Abstract
Many parents, grandparents, and clinicians have associated a baby’s ability to eat and gain weight as a sign of good health, and clinicians typically only call significant attention to infant growth if a baby is failing to thrive or showing severe excesses in growth. Recent evidence, however, has suggested that pediatric healthcare providers should pay closer attention to growth patterns during infancy. Both higher weight and upward crossing of major percentile lines on the weight-for-age growth chart during infancy have long term health consequences, and are associated with overweight and obesity later in life. Clinicians should utilize the numerous available opportunities to discuss healthy growth and growth charts during health maintenance visits in the first two years after birth. Further, providers should instruct parents on strategies to promote healthy behaviors that can have long lasting obesity preventive effects.
Keywords: Obesity, Prevention, Infant, Breastfeeding, Sleep
Weight Gain during Infancy and Long-Term Effects
Are chubby babies healthy babies? While most appear well during infancy, evidence is increasing that heavier babies have a poorer long-term health trajectory than their trimmer counterparts. Data have emerged over the past two decades that early life growth patterns and behaviors play an important role in the etiology of obesity, yet there has been very little focus on the primary prevention of obesity during infancy by the medical, behavioral health, and public health communities. A recent report from the National Health and Nutrition Examination Survey (NHANES) highlighted the need for very early intervention when it revealed that between 2003-2006, a staggering 24.4% of children aged 2 to 5 years already were overweight or obese (Body Mass Index [BMI] 85th-94th and ≥95th percentiles, respectively).1 NHANES data also have described obesity (weight-for-length/height ≥ 95th percentile) among infants less than 2 years of age (Figure 1). Between the late 1970s and 2000, the prevalence of obesity among infants 6-23 months of age increased by over 60%.2 Similarly, reports from the Centers for Disease Control and Prevention (CDC) Pediatric Nutrition Surveillance System3 and a Massachusetts Health Maintenance Organization4 both showed significant increases in the prevalence of overweight for infants and toddlers for all age groups since the 1980s.
Figure 1.
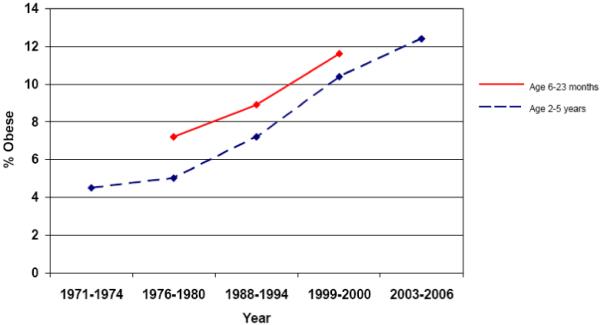
Trends in infant (weight-for-length ≥95th percentile) and toddler (BMI ≥95th percentile) obesity.1, 2, 5
The Institute of Medicine publication, “Preventing Childhood Obesity: Health in the Balance,” stated that the prevention of obesity in children should be a national public health priority.5 More specific to younger children was the summary of the “Conference on Preventing Childhood Obesity,” where it was remarked, “The prenatal period, infancy, and early childhood may be stages of particular vulnerability to obesity development because they are unique periods for cellular differentiation and development. This unique vulnerability might make it possible for actions taken at these stages to determine the future course of adiposity.” 6 This statement has been magnified by the numerous studies demonstrating the association between rapid or accelerated infant weight gain and subsequent obesity,7-24 as well as hypertension,25-28 coronary heart disease,29, 30 and type 2 diabetes mellitus.31, 32 Further, numerous studies have now shown that overweight infants and toddlers are at increased risk of staying overweight as they age.9, 16, 33-46 It has been theorized that over-nutrition in infancy adversely “programs” the components of the metabolic syndrome and the way energy is stored.47, 48 These relationships may be especially true for those born to overweight parents as genetic and familial influences, combined with pregnancy weight gain are strongly associated with obesity in offspring.19, 34, 35, 49, 50
While all of the concerns about infant growth and subsequent morbidity make a strong case for very early intervention, there is little evidence regarding what, if anything, works to prevent the development of obesity during the first years of life although the extant literature provides some suggestions regarding potentially promising approaches.5, 51 Early intervention and prevention hold great promise for interrupting the vicious cycle of obese children becoming obese adults who subsequently have obese offspring themselves. The following sections summarize numerous aspects of infant life that affect weight status, the way information on this subject should be communicated with parents, and interventions that can be suggested to families to prevent the development of obesity based on the currently available evidence.
Obesity Prevention during the Newborn Period and Early Infancy
Role of Clinicians in Addressing Infant Weight Gain
Many parents, grandparents, and clinicians propagate the belief that “a chubby baby is a healthy baby” despite evidence even in the short term to the contrary, 52-55 and substantial long term evidence as described above. During infancy, growth charts are typically used by healthcare providers to ensure adequate and proportional growth with respect to weight, length, and head circumference, but information is usually communicated to parents without significant explanation so long as the child does not either a) raise concern for failure to thrive or b) demonstrate disproportionate or very excessive growth on one of the three measurements.
Additionally, there is often a disconnect between healthcare provider definitions of overweight and obesity and parents interpretation of these terms.53, 56-65 Many parents believe heavier infant weight and appearance indicates good infant health and higher levels of parenting competence, particularly parents from poor or minority backgrounds.57, 65-70 In contrast, parents often perceive their children as picky eaters even when their weight gain is progressing normally,71 and infants and children perceived as too small often are given developmentally inappropriate nutrition, including the early introduction of solids and/or table foods.68, 70 The association of food with love in some cultures may also contribute to higher infant weight.72
Potential Intervention
Given the childhood obesity epidemic and the evidence that early upward crossing of major percentile lines on the growth curve is associated with later obesity,7-11, 13-15, 73 clinicians must pay closer attention to patterns of growth during early childhood and the way parents interpret infant growth. Providers must better understand healthy infant growth patterns and communicate this information regularly and accurately to parents. Additionally, they must be familiar with early interventions that can prevent unhealthy patterns of weight gain in infancy and corrective interventions when problems are identified (Table 1).
Table 1.
Potential interventions to prevent and/or address obesity during infancy
| Opportunity | Intervention |
|---|---|
| Early Infancy | |
|
|
|
|
|
|
|
|
|
|
| Later Infancy | |
|
|
|
|
|
|
|
|
|
|
Early Feeding Mode
Epidemiologic and experimental evidence has consistently indicated that breastfeeding offers modest protection against obesity later in life as compared to formula feeding,74-80 and both exclusivity and duration of breastfeeding strengthen this association.77, 78, 80-84 There are several reasons or mechanisms by which this protection may occur. First, breastfeeding promotes self-regulation of intake by the infant, and breastfed infants regulate the volume of feeds in response to the energy density of breast milk.85 In contrast, formula feeding is a more parent-driven feeding activity, with the regulation of intake directed by the parents rather than the infant. As compared to nursing infants, bottle fed infants are fed on a more regular schedule and the volume of feeds is very consistent suggesting that parents are driving intake patterns.86 Subsequent research has shown that common bottle feeding practices, such as “emptying the bottle” and serving larger volumes of formula at feedings, are associated with excess weight gain in the first six months of life.87
The composition of breast milk may also contribute to the protective effects of breastfeeding. Human breast milk contains hundreds of components serving both nutritive and non-nutritive functions within the infant,88 both of which may affect short- and long-term growth patterns of children.89 Interspecies comparisons suggest that the high lactose and cholesterol content of human milk supports growth of the central nervous system, whereas the high protein and mineral content of other species’ milk (e.g. cow’s milk) supports substantial and rapid gains in physical size.89, 90 Recent experimental research in humans suggest that the high levels of protein and minerals in formula may stimulate excess physical growth later in infancy, with persistent effects even at 2 years of age.91
Other “bioactive” components of breast milk may have potential roles in the regulation of growth and development of the infant.92 Human milk contains growth-regulating components such as leptin, ghrelin, insulin-like growth factor-1, and adiponectin,93-95 and blood leptin levels in breastfed infants are comparatively higher to formula fed infants.93 Subsequent research focused solely on breastfed infants has shown that maternal milk leptin levels are negatively associated with weight gain during early infancy and through 2 years of age.96, 97
The sum of this early feeding experience for breastfed and formula fed infants produces clear growth differences by feeding mode that persist for at least the first two years after birth.98 Limited research assessing body composition has shown that growth differences are likely due to increases in adiposity in formula fed infants between 6 months and 24 months of age.99 Historically these growth differences were viewed as a sign that breastfed infants were not thriving, and the widely used CDC 2000 growth reference has been criticized as inadequate for monitoring the growth of breastfed infants because it is based predominantly on data from formula fed infants in the U.S. The creation of the World Health Organization (WHO) International Growth Standards, based on an international sample of healthy breast fed infants, has helped to support the perception of breastfeed infants’ growth as the “reference” growth pattern and formula fed infants’ growth as deviant from this reference.100-102 Notably, when comparing how breastfed infants’ growth trajectories track along the CDC versus the WHO charts across the first two years after birth, substantial differences in expected growth are apparent.102 With this comparison, when using the WHO chart as the growth reference, a normal deceleration of growth for breastfed infants is easily apparent after 2 months of age and a slower rate of growth is evident through the first year after birth. In contrast, when using the CDC chart as the growth reference, the average breastfed infant would cross below the 50th percentile at age 7 months and proceed further below the 50th percentile through the first year. Without reference to a growth chart for breastfed infants, some infants might come to attention for failure to thrive when in fact their growth is normal. Further highlighting this is the fact that at age 12 months, the WHO median weight for age is 1.2 kg lower for females and 1.5 kg lower for males in comparison to CDC charts.
Potential Intervention
The CDC Guide to Breastfeeding Interventions outlines evidence-based practices for promoting breastfeeding and improving breastfeeding duration and exclusivity.103 Optimal breastfeeding practices can be promoted through a variety of avenues, including the health care system, places of work/employment, the community, and broader society. Among the interventions that can improve breastfeeding rates are several changes that can be made within the health care system. Prenatal, intrapartum, and postpartum education to improve breastfeeding knowledge and skills is an integral part of promotion of breastfeeding. In addition, access to professional support (e.g. lactation consultants, nurses, physicians) when families experience problems is a critical component of a supportive health care system. Institutional changes within the hospital and/or clinical setting have been shown to improve breastfeeding initiation and duration rates. The changes may be discrete, such as not handing out formula promotion gift packs to families, or they may be comprehensive, such as becoming a designated Baby Friendly Hospital Initiative hospital.103
For physicians who monitor the growth of infants, practice guidelines should emphasize the expected, natural, and health-promoting aspects of “slower” growth in breastfed infants during the second six months after birth and beyond. Physicians should reassure parents who may be concerned about their infant’s performance on CDC growth charts that the growth patterns of breastfed infants are healthy. Plotting children on the appropriate WHO growth standard may provide both physicians and parents with needed reassurance.
For families choosing to formula feed their infant, parents should be given specific education aimed at reducing problematic bottle feeding behaviors. For example, parents should be encouraged to feed their infants when they are hungry, rather than on a set schedule outside of the immediate newborn period. Parents should be instructed to be responsive to infant cues for satiety, rather than ensuring their infant finishes the bottle contents. Age-specific guidelines for how much formula should be dispensed at a feeding would help parents start the feed with an appropriate portion size for their infant. Finally, encouraging parents to discern whether an infant is hungry or needing alternative soothing may reduce overfeeding of the bottle-fed infant.
