multiple reasons, and six reasons for placing telephone calls were identified. Lucia et al included categories not used in our analysis (eg, psychological support and treatment information only); five additional categories were reported in their study. The distribution of reasons for telephone calls is not consistent across studies and may reflect varying practice patterns.
The results of our descriptive study confirm that telephone calls make up a large component of ambulatory oncology practice. The workload involved in managing these telephone calls is clinically and administratively significant, complex, and highly variable. Data from our investigation provide foundational information about the oncology practice of one oncology academic medical center.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Acknowledgment
We acknowledge the funding, data entry, and mentoring support of the University of Rochester School of Nursing; Michele Haller, RN, BSN, nurse manager; Judy Brasch, RN, BSN, project coordinator; and the University of Rochester School of Nursing Fuld Scholar undergraduates who assisted with the project.
References
- 1.Hickey M, Newton S: Telephone Triage for Oncology Nurses. Pittsburgh, PA, Oncology Nursing Society, 2005
- 2.Nauright LP, Moneyham L, Williamson J: Telephone triage and consultation: An emerging role for nurses. Nurs Outlook 47:219-226, 1999 [DOI] [PubMed] [Google Scholar]
- 3.Wheeler S: Telephone Triage: Theory, Practice and Protocol Development. Albany, NY, Delmar Publishers, 1993
- 4.Preston FA: Telephone triage. Clin J Oncol Nurs 4:294-296, 2000 [PubMed] [Google Scholar]
- 5.Cox K, Wilson C: Follow-up for people with cancer: Nurse-led services and telephone interventions. J Adv Nurs 43:51-61, 2003 [DOI] [PubMed] [Google Scholar]
- 6.Nail M, Greene D, Jones LS, et al: Nursing care by telephone: Describing practice in an ambulatory oncology center. Oncol Nurs Forum 16:387-395, 1989 [PubMed] [Google Scholar]
- 7.Lucia VC, Decker VB, Israel CE, et al: Telephone contacts between triage nurses and cancer patients: An integral part of a community oncology practice. Community Oncol 4:350-354, 2007 [Google Scholar]