Abstract
Purpose
To describe variability of intraocular pressure (IOP) measurements within the same eye and between right and left eyes over a 60 month period in participants in the Ocular Hypertension Treatment Study.
Design
Analysis of data from a prospective randomized clinical trial.
Participants
810 participants randomized to the observation group.
Methods
IOP measurements were taken at the baseline visit and every 6 months thereafter. Pearson correlation coefficients were calculated for IOP measurements in the same eye between visits and for IOP measurements between right and left eyes of participants at each visit. Differences in IOP measurements between visits are reported in percent change (>15%, >20%, and >30%) and mmHg (<3mmHg, 3–5mmHg, and >5mmHg). We examined the effects of regression to the mean, consistency in time of day, and sequence of IOP measurement of right and left eyes.
Main Outcome Measures
Correlation of IOP measurements between consecutive six-month visits.
Results
The correlation of IOP measurements within the same eye between consecutive visits was r=0.62; whereas the correlation of IOP measurements between right and left eyes at the same visit was r=0.72. Thirteen percent of eyes had >20% change in IOP between consecutive visits. Sixty-six percent of eyes had a change in IOP within 3mmHg and 10% of eyes had a change in IOP >5mmHg between visits. Eyes with a higher baseline IOP tended to have a lower IOP measurement at 6 months. IOP measurements performed within 2 hours of the time of day of the previous visit were more highly correlated (r=0.56) than those performed >2 hours apart (r=0.39). IOP of the right eye, which was measured first, was 0.3±2.8 mmHg higher than the left eye.
Conclusion
The variability of IOP measurements in the same eye between consecutive visits is moderate and is greater than the variability of IOP measurements between right and left eyes at the same visit. Factors affecting the variability of IOP measurement include regression to the mean, time of day, and measurement order. Knowledge of variability in IOP and its measurements may help clinicians establish a more accurate baseline IOP, target IOP, and assessment of medication effect.
Introduction
Intraocular pressure (IOP) variability is a well known phenomenon which may be due to true variability (e.g. diurnal variation, progression of disease) or variability in IOP measurement (e.g. technician error, uncalibrated tonometer). Understanding variability in IOP and IOP measurement is important to diagnose and manage patients with glaucoma accurately. A clinician’s understanding of a patient’s IOP fluctuation may help establish a more accurate baseline and target IOP as well as determine IOP-lowering response to ocular hypotensive medications. In addition, knowledge regarding variability in IOP may help clarify whether methods to determine response to a medication, such as the monocular trial, are valid in a clinical setting.
Most prior studies of IOP fluctuation have focused on diurnal curves and have reported conflicting results with regards to symmetry between eyes.1–7 Only a few studies have examined long-term variability in diurnal curve patterns or IOP measurement either between eyes or within the same eye.1,3,8 These studies, conducted over several months, also report disparate results on the amount of variability of IOP. Furthermore, factors which may affect the variability of IOP and IOP measurements over time have not been fully examined.
The Ocular Hypertension Treatment Study (OHTS) is a multicenter, randomized, clinical trial designed to evaluate whether lowering intraocular-pressure by topical ocular hypotensive medication delays or prevents the onset of primary open angle glaucoma (POAG) in participants with ocular hypertension.9 Participants were randomized to either medication or observation. IOP measurements were taken every 6 months using a well-defined standardized protocol.10 The purpose of this report is to describe variability of IOP measurements within the same eye and between right and left eyes of participants in the observation group in the OHTS over 60 months. The main focus of this report is descriptive. A careful comprehensive analysis of factors affecting variability of IOP measurement is beyond the scope of this paper.
Patients and Methods
The Ocular Hypertension Treatment Study
The OHTS is a multicenter, randomized, clinical trial with 22 participating clinical centers. Each clinical center received approval for the study by its institutional review board. The OHTS is registered at www.clinicaltrials.gov, the registration number is NCT00000125. The study protocol has been described in detail previously10 and the manual of procedures can be viewed online (https://vrcc.wustl.edu/mop/ohtsmop.pdf) accessed September 22,2008.11 Participants 40–80 years of age with no evidence of glaucoma by optic disc examination, review of optic disc photographs, or visual field testing were recruited for the study between February 1994 and October 1996. Eligibility criteria included IOP between 24 mmHg and 32 mmHg in one eye and between 21 mmHg and 32 mmHg in the fellow eye. Qualifying IOP was calculated from two consecutive measurements on separate visits. These visits occurred within 12 weeks of each other and were scheduled at the same time of day (±2 hours). Participants who met eligibility criteria returned for a baseline randomization visit in which they were randomized to either topical ocular hypotensive medication or close observation without treatment. This report includes only data from participants randomized to close observation. There were no minimum or maximum IOP criteria required at the randomization visit. Participants completed follow-up visits every 6 months.
All IOP measurements were performed by two OHTS-certified examiners using calibrated Goldmann applanation tonometers. One operator viewed the mires and rotated the tonometer dial while the second operator recorded the result. Two IOP measurements were taken but if the readings differed by greater than 2 mmHg a third measurement was taken. The IOP in the right eye was measured first. The visit IOP was defined as the mean of two IOP measurements or the median of three measurements. The baseline IOP was defined as the mean of two or three IOP measurements recorded at the baseline randomization visit. Baseline IOP did not include IOP measurements used to determine eligibility in order to minimize potential regression to the mean. Diurnal IOPs were not performed in the OHTS. The protocol specified for follow-up visits to be scheduled within 2 hours of the time of day as the baseline visit.
After the June 2002 publication of the primary outcome article which demonstrated that treatment of participants with ocular hypertension delayed or prevented the onset of POAG, participants initially randomized to the observation group were offered ocular hypotensive medication.9 Therefore, data from observation participants after June 2002 were excluded from this analysis. Prior to this date, there were participants in the observation group who were started on ocular medications in one or both eyes due to clinical concern by their physicians. Data from participants are censored after they were started on an ocular medication in one or both eyes or after a diagnosis of glaucoma was established in one or both eyes. More than 70% of the participants had completed their 60 month visit by June 2002; therefore we report data through 60 months.
