Short abstract
The combination of a shortfall in oncologists and primary care physicians and an increased number of patients using more health care resources raises concerns about our health care system's ability to accommodate future patients with cancer and cancer survivors.
Abstract
Studies have predicted a shortfall in the workforces of oncologists and primary care physicians in the coming years. These estimates are based on the number of current physicians, those leaving the profession, and the rate of new physicians joining each profession, as benchmarked against the number of patients needing care. For active cancer treatment, and particularly for the care of cancer survivors, it is likely that current calculations underestimate the shortfalls which will occur in the next 5 to 10 years. Ever more complex cancer therapies are leading to better outcomes with improved cure rates and prolonged survivals even for patients who ultimately succumb to their disease, resulting in a substantial increase in utilization of health care resources. Due to these factors, utilization of health care resources by cancer patients and cancer survivors is climbing at a rate greater than would be predicted by patient numbers alone. The combination of an increased number of patients utilizing more resources calls into question the ability of our healthcare system to meet the needs of cancer patients and cancer survivors in the future. It is crucial that innovative models of care (utilizing nonphysician providers) be developed and evaluated to assure quality care and services for this growing population.
Introduction
Studies have predicted that the number of oncologists will be insufficient to meet the needs of patients with cancer and cancer survivors in the years to come. It has been suggested that cancer survivors should be more quickly transitioned to care by primary care physicians so that oncologists can concentrate their efforts on caring for patients receiving active therapy. There is, though, concern that the number of primary care physicians, even if trained to address the complex needs of cancer survivors, will also be inadequate to meet the needs of the US population overall, and therefore may be unable to assume care of these patients.1–6 In this article we document these parallel trends and propose initial steps for a long-term manpower strategy.
Increasing Needs for Care
The number of patients living with or after cancer in the United States has increased steadily over the past decades, though most recent data suggest this trend may be reversing.7 Newer therapies used to treat these patients are becoming more complex, and the number of cancer survivors is increasing as a result of improved treatment and earlier detection. The impact on the health care system is significantly greater than the increased numbers of patients would suggest, due in part to the increased complexity of care and prolonged survivals. Without taking this into account, we will greatly underestimate the projected shortage of health professionals needed to care for these patients.
As patients are living longer, both oncologists and primary care physicians are playing major roles in caring for them across the cancer trajectory. Although the current supply of oncologists is adequate, recent analyses suggest that the United States may face an acute shortage of medical oncologists in the near future.4,8 In addition, the well-documented shortage of primary care physicians, as well as inadequate preparation of these providers to address the complex concerns of patients with cancer, calls into question the capacity of our health care system to meet the needs of these patients in coming years, both during active therapy and, just as important, throughout short- and long-term survivorship.1–3,5,6
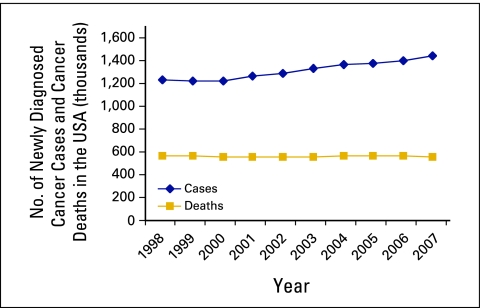
A growing aging population, improved screening, and more effective therapies are resulting in a rapidly increasing number of patients with cancer and cancer survivors. As shown in Figure 1, the number of newly diagnosed patients with cancer in the United States has risen steadily over the past 10 years and now exceeds 1.4 million persons per year.9,10 During this same period, the number of patients dying of cancer has remained relatively stable at less than 600,000 per year as a result of early detection and improved therapies that are reducing mortality rates. Therefore, nearly two thirds of the newly diagnosed patients will survive their cancer for more than 5 years, requiring continued active treatment and/or ongoing care. With time, this will dramatically increase the total number of patients with cancer and cancer survivors under active care and/or surveillance.
Figure 1.
