Abstract
Objective
We evaluated the impact of Seguro Popular (SP), a program introduced in 2001 in Mexico primarily to finance health care for the poor. We focused on the effect of household enrollment in SP on pregnant women’s access to obstetrical services, an important outcome measure of both maternal and infant health.
Data
We relied upon data from the cross-sectional 2006 National Health and Nutrition Survey (ENSANUT) in Mexico. We analyzed the responses of 3,890 women who delivered babies during 2001–2006 and whose households lacked employer-based health care coverage.
Methods
We formulated a multinomial probit model that distinguished between three mutually exclusive sites for delivering a baby: a health unit specifically accredited by SP; a non-SP-accredited clinic run by the Department of Health (Secretaría de Salud, or SSA); and private obstetrical care. Our model accounted for the endogeneity of the household’s binary decision to enroll in the SP program.
Results
Women in households that participated in the SP program had a much stronger preference for having a baby in a SP-sponsored unit rather than paying out of pocket for a private delivery. At the same time, participation in SP was associated with a stronger preference for delivering in the private sector rather than at a state-run SSA clinic. On balance, the Seguro Popular program reduced pregnant women’s attendance at an SSA clinic much more than it reduced the probability of delivering a baby in the private sector. The quantitative impact of the SP program varied with the woman’s education and health, as well as the assets and location (rural versus urban) of the household.
Conclusions
The SP program had a robust, significantly positive impact on access to obstetrical services. Our finding that women enrolled in SP switched from non-SP state-run facilities, rather than from out-of-pocket private services, is important for public policy and requires further exploration.
1. Introduction
This paper contributes to three important strands in the health economics literature. First, we add to the emerging body of knowledge on the impacts of novel public policies to finance the health care of the poor in developing economies (Gaviria, Medina et al. (2006); Trujillo, Portillo et al. (2005); Wagstaff (2007); Wagstaff, Lindelow et al. (2007)), including recent innovative interventions in Mexico (Knaul and Frenk (2005); Frenk, Sepulveda et al. (2003); Gakidou, Lozano et al. (2006); Sepúlveda, Bustreo et al. (2006)). We find that the recently established “Seguro Popular” (or “People’s Insurance”) program in Mexico has had a robust, significantly positive effect on the access of poor women to obstetrical care, an important outcome measure of maternal and infant health.
Second, we add to the growing literature on the use of multinomial discrete choice models of the selection of health care providers, including Schwartz, Akin et al. (1988) in the setting of the Philippines, Akin, Guilkey et al. (1995) in Nigeria, Bolduc, Lacroix et al. (1996) in Benin, and Leonard (2007) in Tanzania, as well as recent path-breaking work on multi-equation models involving discrete variables (Balia and Jones (2004); Deb, Munkin et al. (2006)). We formulate a multinomial probit model that distinguishes between three mutually exclusive sites for delivering a baby: a health unit specifically accredited by Seguro Popular (SP); a non-SP-accredited clinic run by the Department of Health (Secretaría de Salud, or SSA); and private obstetrical services. In what appears to be the first instance of such a technique, we then modify the standard multinomial probit model to explicitly account for the possible endogeneity of the household’s binary decision to participate in Seguro Popular. Women in households that participated in the SP program, we find, had a much stronger preference for having a baby in a SP-sponsored unit rather than paying out of pocket for a private delivery. At the same time, participation in SP was associated with a stronger preference for delivering in the private sector rather than at an SSA-sponsored clinic. On balance, the Seguro Popular program reduced pregnant women’s attendance at an SSA-sponsored clinic much more than it reduced the probability of delivering a baby in the private sector.
Third, we contribute to the nascent but expanding body of work on the heterogeneous impacts of policy interventions in the developing world, including the effect of antiretroviral treatment on labor force participation in Western Kenya (Thirumurthy, Zivin et al. (2006)), the effect of conditional cash transfers on schooling and nutrition in Nicaragua (Dammert (2007)) and Mexico (Djebbari and Smith (2005); Chávez-Martín del Campo (2006)). Here, we find that the quantitative impact of the SP program varied with the woman’s education and health, as well as the assets and location (rural versus urban) of the household.
In Section 2, we review the problem of access to obstetric care for poor women in Mexico, the basic structure of the Mexican health care system, and the introduction of Seguro Popular in 2001. In Section 3, we describe an econometric model of discrete household decision-making concerning the use obstetrical services. The model captures the possibility that a demand-side subsidy such as Seguro Popular can affect the household’s relative ranking of the three obstetric service sites. We explicitly take into account the potential endogeneity of the decision to participate in Seguro Popular, and describe our strategy for evaluating heterogeneous impacts. Section 4 describes our database, the 2006 National Survey of Health and Nutrition (Encuesta Nacional de Salud y Nutrición, or ENSANUT; see Instituto Nacional de Salud Pública (2006)). Section 5 details our empirical results. Section 6 summarizes our findings, discusses the limitations of our research, and considers its implications for public policy and future research on health policy in developing economies.
2. Mexico’s Health Care System and the “Seguro Popular” Program
2.1. Health Care Access and Financing in Mexico
Historically, access to health insurance coverage in Mexico was tied to employment in the formal economy. The principal sources of coverage for workers in these sectors were the Mexican Social Insurance Institute (Instituto Mexicano del Seguro Social, or IMSS), the Government Workers’ Social Security and Services Institute (Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado, or ISSSTE), as well as insurance programs for employees of such state-run enterprises as PEMEX (petroleum) and SEDENA (national defense). Workers outside these specific sectors and participants in the informal economy had to attend government-sponsored facilities through the Department of Health (Secretaría de Salud, or SSA) or pay out of pocket for medical care at private hospitals or doctors’ offices. These private facilities varied considerably in price, quality, and availability. On the one hand, a modern network of private health services for the middle and upper classes, located mainly in urban areas, served those individuals who had insurance coverage or could pay out of pocket for their health care. On the other hand, lower-priced private health services of variable quality, including informal providers such as midwives and traditional healers, were available to poor urban and rural families (Parker and Wong (1997); Nigenda, Troncoso et al. (2003); Pagan, Puig et al. (2007)).
The poorest households in the informal sector were thus left with essentially three options: foregoing health care; seeking whatever care was available from state-sponsored SSA clinics or other low-cost informal providers; or spending a large part of their income on private health care. This has, in fact, been the predicament of the poor in many developing economies (Wagstaff (2007)).
In recent years, Mexico has adopted public policies intended to overcome these historical inequalities in health care coverage (Frenk, Sepulveda et al. (2003)). One especially important initiative has been PROGRESA (Program for Education, Health and Nutrition), later renamed Oportunidades, an incentive-based program designed to improve the health, nutrition and education of poor families with children (Behrman and Skoufias (2006); Gertler (2000); Gertler (2004); Hoddinott and Skoufias (2004); Skoufias and Parker (2001; Skoufias (2005)). While PROGRESA/Oportunidades has increased poor families’ demand for preventive health services and some types of primary care, coverage for more advanced forms of care has remained lacking. For a poor family, essentially any major illness was catastrophic.
2.2. Seguro Popular
In 2001, the government of Mexico launched Seguro Popular, a major new effort to improve access of the poor to qualified public health services. The Seguro Popular program specifically targeted poor families in both urban and rural areas of Mexico without access to any other form of private or public coverage (Torres and Knaul (2003)). Under this voluntary insurance plan, a household makes subsidized contributions, based on ability to pay, to a public fund to cover catastrophic spending on health care (Frenk, Sepulveda et al. (2003)). Access to medical care is guaranteed and provided through a publicly sponsored network of ambulatory health units, general and specialized hospitals. All SP-sponsored health facilities are certified as providing a minimum level of quality of care. Health centers and hospitals are accredited on the basis of their infrastructure, equipment, health personnel, range of medical services and other criteria.
In order to accommodate the process of health unit accreditation, Seguro Popular was rolled out gradually during 2001–2005. Five states (Aguascalientes, Campeche, Colima, Jalisco and Tabasco) were incorporated into the program in 2001 as part of a pilot study. An additional 15 states were integrated in the program in 2002; four more states were incorporated in 2003; and the remaining states were incorporated in during 2004 and 2005. By the end of 2005, all 32 of Mexico’s states had been incorporated, and approximately 4 million families (comprising about 12 million individuals) had signed up for the voluntary program (Secretaría de Salud (2006)).