Sleep
Short sleep duration may have other health effects other than fatigue. There is some evidence that it may be a contributor to the development of obesity. During the past 40 years, sleep duration in the U.S. has decreased by 1 to 2 hours per day while the prevalence of obesity has markedly increased.104-106 It is estimated that children, a group with a rapid rise in the prevalence of obesity, are currently sleeping 1 to 2 hours less than they require, and that approximately 15 million American children are affected by inadequate sleep.107, 108
The link between short sleep duration and childhood obesity was first shown in a study of French 5-year olds where investigators found a significant risk for overweight among children who slept less than 11 hours per day.109 Since the publication of that study, several investigations have shown that short sleep duration during early childhood (ages 3-5 years) is associated with overweight, obesity, and higher body fat during school age.9, 11, 74, 110, 111 Most recently, Taveras et al. demonstrated that sleep duration of less than 12 hours during infancy is a risk factor for overweight and adiposity in preschool-aged children.112
There are several mechanisms by which shorter sleep duration may lead to overweight even among the youngest of children. The first two months after birth represent a critical period in the development of sleep patterns, a period where feeding and sleeping are inextricably linked with infants waking every 2-4 hours, typically to feed.113-116 These first months are also central for the development of normal circadian rhythms.117 As a result of these rhythms, infants have periods of arousal from sleep, and how parents handle the infant’s night waking represents a source of variability in infants’ developing nighttime sleep patterns.118, 119
To evaluate different parenting styles and the impact on sleep, St. James-Roberts evaluated a “proximal care” model of parenting infants characterized by prolonged holding, frequent breastfeeding, rapid response to infant frets and cries, and co-sleeping with infants at night with other approaches to infant care that have less parent-infant contact per day.118 He found that the proximal care group of infants had more frequent night waking and crying at 12 weeks of age. In another investigation, infants whose parents were present when their child fell asleep were more likely to wake at night than infants whose parents were not present, suggesting that infants who were able to self-soothe in the absence of feeding were more likely to sleep through the night.120
The early development of sleeping through the night and its association with subsequent weight status is based on several findings. First, children who are unable to achieve a sleep duration of 6 hours by age 5 months have a much greater risk of short sleep duration and sleep problems later in childhood.121, 122 Second, relative sleep duration for age compared with norms for age was shown to remain constant for approximately 90% of children in a recent longitudinal study of sleep in children.123
Next, to understand a potential physiologic mechanism for a relationship between sleep and obesity, one might consider adult data that have demonstrated that sleep restriction results in a significant reduction in the anorexigenic hormone, leptin, and an increase in the appetite stimulating peptide, ghrelin.124 Reduced leptin and increased ghrelin were associated with a significant increase in hunger and appetite. The relationship between short sleep duration, reduced leptin, and increased ghrelin was also found in another investigation with over 1000 participants where the links were shown to exist independent of BMI.125 Though limited data on this subject exist for infants and children, lower cord blood ghrelin levels have been linked to slower weight gain from 0 to 3 months of age.126 These findings suggest that efforts to increase sleep duration for children could result in lower ghrelin levels, which could limit rapid weight gain during infancy. The importance of research studying potential links between sleep and obesity in children is becoming apparent and was emphasized in a recent editorial in the Archives of Internal Medicine.127 There, Bass and Turek wrote, “It is now critical to determine the importance of a lack of sleep during the early formative years in putting our youth on a trajectory towards obesity and the metabolic syndrome - a trajectory that could be altered if sleep loss is indeed playing a role in this epidemic.” In summary, the roots of short sleep duration can be found in infancy, and are linked to parenting practices surrounding sleeping and feeding with potential long-term consequences for weight status.
Two seemingly conflicting theories regarding the prevention of obesity intersect in the discussion of sleep. While prolonged sleep duration may be protective for obesity, breastfeeding, which is also protective for obesity, is associated with shorter sleep segments, increased night waking, and reduced total daily sleep.122, 128-131 This shorter sleep duration can persist even after the child has been weaned.122, 128 Breastfed infants also may be more easily aroused from sleep than those that are bottle fed.132 Further, more frequent night waking has been described as a source of distress for mothers and a cause for them changing from breastfeeding to formula feeding.122, 133 Clearly the relationship between sleep duration, breastfeeding, and weight status is complex, but as described below, interventions to promote longer sleep duration could achieve objectives of breastfeeding promotion and obesity prevention.
Potential Intervention
Because short sleep duration in infancy and childhood is linked to childhood obesity, interventions designed increase sleep duration during infancy may have long-term protective effects against obesity. Importantly, some research suggests that sleep duration during infancy can be significantly lengthened with appropriate interventions, even for breastfed infants. An intervention developed by Pinilla and Birch was very successful in increasing nocturnal sleep duration in breastfed infants, who were taught to sleep for at least 5 consecutive hours by 8-weeks of age.134 In this study, parents in the treatment group were given a simple set of instructions to gradually lengthen intervals between middle-of-the-night feedings by carrying out alternative caregiving behaviors prior to feeding (e.g., re-swaddling, diapering, rocking). By age 3 weeks, treatment infants showed significantly longer sleep episodes at night, and by 8-weeks 100% of treatment infants were sleeping a 5-hour duration overnight, compared to 23% of control infants. Importantly, infants made up for the reduced nocturnal milk consumption with a larger early morning feed. One of the interventions described in the study, swaddling, has been shown to calm infants, reduce arousals during sleep, improve sleep efficiency, and reduce spontaneous awakenings.135, 136 Additionally, other pediatric practitioners have expanded upon these techniques in an attempt to calm and soothe infants and improve infant sleep through the addition of “white noise”, gentle rocking, and non-nutritive sucking.137, 138 However, like the use of pacifiers, the techniques described in this study should not be attempted until breastfeeding success is well established.
While those who advocate for breastfeeding “on demand” may initially be averse to attempts to lengthen sleep duration, it is important to recognize that there is no uniform definition of “on demand” and mothers may interpret “feeding on demand” in a highly variable fashion. Thus, teaching mothers sleep lengthening techniques may potentially enhance their ability to distinguish hunger cues from other distress cues, improve feelings of parental competence, reduce formula use, and increase the duration of breastfeeding.
Parental regulation of distress, temperament, and self-regulation of emotion
The ability to regulate behavior and emotion are important developmental tasks.139 Moreover, the inability to successfully regulate one’s emotional state characterizes many childhood problem behaviors.140 The self-regulation of emotion may also have important implications for other areas of development such as physical health, more specifically weight gain. There are several possible reasons why emotion regulation may be important in understanding and potentially preventing abnormal weight gain. First, infant difficultness, a temperamental quality characterized by fussiness and difficulty soothing, has been related to rapid weight gain141 and later body composition142 in childhood while negative child emotionality has been linked to adult body mass.143 Next, studies of emotion and eating in adults show emotions, particularly negative emotions, to be related to increased eating, prompting theorists to hypothesize that obese individuals eat to reduce discomfort.144 Finally, there is increasing evidence that mental health problems such as depression and conduct disorder are strong predictors of adulthood obesity.145 This link may be biological as several central nervous system processes responsible for feeding regulation also are involved in regulating emotion.146 Taken together, these data suggest that the ability to self-regulate emotion may be an important factor in preventing obesity.
Developmental theorists agree that the soothing environment provided by the parent serves not only to alleviate immediate distress, but also facilitates the infant’s development of self-regulation.139, 147 Soothing a distressed infant models emotion regulatory strategies and demonstrates the effectiveness of various behaviors for reducing distress. Previous research has shown parental sensitivity, or contingent responsiveness to infant cues predict infant crying and behavior.148 That is, parents exhibiting high sensitivity had infants who cried less both concurrently and longitudinally. Furthermore, while some researchers have examined the effect of certain soothing techniques on reducing infant distress or supporting concurrent infant regulation,149, 150 only one study has demonstrated the carry-over effect of parental regulation to infant self-regulation. Jahromi and Stifter found that mothers who were most effective in soothing their infants at 2 months had infants who cried less with immunization injections 4 months later.149
Unfortunately from an obesity prevention perspective, many parents use feeding as a method to soothe a distressed infant, and this practice may have negative consequences for weight gain.151 Similarly, using food to reward or punish behavior in children has been associated with binge eating and heavier weight status when those children become adults.152 Thus, while parent regulation of distress is important to the development of the child’s ability to self-regulate his/her emotion, the use of food to soothe or reward may contribute to unhealthy outcomes.
Potential Intervention
As feeding in infancy is predominantly under the control of the parent, using food in circumstances unrelated to hunger and sustenance may lead to children’s understanding that food has other ‘reward-like’ qualities. Infants may learn to eat in response to cues other than hunger, such as the presence of food, or their own emotional distress. This compromised ability to self-regulate their food intake may put them at risk for overweight. Given this evidence and that parents report using food to soothe their children,67 parental regulation appears to be a critical variable in the development of children’s overall self-regulation skills.
One simple strategy parents can employ is to use non-food items to soothe during early infancy and non-food rewards for good behaviors during later infancy. Alternative soothing strategies for young infants are discussed above in relation to sleep and can be applied during the day as well. For older infants, praise or rewards with stickers, toys, book reading, singing songs, playing, or visits to special places may be good alternatives to rewarding good behaviors with food.
As for the core issue of improving parental regulation, the results of two studies suggest that the effect of improving parental sensitivity may be most important for the highly reactive infant. In one study, an intervention focused on mothers of irritable infants found that training mothers to respond contingently and appropriately to the fussing and crying of the infant improved maternal interactive behavior and infant self soothing, exploration, and attachment.153 In the second study, an intervention aimed to improve mother-infant attachment found the effect to be greatest for those infants who were highest in negative emotionality.154 Taken together, these studies suggest that parents should 1) recognize that infant distress is a signal to act, 2) respond quickly as waiting does not reduce crying, and 3) use strategies such as rocking, presenting alternative activities, and providing a pacifier, to reduce the crying and fussing. Not only does this ameliorate the infant’s distress but, if applied consistently, will enhance the parent-child relationship, and demonstrate how the child might self-regulate their own emotions in the future. Promoting improved parental regulation of infant distress as well as less intense negative responses from the infant appears to be essential to the development of the child’s ability to self-regulate. Furthermore, interventions that provide the parents with alternative strategies to using food to soothe may not only be practical and economical, but may directly prevent childhood obesity.
Introduction of Solid Foods
Timing of solid food introduction
The American Academy of Pediatrics (AAP) suggests that the introduction of solid foods should begin between 4 and 6 months because, in general, exclusive milk feeding is adequate to support growth until this time, and supplementary foods are not needed.155, 156 Others add that solids should not be introduced until an infant has good head and neck control and can sit with support.157 Recent NHANES data suggests, however, that about 30% of breastfed infants and about 50% of formula fed infants are consuming some infant cereal by 2-3 months.158 Further, data from the Early Childhood Longitudinal Study showed that in a nationally representative cohort, children placed in child care prior to 3 months of age were nearly twice as likely to receive introduction of solids prior to turning 4 months of age.159 Also, many parents continue to add cereal to their infant’s bottle, a practice not supported by the AAP because it can lead to excessive weight gain.160 Related to the previous discussion about sleep and regulation of distress, one commonly attempted approach to improve infant sleep is to give infant cereal at bedtime, a practice that has not been shown to be effective at helping infants sleep despite widespread belief that the early addition of solids promotes sleeping through the night.161 Importantly, the time when solids are first introduced may be related to increased caloric intake, rapid weight gain and the subsequent development of overweight.