Number of patients with newly diagnosed cancer and cancer deaths in the United States between 1998 and 2007. Data adapted with permission.9,10
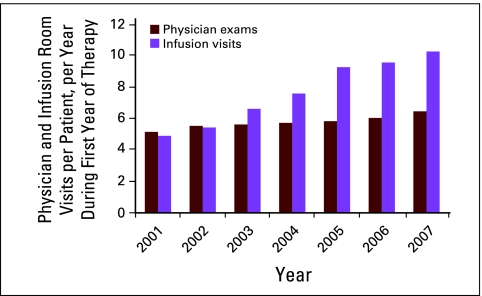
In addition, with the introduction of new anticancer therapies, cancer care is becoming more complex, resulting in a greater utilization of health care resources and an increased number of physician and infusion room visits for any given patient over a set period of time. These data are not routinely collected in most centers; however, an academic cancer center in New England tracked this information and identified that in 7 years (2001-2007), the average number of physician visits per patient per year rose 25% during the first year of treatment (Figure 2; Lawrence N. Shulman, MD, personal communication, October 2008). More dramatically, the number of infusion visits for a given patient during the first year of his/her therapy more than doubled, increasing 111%.
Figure 2.
Physician and infusion room visits per patient per year during the first year of therapy from 2001 to 2007. Data adapted with permission from the Dana-Farber Cancer Institute.
One example that illustrates this trend is the woman with node-positive breast cancer whose tumor overexpresses human epidermal growth factor receptor 2/neu (HER2/neu). In 2001, she might have had, on average, eight visits for chemotherapy in her first year. When it was discovered in 2005 that adding trastuzumab to standard chemotherapy reduced the likelihood of disease recurrence by half for these patients, this regimen quickly became standard of care.11 The addition of trastuzumab to standard therapy results in approximately 27 treatment visits during the first year, rather than eight, as well as increased monitoring for cardiac and other toxicities. Trastuzumab in this setting is one of the major recent advances in cancer medicine, resulting in a significant decrease in mortality in these patients. These women, who in the past would not have survived, will now continue to utilize physician, nurse, and other heath care services to monitor for disease recurrence and to provide care for non–cancer-related acute and chronic illnesses.
Another example is in the treatment of metastatic colon cancer. Fifteen years ago, fluorouracil was the only approved agent for patients with metastatic colon cancer, and survival averaged 10 months. Now irinotecan, oxaliplatin, cetuximab, and bevacizumab are all available, and survival has doubled to 20 months. No one would consider this the ultimate treatment outcome; however, the benefit is substantial. Once again, this results in greater utilization of physician, nurse, and other healthcare resources. Furthermore, each patient will now use additional health care resources for twice the length of time. Consequently, a cancer center seeing a fixed number of new patients with metastatic colon cancer per year will, at any given time, provide care for twice the number of patients as compared with a decade ago. Clearly, improved cure rates and the prolongation of survival for patients not cured result in a dramatic increase in the number of patients with cancer requiring short- and long-term care, even without considering the increase in the number of newly diagnosed patients entering the system.
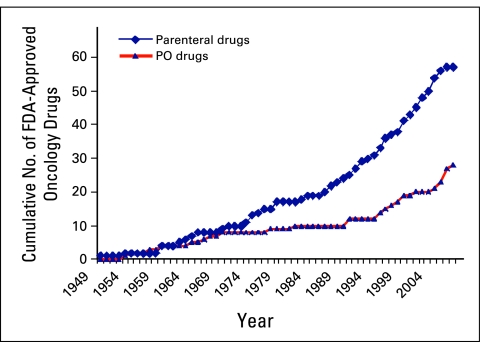
The concept that cancer will become a chronic disease, easily managed with oral agents such as kinase inhibitors, has clearly not yet become reality. Though there has been an increase in new oral therapies for cancer over the past decade, there has been an even greater increase in parenteral medications requiring infusion room visits and close monitoring. Figure 3 shows the cumulative number of parenteral and oral anticancer agents approved by the US Food and Drug Administration since 1949, demonstrating these facts.
Figure 3.
Cumulative number of US Food and Drug Administration (FDA) -approved oncology drugs by year and route of administration. Data adapted from www.fda.gov. PO, oral.
