Abstract
Injury is a major global disease burden for the twenty-first century. There are, however, few studies of unintentional household injury in Asian urban settings where living environments are characterized by extremely compact, high-living-density, multistory apartments. This study investigated the association between nonfatal unintentional household injuries with the resident’s sociodemographic attributes and household characteristics in Hong Kong, the city with the world’s highest population density. A cross-sectional retrospective recall study was conducted in May 2007 using a random telephone survey with a modified Chinese version of the World Health Organization Injury and Violence instrument. The study sample included 1,001 noninstitutionalized Cantonese-speaking Hong Kong residents of all ages, including foreign live-in domestic helpers. Multivariate regression was conducted to identify risk factors for nonfatal unintentional injuries in Hong Kong. Among a predominantly adult sample, household size and time spent at home were not associated with nonfatal unintentional household injuries in the general population in Hong Kong. The multivariate analyses indicated that female gender, owners of private homes, lower square footage of living space per person, and those with slip prevention devices in the bathroom were significantly associated with household injuries. Injured and noninjured groups were found to have adopted different injury prevention strategies toward household injuries. The results identified potential target groups for household injury prevention programs.
Keywords: Nonfatal unintentional household injury, Urban health, Living density, Environmental risk factors, Home injury, Socioeconomic risk factors, Accidents, Asia, China
Introduction
The Global Burden of Disease Study reports that 10% of global mortality is due to injuries1 and unintentional injuries, representing the leading cause of death among young people in developed countries in the West2 and Asia.3–6 Research has indicated that at least 41% of these injuries required medical attention.7 In addition to the direct medical cost, nonfatal unintentional injuries also incur a large economic burden for the population at large due to lost work days,8,9 insurance costs for extended disability,8 absences from school for children,3,10–12 and high emotional burden for caregivers of those with severe or long-term injuries.13
Past research has shown that individual-level risk factors for unintentional injuries include very young and very old age,3,10,14–17 gender,18,19 marital status,19 lower socioeconomic status (SES),2,20 lower educational attainment,14,17 unemployment status,17 parental behavioral factors such as alcohol use,21 sleep patterns,14 inappropriate safety equipment use,22,23 and risk perceptions.24 Housing-related factors such as dimness, clutter, and structural disrepair14,25 as well as neighborhood characteristics such as SES indices26 and rural location19 have also been linked to higher past-year injury rates. Epidemiological data of unintentional household injury in Asia urban metropolitan areas such as Hong Kong, characterized by high-rise building, high density living, are nevertheless limited.27 The majority of population-based household injury studies have been conducted in industrialized countries in the West, where populations typically reside in suburban single-family houses or among slum-dwelling populations in developing countries18 or in agrarian populations.19 Moreover, previous studies in Asian urban settings have either focused upon specific population groups such as children3–5,28–30 or specific injury topics such as falls in the elderly or burn patients in the emergency wards.18,31 There is a dearth of population-based data for investigating the association between the sociodemographic and environmental factors with unintentional injuries in urban households of a densely populated industrialized area. A previously conducted study limited to Hong Kong children under the age of 16 revealed that male gender was a significant predictor of nonfatal injury among children,5 yet it was unclear whether living density and duration of time spent at home were significant predictors for such injuries. A recently conducted survey of nonfatal household injuries among the general population of Hong Kong revealed that in the 12 months preceding the survey 40.2% of respondents reported an unintentional household injury and 30.9% reported more than one episode with contusions/crushing injuries (60.4%), open wounds (20.4%), and burns/scalding injuries (12.9%). These were the three most commonly reported injuries.27 The vast majority of respondents with injuries (90.3%) did not seek postinjury treatment from any kind of health professional.27
Using the same dataset as the above-mentioned study, this investigation examined the patterns of unintentional household injury by investigating whether the predisposing living characteristics such as living density, housing type, size of living quarters, and amount of time at home are be associated with nonfatal unintentional household injuries for the general population. The results will provide evidence to assist public health planners in tailoring appropriate injury prevention programs for urban residents.
Methods
An anonymous, population-based, cross-sectional telephone survey was undertaken in May 2007, using a structured questionnaire to examine the past-year incidence of nonfatal unintentional household injury in the general population in Hong Kong, as well as the characteristics of risk factors for such injuries.
Data Collection and Instrument
A modified Chinese questionnaire based on the World Health Organization’s Guidelines for Conducting Community Surveys on Injuries and Violence32 was used for data collection. The questionnaire was translated into Cantonese(the local dialect in Hong Kong) and questions in the original version that did not apply to urban living were deleted in the final modified questionnaire. A pilot study was conducted to verify the instrument’s reliability. The questionnaire had a high 1-week test–retest reliability coefficient of K coefficient >0.89. Nonfatal unintentional household injuries were defined as those injuries occurring within the confines of home, including all common areas of the residence (such as exercise rooms, stairwells, car parks, and common entry ways).27 This study excluded any intentional injuries such as interpersonal violence, domestic abuse, child abuse, self-inflicted harm, or crime.
The telephone survey sampling methodology was published in detail elsewhere.27 In summary, random telephone numbers were selected from an up-to-date telephone directory. Telephone calls were made by trained interviewers from 6:30 p.m. to 10:00 p.m. to avoid overrepresentation of unemployed persons. Respondents were selected by asking a Cantonese-speaking household member (which included live-in Cantonese-speaking domestic helper), whose birthday was closest to the date of the interview to participate for each telephone interview. Parental consent was obtained for respondents under 18. For respondents who were younger than 15 years old or those with difficulties in communicating (e.g., mentally handicapped individuals), proxy responses from a family member of the chosen respondents were accepted. When necessary, the interviewer would consult another family member to clarify answers from the initial respondent such as information about health service costs for injuries. Each interview took approximately 10 to 15 min to complete. For unanswered calls, at least three other independent calls were made, before considering the numbers to be unanswered. The number of residents in the contacted households, whether able or unable to be interviewed, was recorded.