When the topic of the relationship between the timing of introduction of complimentary foods and subsequent obesity has been evaluated in large, population based studies, there has been minimal to little influence of this variable on the development of obesity.79, 80 However, several more focused studies have revealed important associations. Shukla et al. found that overweight status at 13 weeks was related to the extra calories provided by solid foods early in life, and overweight status at age 13 weeks persisted through age 1 year.162 Similarly, von Kries et al showed a relationship between introduction of solids before age 4 months and the risk of overweight status between ages 5 and 6 years.11 Others have further characterized this relationship by showing the association between increased rate of weight gain in the first 6-12 months after birth and early introduction of solids particularly for formula fed infants.159, 163-165 Baker and colleagues analysis of the Danish National Birth Cohort revealed perhaps the most intriguing data on this subject. Their regression analyses showed that the relationship between maternal obesity and greater weight gain during the first year could be nearly eliminated by breastfeeding for more than 40 weeks and delaying the introduction of complimentary foods until after 20 weeks of age.166
Method of solid food introduction and the use of repeated exposure
Across cultures, dietary diversity is vast, but all infants begin life consuming the same food: milk. However, as omnivores, they are prepared to learn to consume the diet of their culture. Infants “come equipped” to prefer sweet and salty tastes, to be “neophobic” and reject new foods when they are first offered (at least those that are not sweet or salty), and to learn to like foods of the adult diet of their culture and ethnicity, via various associative conditioning processes that involve the pairing of food with the aspects of the social contexts and physiological consequences of eating.167 Given this set of predispositions, all normal infants will readily accept sweet and salty foods such as French fries and sweetened drinks. In contrast, many healthy foods such as pureed vegetables, infant cereals, meats and dairy products, which are not high in sugar or salt, will be initially rejected by infants. These findings have revealed that infants typically need several opportunities to sample these new foods before intake will increase.168, 169 The liking for complex food flavors that are not dominated by sweet or salty tastes must be learned.
Potential Intervention
In addition to delaying the introduction of complimentary foods until 4-6 months of age, parents should be instructed on the infant neophobic response to new foods. Parents often interpret the initial rejection of new foods as “She doesn’t like it”, and the food is not offered again. However, the infant’s initial neophobic response is usually transient, and that infants’, toddlers’ and preschoolers’ intake of new healthy foods will typically increase if the infant has repeated opportunities to taste them.168-171 As few as 1 or 2 exposures169 or as many as 5 or 10 exposures170 may be needed, depending on the age of the child; and all foods will not be accepted by some children, despite repeated exposure. However, parents must be instructed that such repeated exposure is necessary if not sufficient for acceptance of new foods that are not very sweet or salty. Most of the healthy foods that are developmentally appropriate for infants and toddlers fall into this category, including most vegetables, complex carbohydrates, and meat and dairy products. While exceptions to these instructions are cases in which food aversions and dislikes develop when consumption is followed nausea or vomiting, or when eating is coerced or unpleasant, parents need guidance on how to introduce new foods to increase the likelihood that the child will learn to consume a variety of foods that will constitute a balanced diet that promotes healthy weight gain.
In addition to repeated exposure to healthy foods, parents should be alerted to cues for fullness when feeding complimentary foods. Pursed lips, closed mouth, spitting out food, turning of the head, and leaning back are examples of cues to stop feeding.157
Obesity Prevention during Later Infancy and the Early Toddler Years
Parent Feeding Style
During the first years of life, infants and young children are learning an enormous amount about food and eating, as they are being introduced to the adult diet of their culture. They learn when to eat, what is food and what is not, how much to eat, and as a result of their experiences with food and eating, are developing food preferences and dislikes. The period from birth to 3 years is also a crucial one for the development of the controls of food intake and the development of food preferences and eating behaviors.167 There is evidence that early feeding practices are linked to patterns of food acceptance and the developing controls of food intake.167, 172, 173 A feeding style using coercion is unlikely to be successful in the short term, and can result in unhealthy weight status in the long term as recent data suggest that maternal control of feeding during the first years after birth moderates infant weight gain.174, 175 Coercive feeding practices include tactics such as 1) pressuring children to finish their vegetables, or 2) restricting their access to sweets and junk food, or using such foods as rewards.71 In addition to promoting dislikes for healthy foods, and increased liking and wanting of restricted junk foods, coercive practices can also promote dysregulation of intake by promoting over eating, and learning to eat in response to the presence of food on the plate (as in “finish your vegetables”).176-178
Potential Intervention
When introducing solids, parents should be aware that new foods may be initially rejected, and should be advised to be patient, as learning to like new foods takes time. If parents offer new foods repeatedly, over a series of 5 or 10 days, many of these foods will eventually be accepted and even preferred.168-170 However, pressuring or coercive feeding practices engender resistant and foster dislikes, and should be discouraged in favor of providing repeated experience in positive contexts. During the transition to table foods, parents can be effective positive models promoting infant acceptance and liking for healthy foods by consuming healthy foods and avoiding “junk foods” at family meals. The use of positive feeding practices such as repeated exposure and modeling are more likely to promote the establishment of healthy diets than the use of coercive feeding practices.179 Parents should be advised to avoid pressure and restriction in feeding, and encouraged to put their efforts into promoting liking and acceptance of table foods that are part of a healthy diet.
Transition from Human Milk or Formula to Cow’s Milk
While consumption of human milk or infant formula may continue for over one year, the majority of infants transition to cow’s milk at 1 year of age. As opposed to children 2 years of age or older, however, many do not recommend the use of non-fat or low-fat milk for children 12-23 months of age.180-183 This recommendation likely stems from concerns from years ago that infants consume a sufficient quantity of dietary fat and essential fatty acids for normal growth and development. However, as opposed to the evidence for infants less than 12 months, the recommendation for 12-23 month olds is not evidence based.184
The question of milk fat intake is important since the preference for high-fat foods develops early in life and children still consume 20-25% of their calories from cow’s milk between ages 1 and 2 years.185, 186 Further, a majority of pre-school children drink whole milk, particularly those children who are minorities or from low-income households.187, 188
Potential intervention
Reducing milk fat intake has been previously identified as a target for dietary fat reduction and obesity prevention in toddlers and pre-school children,189-191 and reducing fat intake among infants and toddlers has been shown to be well tolerated without adverse effects on growth, nutrient intake, or development.192-194 Conversely, high fat intake between 12 and 23 months of age has been associated with inhibition of the normal decrease in body fat between 2 and 5 years of age.195 Given that contemporary diets for children over age 1 year typically contain a significant amount of dietary fat from non-milk sources,196 the common advice to only use whole milk for children ages 12-23 months is no longer necessary for infants that consume a well-balanced diet.187 In fact, the 2008 AAP policy statement, “Lipid Screening and Cardiovascular Health in Childhood” includes as its first recommendation the use of reduced fat milk for 12-23 month old children.197 While studies of older children have suggested that consumption of dairy fat is not associated with weight gain,198 since each cup of whole milk contains 146 kilocalories compared with only 86 kilocalories per cup from nonfat milk,199 a change to low-fat or even non-fat milk could reduce energy consumption without adverse effects for infants.
Sweet Beverage Consumption
Over the past three decades, the percentage of daily calories obtained from soft drinks, fruit drinks, sweetened beverages, and fruit juice each have steadily increased among American children.200 Among children 12-24 months old, 100% juice and sweetened beverages account for the second and third greatest source of dietary calories respectively, exceeded only by milk.186 While data have, in general, not supported a link between consumption of 100% juice and obesity unless consumed in excess,201 there is a strong association between sweetened beverages and soft drinks with obesity.202 Further, as suggested by Skinner et al., because early life diet preferences predict later preferences, the development of beverage consumption patterns prior to age two years is important for long term consumption.203
Regarding infant and toddler consumption of juice, the AAP has recommended that juice a) not be given to infants less than 6 months of age, b) only be given to infants that can drink from a cup and never given in a bottle, c) not be given in a fashion that allows for a child to easily transport it with easy consumption throughout the day, and d) not be given in quantities greater than 6 ounces per day.204 Data from the Feeding Infants and Toddlers Study (FITS), a national dietary survey, demonstrated that many infants consume fruit juice prior to 6 months and exceed the recommended amount of juice later during infancy and the toddler years.203
Unlike fruit juice, the AAP has no formal policy statement or recommendation regarding the consumption of other sweetened beverages and soft drinks prior to school entry, but the Institute of Medicine has recommended the avoidance of high calorie, nutrient poor beverages.5 Notably, consumption of sweet drinks has been associated with obesity even among pre-school children.205, 206 Additionally, in FITS, sweetened drinks and soda also were being consumed at the expense of milk in this sample of infants and toddlers.204 Further, several authors have suggested that reducing intake of sweetened beverages is one of the most important and promising obesity prevention strategies.205-208
Potential Intervention
Given the current evidence, adherence to the AAP policy regarding fruit juice is appropriate. Further, because they have no nutritional benefit and are associated with obesity and other morbidities, the use of sweetened beverages, soft drinks, and fruit drinks should be totally discouraged for infants and toddlers. Given the alternatives of milk, water, and the now increasingly available, low-calorie flavored water, there are sufficient options for parents to give their young children.
Transitional Feeding and Table Foods
The transition from the exclusive milk diet of infancy to a modified adult diet is completed by age 3 years, and during this early period children already have begun acquiring food preferences and aversions.167 They are learning a great deal about when, what, and how much to eat. Unfortunately, recent data from FITS revealed that energy intakes among typical infants and toddlers exceed requirements by 20-30%.209 Notably, in FITS this excess already was apparent in infants aged 4-6 months where intake exceeded energy requirements by 10%, suggesting that patterns of intake were being established at an early age that were promoting excessive weight gain and obesity. In addition to consuming too much energy, from an early age (4 to 24 months) children consume significant amounts of developmentally inappropriate foods, high in energy density and low in nutrients, while consuming too few of the foods that should form the basis of a healthy weaning diet.196 The high energy density of foods offered appeared to be the same ones that contribute to energy intakes that were in excess of energy requirements in other age groups studied.209 For example, in children aged 7 and 24 months, 18% and 33% consumed no servings of vegetables, respectively, during a given 24-hour period. Twenty-three percent of 7-month old and 33% of 24-month old children did not consume any fruits. Further, parents reported that French fries were the third most common vegetable consumed by infants 9 to 11 months of age, and by 15 to 18 months were the most common vegetable consumed. The diets of infants in this age group may, not surprisingly, be deficient of key nutrients.210
Potential Intervention
The FITS findings underscore the need to provide parents with anticipatory guidance regarding the transition to a modified adult diet. The Start Healthy Feeding Guidelines for Infants and Toddlers provides excellent guidance on the nutritional needs of children less than two year of age.211 As opposed to giving children French fries, parents should be encouraged to meet these nutritional requirements with fresh fruits, cooked vegetables, cheese, yogurt, whole grain breads and crackers, and cereals.157, 212, 213 All of these foods should not have added sugar or salt.