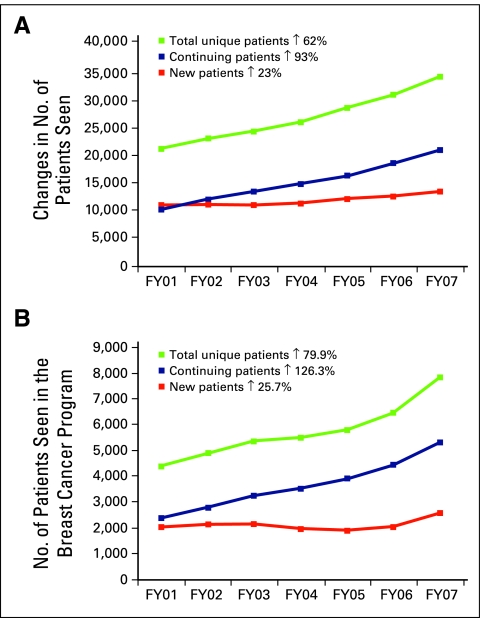
The increased accumulation of patients with cancer can be seen in Figure 4 (Lawrence N. Shulman, personal communication, October 2008). These data are for fiscal years 2001 to 2007 from the same academic cancer center noted in Figure 2. The number of new patients seen each year increased modestly during this period, while the number of patients receiving ongoing care rose 93%. These data are even more dramatic for a disease such as breast cancer, where long-term survival rates are greater than 80% in the United States. In the case of breast cancer, in this 7-year period, with no increase in new patients seen per year, the number of patients receiving care more than doubled, rising 126% (Figure 4B). Increases will be less dramatic for other diseases such as lung cancer, for which survival rates are lower; however, the same general concepts apply. Anticipated improvements in therapies and outcomes in other diseases will further accelerate these trends.
Figure 4.
(A) Changes in numbers of patients seen at an academic cancer center from fiscal year (FY) 2001 to FY 2007. (B) Number of patients seen in the breast cancer program from FY 2001 to FY 2007. New patients are those seen for the first time in the year listed; continuing patients are those seen in previous years, who return for care in the year listed; and total unique patients represent the sum of new patients and those continuing their care. Data adapted with permission from the Dana-Farber Cancer Institute.
Physician Shortage for Oncology Care and Follow-Up
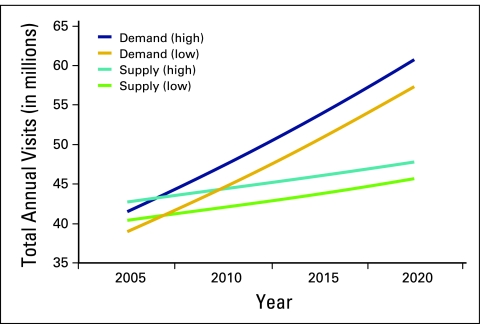
In the aggregate these factors will create, over time, a far larger gap than currently predicted between the number of patients needing care and the number of medical oncologists and primary care physicians available to provide that care. The American Society of Clinical Oncology recently reported, as shown in Figure 5, that there is likely to be a growing relative shortage of oncologists to care for this country's patients with cancer in the next few years.8 As oncologists are faced with the strain of taking care of an increasing number of patients receiving ever more complex care, they will possibly need to choose between caring for patients with cancer who are receiving active therapy and cancer survivors. One might expect that oncologists will be forced to focus their energy and time on patients undergoing therapy for cancer or other related acute problems.
Figure 5.
Projected supply of and demand for oncologists between 2005 and 2020. Data adapted with permission.8
Care of Cancer Survivors
The fact that medical oncologists will have an increasingly difficult time caring for the growing number of patients with active cancer receiving increasingly complex therapy has prompted the suggestion that the care of many or most cancer survivors could be best transitioned to primary care physicians and/or other providers sooner after treatment. To accomplish this, adequate communication and coordination of care is critical to ensure a seamless transition from oncology to other care providers.