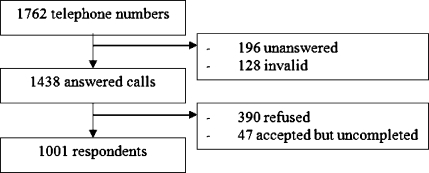
The anonymity and confidentiality of responses were ensured; an enquiry hotline telephone number was provided and maintained during the research operation to handle enquiries regarding the survey and other issues related to the study (e.g., verification of identity of the interviewer or making an appointment for the interview). All telephone interviewers were trained to conduct the interviews in Cantonese. Verbal informed consent was obtained from the respondents, and ethics approval was obtained from the Ethics Committee of the Chinese University of Hong Kong. A total of 1,762 telephone numbers were dialed with 196 unanswered and 128 invalid. Among the 1,438 answered calls, 390 refused, 47 accepted but did not complete the interviews, and 1,001 respondents completed the interviews. The final survey response rate according to answered calls was 69.5%. Figure 1 shows the study design algorithm.
FIGURE 1.
Logarithm of the data collection process for the telephone survey conducted on May 2007.
Variables
Outcome Variables Unintentional household injury was defined by injuries that occurred within the residence and were sustained in the past 12 months. The incident might or might not have modified daily activity or required medical attention. Respondents with any of the seven major categories of injuries were asked about the details of the injury. Injuries were classified into seven major categories (Table 1): (a) sprain and strain, (b) fracture, (c) cuts and puncture wounds, (d) caustic and poisoning, (e) contusion and crushing (including falls), (f) burns, and (g) all other injuries (includes rare injuries such as electrocutions and animal bites). Information of the potential risk factors associated with the household was collected. These included sociodemographic and background data (age, gender, education, family income, occupation and employment status, and medical insurance coverage), general living arrangements (i.e., size of living area, housing type (public, subsidized, private, rental quarters)), average hours spent at home (per day), living density (square feet per person), residential characteristics specific to Hong Kong (i.e., type of floor materials which include plastic, wood, marble, brick, rug/carpeted, and cemented tiles), presence of stairs at home, the presence of bunk beds, presence of window sills), individual household characteristics (regular presence of sundries on the floor that may impede traffic, presence of exercise equipments at home, whether the household required repair or maintenances), use of injury prevention equipment (such as bathroom slip prevention tools), and the availability of self-treatment device at home (unlocked medical box and first aid kits). The instrument also asked about potential personal risk factors for injuries (use of eye glasses, mobility problems), chronic diseases, self-reported chronic medication, and regular alcohol use. The study instrument also collected the information on the health-seeking behavior for injuries but these data will be reported elsewhere.
Table 1.
Seven major categories of injury examined in this study
| Main categories of unintentional injuries |
|---|
| Sprain and strain |
| Fractures |
| Cuts and puncture wounds |
| Caustic and poisoning injuries |
| Contusion and crushing injuries (including falls) |
| Burns and scalding injuries |
| All other injuries (includes rare injuries such as electrocutions and animal bites) |
Statistical Analysis
Descriptive statistics, stratified by age and gender, were reported on past-year episode-based incidence of various types of injury. Univariate logistic analysis was first conducted, using the most recent household injury episode as the outcome variable, to identify significant associations with socioeconomic factors, living characteristics, underlying risk factors, and preventive measures taken at home. A stepwise multivariable logistic regression was then conducted on variables with at least marginal statistical association in the univariate analysis (p < 0.20) in order to determine the independent associations with household injuries. Further subgroup analyses were also performed on the most prevalent subtypes of nonfatal household injuries and the injury prevention methods adopted by respondents. All statistical analyses were conducted using SPSS for Windows version 14.0. (SPSS, 2006). Statistical significance was set at α = 0.05.
Results
The details of our study respondents27 were generally comparable to the Hong Kong 2006 population census.33 When comparing the injured and noninjured respondents, significant differences were found for gender (p < 0.001), age (p = 0.003), family income (p = 0.025), insurance type (p = 0.007), and number of family members living within the same household (p = 0.037) and having taken precaution, meaning that the respondents have utilized safety prevention equipments in household (as shown as the list of prevention methods in Table 3) to prevent household injuries (p < 0.001). No differences were found for living characteristics such as living density, living area, and housing types. Table 2 shows the comparison of sociodemographic characteristics among injured and noninjured study sample as well as the general population.
Table 3.