2.3. Maternal Health Services
During the past two decades, policy makers in Mexico have adopted several different approaches to improving the health of mothers and infants. One strategy has been to enhance access to services within the existing system of state-run SSA-sponsored clinics. This approach, however, has had limited impact. Those state-run SSA-sponsored units that did provide some obstetrical services lacked the full range of drugs and equipment, hired deficiently trained personnel, and maintained reduced hours of operation. As a consequence, a significant proportion of pregnant women preferred delivering their babies in the private sector, even though they had direct contact with state-run health facilities for their prenatal care, and even though many private-sector providers were unqualified midwives and traditional birth attendants (Instituto Nacional de Salud Pública (2000)). Such a pattern of prenatal care at public facilities followed by birth attendance in the private sector has been observed in other developing economies (Schwartz, Akin et al. (1988)).
One objective of the Seguro Popular program was to remedy these persistent deficiencies. Apart from subsidizing health insurance coverage, the program has invested considerable resources in improving the quality and availability of secondary medical care provided in public facilities, including obstetric care. Accordingly, in the present research, we sought to evaluate whether enrollment in SP has specifically improved pregnant women’s attendance at SP-accredited obstetrical facilities. Given the historical preference for private obstetrical services over state-run facilities, we therefore distinguished between three different sites of care: an SP-accredited obstetric facility; a non-SP state-run health unit; and a private provider, including physicians and midwives.
3. Econometric Model
3.1. Multinomial Choice Model with a Discrete Endogenous Variable
We observe the discrete choice, y1, made by a pregnant woman among three mutually exclusive sites for her obstetric care: a site run by the Department of Health (Secretaría de Salud, or SSA); a facility specifically accredited by Seguro Popular (SP); or delivery by a physician or midwife in a private facility or at home. We denote these three choices by y1 = 0,1,2, respectively. (For clarity, we omit subscripts specific to each pregnant woman.) We also observe the binary decision, y2, made by the woman’s household to enroll in Seguro Popular, where y2 = 1 if the household enrolls in SP, and y2 = 0 otherwise.
Let the quantities {w0*, w1*, w2*} represent the respective latent utilities associated with the three sites of obstetric care. We assume that the observed choice of the site of obstetric care is utility maximizing:
| (1) |
We further assume that the latent utilities depend linearly on observed exogenous variables, on the household’s enrollment status in SP, and unobserved error terms:
| (2) |
where (X0, X1) are vectors of observable explanatory variables, (β0, β1) are conformal vectors of unknown parameters, (γ0, γ1) are additional unknown coefficients of the variable y2 that indicates enrollment in Seguro Popular, and (ε0, ε1) are unobserved error terms to be characterized shortly. Given that we observed only the choice with the highest latent utility, we recognize that we can identify only the differences in latent utility, and therefore we set the latent utility of private obstetric care equal to zero.
We further specify a binary discrete choice model of enrollment in Seguro Popular:
| (3) |
where y2 * is an unobserved latent variable, X2 is a vector of determinants of the decision to enroll, β2 is a conformal vector of unknown parameters, and ε2 is a stochastic error term that we characterize below.
While the Mexican government has phased in Seguro Popular over time, thus determining when specific communities will be eligible for the program, the household’s decision to enroll in SP nonetheless remains voluntary. Accordingly, we cannot exclude the possibility that the binary variable y2 is endogenous. This potential endogeneity can be captured by correlations between the error term ε2 in equation (3) and the error terms ε0 and ε1 in equation (2). To parameterize these correlations, we assume that each of the error terms ε0 and ε1 has a marginal unit normal distribution N (0,1), and that:
| (4) |
where σ0 and σ1 are unknown parameters, and ν is also a unit normal N (0,1) random variable that is distributed independently of ε0 and ε1. (For a similar error parameterization, see p. 1084 of Deb, Munkin et al. (2006).) This error structure admits two types of unobserved heterogeneity. When the parameter ε0 is non-zero, households have unobserved characteristics that influence their decision to enroll in SP and, at the same time, influence the pregnant woman’s preferences for SSA-sponsored public clinic over private health care. When the parameter ε1 is non-zero, households have unobserved characteristics that influence their decision to enroll in SP and, at the same time, influence the pregnant woman’s preferences for an SP-sponsored unit over a private site.
Given (4), the error terms (ε0, ε1, ε2) have a trivariate normal distribution N (0, Σ), where
| (5) |
The variance-covariance matrix Σ is positive definite for all values of the parameters σ0 and σ1. The corresponding correlation coefficients are and , where . We estimate the parameters β = (β0, β1, β2), γ = (γ0, γ1), σ = (σ0, σ1) in the model of equations (1) through (4) by maximum likelihood. The details of construction of the likelihood function and parameter estimation are given in Appendix A.
3.2. Parameter Identification
To identify the parameters of our structural model, we impose exclusion restrictions on the explanatory variables in X = (X0, X1, X2). Specifically, we took advantage of the fact that Seguro Popular has been gradually phased in over time in different states within Mexico. We therefore constructed three dummy variables, indicating whether the woman’s locality of residence had been formally incorporated into Seguro Popular by the years 2002, 2003, and 2004. For example, a women residing in a locality incorporated in the year 2003 would be encoded as having dummies equal to 0 for 2002, 1 for 2003, and 1 for 2004. A woman residing in a locality that was not incorporated until 2005, when all remaining states were incorporated, would have zero-values for all three dummy variables. Thus, 2005 served as a reference year, while each dummy variable measured the marginal effect of incorporation into SP one year earlier. Because SP was only in the pilot phase during 2001, we did not specify a dummy variable for that year. We included the three dummy variables in the participation equation (3) but excluded them from the health care utilization equations (1–2). In sensitivity analyses, we considered alternative measures of the availability of SP in the pregnant woman’s state of residence, including an additional dummy variable for the pilot year 2001, a single binary variable indicating whether SP had been incorporated in the specific state at the time of delivery, as well as a continuous variable measuring the number of years that SP had been incorporated in the state at the time of delivery.
3.3. Measuring Individual-Level Impacts
Given estimates of the parameters (β̂, γ̂, σ̂) and any given vector of household characteristics X, we can compute the respective joint probabilities Pi∩j (X) = Pr{y1 = i, y2 = j|X, β̂, γ̂, σ̂} for all i = 0,1,2 and j = 0,1. We can also compute the marginal probabilities Pj (X) = Pr{y2 = j|X, β̂, γ̂, σ̂} for j = 0,1, where, for example, P1 (X) is the probability of enrollment in SP. From these estimates we can also compute the conditional probabilities Pi j (X) = Pi∩j (X)/Pj (X) for all i = 0,1,2 and j = 0,1, where, for example, P2|1 (X) denotes the predicted probability that a woman in a household with exogenous characteristics X will choose a private obstetrical site given that the household is enrolled in Seguro Popular.
We measured the individual-level impacts of SP on the probability of choosing site i = 0,1,2 as the difference in conditional probabilities:
| (6) |
These site-specific measures of impact represent a generalization of the classic treatment effect. For a fixed vector of maternal and household characteristics X, the three sitespecific measures of the individual-level impact of Seguro Popular necessarily sum to zero, that is, I0 (X) + I1 (X) + I2 (X) = 0.
We computed these measures of individual impact Ii (X) for several prespecified values of the vector X, as described in the following section. We used Monte Carlo simulation methods to compute 95% confidence intervals, making repeated random draws from a multivariate joint normal distribution with mean (β̂,γ̂,σ̂) and estimated asymptotic variance-covariance matrix V̂, and with each draw re-computing the impact measures Ii (X) for the specified value of X. The confidence intervals for each impact measure were then computed from the range of recomputed values of Ii (X).
3.4. Analysis of Heterogeneity of Impact
Because our model is nonlinear, the marginal effects of changes in the principal treatment variable (that is, affiliation with Seguro Popular, or y2) depend on the values of the explanatory variables (that is, maternal and household characteristics, or X). Although it is commonplace to report these marginal effects at the sample means, we focused on the extent of heterogeneity in the impact of Seguro Popular at the individual level. We therefore computed the individual-level impact measures Ii (X) for four prototypical households or “cases,” that is, four different sets of explanatory variables X. To assess whether the nonlinearity of our model was the principal source of heterogeneous treatment effects, we also tested interaction models, in which the structural parameters γ0 and γ1 in (2) depended linearly on the exogenous explanatory variables.
3.5. Comparison with Simplified Bivariate Probit Model
We compared our multinomial choice model (equations (1)–(4)) with a simplified bivariate probit model, in which a pregnant woman has only two choices: a birth attended at a SP-sponsored facility (y1 = 1), or a birth elsewhere (y1 = 0). In place of equations (1) and (2), we write:
| (7) |
which is equivalent to a probit specification in which a non-SP obstetric facility is the reference category. Retaining equation (3) for y2 and setting ε0 = 0 in equation (2), we obtain a two-equation probit model with a discrete endogenous variable (that is, y2) and an unconstrained correlation coefficient between the error terms. Such a model can be estimated by maximum likelihood as if it were a simple bivariate probit model. (See, for example, p. 183 in Maddala (1983) and p. 853 in Greene (2000).) For this purpose, we used the “biprobit” routine in Stata (StataCorp (2005)).
