Abstract
Stress is known to suppress immune function and increase susceptibility to infections and cancer. Paradoxically, stress is also known to exacerbate asthma, and allergic, autoimmune and inflammatory diseases, although such diseases should be ameliorated by immunosuppression. Moreover, the short-term fight-or-flight stress response is one of nature's fundamental defense mechanisms that enables the cardiovascular and musculoskeletal systems to promote survival, and it is unlikely that this response would suppress immune function at a time when it is most required for survival (e.g. in response to wounding and infection by a predator or aggressor). These observations suggest that stress may suppress immune function under some conditions while enhancing it under others. The effects of stress are likely to be beneficial or harmful depending on the type (immunoprotective, immunoregulatory/inhibitory, or immunopathological) of immune response that is affected. Studies have shown that several critical factors influence the direction (enhancing vs. suppressive) of the effects of stress or stress hormones on immune function: (1) Duration (acute vs. chronic) of stress: Acute or short-term stress experienced at the time of immune activation can enhance innate and adaptive immune responses. Chronic or long-term stress can suppress immunity by decreasing immune cell numbers and function and/or increasing active immunosuppressive mechanisms (e.g. regulatory T cells). Chronic stress can also dysregulate immune function by promoting proinflammatory and type-2 cytokine-driven responses. (2) Effects of stress on leukocyte distribution: Compartments that are enriched with immune cells during acute stress show immunoenhancement, while those that are depleted of leukocytes, show immunosuppression. (3) The differential effects of physiologic versus pharmacologic concentrations of glucocorticoids, and the differential effects of endogenous versus synthetic glucocorticoids: Endogenous hormones in physiological concentrations can have immunoenhancing effects. Endogenous hormones at pharmacologic concentrations, and synthetic hormones, are immunosuppressive. (4) The timing of stressor or stress hormone exposure relative to the time of activation and time course of the immune response: Immunoenhancement is observed when acute stress is experienced at early stages of immune activation, while immunosuppression may be observed at late stages of the immune response. We propose that it is important to study and, if possible, to clinically harness the immunoenhancing effects of the acute stress response, that evolution has finely sculpted as a survival mechanism, just as we study its maladaptive ramifications (chronic stress) that evolution has yet to resolve. In view of the ubiquitous nature of stress and its significant effects on immunoprotection as well as immunopathology, it is important to further elucidate the mechanisms mediating stress-immune interactions and to meaningfully translate findings from bench to bedside.
Key Words: Acute stress-induced enhancement; Fight-or-flight stress; Immune cell distribution; Immune function, effects of stress; Immune function, enhancing vs. suppressive effects; Immunoprotection vs. immunopathology; Innate/primary immune responses; Leukocyte trafficking; Adaptive/secondary immune responses
Introduction
Numerous studies have demonstrated adverse effects of stress on health [1, 2]. These studies show that chronic or long-term stressors can have health-aversive effects, some of which are mediated through immune mechanisms. However, it is also important to appreciate that a psychophysiological stress response is one of nature's fundamental survival mechanisms. Without a fight-or-flight stress response, a lion has no chance of catching a gazelle, just as the gazelle has no chance of escape. During such short-term stress responses observed in nature, physiological systems act in synchrony to enable survival. Therefore, we hypothesized that just as the stress response prepares the cardiovascular, musculoskeletal and neuroendocrine systems for fight or flight, under certain conditions, stress may also prepare the immune system for challenges (e.g. wounding or infection) that may be imposed by a stressor (e.g. predator or surgical procedure) [3, 4]. Studies have shown that short duration stressors induce a redistribution of immune cells within the body and that immune function is significantly enhanced in organs like the skin to which leukocytes traffic during acute stress. Studies have also identified mechanisms involving dendritic cell, neutrophil, macrophage, and lymphocyte trafficking, maturation, and function through which acute stressors may enhance innate as well as adaptive immunity. We suggest that the acute stress response may serve as an endogenous psychophysiological adjuvant that enhances immune responses and may have evolved by virtue of the fact that many stressful situations (aggression, accident) result in immune activation (wounding, infection) and vice versa. Interestingly, in modern times, many situations involving immune activation (vaccination, surgery, injury) also induce a stress response. It is also important to recognize that while acute stress-induced immunoenhancement may serve to increase immunoprotection during exposure to infectious agents or wounding, it may also exacerbate immunopathology if the enhanced immune response is directed against innocuous or self-antigens, or dysregulated following prolonged activation as seen during chronic stress.
In contrast to acute stress, chronic stress has been shown to dysregulate immune responses [5, 6] by altering the cytokine balance from type-1 to type-2 cytokine-driven responses [7] and accelerating immunosenescence [8], and to suppress immunity by decreasing numbers [9], trafficking [9], and function of protective immune cells while increasing regulatory/suppressor T cells [10]. This paper discusses the effects of stress on immune function and implications of these effects for immunoprotection versus immunopathology.
Stress: Definition, Mediators, and Individual Differences
Although the word ‘stress' generally has negative connotations, stress is a familiar and ubiquitous aspect of life, being a stimulant for some, but a burden for many others. Numerous definitions have been proposed for the concept of stress. Each definition focuses on aspects of an internal or external challenge, disturbance, or stimulus, on perception of a stimulus by an organism, or on a physiological response of the organism to the stimulus [11,12,13]. Physical stressors have been defined as external challenges to homeostasis and psychological stressors as the ‘anticipation justified or not, that a challenge to homeostasis looms' [13]. An integrated definition states that stress is a constellation of events, consisting of a stimulus (stressor), that precipitates a reaction in the brain (stress perception), that activates physiological fight-or-flight systems in the body (stress response) [9]. It is important to understand that the only way that a stressor can affect the brain or body is by inducing biological changes in the organism. Therefore, the physiological stress response is critical for mediating the effects of stress on health. This response results in the release of neurotransmitters, hormones, peptides and other factors into the circulation or locally within tissues. Even cytokines, factors that were traditionally thought to be the domain of the immune system, have relatively recently been shown to be released in the systemic circulation during psychological stress [14]. The major mediators of stress effects are norepinephrine and epinephrine that are released by the sympathetic nervous system, and corticotropin-releasing hormone, adrenocorticotropin (ACTH), and cortisol, that make up the hypothalamic-pituitary-adrenal (HPA) axis. Since virtually every cell in the body expresses receptors for one or more of these factors, they can induce changes in almost all cells and tissues and inform them about the presence of a stressor.
Although stress can be harmful when it is chronic or long-lasting [1, 5, 6, 15], it is often overlooked that a stress response has salubrious adaptive effects in the short run [16, 17]. Therefore, major distinguishing characteristics of stress are duration and intensity. Acute stress has been defined as stress that lasts for a period of minutes to hours, and chronic stress as stress that persists for several hours per day for weeks or months [9]. Dysregulation of the circadian cortisol rhythm is one marker that appears to coincide with the deleterious effects of chronic stress [9, 10, 18]. The intensity of stress may be gauged by the peak levels of stress hormones, neurotransmitters, and other physiological changes such as increases in heart rate and blood pressure, and by the amount of time for which these changes persist during stress and following the cessation of stress. It is important to note that significant individual differences in stress perception, processing, and coping have been observed [17, 19]. Individual differences become particularly relevant while studying human subjects because stress perception, processing, and coping mechanisms can have significant effects on the kinetics and peak levels of circulating stress hormones and on the duration for which these hormone levels are elevated. Animal studies showing significant strain differences in stress reactivity and peak hormone levels [20, 21], adaptation to stress [22], and in distribution and activation of adrenal steroid receptors and corticosteroid-binding globulin levels [20, 23], suggest that genetic as well as environmental factors play a role in establishing individual differences [20,22,23,24]. The ability of humans to generate and experience internal psychological stressors in the absence of external stressors can result in long-term activation of the physiological stress response that often has deleterious effects. The magnitude and duration of stress-induced elevations in catecholamine and glucocorticoid hormones can have significant effects on immune cell distribution and function [4, 25, 26].
Immune Responses Defined in Terms of Their End Effects: Immunoprotective, Immunopathological, and Immunoregulatory/Inhibitory
While discussing immune responses, it is useful to categorize them in terms of their principal cellular and molecular components. For example, innate, adaptive, type-1 and type-2 cytokine-driven immune responses are all defined in terms of their cellular and cytokine components. In addition to these categorizations, it is also useful to define immune responses in terms of their end-effects. Therefore, we suggest that immune responses can be categorized as being immunoprotective, immunopathological, and immunoregulatory/inhibitory. It is important to bear in mind that while all these categories provide useful constructs with which to organize ideas, concepts and models, an overall in vivo immune response is likely to consist of several types of responses with varying amounts of dominance from each category. Each of the proposed end-effect-based categories is defined below:
Immunoprotective responses are defined as responses that promote efficient wound healing, eliminate viral infections and cancer, and mediate vaccine-induced immunological memory. Key characteristics of immunoprotection involve active immune surveillance, a rapid and robust response upon immune activation, efficient clearance of the activating agent or pathogen, followed by rapid resolution of inflammation. Immunoprotective responses are critical for completion of the proliferative and remodeling phases of wound healing. Wound healing is important not only for frank wounds where the initiating event is tissue damage itself, but also for tissue-intrinsic ‘wounds' where the initiating event is an immune response precipitated by intracellular infection during which there can be collateral tissue damage. Innate and/or adaptive type-1 or type-2 immune responses can all confer immunoprotection depending on the type of the pathogen (viral, bacterial, protozoan, fungal, helminthic), on whether it is intra- or extracellular, and on the accompanying wounding conditions (e.g. sterile, infected, external or internal).
Immunopathological responses are defined as those that are directed against self- (autoimmune disease like multiple sclerosis, arthritis, lupus) or innocuous antigens (asthma, allergies) and responses that involve chronic, non-resolving inflammation. Immunopathology is also involved during low-level, long-term elevations in local and/or systemic inflammatory mediators that are thought to contribute to disorders like cardiovascular disease, obesity, and depression [27,28,29].
Immunoregulatory/inhibitory responses are defined as those that involve immune cells and factors that inhibit the function of other immune cells. Although the previous concept of suppressor T cells became mired in controversy, recent studies suggest that there is an arm of the immune system that functions to inhibit immune responses. Regulatory CD4+CD25+FoxP3+ T cells, interleukin (IL)-10, and TGF-β have been shown to have immunoregulatory/inhibitory functions. The physiological function of these factors is to keep proinflammatory, allergic, and autoimmune responses in check [30]. However, it has also been suggested that immunoregulatory/inhibitory factors may suppress antitumor immunity and be indicative of negative prognosis for cancer [31].
Factors That May Determine Whether Stress Will Enhance or Suppress Immune Function and the Potential Health Consequences of These Effects of Stress
Several critical factors are likely to influence the direction (enhancing vs. suppressive) of the effects of stress or stress hormones, and the nature of the immune response (immunoprotective, immunoregulatory/inhibitory, or immunopathological) that is affected. These include: (1) the effects of stress on leukocyte distribution in the body; (2) the duration (short-term/acute vs. long-term/chronic) of stress; (3) the differential effects of physiologic versus pharmacologic concentrations of glucocorticoids, and the differential effects of endogenous (e.g. cortisol, corticosterone) versus synthetic (e.g. dexamethasone) glucocorticoids, and (4) the timing of stressor or stress hormone exposure relative to the time of activation and ensuing time course of the immune response. It is important to recognize that factors such as gender, genetics, age, the route of administration and nature of the immunizing antigen, and time of day, may additionally affect the relationship between stress and immune function.