Univariate and multivariate analyses of risk factors associated with all types of nonfatal unintentional household injury
| Variables | ORunadj | 95% CI | p value | ORMV | 95% CI | p value |
|---|---|---|---|---|---|---|
| Gender | <0.001a | |||||
| Male (reference) | 1 | – | – | 1.00 | – | – |
| Female | 2.26 | (1.74–2.93) | <0.001a | 3.10 | 1.99–4.84 | <0.001a |
| Age | 0.001a | |||||
| 0–19 (reference) | 1 | – | – | NS | NS | NS |
| 20–39 | 0.98 | (0.68–1.42) | 0.93 | NS | NS | NS |
| 40–59 | 0.77 | (0.53–1.11) | 1.67 | NS | NS | NS |
| ≥60 | 0.46 | (0.29–0.71) | 0.001a | NS | NS | NS |
| Education level | 0.13 | |||||
| Primary or less (reference) | 1 | – | – | NS | NS | NS |
| Form 1 to 5 | 1.18 | (0.85–1.65) | 0.31 | NS | NS | NS |
| Form 6 to higher diploma | 1.47 | (0.91–2.36) | 0.12 | NS | NS | NS |
| Degree or above | 1.55 | (1.04–2.31) | 0.03 | NS | NS | NS |
| Family income | 0.58 | |||||
| <10,000 (reference) | 1 | – | – | – | – | – |
| 10,000–19,999 | 0.87 | (0.62–1.22) | 0.42 | – | – | – |
| 20,000–29,999 | 1.26 | (0.74–2.14) | 0.39 | – | – | – |
| ≥30,000 | 1.15 | (0.68–1.94) | 0.61 | – | – | – |
| Occupation | 0.05 | |||||
| Managers and administrators (reference) | 1 | – | – | NS | NS | NS |
| Professionals | 0.9 | (0.34–2.42) | 0.84 | NS | NS | NS |
| Associate professionals | 1.22 | (0.45–3.26) | 0.7 | NS | NS | NS |
| Clerks | 1.53 | (0.61–3.83) | 0.37 | NS | NS | NS |
| Service workers and shop sales workers | 1.25 | (0.48–3.25) | 0.64 | NS | NS | NS |
| Craft and related workers | 0.42 | (0.14–1.25) | 0.12 | NS | NS | NS |
| Plant and machine operators and assemblers | 0.68 | (0.23–2.05) | 0.5 | NS | NS | NS |
| Elementary occupations | 0.78 | (0.23–2.67) | 0.69 | NS | NS | NS |
| Unemployed | 0.56 | (0.15–2.08) | 0.38 | NS | NS | NS |
| Living size | 0.24 | |||||
| <400 ft2 (reference) | 1 | – | – | – | – | – |
| 400–599 ft2 | 1.18 | (0.78–1.78) | 0.44 | – | – | – |
| 600–799 ft2 | 1.33 | (0.85–2.07) | 0.21 | – | – | – |
| 800–999 ft2 | 1.69 | (1.00–2.84) | 0.49 | – | – | – |
| ≥1,000 ft2 | 1.15 | (0.67–1.00) | 0.61 | – | – | – |
| Housing type | 0.06 | |||||
| Public housing (reference) | 1 | – | – | 1.00 | – | – |
| Subsidized sales flat | 1.13 | (0.76–1.68) | 0.55 | 0.81 | 0.38–1.72 | 0.59 |
| Private flat and house | 1.46 | (1.10–1.95) | 0.01 | 2.26 | 1.27–4.03 | 0.01 |
| Rental/quarters | 0.79 | (0.20–3.13) | 0.74 | 0.30 | 0.03–2.83 | 0.30 |
| Time spent at home | 0.04 | |||||
| <6 h/day (reference) | 1 | – | – | NS | NS | NS |
| 7–12 h/day | 1.67 | (0.77–3.61) | 0.2 | NS | NS | NS |
| 13–24 h/day | 1.22 | (0.56–2.65) | 0.61 | NS | NS | NS |
| Living densitya | 0.51 | |||||
| 0–99 ft2 per person (reference) | 1 | – | – | 1.00 | – | – |
| 100–499 ft2 per person | 0.77 | (0.48–1.23) | 0.28 | 0.22 | 0.09–0.54 | <0.00a |
| ≥500 ft2 per person | 0.91 | (0.40–2.06) | 0.81 | 0.20 | 0.05–0.82 | 0.03 |
| Type of floor | 0.17 | |||||
| Plastics (reference) | 1 | – | – | NS | NS | NS |
| Wood | 1.46 | (0.91–2.36) | 0.12 | NS | NS | NS |
| Marble/brick/cement | 1.11 | (0.7–1.77) | 0.66 | NS | NS | NS |
| Rug/carpeted | 1.81 | (0.11–29.96) | 0.68 | NS | NS | NS |
| Stairs at home | 0.33 | |||||
| None (reference) | 1 | – | – | – | – | – |
| Yes | 1.21 | (0.83–1.78) | 0.33 | – | – | – |
| Have windowsill | 0.07 | |||||
| None (reference) | 1 | – | – | NS | NS | NS |
| Yes | 1.27 | (0.98–1.64) | 0.07 | NS | NS | NS |
| Bunk bed | 0.05 | |||||
| None (reference) | 1 | – | – | NS | NS | NS |
| Yes | 1.3 | (1.0–1.67) | 0.05 | NS | NS | NS |
| Misplaced objects or obstacles on the floor | 0.08 | |||||
| None (reference) | 1 | – | – | NS | NS | NS |
| Yes | 1.27 | (0.97–1.65) | 0.08 | NS | NS | NS |
| Exercise equipment at home | 0.01 | |||||
| None (reference) | 1 | – | – | NS | NS | NS |
| Yes | 1.69 | (1.16–2.48) | 0.01 | NS | NS | NS |
| Household need further maintenance | 0.84 | |||||
| None (reference) | 1 | – | – | – | – | – |
| Yes | 0.96 | (0.63–1.46) | 0.84 | – | – | – |
| Eye glasses | 0.24 | |||||
| Normal vision (reference) | 1 | – | – | – | – | – |
| Need eyeglasses, have worn eyeglasses | 0.93 | (0.72–1.21) | 0.61 | – | – | – |
| Need eyeglass, but did not wear eyeglasses | 0.6 | (0.33–1.08) | 0.09 | – | – | – |
| Mobility problem | 0.1 | |||||
| None (reference) | 1 | – | – | NS | NS | NS |
| Yes | 0.53 | (0.24–1.14) | 0.1 | NS | NS | NS |
| Chronic disease | 0.93 | |||||
| None (reference) | 1 | – | – | – | – | – |
| Yes | 0.98 | (0.69–1.41) | 0.93 | – | – | – |
| Chronic use of medication | 0.72 | |||||
| None (reference) | 1 | – | – | – | – | – |
| Yes | 0.94 | (0.66–1.34) | 0.72 | – | – | – |
| Installation of slip prevention devices in bathroom | <0.001a | |||||
| None (reference) | 1 | – | – | 1.00 | – | – |
| Yes | 1.81 | (1.40–2.35) | <0.001a | 1.93 | 1.23–3.01 | <0.001 |
Remarks:
ORMV odds ratio of multivariate analysis (nonsignificant refers to p > 0.05 and those nonsignificant variables during univariate analysis were not include for the multivariate analysis and thus were denoted as –)
aLiving density = living area (square feet)/number of household members, MV: used p < 0.2 as candidate variable for MU regression analyses
Table 2.
