Abstract
Background
Indications for immediate cardiac catheterization in cardiac arrest survivors without ST elevation myocardial infarction (STEMI) are uncertain as electrocardiographic and clinical criteria may be challenging to interpret in this population. We sought to evaluate rates of early catheterization after in-hospital ventricular fibrillation (VF) arrest and the association with survival.
Methods
Using a billing database we retrospectively identified cases with an ICD-9 code of cardiac arrest (427.5) or VF (427.41). Discharge summaries were reviewed to identify in-hospital VF arrests. Rates of catheterization on the day of arrest were determined by identifying billing charges. Unadjusted analyses were performed using chi square, and adjusted analyses were performed using logistic regression.
Results
110 in-hospital VF arrest survivors were included in the analysis. Cardiac catheterization was performed immediately or within one day of arrest in 27% (30/110) of patients and of these patients, 57% (17/30) successfully received percutaneous coronary intervention. Of those who received cardiac catheterization the indication for the procedure was STEMI or new left bundle branch block (LBBB) in 43% (13/30). Therefore, in the absence of standard ECG data suggesting acute myocardial infarction, 57% (17/30) received angiography. Patients receiving cardiac catheterization were more likely to survive than those who did not receive catheterization (80% vs. 54%, p<.05).
Conclusion
In patients receiving cardiac catheterization, more than half received this procedure for indications other than STEMI or new LBBB. Cardiac catheterization was associated with improved survival. Future recommendations need to be established to guide clinicians on which arrest survivors might benefit from immediate catheterization.
Keywords: cardiac arrest, post-resuscitation period, ventricular fibrillation, cardiac catheterization
Introduction
Coronary artery disease is common in patients who experience out-of-hospital cardiac arrest (OHCA). Acute coronary artery occlusion has been identified as the etiology of arrest in up to 48% of post-arrest survivors.1 In autopsy series, coronary artery thrombi or atherosclerotic plaque fissuring have been identified in up to 95% of patients with sudden cardiac death.2, 3 Identifying post-arrest patients likely to have acute coronary artery occlusion can be challenging because electrocardiographic (ECG) findings and clinical data may be unreliable in this population. 1 Immediate coronary angiography is considered to be helpful for determining the presence and or extent of coronary pathology. In those with coronary occlusion complicated by cardiac arrest, percutaneous coronary intervention (PCI) is associated with improved survival. 1, 4–6
The mechanisms and pathophysiology leading to in-hospital cardiac (IHCA) arrest may be different from out-of-hospital events. For example, severe infection, respiratory compromise, and pulmonary embolism are often precipitating events for IHCA.7 Survival after in-hospital arrest is generally higher than OHCA 8, 9, in part because rapid assessment and treatment of these and other precipitating events can occur.
The number of IHCA survivors who could benefit from immediate cardiac catheterization and PCI is unknown. We sought to evaluate the number of in-hospital post-arrest patients who received cardiac catheterization. We also evaluated rates of survival to hospital discharge after IHCA and factors that could be associated with improved outcomes.
Methods
This study was an Institutional Review Board approved retrospective review of adult (age >18) in-hospital cardiac arrests that occurred between June 1, 2000 and June 31, 2005 at the University of Chicago hospital. An arrest was considered “in-hospital” using criteria defined by the in-hospital National Registry of Cardiopulmonary Resuscitation (NRCPR). 8 Our hospital does not have a specific medical response team that responds pre-arrest to decompensating patients.
Using the hospital computerized billing database we retrospectively identified all cases with an International Classification of Diseases, 9th revision (ICD-9) principal or secondary diagnosis of cardiac arrest (427.5) or ventricular fibrillation (427.41). We specifically reviewed cases with ventricular fibrillation (VF) as the initial arrest rhythm assuming that this group was more likely to have an arrest of cardiac etiology.
Demographic data, length of stay, procedures, admission source, and discharge to home or facility were obtained from billing records about each case. Using these data, several criteria were applied to identify survivors of in-hospital cardiac arrest. Patients with only outpatient charges were excluded. All patients with a length of stay of zero and discharged home were excluded. We reviewed discharge summaries from a random 5% sample of this group and none of these patients were noted to have experienced a cardiac arrest.