4. Data
4.1. ENSANUT Survey Data and Analytical Sample
Our principal source of data is the 2006 Mexican National Health and Nutrition Survey (Encuesta Nacional de Salud y Nutrición, or ENSANUT), conducted during November 2005 – May 2006 (Instituto Nacional de Salud Pública (2006)), a nationally representative cross-section of 48,304 households containing 206,700 individuals. ENSANUT contained information on respondents’ education, employment, socioeconomic and demographic characteristics, prevalence of self-reported acute and chronic illnesses, as well as health care utilization and source of payment.
We focused on the 5,988 female respondents of reproductive age (15–49 years) who reported having delivered their last baby during 2001–2006. We then excluded 1,900 respondents who reported delivering at a facility sponsored by employer-based health insurance (IMSS, ISSSTE, and PEMEX), as well as an additional 198 observations that had missing values of the explanatory variables to be described below. These exclusions resulted in a sample of 3,890, which served as the principal basis for our statistical analyses. We refer to this sample as the analytic sample.
Households covered by Mexico’s employer-based plans are not legally entitled to participate in Seguro Popular. Accordingly, the exclusion of households covered by employer-based plans permitted us to focus sharply on the target population eligible for the Seguro Popular program. Given the lack of flexibility in Mexico’s labor market, we considered it unlikely that our exclusion of women covered by employer-based plans produced a significant bias of self-selection. Nonetheless, in order to check the sensitivity of our results to our exclusion criterion, we repeated our analyses with two alternative samples that were not drawn on the basis of household insurance coverage: (1) an enlarged sample of 5,762 adult women who had a baby since 2001 and who had no missing values for any explanatory variables; and (2) a restricted sample of 1,934 adult women whose household resided in a locality with a moderately high or very high index of socioeconomic marginality (“índice de marginación”) (CONAPO (2005)).
4.2. Dependent Variables
As noted in Section 3, our two discrete dependent variables were: y1, the site of obstetric care; and y2, the binary decision to enroll in Seguro Popular. With respect to the former, each respondent to ENSANUT who had her last baby during 2001–2006 was asked where she delivered her baby. With respect to the latter, the person in charge of the household was asked about each household member’s medical coverage.
Table 1 shows the joint distribution of the two dependent variables in our analytic sample of 3,890 women. Among the households who did not participate in SP, nearly half paid out of pocket for obstetrical services in the private sector, while the other half had their babies in clinics sponsored by the Secretaría de Salud. Among the households that did participate in SP, the great majority of women (72 percent) had their babies in an SP-sponsored unit, but nearly 21 percent still paid out of pocket for private obstetrical services. Table 1 shows that about 2 percent of women whose households reported not enrolling SP nonetheless reported a birth at an SP-sponsored facility. Apparently, some women whose households had not been enrolled in SP during their pregnancies were enrolled in SP “on the spot” upon their arrival in labor at an SP-sponsored facility.
Table 1.
Obstetric Care in Mexico, by Type of Facility Sponsorship, for Women in Families with and without Seguro Popular (SP), 2001–2006*
| With SP |
Without SP |
|||
|---|---|---|---|---|
| Childbirth in a Facility Sponsored by: | N | (%) | N | (%) |
| Secretaría de Salud (SSA) | 65 | 7.13 | 1,514 | 50.84 |
| Seguro Popular (SP) | 657 | 72.04 | 49 | 1.65 |
| Private Facility | 190 | 20.83 | 1,415 | 47.52 |
| Total | 912 | 100.00 | 2,978 | 100.00 |
Based upon all women who reported their most recent birth during 2001–2006, exclusive of all women whose households reported insurance through IMSS, ISSSTE, PEMEX, SEDENA or other form of Seguridad Social (Social Security).
Source: Calculations based on ENSANUT (Instituto Nacional de Salud Pública (2006)).
Given that the measurement of these dependent variables was based on selfreported survey responses, we performed a number of checks for reliability. To check whether the decision to participate in Seguro Popular is made at the household level, we verified that 90 percent of the respondents who reported themselves as enrolled in SP belonged to households in which the remaining members were likewise enrolled in the SP program. Moreover, we verified that 95 percent of the women reporting participation in SP lived in a household where the person in charge reported a date of affiliation in SP for at least one household member.
We also addressed the possibility that some women who reported current SP participation were not in fact eligible for SP at the time of their delivery. Seguro Popular was rolled out gradually over time in different states throughout Mexico, with most states enrolling in 2002–2004 and all states enrolled by 2005. The official dates of incorporation of each state in SP need to be regarded as approximate, as many localities may not have complied with legally established deadlines. In a separate sensitivity analysis, we reclassified a total of 195 women as not enrolled in SP and not delivering a baby in an SP-accredited facility if the woman reported a date of delivery at an SP-sponsored facility before the official year of incorporation of SP in the state or before the reported date of enrollment reported on the household questionnaire. We then repeated our analyses on this reclassified sample.
4.3. Independent Variables and Instrumental Variables
Our independent variables consisted of individual- and household-level data from ENSANUT, supplemented by data from external sources on the characteristics of the locality or state of the woman’s residence (Secretaría de Salud (2005)). Individual-level variables included the woman’s age and age squared, educational attainment, marital status, parity, primary language (indigenous versus Spanish), and the presence or absence of three self-reported conditions: depression, diabetes, and high blood pressure. (The Spanish texts of these and the previously noted questionnaire items are given in Sosa-Rubí, Galárraga et al. (2007).) Household-level variables included: the presence of young children; rural versus urban location; the proportion of women in the locality who had employment-based health insurance (IMSS, ISSSTE, etc.); the density of public health units in the locality; and an asset index, based upon household infrastructure, building materials, and ownership of certain durable assets, as a proxy for household’s wealth (McKenzie (2004)).
Table 2 shows the descriptive statistics for the independent variables, as well as the marginal proportions of the dependent variables, in our analytic sample. Approximately half of the women had no more than a primary school education, more than a third lived in a rural area, and nearly a quarter spoke an indigenous language. The average family in our sample had low assets and lived in a locality where only 1 in 10 families had employment-based health insurance, and where there were fewer than 1 health center per 100 women. The ratio of the maximum to the minimum density of health centers was nearly two orders of magnitude, and indicated enormous variability in access to formal health services.
Table 2.
Descriptive Statistics
| Analytic Sample (N = 3,890)* |
||||
|---|---|---|---|---|
| Mean | SD | Min | Max | |
| Individual characteristics of woman | ||||
| Age | 29.80 | 6.49 | 18 | 49 |
| Educational attainment: No education¶ | 0.06 | 0.23 | 0 | 1 |
| Educational attainment: Primary school¶ | 0.43 | 0.50 | 0 | 1 |
| Educational attainment: High school¶ | 0.31 | 0.46 | 0 | 1 |
| Educational attainment: Professional/University¶ | 0.20 | 0.40 | 0 | 1 |
| Married¶ | 0.82 | 0.38 | 0 | 1 |
| Speaks indigenous language¶ | 0.23 | 0.42 | 0 | 1 |
| Parity | 3.43 | 2.19 | 1 | 18 |
| Childbirth in a facility sponsored by: | ||||
| Secretaría de Salud (SSA)¶ | 0.41 | |||
| Seguro Popular¶ | 0.18 | |||
| Private¶ | 0.41 | |||
| Reported depression¶ | 0.11 | 0.31 | 0 | 1 |
| Reported diabetes¶ | 0.01 | 0.10 | 0 | 1 |
| Reported high blood pressure¶ | 0.11 | 0.31 | 0 | 1 |
| Household characteristics | ||||
| Family with Children ≤ 7 years old¶ | 0.92 | 0.27 | 0 | 1 |
| Asset Index | −0.25 | 0.91 | −1.99 | 1.58 |
| Access to Seguro Popular program by the family¶ | 0.23 | 0.42 | 0 | 1 |
| Household in rural locality¶ | 0.36 | 0.48 | 0 | 1 |
| Municipality and state characteristics | ||||
| Proportion of households with Seguridad Social§ | 0.10 | 0.08 | 0 | 0.67 |
| Health centers per 100 women† | 0.84 | 0.62 | 0.08 | 5.17 |
| State incorporated into SP program by 2002¶ | 0.64 | |||
| State incorporated into SP program by 2003¶ | 0.79 | |||
| State incorporated into SP program by 2004¶ | 0.92 | |||
Based upon all women who reported their most recent birth during 2001–2006, exclusive of all women whose households reported insurance through Seguridad Social.
Binary variable.
Seguridad Social includes: IMSS, ISSSTE, PEMEX, SEDENA or other form of Social Security.