A comparison of sociodemographic characteristics among sample population (injured and noninjured) and general population in Hong Kong
| Demographic characteristics of the study population (as percentage of respondents) | |||||
|---|---|---|---|---|---|
| Noninjured % (N = 599) | Injured % (N = 402) | p value noninjured vs. injureda | All% (N = 1,001) | Hong Kong 2006 population census | |
| Gender | N = 599 | N = 402 | N = 1,001 | ||
| Male | 55.8 | 35.8 | <0.001** | 47.8 | 47.7 |
| Female | 44.2 | 64.2 | 52.2 | 52.3 | |
| Age | N = 599 | N = 402 | N = 1,001 | ||
| 0–14 | 7.2 | 10 | 0.003** | 8.3 | 13.7 |
| 15–24 | 16.4 | 20.4 | 18 | 13.2 | |
| 25–34 | 13.7 | 16.4 | 14.8 | 15.3 | |
| 35–44 | 20.7 | 19.9 | 20.4 | 18.2 | |
| 45–54 | 16.2 | 15.9 | 16.1 | 17.4 | |
| 55–64 | 10.2 | 10.2 | 10.2 | 9.7 | |
| 65+ | 15.7 | 7.2 | 12.3 | 12.4 | |
| Education | N = 594 | N = 400 | N = 994 | ||
| None | 6.2 | 3.2 | 0.257 | 5 | 7.1 |
| Primary | 18 | 16.5 | 17.4 | 18.3 | |
| Form 3 level | 18 | 18.8 | 18.3 | 19 | |
| Form 5 level | 31.5 | 29 | 30.5 | 32.6 | |
| Form 6 to form 7 | 5.1 | 6 | 5.4 | 5.9 | |
| Diploma and higher diploma | 4.3 | 5.3 | 4.7 | 7.6 | |
| University or above | 16.8 | 21.4 | 18.6 | 15.4 | |
| Occupation | N = 268 | N = 174 | N = 442 | ||
| Managers and administrators | 5.2 | 5.1 | 0.053 | 5.2 | 10.8 |
| Professionals | 14.2 | 12.6 | 13.6 | 6.1 | |
| Associate professionals | 11.9 | 14.4 | 12.9 | 16.1 | |
| Clerks | 19.8 | 29.9 | 23.8 | 16.9 | |
| Service workers and shop sales workers | 15.3 | 19 | 16.7 | 16.4 | |
| Craft and related workers | 13.8 | 5.7 | 10.6 | 8.5 | |
| Plant and machine operators and assemblers | 9.3 | 6.3 | 8.1 | 6.2 | |
| Elementary occupations | 5.2 | 4 | 4.8 | 18.8 | |
| Unemployed | 5.2 | 2.9 | 4.3 | NA | |
| Family income | N = 421 | N = 280 | N = 701 | ||
| <5,000 | 13.5 | 6.7 | 0.025* | 10.8 | 12 |
| 5,000–9,999 | 8.8 | 10 | 9.3 | 15.9 | |
| 10,000–19,999 | 29 | 27.1 | 28.2 | 27.8 | |
| 20,000–29,999 | 20 | 17.1 | 18.8 | 17.4 | |
| 30,000–39,999 | 12.6 | 15 | 13.6 | 9.9 | |
| ≥40,000 | 16.2 | 23.9 | 19.3 | 17 | |
| Average hours of staying at home everyday | N = 588 | N = 396 | N = 984 | ||
| 1–6 h | 3.5 | 2.5 | 0.087 | 3.1 | NA |
| 7–12 h | 45.9 | 53 | 48.8 | ||
| 13–18 h | 31.4 | 30.1 | 30.9 | ||
| 19–24 h | 19.2 | 14.4 | 17.3 | ||
| Insurance typeb (not mutually exclusive) | N = 655 | N = 436 | N = 1,091 | ||
| None | 34.96 | 29.82 | 0.007* | 32.91 | NA |
| Personal/private | 45.95 | 54.13 | 49.22 | ||
| Employment related | 18.63 | 14.68 | 17.05 | ||
| Household | 0.46 | 1.38 | 0.82 | ||
| Housing type | N = 593 | N = 396 | N = 989 | ||
| Public estate | 35.6 | 28.8 | 0.057 | 32.9 | 31 |
| Subsidized sale flat | 16 | 14.6 | 15.5 | 17.8 | |
| Private flat and housing | 47.2 | 55.8 | 50.7 | 49.3 | |
| Rental and Quarters | 1.2 | 0.8 | 1 | 1.9 | |
| Size of living area (ft2) | N = 594 | N = 401 | N = 995 | ||
| <400 | 15.7 | 12.2 | 0.236 | 14.3 | NA |
| 400–599 | 32.8 | 30.2 | 31.8 | ||
| 600–799 | 20.7 | 21.4 | 21 | ||
| 800–999 | 9.1 | 12 | 10.3 | ||
| ≥1,000 | 9.4 | 8.5 | 9 | ||
| Unknown | 12.3 | 15.7 | 13.7 | ||
| Number of family members at the household | N = 596 | N = 399 | N = 995 | ||
| Living alone | 6 | 4 | 0.037* | 5.2 | NA |
| 2 to 3 members | 43.5 | 36.8 | 40.8 | ||
| 4 to 5 members | 45.1 | 54.1 | 48.7 | ||
| ≥6 | 5.4 | 5 | 5.2 | ||
| Living densityc | N = 520 | N = 336 | N = 856 | ||
| 0–99 ft2 per person | 8.3 | 10.4 | 0.512 | 9.1 | NA |
| 100–499 ft2 per person | 88.1 | 85.4 | 87 | ||
| ≥500 ft2 per person | 3.7 | 4.2 | 3.9 | ||
| Taken any precaution to prevent the household injuryd | N = 584 | N = 399 | <0.001** | N = 983 | |
| No, prevention | 79.6 | 69.4 | 69.4 | NA | |
| Yes, prevention | 20.4 | 30.6 | 30.6 | ||
Hong Kong 2006 Population Census data; # may not add up to 100% due to missing data