Physical Activity and Sedentary Behaviors
There is substantial epidemiological evidence that regular physical activity is essential for good physical and psychological health and disease prevention among children and adults. However, to date, the recommendations for infant and toddler physical activity (from birth to age 5 years) have not been evidence-based. Rather, the guidelines developed by the National Association for Sport and Physical Education214 were adapted from evidence accumulated among older children and adolescents.215 The recommendations for infants suggest that they should be: 1) interacting with caregivers in daily physical activities that promote movement and exploration of their environment, 2) engaging in activities that promote the development of movement skills and large muscle activities, and 3) placed in safe settings that facilitate physical activity and do not restrict physical activity for prolonged periods of time. These recommendations suggest that toddlers should: 1) accumulate at least 30 minutes of daily structured physical activity, 2) engage in at least 60 minutes and up to several hours a day of unstructured physical activity and should not be sedentary for more than 60 minutes at a time except when sleeping, and 3) develop movement skills that are building blocks for more complex movement behaviors.214 Nonetheless, because physical activity and sedentary patterns, much like feeding and sleeping behaviors, become established in the early years, there is increasing support for promoting physical activity and reducing sedentary behaviors as soon as possible during the early infancy period.214, 216
Environmental risk factors associated with sedentary activities during the early infancy and toddler periods may predispose children to low levels of physical activity in later childhood. For example, restricting infants to car seats, swings, carriers, strollers, and small play spaces for long periods of time may limit motor development and delay physical activity such as crawling and walking.214, 217 Also, limited time for leisure activities and parent-child play, concern for neighborhood safety, and using television or computer games to occupy a child’s attention may promote sedentary lifestyle during the first three years after birth.217, 218 Television viewing during the infancy and toddler years appears to be one particular sedentary practice that is an environmental risk factor for obesity development. It is reported that 82% of 1-year old (11 average hours per week) and 96% of 2-year old (15 average hours per week) children watch television or videos, and having a television in the bedroom elevates the risk of being overweight.219 Also, Taveras and colleagues found that children who slept less than 12 hours per day and viewed 2 hours per day or more of television had a 3 year old obesity probability of 17%.112
Potential Intervention
Although there is little debate that physical activity is important for obesity prevention, questions remain about how much and what types of physical activity during the infant and early toddler years is needed to prevent later obesity. In general, parents of infants should choose physical activities that are interactive, stimulating, easy to do, and incorporated into their daily routine to reinforce the concept that physical activity is rewarding.214, 216
Additionally, two existing programs offer possible blueprints for more extensive prevention efforts. The Infant Feeding Activity and Nutrition Trial is an early intervention to prevent childhood obesity that targets infants through age 18 months in Victoria, Australia. This program teaches parents about the development of positive diet and physical activity behaviors while reducing sedentary behaviors during infancy.220 Parents in the program learn about age-appropriate physical activity behaviors, the risks associated with sedentary behaviors, and how parental modeling of physical activity and sedentary behaviors influences their child’s behaviors.
The second program, Fighting Fit Tots, also aims to prevent obesity in the first years of life by promoting toddler physical activity and parent lifestyle education.221 This program is currently being implemented in Lambeth, South London and consists of 11 weekly 2-hour sessions that include guided parent-child physical activity (e.g., jumping, skipping, hopping, dancing, singing), snack (water and fruit), and parental education (e.g., healthy lifestyle workshop) aimed at increasing physical activity behaviors, confidence, and decreasing BMI and waist circumference among children aged 18-30 months.
Regarding sedentary behavior, one clear target for intervention is television viewing. Because most children watch television by age 2 years, educational efforts and interventions about limiting television/video viewing need to be implemented before this age to potentially impact overweight development. Importantly, the AAP discourages television watching for children less than 2 years and suggests that televisions never be placed in children’s bedrooms.222
Conclusions
Given the vast array of topics that are important to cover at infant health maintenance visits, extensive discussion about growth, growth charts, and healthy lifestyle may be challenging for providers. Nonetheless, obesity and its co-morbidities threaten both individual patients and our healthcare system. To break the vicious cycle of obese children becoming obese adults who have obese offspring, preventing behaviors that lead to obesity must be implemented during the very earliest periods of life, the prenatal period and infancy. For pediatric care providers, there are numerous opportunities to intervene, and good communication with families about healthy growth and lifestyle are a good beginning.
Acknowledgments
Project Support: This work was supported by grants DK72996 and DK075867 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Additional support was received from the Penn State Children, Youth and Families Consortium.
Abbreviations
- NHANES
National Health and Nutrition Examination Survey
- BMI
Body Mass Index
- CDC
Centers for Disease Control and Prevention
- WHO
World Health Organization
- AAP
American Academy of Pediatrics
- FITS
Feeding Infants and Toddlers Study
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure and Conflicts of Interest: None
References
- 1.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003-2006. JAMA. 2008;299:2401–5. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999-2000. Jama. 2002;288:1728–32. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 3.Mei Z, Scanlon KS, Grummer-Strawn LM, Freedman DS, Yip R, Trowbridge FL. Increasing prevalence of overweight among US low-income preschool children: the Centers for Disease Control and Prevention pediatric nutrition surveillance, 1983 to 1995. Pediatrics. 1998;101:E12. doi: 10.1542/peds.101.1.e12. [DOI] [PubMed] [Google Scholar]
- 4.Kim J, Peterson KE, Scanlon KS, et al. Trends in overweight from 1980 through 2001 among preschool-aged children enrolled in a health maintenance organization. Obesity (Silver Spring) 2006;14:1107–12. doi: 10.1038/oby.2006.126. [DOI] [PubMed] [Google Scholar]
- 5.Koplan JP, Liverman CT, Kraak VI, editors. Preventing childhood obesity: Health in the balance. The National Academies Press; Washington, D.C.: 2005. [PubMed] [Google Scholar]
- 6.Lederman SA, Akabas SR, Moore BJ. Editors’ overview of the conference on preventing childhood obesity. Pediatrics. 2004;114:1139–45. [Google Scholar]
- 7.Eid EE. Follow-up study of physical growth of children who had excessive weight gain in first six months of life. Br Med J. 1970;2:74–6. doi: 10.1136/bmj.2.5701.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ong KK, Ahmed ML, Emmett PM, Preece MA, Dunger DB. Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. Bmj. 2000;320:967–71. doi: 10.1136/bmj.320.7240.967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reilly JJ, Armstrong J, Dorosty AR, et al. Early life risk factors for obesity in childhood: cohort study. Bmj. 2005;330:1358–60. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stettler N, Zemel BS, Kumanyika S, Stallings VA. Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics. 2002;109:194–9. doi: 10.1542/peds.109.2.194. [DOI] [PubMed] [Google Scholar]
- 11.von Kries R, Toschke AM, Wurmser H, Sauerwald T, Koletzko B. Reduced risk for overweight and obesity in 5- and 6-y-old children by duration of sleep--a cross-sectional study. Int J Obes Relat Metab Disord. 2002;26:710–6. doi: 10.1038/sj.ijo.0801980. [DOI] [PubMed] [Google Scholar]
- 12.Cameron N, Pettifor J, De Wet T, Norris S. The relationship of rapid weight gain in infancy to obesity and skeletal maturity in childhood. Obes Res. 2003;11:457–60. doi: 10.1038/oby.2003.62. [DOI] [PubMed] [Google Scholar]
- 13.Mellbin T, Vuille JC. Physical development at 7 years of age in relation to velocity of weight gain in infancy with special reference to incidence of overweight. Br J Prev Soc Med. 1973;27:225–35. doi: 10.1136/jech.27.4.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stettler N, Kumanyika SK, Katz SH, Zemel BS, Stallings VA. Rapid weight gain during infancy and obesity in young adulthood in a cohort of African Americans. Am J Clin Nutr. 2003;77:1374–8. doi: 10.1093/ajcn/77.6.1374. [DOI] [PubMed] [Google Scholar]
- 15.Ekelund U, Ong K, Linne Y, et al. Upward weight percentile crossing in infancy and early childhood independently predicts fat mass in young adults: the Stockholm Weight Development Study (SWEDES) Am J Clin Nutr. 2006;83:324–30. doi: 10.1093/ajcn/83.2.324. [DOI] [PubMed] [Google Scholar]
- 16.Monteiro PO, Victora CG, Barros FC, Monteiro LM. Birth size, early childhood growth, and adolescent obesity in a Brazilian birth cohort. Int J Obes Relat Metab Disord. 2003;27:1274–82. doi: 10.1038/sj.ijo.0802409. [DOI] [PubMed] [Google Scholar]
- 17.Wells JC, Hallal PC, Wright A, Singhal A, Victora CG. Fetal, infant and childhood growth: relationships with body composition in Brazilian boys aged 9 years. Int J Obes (Lond) 2005;29:1192–8. doi: 10.1038/sj.ijo.0803054. [DOI] [PubMed] [Google Scholar]
- 18.Sachdev HS, Fall CH, Osmond C, et al. Anthropometric indicators of body composition in young adults: relation to size at birth and serial measurements of body mass index in childhood in the New Delhi birth cohort. Am J Clin Nutr. 2005;82:456–66. doi: 10.1093/ajcn.82.2.456. [DOI] [PubMed] [Google Scholar]