1,010 observations were imputed at the sample mean value.
Source: Calculations based on ENSANUT (Instituto Nacional de Salud Pública (2006); Secretaría de Salud (2005); Secretaría de Salud (2006)).
For instrumental variables, as described in Section 3.2 above, we constructed dummy variables for each of three years (2002, 2003, and 2004), where the dummy variable for a particular year indicated whether the Seguro Popular had been officially incorporated in the woman’s state of residence by that year. The process of incorporation entailed decisions at the state and federal level, rather than at the level of the individual client or health center. We know of no evidence that such decisions suffered from “policy endogeneity,” that is, states with the highest probability of attracting a pregnant mother to a health center were incorporated earlier. We recognize that the official dates of incorporation are not exact indicators of program availability, since some health centers were still undergoing accreditation by the end of the year. We therefore view these instruments as indicators of likelihood that SP was available to each household in the survey. Our use of year-of-incorporation dummies as instruments is thus analogous to Duflo’s use of distance from schools as instruments in her study of impact of school construction on educational attainment and wages in Indonesia (Duflo (2001)). The year-of-incorporation dummies were thus excluded from the equations (1) and (2) determining the effect of SP enrollment on the site of delivery. However, in a sensitivity analysis to test for the possibility of nationwide trends in obstetric utilization, we did include in equations (1) and (2) dummy variables representing the year in which a pregnant woman delivered her baby.
5. Results
Table 3 presents the results of the simplified bivariate probit model of obstetric care utilization and enrollment in SP for the analytic sample. We show the estimated marginal effects only for the utilization equation on the left (corresponding to equation (7) above), but not for the enrollment equation on the right (corresponding to equation (3) above). In the utilization equation, the significantly positive coefficient for enrollment in SP supported the hypothesis that Seguro Popular has had an effect on obstetric utilization. The estimated marginal effect, which is equivalent to our measure of the impact of the individual-level impact of SP, is 0.430. That is, controlling for other factors affecting the choice of delivery site, a woman in a family enrolled in SP had a probability of giving birth at an SP-accredited facility that was 43 percentage points higher than a woman in a family not enrolled in SP.
Table 3.
Bivariate Probit Model of Obstetric Care Utilization and Enrollment in Seguro Popular
| Childbirth in SP-sponsored facility |
Enrollment in Seguro Popular (SP) |
||
|---|---|---|---|
| Coefficient | Marginal Effect† | Coefficient | |
| Individual characteristics | |||
| Age/10 | −0.038 [0.462] | −0.003 [0.037] | 0.159 [0.296] |
| (Age/10)2 | −0.006 [0.074] | −0.0004 [0.006] | −0.023 [0.047] |
| Primary education¶ | −0.186 [0.157] | −0.014 [0.012] | 0.267 [0.105]* |
| Secondary education¶ | −0.286 [0.168]+ | −0.021 [0.011]+ | 0.298 [0.112]** |
| University education¶ | −0.195 [0.188] | −0.014 [0.012] | −0.115 [0.127] |
| Married¶ | 0.170 [0.105] | 0.012 [0.007]+ | 0.085 [0.064] |
| Speaks indigenous language¶ | −0.103 [0.106] | −0.008 [0.007] | −0.287 [0.059]** |
| Parity | −0.009 [0.021] | −0.001 [0.002] | 0.009 [0.010] |
| Reported depression¶ | 0.086 [0.112] | 0.007 [0.010] | 0.099 [0.078] |
| Reported diabetes¶ | 0.163 [0.261] | 0.015 [0.027] | 0.453 [0.201]* |
| Reported high blood pressure¶ | −0.055 [0.112] | −0.004 [0.008] | 0.107 [0.074] |
| Household characteristics | |||
| Enrollment in Seguro Popular¶ | 2.153 [0.319]** | 0.430 [0.117]** | |
| Household in rural locality¶ | 0.005 [0.103] | 0.0004 [0.008] | 0.323 [0.057]** |
| Family with children ≤ 7 years old¶ | −0.096 [0.121] | −0.008 [0.011] | −0.082 [0.084] |
| Asset Index | −0.042 [0.051] | −0.003 [0.004] | −0.012 [0.034] |
| Locality and state characteristics | |||
| Proportion of households with Seguridad Social§ | 2.950 [0.537]** | 0.234 [0.0523]** | −2.386 [0.378]** |
| Health centers per 100 women | −0.020 [0.064] | −0.002 [0.005] | 0.204 [0.038]** |
| State incorporated into SP by 2002‡ | 0.296 [0.065]** | ||
| State incorporated into SP by 2003‡ | −0.158 [0.084]+ | ||
| State incorporated into SP by 2004‡ | 0.414 [0.120]** | ||
| Constant | −2.218 [0.730]** | −1.745 [0.484]** | |
| Coefficient of correlation of error terms | −0.537 [0.232]* | ||
| Observations | 3,890 | 3,890 | 3,890 |
Binary variable.
Marginal effects evaluated at the mean values of the independent variables (as given in Table 2). Marginal effects correspond to discrete changes of dummy variables from 0 to 1.
Seguridad Social includes: IMSS, ISSSTE, PEMEX, SEDENA or other form of Social Security
Instrumental variable.
Standard errors in brackets;
significant at 10%;
significant at 5%;
significant at 1%
In Table 3, the estimated coefficient of correlation of the error terms is negative and significantly different from zero. While the finding of a non-zero correlation coefficient might support the conclusion that enrollment in SP is an endogenous variable, the negative sign is difficult to explain on the basis of the estimates alone. The other covariates in the enrollment equation do not reveal any related anomalies. In particular, women in rural localities with a higher availability of health centers are more likely to enroll in SP. One might conclude that unobserved factors enhanced the probability of enrollment in SP and, at the same time, diminished the probability of having a baby at an SP-accredited facility. An alternative interpretation, however, is that the simplified bivariate model is not correctly specified.
We therefore turn to Table 4, which shows the results of our full multinomial probit model (equations 1–4) for the analytic sample. The column denoted “SSA vs. Private” refers to a woman’s preference for giving birth at an SSA-sponsored facility in comparison to a private facility, which serves as the reference category. It corresponds to the equation for the latent variable w0 * in equation (2) above. The column denoted “SP vs. Private” refers to a woman’s preference for having a baby at a SP-sponsored facility in comparison to a private facility. It corresponds to the equation for the latent variable w1 * in equation (2) above. Finally, the column denoted “SP Enrollment” refers to the household’s preference for enrollment in Seguro Popular, and corresponds to the equation for the latent variable y2 *, that is, equation (3).
Table 4.
Multinomial Probit Model
| SSA vs. | SP vs. | SP | |
|---|---|---|---|
| Private | Private | Enrollment | |
| Individual characteristics | |||
| Age/10 | 0.316 [0.270] | 0.783 [0.466]+ | 0.149 [0.401] |
| (Age/10)2 | −0.072 [0.043]+ | −0.120 [0.074] | −0.020 [0.064] |
| Primary education¶ | 0.226 [0.097]* | −0.328 [0.164]* | 0.338 [0.154]* |
| Secondary education¶ | 0.168 [0.103] | −0.314 [0.176]+ | 0.372 [0.163]* |
| University education¶ | −0.387 [0.111]** | −0.613 [0.197]** | −0.184 [0.173] |
| Married¶ | −0.206 [0.059]** | −0.021 [0.104] | 0.105 [0.088] |
| Speaks indigenous language¶ | −0.321 [0.055]** | −0.260 [0.099]** | −0.372 [0.103]** |
| Parity | −0.001 [0.009] | −0.034 [0.022] | 0.011 [0.013] |
| Reported depression¶ | 0.067 [0.071] | −0.141 [0.120] | 0.140 [0.109] |
| Reported diabetes¶ | 0.549 [0.233]* | 0.593 [0.301]* | 0.613 [0.290]* |
| Reported high blood pressure¶ | 0.202 [0.071]** | 0.094 [0.117] | 0.176 [0.109] |
| Household characteristics | |||
| Family with children ≤ 7 years old¶ | −0.072 [0.080] | −0.126 [0.130] | −0.146 [0.119] |
| Asset Index | −0.143 [0.031]** | −0.070 [0.052] | −0.041 [0.048] |
| Household in rural locality¶ | 0.169 [0.061]** | 0.030 [0.102] | 0.417 [0.108]** |
| Proportion of households with Seguridad Social§ | 0.297 [0.391] | 1.828 [0.595]** | −3.420 [0.858]** |
| Locality and state characteristics | |||
| Health centers per 100 women | 0.204 [0.039]** | 0.104 [0.064] | 0.270 [0.071]** |
| State incorporated into SP by 2002‡ | 0.384 [0.106]** | ||
| State incorporated into SP by 2003‡ | −0.324 [0.135]* | ||
| State incorporated into SP by 2004‡ | 0.588 [0.194]** | ||
| Constant | −0.060 [0.426] | −2.828 [0.748]** | −2.110 [0.733]** |
| γ0 | −1.988 [0.165]** | ||
| γ1 | 2.792 [0.286]** | ||
| σ0 | 0.901 [0.390]* | ||
| σ1 | −0.143 [0.259] | ||
| Coefficient of correlation ρ0 | 0.666 [0.159]** | ||
| Coefficient of correlation ρ1 | −0.106 [0.187] | ||
| Observations | 3,890 | 3,890 | 3,890 |
Binary variable.