Statistical Design and Methods
The primary outcomes of interest in this report were the association of IOP in the same eye between visits and the association of IOP between right and left eyes of participants at each visit. The effects on IOP from regression to the mean, time of day of IOP measurement, and sequence of IOP measurement (right eye measured first) were also examined.
Descriptive statistics (mean and standard deviations) are reported for IOP of both the right and left eyes at the baseline and follow-up visits. We describe the variability of IOP measurements within the same eye between consecutive 6 month visits over 60 months in the following manner: 1. Pearson correlation coefficients of IOP in the same eye between consecutive visits (e.g. IOP at baseline correlated to IOP at 6 months, IOP at 6 months correlated to IOP at 12 months) 2. the proportion of eyes whose IOP measurement changed (increased or decreased) by >15%, >20%, and >30% between consecutive visits 3. the proportion of eyes with an absolute difference in IOP measurement of <3mmHg, 3–5mmHg, or >5mmHg between two consecutive visits. We report the proportion of eyes with an absolute difference in IOP change of >3mmHg because 3 mmHg has been reported to be within the errors of measurement of applanation tonometry between two examiners.12
Symmetry of IOP between eyes is defined here as the association of IOP measurement in one eye to IOP measurement in the fellow eye at the same visit. We describe IOP symmetry between eyes as follows: 1. Pearson correlation coefficients of IOP measurements of right and left eyes at each 6 month follow-up visit from baseline to 60 months (e.g. IOP of right eye at 6 months correlated to IOP of left eye at 6 months) 2. the proportion of participants with asymmetric fluctuation of IOP measurements between eyes across two visits. We defined asymmetric fluctuation between eyes as the absolute difference in IOP change of ≥3 mmHg between visits [|(IOP change right eye) minus (IOP change left eye)|]. For example, if the IOPs measured at the 6 month visit were 21 in the right eye and 24 in the left eye and the IOPs measured at the 12 month visit were 25 in the right eye and 23 in the left eye then the amount of fluctuation between the eyes between these two visits would be 5 mmHg {(25–21) minus (23–24)= 5}.
Regression to the mean was examined by comparing baseline IOP and 6 month IOP in the eye with the higher baseline IOP between the two eyes. When right and left eyes had the same IOP at baseline, one eye was selected randomly as the eye with the higher IOP. Descriptive statistics (mean and standard deviations) for IOP are reported.
The effect of consistency of time of day of IOP measurements was assessed by dividing participants into two groups: those whose 6 month IOP was measured within 2 hours of the same time of day as the baseline IOP and those whose 6 month IOP was measured greater than 2 hours of the same time of day as the baseline IOP. Descriptive statistics (mean and standard deviation) of IOP for both groups are reported at the baseline visit and the 6 month visit. A Pearson correlation of IOP at baseline and 6 months was performed for both groups to determine whether the consistency of time of day of IOP measurement affects variability of IOP.
The association of measurement sequence and the IOP measured was examined by analyzing the IOP measurements in the order performed: IOP1 right eye, IOP2 right eye, IOP1 left eye, IOP2 left eye. Descriptive statistics (mean and standard deviations) are reported by the order of each IOP measurement at the baseline visit. All data were analyzed using SAS® (Cary, NC, Version 9.1).
Results
Of the 819 participants in the observation group, 810 participants had completed both a baseline visit and at least one follow-up visit over a 60 month period for inclusion in this report. Baseline characteristics of these participants are reported in Table 1. The mean follow-up time for participants included in the analysis was 53.2 ±13.7 months. Of the 810 initial participants, data was available for 574 participants (71%) at the 60 month visit.
Table 1.
Baseline Characteristics
| Mean ± Standard Deviation or % (n=810) |
||
|---|---|---|
| Age (years) | 56.2 ± 9.7 | |
| Gender | Male | 42.1% |
| Female | 57.9% | |
| Race | African American | 24.8% |
| Other | 75.2% | |
| Educational Status | High school or less | 33.0% |
| College or more | 67.0% | |
| Marital Status | Married | 65.1% |
| Not Married or Widowed | 34.9% | |
| Diabetes | Yes | 12.1% |
| No | 87.9% | |
| High Blood Pressure | Yes | 38.2% |
| No | 61.8% | |
| Heart Disease | Yes | 6.7% |
| No | 93.3% | |
| Mean Central Corneal Thickness of Right and Left Eyes (µm) | 574.5 ± 37.7 (n=719) | |
Data from 116 participants were censored from this analysis. Data were censored after the date a participant was diagnosed with glaucoma in one or both eyes (n=79) or if medication was initiated in one or both eyes (n=80) with 43 participants meeting both criteria. The mean follow-up time for participants with data censored was 32.9 ±17.3 months. A downward trend in IOP measurement of 1.6–1.7 mmHg was observed over 60 months in the analysis sample. We assessed whether censoring of data after the development of POAG and clinician initiated medication affected the overall mean IOP in the analysis sample. We used the last pre-censored IOP measurement for participants with censored data and carried it forward through 60 months. We found that censoring of data from these participants accounted for 0.6mmHg of the downward trend of IOP.