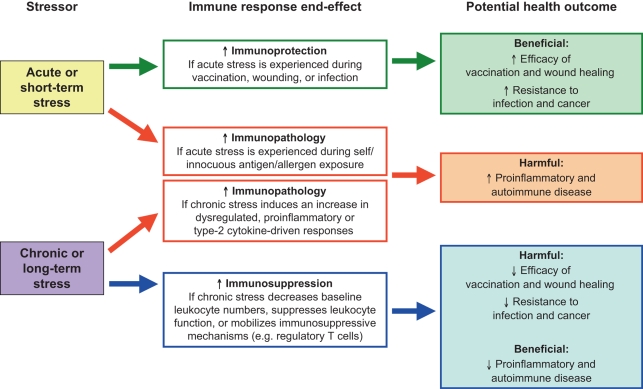
It is also important to bear in mind that whether a stressor enhances or suppresses immune function, it is the end-effect of the affected immune response that affects the health of the organism or individual (fig. 1). Given the definitions in the preceding section, stress-induced enhancement of immunoprotection is likely to have beneficial effects while stress-induced suppression of immunoprotection is likely to be harmful. Similarly, stress-induced enhancement of immunopathology or long-term proinflammation is also likely to be harmful. Finally, stress-induced enhancement of active immunoregulation/inhibition is likely to be beneficial in case of autoimmune and proinflammatory disorders and harmful in case of infections and cancer.
Fig. 1.
The relationship among stress, immune function, and health outcomes. Acute stress experienced during vaccination, wounding, or infection may enhance immunoprotective responses. Acute stress experienced during immune activation in response to self/innocuous antigens or allergens may exacerbate proinflammatory and autoimmune disorders. Chronic stress-in duced increases in proinflammatory or type-2 cytokine-mediated immune responses may also exacerbate inflammatory and autoimmune disease. Chronic stress-induced suppression of immune responses may decrease the efficacy of vaccination and wound healing and decrease resistance to infection and cancer.
Stress-Induced Changes in Immune Cell Distribution
Effective immunoprotection requires rapid recruitment of leukocytes into sites of surgery, wounding, infection, or vaccination. Immune cells circulate continuously on surveillance pathways that take them from the blood, through various organs, and back into the blood. This circulation is essential for the maintenance of an effective immune defense network [32]. The numbers and proportions of leukocytes in the blood provide an important representation of the state of distribution of leukocytes in the body and of the state of activation of the immune system. The ability of acute stress to induce changes in leukocyte distribution within different body compartments is perhaps one of the most underappreciated effects of stress and stress hormones on the immune system [3].
Numerous studies have shown that stress and stress hormones induce significant changes in absolute numbers and relative proportions of leukocytes in the blood. In fact, changes in blood leukocyte numbers were used as a measure of stress before methods were available to directly assay the hormone [33]. Studies have also shown that glucocorticoid [34, 35] and catecholamine hormones [26] induce rapid and significant changes in leukocyte distribution and that these hormones are the major mediators of the effects of stress. Stress-induced changes in blood leukocyte numbers have been reported in numerous species including humans [3,36,37,38,39,40]. This suggests that the phenomenon of stress-induced leukocyte redistribution has a long evolutionary lineage, and that perhaps it has important functional significance.
Studies have shown that stress-induced changes in blood leukocyte numbers are characterized by a significant decrease in numbers and percentages of lymphocytes and monocytes, and by an increase in numbers and percentages of neutrophils [3, 37]. Flow cytometric analyses revealed that absolute numbers of peripheral blood T cells, B cells, NK cells, and monocytes all show a rapid and significant decrease (40–70% lower than baseline) during stress [3]. Moreover, it has been shown that stress-induced changes in leukocyte numbers are rapidly reversed upon the cessation of stress [3]. In apparent contrast to animal studies, human studies have shown that stress increases rather than decreases blood leukocyte numbers [39, 41, 42]. This apparent contradiction may be resolved by taking the following factors into consideration: First, stress-induced increases in blood leukocyte numbers in humans have been studied using stress conditions which result in the activation of primarily the sympathetic nervous system. These stressors are often of a short duration (few minutes) or relatively mild (e.g. public speaking) [39, 41, 42]. Second, the increase in total leukocyte numbers may be accounted for mainly by stress- or catecholamine-induced increases in granulocytes and NK cells [26, 39, 41, 42]. Third, stress or pharmacologically-induced increases in glucocorticoid hormones induce a significant decrease in blood lymphocyte and monocyte numbers [33, 35, 39]. Thus, stress conditions that result in a significant and sustained activation of the HPA axis result in a decrease in blood leukocyte numbers.
It has been proposed that acute stress induces an initial increase followed by a decrease in blood leukocyte numbers [4]. Stress conditions that result in activation of the sympathetic nervous system, especially conditions that induce high levels of norepinephrine, may induce an increase in circulating leukocyte numbers. These conditions may occur during the beginning of a stress response, very-short-duration stress (order of minutes), mild psychological stress, or during exercise. In contrast, stress conditions that result in the activation of the HPA axis induce a decrease in circulating leukocyte numbers. These conditions often occur during the later stages of a stress response, long-duration acute stressors (order of hours), or during severe psychological, physical or physiological stress. An elegant and interesting example in support of this hypothesis comes from Schedlowski et al. [39] who measured changes in blood T-cell and NK cell numbers as well as plasma catecholamine and cortisol levels in parachutists. Measurements were made 2 h before, immediately after, and 1 h after the jump. Results showed a significant increase in T-cell and NK cell numbers immediately (minutes) after the jump that was followed by a significant decrease 1 h after the jump. An early increase in plasma catecholamines preceded early increases in lymphocyte numbers, whereas the more delayed rise in plasma cortisol preceded the late decrease in lymphocyte numbers [39]. Importantly, changes in NK cell activity and antibody-dependent cell-mediated cytotoxicity closely paralleled changes in blood NK cell numbers, thus suggesting that changes in leukocyte numbers may be an important mediator of apparent changes in leukocyte ‘activity’. Similarly, Rinner et al. [43] have shown that a short stressor (1 min handling) induced an increase in mitogen-induced proliferation of T and B cells obtained from peripheral blood, while a longer stressor (2 h immobilization) induced a decrease in the same proliferative responses. In another example, Manuck et al. [44] showed that acute psychological stress induced a significant increase in blood CTL numbers only in those subjects who showed heightened catecholamine and cardiovascular reactions to stress.
Thus, an acute stress response may induce biphasic changes in blood leukocyte numbers. Soon after the beginning of stress (order of minutes) or during mild acute stress, or exercise, catecholamine hormones and neurotransmitters induce the body's ‘soldiers' (leukocytes), to exit their ‘barracks' (spleen, lung, marginated pool and other organs) and enter the ‘boulevards' (blood vessels and lymphatics). This results in an increase in blood leukocyte numbers, the effect being most prominent for NK cells and granulocytes. As the stress response continues, activation of the HPA axis results in the release of glucocorticoid hormones which induce leukocytes to exit the blood and take position at potential ‘battle stations' (such as the skin, lung, gastrointestinal and urinary-genital tracts, mucosal surfaces, and lymph nodes) in preparation for immune challenges which may be imposed by the actions of the stressor [3, 4, 45]. Such a redistribution of leukocytes results in a decrease in blood leukocyte numbers. Thus, acute stress may result in a redistribution of leukocytes from the barracks, through the boulevards, and to potential battle stations within the body.
Since the blood is the most accessible and commonly used compartment for human studies, it is important to carefully evaluate how changes in blood immune parameters might reflect in vivo immune function in the context of the specific experiments or study at hand. Moreover, since most blood collection procedures involve a certain amount of stress, since all patients or subjects will have experienced acute and chronic stress, and since many studies of psychophysiological effects on immune function focus on stress, the effects of stress on blood leukocyte distribution become a factor of considerable importance.
Dhabhar et al. [37, 46] were the first to propose that stress-induced changes in blood leukocyte distribution may represent an adaptive response. They suggested that acute stress-induced changes in blood leukocyte numbers represent a redistribution of leukocytes from the blood to organs such as the skin, draining sentinel lymph nodes, and other compartments [4, 45]. They hypothesized that such a leukocyte redistribution may enhance immune function in compartments to which immune cells traffic during stress. In agreement with this hypothesis, it was demonstrated that a stress-induced redistribution of leukocytes from the blood to the skin is accompanied by a significant enhancement of skin immunity [45,46,47].
Functional Consequences of Stress-Induced Changes in Immune Cell Distribution
When interpreting data showing stress-induced changes in functional assays such as lymphocyte proliferation or NK activity, it may be important to bear in mind the effects of stress on the leukocyte composition of the compartment in which an immune parameter is being measured. For example, it has been shown that acute stress induces a redistribution of leukocytes from the blood to the skin and that this redistribution is accompanied by a significant enhancement of skin cell-mediated immunity (CMI) [16, 45]. In what might at first glance appear to be contradicting results, acute stress has been shown to suppress splenic and peripheral blood responses to T-cell mitogens [48] and splenic IgM production [49]. However, it is important to note that in contrast to the skin that is enriched in leukocytes during acute stress, peripheral blood and spleen are relatively depleted of leukocytes during acute stress [50]. This stress-induced decrease in blood and spleen leukocyte numbers may contribute to the acute stress-induced suppression of immune function in these compartments.
Moreover, in contrast to acute stress, chronic stress has been shown to suppress skin CMI and a chronic stress-induced suppression of blood leukocyte redistribution is thought to be one of the factors mediating the immunosuppressive effect of chronic stress [9]. Again, in what might appear to be contradicting results, chronic stress has been shown to enhance mitogen-induced proliferation of splenocytes [51] and splenic IgM production [49]. However, the spleen is relatively enriched in T cells during chronic glucocorticoid administration, suggesting that it may also be relatively enriched in T cells during chronic stress [52], and this increase in spleen leukocyte numbers may contribute to the chronic stress-induced enhancement of immune parameters measured in the spleen.
It is also important to bear in mind that the heterogeneity of the stress-induced changes in leukocyte distribution [3] suggests that using equal numbers of leukocytes in a functional assay may not account for stress-induced changes in relative percentages of different leukocyte subpopulations in the cell suspension being assayed. For example, samples that have been equalized for absolute numbers of total blood leukocytes from control versus stressed animals may still contain different numbers of specific leukocyte subpopulations (e.g. T cells, B cells or NK cells). Such changes in leukocyte composition may contribute to the effects of stress even in functional assays using equalized numbers of leukocytes from different treatment groups. Therefore, stress may affect immune function at a cellular level (e.g. phagocytosis, antigen presentation, killing, antibody production) and/or through leukocyte redistribution that could increase or decrease the number of cells with a specific functional capacity in the compartment being studied.
