Abstract
AIM: To evaluate the utility of assessing iodized oil uptake with cone-beam computed tomography (CT) in transarterial chemoembolization (TACE) for small hepatocellular carcinoma (HCC).
METHODS: Cone-beam CT provided by a biplane flat-panel detector angiography suite was performed on eighteen patients (sixteen men and two women; 41-76 years; mean age, 58.9 years) directly after TACE for small HCC (26 nodules under 30 mm; mean diameter, 11.9 mm; range, 5-28 mm). The pre-procedural locations of the tumors were evaluated using triphasic multi-detector row helical computed tomography (MDCT). The tumor locations on MDCT and the iodized oil uptake by the tumors were analyzed on cone-beam CT and on spot image directly after the procedures.
RESULTS: All lesions on preprocedural MDCT were detected using iodized oil uptake in the lesions on cone-beam CT (sensitivity 100%, 26/26). Spot image depicted iodized oil uptake in 22 of the lesions (sensitivity 85%). The degree of iodized oil uptake was overestimated (9%, 2/22) or underestimated (14%, 3/22) on spot image in five nodules compared with that of cone-beam CT.
CONCLUSION: Cone-beam CT is a useful and convenient tool for assessing the iodized oil uptake of small hepatic tumors (< 3 cm) directly after TACE.
Keywords: Chemoembolization, Computed tomography, Hepatocellular carcinoma, Liver
INTRODUCTION
Transarterial chemoembolization (TACE) is a regional therapeutic modality that has become an accepted treatment for unresectable hepatocellular carcinoma (HCC). Triphasic multi-detector computed tomography (MDCT) is commonly used for the detection and preprocedural localization of hypervascular HCCs greater than 1 cm in diameter[1-3].
Diagnostic angiography using digital subtraction angiography (DSA) is performed before TACE in order to detect hypervascular HCCs. Occasionally, the small neoplastic foci are uncertain, and difficult to detect. Some studies have reported that the detection rate of small HCCs, less than 3 cm, in DSA was about 70%[4,5], and other studies showed higher sensitivity in nodule detection in helical biphasic CT than in DSA[6]. This discrepancy can make it difficult to determine whether or not the same nodules exist on MDCT in cases of small tumor nodules.
Iodized oil retention pattern after TACE is a posttreatment prognostic marker and significant factors affect local recurrence[7-9], however, a method for evaluating this immediately after TACE, is to take a spot image Follow-up unenhanced CT is usually performed within 1 mo after TACE, but it is sometimes difficult to determine whether there is washout of iodized oil uptake or initial failure of iodized oil uptake when there is partial iodized oil uptake in a lesion on the first follow-up CT. The exact method for comparing iodized oil retention in hypervascular nodules on preprocedural MDCT is to check the postprocedural CT directly after TACE and for this the patient must be transported from the angiography suite to the nearest CT scanner.
Cone-beam CT is a new technology provided by the combined angiography/CT suite that uses flat-panel detector (FD) technology. It provides images similar to those of CT and is able to obtain 3D reconstructions such as multiplanar reformat (MPR), maximum intensity projection (MIP), and 3D volume rendering (VR) with these data sets.
The purpose of this study was to evaluate the clinical value of cone-beam CT in the assessment of iodized oil uptake in TACE for small HCCs.
MATERIALS AND METHODS
Patients
From March 2006 to June 2006, eighteen patients (sixteen males and two females; 41-76 years; mean age, 58 years) with small HCCs (26 nodules; mean diameter 11.9 mm; range, 5-28 mm), underwent cone-beam CT and TACE consecutively. All patients had underlying liver cirrhosis. The diagnosis of HCC was made clinically in these patients by using typical imaging findings on MDCT and an elevated level of serum alpha fetoprotein. The size and location of the tumors were evaluated with triphasic MDCT before TACE (Figures 1 and 2). Eleven patients had previously undergone TACE for multiple nodules. The first TACE was performed in seven patients who were not candidates for surgery. According to our institutional guidelines, institutional review board approval was not required for this report.