- 19.Blair NJ, Thompson JM, Black PN, et al. Risk factors for obesity in 7-year-old European children: the Auckland Birthweight Collaborative Study. Arch Dis Child. 2007;92:866–71. doi: 10.1136/adc.2007.116855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dennison BA, Edmunds LS, Stratton HH, Pruzek RM. Rapid infant weight gain predicts childhood overweight. Obesity (Silver Spring) 2006;14:491–9. doi: 10.1038/oby.2006.64. [DOI] [PubMed] [Google Scholar]
- 21.Hui LL, Schooling CM, Leung SS, et al. Birth weight, infant growth, and childhood body mass index: Hong Kong’s children of 1997 birth cohort. Arch Pediatr Adolesc Med. 2008;162:212–8. doi: 10.1001/archpediatrics.2007.62. [DOI] [PubMed] [Google Scholar]
- 22.Botton J, Heude B, Maccario J, Ducimetiere P, Charles MA. Postnatal weight and height growth velocities at different ages between birth and 5 y and body composition in adolescent boys and girls. Am J Clin Nutr. 2008;87:1760–8. doi: 10.1093/ajcn/87.6.1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yliharsila H, Kajantie E, Osmond C, Forsen T, Barker DJ, Eriksson JG. Body mass index during childhood and adult body composition in men and women aged 56-70 y. Am J Clin Nutr. 2008;87:1769–75. doi: 10.1093/ajcn/87.6.1769. [DOI] [PubMed] [Google Scholar]
- 24.Chomtho S, Wells JC, Williams JE, Davies PS, Lucas A, Fewtrell MS. Infant growth and later body composition: evidence from the 4-component model. Am J Clin Nutr. 2008;87:1776–84. doi: 10.1093/ajcn/87.6.1776. [DOI] [PubMed] [Google Scholar]
- 25.Singhal A, Cole TJ, Fewtrell M, Deanfield J, Lucas A. Is slower early growth beneficial for long-term cardiovascular health? Circulation. 2004;109:1108–13. doi: 10.1161/01.CIR.0000118500.23649.DF. [DOI] [PubMed] [Google Scholar]
- 26.Huxley RR, Shiell AW, Law CM. The role of size at birth and postnatal catch-up growth in determining systolic blood pressure: a systematic review of the literature. J Hypertens. 2000;18:815–31. doi: 10.1097/00004872-200018070-00002. [DOI] [PubMed] [Google Scholar]
- 27.Law CM, Shiell AW, Newsome CA, et al. Fetal, infant, and childhood growth and adult blood pressure: a longitudinal study from birth to 22 years of age. Circulation. 2002;105:1088–92. doi: 10.1161/hc0902.104677. [DOI] [PubMed] [Google Scholar]
- 28.Parker L, Lamont DW, Unwin N, et al. A lifecourse study of risk for hyperinsulinaemia, dyslipidaemia and obesity (the central metabolic syndrome) at age 49-51 years. Diabet Med. 2003;20:406–15. doi: 10.1046/j.1464-5491.2003.00949.x. [DOI] [PubMed] [Google Scholar]
- 29.Eriksson JG, Forsen T, Tuomilehto J, Winter PD, Osmond C, Barker DJ. Catch-up growth in childhood and death from coronary heart disease: longitudinal study. Bmj. 1999;318:427–31. doi: 10.1136/bmj.318.7181.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barker DJ, Osmond C, Forsen TJ, Kajantie E, Eriksson JG. Trajectories of growth among children who have coronary events as adults. N Engl J Med. 2005;353:1802–9. doi: 10.1056/NEJMoa044160. [DOI] [PubMed] [Google Scholar]
- 31.Forsen T, Eriksson J, Tuomilehto J, Reunanen A, Osmond C, Barker D. The fetal and childhood growth of persons who develop type 2 diabetes. Ann Intern Med. 2000;133:176–82. doi: 10.7326/0003-4819-133-3-200008010-00008. [DOI] [PubMed] [Google Scholar]
- 32.Bhargava SK, Sachdev HS, Fall CH, et al. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med. 2004;350:865–75. doi: 10.1056/NEJMoa035698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fisch RO, Bilek MK, Ulstrom R. Obesity and leanness at birth and their relationship to body habitus in later childhood. Pediatrics. 1975;56:521–8. [PubMed] [Google Scholar]
- 34.Charney E, Goodman HC, McBride M, Lyon B, Pratt R. Childhood antecedents of adult obesity. Do chubby infants become obese adults? N Engl J Med. 1976;295:6–9. doi: 10.1056/NEJM197607012950102. [DOI] [PubMed] [Google Scholar]
- 35.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 36.Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. 2002;76:653–8. doi: 10.1093/ajcn/76.3.653. [DOI] [PubMed] [Google Scholar]
- 37.Mei Z, Grummer-Strawn LM, Scanlon KS. Does overweight in infancy persist through the preschool years? An analysis of CDC Pediatric Nutrition Surveillance System data. Soz Praventivmed. 2003;48:161–7. doi: 10.1007/s00038-003-2022-x. [DOI] [PubMed] [Google Scholar]
- 38.Sayer AA, Syddall HE, Dennison EM, et al. Birth weight, weight at 1 y of age, and body composition in older men: findings from the Hertfordshire Cohort Study. Am J Clin Nutr. 2004;80:199–203. doi: 10.1093/ajcn/80.1.199. [DOI] [PubMed] [Google Scholar]
- 39.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: The Bogalusa heart study. Pediatrics. 2005;115:22–7. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 40.Nader PR, O’Brien M, Houts R, et al. Identifying risk for obesity in early childhood. Pediatrics. 2006;118:e594–601. doi: 10.1542/peds.2005-2801. [DOI] [PubMed] [Google Scholar]
- 41.Vogels N, Posthumus DL, Mariman EC, et al. Determinants of overweight in a cohort of Dutch children. Am J Clin Nutr. 2006;84:717–24. doi: 10.1093/ajcn/84.4.717. [DOI] [PubMed] [Google Scholar]
- 42.Jouret B, Ahluwalia N, Cristini C, et al. Factors associated with overweight in preschool-age children in southwestern France. Am J Clin Nutr. 2007;85:1643–9. doi: 10.1093/ajcn/85.6.1643. [DOI] [PubMed] [Google Scholar]
- 43.Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22:167–77. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- 44.Garn SM, LaVelle M. Two-decade follow-up of fatness in early childhood. Am J Dis Child. 1985;139:181–5. doi: 10.1001/archpedi.1985.02140040083033. [DOI] [PubMed] [Google Scholar]
- 45.Rolland-Cachera MF, Deheeger M, Guilloud-Bataille M, Avons P, Patois E, Sempe M. Tracking the development of adiposity from one month of age to adulthood. Ann Hum Biol. 1987;14:219–29. doi: 10.1080/03014468700008991. [DOI] [PubMed] [Google Scholar]
- 46.Muramatsu S, Sato Y, Miyao M, Muramatsu T, Ito A. A longitudinal study of obesity in Japan: relationship of body habitus between at birth and at age 17. Int J Obes. 1990;14:39–45. [PubMed] [Google Scholar]
- 47.Singhal A, Lucas A. Early origins of cardiovascular disease: is there a unifying hypothesis? Lancet. 2004;363:1642–5. doi: 10.1016/S0140-6736(04)16210-7. [DOI] [PubMed] [Google Scholar]
- 48.Gillman MW. The first months of life: a critical period for development of obesity. Am J Clin Nutr. 2008;87:1587–9. doi: 10.1093/ajcn/87.6.1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oken E, Taveras EM, Kleinman KP, Rich-Edwards JW, Gillman MW. Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol. 2007;196:322 e1–8. doi: 10.1016/j.ajog.2006.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Whitaker RC. Predicting preschooler obesity at birth: the role of maternal obesity in early pregnancy. Pediatrics. 2004;114:e29–36. doi: 10.1542/peds.114.1.e29. [DOI] [PubMed] [Google Scholar]
- 51.Gillman MW, Rifas-Shiman SL, Kleinman K, Oken E, Rich-Edwards JW, Taveras EM. Developmental origins of childhood overweight: potential public health impact. Obesity (Silver Spring) 2008;16:1651–6. doi: 10.1038/oby.2008.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jaffe M, Kosakov C. The motor development of fat babies. Clin Pediatr (Phila) 1982;21:619–21. doi: 10.1177/000992288202101011. [DOI] [PubMed] [Google Scholar]
- 53.Shibli R, Rubin L, Akons H, Shaoul R. Morbidity of overweight (>or=85th percentile) in the first 2 years of life. Pediatrics. 2008;122:267–72. doi: 10.1542/peds.2007-2867. [DOI] [PubMed] [Google Scholar]
- 54.Wake M, Hardy P, Sawyer MG, Carlin JB. Comorbidities of overweight/obesity in Australian preschoolers: a cross-sectional population study. Arch Dis Child. 2008;93:502–7. doi: 10.1136/adc.2007.128116. [DOI] [PubMed] [Google Scholar]
- 55.Taveras EM, Rifas-Shiman SL, Camargo CA, Jr., et al. Higher adiposity in infancy associated with recurrent wheeze in a prospective cohort of children. J Allergy Clin Immunol. 2008;121:1161–6 e3. doi: 10.1016/j.jaci.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jain A, Sherman SN, Chamberlin LA, Carter Y, Powers SW, Whitaker RC. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics. 2001;107:1138–46. doi: 10.1542/peds.107.5.1138. [DOI] [PubMed] [Google Scholar]
- 57.Sherry B, McDivitt J, Birch LL, et al. Attitudes, practices, and concerns about child feeding and child weight status among socioeconomically diverse white, Hispanic, and African-American mothers. J Am Diet Assoc. 2004;104:215–21. doi: 10.1016/j.jada.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 58.Jackson J, Strauss CC, Lee AA, Hunter K. Parents’ accuracy in estimating child weight status. Addict Behav. 1990;15:65–8. doi: 10.1016/0306-4603(90)90007-k. [DOI] [PubMed] [Google Scholar]
- 59.Baughcum AE, Chamberlin LA, Deeks CM, Powers SW, Whitaker RC. Maternal perceptions of overweight preschool children. Pediatrics. 2000;106:1380–6. doi: 10.1542/peds.106.6.1380. [DOI] [PubMed] [Google Scholar]
- 60.Maynard LM, Galuska DA, Blanck HM, Serdula MK. Maternal perceptions of weight status of children. Pediatrics. 2003;111:1226–31. [PubMed] [Google Scholar]
- 61.Jeffery AN, Voss LD, Metcalf BS, Alba S, Wilkin TJ. Parents’ awareness of overweight in themselves and their children: cross sectional study within a cohort (EarlyBird 21) Bmj. 2005;330:23–4. doi: 10.1136/bmj.38315.451539.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Carnell S, Edwards C, Croker H, Boniface D, Wardle J. Parental perceptions of overweight in 3-5 y olds. Int J Obes (Lond) 2005;29:353–5. doi: 10.1038/sj.ijo.0802889. [DOI] [PubMed] [Google Scholar]
- 63.Eckstein KC, Mikhail LM, Ariza AJ, Thomson JS, Millard SC, Binns HJ. Parents’ perceptions of their child’s weight and health. Pediatrics. 2006;117:681–90. doi: 10.1542/peds.2005-0910. [DOI] [PubMed] [Google Scholar]
- 64.Campbell MW, Williams J, Hampton A, Wake M. Maternal concern and perceptions of overweight in Australian preschool-aged children. Med J Aust. 2006;184:274–7. doi: 10.5694/j.1326-5377.2006.tb00236.x. [DOI] [PubMed] [Google Scholar]
- 65.Reifsnider E, Flores-Vela AR, Beckman-Mendez D, Nguyen H, Keller C, Dowdall-Smith S. Perceptions of children’s body sizes among mothers living on the Texas-Mexico border (La Frontera) Public Health Nurs. 2006;23:488–95. doi: 10.1111/j.1525-1446.2006.00588.x. [DOI] [PubMed] [Google Scholar]
- 66.Kramer MS, Barr RG, Leduc DG, Boisjoly C, Pless IB. Maternal psychological determinants of infant obesity. Development and testing of two new instruments. J Chronic Dis. 1983;36:329–35. doi: 10.1016/0021-9681(83)90118-2. [DOI] [PubMed] [Google Scholar]