Effects of Acute Stress on Leukocyte Trafficking to a Site of Surgery or Immune Activation
Viswanathan and Dhabhar [53] used a subcutaneously implanted surgical sponge model to elucidate the effects of stress on the kinetics, magnitude, subpopulation, and chemoattractant specificity of leukocyte trafficking to a site of immune activation or surgery. Mice that were acutely stressed before subcutaneous implantation or the surgical sponge showed a two- to threefold higher neutrophil, macrophage, NK cell and T-cell infiltration than non-stressed animals. Leukocyte infiltration was evident as early as 6 h and peaked between 24 and 48 h. Importantly, at 72 h, sponges from non-stressed and acutely stressed mice had comparable and significantly lower leukocyte numbers indicating effective resolution of inflammation in both groups. These authors also examined the effects of stress on early (6 h) leukocyte infiltration in response to a predominantly proinflammatory cytokine, tumor necrosis factor-α (TNF-α), and lymphocyte-specific chemokine, lymphotactin (LTN). Acute stress significantly increased infiltration of macrophages, in response to saline, LTN or TNF-α; neutrophils, only in response to TNF-α, and NK and T cells only in response to LTN. These results showed that acute stress significantly enhances the kinetics and magnitude of leukocyte infiltration into a site of immune activation or surgery in a subpopulation and chemoattractant-specific manner, with tissue damage, antigen-, or pathogen-driven chemoattractants synergizing with acute stress to further determine the specific subpopulations that are recruited [53]. Thus, depending on the primary chemoattractants driving an immune response, acute stress may selectively mobilize specific leukocyte subpopulations into sites of surgery, wounding, or inflammation. Such a stress-induced increase in leukocyte trafficking may be an important mechanism by which acute stressors alter the course of different (innate vs. adaptive, early vs. late, acute vs. chronic) protective or pathological immune responses.
Acute Stress-Induced Enhancement of Innate/Primary Immune Responses
In view of the skin being one of the target organs to which leukocytes traffic during stress, studies were conducted to examine whether skin immunity is enhanced when immune activation/antigen exposure occurs following a stressful experience. Studies showed that acute stress experienced at the time of novel or primary antigen exposure results in a significant enhancement of the ensuing skin immune response [16]. Compared to controls, mice restrained for 2.5 h before primary immunization with keyhole limpet hemocyanin (KLH) showed a significantly enhanced immune response when re-exposed to KLH 9 months later. This immunoenhancement was mediated by an increase in numbers of memory and effector helper T cells in sentinel lymph nodes at the time of primary immunization. Further analyses showed that the early stress-induced increase in T-cell memory may have stimulated the robust increase in infiltrating lymphocyte and macrophage numbers observed months later at a novel site of antigen re-exposure. Enhanced leukocyte infiltration was driven by increased levels of the type-1 cytokines, IL-2 and γ-interferon (IFN-γ), and TNF-α, observed at the site of antigen re-exposure in animals that had been stressed at the time of primary immunization. Given the importance of inducing long-lasting increases in immunological memory during vaccination, it has been suggested that the neuroendocrine stress response is nature's adjuvant that could be psychologically and/or pharmacologically manipulated to safely increase vaccine efficacy.
In a series of elegant experiments, Saint-Mezard et al. [54] similarly showed that acute stress experienced at the time of sensitization resulted in a significant increase in the contact hypersensitivity (CHS) response. These investigators showed that acute stress experienced during sensitization enhanced dendritic cell migration from skin to sentinel lymph nodes and also enhanced priming of lymph node CD8+ T cells. These CD8+ T cells responded in greater numbers at the site of antigen re-exposure during the recall phase of the CHS response. These studies also suggested that the effects of acute stress in this case were mediated primarily by norepinephrine [54]. Other investigators have similarly reported stress-induced enhancement of type-1 cytokine-driven CMI [55,56,57] and type-2 cytokine-driven humoral immunity [57, 58].
Viswanathan et al. [59] further elucidated the molecular and cellular mediators of the immunoenhancing effects of acute stress. They showed that compared to non-stressed mice, acutely stressed animals showed significantly greater pinna swelling, leukocyte infiltration, and upregulated macrophage chemoattractant protein-1 (MCP-1), macrophage inflammatory protein-3α (MIP-3α), IL-1α, IL-1β, IL-6, TNF-α, and IFN-γ gene expression at the site of primary antigen exposure. Stressed animals also showed enhanced maturation and trafficking of dendritic cells from skin to lymph nodes, higher numbers of activated macrophages in skin and lymph nodes, increased T-cell activation in lymph nodes, and enhanced recruitment of surveillance T cells to skin. These findings showed that important interactive components of innate (dendritic cells and macrophages) and adaptive (surveillance T cells) immunity are mediators of the stress-induced enhancement of a primary immune response. Such immunoenhancement during primary immunization may induce a long-term increase immunologic memory resulting in subsequent augmentation of the immune response during secondary antigen exposure.
In addition to elucidating mechanisms that could be targeted to reduce stress-induced exacerbation of allergic, autoimmune, and proinflammatory reactions, the above-mentioned studies provide further support for the idea that a psychophysiological stress response is nature's fundamental survival mechanism that could be therapeutically harnessed to augment immune function during vaccination, wound healing or infection.
Acute Stress-Induced Enhancement of Adaptive/Secondary Immune Responses
Studies have shown that in addition to enhancing primary cutaneous immune responses, acute stress experienced at the time of antigen re-exposure can also enhance secondary or recall responses in skin [45]. Compared to non-stressed controls, mice that were acutely stressed at the time of antigen re-exposure showed a significantly larger number of infiltrating leukocytes at the site of the immune reaction. These results demonstrated that a relatively mild behavioral manipulation can enhance an important class of immune responses that mediate harmful (allergic dermatitis) as well as beneficial (resistance to certain viruses, bacteria, and tumors) aspects of immune function.
Blecha et al. [55] reported a similar stress-induced enhancement of CHS reactions in mice, and Flint et al. [60] showed that acute stress enhanced CHS responses in both male and female mice and that immunoenhancement was partially dependent on glucocorticoid hormones, and a stress-induced enhancement of the elicitation phase of skin CMI has also been reported in hamsters [36]. Taken together, studies show that acute stress can significantly enhance the immunization/sensitization/induction as well as the re-exposure/elicitation/recall phases of skin CMI.
Hormone and Cytokine Mediators of Stress-Induced Enhancement of Immune Function
Although much work remains to be done, to identify molecular, cellular, and physiological mechanisms mediating the adjuvant-like, immunoenhancing effects of acute stress, several studies have begun to identify endocrine and immune mediators of these effects. Studies have shown that corticosterone and epinephrine are important mediators of an acute stress-induced immunoenhancement [46]. Adrenalectomy, which eliminates the glucocorticoid and epinephrine stress response, eliminated the stress-induced enhancement of skin CMI. Low-dose corticosterone or epinephrine administration significantly enhanced skin CMI [46]. In contrast, high-dose corticosterone, chronic corticosterone, or low-dose dexamethasone administration significantly suppressed skin CMI. These results suggested a novel role for adrenal stress hormones as endogenous immunoenhancing agents. They also showed that stress hormones released during a circumscribed or acute stress response may help prepare the immune system for potential challenges (e.g. wounding or infection) for which stress perception by the brain may serve as an early warning signal. Studies by Flint et al. [60] have also suggested that corticosterone is a mediator of the stress-induced enhancement of skin CHS, while Saint-Mezard et al. [54] have suggested that the adjuvant-like effects of stress on dendritic cell and CD8+ T-cell migration and function are mediated by norepinephrine.
Studies have also examined the immunological mediators of an acute stress-induced enhancement of skin immunity. Since IFN-γ is a critical cytokine mediator of CMI and delayed as well as CHS, studies were conducted to examine its role as a local mediator of the stress-induced enhancement of skin CMI [47]. The effect of acute stress on skin CMI was examined in wild-type and IFN-γ receptor gene knockout mice (IFN-γR–/–) that had been sensitized with 2,4-dinitro-1-fluorobenzene (DNFB). Acutely stressed wild-type mice showed a significantly larger CMI response than non-stressed mice. In contrast, IFN-γR–/– mice failed to show a stress-induced enhancement of skin CMI. Immunoneutralization of IFN-γ in wild-type mice significantly reduced the stress-induced enhancement of skin CMI. In addition, an inflammatory response to direct IFN-γ administration was significantly enhanced by acute stress. These results showed that IFN-γ is an important local mediator of a stress-induced enhancement of skin CMI [47]. In addition to IFN-γ, TNF-α, MCP-1, MIP-3α, IL-1, and IL-6 have also been associated with a stress-induced enhancement of the immunization/sensitization phase of skin CMI [16, 59]. It is clear that further investigation is necessary in order to identify the most important molecular, cellular and physiological mediators of a stress-induced enhancement of skin immunity.
Acute Stress Psychophysiology as an Endogenous Adjuvant
We initially suggested that just as the acute stress response prepares the cardiovascular, musculoskeletal, and neuroendocrine systems for flight or flight, it may also prepare the immune system for challenges such as wounding and infection that are likely to result due to the actions of the stressor (predator, or process of undergoing surgery) [45, 50]. Upon seeing the evidence in support of the above hypothesis, we put forth the novel hypothesis that a psychophysiological stress response is nature's fundamental survival mechanism that could be therapeutically harnessed to augment immune function during vaccination, wound healing or infection [16]. In keeping with this hypothesis, studies conducted by our group have shown that patients undergoing knee surgery, who show a robust and adaptive immune cell redistribution profile during the acute stress of surgery, also show significantly enhanced recovery. Similarly, studies conducted by Edwards et al. [61, 62] have shown that acute stressors can enhance vaccine-induced humoral and CMI in human subjects. Further research is required to test the hypothesis that behavioral and/or pharmacological induction of the acute psychophysiological stress response can be used therapeutically to enhance protective immunity during wound healing, infection, and cancer and to enhance vaccine efficacy. Such intervention is likely to allow for safe and effective enhancement of protective immunity because it would tap into the body's natural, endogenous adjuvant mechanisms to enhance immune function.
Chronic Stress Can Suppress Immunoprotection, While Enhancing Immunopathological and Immunoregulatory/Suppressive Responses
In contrast to acute stressors, chronic stress has been shown to suppress type-1 cytokine-driven protective immune responses while enhancing proinflammatory and type-2 cytokine-driven immune responses [5]. Chronic stress also appears to mobilize immunoregulatory/inhibitory mechanisms [10]. Therefore, chronic stress is likely to exacerbate proinflammatory diseases and increase susceptibility to infections and cancer. Dhabhar and McEwen [9] conducted studies designed to examine the effects of increasing the intensity and duration of acute stress as well as the transition from acute to chronic stress on skin immune function. These studies showed that acute stress administered for 2 h prior to antigenic challenge significantly enhanced skin CMI [9]. Increasing the duration of stress from 2 to 5 h produced the same magnitude immunoenhancement. Interestingly, increasing the intensity of acute stress produced a significantly larger enhancement of the CMI response that was accompanied by increasing magnitudes of leukocyte redeployment. In contrast, these studies found suppression of the skin immune response when chronic stress exposure was begun 3 weeks before sensitization and either discontinued upon sensitization, or continued an additional week until challenge, or extended for 1 week after challenge [9]. Interestingly, acute stress-induced redistribution of peripheral blood lymphocytes was attenuated with increasing duration of stressor exposure and correlated with attenuated glucocorticoid responsivity. These results suggested that stress-induced alterations in lymphocyte redeployment may play an important role in mediating the bidirectional effects of stress on cutaneous CMI [9]. An association between chronic stress and reduced skin CMI has also been reported in human subjects [63].