Hewett et al's12 report, From Cancer Patient to Cancer Survivor: Lost in Transition, identified survivorship as a distinct phase of the cancer trajectory, and coordination of care between specialists and primary care providers was identified as an essential component of cancer care. The Institute of Medicine also convened several committees and workshops to examine the gaps which currently exist in the care of these patients.12–16 It was determined that these patients confront significant physical and emotional challenges both in the short- and long-term. As treatments become more complex and include many new agents whose late effects are not always fully understood, adequate ongoing medical care is particularly critical.
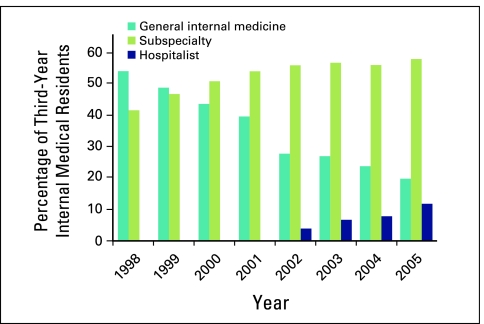
One barrier to the transfer of care to primary care physicians solution is illustrated by the sobering statistics outlined in Figure 6. These data suggest that the number of internal medicine trainees going into primary care is falling progressively. The number of primary care physicians has declined for a variety of reasons as the demands on primary care physicians are increasing, perhaps even more dramatically than for oncologists.6,17 In addition to providing care to an aging population, primary care providers must comply with pay-for-performance measures, participate in health maintenance initiatives, keep up with a vast and rapidly changing body of medical literature, and master the utilization of new drugs used to treat complex diseases. Productivity, as measured by number of patient visits per day, may well fall for primary care physicians in the coming years. As in the case of the oncologist, the primary care physician will be faced with choosing between caring for patients with acute illnesses requiring immediate intervention and cancer survivors who may be relatively well but at risk for numerous medical problems that require ongoing surveillance. It is likely, and appropriate, then that with limited resources the patient requiring acute intervention will be given priority.
Figure 6.
Proportions of third-year internal medical residents choosing careers as generalists, subspecialists, and hospitalists. Data adapted with permission.17
Options for Care of Cancer Survivors
There are no current plans that are likely to yield sufficiently increased numbers of either oncologists or primary care physicians to meet the needs of our country's patients with cancer and cancer survivors over the next 5 to 10 years. Innovative care models for patients receiving active cancer care and for cancer survivors are currently being developed and tested in a few cancer centers across the country utilizing physician extenders, such as nurse practitioners and physician assistants, as well as registered nurses. The use of these models may provide a solution, at least in part, to this problem. The collaborative practice model, in which the oncologist partners with a nurse practitioner or physician's assistant, can be structured in several ways that will allow the physician to see more new patients and patients with complex medical problems, while the nurse practitioner or physicians' assistant follows the patients in treatment, patients with routine follow-up, and/or provide ongoing care to the long-term survivors in the practice. In many institutions, nurse practitioners see patients independently and bill for these services. Models of care with physician extenders working in freestanding survivorship clinics are also being developed at a few centers across the country.
Each of these models of care include a survivorship visit with a physician extender at the end of active treatment focused on developing and discussing a formal end-of-treatment summary and follow-up care plan developed for the cancer survivor, based on data-derived guidelines developed by oncologists and primary care physicians, linked with quality-of-care measures as currently used for diabetes and heart disease care.18–21 A formal treatment summary and care plan document would facilitate the transition of a patient from oncology to primary care. Efforts to better inform primary care physicians on issues related to cancer survivors are critical, and these documents would provide the primary care provider with guidance regarding the treatment a patient received and the recommended follow-up care specific to that survivor's treatment history and related medical risks.
In addition, more creative ways for oncologists and primary care physicians to work together in the care of cancer survivors might be both more efficient and provide better-coordinated care. The development of a cohort of primary care physicians with a focused interest and education in cancer survivorship may be worth exploring. Physician extenders specializing in cancer survivorship working in primary care practices might also facilitate the care of these patients. Formal programs to prepare an adequate number of primary care providers and primary care physician extenders with expertise in cancer survivorship would be helpful.