Seguridad Social includes: IMSS, ISSSTE, PEMEX, SEDENA or other form of Social Security
Instrumental variable.
Standard errors in brackets;
significant at 10%;
significant at 5%;
significant at 1%
In the column “SSA vs. Private,” the estimate of the parameter γ0 is negative and highly significant, while in the column “SP vs. Private,” the estimate of the parameter γ1 is positive and highly significant. Accordingly, women in households that participated in the SP program had a much stronger preference for having a baby in a SP-sponsored unit rather than paying out of pocket for a private delivery. At the same time, however, participation in SP was associated with a stronger preference for delivering in the private sector rather than at an SSA-sponsored clinic.
The estimated correlation coefficients ρ0 and ρ1 in the multinomial probit model of Table 4 present a different pattern than that observed in the simplified bivariate probit model of Table 3. The estimate of ρ0 is significantly positive, while the estimate of ρ1 is indistinguishable from zero. Accordingly, there were unobserved factors that enhanced the probability of enrollment in SP and, at the same time, enhanced the probability of preferring an SSA-sponsored facility to a private delivery. In less formal terms, mothers in households attracted to Seguro Popular were more likely to prefer a delivery in staterun SSA-sponsored facilities than to pay out of pocket for a private delivery. The ability of our multinomial model to differentiate between two different types of endogeneity (as specified in equations (2) and (4)) thus permits us to resolve the apparent paradox of a negative correlation coefficient in the simplified bivariate probit model of Table 3.
The estimates in the enrollment equation in Table 4 supported the validity of our year-of-incorporation dummy variables as instruments. The dummy variables for all three years were significant. The significant negative coefficient for the year 2003, during which only four of Mexico’s 32 states were incorporated into SP, implies a reduced marginal effect on enrollment in that year compared to 2004. However, the sum of the dummy variables for 2003 and 2004, which represents the cumulative effect of early incorporation from 2003 onward, was positive (that is, −0.324 + 0.588 = 0.264, standard error 0.142). Likewise, the sum of the three dummy variables, which represents the cumulative effect of early incorporation from 2002 onward, was significantly positive (that is, +0.384 − 0.324 + 0.588 = 0.648, standard error 0.145). Alternative specifications for these instrumental variables, including the addition of a dummy variable for 2001, the specification of a single indicator of the incorporation of SP at the time of delivery, as well as the number of years that SP had been incorporated at the time of delivery, all gave very similar parameter estimates. (Results not shown.)
Moreover, in the enrollment equation in Table 4, residence in a rural locality, a lower proportion of families enrolled in employment-based insurance, and a higher density of health centers all had a significant positive effect, while the women’s speaking an indigenous language had a significant negative coefficient. Self-reported diabetes, education, and indigenous language had significant effects in the site of delivery equations as well.
As noted in Section 3.4 above, we tested interaction models in which the structural parameters γ0 and γ1 in equation (2) depended linearly on the exogenous explanatory variables. However, these models generally did not show significant interaction effects. (Results not shown.) As noted in Section 4.3 above, we also conducted a sensitivity analysis to test for the possibility of nationwide trends in obstetric utilization. To that end, we added dummy variables representing the year in which a pregnant woman delivered her baby into equations (1) and (2). However, none of these annual dummy variables was significant and they were thus dropped from analyses reported in Table 4.
Given the parameter estimates based upon the multinomial probit model in Table 4, we computed the measures of individual-level impact described in Section 3.3. At the mean values of the independent variables, the predicted probability of enrollment in SP (that is, P1 (X) in Section 4.3) was 20.9 percent, and the corresponding individual-level impact on having a baby at an SP-accredited facility (that is, I1 (X) in equation (6)) was 70.6 percent (95% CI, 65.7–75.0). The latter measure of impact was significantly larger than the marginal effect of 40.3 percent estimated from the simplified bivariate probit model in Table 3. In less formal terms, our multinomial probit model detected an impact of Seguro Popular on the decision to have a baby at an SP-accredited site that was nearly double the impact estimated from a simplified bivariate probit model.
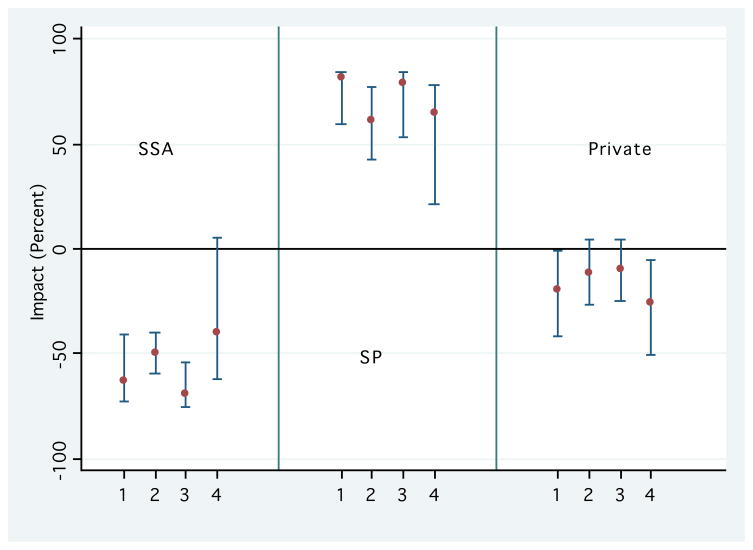
Table 5 and Figure 1 show our computations of the individual-level impact of SP enrollment for four representative cases, that is, four profiles of women based on different values of the explanatory variables. The details of each profile are shown in the notes to Table 5. Cases 1 and 2 refer to women residing in rural areas. For Case 1 (a rural woman without any formal education, who speaks an indigenous language, has low socioeconomic status and reports all three medical conditions), the probability of enrollment in SP was P1 (X) = 43.65 percent, while the individual-level impact was I1 (X) = 82.09 percent (95% CI, 59.13–84.29). By contrast, for Case 2 (a rural woman with at least primary school, who speaks Spanish, has comparatively higher socioeconomic status and does not report medical conditions), the estimated probability of enrollment in the SP was higher (51.51%), but the individual-level impact was notably lower (61.24%; 95% CI, 43.00–72.05). The difference between the individual-level impacts in Case 1 and Case 2 was 20.85 percent (95% CI, −6.96–35.88).
Table 5.
Individual-Level Impacts of Seguro Popular on Obstetric Care Utilization in Mexico, by Rural versus Urban Area, Health and Socioeconomic Status (SES)*
| Probability (%) |
|||
|---|---|---|---|
| Mean | [95% C.I.] | ||
| Case 1: Rural Area, Low Health & SES | |||
| Probability of enrollment in Seguro Popular | 43.65 | ||
| Impact of SP on Probability of Delivering a Baby at: | |||
| Secretaría de Salud (SSA) | −62.56 | −72.31 | −41.20 |
| Seguro Popular | 82.09 | 59.13 | 84.29 |
| Private | −19.52 | −41.98 | −0.69 |
| Case 2: Rural Area, Medium Health & SES | |||
| Probability of enrollment in Seguro Popular | 51.51 | ||
| Impact of SP on Probability of Delivering a Baby at: | |||
| Secretaría de Salud (SSA) | −49.32 | −59.03 | −39.61 |
| Seguro Popular | 61.24 | 43.00 | 77.05 |
| Private | −11.91 | −26.19 | 4.46 |
| Case 3: Urban Area, Medium Health & SES | |||
| Probability of enrollment in Seguro Popular | 53.43 | ||
| Impact of SP on Probability of Delivering a Baby at: | |||
| Secretaría de Salud (SSA) | −68.80 | −75.33 | −54.04 |
| Seguro Popular | 78.91 | 53.29 | 84.33 |
| Private | −10.11 | −25.22 | 4.25 |
| Case 4: Urban Area, High Health & SES | |||
| Probability of enrollment in Seguro Popular | 0.16 | ||
| Impact of SP on Probability of Delivering a Baby at: | |||
| Secretaría de Salud (SSA) | −39.77 | −62.25 | 5.51 |
| Seguro Popular | 65.15 | 21.41 | 78.54 |
| Private | −25.38 | −50.74 | −5.26 |
Derived from multivariate probit estimates at different values of explanatory variables, described below:
Case 1: A 30-year-old woman, without primary education, speaks an indigenous language, parity 5, married in a household with a minimum asset index and with young children at home, lives in a rural locality with an average density of health centers but no households enrolled in Social Security, and reports depression, diabetes, and high blood pressure.