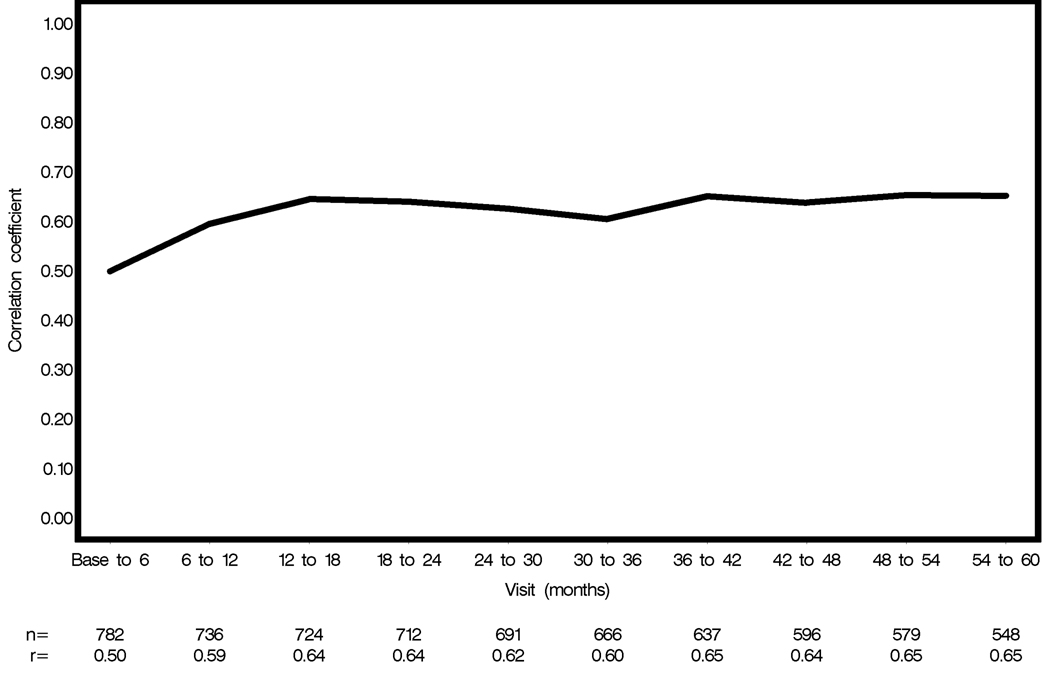
Variability of IOP measurements of the same eye between visits
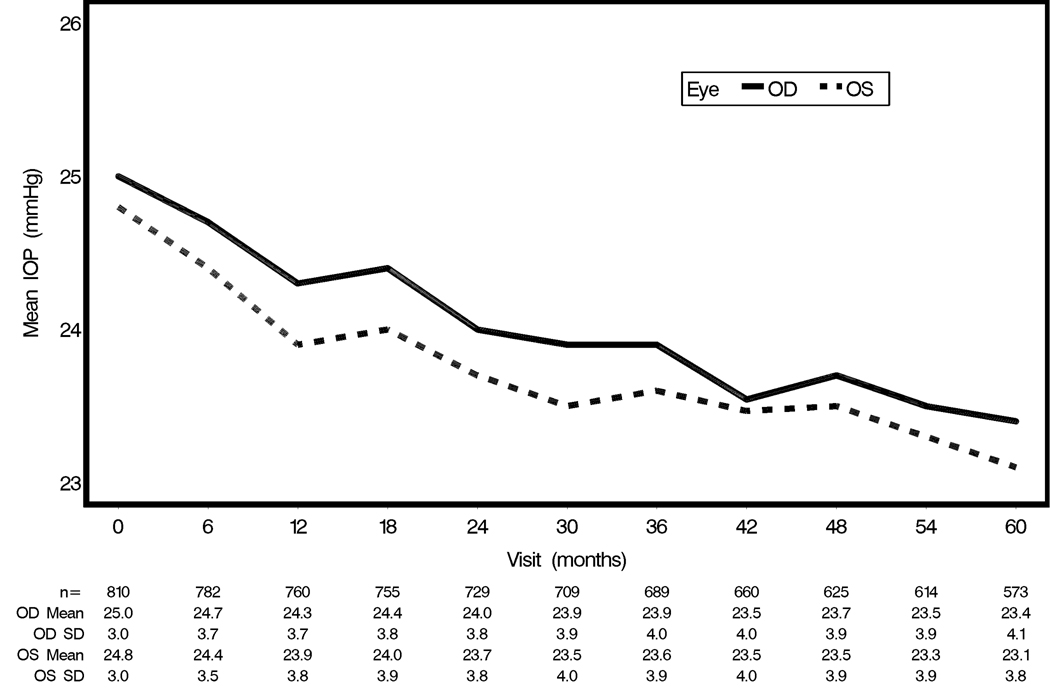
The mean IOP (± SD) of right and left eyes over the 60 month period was 24.1 ± 3.8 mmHg and 23.8 ± 3.8 mmHg respectively. Figure 1 displays the mean IOP of right and left eyes for each visit from baseline to 60 months. Across all visits for all patients, the Pearson correlation coefficient (r) of IOP measurements between consecutive visits (e.g. baseline to 6 month, 6 month to 12 month) in the same randomly selected eye was r=0.62 and ranged from r=0.50–0.65 between visits (Figure 2). The correlation coefficient of a randomly selected eye is reported due to similar results for right and left eyes.
Figure 1.
Mean IOP (±SD) of right and left eyes from baseline to 60 months. IOP = intraocular pressure; OD = right eye; OS = left eye; SD=standard deviation.
Figure 2.
Correlation of IOP measurements in the same randomly selected eye between consecutive visits at 6 month intervals through 60 months. IOP = intraocular pressure.
Over the 60 month follow-up period, 810 participants completed a total of 6671 consecutive visits. Of these 6671 consecutive visits, 13% of the eyes had a difference in IOP >20% between any two consecutive visits. Of these, 5% of eyes had a decrease in IOP measurement >20% at the second visit compared to the first visit and 8% of eyes had an increase in IOP measurement >20% at the second visit compared to the first visit. Table 2 displays the percent of eyes with differences in IOP measurements of >15%, >20%, and >30% between consecutive visits within the same eye.
Table 2.