Because arrest date, initial rhythm, and suspected arrest etiology could not be obtained from billing data alone, we reviewed patient charts and discharge summaries when necessary to identify this information. We excluded OHCA, arrests with an initial rhythm other than VF, and arrests without return of spontaneous circulation (ROSC).
Billing data were used to identify in-hospital charges for left heart cardiac catheterization. Because service charges were recorded by day and not time, we reviewed all records with a charge for cardiac catheterization on the day of arrest (day 0) or day after arrest (day 1). Catheterization procedures occurring on day 0 and noted in the procedure report to be pre-arrest were excluded. Cardiac catheterization reports were reviewed to determine such factors as proximity of arrest to procedure, indications for the procedure, and angiographic findings. Clinically insignificant coronary artery disease was considered stenosis less than 50% and clinically significant stenosis was considered stenosis greater than 50%. If documentation of PCI was present, successful PCI was considered residual stenosis < 50% and Thrombolysis in Myocardial Infarction (TIMI) 3 flow.
ECG’s on the day of arrest were also reviewed. STEMI or left bundle branch block (LBBB) was identified by ECG report and/or documentation in the “indication for procedure” on the cardiac catheterization report. In patients with LBBB additional ECG’s and chart review occurred to determine if the LBBB was new or old.
In addition to cardiac catheterization, we also evaluated use of post-arrest therapeutic hypothermia as this procedure is associated with improved neurologic outcomes and survival. 10, 11 Charges for post-arrest hypothermia were not included in the billing database, so we used discharge summaries and charts to evaluate for implementation of cooling.
Data were managed using a spreadsheet application (Microsoft Excel, Redmond, WA) and analyzed in a statistical software application (Stata Version 9.0, College Station, TX). Descriptive statistics (mean, SD) are primarily presented. Factors thought to be related to survival were analyzed using chi-square and logistic regression. Alpha <.05 was considered significant.
Results
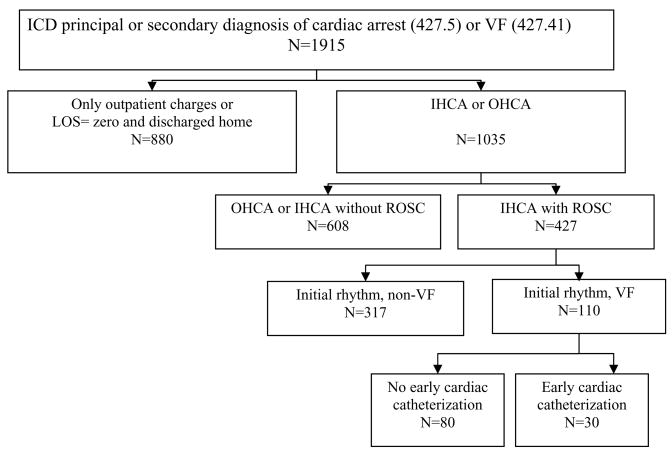
There were 110 patients who survived in-hospital cardiac arrest with an initial rhythm of VF (Figure 1). Cardiac catheterization was performed in 27% (30/110) of these patients on the day of arrest. When comparing demographic data for patients who received cardiac catheterization with those who did not receive the procedure, age and gender were similar across groups but patients receiving catheterization were more likely to be African-American and have a history of cardiovascular disease (Table 1). Rates of post-arrest hypothermia were low in both groups (n=5), with 2 patients in the catheterization group receiving hypothermia and 3 patients in the non-catheterization group receiving hypothermia.
Figure 1.
Flow diagram of study population
This figure illustrates how exclusion criteria were applied to determine the final study population: in-hospital cardiac arrest patients with return of spontaneous circulation and an initial rhythm of ventricular fibrillation
ICD: International Classification of Diseases; VF: ventricular fibrillation; LOS: length of stay; IHCA: in-hospital cardiac arrest; OHCA: out-of hospital cardiac arrest; ROSC: return of spontaneous circulation
Table 1.