Conclusions
The increasing complexity of cancer care, and the improving survival rates for patients with cancer and survivors will progressively strain the medical system in the next 5 to 10 years, in ways that may be underestimated by current calculations. It is important to take into consideration both the oncology and primary care workforces to better understand and prepare to meet this expanding need, and to devote research efforts and pilot programs to develop innovative, effective, and corrective strategies as soon as possible.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Acknowledgment
We thank Edward S. Salsberg, Director, Center for Workforce Studies, Association of American Medical Colleges, for his reading of the manuscript and many helpful suggestions; and Elizabeth Liebow for her work in preparing the patient demographic data from Dana-Farber Cancer Institute.
References
- 1.Salsberg E, Forte G: Trends in the physician workforce, 1980-2000. Health Aff (Millwood) 21:165-173, 2002 [DOI] [PubMed] [Google Scholar]
- 2.Salsberg E, Grover A: Physician workforce shortages: Implications and issues for academic health centers and policymakers. Acad Med 81:782-787, 2006 [DOI] [PubMed] [Google Scholar]
- 3.Kindig DA: Strategic issues for managing the future physician workforce. Baxter Health Policy Rev 2:149-182, 1996 [PubMed] [Google Scholar]
- 4.Warren J, Mariotto A, Meekins A, et al: Current and future utilization of services from medical oncologists. J Clin Oncol 26:3242-3247, 2008 [DOI] [PubMed] [Google Scholar]
- 5.Goodman D, Fisher E: Physician workforce crisis? Wrong diagnosis, wrong prescription. N Engl J Med 358:1658-1661, 2008 [DOI] [PubMed] [Google Scholar]
- 6.Starfield B, Fryer G: The primary care physician workforce: Ethical and policy implications. Annals of Family Med 5:486-491, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jemal A, Thun MJ, Ries LAG, et al: Annual report to the nation on the status of cancer, 1975-2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Inst 100:1672-1694, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Erikson C, Salsberg Ed, Forte G, et al: Future supply and demand for oncologists: Challenges to assuring access to oncology services. J Oncol Practice 3:79-86, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Data derived from www.cancer.gov
- 10.Data derived from www.acs.org
- 11.Romond EH, Perez EA, Bryant J, et al: Trastuzumab plus adjuvant chemotherapy for operable HER-2-positive breast cancer. N Engl J Med 353:1673-1684, 2005 [DOI] [PubMed] [Google Scholar]
- 12.Hewitt M, Greenfield S, Stovall E: From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC, National Academies Press, 2006
- 13.Institute of Medicine, National Research Council: Childhood Cancer Survivorship: Improving Care and Quality of Life. Washington, DC, National Academies Press, 2003 [PubMed]
- 14.Hewitt ME, Bamundo A, Day R, et al: Perspectives on post-treatment cancer care: Qualitative research with survivors, nurses, and physicians. J Clin Oncol 25:2270-2273, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Hewitt M, Ganz PA: Lost in Transition—An American Society of Clinical Oncology and Institute of Medicine Symposium. From Cancer Patient to Cancer Survivor, Washington, DC, National Academies Press, 2006
- 16.Hewitt M, Ganz PA: Implementing Cancer Survivorship Care Planning: Workshop Summary. Washington, DC, National Academies Press, 2007
- 17.Bodenheimer T: Primary care: Will it survive? N Engl J Med 355:861-864, 2006 [DOI] [PubMed] [Google Scholar]
- 18.Nissen M, Beran M, Lee M, et al: Views of primary care providers on follow-up care and cancer patients. Family Medicine 39:477-482, 2006 [PubMed] [Google Scholar]
- 19.Earle CC, Nevill BA: Underuse of necessary care among cancer survivors. Cancer 101:1712-1719, 2004 [DOI] [PubMed] [Google Scholar]
- 20.Earle CC, Burstein HJ, Winer EP, et al: Quality of non–breast cancer health maintenance among elderly breast cancer survivors. J Clin Oncol 21:1447-1451, 2003 [DOI] [PubMed] [Google Scholar]
- 21.Snyder CF, Earle CC, Herbert RJ, et al: Preventive care for colorectal cancer survivors: A 5-year longitudinal study. J Clin Oncol 26:1073-1079, 2008 [DOI] [PubMed] [Google Scholar]