The percent of eyes with greater than 15%, 20%, and 30% change in IOP between consecutive visits (n=6671) over 60 months. One eye was selected randomly per participant.
| Percent change in IOP between two consecutive visits |
Increase | Decrease | Total |
|---|---|---|---|
| >15% | 13% (n=856) | 11% (n=746) | 24% (n=1602) |
| >20% | 8% (n=527) | 5% (n=352) | 13% (n=879) |
| >30% | 3% (n=221) | 1% (n=75) | 4% (n=296) |
IOP = intraocular pressure
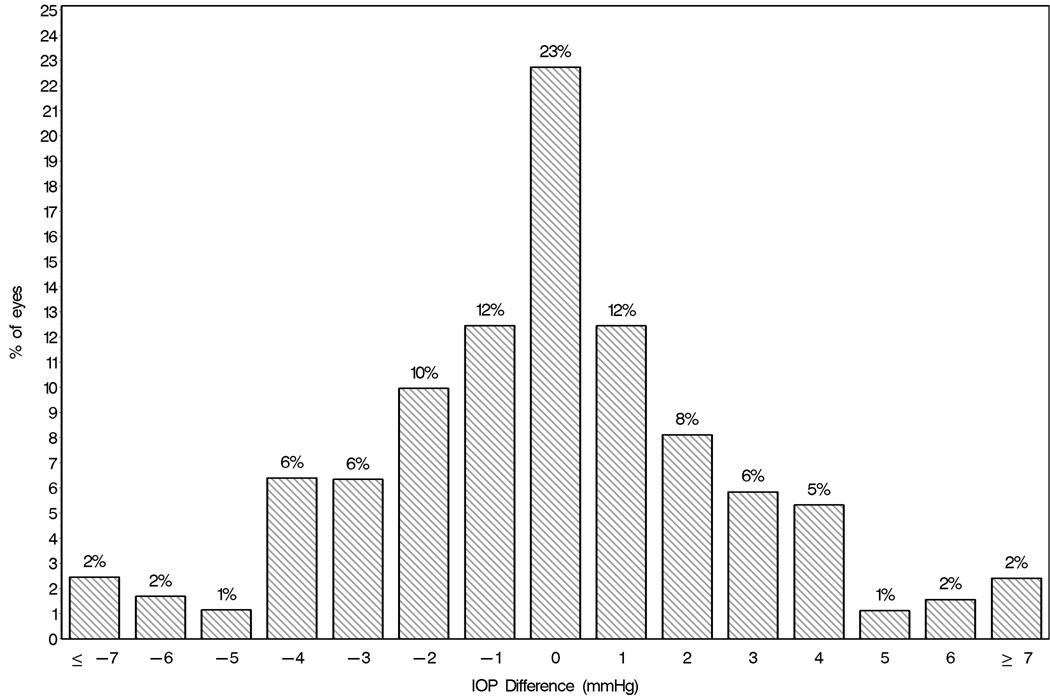
Between all consecutive visits, the mean absolute difference in IOP measured within the same eye was <3mmHg in 66% of eyes, between 3–5 mmHg in 24% of eyes, and >5mmHg in 10% of eyes. Figure 3 displays the distribution in the difference of IOP measured at the baseline and 6 month visits.
Figure 3.
Distribution of differences between baseline IOP and 6 month IOP (6 month IOP minus baseline IOP) for a randomly selected eye of each participant (n=782). Positive values indicate that IOP measured at 6 months was higher than at baseline and negative values indicate that IOP measured at 6 months was lower than at baseline. IOP = intraocular pressure.
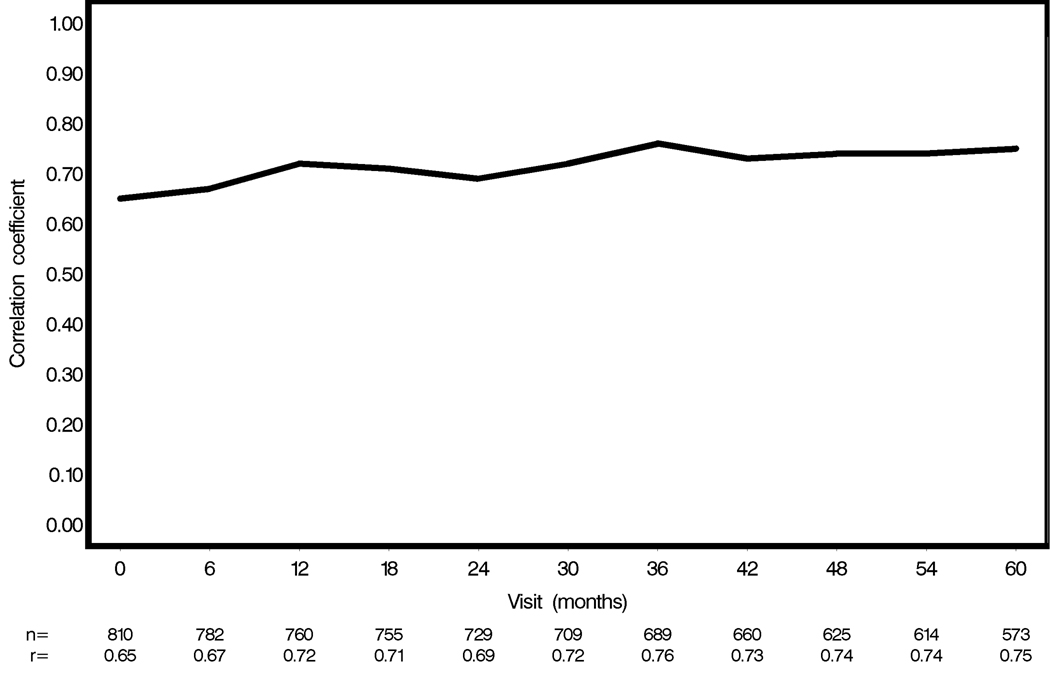
Symmetry of IOP measurements between eyes at each visit
Across all visits for all patients, the Pearson correlation coefficient (r) of the IOP measurements between right and left eyes at each visit was r=0.72 and ranged from r=0.65–0.76 (Figure 4). Twenty-four percent of participants had asymmetric fluctuation ≥3 mmHg between eyes between two consecutive visits over the 60 month period.
Figure 4.
Correlation of IOP measurement between right and left eyes at each visit over 60 months. IOP = intraocular pressure.