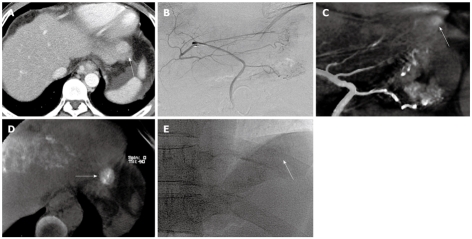
Figure 1.
A 47-year-old man with hepatocellular carcinoma in S2 for 2nd TACE. A: Preprocedural late arterial phase MDCT scan reveals hypervascular HCC near the diaphragm (arrow); B: Left gastric angiogram shows aberrant left hepatic artery with no tumor staining in suspected area; C: Tumor staining (arrow) and feeder artery are found after acquiring MIP image from cone-beam CT hepatic arteriography (Cone-beam CTHA); D: Cone-beam CT directly after TACE shows good grade iodized oil uptake in S2 (arrow); E: Spot image shows subtle lipiodol uptake near the left hemidiaphragm (arrow), but nodular iodized oil uptake is not observed.
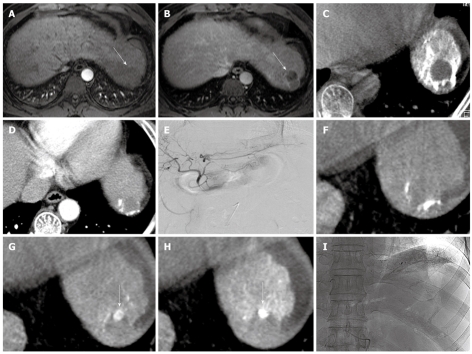
Figure 2.
A 52-year-old man with HCC in S2 for 2nd TACE. A, B: Early arterial phase (A) and delayed phase (B) of MRI reveals nodule (arrow) in segment 2 with no enhancement (arrow); C: Cone-beam CT after TACE shows poor grade of iodized oil uptake by the tumor; D: Early arterial phase of MDCT shows washout of iodized oil uptake near nodule, but no enhancing portion within the nodule 3 mo later; E: Left hepatic angiogram during TACE reveals no tumor and feeding artery 1 mo later; F, G: Cone-beam CT with (F) and without (G) hepatic arteriography shows small enhancing nodule (arrow) in the nodule; H, I: Cone-beam CT after infusion of emulsion (H) shows excellent grade iodized oil uptake by the nodule (arrow). This case shows typical “nodule-in-nodule” appearance of HCC, but spot image (I) did not distinguish nodular uptake.
TACE
Angiography was conducted using the AXIOM Artis FD Biplane Angio suite with cone-beam CT (DynaCT, Siemens Medical Solutions, Erlangen, Germany). For angiography, a 5-Fr catheter was inserted using the Seldinger technique from the right common femoral artery into the celiac trunk. After confirming the location of the tumor and its feeding artery, a 3-Fr 100-cm-long microcatheter (Progreat; Terumo, Tokyo, Japan) with a 0.016-inch, 150-cm long guidewire covered by hydrophilic polymer (Radiofocus; Terumo, Tokyo, Japan), was advanced through a 5-Fr catheter into the peripheral portion of the feeding artery as close to the lesion as possible (Figures 1 and 2). If tumor staining or feeders were uncertain, cone-beam CT hepatic arteriography (cone-beam CTHA) was performed (contrast media injection rate was 2 mL/s; X-ray delay used in 1.5 s). After these baseline studies, TACE using an emulsion of epirubicin hydrochloride (Pharmorubicin; Ildong, Seoul, Korea) dissolved in meglumine ioxitalamate (Telebrix; Guerbet, Aulnay-sous-Bois, France) mixed with iodized oil (Lipiodol Ultra Fluid; Guerbet, Aulnay-sous-Bois, France) was performed. The end point of TACE was when an “oily portogram” was achieved. Finally, spot image and cone-beam CT were performed to determine the deposition of iodized oil.
Cone-beam CT
Cone-beam CT acquisition was obtained using the following parameters: 10-s rotation; 0.4° increment; 1024 × 793 matrix in projections at zoom 0 after resampling; 217° total angle; and 11°/s, 27 frames/s, system dose 0.36 μGy/pulse, total 273 projections. The image reconstruction was performed on a commercially available dedicated workstation (X-Leonardo with DynaCT; Siemens Medical Solutions). The volume dataset was displayed on the monitor in the MPR.