Demographics of the study population
| Cardiac catheterization (n=30) | No cardiac catheterization (n=80) | |
|---|---|---|
| Race | ||
| African-American | 18(60%) | 32(40%) |
| Caucasian | 6(20%) | 29(36%) |
| Other/Unknown | 6(20%) | 19(24%) |
| Gender (male) | 18(60%) | 47(59%) |
| Age mean±sd, (range) | 67±11, (43–83) | 63±15(18–90) |
| Past medical history | ||
| Hypertension | 20(67%) | 41(51%) |
| Congestive heart failure | 4(13%) | 16(20%) |
| Coronary artery disease | 15(50%) | 25(31%) |
| Myocardial infarction | 7(23%) | 15(19%) |
| Diabetes | 13(43%) | 26(33%) |
| Malignancy | 4(13%) | 9(11%) |
| Length of stay mean (range) | 11,(1–44) | 19,(1–66) |
sd, standard deviation
In patients who received cardiac catheterization, the indication for the procedure was STEMI or new LBBB in 43% (13/30). Of note only one patient had a new LBBB. All of these patients had clinically significant coronary artery disease (13/13) and 92% (12/13) had successful PCI.
Several patients received cardiac catheterization for indications other than STEMI or new LBBB 57% (17/30). Of this group, PCI was attempted in 35% (6/17) of patients and successful in 29% (5/17). Two patients (12%) also received coronary artery bypass graft (CABG) surgery (Table 2).
Table 2.
Angiographic Data
| Indication for post-arrest cardiac catheterization | ||
|---|---|---|
| STEMI or new LBBB (n=13) | Not STEMI or new LBBB (n=17) | |
| Presumed arrest etiology: | ||
| Acute coronary artery occlusion (total occlusion) | 10(77%) | 6(35%) |
| Coronary artery disease (90% occlusion) | 3(23%) | 4(23%) |
| Coronary vasospasm | 0 | 1(6%) |
| Metabolic/electrolyte abnormality | 0 | 2(12%) |
| Cardiogenic shock | 0 | 1(6%) |
| Acute respiratory insufficiency | 0 | 2(12%) |
| Unknown | 0 | 1(6%) |
| Normal coronary arteries | 0 | 5(29%) |
| Clinically insignificant coronary artery disease (<50% stenosis) | 0 | 2(12%) |
| Clinically significant coronary artery disease (>50% stenosis) | ||
| 1 vessel | 3(23%) | 2(12%) |
| 2 vessels | 7(54%) | 4(24%) |
| 3 vessels | 3(23%) | 4(24%) |
| PCI attempted | 13(100%) | 6(35%) |
| PCI successful | 12(92%) | 5(29%) |
| IABP inserted | 4(31) | 3(18) |
| CABG | 0 | 2(12%) |
STEMI: ST elevation myocardial infarction; LBBB: left bundle branch block; PCI: percutaneous coronary intervention; IABP: intra-aortic balloon pump; CABG: coronary artery bypass graft
Patients who received cardiac catheterization were more likely to survive than those who did not receive cardiac catheterization (80% vs. 54%, p<.05). Survivors were more likely to be discharged to home instead of to an inpatient facility (Table 3). Those successfully receiving PCI were also more likely to survive (76% vs. 58%, p<.05) when compared with those who did not receive the procedure.
Table 3.
Hospital discharge location
| Cardiac catheterization (n=30) | No cardiac catheterization (n=80) | |
|---|---|---|
| Died | 6(20%) | 37(46%) |
| Lived | ||
| Home | 18(60%) | 22(28%) |
| Home health | 3(10%) | 3(4%) |
| Short term care facility | 0 | 2(2%) |
| Long term care facility/inpatient rehabilitation | 3(10%) | 16(20%) |
Controlling for age, gender, race, and hypothermia using logistic regression, the relationship between cardiac catheterization and survival persisted with patients undergoing cardiac catheterization having an almost 4-fold increased odds of survival (OR 3.8, 95% CI 1.35–10.90, p<.05). We next considered patients with STEMI or new LBBB and patients without STEMI or new LBBB who received cardiac catheterization separately. Among patients with STEMI or new LBBB all received cardiac catheterization, thus an OR could not be calculated. 85% (11/13) of this group survived to hospital discharge. Among patients without STEMI or new LBBB, 76% (13/17) survived to hospital discharge, but this was not significant, OR 3.01, (95% CI 0.84–10.8, p=.091)
Of the patients who did not receive a cardiac catheterization within 1 day (n=80), one patient was offered the procedure but the family refused. The etiology of arrest could not be determined from discharge summary or chart review in 59% (47/80) of this group.