Regression to the mean
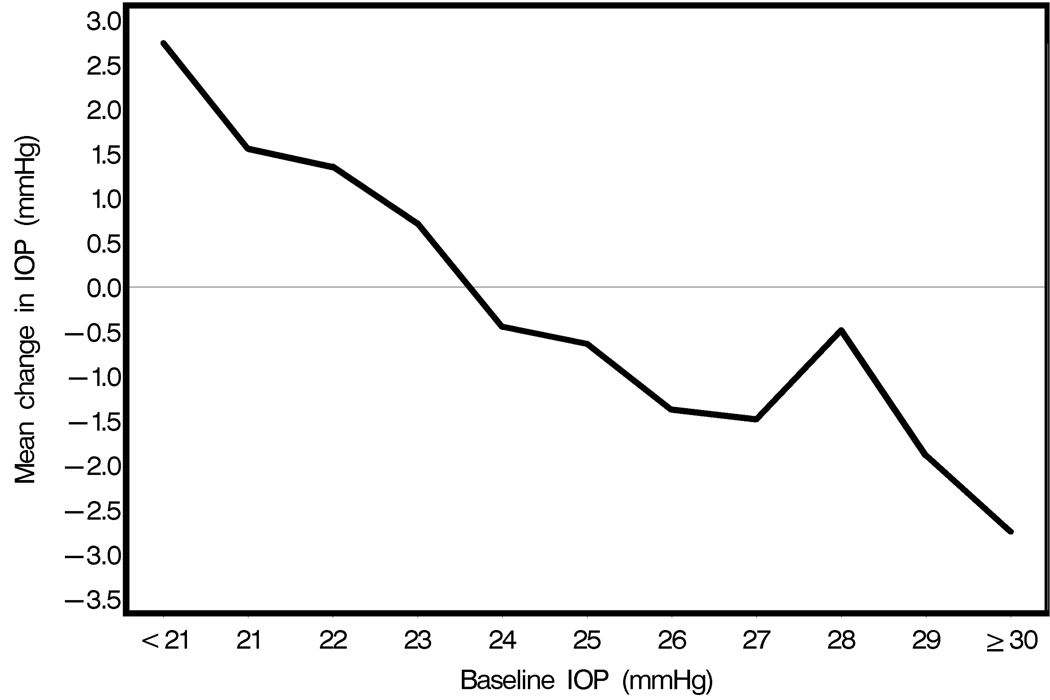
Eyes with a higher baseline IOP had a mean decrease of IOP (±SD) of 0.6±3.5 mmHg between the baseline and 6 month visits (p<0.0001, matched-pair t test) while eyes with a lower baseline IOP had a mean change of 0.0±3.1 mmHg between the same visits (p=0.98, matched-pair t test). Figure 5 displays the mean change in IOP between baseline and 6 month visits of all eyes. In general, eyes with IOP on the higher end at the baseline visit had a decrease in IOP at the 6 month visit and eyes with IOP on the lower end at the baseline visit had an increase in IOP at the 6 month visit.
Figure 5.
Mean difference in IOP from baseline to 6 months in eyes with a higher baseline IOP compared to their fellow eyes (n=782). Positive values indicate that IOP measured at 6 months was higher than at baseline and negative values indicate that IOP measured at 6 months was lower than at baseline. IOP = intraocular pressure.
Consistency of time of day of IOP measurement
There were 781 participants who had a baseline visit, a 6 month visit, and a recorded time of day for IOP measurements for both visits. Participants (n=524) whose IOP at 6 months was measured within 2 hours (mean 0.8 hours; range 0–2 hours) of the time of day as baseline had a mean IOP in a randomly selected eye of 24.9±2.9 mmHg at baseline and 24.8±3.6 mmHg at 6 months (Pearson correlation coefficient, r=0.56). Participants (n=257) whose IOP at 6 months was measured greater than 2 hours (mean 4.0 hours; range 2.1–8.2 hours) of the time of day as baseline had a mean IOP in a randomly selected eye of 24.9±3.3 mmHg at baseline and 24.3±3.5 mmHg at 6 months (Pearson correlation coefficient, r=0.39). The difference between these correlations (r=0.56 and r=0.39) was statistically significant (p<0.003).
Sequence of IOP measurement
IOP measurement in the right eye was consistently higher than IOP measurement in the left eye at each visit over 60 months with a mean IOP of 0.3±2.8mmHg higher in right eyes than left eyes (Figure 1). In order to determine whether measurement order explains why IOP in the right eye was measured higher than the left eye we examined the mean IOP according to measurement sequence from the first to fourth baseline IOP measurement in a given OHTS visit. The mean IOP in order of sequence was: 25.1 ± 3.0 mmHg (IOP1 right eye), 25.0 ± 3.0 mmHg (IOP2 right eye), 24.9 ± 3.0 mmHg (IOP1 left eye), 24.7 ± 3.1 mmHg (IOP2 left eye). A repeated measures analysis-of-variance showed a significant difference among the four measurements (p<0.0001). There was also a significant difference between IOP1 right eye and IOP1 left eye (p=0.0028) and between IOP2 right eye and IOP2 left eye (p=0.0023).
Discussion
To our knowledge, the OHTS provides the largest available database to date to investigate long-term variability of IOP within the same eye and between right and left eyes of individuals with untreated ocular hypertension. Our results suggest that the variability in IOP measurement in the same eye between visits is moderate and is greater than the variability in IOP measurement between right and left eyes at each visit.
Data from the OHTS was collected using a standardized protocol with strict quality assurance for IOP measurements. Measurement variability and observer bias were reduced by using a calibrated Goldmann applanation tonometer and a two-operator system with a minimum of two IOP measurements and a third IOP measurement if needed per eye each visit. Diurnal variability was reduced by attempts to schedule visits within 2 hours of the same time of day as the baseline visit.
IOP variability within the same eye
Prior studies regarding long-term IOP variability within the same eye report mainly on stability of diurnal curve patterns over time. Wilensky et al. found that 28% of ocular hypertensive patients (n=32) and 44% of open angle glaucoma patients (n=43) showed similar diurnal curve patterns of the same eye on a repeat test (1 to 45 months apart) using hometonometry.3 Langley et al. reported 66% of patients (n=16) with a similar curve type between two visits separated by months.13 Both of these studies, however, analyze long-term IOP stability within the same eye through diurnal curve patterns as opposed to quantifying differences in IOP measurements as in our analysis.