Given the importance of cutaneous CMI in elimination of immunoresponsive tumors like squamous cell carcinoma (SCC) [64, 65], Saul et al. [10] examined the effects of chronic stress on susceptibility to ultraviolet (UV) radiation-induced SCC. Mice were exposed to a minimal erythemal dose of UVB three times a week for 10 weeks. Half of the UVB-exposed mice were left non-stressed (i.e., they remained in their home cages) and the other half were chronically stressed (i.e., restrained during weeks 4–6). UV-induced tumors were measured weekly from week 11 through week 34, blood was collected at week 34, and tissues were collected at week 35. mRNA expression of IL-12p40, IFN-γ, IL-4, IL-10, CD3∊, and CCL27/CTACK, the skin T-cell-homing chemokine, in dorsal skin was quantified using real-time polymerase chain reaction. CD4+, CD8+, and CD25+ leukocytes were counted using immunohistochemistry and flow cytometry. Stressed mice had a shorter median time to first tumor (15 vs. 16.5 weeks) and reached 50% incidence earlier than controls (15 vs. 21 weeks). Stressed mice also had lower IFN-γ, CCL27/CTACK, and CD3∊ gene expression and lower CD4+ and CD8+ T cells infiltrating within and around tumors than non-stressed mice. In addition, stressed mice had higher numbers of tumor infiltrating and circulating CD4+CD25+ suppressor cells than non-stressed mice. These studies showed that chronic stress increased susceptibility to UV-induced SCC by suppressing skin immunity, type-1 cytokines, and protective T cells, and increasing active immunosuppression through regulatory/suppressor T cells [10]. In addition, chronic stress has also been shown to suppress several other indices of immunoprotection [15, 66] and to enhance proinflammatory and type-2 cytokine-driven conditions and disorders [7, 67].
Bidirectional Effects of Glucocorticoid Hormones on Immune Function
In contrast to the well-known immunosuppressive effects of glucocorticoids, several studies have revealed that glucocorticoid hormones also exert immunomodulating [68] and immunoenhancing effects [17, 69]. In general, pharmacological concentrations of glucocorticoids exert immunosuppressive effects, whereas under different conditions, physiologic concentrations may exert immunomodulatory, immunoenhancing, or immunosuppressive effects. It is important to recognize that the source (natural vs. synthetic) and concentration (physiologic vs. pharmacologic) of glucocorticoid hormones, the effects of other physiologic factors (hormones, cytokines, and neurotransmitters), and the state of activation of an immune parameter (naive vs. activated leukocyte, early vs. late activation, etc.) are all important factors which ultimately determine the nature of the effects of glucocorticoids on a given immune response. Immunoenhancing effects of glucocorticoids are discussed below, whereas immunosuppressive effects are discussed in the following section.
Acute stress-induced enhancement of skin CMI is mediated by adrenal stress hormones [46]. Adrenalectomy, which eliminates the glucocorticoid and epinephrine stress response, eliminated the stress-induced enhancement of skin CMI. Low-dose corticosterone or epinephrine administration significantly enhanced skin CMI and produced a significant increase in T-cell numbers in lymph nodes draining the site of the CMI reaction [46]. Moreover, simultaneous administration of these two stress hormones produced an additive increase in the skin CMI response. These results showed that hormones released during an acute stress response may help prepare the immune system for potential challenges (e.g. wounding or infection) for which stress perception by the brain may serve as an early warning signal [46].
A permissive role for glucocorticoids in antibody production was described over 30 years ago. Several investigators reported that low levels of cortisol were a necessary factor in cell culture media in order to obtain in vitro antibody production [70]. Moreover, glucocorticoids were determined to be the critical permissive component present in serum supplements of culture media, and it was suggested that variability in antibody production assays may be the result of variability of glucocorticoid content in different batches of serum [70]. Under some conditions, glucocorticoids have been shown to shift the balance of an immune response towards humoral immunity [71,72,73]. Physiological doses of glucocorticoids have been shown to enhance immunoglobulin production by mitogen-stimulated human lymphocytes in culture [74], and glucocorticoids have been shown to stimulate B-cell number and antibody production in vitro and in vivo [75].
Studies examining the effects of corticosterone on T-lymphocyte proliferation in vitro demonstrate an important mechanism by which corticosterone may mediate the enhancement of immune function [76]. These studies have shown that during the early stages of T-cell activation, low levels of corticosterone potently enhance anti-T-cell receptor (TCR)-induced lymphocyte proliferation. Furthermore, they showed that corticosterone had to be present during the process of TCR activation in order to enhance the proliferative response. Other studies have suggested that low concentration corticosterone-induced enhancement of concanavalin A-stimulated mitogenesis of splenocytes from ADX animals may be mediated by the type-1 or mineralocorticoid receptor [77]. Finally, it was shown that corticosterone increases T-cell responsiveness to IL-2 and proliferation under conditions of high cell densities in vitro, that mimic conditions that are likely to be found in lymph nodes in vivo [78]. Thus, these in vitro studies indicate a possible mechanism by which stress and stress hormones may enhance immune function in vivo.
Several lines of evidence indicate that glucocorticoid stress hormones may act synergistically with cytokines to enhance specific immune reactions. Thus, while glucocorticoids inhibit the synthesis of cytokines under some conditions, they have also been shown to induce the release and potentiate the actions of cytokines under other conditions. For example, acute psychological stress has been shown to increase circulating TNF-α, IL-1β and IL-10 levels in human subjects [14] and acute stress increases circulating IL-1β and IL-6 in rodents [79, 80]. Glucocorticoids have been shown to induce the production of migration inhibitory factor [81]. Moreover, glucocorticoids synergistically enhance the induction of acute-phase proteins by IL-1 and IL-6 [82]. Glucocorticoids similarly enhance the biological responses of other cytokines such as IL-2, IFN-γ, granulocyte colony-stimulating factor, granulocyte macrophage colony-stimulating factor, and oncostatin M [for review, see [83]].
Synergistic interactions between glucocorticoids and cytokines may be mediated by glucocorticoid-induced upregulation of cytokine receptors on target cells as determined by increased cytokine binding or cytokine receptor mRNA expression. For example, glucocorticoid-induced TNF receptor has been shown to promote survival and serve as a costimulatory receptor for T cells [84, 85], and glucocorticoids increase IL-1 binding to human peripheral blood B cells [86]. Glucocorticoids also act synergistically with IFN-γ to induce high-affinity Fcγ receptors on human monocytic cell lines [87] and stress-induced increases in endogenous glucocorticoids also appear to facilitate the expression of low-affinity Fcγ receptors on peritoneal macrophages [88]. While some studies have reported that glucocorticoids inhibit IL-2 receptor (IL-2R) expression in leukocytes [89], a recent study indicates that the reduced IL-2R expression is secondary to glucocorticoid suppression of IL-2 [90]. In contrast, studies have found a stimulating effect of glucocorticoids on IL-2 induction of IL-2R mRNA levels in several T-cell lines [91].
Several books and articles have extensively reviewed the anti-inflammatory or immunosuppressive effects of glucocorticoid hormones [92,93,94]. It is apparent from these reviews that under specific conditions, glucocorticoids have been shown to suppress immunoglobulin, prostaglandin, leukotriene, histamine, and cytokine production, neutrophil superoxide production, macrophage function, mitogen- and antigen-induced lymphocyte proliferation, lymphocyte differentiation, NK cell activity and leukocyte migration and activation. Due to their potently immunosuppressive actions, glucorticoids are widely used in the clinic as anti-inflammatory agents [93].
It has been hypothesized that an important physiologic role of endogenous glucocorticoids might be to suppress an ongoing immune response so as to prevent it from reaching levels of reactivity which might cause damage to self [21, 92, 95, 96]. Strong support for this hypothesis comes from studies that show that adrenalectomized rats die within 24–48 h after being immunized with horse serum or Freund's complete adjuvant, but they can be rescued by corticosterone replacement therapy [97]. A number of studies involving animal models of inflammatory disorders and autoimmune disease also lend support for this hypothesis [73]. These studies have demonstrated the existence of a negative feedback loop between the immune system and the HPA axis, such that proinflammatory mediators arising from an ongoing immune reaction stimulate the HPA axis [92, 98, 99], which in turn results in the secretion of corticosterone which suppresses the immune response and prevents it from potentially damaging the host. The protective effects of immunosuppression by endogenous glucocorticoids are discussed below.
Immunomodulatory Effects of Timing of Stress or Stress Hormone Administration Relative to the Timing of Immune Activation and the Time Course of the Ensuing Immune Response
Under certain conditions, physiological levels of endogenous glucocorticoids have immunoenhancing effects while under other conditions similar hormone levels suppress autoimmune and inflammatory reactions. We hypothesize that these differential effects are achieved by differences in overall glucocorticoid sensitivity or receptivity of the immune response being affected. At the very beginning of an immune response, certain components such as leukocyte trafficking, antigen presentation, helper T-cell function, leukocyte proliferation, cytokine and chemokine function, and effector cell function may all be receptive to glucocorticoid-mediated immunoenhancement. In contrast, at a later, more advanced stage of an immune response these components may be more receptive to glucocorticoid-mediated immunosuppression. While this hypothesis needs to be tested through further experiments, examples from studies showing temporal differences in the sensitivity of immune reactions to the effects of physiologic concentrations of glucocorticoid hormones are presented below.
Studies examining the effects of corticosterone on T-lymphocyte proliferation in vitro support the hypothesis that there may be temporal differences in the receptivity of an immune response to the enhancing versus suppressive effects of endogenous glucocorticoid hormones [76]. These studies have shown that during the early stages of T-cell activation, low levels of corticosterone potently enhance anti-TCR-induced lymphocyte proliferation. However, during later stages of culture, the same levels of corticosterone suppress T-lymphocyte proliferation. Furthermore, Wiegers et al. [76] showed that corticosterone had to be present during the process of TCR activation in order to enhance the proliferative response. If corticosterone was added to the culture system more than 2 h after the initiation of TCR activation, the enhancement of lymphoproliferation was not observed.