Discussion
We used a hospital billing database to identify survivors of in-hospital VF arrest who received cardiac catheterization. Limited data exist to help clinicians determine which post-arrest patients warrant early cardiac catheterization. Previous reports have demonstrated that emergent angiography and PCI are beneficial in patients with STEMI complicated by cardiac arrest. Survival rates of 54–70% have been reported in this patient group. 4, 6, 12, 13 In addition, Gorjup et al. reported that a subset of OHCA patients with STEMI and subsequent PCI who survived to hospital discharge had a long term prognosis similar to non-arrest STEMI patients with early PCI.14 Further research is needed regarding outcomes in this patient population however, because less than 5% of patients with STEMI who receive cardiac catheterization are post-arrest and these patients are often excluded from large clinical trials.
We suspect that cardiac catheterization may be underutilized because ECG and clinical data are not always reliable predictors for determining which patients will have clinically significant coronary disease.1 Cardiac enzymes may also not be helpful for risk stratifying post-arrest patients as enzyme release may have occurred secondary to defibrillation or global ischemia reperfusion injury. 15–18 Spaulding et al. performed angiography on a consecutive series of patients with return of spontaneous circulation after OHCA.1 Patients were excluded if they were <30 or >75 years of age or had an obvious non-cardiac cause of arrest. In this subset, they reported that almost half, 48% (40/84) had acute occlusion and 70% (28/40) of this group successfully received PCI. ECG and clinical findings were also poor predictors of disease as 26% (9/35) presented without chest pain or ST-segment elevation on ECG and had evidence of a recent coronary artery occlusion on angiography.
We suspect that some of the patients with an unknown etiology of arrest who did not receive emergent cardiac catheterization (59%) may also have benefited from angiography. In an effort to determine if patients without STEMI were just receiving the procedure on day 2 or 3 post-arrest, we also evaluated billing data 72 hours post-arrest. An additional 2 patients received catheterization on day 2 (one with PCI) and 3 patients on day 3. These findings further support the notion that early post-arrest cardiac catheterization is probably underutilized. Further research is needed to determine if there are post-arrest markers other than STEMI or new LBBB that can be useful in determining which patients are likely to benefit from immediate versus delayed angiographic evaluation.
At present, with the exception of therapeutic hypothermia, few uniform guidelines exist for post-resuscitation care. The American College of Cardiology guidelines for management of non-STEMI also do not specifically address indications for immediate cardiac catheterization in post cardiac arrest patients without ECG findings to suggest acute myocardial infarction.19 Several studies have demonstrated that it is feasible to treat post-arrest survivors with both therapeutic hypothermia and PCI and yield favorable outcomes.20, 21 A report by Sunde et al. also suggests that more patients may benefit from post-arrest angiographic evaluation than currently receive the therapy.20 They reported that prior to implementing a post-resuscitation protocol only 3% of OHCA survivors received reperfusion therapy (PCI or thrombolytics). After the protocol was adopted, 53% received emergent reperfusion and overall survival improved. Therapeutic hypothermia was probably an important factor in the improvement in survival. Only a few patients in our study (n=5) received post-arrest hypothermia but this does not reflect overall cooling at our institution as patients were cooled during our study time period after OHCA and other rhythms such as asystole and pulseless electrical activity. A cooling protocol also was not implemented at our institution until 2004. Additional studies will need to be conducted to determine if there are early indicators which predict which patients are most likely to benefit from early intervention. Determining optimal implementation and monitoring strategies will be essential for assessing the potential benefit of this therapy in survivors of both in and out-of-hospital cardiac arrest.