Case 2: A 30-year-old woman, with secondary education, speaks Spanish, parity 3, married in a household with an average asset index and young children at home, lives in a rural locality with an average density of health centers but no households enrolled in Social Security, and does not report depression, diabetes or high blood pressure.
Case 3: A 30-year-old woman, with primary education, speaks Spanish, parity 5, married in a household with a minimum asset index and young children at home, lives in an urban locality with an average density of health centers but no households enrolled in Social Security, and reports depression, diabetes or high blood pressure.
Case 4: A 30-year-old woman, with university education, speaks Spanish, parity 1, married in a household with a mean asset index and young children at home, lives in an urban locality with an average density of health centers and the highest density of households enrolled in Social Security, and does not report depression, diabetes or high blood pressure.
Figure 1.
Individual-Level Impact of Seguro Popular on the Probability of Delivering a Baby at a Site Run by the Department of Health (SSA), a Unit Sponsored by Seguro Popular (SP), and a Private Facility.
Cases 3 and 4 refer to women residing in urban areas. For Case 3 (an urban woman with primary education, who speaks Spanish, has low socioeconomic status and reports depression, diabetes, and high blood pressure), the probability of enrollment in SP was 53.43 percent, while the individual-level impact was 78.91 percent. By contrast, for Case 4 (an urban woman with a university education, who speaks Spanish, has elevated socioeconomic status and does not report medical conditions), the estimated probability of enrollment in the SP was 0.16 percent. Among the very few women with this profile who enroll in SP, the individual-level impact on delivering in an SP-accredited facility was 65.15 percent.
Table 5 and Figure 1 show not only the individual-level impacts on delivering at a SP-accredited facility, but also the corresponding individual-level impacts on having a baby at a SSA-sponsored health unit (that is, I0 (X)) and a private facility (that is, I2 (X)). In each of the four cases, but especially in Cases 1 through 3, the Seguro Popular program reduced pregnant women’s attendance at an SSA-sponsored clinic much more than it reduced the probability of delivering a baby in the private sector.
As noted above, we carried out sensitivity analyses on three alternative samples: the extended sample, the restricted sample, and the reclassified sample. In all cases, our multinomial probit estimates were robust with respect to different assumptions about the study population and the definitions of the dependent variables. The full results are reported in Sosa-Rubí, Galárraga et al. (2007).
6. Discussion and Conclusions
In this paper, we found that the recently established Seguro Popular program in Mexico has had a significantly positive effect on the access of poor women to obstetrical care, an important outcome measure of maternal and infant health. Women in households that participated in the SP program, we found, had a much stronger preference for having a baby in a SP-sponsored unit rather than paying out of pocket for a private delivery. At the same time, participation in SP was associated with a stronger preference for delivering in the private sector rather than at an SSA-sponsored clinic. On balance, the Seguro Popular program reduced pregnant women’s attendance at an SSA-sponsored clinic much more than it reduced the probability of delivering a baby in the private sector. These findings were robust with respect to variations in the population under study, the classification of subjects’ survey responses, and the specification of the statistical model.
We formulated a multinomial probit model that permitted us to go beyond the standard two-way dichotomy between utilization and non-utilization as outcome measures in the evaluation of policies designed to subsidize and increase access to health care. We found that the conventional bivariate probit approach suffered from apparent problems of model misspecification, with a peculiarly negative correlation coefficient between error terms in the obstetrical utilization and Seguro Popular enrollment equations. What is more, estimates based the standard two-equation approach understated the impact of Seguro Popular on obstetrical utilization by 40 percent.
Our modification of the multivariate probit model to account of a discrete endogenous variable appears to be the first instance of such a model specification. Early applications of multinomial discrete choice models in the selection of health care providers include the works of Schwartz, Akin et al. (1988) in the setting of the Philippines, Akin, Guilkey et al. (1995) in Nigeria, and Bolduc, Lacroix et al. (1996) in Benin, and most recently Borah (2006) in India and Leonard (2007) in Tanzania. However, these papers did not explicitly incorporate endogeneity of the treatment or policy variable into the multinomial choice framework.
Other investigators have employed variations of the now-standard bivariate probit model, in which an endogenous binary participation variable enters on the right-hand side of a probit utilization equation. (See Bertranou (1998) in the setting of Argentina; Cameron, Trivedi et al. (1988) in Australia; Gitto, Santoro et al. (2006) in Sicily; Sapelli and Vial (2003) in Chile; Suraratdecha, Saithanu et al. (2005) in Thailand; and Waters (1999) in Ecuador.) Trujillo (2003) specified a binary utilization variable as well as two endogenous binary variables to represent participation in both public and private insurance programs in Colombia.
Still other researchers have considered multi-equation models in which one or more equations entailed a discrete endogenous variable. Munkin and Trivedi (2003) specified a three-equation model in which one demand equation entailed Poisson-distributed count data, the second demand equation contained a continuous exponential dependent variable, and the third participation equation involved a binary dependent variable representing self-selection of insurance coverage. Deb, Munkin et al. (2006) specified a multi-equation model for health care utilization, in which the first equation was a probit model of non-zero health-care utilization, the second was conditional log-linear expenditure model, and the third was a multinomial probit model for choice of insurance coverage. The latter model, like that of Munkin and Trivedi (2003), was estimated by Markov chain Monte Carlo simulation techniques. Balia and Jones (2004), in a study of health habits and mortality, specified a recursive multi-equation model, in which each binary lifestyle variable (such as smoking) served as a dependent variable in a behavioral equation and as a regressor in a mortality equation. Meyerhoefer and Pylypchuk (2008) specified a three-category ordered probit model for body mass index that contained a discrete endogenous variable representing participation in the US Food Stamp Program. Our model in this paper can be readily estimated by full maximum likelihood, taking advantage of now-standard techniques to evaluate three-dimensional probit integrals, such as the GHK simulator written by Cappellari and Jenkins (2006). (See Appendix A.)
We based our analysis of heterogeneous impacts on four cases, which represented different profiles of women based on the values of the observed independent variables. While the simulated confidence intervals around the impact measures were relatively wide, nonetheless we observed significant variability in individual-level impacts. A comparison of Cases 1 and 2, both women residing in urban areas, is illustrative. A woman in Case 1 spoke an indigenous language, had low socioeconomic status and reported multiple medical conditions, while a woman in Case 2 had a primary school education, spoke Spanish, had comparatively higher socioeconomic status, and did not report any medical conditions. In Case 1, the individual-level impact of Seguro Popular on the probability of having a baby at a SP-accredited facility was 21 percentage points higher than in Case 2, and the 95% confidence interval of this difference in individual-level impacts ranged from −7% to +36%.
In our analysis of heterogeneous impacts, we relied upon the nonlinearity of our econometric model. In addition, we tested the effects of interactions between treatment variables and other explanatory variables. Having specified a parametric joint distribution for the error terms (ε0, ε1, ε2), we did not explore more generalized nonparametric procedures, such as quantile treatment effects regression (Djebbari and Smith (2005); Dammert (2007)), and thus our analysis does not capture the full extent of heterogeneity of program impact due to variations in unobservables.
Our empirical findings on the substantial impact of Seguro Popular confirm the preliminary results reported by Gakidou, Lozano et al. (2006), who found a positive relation between hospital discharge rates per capita and the rate of SP enrollment in a regression analysis of a cross-section of Mexican municipalities. These authors also reported a positive relation between the probability of using health services and SP enrollment, conditional on perceived need, based upon a cross-sectional regression study of the 2006 ENSANUT survey, but details of the methodology were not reported.
Our observational study has a number of limitations. We relied upon selfreported data, which inevitably contains response errors. Although we performed a number of reliability checks of our data, uncertainty due to errors in reporting cannot be eliminated. Nonetheless, our results remained robust with respect to changes in the sample analyzed and the definitions of the dependent variables. We have no direct measures of the characteristics of the obstetric facilities selected by the pregnant women and their families. It is well recognized that such characteristics are a critical determinant of the choice of site of care (Leonard (2007)). In the case of obstetric services in Mexico, direct measurement of the level of training of personnel, accessibility of rural sites, and the state of medical equipment would be very valuable, especially if we are to assess the adequacy of the accreditation process employed by Seguro Popular. Measurement of the quality of state-run SSA-sponsored sites would be valuable in determining why SP-enrolled women expressed a much stronger preference for SP-accredited sites over SSA-sponsored sites.