Image analysis
The tumor locations, as shown on MDCT, iodized oil uptake by the tumor in the lesion on cone-beam CT and spot image, were determined directly after the procedures were analyzed. The enhancing tumor locations as shown on MDCT and iodized oil uptake by the tumors were compared. The degree of iodized oil uptake by the tumor (excellent, 100% deposition of iodized oil in the lesion; good, 51%-99%; poor, ≤ 50%) on cone-beam CT and spot image were also compared. The spot images were evaluated at the workstation, while cone-beam CT images were evaluated by images created by MPR, and MIP (maximum intensity projection). All images were graded by two radiologists, and decisions were reached by consensus.
RESULTS
Cone-beam CT was successfully completed in all study patients. It only took about 5 min to obtain MPR images. Cone-beam CT visualized the iodized oil uptake in all the nodules (26/26, sensitivity 100%), but spot image only visualized iodized oil uptake in 22 of the lesions (sensitivity 85%) (Figures 1 and 2).
Degree of iodized oil uptake in tumors
The degree of iodized oil uptake was somewhat different in the two modalities (Table 1). Cone-beam CT depicted iodized oil uptake in the nodules more clearly than spot image. Two nodules were not seen in spot image but were clearly evaluated with cone-beam CT. There was discordance between the two modalities in 5 nodules and iodized oil uptake was over-(9%, 2/22) or underestimated (14%, 3/22) in spot image compared with cone-beam CT.
Table 1.
Degree of iodized oil uptake by the tumors
| Degree | Spot image | Cone-beam CT |
| Excellent | 11 | 16 |
| Good | 8 | 7 |
| Poor | 3 | 3 |
| Total | 22 | 26 |
Discordance between the two modalities-5 nodules [over-: 9% (2/22), underestimated: 14% (3/22) in spot image]. CT: Computed tomography.
The iodized oil uptake in 4 nodules was not seen in spot image, two nodules were less than 1 cm, one was between 1 cm and 2 cm, and one was over 2 cm. The discordance between the two modalities occurred in nodules less than 2 cm (Table 2).
Table 2.
Degree of iodized oil uptake by the tumors according to size
| Size |
Degree of iodized oil uptake in spot image |
Degree of iodized oil uptake in cone-beam CT |
||||
| Excellent | Good | Poor | Excellent | Good | Poor | |
| ≤ 1 | 5 | 3 | 1 | 7 | 4 | |
| ≤ 2 | 6 | 4 | 2 | 8 | 2 | 3 |
| ≤ 3 | 1 | 1 | 1 | |||
| Total | 11 | 8 | 3 | 16 | 7 | 3 |
Discordance in degree of iodized oil uptake occurred in nodules less than 2 cm (3 nodules less than 1 cm).
Nodules with atypical enhancement patterns in MDCT
Three nodules showed atypical enhancement patterns in MDCT, and additional dynamic magnetic resonance imaging (MRI) was performed for one nodule (Figure 2). Their feeders were uncertain on selective right or left hepatic arteriography, but were detected with cone-beam CTHA. Enhancement patterns and iodized oil uptake in the nodules are shown in Table 3.
Table 3.
Enhancement patterns and iodized oil uptake in three nodules without typical enhancement patterns of HCCs on MDCT and MRI
| Nodule | Modality |
Phase |
Degree of iodized oil uptake |
||
| EA | Delayed | Spot image | Cone-beam CT | ||
| 1 | CT | Subtle E | Washout | Poor | Poor |
| 21 | CT | No E | No E | Poor | Excellent |
| 3 | MRI | Subtle E | Washout | Invisible | Good |
Same patient in Figure 2. EA: Early arterial phase; Delayed: Delayed phase; Subtle E: Subtle enhancement; No E: No enhancement. HCC: Hepatocellular carcinoma; MDCT: Multi-detector row helical computed tomography; MRI: Magnetic resonance imaging.