- 67.Baughcum AE, Burklow KA, Deeks CM, Powers SW, Whitaker RC. Maternal feeding practices and childhood obesity: a focus group study of low-income mothers. Arch Pediatr Adolesc Med. 1998;152:1010–4. doi: 10.1001/archpedi.152.10.1010. [DOI] [PubMed] [Google Scholar]
- 68.Bentley M, Gavin L, Black MM, Teti L. Infant feeding practices of low-income, African-American, adolescent mothers: an ecological, multigenerational perspective. Soc Sci Med. 1999;49:1085–100. doi: 10.1016/s0277-9536(99)00198-7. [DOI] [PubMed] [Google Scholar]
- 69.Contento IR, Basch C, Zybert P. Body image, weight, and food choices of Latina women and their young children. J Nutr Educ Behav. 2003;35:236–48. doi: 10.1016/s1499-4046(06)60054-7. [DOI] [PubMed] [Google Scholar]
- 70.Boyington JA, Johnson AA. Maternal perception of body size as a determinant of infant adiposity in an African-American community. J Natl Med Assoc. 2004;96:351–62. [PMC free article] [PubMed] [Google Scholar]
- 71.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–49. [PubMed] [Google Scholar]
- 72.Bruss MB, Morris J, Dannison L. Prevention of childhood obesity: sociocultural and familial factors. J Am Diet Assoc. 2003;103:1042–5. doi: 10.1016/s0002-8223(03)00472-3. [DOI] [PubMed] [Google Scholar]
- 73.Karaolis-Danckert N, Buyken AE, Bolzenius K, Perim de Faria C, Lentze MJ, Kroke A. Rapid growth among term children whose birth weight was appropriate for gestational age has a longer lasting effect on body fat percentage than on body mass index. Am J Clin Nutr. 2006;84:1449–55. doi: 10.1093/ajcn/84.6.1449. [DOI] [PubMed] [Google Scholar]
- 74.Lederman SA, Akabas SR, Moore BJ, et al. Summary of the presentations at the conference on preventing childhood obesity, December 8, 2003. Pediatrics. 2004;114:1146–73. [Google Scholar]
- 75.Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics. 2005;115:1367–77. doi: 10.1542/peds.2004-1176. [DOI] [PubMed] [Google Scholar]
- 76.Owen CG, Martin RM, Whincup PH, Davey-Smith G, Gillman MW, Cook DG. The effect of breastfeeding on mean body mass index throughout life: a quantitative review of published and unpublished observational evidence. Am J Clin Nutr. 2005;82:1298–307. doi: 10.1093/ajcn/82.6.1298. [DOI] [PubMed] [Google Scholar]
- 77.Arenz S, Ruckerl R, Koletzko B, von Kries R. Breast-feeding and childhood obesity--a systematic review. Int J Obes Relat Metab Disord. 2004;28:1247–56. doi: 10.1038/sj.ijo.0802758. [DOI] [PubMed] [Google Scholar]
- 78.Dewey KG. Is breastfeeding protective against child obesity? J Hum Lact. 2003;19:9–18. doi: 10.1177/0890334402239730. [DOI] [PubMed] [Google Scholar]
- 79.Hediger ML, Overpeck MD, Kuczmarski RJ, Ruan WJ. Association between infant breastfeeding and overweight in young children. Jama. 2001;285:2453–60. doi: 10.1001/jama.285.19.2453. [DOI] [PubMed] [Google Scholar]
- 80.Gillman MW, Rifas-Shiman SL, Camargo CA, Jr., et al. Risk of overweight among adolescents who were breastfed as infants. Jama. 2001;285:2461–7. doi: 10.1001/jama.285.19.2461. [DOI] [PubMed] [Google Scholar]
- 81.Bogen DL, Hanusa BH, Whitaker RC. The effect of breastfeeding with and without concurrent formula feeding on the risk of obesity at 4 years of age: a retrospective cohort study. Obesity Research. 2004;12:1527–35. doi: 10.1038/oby.2004.190. [DOI] [PubMed] [Google Scholar]
- 82.von Kries R, Koletzko B, Sauerwald T, et al. Breast feeding and obesity: cross sectional study. Bmj. 1999;319:147–50. doi: 10.1136/bmj.319.7203.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics. 2005;115:1367–77. doi: 10.1542/peds.2004-1176. [DOI] [PubMed] [Google Scholar]
- 84.Harder T, Bergmann R, Kallischnigg G, Plagemann A. Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol. 2005;162:397–403. doi: 10.1093/aje/kwi222. [DOI] [PubMed] [Google Scholar]
- 85.Dewey KG, Heinig MJ, Nommsen LA, Lonnerdal B. Maternal versus infant factors related to breast milk intake and residual milk volume: the DARLING study. Pediatrics. 1991;87:829–37. [PubMed] [Google Scholar]
- 86.Wright P, Fawcett J, Crow R. The development of differences in the feeding behaviour of bottle and breast fed human infants from birth to two months. Behavioural Processes. 1980;5:1–20. doi: 10.1016/0376-6357(80)90045-5. [DOI] [PubMed] [Google Scholar]
- 87.Dewey KG, Nommsen-Rivers LA, Lonnerdal B. Plasma insulin and insulin-releasing amino acid (IRAA) concentrations are higher in formula fed than breastfed infants at 5 months of age. Experimental Biology. 2004 abstract # 1124. [Google Scholar]
- 88.Jensen RG, editor. Handbook of Milk Composition. Academic Press; San Diego: 1995. [Google Scholar]
- 89.Hambraeus L. Proprietary milk versus human breast milk in infant feeding. A critical appraisal from the nutritional point of view. Pediatr Clin North Am. 1977;24:17–36. doi: 10.1016/s0031-3955(16)33384-3. [DOI] [PubMed] [Google Scholar]
- 90.Oftedal OT, Iverson SJ. Comparative analysis of nonhuman milks: phylogenetic variation in the gross composition of milks. In: Jensen RG, editor. Handbook of Milk Composition. Academic Press; San Diego: 1995. pp. 749–89. [Google Scholar]
- 91.EU Childhood Obesity Programme . EU Childhood Obesity Programme press pack. Budapest: Apr 20, 2007. 2007. [Google Scholar]
- 92.Read LC, Penttila IA, Howarth GS, Clarke JM, Regester GO. Role and function of growth factors in infant nutrition. In: Raiha NCR, Rubaltelli FF, editors. Infant formula: closer to the reference. Vevey/Lippincott Williams & Wilkins; Philadelphia: 2002. pp. 185–95. [Google Scholar]
- 93.Savino F, Fissore MF, Grassino EC, Nanni GE, Oggero R, Silvestro L. Ghrelin, leptin and IGF-I levels in breast-fed and formula-fed infants in the first years of life. Acta Paediatr. 2005;94:531–7. doi: 10.1111/j.1651-2227.2005.tb01934.x. [DOI] [PubMed] [Google Scholar]
- 94.Elmlinger MW, Hochhaus F, Loui A, Frommer KW, Obladen M, Ranke MB. Insulin-like growth factors and binding proteins in early milk from mothers of preterm and term infants. Horm Res. 2007;68:124–31. doi: 10.1159/000100488. [DOI] [PubMed] [Google Scholar]
- 95.Martin LJ, Woo JG, Geraghty SR, et al. Adiponectin is present in human milk and is associated with maternal factors. Am J Clin Nutr. 2006;83:1106–11. doi: 10.1093/ajcn/83.5.1106. [DOI] [PubMed] [Google Scholar]
- 96.Dundar NO, Anal O, Dundar B, Ozkan H, Caliskan S, Buyukgebiz A. Longitudinal investigation of the relationship between breast milk leptin levels and growth in breast-fed infants. J Pediatr Endocrinol Metab. 2005;18:181–7. doi: 10.1515/jpem.2005.18.2.181. [DOI] [PubMed] [Google Scholar]
- 97.Miralles O, Sanchez J, Palou A, Pico C. A physiological role of breast milk leptin in body weight control in developing infants. Obesity (Silver Spring) 2006;14:1371–7. doi: 10.1038/oby.2006.155. [DOI] [PubMed] [Google Scholar]
- 98.Dewey KG. Growth characteristics of breast-fed compared to formula-fed infants. Biol Neonate. 1998;74:94–105. doi: 10.1159/000014016. [DOI] [PubMed] [Google Scholar]
- 99.Dewey KG, Heinig MJ, Nommsen LA, Peerson JM, Lonnerdal B. Breast-fed infants are leaner than formula-fed infants at 1 y of age: the DARLING study. Am J Clin Nutr. 1993;57:140–5. doi: 10.1093/ajcn/57.2.140. [DOI] [PubMed] [Google Scholar]
- 100.American Academy of Pediatrics policy statement: breastfeeding and the use of human milk. Pediatrics. 2005;115:496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- 101.de Onis M, Garza C, Victora CG, Onyango AW, Frongillo EA, Martines J. The WHO Multicentre Growth Reference Study: planning, study design, and methodology. Food Nutr Bull. 2004;25:S15–26. doi: 10.1177/15648265040251S103. [DOI] [PubMed] [Google Scholar]
- 102.de Onis M, Garza C, Onyango AW, Borghi E. Comparison of the WHO child growth standards and the CDC 2000 growth charts. J Nutr. 2007;137:144–8. doi: 10.1093/jn/137.1.144. [DOI] [PubMed] [Google Scholar]
- 103.Shealy K, Li R, Benton-Davis S, Grummer-Strawn L. In: The CDC Guide to Breastfeeding Interventions. US Department of Health and Human Services CfDCaP, editor. Atlanta: 2005. [Google Scholar]
- 104.National Sleep Foundation . 2000 “Sleep in America” Poll. National Sleep Foundation; Washington, D.C.: 2000. [Google Scholar]
- 105.National Sleep Foundation . 2001 “Sleep in America” Poll. National Sleep Foundation; Washington, D.C.: 2001. [Google Scholar]
- 106.National Sleep Foundation . 2002 “Sleep in America” Poll. National Sleep Foundation; Washington, D.C.: 2002. [Google Scholar]
- 107.National Sleep Foundation . 2004 “Sleep in America” Poll. National Sleep Foundation; Washington, D.C.: 2004. [Google Scholar]
- 108.Smaldone A, Honig JC, Byrne MW. Sleepless in America: inadequate sleep and relationships to health and well-being of our nation’s children. Pediatrics. 2007;119(Suppl 1):S29–37. doi: 10.1542/peds.2006-2089F. [DOI] [PubMed] [Google Scholar]
- 109.Locard E, Mamelle N, Billette A, Miginiac M, Munoz F, Rey S. Risk factors of obesity in a five year old population. Parental versus environmental factors. Int J Obes Relat Metab Disord. 1992;16:721–9. [PubMed] [Google Scholar]
- 110.Sekine M, Yamagami T, Hamanishi S, et al. Parental obesity, lifestyle factors and obesity in preschool children: results of the Toyama Birth Cohort study. J Epidemiol. 2002;12:33–9. doi: 10.2188/jea.12.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Agras WS, Hammer LD, McNicholas F, Kraemer HC. Risk factors for childhood overweight: a prospective study from birth to 9.5 years. J Pediatr. 2004;145:20–5. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 112.Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP, Gillman MW. Short sleep duration in infancy and risk of childhood overweight. Arch Pediatr Adolesc Med. 2008;162:305–11. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Moore T, Ucko LE. Night waking in early infancy. Arch Dis Child. 1957;32:333–42. doi: 10.1136/adc.32.164.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Parmelee AH, Wenner WH, Schulz HR. Infant sleep patterns: From birth to 16 weeks of age. J Pediatr. 1964;65:576–82. doi: 10.1016/s0022-3476(64)80291-2. [DOI] [PubMed] [Google Scholar]
- 115.Anders TF, Keener M. Developmental course of nighttime sleep-wake patterns in full-term and premature infants during the first year of life. I. Sleep. 1985;8:173–92. doi: 10.1093/sleep/8.3.173. [DOI] [PubMed] [Google Scholar]
- 116.James-Roberts IS, Conroy S, Hurry J. Links between infant crying and sleep-waking at six weeks of age. Early Hum Dev. 1997;48:143–52. doi: 10.1016/s0378-3782(96)01845-2. [DOI] [PubMed] [Google Scholar]
- 117.Glotzbach SF, Edgar DM, Boeddiker M, Ariagno RL. Biological rhythmicity in normal infants during the first 3 months of life. Pediatrics. 1994;94:482–8. [PubMed] [Google Scholar]