aUnivariate analysis p value
bMore than one type of insurance allowed per respondent
cLiving density = living area (square feet)/# household member
dAmong the respondents, 241 numbers of respondents had adopted some preventive strategy to prevent injury. Seventeen persons responded do not know and one refused to respond
Factors in Association with Unintentional Household Injury
The univariate and multivariable analyses of the factors significantly associated with unintentional household injury are shown in Table 3. The unadjusted analyses indicated that female gender (odds ratio (OR) = 2.26, 95% confidence interval (CI) 1.74–2.93, p < 0.001) was associated with a higher likelihood of injury while age 60 or over (OR = 0.46, 95% CI 0.29–0.71, p < 0.001) was associated with lower likelihood of injury. Educational attainment of a college degree or above (OR = 1.55, 95% CI 1.04–2.31, p = 0.03), residing in private housing (OR = 1.46, 95% CI: 1.10–1.95, p = 0.01), and having a bunk bed (OR = 1.30, 95% CI 1.01–1.67, p = 0.05) and exercise equipment at home (OR = 1.69, 95% CI 1.16–2.48, p = 0.007) were significantly associated with injury in the unadjusted analyses. On the other hand, living arrangements such as size of living area, income, and time spent at home per day were found to be nonsignificant risk factors towards sustaining unintentional household injuries. Of note, the installation of slip prevention devices in the bathroom (OR = 1.81, 95% CI 1.40–2.35, p < 0.001) was also significantly associated with a greater likelihood of injury in the univariate analysis.
Variables (with p < 0.2 in the univariate analyses) used in the multivariate analysis included: gender, age, education level, occupation, housing type, time spent at home, floor types, having a window sill, bunk bed, misplaced objects or obstacles on the floor, exercise equipment at home, mobility problem, and installation of slip prevention devices in bathroom. Multivariate analysis results indicated that only female gender (ORMV = 3.10, 95% CI 1.99–4.84, p < 0.001), living in private flat/house (ORMV = 2.26, 95% CI 1.27–4.03, p = 0.01), and installation of slip prevention devices in bathroom (ORMV = 1.93, 95% CI 1.23–3.01, p ≤ 0.001) remained significantly associated with a higher likelihood of nonfatal unintentional household injuries whereas having greater square footage of living space per resident(ORMV = 0.20, 95% CI 0.05–0.82, p = 0.03) was negatively associated with risk of past-year injury. This may imply lower living density may be protective of incurring household injury.
Tables 4 and 5 compared the pattern difference of injury precautions taken between the injured and noninjured groups. Overall, 24.5% (n = 241) of respondents had adopted some active form of injury prevention, but the specific time as to when the prevention took place was not recorded in the interview. Our findings indicated there was a significant difference (p < 0.001) in the uptake of injury prevention effort between the noninjured and injured group. As shown in Table 5, results indicate that the injured group (85%) was more likely to rely on themselves (“to be more careful”) than the noninjured group (50%).
Table 4.
Comparison of precaution taken to prevent household injury between the noninjured and the injured group
| Group of noninjury, N = 584 | Percentage | Group of injury, N = 399 | Percentage | p value | |
|---|---|---|---|---|---|
| No, prevention | 465 | 79.60 | 277 | 69.40 | <0.001 |
| Yes, prevention | 119 | 20.40 | 122 | 30.60 | |
| 584 | 100 | 399 | 100 |
Among the respondents, 241 numbers of respondents had reported some preventive strategy to prevent injury. Seventeen persons responded did not know and one refused to respond
Table 5.