Interestingly, Wiegers and Reul [for review, see [83]] have shown that these bidirectional effects of corticosterone on different stages of T-lymphocyte proliferation are mediated by opposing effects of corticosterone on IL-2R versus the cytokine itself. Thus, during the early stages of lymphocyte proliferation, corticosterone induces an increase in IL-2Rα expression. This increases the IL-2 receptivity of lymphocytes and is reflected by an increase in lymphocyte proliferation [76]. Although corticosterone reduces the production of IL-2 under these conditions, this decrease is not rate-limiting at this stage since exogenously added IL-2 fails to increase proliferation. However, if corticosterone is administered at later stages, the enhancement in IL-2R expression is absent, while the suppression of IL-2 production is still present. Under these conditions, the availability of IL-2 does become rate-limiting and hence corticosterone suppresses the lymphoproliferative response. Thus, these studies indicate an important mechanism mediating an endogenous glucocorticoid-induced immunoenhancement during the early stages, and an endogenous glucocorticoid-induced immunosuppression during the later stages of an immune response.
In a series of seminal studies, Sternberg et al. [21, 100, 101] showed that decreased HPA axis reactivity to inflammatory stimuli results in increased susceptibility to experimental arthritis. A similar role for HPA axis-mediated endogenous immunoregulation has been shown for development of autoimmune thyroiditis, lupus erythematosus, and avian scleroderma in obese-strain (OS) chickens [102]. Sternberg et al. [21, 95, 96, 100] investigated the influence of the HPA axis on the development of streptococcal cell wall (SCW)-induced arthritis in female rats belonging to the genetically related Lewis/N (LEW/N) and Fischer 344/N (F344/N) strains. The F344/N strain is resistant to the development of SCW-induced arthritis, whereas the LEW/N strain is susceptible. Interestingly, the F344/N strain mounts a significantly greater corticosterone and ACTH response than the LEW/N strain when challenged with a variety of stressors or with inflammatory mediators like SCW peptidoglycan polysaccharide, or IL-1α [20, 21, 23, 100], and compared to the F344 strain, the LEW strain shows a significantly greater habituation or adaptation to an acute or chronic stressor [22]. F344/N rats treated with the glucocorticoid receptor antagonist, RU-486, are rendered susceptible to SCW-induced arthritis indicating that they do carry the immune response genes with potential for triggering autoimmunity [21, 100]. Conversely, LEW rats treated with pharmacologic doses of dexamethasone become completely resistant to the development of SCW-induced arthritis [21, 100]. Furthermore, compared to F344 rats, adrenal steroid receptors in neural and immune tissues of LEW rats show a significantly lower magnitude of activation in response to stress-induced increases in plasma corticosterone [20, 23]. Thus, strain differences in plasma corticosterone levels are also manifest as significant differences in the extent of activation of corticosterone receptors in target tissues.
Experimental allergic encephalomyelitis (EAE) is another animal model of an autoimmune disease in which a similar immunosuppressive role for the HPA axis has been proposed [for review, see [73]]. The LEW strain shows a greater susceptibility to EAE [73]. MacKenzie et al. [103] have suggested that during the preclinical phase of EAE, elevations in plasma corticosterone may regulate the lymphoproliferative stage of the disease, and that during the clinical phase of the disease, elevations in plasma corticosterone as well as splenic norepinephrine may regulate other recovery-oriented immune mechanisms. Similar correlations between HPA axis hyporeactivity and susceptibility to autoimmune disease have been observed for autoimmune conditions in chickens [102]. In an elegant series of studies using an EAE model, del Rey et al. [104] demonstrated that a proinflammatory/autoimmune response itself stimulates the HPA axis primarily through cytokines like IL-1, and that HPA axis activation is independent of the stress and discomfort associated with EAE-induced paralysis.
Complementing these preclinical studies, a series of elegantly conducted clinical studies [105, 106] have shown that patients with atopic dermatitis [107] and asthma [108] show decreased reactivity of their HPA axis [109]. A more complex role for sympathetic nervous system involvement in autoimmune disease has also been proposed [110].
Glucocorticoid hormones may exert their protective immunosuppressive effects by inhibiting the production or actions of proinflammatory molecules as discussed previously. In addition, it has been hypothesized that glucocorticoids may suppress certain autoimmune reactions by inducing a shift towards a Th2 or humoral immune response [67, 73, 111]. For example, stimulation of the HPA axis by inflammatory mediators released during the initiation of an autoimmune response results in increased plasma corticosterone. Increased corticosterone levels may shift the balance of the ongoing immune reaction from a Th1-directed (cell-mediated) response towards a Th2-directed (antibody-mediated) response, by promoting the production of IL-4 and suppressing the production of IL-2 [71].
The Stress-Immune Spectrum
It is often overlooked that a stress response has salubrious adaptive effects in the short run [3, 16, 17, 45, 46, 53, 69], although stress can be harmful when it is long-lasting [1, 5, 9]. In order to reconcile these seemingly contradictory effects of stress, we proposed that a stress response and its effects on immune function be viewed in the context of a stress spectrum[4, 9] (fig. 2). One region of this spectrum is characterized by acute stress or eustress, i.e., conditions of short-duration stress that may result in immunopreparatory or immunoenhancing physiological conditions. An important characteristic of acute stress is a rapid physiological stress response mounted in the presence of the stressor, followed by a rapid shutdown of the response upon cessation of the stressor. The other region of the stress spectrum is characterized by chronic stress or distress, i.e., repeated or prolonged stress which may result in dysregulation or suppression of immune function. An important characteristic of chronic stress is that the physiological response either persists long after the stressor has ceased, or is activated repeatedly to result in an overall integrated increase in exposure of the organism to stress hormones. The concept of ‘allostatic load’ has been proposed to define the ‘psychophysiological wear and tear’ that takes place while different biological systems work to stay within a range of equilibrium (allostasis) in response to demands placed by internal or external chronic stressors [for review, see [1, 12]]. We suggest that conditions of high allostatic load would result in dysregulation or suppression of immune function. Importantly, a disruption of the circadian corticosterone/cortisol rhythm may be an indicator and/or mediator of distress or high allostatic load [9]. The stress spectrum also proposes that acute or chronic stress is generally superimposed on a psychophysiological health maintenance equilibrium (fig. 2). The extent and efficiency with which an organism returns to its health maintenance equilibrium after stress depends on resilience, which we define as reserve capacity of psychophysiological systems to recover from challenging conditions (fig. 2). Factors such as coping mechanisms, sense of control, optimism, social support, early life experiences, learning, genetics, and sleep may be important mediators of psychological resilience (fig. 2). Factors such as neuroendocrine reactivity, genetics, environment, nutrition, and sleep may be important mediators of physiological resilience (fig. 2). The psychophysiological basis of resilience and reserve capacity are underinvestigated and provide an important opportunity for future research.
Fig. 2.
The stress spectrum model. We have proposed a definition of stress as a constellation of events, consisting of a stimulus (stressor), that precipitates a reaction in the brain (stress perception & processing), that activates physiologic fight-or-flight systems in the body (physiological stress response) [9] . The duration of a physiological stress response is the critical determinant of its effects on immune function and health. The stressor itself may be acute (e.g. narrowly missing being hit by a car) or chronic (e.g. caring for a chronicallyill child, spouse or parent). Stress perception and processing by the brain are critical for determining the duration and magnitude of the physiological stress response stimulated by any given stressor. Acute or chronic stress is generally superimposed on a psychophysiological health maintenance steady state. The extent and efficiency with which an organism returns to its health maintenance steady state after stress depends on resilience, which we define as the capacity of psychological and interacting physiological systems to recover from challenging conditions. Factors such as coping mechanisms, sense of control, optimism, social support, early life experiences, learning, genetics, and sleep are important mediators of psychological resilience . Factors such as neuroendocrine reactivity, genetics, environment, nutrition, and sleep are important mediators of physiological resilience . Psychological resilience mechanisms are especially important in humans because they can limit the duration and magnitude of chronic stress responses. By the same token, psychogenic stressors can be particularly detrimental in human subjects because they may generate stress responses long after stressor exposure or even in the absence of physical stressors or salient threats. The physiological stress response is the ultimate effector arm of the stress spectrum. It may consist of acute or chronic physiological activation (neurotransmitters, hormones, and their molecular, cellular, organ-level and systemic effects) that results in psychophysiological states that have different effects on health. Acute stress generally results in activation of mechanisms that include enhancement of immune function, while chronic stress results in health-aversive conditions that result in dysregulation or suppression of immune function. The molecular mechanisms me diating conversion from positive to negative effects of stress on immune function and health are slowly beginning to emerge, and merit further investigation. Reprinted from Dhabhar and McEwen [17], with permission.
The stress spectrum, taken together with the preceding discussion, shows that the duration, intensity/concentration, and timing of exposure to stressor-induced physiological activation (neurotransmitters, hormones, and their molecular, cellular, organ-level and systemic effects) are critical for determining whether stress will enhance or suppress/dysregulate immune function. The model shows that the stressor itself can be acute or chronic (fig. 2). Stress perception and processing by the brain and mechanisms mediating psychological and physiological resilience are critical for determining the duration and magnitude of the physiological stress response (fig. 2). Psychological resilience mechanisms are especially important in humans because they can limit the duration and magnitude of chronic stress responses. Psychogenic stressors are also very important in human subjects because they can generate stress responses long after stressor exposure (e.g. posttraumatic stress disorder following a severe traumatic experience, or in a milder form, lingering anger/mood disturbance following a social altercation) or even in the absence of a physical stressor or salient threat (e.g. worrying about whether one's romantic feelings will be reciprocated). Therefore, following stressor exposure and its processing by the brain, there ensues a physiological stress response. This response may consist of acute or chronic physiological activation (neurotransmitters, hormones, and their molecular, cellular, organ-level and systemic effects) which results in psychophysiological states that have different effects on overall health and immune function as shown in figure 2. While there is significant evidence from animal studies to support this model, it needs to be further examined in studies involving human subjects.
Conclusion
Stress has long been suspected to play a role in the etiology of many diseases, and numerous studies have shown that stress can be immunosuppressive and hence may be detrimental to health. Moreover, glucocorticoid stress hormones are widely regarded as being immunosuppressive, and are used clinically as anti-inflammatory agents. However, studies have shown that the acute stress response may play a critical adaptive and protective role, with stress hormones and neurotransmitters preparing the immune system for potential challenges (e.g. wounding or infection) that are perceived by the brain (e.g. the detection of predator or attacker) [9, 16, 37, 45, 53]. It may be useful to further study, and clinically harness, the acute stress response that evolution has finely sculpted to be one of nature's crucial survival mechanisms, at least as much as we study its maladaptive ramifications (chronic stress) that evolution yet has to catch up with.
This paper illustrates the complex role that stress and stress hormones play as modulators and regulators of an immune response. Stress and glucocorticoid hormones can either enhance or suppress immune function depending on the following factors: (1) The duration (acute vs. chronic) of stress. (2) Changes in leukocyte distribution within the body, and the compartments in which the immune response occurs. (3) The concentration (physiologic vs. pharmacologic), duration (acute vs. chronic) and nature (endogenous vs. synthetic) of glucocorticoid hormone exposure. (4) The timing of stress or stress hormone exposure relative to the stage (early vs. late) of an immune response. Further elucidation of the interactions among the above-mentioned factors and other nervous, endocrine, and genetic factors in mediating the effects of stress on immune function is necessary. Importantly, whether a stressor enhances or suppresses immune function, it is the end-effect of the affected immune response that affects the health of the organism or individual. For example, stress-induced enhancement of immunoprotective responses is likely to be beneficial while stress-induced enhancement of immunopathology is harmful. These findings need to be explored and investigated further and translated from bench to bedside.