DISCUSSION
Several treatment options for small HCCs have been introduced for patients who are not surgical candidates. These options include TACE, percutaneous ethanol injection (PEI), radiofrequency ablation (RFA), microwave coagulation therapy (MCT), laser thermal ablation (LTA), and combination therapy[10,11]. Among them, TACE is widely performed, because it is minimally invasive, repeatable, and more effective in combination with other treatments[10-15].
TACE was found to be as effective as hepatic resection for early stage tumors when iodized oil was compactly retained within the tumor[8]. Iodized oil uptake pattern can be a prognostic index[7]. Various studies have suggested that iodized oil uptake in a tumor can correlate well with hepatic necrosis, and compact iodized oil uptake on unenhanced CT may represent necrosis[16,17]. Takayasu et al[16] reported that the highest degree of necrosis usually occurs immediately after TACE and the regrowth of viable cancer cells will occur later if complete necrosis of the tumor was not achieved. At this point, compact iodized oil uptake by the tumor directly after the procedure prevents regrowth of tumors, but to confirm this, only spot image is usually acquired. If the tumor is large enough to appear on spot images, it is easy to determine the degree of iodized oil uptake, but if the tumor is small, especially less than 2 cm, the degree of iodized oil uptake is incorrectly determined, which can cause tumor regrowth. It is also impossible to refuse chemotherapeutic agents directly if there is partial iodized oil uptake in a lesion on the first follow-up CT.
Cone-beam CT was first used in neuroendovascular procedures, and the image quality is sufficient to make a diagnosis when a complication is suspected[18]. In the era of assessing the degree of iodized oil uptake, cone-beam CT is also a convenient tool during and after TACE and clearly correlates with MDCT. If cone-beam CT images shows non-compact iodized oil uptake, immediate reintervention can be achieved. The disadvantages of this CT-like image are low temporal resolution and a small field of view, however, it is sufficient to locate lesions previously diagnosed on MDCT[19].
Takayasu et al[9] reported “targeted transarterial oily chemoembolization” which is a similar method to ours, but these authors used a unified helical CT and angiography system. Our system is only a DSA machine without a helical CT system and has more simple structures.
The radiation dose from cone-beam CT was not measured, however, Hirota et al[20] measured the radiation dose of cone-beam CT with a flat-panel-detector digital angiography system (similar system with ours) and single helical CT using a cylindrical phantom model of CT dose index with a dosimeter. They reported that the radiation dose by cone-beam CT was less than that of single helical CT. In addition, the radiation dose from cone-beam CT can be calculated via a pre-set radiation dose (0.36 μGy/pulse) and total fluoro time (7.5 pulse/s, 10 s). Compared with nonenhanced MDCT for TACE follow-up, the calculated radiation dose of cone-beam CT is low.
Cone-beam CTHA placing the microcatheter in the nearest arteries was performed in only three nodules in this study. Another study[20] also reported this method, and this technique is very useful to confirm a perfusion area in the artery. Although a small number of cases were included in this study, this method is a very useful and time-saving technique in TACE and other interventional procedures, especially for small lesions.
In conclusion, cone-beam CT is a useful and convenient tool for assessing the iodized oil uptake by small hepatic tumors (< 3 cm) directly after TACE. In addition, in cases with suspected small HCC nodules without typical enhancement patterns on CT, cone-beam CTHA will be very useful, however, further study is required.
COMMENTS
Background
Iodized oil retention pattern after transarterial chemoembolization (TACE) is a posttreatment prognostic marker, and significant factors affect local recurrence, however, a method for evaluating this immediately after TACE is to take a spot image Follow-up unenhanced computed tomography (CT) is usually performed within 1 mo after TACE, but it is sometimes difficult to determine whether there is washout of iodized oil uptake or initial failure of iodized oil uptake when there is partial iodized oil uptake in a lesion on the first follow-up CT.
Research frontiers
Comparing iodized oil retention in small hypervascular nodules on preprocedural multi-detector row helical computed tomography (MDCT) directly after TACE is possible without transporting patients from the angiography suite to the nearest CT scanner.
Innovations and breakthroughs
In the present study, the authors investigated the efficacy of cone-beam CT with regard to iodized oil uptake after TACE for small hepatocellular carcinoma (HCC)s.