Typical household injury prevention methods adopted by respondents (not mutually exclusive)
| Prevention methods | Group of noninjury, N = 154 | Percentage | Group of injury, N = 127 | Percentage |
|---|---|---|---|---|
| Take care myself (be more precautious) | 77 | 50 | 108 | 85.0 |
| Safety training | 0 | 0 | 0 | 0 |
| Preventive tool | 42 | 27.27 | 15 | 11.81 |
| Window sill (guards to prevent fall) | 18 | 11.69 | 1 | 0.79 |
| Bed casing (a rail that prevented fall) | 7 | 4.55 | 1 | 0.79 |
| Place children at guarded nursery device (e.g., fenced gates or playpen) | 0 | 0 | 0 | 0 |
| Safety bell | 10 | 6.49 | 0 | 0 |
| Clean out the sundries | 0 | 0 | 2 | 1.57 |
Discussion
This is the first study conducted in a Chinese community which examines the associations between sociodemographics, living density, size of quarters, and housing type and the pattern of occurrence of nonfatal unintentional household injury. Our previous study discovered that the incidence rate of event-based nonfatal unintentional household injuries was 40.2% within the past year (12 months). While a previous study of nonfatal household unintentional injuries in children aged under 16 identified boys as more likely to sustain injuries than girls4 and had hypothesized that living density and hours and duration of time spent at home might be significant predictors for childhood home injuries; our multivariate analyses only found that females and populations living in higher-density residences are more susceptible to nonfatal household injuries. Duration spent at home is not associated with home accidents in our study. The discrepancy of our results with the previous study might be due to the difference in injury definition as well as the difference in the sampled population since our study focused on the general population instead of children under 16 as in the previous study. Another potential explanation for the demographic pattern difference between younger age groups and general populations may be that risks to unintentional injuries are associated with developmental stage or age.34
In addition, contrary to the hypothesis that public housing, which tends to have a higher living density and constitutes about 31% of the living arrangements in Hong Kong,33 may be associated with higher injury rate, our findings suggest that public housing, as a housing type that is characterized by greater structural size, uniformity in interior design, and regulated living density, might be more robust in injury prevention than private housing which tends to be more diverse in design and living density. Of note, related to living density, findings suggested lower living density appeared to be protective of incurring nonfatal home accidents.
The difference in injury prevention strategies adopted between noninjured and injured groups indicated that a variety of injury prevention strategies35 should be designed to target household injury risk perceptions of the general population. Local public health researchers have long noted in work9,36 and school30,37,38 settings that high-risk individuals31 do not always use safety equipment or engage in preventive behaviors. There is also some evidence that low-risk perception39 and low levels of safety knowledge40 contribute to accidental injuries in Hong Kong. In addition, a number of previous studies have affirmed the cost-effectiveness of injury prevention programs in terms of their capacity to prevent high morbidity and economic costs.7,20,41–46 These benefits extend not only to primary care but also to emergency room and hospital admissions. Nevertheless, when examining preventive strategies adopted by individuals, our data found that the noninjured respondents had reported a more extensive range of measures than the injured group, and an interesting pattern emerged of accident-prone individuals being more likely to quote “taking care of themselves” as an injury prevention method. Our findings regarding the installation of slip prevention device in the bathroom may reflect the cross-sectional nature of the study design as it is unclear whether the devices were installed before or after injury. Further studies might be necessary to understand what factors affect the pattern and utilization of household injury prevention measures and, perhaps from a public health perspective, the real effectiveness of these measures.
Information Bias
This study has a number of limitations. First and foremost, the episodes of injury in this study were self-reported and unverified. The results were subjected to the respondents’ definition of their injuries and their subjective assessment of the degree of severity. In addition, the most severe household injuries which lead to death were not captured by this study.
Recall Bias
We acknowledge the limited time available during telephone interviews, which allow only the most recent episode of in-depth injury experience to be examined. To address this issue, we have reported previously27 that we have revised our survey using simplified body parts, instead of the original, clinically based injury coding (International Classification of Diseases 9) used by the World Health Organization questionnaire, when enquiring about injury patterns. Our findings illustrated that although constrained, the methodology still enables a reasonable scope of relevant information for health promotion and future research planning of the subject area. Regarding recall bias for a period of 12 months, we have to acknowledge the potential recall bias towards some minor injuries that might be forgotten during reporting, and inaccuracies in recall may lead to underestimation of the injury rates over the 12-month period prior to the survey.47,48 Yet, for those injuries that might have led to health service resource utilization and health care expenditure, we believe a 12-month recall period was acceptable and that any recall bias would be moderate and would be likely to be an underestimation of the true service utilization levels.
Selection Bias
A major disadvantage of a telephone survey is that it might potentially miss households who do not possess a land-based telephone service. Nevertheless, in Hong Kong, almost all households have home-based telephone service. In addition, a large number of locally published studies on SARS or influenza vaccination49–51 have utilized this research method and found credible estimations. This study managed to achieve a response rate of 69.9%, which is similar to many of the other local studies that have been published. Furthermore, although our sample has similar gender and age distributions of the general adult population with the local midyear 2006 census data,33 there was possible selection bias as the youngest age subgroup and elementary occupational group, might be underrepresented.
As an exploratory investigation, the cost and uncertainty with parameters had led to the decision of the current sample size for testing of our research survey tool. The findings would help to refine a large-scale in-depth prospective study and the current cross-sectional study would be inadequate to understand the temporal relationship between risk behavior and outcomes. It is also important to point out that a household injury study would frequently require face-to-face home visits to assess the environmental risk factors (spatial and setting hazards).
Conclusion
Contrary to the hypothesis of previous studies for nonfatal unintentional household injuries for pediatric populations in Hong Kong,4 living characteristics such as household size, density, and time spent at home were found not to be associated with nonfatal unintentional household injuries in the general population of Hong Kong. Instead, our results indicated certain characteristics (e.g., gender, age, living in private flats/houses, and the presence of slip prevention device in bathroom) to be significantly associated with household injuries in the general population in Hong Kong. One of the reasons might be due to the difference in sample population since our study recruited subjects of all age ranges, whereas the other studies only focused on children and adolescents. More focused studies should be done to clarify the underlying reasons for these observed injury patterns, so that community health education may be better designed to protect high-risk groups from morbidity incidences incurred from these injuries.
Acknowledgements
The authors gratefully acknowledged the time and effort given by the telephone survey interviewers and Ms. Queenie Ng for data collection; Ms. Carol Suen, Ms. Jacqueline Kim, and Ms. Joyce Leung who assisted in the preparation and editing of this manuscript. The views expressed in this article are those of the authors and do not necessarily reflect the policies of any organization.