It is important to recognize that humans as well as animals experience stress as an intrinsic part of life, and in conjunction with many standard diagnostic, clinical, and experimental manipulations. Unintended stressors may significantly affect these measures and overall health outcomes. Thus, when conducting clinical, diagnostic, or experimental procedures, it may be important to account for the effects of stress on the specific physiologic parameter or health outcome being measured. For example, it is critical to elucidate and account for the effects of stress and/or stress hormones on changes in leukocyte distribution within different body compartments. Where possible, redistribution needs to be monitored in terms of changes in absolute numbers of specific subpopulations of leukocytes. Stress-induced changes in immune cell numbers and/or function could significantly affect results (in case of experiments), diagnosis (in case of medical tests), or outcome (in case of treatment procedures and surgery).
Due to a host of psycho-sociopolitical factors, stress has unfortunately become an increasing and inevitable part of people's lives. Stress is also a major factor during the diagnosis, treatment, and follow-up for most diseases. Chronic stress has been shown to dysregulate immune function and is thought to play a role in the etiology of many diseases. In contrast, it has been shown that activation of acute stress physiology may enhance protective immune responses [3, 16, 45, 59]. We propose that it is important to further study, and clinically harness the immunological effects of the acute stress response, that evolution has finely sculpted as a survival mechanism, just as we study its maladaptive ramifications (chronic stress) that evolution has yet to resolve. A determination of the physiologic mechanisms through which stress and stress hormones enhance or suppress immune responses is critically important for elucidating risk, developing preventative and therapeutic interventions, and optimizing a patient's response to treatment. The elucidation of such mechanisms would facilitate development of biomedical treatments designed to harness an individual's physiology to selectively enhance (during vaccination, wounding, infections, or cancer) or suppress (during autoimmune or inflammatory disorders) the immune response depending on the outcome most beneficial for the patient.
Acknowledgements
I wish to thank current and previous members of my laboratory, particularly, Jean Tillie, Dr. Kavitha Viswanathan, Dr. Alison Saul, Kanika Ghai, and Christine Daugherty, whose work and publications are among those discussed in this chapter. The work described here was supported by grants from the NIH (AI48995 and CA107498) and The Dana Foundation.
References
- 1.McEwen BS. Protective and damaging effects of stress mediators: allostasis and allostatic load. N Engl J Med. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 2.Ader R. Psychoneuroimmunology. ed 4. San Diego: Academic Press; 2006. [Google Scholar]
- 3.Dhabhar FS, Miller AH, McEwen BS, Spencer RL. Effects of stress on immune cell distribution – dynamics and hormonal mechanisms. J Immunol. 1995;154:5511–5527. [PubMed] [Google Scholar]
- 4.Dhabhar FS, McEwen BS. Bidirectional effects of stress and glucocorticoid hormones on immune function: possible explanations for paradoxical observations. In: Ader R, Felten DL, Cohen N, editors. Psychoneuroimmunology. ed 3. San Diego: Academic Press; 2001. pp. 301–338. [Google Scholar]
- 5.Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol. 2005;5:243–251. doi: 10.1038/nri1571. [DOI] [PubMed] [Google Scholar]
- 6.Chrousos GP, Kino T. Glucocorticoid action networks and complex psychiatric and/or somatic disorders. Stress. 2007;10:213–219. doi: 10.1080/10253890701292119. [DOI] [PubMed] [Google Scholar]
- 7.Glaser R, MacCallum RC, Laskowski BF, Malarkey WB, Sheridan JF, Kiecolt-Glaser JK. Evidence for a shift in the Th1 to Th2 cytokine response associated with chronic stress and aging. J Gerontol A Biol Sci Med Sci. 2001;56:M477–M482. doi: 10.1093/gerona/56.8.m477. [DOI] [PubMed] [Google Scholar]
- 8.Epel E, Blackburn EH, Lin J, Dhabhar FS, Adler NE, Morrow JD, Cawthon RM. Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci USA. 2004;101:17312–17315. doi: 10.1073/pnas.0407162101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dhabhar FS, McEwen BS. Acute stress enhances while chronic stress suppresses immune function in vivo: a potential role for leukocyte trafficking. Brain Behav Immun. 1997;11:286–306. doi: 10.1006/brbi.1997.0508. [DOI] [PubMed] [Google Scholar]
- 10.Saul AN, Oberyszyn TM, Daugherty C, Kusewitt D, Jones S, Jewell S, Malarkey WB, Lehman A, Lemeshow S, Dhabhar FS. Chronic stress and susceptibility to skin cancer. J Nat Cancer Inst. 2005;97:1760–1767. doi: 10.1093/jnci/dji401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldstein DS, McEwen B. Allostasis, homeostats, and the nature of stress. Stress. 2002;5:55–58. doi: 10.1080/102538902900012345. [DOI] [PubMed] [Google Scholar]
- 12.McEwen BS. The End of Stress as We Know It. Washington: Dana Press; 2002. [Google Scholar]
- 13.Sapolsky RM. The influence of social hierarchy on primate health. Science. 2005;308:648–652. doi: 10.1126/science.1106477. [DOI] [PubMed] [Google Scholar]
- 14.Altemus M, Rao B, Dhabhar FS, Ding W, Granstein R. Stress-induced changes in skin barrier function in healthy women. J Invest Dermatol. 2001;117:309–317. doi: 10.1046/j.1523-1747.2001.01373.x. [DOI] [PubMed] [Google Scholar]
- 15.Irwin M, Patterson T, Smith TL, Caldwell C, Brown SA, Gillin CJ, Grant I. Reduction of immune function in life stress and depression. Biol Psychiatry. 1990;27:22–30. doi: 10.1016/0006-3223(90)90016-u. [DOI] [PubMed] [Google Scholar]
- 16.Dhabhar FS, Viswanathan K. Short-term stress experienced at the time of immunization induces a long-lasting increase in immunological memory. Am J Physiol. 2005;289:R738–R744. doi: 10.1152/ajpregu.00145.2005. [DOI] [PubMed] [Google Scholar]
- 17.Dhabhar FS, McEwen BS. Bidirectional effects of stress on immune function: possible explanations for salubrious as well as harmful effects. In: Ader R, editor. Psychoneuroimmunology. ed 4. San Diego: Elsevier; 2007. pp. 723–760. [Google Scholar]
- 18.Sephton S, Spiegel D. Circadian disruption in cancer: a neuroendocrine-immune pathway from stress to disease? Brain Behav Immun. 2003;17:321–328. doi: 10.1016/s0889-1591(03)00078-3. [DOI] [PubMed] [Google Scholar]
- 19.Gunnar M, Quevedo K. The neurobiology of stress and development. Annu Rev Psychol. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- 20.Dhabhar FS, McEwen BS, Spencer RL. Stress response, adrenal steroid receptor levels, and corticosteroid-binding globulin levels – a comparison between Sprague-Dawley, Fischer 344, and Lewis rats. Brain Res. 1993;616:89–98. doi: 10.1016/0006-8993(93)90196-t. [DOI] [PubMed] [Google Scholar]
- 21.Sternberg EM, Hill JM, Chrousos GP, Kamilaris T, Listwak SJ, Gold PW, Wilder RL. Inflammatory mediator-induced hypothalamic-pituitary-adrenal axis activation is defective in streptococcal cell wall arthritis-susceptible Lewis rats. Proc Natl Acad Sci USA. 1989;86:2374–2378. doi: 10.1073/pnas.86.7.2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dhabhar FS, McEwen BS, Spencer RL. Adaptation to prolonged or repeated stress – comparison between rat strains showing intrinsic differences in reactivity to acute stress. Neuroendocrinology. 1997;65:360–368. doi: 10.1159/000127196. [DOI] [PubMed] [Google Scholar]
- 23.Dhabhar FS, Miller AH, McEwen BS, Spencer RL. Differential activation of adrenal steroid receptors in neural and immune tissues of Sprague-Dawley, Fischer 344, and Lewis rats. J Neuroimmunol. 1995;56:77–90. doi: 10.1016/0165-5728(94)00135-b. [DOI] [PubMed] [Google Scholar]
- 24.Gomez-Serrano M, Tonelli L, Listwak S, Sternberg E, Riley AL. Effects of cross-fostering on open-field behavior, acoustic startle, lipopolysaccharide-induced corticosterone release, and body weight in Lewis and Fischer rats. Behav Genet. 2001;31:427–436. doi: 10.1023/a:1012742405141. [DOI] [PubMed] [Google Scholar]
- 25.Schwab CL, Fan R, Zheng Q, Myers LP, Hebert P, Pruett SB. Modeling and predicting stress-induced immunosuppression in mice using blood parameters. Toxicol Sci. 2005;83:101–113. doi: 10.1093/toxsci/kfi014. [DOI] [PubMed] [Google Scholar]
- 26.Benschop RJ, Rodriguez-Feuerhahn M, Schedlowski M. Catecholamine-induced leukocytosis: early observations, current research, and future directions. Brain Behav Immun. 1996;10:77–91. doi: 10.1006/brbi.1996.0009. [DOI] [PubMed] [Google Scholar]
- 27.Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444:875–880. doi: 10.1038/nature05487. [DOI] [PubMed] [Google Scholar]
- 28.Dantzer R, O'Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maes MA. A review on the acute phase response in major depression. Rev Neurosci. 1993;4:407–416. doi: 10.1515/revneuro.1993.4.4.407. [DOI] [PubMed] [Google Scholar]
- 30.Bluestone JA, Tang Q. How do CD4+CD25+ regulatory T cells control autoimmunity? Curr Opin Immunol. 2005;17:638–642. doi: 10.1016/j.coi.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 31.Finn OJ. Cancer immunology. N Engl J Med. 2008;358:2704–2715. doi: 10.1056/NEJMra072739. [DOI] [PubMed] [Google Scholar]
- 32.Sprent J, Tough DF. Lymphocyte lifespan and memory. Science. 1994;265:1395–1400. doi: 10.1126/science.8073282. [DOI] [PubMed] [Google Scholar]