There are several limitations in our study common to billing data and chart review. Prospectively discussing each case with the treating physician and detailed chart review may have provided further information about practice variability and helped determine why some patients received cardiac catheterization and others did not. This may have also yielded additional information about neurologic functioning (pre and post catheterization) and arrest etiology which we were unable to determine in many of the cases in our study. Previous literature suggests multi-system organ failure is a common etiology of IHCA and patients in our study who did not receive cardiac catheterization may have had worse outcomes because of significant organ failure.22
Generalizability of our findings is also restricted because the overall number of patients that received cardiac catheterization in our study sample was small. In addition, the association between improved survival and prompt catheterization may reflect selection bias by the treating physician, which limits our ability to draw inference or causality. In addition, we do not know if patients who received PCI needed the procedure emergently or if similar outcomes would have resulted with a diagnostic cardiac catheterization at another time point. Future studies are needed to determine which post-arrest patients without STEMI or new LBBB are likely to have acute occlusion which requires immediate intervention.
Conclusion
We demonstrated that in-hospital VF arrest patients infrequently receive early cardiac catheterization. Furthermore, several patients without STEMI or new LBBB received cardiac catheterization and were found to have significant coronary artery disease warranting PCI. Additional research is needed to identify patients most likely to benefit from emergent catheterization after in-hospital arrest.
Acknowledgments
We wish to thank Lynne Harnish, Ameena Al-Amin, and Noah Sugerman for administrative assistance. Joel Roth was also extremely helpful in providing information on billing data review and interpretation.
Funding source: Philips Medical Research Grant.
This funding organization played no role in the study design, collection, analysis/interpretation of data, writing of the manuscript, or decision to submit the manuscript for publication.
Footnotes
Conflicts of interest:
Raina M. Merchant, MD: no conflict of interest
Benjamin S. Abella, MD, MPhil: Grants (Philips Medical Systems, Cardiac Science Corp), Honoraria/Speaking Fees (Medic First Aid, Alsius Corp, Laerdal)
Monica Khan: no conflict of interest
Kuang-Ning Huang, BA: no conflict of interest
David B. Beiser, MD: no conflict of interest
Robert W. Neumar, MD PhD: no conflict of interest
Brendan G. Carr, MD MA: no conflict of interest
Lance B. Becker, MD: Grants (Phillips Medical Systems, Laerdal Medical, Alsius Corporation, NIH, Cardiac Science), Scientific consultant (honoraria/speaking fees): (Abbott Labs, Philips Medical Systems), Patents (Hypothermia Induction Patents), Ownership, equity, royalties in privately held companies (Inventor’s equity and royalties from Cold Core Therapeutics’, INC, a company developing cooling technologies for medical cooling using “slurry” technology)
Terry L. Vanden Hoek, MD: Grants (Department of Defense, Office of Naval Research, Philips Medical Systems), Research Support (Medivance), Patents (Hypothermia Induction Devices and Methods)
References
- 1.Spaulding CM, Joly LM, Rosenberg A, et al. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med. 1997;336:1629–33. doi: 10.1056/NEJM199706053362302. [DOI] [PubMed] [Google Scholar]
- 2.Davies MJ, Thomas A. Thrombosis and acute coronary-artery lesions in sudden cardiac ischemic death. N Engl J Med. 1984;310:1137–40. doi: 10.1056/NEJM198405033101801. [DOI] [PubMed] [Google Scholar]
- 3.Myerburg RJ, Kessler KM, Estes D, et al. Long-term survival after prehospital cardiac arrest: analysis of outcome during an 8 year study. Circulation. 1984;70:538–46. doi: 10.1161/01.cir.70.4.538. [DOI] [PubMed] [Google Scholar]