- 118.St James-Roberts I, Alvarez M, Csipke E, Abramsky T, Goodwin J, Sorgenfrei E. Infant crying and sleeping in London, Copenhagen and when parents adopt a “proximal” form of care. Pediatrics. 2006;117:e1146–55. doi: 10.1542/peds.2005-2387. [DOI] [PubMed] [Google Scholar]
- 119.Anders TF. Night-waking in infants during the first year of life. Pediatrics. 1979;63:860–4. [PubMed] [Google Scholar]
- 120.Adair R, Bauchner H, Philipp B, Levenson S, Zuckerman B. Night waking during infancy: role of parental presence at bedtime. Pediatrics. 1991;87:500–4. [PubMed] [Google Scholar]
- 121.Touchette E, Petit D, Paquet J, et al. Factors associated with fragmented sleep at night across early childhood. Arch Pediatr Adolesc Med. 2005;159:242–9. doi: 10.1001/archpedi.159.3.242. [DOI] [PubMed] [Google Scholar]
- 122.Wolke D, Meyer R, Ohrt B, Riegel K. Co-morbidity of crying and feeding problems with sleeping problems during infancy: concurrent and predictive associations. Early Dev Parenting. 1995;4:191–208. [Google Scholar]
- 123.Jenni OG, Molinari L, Caflisch JA, Largo RH. Sleep duration from ages 1 to 10 years: variability and stability in comparison with growth. Pediatrics. 2007;120:e769–76. doi: 10.1542/peds.2006-3300. [DOI] [PubMed] [Google Scholar]
- 124.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 125.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.James RJ, Drewett RF, Cheetham TD. Low cord ghrelin levels in term infants are associated with slow weight gain over the first 3 months of life. J Clin Endocrinol Metab. 2004;89:3847–50. doi: 10.1210/jc.2003-032167. [DOI] [PubMed] [Google Scholar]
- 127.Bass J, Turek FW. Sleepless in America: A pathway to obesity and the metabolic syndrome? Arch Int Med. 2005;165:15–6. doi: 10.1001/archinte.165.1.15. [DOI] [PubMed] [Google Scholar]
- 128.Wright P, MacLeod HA, Cooper MJ. Waking at night: the effect of early feeding experience. Child Care Health Dev. 1983;9:309–19. doi: 10.1111/j.1365-2214.1983.tb00329.x. [DOI] [PubMed] [Google Scholar]
- 129.Elias MF, Nicolson NA, Bora C, Johnston J. Sleep/wake patterns of breast-fed infants in the first 2 years of life. Pediatrics. 1986;77:322–9. [PubMed] [Google Scholar]
- 130.Eaton-Evans J, Dugdale AE. Sleep patterns of infants in the first year of life. Arch Dis Child. 1988;63:647–9. doi: 10.1136/adc.63.6.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Scher A, Tirosh E, Jaffe M, Rubin L, Sadeh A, Lavie P. Sleep patterns of infants and young children in Israel. Int J Behavioral Development. 1995;18:701–11. [Google Scholar]
- 132.Horne RS, Parslow PM, Ferens D, Watts AM, Adamson TM. Comparison of evoked arousability in breast and formula fed infants. Arch Dis Child. 2004;89:22–5. [PMC free article] [PubMed] [Google Scholar]
- 133.Ball HL. Breastfeeding, bed-sharing, and infant sleep. Birth. 2003;30:181–8. doi: 10.1046/j.1523-536x.2003.00243.x. [DOI] [PubMed] [Google Scholar]
- 134.Pinilla T, Birch LL. Help me make it through the night: behavioral entrainment of breast-fed infants’ sleep patterns. Pediatrics. 1993;91:436–44. [PubMed] [Google Scholar]
- 135.Gerard CM, Harris KA, Thach BT. Spontaneous arousals in supine infants while swaddled and unswaddled during rapid eye movement and quiet sleep. Pediatrics. 2002;110:e70. doi: 10.1542/peds.110.6.e70. [DOI] [PubMed] [Google Scholar]
- 136.Franco P, Seret N, Van Hees JN, Scaillet S, Groswasser J, Kahn A. Influence of swaddling on sleep and arousal characteristics of healthy infants. Pediatrics. 2005;115:1307–11. doi: 10.1542/peds.2004-1460. [DOI] [PubMed] [Google Scholar]
- 137.Karp H. The happiest baby on the block. Bantam Books; New York, NY: 2002. [Google Scholar]
- 138.Karp H. The “fourth trimester”: A framework and strategy for understanding and resolving colic. Contemporary Pediatrics. 2004;21:94–116. [Google Scholar]
- 139.Kopp CB. Regulation of distress and negative emotions: A developmental review. Developmental Psychology. 1989;25:343–54. [Google Scholar]
- 140.Loeber R, Hay D. Key issues in the development of aggression and violence from childhood to early adulthood. Annu Rev Psychol. 1997;48:371–410. doi: 10.1146/annurev.psych.48.1.371. [DOI] [PubMed] [Google Scholar]
- 141.Carey W, Hegvik R, McDevitt S. Temperamental factors associated with rapid weight gain and obesity in middle childhood. Developmental and Behavioral Pediatrics. 1988;9:197–8. [PubMed] [Google Scholar]
- 142.Wells JC, Stanley M, Laidlaw AS, Day JM, Stafford M, Davies PS. Investigation of the relationship between infant temperament and later body composition. Int J Obes Relat Metab Disord. 1997;21:400–6. doi: 10.1038/sj.ijo.0800420. [DOI] [PubMed] [Google Scholar]
- 143.Pulkki-Raback L, Elovainio M, Kivimaki M, Raitakari OT, Keltikangas-Jarvinen L. Temperament in childhood predicts body mass in adulthood: the Cardiovascular Risk in Young Finns Study. Health Psychol. 2005;24:307–15. doi: 10.1037/0278-6133.24.3.307. [DOI] [PubMed] [Google Scholar]
- 144.Canetti L, Bachar E, Berry EM. Food and emotion. Behav Processes. 2002;60:157–64. doi: 10.1016/s0376-6357(02)00082-7. [DOI] [PubMed] [Google Scholar]
- 145.Pine DS, Cohen P, Brook J, Coplan JD. Psychiatric symptoms in adolescence as predictors of obesity in early adulthood: a longitudinal study. Am J Public Health. 1997;87:1303–10. doi: 10.2105/ajph.87.8.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kishi T, Elmquist JK. Body weight is regulated by the brain: a link between feeding and emotion. Mol Psychiatry. 2005;10:132–46. doi: 10.1038/sj.mp.4001638. [DOI] [PubMed] [Google Scholar]
- 147.Thompson RA. Emotion regulation: a theme in search of definition. Monogr Soc Res Child Dev. 1994;59:25–52. [PubMed] [Google Scholar]
- 148.Crockenberg S, Leerkes E. The family context of infant development. In: Zenah C, editor. Handbook of infant mental health. Guilford; New York: 1999. pp. 60–90. [Google Scholar]
- 149.Jahromi LB, Putnam SP, Stifter CA. Maternal regulation of infant reactivity from 2 to 6 months. Dev Psychol. 2004;40:477–87. doi: 10.1037/0012-1649.40.4.477. [DOI] [PubMed] [Google Scholar]
- 150.Crockenberg SC, Leerkes EM. Infant and maternal behaviors regulate infant reactivity to novelty at 6 months. Dev Psychol. 2004;40:1123–32. doi: 10.1037/0012-1649.40.6.1123. [DOI] [PubMed] [Google Scholar]
- 151.Baughcum AE, Powers SW, Johnson SB, et al. Maternal feeding practices and beliefs and their relationships to overweight in early childhood. J Dev Behav Pediatr. 2001;22:391–408. doi: 10.1097/00004703-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 152.Puhl RM, Schwartz MB. If you are good you can have a cookie: How memories of childhood food rules link to adult eating behaviors. Eat Behav. 2003;4:283–93. doi: 10.1016/S1471-0153(03)00024-2. [DOI] [PubMed] [Google Scholar]
- 153.van den Boom D. Behavioral management of early infant crying in irritable babies. In: Barr RG, St James-Roberts I, Keefe MR, Brody RI, editors. New evidence on unexplained infant crying: Its origins, nature, and management. Johnson & Johnson Pediatric Institute; New Brunswick, NJ: 2001. pp. 209–28. [Google Scholar]
- 154.Velderman MK, Bakermans-Kranenburg MJ, Juffer F, van IMH. Effects of attachment-based interventions on maternal sensitivity and infant attachment: differential susceptibility of highly reactive infants. J Fam Psychol. 2006;20:266–74. doi: 10.1037/0893-3200.20.2.266. [DOI] [PubMed] [Google Scholar]
- 155.Kleinman RE, editor. Pediatric Nutrition Handbook. American Academy of Pediatrics; 2004. Chapter 6: Complimentary feeding. [Google Scholar]
- 156.Gartner LM, Morton J, Lawrence RA, et al. Breastfeeding and the use of human milk. Pediatrics. 2005;115:496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- 157.Parents’ Survival Guide to Transitional Feeding. The Institute of Pediatric Nutrition; 2003. [Google Scholar]
- 158.US Department of Health and Human Services. National Center for Health Statistics. Third National Health and Nutrition Survey . NHANES III. Examination Data File: CD-ROM series 11 No 1A and No 2A. Hyattsville, MD: Apr, 1998. 1988-1994. Public Use Data File Documentation Number 76200; July 1997 and. respectively. [Google Scholar]
- 159.Kim J, Peterson KE. Association of infant child care with infant feeding practices and weight gain among US infants. Arch Pediatr Adolesc Med. 2008;162:627–33. doi: 10.1001/archpedi.162.7.627. [DOI] [PubMed] [Google Scholar]
- 160.Shelov SP, Hannemann RE, editors. Caring for your baby and young child: Birth to age 5. 4th ed Bantam Books; 2004. [Google Scholar]
- 161.Macknin ML, Medendorp SV, Maier MC. Infant sleep and bedtime cereal. Am J Dis Child. 1989;143:1066–8. doi: 10.1001/archpedi.1989.02150210100027. [DOI] [PubMed] [Google Scholar]
- 162.Shukla A, Forsyth HA, Anderson CM, Marwah SM. Infantile overnutrition in the first year of life: a field study in Dudley, Worcestershire. Br Med J. 1972;4:507–15. doi: 10.1136/bmj.4.5839.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Ferris AG, Laus MJ, Hosmer DW, Beal VA. The effect of diet on weight gain in infancy. Am J Clin Nutr. 1980;33:2635–42. doi: 10.1093/ajcn/33.12.2635. [DOI] [PubMed] [Google Scholar]
- 164.Kramer MS, Barr RG, Leduc DG, Boisjoly C, McVey-White L, Pless IB. Determinants of weight and adiposity in the first year of life. J Pediatr. 1985;106:10–4. doi: 10.1016/s0022-3476(85)80456-x. [DOI] [PubMed] [Google Scholar]
- 165.Ong KK, Emmett PM, Noble S, Ness A, Dunger DB. Dietary energy intake at the age of 4 months predicts postnatal weight gain and childhood body mass index. Pediatrics. 2006;117:e503–8. doi: 10.1542/peds.2005-1668. [DOI] [PubMed] [Google Scholar]
- 166.Baker JL, Michaelsen KF, Rasmussen KM, Sorensen TIA. Maternal prepregnant body mass index, duration of breastfeeding, and timing of complementary food introduction are associated with infant weight gain. Am J Clin Nutr. 2004;80:1579–88. doi: 10.1093/ajcn/80.6.1579. [DOI] [PubMed] [Google Scholar]
- 167.Birch LL. Development of food preferences. Annu Rev Nutr. 1999;19:41–62. doi: 10.1146/annurev.nutr.19.1.41. [DOI] [PubMed] [Google Scholar]
- 168.Sullivan SA, Birch LL. Infant dietary experience and acceptance of solid foods. Pediatrics. 1994;93:271–7. [PubMed] [Google Scholar]
- 169.Birch LL, Gunder L, Grimm-Thomas K, Laing DG. Infants’ consumption of a new food enhances acceptance of similar foods. Appetite. 1998;30:283–95. doi: 10.1006/appe.1997.0146. [DOI] [PubMed] [Google Scholar]
- 170.Birch LL, Marlin DW. I don’t like it; I never tried it: effects of exposure on two-year-old children’s food preferences. Appetite. 1982;3:353–60. doi: 10.1016/s0195-6663(82)80053-6. [DOI] [PubMed] [Google Scholar]