- 33.Hoagland H, Elmadjian F, Pincus G. Stressful psychomotor performance and adrenal cortical function as indicated by the lymphocyte response. J Clin Endocrinol. 1946;6:301–311. doi: 10.1210/jcem-6-4-301. [DOI] [PubMed] [Google Scholar]
- 34.Fauci AS, Dale DC. The effect of in vivo hydrocortisone on subpopulations of human lymphocytes. J Clin Invest. 1974;53:240–246. doi: 10.1172/JCI107544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dhabhar FS, Miller AH, McEwen BS, Spencer RL. Stress-induced changes in blood leukocyte distribution – role of adrenal steroid hormones. J Immunol. 1996;157:1638–1644. [PubMed] [Google Scholar]
- 36.Bilbo SD, Dhabhar FS, Viswanathan K, Saul A, Yellon SM, Nelson RJ. Short day lengths augment stress-induced leukocyte trafficking and stress-induced enhancement of skin immune function. Proc Natl Acad Sci USA. 2002;99:4067–4072. doi: 10.1073/pnas.062001899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dhabhar FS, Miller AH, Stein M, McEwen BS, Spencer RL. Diurnal and stress-induced changes in distribution of peripheral blood leukocyte subpopulations. Brain Behav Immun. 1994;8:66–79. doi: 10.1006/brbi.1994.1006. [DOI] [PubMed] [Google Scholar]
- 38.Morrow-Tesch JL, McGlone JJ, Norman RL. Consequences of restraint stress on natural killer cell activity, behavior, and hormone levels in rhesus macaques (Macaca mulatta) Psychoneuroendocrinology. 1993;18:383–395. doi: 10.1016/0306-4530(93)90013-b. [DOI] [PubMed] [Google Scholar]
- 39.Schedlowski M, Jacobs R, Stratman G, Richter S, Hädike A, Tewes U, Wagner TOF, Schmidt RE. Changes of natural killer cells during acute psychological stress. J Clin Immunol. 1993;13:119–126. doi: 10.1007/BF00919268. [DOI] [PubMed] [Google Scholar]
- 40.Redwine L, Mills PJ, Sada M, Dimsdale J, Patterson T, Grant I. Differential immune cell chemotaxis responses to acute psychological stress in Alzheimer caregivers compared to non-caregiver controls. Psychosom Med. 2004;66:770–775. doi: 10.1097/01.psy.0000138118.62018.87. [DOI] [PubMed] [Google Scholar]
- 41.Naliboff BD, Benton D, Solomon GF, Morley JE, Fahey JL, Bloom ET, Makinodan T, Gilmore SL. Immunological changes in young and old adults during brief laboratory stress. Psychosom Med. 1991;53:121–132. doi: 10.1097/00006842-199103000-00002. [DOI] [PubMed] [Google Scholar]
- 42.Mills PJ, Berry CC, Dimsdale JE, Ziegler MG, Nelesen RA, Kennedy BP. Lymphocyte subset redistribution in response to acute experimental stress: effects of gender, ethnicity, hypertension, and the sympathetic nervous system. Brain Behav Immun. 1995;9:61–69. doi: 10.1006/brbi.1995.1006. [DOI] [PubMed] [Google Scholar]
- 43.Rinner I, Schauenstein K, Mangge H, Porta S, Kvetnansky R. Opposite effects of mild and severe stress on in vitro activation of rat peripheral blood lymphocytes. Brain Behav Immun. 1992;6:130–140. doi: 10.1016/0889-1591(92)90013-e. [DOI] [PubMed] [Google Scholar]
- 44.Manuck SB, Cohen S, Rabin BS, Muldoon MF, Bachen EA. Individual differences in cellular immune response to stress. Psychol Science. 1991;2:111–115. [Google Scholar]
- 45.Dhabhar FS, McEwen BS. Stress-induced enhancement of antigen-specific cell-mediated immunity. J Immunol. 1996;156:2608–2615. [PubMed] [Google Scholar]
- 46.Dhabhar FS, McEwen BS. Enhancing versus suppressive effects of stress hormones on skin immune function. Proc Natl Acad Sci USA. 1999;96:1059–1064. doi: 10.1073/pnas.96.3.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dhabhar FS, Satoskar AR, Bluethmann H, David JR, McEwen BS. Stress-induced enhancement of skin immune function: a role for IFN-γ. Proc Natl Acad Sci USA. 2000;97:2846–2851. doi: 10.1073/pnas.050569397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cunnick JE, Lysle DT, Kucinski BJ, Rabin BS. Evidence that shock-induced immune suppression is mediated by adrenal hormones and peripheral β-adrenergic receptors. Pharmacol Biochem Behav. 1990;36:645–651. doi: 10.1016/0091-3057(90)90270-r. [DOI] [PubMed] [Google Scholar]
- 49.Zalcman S, Anisman H. Acute and chronic stressor effects on the antibody response to sheep red blood cells. Pharmacol Biochem Behav. 1993;46:445–452. doi: 10.1016/0091-3057(93)90377-6. [DOI] [PubMed] [Google Scholar]
- 50.Dhabhar FS. Stress-induced enhancement of cell-mediated immunity. Ann NY Acad Sci. 1998;840:359–372. doi: 10.1111/j.1749-6632.1998.tb09575.x. [DOI] [PubMed] [Google Scholar]
- 51.Monjan AA, Collector MI. Stress-induced modulation of the immune response. Science. 1977;196:307–308. doi: 10.1126/science.557841. [DOI] [PubMed] [Google Scholar]
- 52.Miller AH, Spencer RL, Hasset J, Kim C, Rhee R, Cira D, Dhabhar FS, McEwen BS, Stein M. Effects of selective type I and type II adrenal steroid receptor agonists on immune cell distribution. Endocrinology. 1994;135:1934–1944. doi: 10.1210/endo.135.5.7956914. [DOI] [PubMed] [Google Scholar]
- 53.Viswanathan K, Dhabhar FS. Stress-induced enhancement of leukocyte trafficking into sites of surgery or immune activation. Proc Natl Acad Sci USA. 2005;102:5808–5813. doi: 10.1073/pnas.0501650102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Saint-Mezard P, Chavagnac C, Bosset S, Ionescu M, Peyron E, Kaiserlian D, Nicolas JF, Berard F. Psychological stress exerts an adjuvant effect on skin dendritic cell functions in vivo. J Immunol. 2003;171:4073–4080. doi: 10.4049/jimmunol.171.8.4073. [DOI] [PubMed] [Google Scholar]
- 55.Blecha F, Barry RA, Kelley KW. Stress-induced alterations in delayed-type hypersensitivity to SRBC and contact sensitivity to DNFB in mice. Proc Soc Exp Biol Med. 1982;169:239–246. doi: 10.3181/00379727-169-41338. [DOI] [PubMed] [Google Scholar]
- 56.Coe CL, Lubach G, Ershler WB. Immunological consequences of maternal separation in infant primates. In: Lewis M, Worobey J, editors. Infant Stress and Coping. vol 45. New York: Jossey-Bass; 1989. [DOI] [PubMed] [Google Scholar]
- 57.Wood PG, Karol MH, Kusnecov AW, Rabin BS. Enhancement of antigen-specific humoral and cell-mediated immunity by electric footshock stress in rats. Brain Behav Immun. 1993;7:121–134. doi: 10.1006/brbi.1993.1014. [DOI] [PubMed] [Google Scholar]
- 58.Cocke R, Moynihan JA, Cohen N, Grota LJ, Ader R. Exposure to conspecific alarm chemosignals alters immune responses in Balb/c mice. Brain Behav Immun. 1993;7:36–46. doi: 10.1006/brbi.1993.1004. [DOI] [PubMed] [Google Scholar]
- 59.Viswanathan K, Daugherty C, Dhabhar FS. Stress as an endogenous adjuvant: augmentation of the immunization phase of cell-mediated immunity. Int Immunol. 2005;17:1059–1069. doi: 10.1093/intimm/dxh286. [DOI] [PubMed] [Google Scholar]
- 60.Flint MS, Miller DB, Tinkle SS. Restraint-induced modulation of allergic and irritant contact dermatitis in male and female B6.129 mice. Brain Behav Immun. 2000;14:256–269. doi: 10.1006/brbi.2000.0604. [DOI] [PubMed] [Google Scholar]
- 61.Edwards KM, Burns VE, Reynolds T, Carroll D, Drayson M, Ring C. Acute stress exposure prior to influenza vaccination enhances antibody response in women. Brain Behav Immun. 2006;20:159–168. doi: 10.1016/j.bbi.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 62.Edwards KM, Burns VE, Adkins AE, Carroll D, Drayson M, Ring C. Meningococcal A vaccination response is enhanced by acute stress in men. Psychosom Med. 2008;70:147–151. doi: 10.1097/PSY.0b013e318164232e. [DOI] [PubMed] [Google Scholar]
- 63.Smith A, Vollmer-Conna U, Bennett B, Wakefield D, Hickie I, Lloyd A. The relationship between distress and the development of a primary immune response to a novel antigen. Brain Behav Immun. 2004;18:65–75. doi: 10.1016/s0889-1591(03)00107-7. [DOI] [PubMed] [Google Scholar]
- 64.Kripke ML. Ultraviolet radiation and immunology: something new under the sun – presidential address. Cancer Res. 1994;54:6102–6105. [PubMed] [Google Scholar]
- 65.Granstein RD, Matsui MS. UV radiation-induced immunosuppression and skin cancer. Cutis. 2004;74:4–9. [PubMed] [Google Scholar]
- 66.Bonneau RH, Sheridan JF, Feng N, Glaser R. Stress-induced effects on cell-mediated innate and adaptive memory components of the murine immune response to herpes simplex virus infection. Brain Behav Immun. 1991;5:274–295. doi: 10.1016/0889-1591(91)90023-4. [DOI] [PubMed] [Google Scholar]
- 67.Elenkov IJ. Glucocorticoids and the Th1/Th2 balance. Ann NY Acad Sci. 2004;1024:138–146. doi: 10.1196/annals.1321.010. [DOI] [PubMed] [Google Scholar]
- 68.Wilckens T, DeRijk R. Glucocorticoids and immune function: unknown dimensions and new frontiers. Immunol Today. 1997;18:418–424. doi: 10.1016/s0167-5699(97)01111-0. [DOI] [PubMed] [Google Scholar]
- 69.Dhabhar FS. Enhancing versus suppressive effects of stress on immune function: implications for immunoprotection versus immunopathology. Allergy Asthma Clin Immunol. 2008;4:2–11. doi: 10.1186/1710-1492-4-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Halliday WJ, Garvey JS. Some factors affecting the secondary immune response in tissue cultures containing hydrocortisone. J Immunol. 1964;93:757–762. [PubMed] [Google Scholar]
- 71.Danes RA, Araneo BA. Contrasting effects of glucocorticoids on the capacity of T cells to produce the growth factors interleukin-2 and interleukin-4. Eur J Immunol. 1989;19:2319–2325. doi: 10.1002/eji.1830191221. [DOI] [PubMed] [Google Scholar]
- 72.Mosmann TR, Coffman RL. Th1 and Th2 cells: different patterns of lymphokine secretion lead to different functional properties. Ann Rev Immunol. 1989;7:145–173. doi: 10.1146/annurev.iy.07.040189.001045. [DOI] [PubMed] [Google Scholar]