Applications
The study showed that cone-beam CT is a useful and convenient tool for assessing the iodized oil uptake by small hepatic tumors directly after TACE.
Terminology
Cone-beam CT is a new technology provided by the combined angiography/CT suite that uses flat-panel detector technology. It provides images similar to those of CT and is able to make 3D reconstructions such as multiplanar reformat, maximum intensity projection, and 3D volume rendering with these data sets.
Peer review
This is an interesting study which shows the advantages of assessing iodized oil uptake after TACE for small HCC with cone-beam CT. It may provide useful information for us.
Footnotes
Supported by A Grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea, A091047
Peer reviewer: Satoshi Mamori, MD, PhD, Department of Gastroenterology and Hepatology, Shinko Hospital, 1-4-47 Wakihama-cho, Chuo-ku, Kobe, Hyogo 651-0072, Japan
S- Editor Wang YR L- Editor Webster JR E- Editor Ma WH
References
- 1.Murakami T, Kim T, Takamura M, Hori M, Takahashi S, Federle MP, Tsuda K, Osuga K, Kawata S, Nakamura H, et al. Hypervascular hepatocellular carcinoma: detection with double arterial phase multi-detector row helical CT. Radiology. 2001;218:763–767. doi: 10.1148/radiology.218.3.r01mr39763. [DOI] [PubMed] [Google Scholar]
- 2.Zhao H, Zhou KR, Yan FH. Role of multiphase scans by multirow-detector helical CT in detecting small hepatocellular carcinoma. World J Gastroenterol. 2003;9:2198–2201. doi: 10.3748/wjg.v9.i10.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim SK, Lim JH, Lee WJ, Kim SH, Choi D, Lee SJ, Lim HK, Kim H. Detection of hepatocellular carcinoma: comparison of dynamic three-phase computed tomography images and four-phase computed tomography images using multidetector row helical computed tomography. J Comput Assist Tomogr. 2002;26:691–698. doi: 10.1097/00004728-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Bartolozzi C, Lencioni R, Caramella D, Palla A, Bassi AM, Di Candio G. Small hepatocellular carcinoma. Detection with US, CT, MR imaging, DSA, and Lipiodol-CT. Acta Radiol. 1996;37:69–74. doi: 10.1177/02841851960371P114. [DOI] [PubMed] [Google Scholar]
- 5.De Santis M, Romagnoli R, Cristani A, Cioni G, Casolo A, Vici FF, Ventura E. MRI of small hepatocellular carcinoma: comparison with US, CT, DSA, and Lipiodol-CT. J Comput Assist Tomogr. 1992;16:189–197. doi: 10.1097/00004728-199203000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Nakayama A, Imamura H, Matsuyama Y, Kitamura H, Miwa S, Kobayashi A, Miyagawa S, Kawasaki S. Value of lipiodol computed tomography and digital subtraction angiography in the era of helical biphasic computed tomography as preoperative assessment of hepatocellular carcinoma. Ann Surg. 2001;234:56–62. doi: 10.1097/00000658-200107000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mondazzi L, Bottelli R, Brambilla G, Rampoldi A, Rezakovic I, Zavaglia C, Alberti A, Ideo G. Transarterial oily chemoembolization for the treatment of hepatocellular carcinoma: a multivariate analysis of prognostic factors. Hepatology. 1994;19:1115–1123. [PubMed] [Google Scholar]
- 8.Lee HS, Kim KM, Yoon JH, Lee TR, Suh KS, Lee KU, Chung JW, Park JH, Kim CY. Therapeutic efficacy of transcatheter arterial chemoembolization as compared with hepatic resection in hepatocellular carcinoma patients with compensated liver function in a hepatitis B virus-endemic area: a prospective cohort study. J Clin Oncol. 2002;20:4459–4465. doi: 10.1200/JCO.2002.02.013. [DOI] [PubMed] [Google Scholar]