We found a moderate correlation of IOP measurements within the same eye between visits (r=0.62) as well as a moderate amount of variability in IOP measurement within the same eye with 13% of eyes having a difference in IOP >20% between visits. Such a level of IOP variability may contribute to improper diagnosis and management of glaucoma. For example, a patient with glaucomatous progression may have a single baseline IOP measured at one visit. This single baseline IOP may be atypically high or low compared to their usual mean IOP resulting in a calculated target IOP that may not be appropriate to prevent further glaucomatous progression. IOP measurements taken on multiple visits would provide a more accurate baseline and target IOP.14 In addition, measuring IOP at more than one visit after a medication is initiated may reduce improper continuation or discontinuation of an ocular hypotensive medication.
Results from previous studies suggest that long-term variability in IOP may be a risk factor for glaucomatous progression.15–19 These results, however, are controversial.20 An analysis using data from the OHTS may help elucidate whether long-term variability of IOP measurement in individuals with untreated ocular hypertension is a risk factor for development of POAG. If so, understanding an individual’s long-term variability of IOP measurement from IOP measurements taken on several different visits may help assess their risk for glaucomatous progression.
Approximately 1/3 of eyes in our sample had an absolute difference in IOP measurement >3mmHg between visits. We chose 3 mmHg as the minimum cut-off to exclude variability in IOP measurement which may be due to measurement error using Goldmann applanation tonometry.12 The measurement error in OHTS, however, is likely even less than 3mmHg given the strict protocol, multiple IOP measurements, and two-operator system.
Interestingly, we observed a downward slope of IOP measurement in both right and left eyes over the 60 month period. This decrease in IOP measurement over time appeared to be partially attributable to censoring of POAG participants. Other possible causes, such as treatment for systemic hypertension, are under investigation.
IOP symmetry between eyes
Previous reports on the symmetry of IOP measurements between right and left eyes have focused on diurnal curves. Earlier studies report conflicting results with regards to the symmetry of diurnal curves between fellow eyes.1–3 More recent studies, however, have found a strong correlation of IOP measurements between right and left eyes using Goldmann applanation tonometry over a 24 hour period in untreated (r=0.84) and treated (r=0.84) glaucoma patients, glaucoma suspects (r=0.78), and normal tension glaucoma patients (r=0.81).4,6 Similar correlations over a 24 hour period were found in older healthy individuals (r=0.77 to 0.86) and patients with untreated POAG (r=0.65 to 0.79) using pneumotonometry.5,7 In our sample of untreated ocular hypertension participants, the measured IOPs of right and left eyes were also well correlated (r=0.72) regardless of the time of day that IOPs were measured.
We found the correlation of IOP between fellow eyes at the same visit was higher than the correlation of IOP within the same eye between visits suggesting that factors that influence IOP measurement are more concordant at the same visit than at different visits. Therefore, when starting a patient on an ocular hypotensive medication in one eye, the fellow eye serves as a better control for IOP variability than the eye starting the medication. For example, a patient may have a baseline IOP of 22 mmHg in both eyes and is started on a glaucoma medication in one eye, the trial eye. On their follow-up visit their IOP measurements are 24mmHg in the trial eye and 30mmHg in the fellow eye. If the clinician uses only the trial eye to determine medication response they may conclude that the trial eye did not have a response to the medication since it increased by 2mmHg between visits. However, if the clinician uses the fellow eye as a control for IOP variability it is apparent that the IOP between eyes was similar at the first visit but differed by 6mmHg at the second visit, with the trial eye having a lower IOP than the fellow eye. Since we know that the correlation of IOP between eyes at each visit should be strong, the clinician would conclude that the large difference in IOP between eyes at the second visit was likely due to medication response in the trial eye as opposed to normal variability in IOP. Therefore, it is useful to use the fellow eye as a guide for IOP variability in addition to using IOP measurements from several visits to determine effectiveness of glaucoma medications.
IOP variability between eyes
Variability of IOP between eyes was determined by the proportion of eyes with asymmetric fluctuation ≥3mmHg between eyes between visits. We report 24% of participants with asymmetric fluctuation between any two visits over a 60 month follow-up period. In a retrospective study, Realini et al. reports asymmetric IOP fluctuation between eyes (defined as >15% change from baseline and greater than 3mmHg IOP change between eyes) occurring at least once between consecutive visits in 50% of normals (n=42) and 63.2% of treated glaucoma patients (n=38).8 The follow-up visits in Realini et al’s study spanned at least one year and had a mean number of 7.8± 2.0 visits for normal participants and 8.4±1.9 visits for glaucoma participants. The proportion of participants with asymmetric fluctuation between eyes may be greater in Realini et al’s study as compared to ours due to a difference in sample populations, sample sizes, and study designs. The OHTS uses a strict protocol for IOP measurement which may decrease measurement error resulting in less variability in IOP measurement compared to that seen in a retrospective study of patients in clinical practice.
Other studies have analyzed asymmetry of fluctuation between eyes over a 24 hour period. When IOP was measured at 6 time points over a 24 hour period, fellow eyes were found fluctuate ≥3mmHg between two time points in 5–22% of untreated patients, 7–17% of treated glaucoma patients, 6–13% of glaucoma suspects, and 7–14% of normal tension glaucoma patients.4,6 In another study, 27.5% patients in their habitual position (sitting during day, supine night) had asymmetric variations ≥ 3 mmHg between eyes between time intervals throughout the day.7 Results from these studies are fairly comparable to ours.
IOP variability which masks/mimics medication effect
In clinical practice it is common to start an ocular hypotensive medication in one eye and aim for an IOP-lowering response between 20–30%. We found that 13% of untreated eyes had either >20% decrease (5% eyes) or >20% increase (8% eyes) in IOP measurement between two consecutive visits. If these participants had initiated an ocular hypotensive medication aiming for a 20% IOP-lowering response, the 5% of participants with a lower IOP at the second visit would appear to have a good medication response when they really did not (IOP variability mimics medication effect) whereas the 8% of participants with a higher IOP at the second visit would appear not to have a good medication response when they really did (IOP variability masks medication effect). Therefore, variability in the IOP measurement may result in erroneous classification of medication response in 13% of patients. These results suggest that determining medication effect from only the treated eye on one return visit may lead to inappropriate continuation or discontinuation of medications.