- 73.Mason D. Genetic variation in the stress response: susceptibility to experimental allergic encephalomyelitis and implications for human inflammatory disease. Immunol Today. 1991;12:57–60. doi: 10.1016/0167-5699(91)90158-P. [DOI] [PubMed] [Google Scholar]
- 74.Grayson J, Dooley NJ, Koski IR, Blaese RM. Immunoglobulin production induced in vitro by glucocorticoid hormones: T-cell-dependent stimulation of immunoglobulin production without B-cell proliferation in cultures of human peripheral blood lymphocytes. J Clin Invest. 1981;68:1539–1547. doi: 10.1172/JCI110408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Plaut M. Lymphocyte hormone receptors. Annu Rev Immunol. 1987;5:621–669. doi: 10.1146/annurev.iy.05.040187.003201. [DOI] [PubMed] [Google Scholar]
- 76.Wiegers GJ, Labeur MS, Stec IE, Klinkert WE, Holsboe RF, Reul JM. Glucocorticoids accelerate anti-T-cell receptor-induced T-cell growth. J Immunol. 1995;155:1893–1902. [PubMed] [Google Scholar]
- 77.Wiegers GJ, Reul JMHM, Holsboer F, De Kloet ER. Enhancement of rat splenic lymphocyte mitogenesis after short-term exposure to corticosteroids in vitro. Endocrinology. 1994;135:2351–2357. doi: 10.1210/endo.135.6.7988417. [DOI] [PubMed] [Google Scholar]
- 78.Wiegers GJ, Stec IE, Klinkert WE, Linthorst AC, Reul JM. Bidirectional effects of corticosterone on splenic T-cell activation: critical role of cell density and culture time. Neuroendocrinology. 2001;73:139–148. doi: 10.1159/000054630. [DOI] [PubMed] [Google Scholar]
- 79.Mekaouche M, Givalois L, Barbanel G, Siaud P, Maurel D, Malaval F, Bristow AF, Boissin J, Assenmacher I, Ixart G. Chronic restraint enhances interleukin-1β release in the basal state and after endotoxin challenge, independently of adrenocorticotropin and corticosterone release. Neuroimmunomodulation. 1994;1:292–299. doi: 10.1159/000097179. [DOI] [PubMed] [Google Scholar]
- 80.Takaki A, Huang QH, Somogyvari-Vigh A, Arimura A. Immobilization stress may increase plasma interleukin-6 via central and peripheral catecholamines. Neuroimmunomodulation. 1994;1:335–342. doi: 10.1159/000097185. [DOI] [PubMed] [Google Scholar]
- 81.Calandra T, Bernhagen J, Metz CN, Spiegel LA, Bacher M, Donnelley T, Cerami A, Bucala R. MIF as a glucocorticoid-induced modulator of cytokine production. Nature. 1995;377:68–71. doi: 10.1038/377068a0. [DOI] [PubMed] [Google Scholar]
- 82.Baumann H, Gauldie J. The acute phase response. Immunol Today. 1994;15:74–80. doi: 10.1016/0167-5699(94)90137-6. [DOI] [PubMed] [Google Scholar]
- 83.Wiegers GJ, Reul JMHM. Induction of cytokine receptors by glucocorticoids: functional and pathological significance. Trends Pharmacol Sci. 1998;19:317–321. doi: 10.1016/s0165-6147(98)01229-2. [DOI] [PubMed] [Google Scholar]
- 84.Esparza EM, Arch RH. Glucocorticoid-induced TNF receptor functions as a costimulatory receptor that promotes survival in early phases of T-cell activation. J Immunol. 2005;174:7869–7874. doi: 10.4049/jimmunol.174.12.7869. [DOI] [PubMed] [Google Scholar]
- 85.Tone M, Tone Y, Adams E, Yates SF, Frewin MR, Cobbold SP, Waldmann H. Mouse glucocorticoid-induced tumor necrosis factor receptor ligand is costimulatory for T cells. Proc Natl Acad Sci USA. 2003;100:15059–15064. doi: 10.1073/pnas.2334901100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Akahoshi T, Oppenheim JJ, Matsushima K. Induction of high-affinity interleukin-1 receptor on human peripheral blood lymphocytes by glucocorticoid hormones. J Exp Med. 1988;167:924–936. doi: 10.1084/jem.167.3.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Girard MT, Hjaltadottir S, Fejes-Toth AN, Guyre PM. Glucocorticoids enhance the γ-interferon augmentation of human monocyte IGG Fc receptor expression. J Immunol. 1987;138:3235–3241. [PubMed] [Google Scholar]
- 88.Kizaki T, Oh-Ishi S, Ookawara T, Yamamoto M, Izawa T, Ohno H. Glucocorticoid-mediated generation of suppressor macrophages with high density FcγRII during acute cold stress. Endocrinology. 1996;137:4260–4267. doi: 10.1210/endo.137.10.8828485. [DOI] [PubMed] [Google Scholar]
- 89.Reed J, Abidi A, Alpers J, Hoover R, Robb R, Nowell P. Effect of cyclosporin A and dexamethasone on interleukin-2 receptor gene expression. J Immunol. 1986;137:150–154. [PubMed] [Google Scholar]
- 90.Boumpas DT, Paliogianni F, Anastassiou ED, Balow JE. Glucocorticosteroid action on the immune system: molecular and cellular aspects. Clin Exp Rheum. 1991;9:413–423. [PubMed] [Google Scholar]
- 91.Lamas M, Sanz E, Martin-Parras L, Espel E, Sperisen P, Collins M, Silva AG. Glucocorticoid hormones upregulate interleukin-2 receptor a gene expression. Cell Immunol. 1993;151:437–450. doi: 10.1006/cimm.1993.1252. [DOI] [PubMed] [Google Scholar]
- 92.Munck A, Guyre PM, Holbrook NJ. Physiological functions of glucocorticoids in stress and their relation to pharmacological actions. Endocr Rev. 1984;5:25–44. doi: 10.1210/edrv-5-1-25. [DOI] [PubMed] [Google Scholar]
- 93.Schleimer RP, Claman HN, Oronsky A, editors. Anti-inflammatory steroid action: basic and clinical aspects. ed 1. San Diego: Academic Press; 1989. pp. 1–564. [Google Scholar]
- 94.Marx J. How the glucocorticoids suppress immunity. Science. 1995;270:232–233. doi: 10.1126/science.270.5234.232. [DOI] [PubMed] [Google Scholar]
- 95.Sternberg EM, Wilder RL. The role of the hypothalamic-pituitary-adrenal axis in an experimental model of arthritis. Prog Neuroendocrinol Immunol. 1989;2:102–108. [Google Scholar]
- 96.Webster JI, Tonelli L, Sternberg EM. Neuroendocrine regulation of immunity. Annu Rev Immunol. 2002;20:125–163. doi: 10.1146/annurev.immunol.20.082401.104914. [DOI] [PubMed] [Google Scholar]
- 97.Dougherty TF. Role of the adrenal gland in the protection against anaphylactic shock. Anat Rec. 1949;103:24. [Google Scholar]
- 98.Kroemer G, Brezinschek HP, Faessler R, Schauenstein K, Wick G. Physiology and pathology of an immunoendocrine feeback loop. Immunol Today. 1988;9:163–165. doi: 10.1016/0167-5699(88)91289-3. [DOI] [PubMed] [Google Scholar]
- 99.Besedovsky H, Del Ray A, Sorkin E, Dinarello CA. Immunoregulatory feedback between interleukin-1 and glucocorticoid hormones. Science. 1986;233:652–655. doi: 10.1126/science.3014662. [DOI] [PubMed] [Google Scholar]
- 100.Sternberg EM, Young WS, Bernadini R, Calogero AE, Chrousos GP, Gold PW, Wilder RL. A central nervous system defect in biosynthesis of corticotropin-releasing hormone is associated with susceptibility to streptococcal cell wall-induced arthritis in Lewis rats. Proc Natl Acad Sci USA. 1989;86:4771–4775. doi: 10.1073/pnas.86.12.4771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sternberg EM, Glowa J, Smith M, Calogero AE, Listwak SJ, Aksentijevich S, Chrousos GP, Wilder RL, Gold PW. Corticotropin-releasing hormone-related behavioural and neuroendocrine responses to stress in Lewis and Fischer rats. Brain Res. 1992;570:54–60. doi: 10.1016/0006-8993(92)90563-o. [DOI] [PubMed] [Google Scholar]
- 102.Wick G, Sgonc R, Lechner O. Neuroendocrine-immune disturbances in animal models with spontaneous autoimmune diseases. Ann NY Acad Sci. 1998;840:591–598. doi: 10.1111/j.1749-6632.1998.tb09598.x. [DOI] [PubMed] [Google Scholar]
- 103.MacKenzie FJ, Leonard JP, Cuzner ML. Changes in lymphocyte β-adrenergic receptor density and noradrenaline content of the spleen are early indicators of immune reactivity in acute experimental allergic encephalomyelitis in the Lewis rat. J Neuroimmunol. 1989;23:93–100. doi: 10.1016/0165-5728(89)90027-1. [DOI] [PubMed] [Google Scholar]
- 104.Del Rey A, Klusman I, Besedovsky HO. Cytokines mediate protective stimulation of glucocorticoid output during autoimmunity: involvement of IL-1. Am J Physiol. 1998;275:R1146–R1151. doi: 10.1152/ajpregu.1998.275.4.R1146. [DOI] [PubMed] [Google Scholar]
- 105.Buske-Kirschbaum A, Hellhammer DH. Endocrine and immune responses to stress in chronic inflammatory skin disorders. Ann NY Acad Sci. 2003;992:231–240. doi: 10.1111/j.1749-6632.2003.tb03153.x. [DOI] [PubMed] [Google Scholar]
- 106.Torpy DJ, Chrousos GP. The three-way interactions between the hypothalamic-pituitary-adrenal and gonadal axes and the immune system. Baillieres Clin Rheumatol. 1996;10:181–198. doi: 10.1016/s0950-3579(96)80014-8. [DOI] [PubMed] [Google Scholar]
- 107.Buske-Kirschbaum A, Geiben A, Hellhammer D. Psychobiological aspects of atopic dermatitis: an overview. Psychother Psychosom. 2001;70:6–16. doi: 10.1159/000056219. [DOI] [PubMed] [Google Scholar]
- 108.Buske-Kirschbaum A, von Auer K, Krieger S, Weis S, Rauh W, Hellhammer D. Blunted cortisol responses to psychosocial stress in asthmatic children: a general feature of atopic disease? Psychosom Med. 2003;65:806–810. doi: 10.1097/01.psy.0000095916.25975.4f. [DOI] [PubMed] [Google Scholar]
- 109.Priftis KN, Papadimitriou A, Nicolaidou P, Chrousos GP. The hypothalamic-pituitary-adrenal axis in asthmatic children. Trends Endocrinol Metab. 2008;19:32–38. doi: 10.1016/j.tem.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 110.Kavelaars A, de Jong-de Vos van Steenwijk T, Kuis W, Heijnen CJ. The reactivity of the cardiovascular system and immunomodulation by catecholamines in juvenile chronic arthritis. Ann NY Acad Sci. 1998;840:698–704. doi: 10.1111/j.1749-6632.1998.tb09608.x. [DOI] [PubMed] [Google Scholar]
- 111.Chrousos GP. Stress, chronic inflammation, and emotional and physical well-being: concurrent effects and chronic sequelae. J Allergy Clin Immunol. 2000;106:S275–S291. doi: 10.1067/mai.2000.110163. [DOI] [PubMed] [Google Scholar]