Competing Interest The authors declare that they have no competing interests.
Authors’ Contributions EC: project design, literature review, data collection, data analysis, and paper writingJK: project design, literature review, data collection, data analysis, and paper writingSG: project design and paper writingJL: project design, data collection, and paper writingIY: project design and paper writing
Funding The study was supported by a grant from the Special Study Grant from the School of Public Health, Chinese University of Hong Kong and Direct Research Grant, Faculty of Medicine, Chinese University of Hong Kong.
Ethical Approval This study obtained ethical approval in March 2007 from the Ethics Approval Committee, Faculty of Medicine, Chinese University of Hong Kong regarding Behavioral and Health Survey Research.
References
- 1.Murray CJL, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997; 349: 1269-1276. [DOI] [PubMed]
- 2.Hussey JM. The effects of race, socioeconomic status, and household structure on injury mortality in children and young adults. Matern Child Health J. 1997; 1: 217-227. [DOI] [PubMed]
- 3.Thein MM, Lee BW, Bun PY. Childhood injuries in Singapore: a community nationwide study. Singapore Med J. 2005; 46: 116-121. [PubMed]
- 4.Chan CC, Luis BPK, Chow CB, Cheung JCY, Wong TW, Chan K. Unintentional residential child injury surveillance in Hong Kong. J Paediatr Child Health. 2003; 39: 420-426. [DOI] [PubMed]
- 5.Tanaka T. Childhood injuries in Japan. Acta Paediatr Jpn. 1993; 35: 179-185. [DOI] [PubMed]
- 6.Coggan C, Hooper R, Adams B. Self-reported injury rates in New Zealand. N Z Med J. 2002; 115: U167. [PubMed]
- 7.Harlan LC, Harlan WR, Parsons PE. The economic impact of injuries: a major source of medical costs. Am J Public Health. 1990; 80: 453-459. [DOI] [PMC free article] [PubMed]
- 8.Johnson WG, Brennan TA, Newhouse JP, et al. The economic consequences of medical injuries. Implications for a no-fault insurance plan. JAMA. 1992; 267: 2487-2492. [DOI] [PubMed]
- 9.Wong TW. Occupational injuries among construction workers in Hong Kong. Occup Med. 1994; 44: 247-252. [DOI] [PubMed]
- 10.Fraser JJ Jr. Nonfatal injuries in adolescents: United States, 1988. J Adolesc Health. 1996; 19: 166-170. [DOI] [PubMed]
- 11.Man DW. Hong Kong family caregivers' stress and coping for people with brain injury. Int J Rehabil Res. 2002; 25: 287-295. [DOI] [PubMed]
- 12.Sathiyasekaran BW. Population-based cohort study of injuries. Injury. 1996;27:695-698. [DOI] [PubMed]
- 13.Fletcher PC, Hirdes JP. Risk factor for accidental injuries within senior citizens' homes: analysis of the Canadian survey on ageing and independence. J Gerontol Nurs. 2005; 31: 49-57. [DOI] [PubMed]
- 14.Chan CC, Cheng JC, Wong TW, et al. An international comparison of childhood injuries in Hong Kong. Inj Prev. 2000; 6: 20-23. [DOI] [PMC free article] [PubMed]
- 15.Leff M, Stallones L, Keefe TJ, Rosenblatt R, Reeds M. Comparison of urban and rural non-fatal injury: the results of a statewide survey. Inj Prev. 2003; 9: 332-337. [DOI] [PMC free article] [PubMed]
- 16.Lindqvist K, Timpka T, Karlsson N. Impact of social standing on injury prevention in a World Health Organization Safe Community—intervention outcome by household employment contract. Int J Epidemiol. 2004; 33: 605-611. [DOI] [PubMed]
- 17.Raven T. Do enforced bicycle helmet laws improve public health evidence is conflicting. BMJ. 2006; 332: 852. [DOI] [PMC free article] [PubMed]
- 18.Stevens M, Holman CD, Bennett N, de Klerk N. Preventing falls in older people: outcome evaluation of a randomized controlled trial. J Am Geriatr Soc. 2001; 49: 1448-1455. [DOI] [PubMed]
- 19.Bangdiwala SI, Anzola-Perez E. The incidence of injuries in young people: II. Log-linear multivariable models for risk factors in a collaborative study in Brazil, Chile, Cuba and Venezuela. Int J Epidemiol. 1990; 19: 125-132. [DOI] [PubMed]
- 20.Bijur PE, Kurzon M, Overpeck MD, Scheidt PC. Parental alcohol use, problem drinking, and children's injuries. JAMA. 1992; 267: 3166-3171. [DOI] [PubMed]
- 21.O'Halloran PD. Effectiveness of hip protectors: it's more the effectiveness of compliance strategies. BMJ. 2006; 332: 729. [DOI] [PMC free article] [PubMed]
- 22.Sellstrom E, Bremberg S, Garling A, Hornquist JO. Risk of childhood injury: predictors of mothers' perceptions. Scand J Public Health. 2000; 28: 188-193. [PubMed]
- 23.Mott JA. Personal and family predictors of children's medically attended injuries that occurred in the home. Inj Prev. 1999; 5: 189-193. [DOI] [PMC free article] [PubMed]
- 24.Potter BK, Speechley KN, Koval JJ, Gutmanis IA, Campbell MK, Manuel D. Socioeconomic status and non-fatal injuries among Canadian adolescents: variations across SES and injury measures. BMC Public Health. 2005; 5: 132. [DOI] [PMC free article] [PubMed]
- 25.Kobusingye O, Guwatudde D, Lett R. Injury patterns in rural and urban Uganda. Inj Prev. 2001; 7: 46-50. [DOI] [PMC free article] [PubMed]
- 26.Chiu KY, Ng TP, Chow SP. Seasonal variation of fractures of the hip in elderly persons. Injury. 1996; 27: 333-336. [DOI] [PubMed]
- 27.Chan EYY, Kim JH, Ng Q, Griffiths S, Lau JTF. A descriptive study of non-fatal, unintentional home based injury in urban settings. Evidence from Hong Kong. Asia Pac J Public Health. 2008; 20: 39-48. [PubMed]
- 28.Hong Kong Childhood Injury Prevention Research Group. Childhood injury prevention in Hong Kong. Hong Kong Med J. 1998; 4: 400-404. [PubMed]
- 29.Hsiang JN, Goh KY, Zhu XL, Poon WS. Features of pediatric head injury in Hong Kong. Childs Nerv Syst. 1996; 12: 611-614. [DOI] [PubMed]
- 30.Maffulli N, Bundoc RC, Chan KM, Cheng JC. Paediatric sports injuries in Hong Kong: a seven year survey. Br J Sports Med. 1996; 30: 218-221. [DOI] [PMC free article] [PubMed]
- 31.Ho WS, Ying SY. An epidemiological study of 1063 hospitalized burn patients in a tertiary burns centre in Hong Kong. Burns. 2001; 27: 119-123. [DOI] [PubMed]
- 32.Sethi D, Habibula S, McGee K, et al. Guidelines for Conducting Community Surveys on Injuries and Violence. Geneva: WHO; 2004. [DOI] [PubMed]
- 33.The Census and Statistics Department. Report of Hong Kong 2006 Population By-census. Hong Kong: HKSAR Government; 2006.