- 171.Birch LL, McPhee L, Shoba BC, Pirok E, Steinberg L. What kind of exposure reduces children’s food neophobia? Looking vs. tasting. Appetite. 1987;9:171–8. doi: 10.1016/s0195-6663(87)80011-9. [DOI] [PubMed] [Google Scholar]
- 172.Birch LL. Development of food acceptance patterns in the first years of life. Proc Nutr Soc. 1998;57:617–24. doi: 10.1079/pns19980090. [DOI] [PubMed] [Google Scholar]
- 173.Dietz WH, Franks AL, Marks JS. The obesity problem. N Engl J Med. 1998;338:1157. author reply 8. [PubMed] [Google Scholar]
- 174.Farrow C, Blissett J. Does maternal control during feeding moderate early infant weight gain? Pediatrics. 2006;118:e293–8. doi: 10.1542/peds.2005-2919. [DOI] [PubMed] [Google Scholar]
- 175.Farrow CV, Blissett J. Controlling feeding practices: cause or consequence of early child weight? Pediatrics. 2008;121:e164–9. doi: 10.1542/peds.2006-3437. [DOI] [PubMed] [Google Scholar]
- 176.Birch LL, McPhee L, Shoba BC, Steinberg L, Krehbiel R. “Clean up your plate”. Effects of child feeding practices on the conditioning of meal size. Learning and Motivation. 1987;18:301–17. [Google Scholar]
- 177.Galloway AT, Fiorito L, Lee Y, Birch LL. Parental pressure, dietary patterns, and weight status among girls who are “picky eaters”. J Am Diet Assoc. 2005;105:541–8. doi: 10.1016/j.jada.2005.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Galloway AT, Fiorito LM, Francis LA, Birch LL. ‘Finish your soup’: counterproductive effects of pressuring children to eat on intake and affect. Appetite. 2006;46:318–23. doi: 10.1016/j.appet.2006.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act. 2008;5:15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Gidding SS, Dennison BA, Birch LL, et al. Dietary recommendations for children and adolescents: a guide for practitioners. Pediatrics. 2006;117:544–59. doi: 10.1542/peds.2005-2374. [DOI] [PubMed] [Google Scholar]
- 181.Green M, editor. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. National Center for Education in Maternal and Child Health; Arlinton, VA: 1994. [Google Scholar]
- 182.Dietz WH, Stern L, editors. American Academy of Pediatrics: Guide to Your Child’s Nutrition. Villard; New York: 1999. [Google Scholar]
- 183.Kleinman RE, editor. Pediatric Nutrition Handbook. 5th edition American Academy of Pediatrics; 2004. [Google Scholar]
- 184.American Academy of Pediatrics. Committee on Nutrition Cholesterol in childhood. Pediatrics. 1998;101:141–7. [PubMed] [Google Scholar]
- 185.Birch LL. Children’s preferences for high-fat foods. Nutr Rev. 1992;50:249–55. doi: 10.1111/j.1753-4887.1992.tb01341.x. [DOI] [PubMed] [Google Scholar]
- 186.Fox MK, Reidy K, Novak T, Ziegler P. Sources of energy and nutrients in the diets of infants and toddlers. J Am Diet Assoc. 2006;106:S28–42. doi: 10.1016/j.jada.2005.09.034. [DOI] [PubMed] [Google Scholar]
- 187.Dennison BA, Erb TA, Jenkins PL. Predictors of dietary milk fat intake by preschool children. Prev Med. 2001;33:536–42. doi: 10.1006/pmed.2001.0939. [DOI] [PubMed] [Google Scholar]
- 188.Kranz S, Lin PJ, Wagstaff DA. Children’s dairy intake in the United States: too little, too fat? J Pediatr. 2007;151:642–6. 6 e1–2. doi: 10.1016/j.jpeds.2007.04.067. [DOI] [PubMed] [Google Scholar]
- 189.Basch CE, Shea S, Zybert P. Food sources, dietary behavior, and the saturated fat intake of Latino children. Am J Public Health. 1992;82:810–5. doi: 10.2105/ajph.82.6.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Sigman-Grant M, Zimmerman S, Kris-Etherton PM. Dietary approaches for reducing fat intake of preschool-age children. Pediatrics. 1993;91:955–60. [PubMed] [Google Scholar]
- 191.Dixon LB, McKenzie J, Shannon BM, Mitchell DC, Smiciklas-Wright H, Tershakovec AM. The effect of changes in dietary fat on the food group and nutrient intake of 4- to 10-year-old children. Pediatrics. 1997;100:863–72. doi: 10.1542/peds.100.5.863. [DOI] [PubMed] [Google Scholar]
- 192.Friedman G, Goldberg SJ. An evaluation of the safety of a low-saturated-fat, low-cholesterol diet beginning in infancy. Pediatrics. 1976;58:655–7. [PubMed] [Google Scholar]
- 193.Niinikoski H, Viikari J, Ronnemaa T, et al. Regulation of growth of 7- to 36-month-old children by energy and fat intake in the prospective, randomized STRIP baby trial. Pediatrics. 1997;100:810–6. doi: 10.1542/peds.100.5.810. [DOI] [PubMed] [Google Scholar]
- 194.Lagstrom H, Seppanen R, Jokinen E, et al. Influence of dietary fat on the nutrient intake and growth of children from 1 to 5 y of age: the Special Turku Coronary Risk Factor Intervention Project. Am J Clin Nutr. 1999;69:516–23. doi: 10.1093/ajcn/69.3.516. [DOI] [PubMed] [Google Scholar]
- 195.Karaolis-Danckert N, Gunther AL, Kroke A, Hornberg C, Buyken AE. How early dietary factors modify the effect of rapid weight gain in infancy on subsequent body-composition development in term children whose birth weight was appropriate for gestational age. Am J Clin Nutr. 2007;86:1700–8. doi: 10.1093/ajcn/86.5.1700. [DOI] [PubMed] [Google Scholar]
- 196.Fox MK, Pac S, Devaney B, Jankowski L. Feeding infants and toddlers study: What foods are infants and toddlers eating? J Am Diet Assoc. 2004;104:s22–30. doi: 10.1016/j.jada.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 197.Daniels SR, Greer FR. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122:198–208. doi: 10.1542/peds.2008-1349. [DOI] [PubMed] [Google Scholar]
- 198.Berkey CS, Rockett HR, Willett WC, Colditz GA. Milk, dairy fat, dietary calcium, and weight gain: a longitudinal study of adolescents. Arch Pediatr Adolesc Med. 2005;159:543–50. doi: 10.1001/archpedi.159.6.543. [DOI] [PubMed] [Google Scholar]
- 199. [Accessed February 7, 2008];USDA National Nutrient Database for Standard Reference. at http://www.nal.usda.gov/fnic/foodcomp/cgi-bin/nut_search_new.pl.
- 200.Nielsen SJ, Popkin BM. Changes in beverage intake between 1977 and 2001. Am J Prev Med. 2004;27:205–10. doi: 10.1016/j.amepre.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 201.O’Connor TM, Yang SJ, Nicklas TA. Beverage intake among preschool children and its effect on weight status. Pediatrics. 2006;118:e1010–8. doi: 10.1542/peds.2005-2348. [DOI] [PubMed] [Google Scholar]
- 202.American Dietetic Association [Accessed February 15, 2007];Childhood overweight evidence analysis project: Factors associated with overweight. at http://www.adaevidencelibrary.com/topic.cfm?cat=2792.
- 203.Skinner JD, Ziegler P, Ponza M. Transitions in infants’ and toddlers’ beverage patterns. J Am Diet Assoc. 2004;104:s45–50. doi: 10.1016/j.jada.2003.10.027. [DOI] [PubMed] [Google Scholar]
- 204.American Academy of Pediatrics: The use and misuse of fruit juice in pediatrics. Pediatrics. 2001;107:1210–3. doi: 10.1542/peds.107.5.1210. [DOI] [PubMed] [Google Scholar]
- 205.Welsh JA, Cogswell ME, Rogers S, Rockett H, Mei Z, Grummer-Strawn LM. Overweight among low-income preschool children associated with the consumption of sweet drinks: Missouri, 1999-2002. Pediatrics. 2005;115:e223–9. doi: 10.1542/peds.2004-1148. [DOI] [PubMed] [Google Scholar]
- 206.Warner ML, Harley K, Bradman A, Vargas G, Eskenazi B. Soda consumption and overweight status of 2-year-old mexican-american children in california. Obesity (Silver Spring) 2006;14:1966–74. doi: 10.1038/oby.2006.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Murray R, Frankowski B, Taras H. Are soft drinks a scapegoat for childhood obesity? J Pediatr. 2005;146:586–90. doi: 10.1016/j.jpeds.2004.12.018. [DOI] [PubMed] [Google Scholar]
- 208.James J, Kerr D. Prevention of childhood obesity by reducing soft drinks. Int J Obes (Lond) 2005;29(Suppl 2):S54–7. doi: 10.1038/sj.ijo.0803062. [DOI] [PubMed] [Google Scholar]
- 209.Devaney B, Ziegler P, Pac S, Karwe V, Barr SI. Nutrient intakes of infants and toddlers. J Am Diet Assoc. 2004;104:s14–21. doi: 10.1016/j.jada.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 210.Picciano MF, Smiciklas-Wright H, Birch LL, Mitchell DC, Murray-Kolb L, McConahy KL. Nutritional guidance is needed during dietary transition in early childhood. Pediatrics. 2000;106:109–14. doi: 10.1542/peds.106.1.109. [DOI] [PubMed] [Google Scholar]
- 211.Butte N, Cobb K, Dwyer J, Graney L, Heird W, Rickard K. The Start Healthy Feeding Guidelines for Infants and Toddlers. J Am Diet Assoc. 2004;104:442–54. doi: 10.1016/j.jada.2004.01.027. [DOI] [PubMed] [Google Scholar]
- 212.Ryan C, Dwyer J. The toddler’s smorgasbord. Nutrition Today. 2003;38:164–9. [Google Scholar]
- 213.McConahy KL, Picciano MF. How to grow a healthy toddler - 12 to 24 months. Nutrition Today. 2003;38:156–63. [Google Scholar]
- 214.National Association for Sport and Physical Education . Active start: A statement of physical activity guidelines for children birth to five years. AAHPERD Publications; New York: 2002. [Google Scholar]
- 215.Corbin C, Pangrazi R, Beighle A, Le Masurier G, Morgan C, Council for Physical Education for Children (COPEC) of the National Association for Sport and Physical Education. an Association of the American Alliance for Health Physical Education and Recreation . Guidelines for appropriate physical activity for elementary school children 2003 update. A position statement. AAHPERD Publications; New York: 2003. [Google Scholar]
- 216.Gunner KB, Atkinson PM, Nichols J, Eissa MA. Health promotion strategies to encourage physical activity in infants, toddlers, and preschoolers. J Pediatr Health Care. 2005;19:253–8. doi: 10.1016/j.pedhc.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 217.Dennison BA, Boyer PS. Risk evaluation in pediatric practice aids in prevention of childhood overweight. Pediatr Ann. 2004;33:25–30. doi: 10.3928/0090-4481-20040101-09. [DOI] [PubMed] [Google Scholar]
- 218.Neumark-Sztainer D. Childhood and adolescent obesity: An ecological perspective. Basic Pediatrics. 2003;101:12–20. [Google Scholar]
- 219.Dennison BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109:1028–35. doi: 10.1542/peds.109.6.1028. [DOI] [PubMed] [Google Scholar]
- 220.Campbell K, Hesketh K, Crawford D, Salmon J, Ball K, McCallum Z. The Infant Feeding Activity and Nutrition Trial (INFANT) an early intervention to prevent childhood obesity: cluster-randomised controlled trial. BMC Public Health. 2008;8:103. doi: 10.1186/1471-2458-8-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Wolman J, Skelly E, Kolotourou M, Lawson M, Sacher P. Tackling toddler obesity through a pilot community-based family intervention. Community Pract. 2008;81:28–31. [PubMed] [Google Scholar]
- 222.American Academy of Pediatrics: Children, adolescents, and television. Pediatrics. 2001;107:423–6. doi: 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]