We distinguished between SP-accredited health units, SSA-sponsored facilities, and private care. While we excluded women who had employment-based health insurance from our analytic sample, the category of “private care” nonetheless remains heterogeneous, ranging from the services of private obstetricians within hospitals to traditional midwives who work outside the hospital setting. In our ENSANUT analytic sample, the latter category comprised only 10.36 percent of all reported deliveries. (Results not shown.) Increasing the number of sites of obstetric care would have required additional computational resources to evaluate a four-dimensional probit model in samples with up to 6,000 observations.
Finally, our analysis covers the time period 2001–2006, during which the Seguro Popular program was being gradually phased in throughout Mexico. Within the limits of currently available data, we cannot test the hypothesis that the impact of Seguro Popular has changed as the Mexican people have come to learn of its advantages, or as the quality of SP-accredited facilities has further improved.
A number of findings in Table 4 give us cause for concern. The coefficients for women who speak an indigenous language are negative, that is, non-Spanish speaking women appeared less likely to enroll in and take advantage of Seguro Popular. The family asset index has a negative coefficient in the equation for SSA versus Private, suggesting that some poor families were still paying out of pocket for private care. The coefficient for a rural household is significant in the SP enrollment equation, but is not significant in the equation for SP versus Private, suggesting that rural households enrolled in SP but pregnant women within those households did not take advantage of the program. These findings suggest a continued focus on the availability of Seguro Popular for the very poorest and particularly indigenous households in rural areas.
Perhaps the most troubling findings, however, are the relative impacts on SSA-sponsored and private obstetrical care that we observed in Table 5. On balance, enrollment in Seguro Popular reduced deliveries at state-run SSA-sponsored facilities much more than it reduced the use of private obstetrical services. One explanation is that SSA-sponsored facilities, in which trained staff and adequate equipment are not guaranteed, may be perceived as low quality. In the language of consumer theory, the obstetric care at state-sponsored SSA facilities may be an inferior good. The demand-side subsidy of medical care for all members of an SP-affiliated household may have an income effect, which may then diminish the demand for SSA-sponsored care. In less formal terms, when SP pays for treatment of the complications of a parent’s diabetes, a pregnant daughter may be able to afford a private obstetrician.
Other possible explanations for the reduced impact of SP on private obstetric care are less compelling. For example, we have no evidence that private providers dropped prices in response to SP entry into the market. Nor do we have evidence SP selectively certified only the highest quality state-run facilities, thus rendering the remaining SSA-sponsored units even less qualified. Likewise we lack evidence that private facilities may be serving as alternatives to SP-sponsored facilities with inadequate capacity. SP-accredited obstetric facilities were not necessarily available in every locality, so that the choice between an SP-accredited and an SSA-sponsored unit was not simply a passive decision made by clinic personnel. More research is required to determine why poor uninsured Mexican women still pay out of pocket for obstetrical care despite the substantial impacts of Seguro Popular documented in this paper.
Acknowledgments
We acknowledge the research assistance of Edson Serván-Mori. We are grateful for the critical comments of our colleagues at the National Institute of Public Health and the Massachusetts Institute of Technology, where we presented seminars based on an earlier version of this paper (Sosa-Rubí, Galárraga et al. (2007)). We are also grateful for the critical comments of an Associate Editor and an anonymous referee. Nonetheless, we alone remain responsible for the contents of this paper.
Appendix A. Construction and Estimation of Log Likelihood Function
We derive the contribution to the log likelihood for each of the six possible cases {(y1,y2)|y1 = 0,1,2; y2= 0,1}.
First consider an observation where y1 = 0,y2 = 1, that is, where the pregnant woman chooses an obstetric site sponsored by the Secretaría de Salud, and where the household decides to enroll in Seguro Popular. From equations (1) through (3), we conclude that-−w0* < 0, w1*−w0*<0, −y2* < 0 or, equivalently, , where and where the vector inequality holds for each coordinate. Given equations (1) through (3), the foregoing implies , or
| (A.1) |
The vector on the left-hand side of (A. 1) has trivariate normal distribution with zero means and variance-covariance matrix where and . Moreover, the expression on the right-hand side of (A.1) is equivalent to . We thus conclude that the contribution of this observation to the log likelihood is
| (A.2) |
In (A.2), the term Φ3(ν,Ω) denotes Pr{V < ν}, where V is a 3-dimensional vector of random variables with a trivariate normal distribution with zero means and 3×3 variance-covariance matrix Ω.
More generally, for each of the six cases {(y1 = j,y2 = k)| j = 0,1,2; k = 0,1}, the vector inequality (A.1) holds for a suitably chosen matrix
| (A.3) |
The corresponding contribution to the log likelihood function is
| (A.4) |
where . These contributions to the log likelihood function entail three-dimensional probit integrals, which we evaluated by means of the GHK simulator written by Cappellari and Jenkins (2006).
Contributor Information
Sandra G. Sosa-Rubi, Email: srubi@insp.mx.
Omar Galárraga, Email: ogalarraga@insp.mx.
Jeffrey E. Harris, Email: jeffrey@mit.edu.
References
- Akin JS, Guilkey DK, et al. Quality of services and demand for health care in Nigeria: a multinomial probit estimation. Soc Sci Med. 1995;40(11):1527–37. doi: 10.1016/0277-9536(94)00274-w. [DOI] [PubMed] [Google Scholar]
- Balia S, Jones AM. Lifestyle and Socio-Economic Status. York: United Kingdom, University of York, Department of Economics; 2004. Mortality. Working Paper. [DOI] [PubMed] [Google Scholar]
- Behrman JR, Skoufias E. Mitigating Myths about Policy Effectiveness: Evaluation of Mexico’s Antipoverty and Human Resource Investment Program. Annals Am Acad Political Social Sci. 2006;606(1):244–275. [Google Scholar]
- Bertranou F. Health care services utilization and health insurance coverage: evidence from Argentina. Revista de Análisis Económico (Universidad Alberto Hurtado Chile) 1998;13:25–52. [Google Scholar]
- Bolduc D, Lacroix G, et al. The choice of medical providers in rural Benin: a comparison of discrete choice models. J Health Econ. 1996;15(4):477–98. doi: 10.1016/s0167-6296(96)00492-4. [DOI] [PubMed] [Google Scholar]
- Borah BJ. A mixed logit model of health care provider choice: analysis of NSS data for rural India. Health Econ. 2006;15(9):915–32. doi: 10.1002/hec.1166. [DOI] [PubMed] [Google Scholar]
- Cameron AC, Trivedi PK, et al. A microeconometric model of the demand for health care and health insurance in Australia. Review of Economic Studies. 1988;55(1):85–106. [Google Scholar]
- Cappellari L, Jenkins SP. Calculation of multivariate normal probabilities by simulation, with applications to maximum simulated likelihood estimation. Colchester UK: University of Essex, Institute for Social and Economic Research; 2006. Working Paper 2006–16. [Google Scholar]
- Chávez-Martín del Campo JC. The Progresa Experience. Ithaca NY: Cornell University, Department of Applied Economics and Management; 2006. Does Conditionality Generate Heterogeneity and Regressivity in Program Impacts? Working Paper 2006–09. [Google Scholar]
- CONAPO. 2005 Distrito Federal. Mexico: Consejo Nacional de Población (CONAPO); 2005. Índice de marginación a nivel localidad. http://www.conapo.gob.mx/publicaciones/indice2005xloc.htm. [Google Scholar]
- Dammert AC. Hamilton, Ontario, Canada: McMaster University, Department of Economics Working Paper; 2007. Heterogeneous impacts of conditional cash transfers: Evidence from Nicaragua. http://socserv.mcmaster.ca/dammert/nicaragua_APRIL07.pdf. [Google Scholar]
- Deb P, Munkin MK, et al. Bayesian analysis of the two-part model with endogeneity: application to health care expenditure. Journal of Econometrics. 2006;21(7):1081–99. [Google Scholar]