Factors which affect IOP variability
IOP variability may be due to true changes in IOP and/or artifactual influences on IOP measurement. Such variability may affect both eyes symmetrically or asymmetrically. Our study analyzes a few factors which may contribute to variability in IOP measurement.
Regression to the mean
Regression to the mean is a statistical phenomenon in which observations that are high relative to the mean, regress towards the mean and have a lower value when measured the second time. Conversely, observations that are low relative to the mean, regress towards the mean and have a higher value when measured the second time. Factors such as diurnal variability, measurement error, and patient-related factors (e.g. ocular squeezing, Valsalva, increased fluid intake) may all play a role in causing the IOP measurement to appear higher or lower than the true mean on any given visit. We found that eyes with high baseline IOPs had lower IOPs at the 6 month visit and eyes with low baseline IOPs had higher IOPs at the 6 month visit. This occurred despite a strict protocol for measuring IOP, multiple IOP measurements per visit, and the use of the IOP at the randomization visit as opposed to the qualifying visit as the baseline IOP. Regression to the mean is likely even greater in the clinical setting. Therefore, clinicians should be wary that IOP of an eye started on medications may be lower at the subsequent visit partially due to effects from regression to the mean as opposed to medication effect alone.
Consistency of time of day
Diurnal variation may cause IOP measurements to differ when taken on different days and different times of the day. Wilensky et al. report similar diurnal patterns of the same eye on a repeat visit in only 28% of ocular hypertensive patients and 44% of glaucoma patients.3 Other studies, however, have shown similar diurnal curves within the same eye on repeat visits.1,13 Horie and Kitazawa report the diurnal peak of IOP occurring within 2 hours between subsequent visits in 94% of eyes.21 While we did not perform diurnal curves in our study, we analyzed how the consistency of time of day of IOP measurements between two visits may affect the variability of IOP measurement. Our analysis reveals that the correlation between baseline IOP and 6 month IOP was stronger when the 6 month IOP was measured within 2 hours from the baseline IOP (r=0.56) than when the IOPs were measured greater than 2 hours apart (r=0.39). These results suggest that variability of IOP within the same eye between visits may be reduced by measuring IOP at a similar time of day.
Measurement order
On average over 60 months, the IOP of the right eye was 0.3mmHg higher than the left eye. Although this difference is clinically insignificant, it is the mean difference and some patients have a greater difference in IOP between the two eyes. The mean IOP was measured higher in the right eye than the left eye in a study of almost 6,000 normal eyes using Goldmann tonometry as well as in a study using pneumotonometry where right eyes were measured prior to left eyes.5,22 Other studies, however, have reported IOP higher in left eye and no difference in IOP between the two eyes. 6,7,23–25
IOP measurement may be slightly higher in the right eye in our study due to either a real IOP difference between eyes or a measurement artifact. We suspect it is due to the order in which IOP measurements were taken (right eye measured first) since there was a slight decrease in IOP associated with the progression of IOP measurements. Instillation of a topical anesthetic in an eye prior to IOP measurement may cause “quenching” of the fluorescein in the tear film resulting in hypofluorescence and an underestimation of IOP measurement.26 This effect may be more prominent with subsequent IOP measurements due to the increased time of contact between the topical anesthetic and the fluorescein.27 Another plausible explanation is that patients may be more anxious with earlier IOP measurements causing an artificially elevated IOP measurement from ocular squeezing or Valsalva. There has been no study to date which has directly addressed this question. If there is a true association of IOP measurement with sequence measured then the order of right and left eye IOP measurement may play a role in variability of IOP measurement. Multiple IOP measurements at a single visit may help decrease variability of IOP due to factors associated with the order of IOP measurement.
This report analyzes only a few factors which may affect variability of IOP measurement. A comprehensive analysis of demographic, clinical (e.g. central corneal thickness) and systemic (e.g. systemic medications) influences on variability of IOP measurement has yet to be conducted in the OHTS. In addition, variability of IOP measurement as a risk factor for glaucoma is an important question which needs further analysis.
The results from our study may not reflect clinical practice due to the strict protocol and multiple IOP measurements taken. In addition, patients were asked to return for follow-up visits within two hours of the baseline visit when possible which may have minimized the amount of IOP variability typically seen in clinical practice. Regression to the mean effects may have been lower in our study due to the multiple IOP measurements which may have reduced measurement error. Furthermore, our results reflect IOP fluctuation in ocular hypertensive patients and may be different in normal or glaucoma patients.
This report illustrates the variability of IOP and the complex factors involved. Multiple IOP measurements on several visits are required to accurately assess IOP fluctuation in any given patient. Our findings also demonstrate how natural variation of IOP between visits may complicate the determination of IOP response to a medication. Factors that affect variability of IOP measurement include regression to the mean, consistency of time of day, sequence of IOP measurements and likely many other factors that are yet to be elucidated.
Supplementary Material
Acknowledgments
This work was supported by awards from the National Eye Institute, the National Center on Minority Health and Health Disparities, National Institutes of Health (grants EY09341, EY09307), awards to the Department of Ophthalmology and Visual Sciences at Washington University, the NIH Vision Core Grant P30 EY 02687, awards to the Department of Ophthalmology at University of Miami, the NIH Vision Core Grant P30 EY 01480; Merck Research Laboratories, White House Station, New Jersey, and unrestricted grants from Research to Prevent Blindness, Inc., New York, New York.
Footnotes
Conflict of Interest: Dr. Kass is a paid consultant for Pfizer Pharmaceuticals. No conflicts of interest exist for any other authors.