- 9.Takayasu K, Muramatsu Y, Maeda T, Iwata R, Furukawa H, Muramatsu Y, Moriyama N, Okusaka T, Okada S, Ueno H. Targeted transarterial oily chemoembolization for small foci of hepatocellular carcinoma using a unified helical CT and angiography system: analysis of factors affecting local recurrence and survival rates. AJR Am J Roentgenol. 2001;176:681–688. doi: 10.2214/ajr.176.3.1760681. [DOI] [PubMed] [Google Scholar]
- 10.Zheng XH, Guan YS, Zhou XP, Huang J, Sun L, Li X, Liu Y. Detection of hypervascular hepatocellular carcinoma: Comparison of multi-detector CT with digital subtraction angiography and Lipiodol CT. World J Gastroenterol. 2005;11:200–203. doi: 10.3748/wjg.v11.i2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrari FS, Stella A, Pasquinucci P, Vigni F, Civeli L, Pieraccini M, Magnolfi F. Treatment of small hepatocellular carcinoma: a comparison of techniques and long-term results. Eur J Gastroenterol Hepatol. 2006;18:659–672. doi: 10.1097/00042737-200606000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Bartolozzi C, Lencioni R, Caramella D, Vignali C, Cioni R, Mazzeo S, Carrai M, Maltinti G, Capria A, Conte PF. Treatment of large HCC: transcatheter arterial chemoembolization combined with percutaneous ethanol injection versus repeated transcatheter arterial chemoembolization. Radiology. 1995;197:812–818. doi: 10.1148/radiology.197.3.7480761. [DOI] [PubMed] [Google Scholar]
- 13.Matsui O, Kadoya M, Yoshikawa J, Gabata T, Arai K, Demachi H, Miyayama S, Takashima T, Unoura M, Kogayashi K. Small hepatocellular carcinoma: treatment with subsegmental transcatheter arterial embolization. Radiology. 1993;188:79–83. doi: 10.1148/radiology.188.1.8390073. [DOI] [PubMed] [Google Scholar]
- 14.Pacella CM, Bizzarri G, Cecconi P, Caspani B, Magnolfi F, Bianchini A, Anelli V, Pacella S, Rossi Z. Hepatocellular carcinoma: long-term results of combined treatment with laser thermal ablation and transcatheter arterial chemoembolization. Radiology. 2001;219:669–678. doi: 10.1148/radiology.219.3.r01ma02669. [DOI] [PubMed] [Google Scholar]
- 15.Qian J, Feng GS, Vogl T. Combined interventional therapies of hepatocellular carcinoma. World J Gastroenterol. 2003;9:1885–1891. doi: 10.3748/wjg.v9.i9.1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takayasu K, Arii S, Matsuo N, Yoshikawa M, Ryu M, Takasaki K, Sato M, Yamanaka N, Shimamura Y, Ohto M. Comparison of CT findings with resected specimens after chemoembolization with iodized oil for hepatocellular carcinoma. AJR Am J Roentgenol. 2000;175:699–704. doi: 10.2214/ajr.175.3.1750699. [DOI] [PubMed] [Google Scholar]
- 17.Choi BI, Kim HC, Han JK, Park JH, Kim YI, Kim ST, Lee HS, Kim CY, Han MC. Therapeutic effect of transcatheter oily chemoembolization therapy for encapsulated nodular hepatocellular carcinoma: CT and pathologic findings. Radiology. 1992;182:709–713. doi: 10.1148/radiology.182.3.1311116. [DOI] [PubMed] [Google Scholar]
- 18.Heran NS, Song JK, Namba K, Smith W, Niimi Y, Berenstein A. The utility of DynaCT in neuroendovascular procedures. AJNR Am J Neuroradiol. 2006;27:330–332. [PMC free article] [PubMed] [Google Scholar]
- 19.Akpek S, Brunner T, Benndorf G, Strother C. Three-dimensional imaging and cone beam volume CT in C-arm angiography with flat panel detector. Diagn Interv Radiol. 2005;11:10–13. [PubMed] [Google Scholar]
- 20.Hirota S, Nakao N, Yamamoto S, Kobayashi K, Maeda H, Ishikura R, Miura K, Sakamoto K, Ueda K, Baba R. Cone-beam CT with flat-panel-detector digital angiography system: early experience in abdominal interventional procedures. Cardiovasc Intervent Radiol. 2006;29:1034–1038. doi: 10.1007/s00270-005-0287-6. [DOI] [PubMed] [Google Scholar]