- Djebbari H, Smith J. Heterogeneous program impacts: Experimental evidence from the PROGRESA program. Ann Arbor, Michigan: University of Michigan, Department of Economics; 2005. Working Paper. [Google Scholar]
- Duflo E. Schooling and Labor Market Consequences of School Construction in Indonesia: Evidence from an Unusual Policy Experiment. American Economic Review. 2001;91(4):795–813. [Google Scholar]
- Frenk J, Sepulveda J, et al. Evidence-based health policy: three generations of reform in Mexico. Lancet. 2003;362(9396):1667–71. doi: 10.1016/S0140-6736(03)14803-9. [DOI] [PubMed] [Google Scholar]
- Gakidou E, Lozano R, et al. Assessing the effect of the 2001–06 Mexican health reform: an interim report card. Lancet. 2006;368(9550):1920–35. doi: 10.1016/S0140-6736(06)69568-8. [DOI] [PubMed] [Google Scholar]
- Gaviria A, Medina C, et al. Evaluating The Impact Of Health Care Reform In Colombia: From Theory To Practice. Bogotá, Colombia: Universidad de Los Andes-CEDE; 2006. Documento CEDE 2006–06. [Google Scholar]
- Gertler PJ. Final Report: The Impact of PROGRESA on Health. Washington DC: International Food Policy Research Institute; 2000. http://www.ifpri.org/themes/progresa/pdf/Gertler_health.pdf. [Google Scholar]
- Gertler PJ. Do conditional cash transfers improve child health? Evidence from PROGRESA’s control randomized experiment. American Economic Review. 2004;94(2):336–341. doi: 10.1257/0002828041302109. [DOI] [PubMed] [Google Scholar]
- Gitto L, Santoro D, et al. Choice of dialysis treatment and type of medical unit (private vs public): application of a recursive bivariate probit. Health Econ. 2006;15(11):1251–6. doi: 10.1002/hec.1139. [DOI] [PubMed] [Google Scholar]
- Greene WH. Econometric Analysis. 4. Upper Saddle River, NJ: Prentice Hall; 2000. [Google Scholar]
- Hoddinott J, Skoufias E. The Impact of PROGRESA on Food Consumption. Economic Development and Cultural Change. 2004;53:37–61. [Google Scholar]
- Instituto Nacional de Salud Pública. Encuesta Nacional de Salud. Cuernavaca, México: Instituto Nacional de Salud Pública; 2000. http://www.insp.mx/ensa/ [Google Scholar]
- Instituto Nacional de Salud Pública. Encuesta Nacional de Salud y Nutrición (ENSANUT) Cuernavaca, México: Instituto Nacional de Salud Pública; 2006. http://www.insp.mx/ensanut/ [Google Scholar]
- Knaul FM, Frenk J. Health insurance in Mexico: achieving universal coverage through structural reform. Health Aff (Millwood) 2005;24(6):1467–76. doi: 10.1377/hlthaff.24.6.1467. [DOI] [PubMed] [Google Scholar]
- Leonard KL. Learning in Health Care: Evidence of Learning about Clinician Quality in Tanzania. Economic Development and Cultural Change. 2007;55:531–555. [Google Scholar]
- Maddala G. Limited Dependent and Qualitative Variables in Econometrics. New York: Cambridge University Press; 1983. [Google Scholar]
- McKenzie DJ. Measuring inequality with asset indicators. Journal of Population Economics. 2004;18(2):229–260. [Google Scholar]
- Meyerhoefer CD, Pylypchuk Y. Does participation in the food stamp program increase the prevalence of obesity and health spending? American Journal of Agricultural Economics. 2008;90(2):287–305. [Google Scholar]
- Munkin MK, Trivedi PK. Bayesian analysis of a self-selection model with multiple outcomes using simulation-based estimation: an application to the demand for healthcare. Journal of Econometrics. 2003;114:197–220. [Google Scholar]
- Nigenda G, Troncoso E, et al. Mezcla público-privada en el sector salud. Reflexiones sobre la situación en México. In: Knaul FM, Nigenda G, editors. Caleidoscopio de la salud: De la investigación a las políticas y de las políticas a la acción. Distrito Federal, México: Fundación Mexicana para la Salud; 2003. pp. 229–242. [Google Scholar]
- Pagan JA, Puig A, et al. Health insurance coverage and the use of preventive services by Mexican adults. Health Econ. 2007 doi: 10.1002/hec.1226. [DOI] [PubMed] [Google Scholar]
- Parker SW, Wong R. Household income and health care expenditures in Mexico. Health Policy. 1997;40(3):237–55. doi: 10.1016/s0168-8510(97)00011-0. [DOI] [PubMed] [Google Scholar]
- Sapelli C, Vial B. Self-selection and moral hazard in Chilean health insurance. J Health Econ. 2003;22(3):459–76. doi: 10.1016/S0167-6296(02)00121-2. [DOI] [PubMed] [Google Scholar]
- Schwartz JB, Akin JS, et al. Price and income elasticities of demand for modern health care: The case of infant delivery in the Philippines. World Bank Economic Review. 1988;2(1):49–76. doi: 10.1093/wber/2.1.49. [DOI] [PubMed] [Google Scholar]
- Secretaría de Salud. Distrito Federal. México: Secretaría de Salud (SSA); 2005. Sistema Nacional de Información en Salud (On-line Database) http://sinais.salud.gob.mx/ [Google Scholar]
- Secretaría de Salud. Distrito Federal. 1–3. México: Secretaría de Salud (SSA), Gobierno de México; 2006. Sistema de Protección Social en Salud. [Google Scholar]
- Sepúlveda J, Bustreo F, et al. Improvement of child survival in Mexico: the diagonal approach. Lancet. 2006;368(9551):2017–27. doi: 10.1016/S0140-6736(06)69569-X. [DOI] [PubMed] [Google Scholar]
- Skoufias E. Washington DC: International Food Policy Research Institute; 2005. PROGRESA and Its Impacts on the Welfare of Rural Households in Mexico (Summary) Research Report 139, http://www.ifpri.org/pubs/abstract/139/rr139toc.pdf. [Google Scholar]
- Skoufias E, Parker SW. Conditional Cash Transfers and Their Impact on Child Work and Schooling: Evidence from the PROGRESA Program in Mexico. Economia. 2001;2(1):45–96. [Google Scholar]
- Sosa-Rubí S, Galárraga O, et al. Cambridge MA: National Bureau of Economic Research; 2007. Heterogeneous impact of the ‘Seguro Popular’ Program on the Utilization of Obstetrical Services in Mexico, 2001–2006: A Multinomial Probit Model with a Discrete Endogenous Variable. Working Paper No. 13498, http://www.nber.org/papers/w13498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 9. College Station TX: StataCorp LP; 2005. [Google Scholar]
- Suraratdecha C, Saithanu S, et al. Is universal coverage a solution for disparities in health care? Findings from three low-income provinces of Thailand. Health Policy. 2005;73(3):272–84. doi: 10.1016/j.healthpol.2004.11.019. [DOI] [PubMed] [Google Scholar]
- Thirumurthy H, Zivin JG, et al. Hatfield, South Africa: Southern Africa Regional Poverty Network; 2006. The economic impact of AIDS Treatment: Labor supply in Western Kenya. http://www.sarpn.org.za/documents/d0001904/Impact-Aids_Jan2006.pdf. [PMC free article] [PubMed] [Google Scholar]
- Torres AC, Knaul FM. Determinantes del gasto de bolsillo en salud e implicaciones para el aseguramiento universal en México: 1992–2000. In: Knaul FM, Nigenda G, editors. Caleidoscopio de la salud: De la investigación a las políticas y de las políticas a la acción. Distrito Federal, México: Fundación Mexicana para la Salud; 2003. pp. 209–225. [Google Scholar]
- Trujillo AJ. Medical care use and selection in a social health insurance with an equalization fund: evidence from Colombia. Health Econ. 2003;12(3):231–46. doi: 10.1002/hec.711. [DOI] [PubMed] [Google Scholar]
- Trujillo AJ, Portillo JE, et al. The impact of subsidized health insurance for the poor: evaluating the Colombian experience using propensity score matching. International Journal of Health Care Finance and Economics. 2005;5(3):211–39. doi: 10.1007/s10754-005-1792-5. [DOI] [PubMed] [Google Scholar]
- Wagstaff A. Washington DC: World Bank Impact Evaluation; 2007. Health insurance for the poor: initial impacts of Vietnam’s health care fund for the poor. Series No. 11, Policy Research Working Paper No. WPS4134, http://www-wds.worldbank.org/external/default/WDSContentServer/IW3P/IB/2007/02/05/000016406_20070205110453/Rendered/PDF/wps4134.pdf. [Google Scholar]
- Wagstaff A, Lindelow M, et al. Washington DC: World Bank Impact Evaluation; 2007. Extending Health Insurance to the Rural Population: An Impact Evaluation of China’s New Cooperative Medical Scheme. Series No. 12, Policy Research Working Paper No. WPS4150, http://www-wds.worldbank.org/external/default/WDSContentServer/IW3P/IB/2007/02/22/000016406_20070222160135/Rendered/PDF/wps4150.pdf. [DOI] [PubMed] [Google Scholar]
- Waters HR. Measuring the impact of health insurance with a correction for selection bias--a case study of Ecuador. Health Econ. 1999;8(5):473–83. doi: 10.1002/(sici)1099-1050(199908)8:5<473::aid-hec453>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]