- 34.Desafey Liller K. Injury Prevention for Children and Adolescents. Research, Practices and Advocacy. Washington DC: American Public Health Association; 2006.
- 35.Kendrick D, Coupland C, Mulvaney C, et al. A home safety education and provision of safety equipment for injury prevention (review). Cochrane Library. 2007; 2: CD005014. [DOI] [PubMed]
- 36.Siu OL, Phillips DR, Leung TW. Age differences in safety attitudes and safety performance in Hong Kong construction workers. J Saf Res. 2003; 34: 199-205. [DOI] [PubMed]
- 37.Sun YH, Yu I, Wong TW, Zhang Y, Fan YP, Guo SQ. Unintentional injuries at school in China-patterns and risk factors. Accid Anal Prev. 2006; 38: 208-214. [DOI] [PubMed]
- 38.Sun YH, Yu I, Zhang Y, Fan YP, Guo SQ, Wong TW. Unintentional injuries among primary and middle school students in Maansshan City, eastern China. Acta Paediatr. 2006; 95: 268-275. [DOI] [PubMed]
- 39.Siu OL, Phillips DR, Leung TW. Safety climate and safety performance among construction workers in Hong Kong. The role of psychological strains as mediators. Accident Anal Prev. 2004; 36: 359-366. [DOI] [PubMed]
- 40.Sze PC, Lam PS, Chan J, Leung KS. A primary fall prevention programme for older people in Hong Kong. Br J Community Nurs. 2005; 10: 166-171. [DOI] [PubMed]
- 41.Macarthur C. Evaluation of Safe Kids Week 2001: prevention of scald and burn injuries in young children. Inj Prev. 2003; 9: 112-116. [DOI] [PMC free article] [PubMed]
- 42.Lindqvist K, Timpka T, Schelp L, Ahlgren M. Evaluation of a home injury prevention program in a WHO Safe Community. Int J Consum Prod Saf. 1999; 6: 25-32.
- 43.Jordan EA, Duggan AK, Hardy JB. Injuries in children of adolescent mothers: home safety education associated with decreased injury risk. Pediatrics. 1993; 91: 481-487. [PubMed]
- 44.Hemmo-Lotem M, Danon Y. Childhood injuries in Israel: status and prevention strategies. Harefurah. 2003; 142(8–9): 609-611. 645, 646. [PubMed]
- 45.Watson R. EU is urged to reduce injuries to children. BMJ. 2005; 331: 1163. [DOI] [PMC free article] [PubMed]
- 46.Larsen ER, Mosekilde L, Foldspang A. Determinants of acceptance of a community-based program for the prevention of falls and fractures among the elderly. Prev Med. 2001; 33: 115-119. [DOI] [PubMed]
- 47.Harel Y, Overpeack MD, Jones DH, et al. The effects of recall on estimating annual nonfatal injury rates for children and adolescents. Am J Public Health. 1994; 84: 599-605. [DOI] [PMC free article] [PubMed]
- 48.Cummings P, Rivara FP, Thomposon RS, Reid RJ. Ability of parents to recall the injuries of their young children. Injury Prev. 2005; 11: 43-47. [DOI] [PMC free article] [PubMed]
- 49.Lau JT, Kim JH, Tsui HY, Griffiths S. Perceptions related to bird-to-human avian influenza, influenza vaccination, and use of face mask. Infection. 2008; 36(5): 434-443. [DOI] [PMC free article] [PubMed]
- 50.Lau JT, Tsui HY, Kim JH, Griffiths S. Perceptions about status and modes of H5N1 transmission and associations with immediate behavioral responses in the Hong Kong general population. Prev Med. 2006; 43(5): 406-410. [DOI] [PubMed]
- 51.Lau JT, Kim JH, Tsui HY, Griffiths S. Perceptions related to human avian influenza and their associations with anticipated psychological and behavioral responses at the onset of outbreak in the Hong Kong Chinese general population. Am J Infect Control. 2007; 35(1): 38-49. [DOI] [PMC free article] [PubMed]