- 4.Kahn JK, Glazier S, Swor R, Savas V, O’Neill WW. Primary coronary angioplasty for acute myocardial infarction complicated by out-of-hospital cardiac arrest. Am J Cardiol. 1995;75:1069–70. doi: 10.1016/s0002-9149(99)80727-9. [DOI] [PubMed] [Google Scholar]
- 5.Garot P, Lefevre T, Eltchaninoff H, et al. Six-month outcome of emergency percutaneous coronary intervention in resuscitated patients after cardiac arrest complicating ST-elevation myocardial infarction. Circulation. 2007;115:1354–62. doi: 10.1161/CIRCULATIONAHA.106.657619. [DOI] [PubMed] [Google Scholar]
- 6.Bendz B, Eritsland J, Nakstad AR, et al. Long-term prognosis after out-of-hospital cardiac arrest and primary percutaneous coronary intervention. Resuscitation. 2004;63:49–53. doi: 10.1016/j.resuscitation.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 7.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–7. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 8.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 9.Tunstall-Pedoe H, Bailey L, Chamberlain DA, Marsden AK, Ward ME, Zideman DA. Survey of 3765 cardiopulmonary resuscitations in British hospitals (the BRESUS Study): methods and overall results. Bmj. 1992;304:1347–51. doi: 10.1136/bmj.304.6838.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–56. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 11.Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–63. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 12.Bulut S, Aengevaeren WR, Luijten HJ, Verheugt FW. Successful out-of-hospital cardiopulmonary resuscitation: what is the optimal in-hospital treatment strategy? Resuscitation. 2000;47:155–61. doi: 10.1016/s0300-9572(00)00217-3. [DOI] [PubMed] [Google Scholar]
- 13.McCullough PA, Prakash R, Tobin KJ, O’Neill WW, Thompson RJ. Application of a cardiac arrest score in patients with sudden death and ST segment elevation for triage to angiography and intervention. J Interv Cardiol. 2002;15:257–61. doi: 10.1111/j.1540-8183.2002.tb01100.x. [DOI] [PubMed] [Google Scholar]
- 14.Gorjup V, Radsel P, Kocjancic ST, Erzen D, Noc M. Acute ST-elevation myocardial infarction after successful cardiopulmonary resuscitation. Resuscitation. 2007;72:379–85. doi: 10.1016/j.resuscitation.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 15.Lin CC, Chiu TF, Fang JY, Kuan JT, Chen JC. The influence of cardiopulmonary resuscitation without defibrillation on serum levels of cardiac enzymes: a time course study of out-of-hospital cardiac arrest survivors. Resuscitation. 2006;68:343–9. doi: 10.1016/j.resuscitation.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 16.Mullner M, Hirschl MM, Herkner H, et al. Creatine kinase-mb fraction and cardiac troponin T to diagnose acute myocardial infarction after cardiopulmonary resuscitation. J Am Coll Cardiol. 1996;28:1220–5. doi: 10.1016/S0735-1097(96)00316-6. [DOI] [PubMed] [Google Scholar]
- 17.Mullner M, Oschatz E, Sterz F, et al. The influence of chest compressions and external defibrillation on the release of creatine kinase-MB and cardiac troponin T in patients resuscitated from out-of-hospital cardiac arrest. Resuscitation. 1998;38:99–105. doi: 10.1016/s0300-9572(98)00087-2. [DOI] [PubMed] [Google Scholar]
- 18.Grubb NR, Fox KA, Cawood P. Resuscitation from out-of-hospital cardiac arrest: implications for cardiac enzyme estimation. Resuscitation. 1996;33:35–41. doi: 10.1016/s0300-9572(96)00971-9. [DOI] [PubMed] [Google Scholar]
- 19.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007;116:e148–304. doi: 10.1161/CIRCULATIONAHA.107.181940. [DOI] [PubMed] [Google Scholar]
- 20.Sunde K, Pytte M, Jacobsen D, et al. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007;73:29–39. doi: 10.1016/j.resuscitation.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 21.Hovdenes J, Laake JH, Aaberge L, Haugaa H, Bugge JF. Therapeutic hypothermia after out-of-hospital cardiac arrest: experiences with patients treated with percutaneous coronary intervention and cardiogenic shock. Acta Anaesthesiol Scand. 2007;51:137–42. doi: 10.1111/j.1399-6576.2006.01209.x. [DOI] [PubMed] [Google Scholar]
- 22.Laver S, Farrow C, Turner D, Nolan J. Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Med. 2004;30:2126–8. doi: 10.1007/s00134-004-2425-z. [DOI] [PubMed] [Google Scholar]