References
- 1.Katavisto M. The diurnal variations of ocular tension in glaucoma. Acta Ophthalmol (Suppl) 1964;78:1–130. [PubMed] [Google Scholar]
- 2.Kitazawa Y, Horie T. Diurnal variation of intraocular pressure in primary open-angle glaucoma. Am J Ophthalmol. 1975;79:557–567. doi: 10.1016/0002-9394(75)90792-8. [DOI] [PubMed] [Google Scholar]
- 3.Wilensky JT, Gieser DK, Dietsche ML, et al. Individual variability in the diurnal intraocular pressure curve. Ophthalmology. 1993;100:940–944. doi: 10.1016/s0161-6420(93)31551-4. [DOI] [PubMed] [Google Scholar]
- 4.Dinn RB, Zimmerman MB, Shuba LM, et al. Concordance of diurnal intraocular pressure between fellow eyes in primary open-angle glaucoma. Ophthalmology. 2007;114:915–920. doi: 10.1016/j.ophtha.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 5.Liu JH, Sit AJ, Weinreb RN. Variation of 24-hour intraocular pressure in healthy individuals: right eye versus left eye. Ophthalmology. 2005;112:1670–1675. doi: 10.1016/j.ophtha.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Shuba LM, Doan AP, Maley MK, et al. Diurnal fluctuation and concordance of intraocular pressure in glaucoma suspects and normal tension glaucoma patients. J Glaucoma. 2007;16:307–312. doi: 10.1097/IJG.0b013e3180316736. [DOI] [PubMed] [Google Scholar]
- 7.Sit AJ, Liu JH, Weinreb RN. Asymmetry of right versus left intraocular pressures over 24 hours in glaucoma patients. Ophthalmology. 2006;113:425–430. doi: 10.1016/j.ophtha.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Realini T, Barber L, Burton D. Frequency of asymmetric intraocular pressure fluctuations among patients with and without glaucoma. Ophthalmology. 2002;109:1367–1371. doi: 10.1016/s0161-6420(02)01073-4. [DOI] [PubMed] [Google Scholar]
- 9.Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open angle glaucoma. Arch Ophthalmol. 2002;120:701–713. doi: 10.1001/archopht.120.6.701. [DOI] [PubMed] [Google Scholar]
- 10.Gordon MO, Kass MA. The Ocular Hypertension Treatment Study: design and baseline description of the participants. Arch Ophthalmol. 1999;117:573–583. doi: 10.1001/archopht.117.5.573. [DOI] [PubMed] [Google Scholar]
- 11.OHTS I Manual of Procedures. [Accessed September 22, 2008];Version 3, Chapter 2: 2-4-37. Available at https://vrcc.wustl.edu/mop/ohtsmop.pdf.
- 12.Thorburn W. The accuracy of clinical applanation tonometry. Acta Ophthalmol (Copenh) 1978;56:1–5. doi: 10.1111/j.1755-3768.1978.tb00461.x. [DOI] [PubMed] [Google Scholar]
- 13.Langley D, Swan L, Jung H. Ocular tension in glaucoma simplex. Br J Ophthalmol. 1951;35:445. doi: 10.1136/bjo.35.8.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Piltz-Seymour J, Jampel H. The one-eye drug trial revisited. Ophthalmology. 2004;111:419–420. doi: 10.1016/j.ophtha.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Lee PP, Walt JW, Rosenblatt LC, et al. Glaucoma Care Study Group. Association between intraocular pressure variation and glaucoma progression: data from a United States chart review. Am J Ophthalmol. 2007;144:901–907. doi: 10.1016/j.ajo.2007.07.040. [DOI] [PubMed] [Google Scholar]
- 16.Nouri-Mahdavi K, Hoffman D, Coleman AL, et al. Predictive factors for glaucomatous visual field progression in the Advanced Glaucoma Intervention Study. Ophthalmology. 2004;111:1627–1635. doi: 10.1016/j.ophtha.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 17.Oliver JE, Hattenhauer MG, Herman D, et al. Blindness and glaucoma: a comparison of patients progressing to blindness from glaucoma with patients maintaining vision. Am J Ophthalmol. 2002;133:764–772. doi: 10.1016/s0002-9394(02)01403-4. [DOI] [PubMed] [Google Scholar]
- 18.Hong S, Seong GF, Hong YJ. Long-term intraocular pressure fluctuation and visual field deterioration in patients with glaucoma and low intraocular pressure after a triple procedure. Arch Ophthalmol. 2007;125:1010–1013. doi: 10.1001/archopht.125.8.1010. [DOI] [PubMed] [Google Scholar]
- 19.Caprioli J, Coleman AL. Intraocular pressure fluctuation. A risk factor for visual field progression at low intraocular pressures in the Advanced Glaucoma Intervention Study. Ophthalmology. 2008;115:1123–1129. doi: 10.1016/j.ophtha.2007.10.031. [DOI] [PubMed] [Google Scholar]
- 20.Bengtsson B, Leske MC, Hyman L, et al. Fluctuation of intraocular pressure and glaucoma progression in the Early Manifest Glaucoma Trial. Ophthalmology. 2007;114:10–19. doi: 10.1016/j.ophtha.2006.07.060. [DOI] [PubMed] [Google Scholar]
- 21.Horie T, Kitazawa Y. The clinical significance of diurnal pressure variation in primary open-angle glaucoma. Jpn J Ophthalmol. 1979;23:310. [Google Scholar]
- 22.Bankes JLK, Perkins ES, Tsolakis S, Wright JE. Bedford Glaucoma Survey. Br Med J. 1968;1:791–796. doi: 10.1136/bmj.1.5595.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Costagliola C, Trapanese A, Pagona M. Intraocular pressure in a healthy population: a survey of 751 subjects. Optom Vis Sci. 1990;67:204–206. doi: 10.1097/00006324-199003000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Graham PA, Hollows FC. Sources of variation in tonometry. Trans Ophthalmol Soc. UK. 1964;84:597–613. [PubMed] [Google Scholar]
- 25.Soeteren T. Scleral rigidity in normal human eyes. Acta Ophthalmol (Copenh) 1960;38:303. doi: 10.1111/j.1755-3768.1960.tb05421.x. [DOI] [PubMed] [Google Scholar]
- 26.Schottenstein EM. Intraocular pressure and tonometry. In: Ritch R, Shields BM, Krupin T, editors. The Glaucomas. Mosby: St. Louis; 1996. p. 414. [Google Scholar]
- 27.Moses RA. Repeated applanation tonometry. Ophthalmologica. 1961;142:663–668. doi: 10.1159/000304168. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.