Although widely recommended, cryopreservation of sperm is sometimes not performed for patients with Hodgkin’s lymphoma because of presumed poor sperm quality related to the disease. In this large study of males with Hodgkin’s lymphoma, 90% had good or intermediate sperm quality, indicating that in most patients with early-stage Hodgkin’s lymphoma sperm quality before treatment is good enough for future fatherhood.
Keywords: Hodgkin’s lymphoma, fertility, male, sperm quality, sperm
Abstract
Background
Although widely recommended, cryopreservation of sperm is sometimes not performed for patients with Hodgkin’s lymphoma because of presumed poor sperm quality related to the disease. We investigated sperm quality and factors determining it in untreated patients with early stage Hodgkin’s lymphoma.
Design and Methods
Of 2362 males who participated in EORTC H6–H9 trials, 474 (20%) had data available. Sperm quality was defined according to World Health Organization guidelines. Determining factors were studied by logistic regression analysis.
Results
The median sperm concentration was 40×106/mL (range, 0–345×106/mL) and the median motility 50% (range, 0–90%). Sperm quality was good (concentration ≥20×106/mL and motility ≥50%), intermediate (concentration ≥5×106/mL) and poor (concentration <5×106/mL but >0) in 41%, 49% and 7% of patients, respectively. Three percent of the patients were azoospermic. No relation was found between sperm quality and age or clinical stage of the Hodgkin’s lymphoma, but B-symptoms and elevated erythrocyte sedimentation rate predicted poor sperm quality. The odds ratios for the association of poor sperm quality with the variables examined were: presence of B-symptoms, 2.77 (95% CI, 1.50–5.12; p=0.001); erythrocyte sedimentation rate of 50 mm/h or greater, 2.35 (95% CI, 1.24–4.43; p=0.009); fever, 3.22 (95% CI, 1.41–7.33; p=0.005), and night sweats, 3.78 (95% CI, 1.97–7.26; p<0.001). There was no relation between sperm quality and pre-treatment follicle stimulating hormone level.
Conclusions
In this large study of males with Hodgkin’s lymphoma, 90% had good or intermediate sperm quality. Three percent were azoospermic. There was an association between sperm quality and the presence or absence of B-symptoms, in particular fever and night sweats. With modern fertilization techniques, in most patients with early-stage Hodgkin’s lymphoma sperm quality before treatment is good enough for future fatherhood.
Introduction
Because Hodgkin’s lymphoma is often diagnosed in patients in young adulthood whose cure rate is between 80 and 90%,1,2 preservation of fertility and semen cryopreservation are important.3 Not only chemotherapy, but also the disease process itself appears to influence spermatogenesis. Data from patients with Hodgkin’s lymphoma hint that before treatment such patients have lower sperm counts and reduced sperm motility compared to healthy subjects,4,5 but data from large series of patients are lacking; the largest series studied thus far comprised 212 patients.6 The cause of the diminishment in semen quality is not completely understood and has been attributed to fever, poor performance, psychological factors7,8 or even immune-mediated mechanisms.9
For many years gonadal toxicity has been studied in trials by the European Organization for Research and Treatment of Cancer (EORTC) Lymphoma Group and the Groupe d’Étude des Lymphomes de l’Adulte (GELA). This gave us the opportunity to study the spermatogenesis of a large cohort of male patients with early-stage Hodgkin’s lymphoma prior to treatment. We compared the quality of sperm in untreated patients with Hodgkin’s lymphoma to that in various general populations. Secondly, we studied factors influencing sperm quality and finally we analyzed the relation between pre-treatment follicle stimulating hormone (FSH) concentration and sperm quality.
Design and Methods
Patients
All male patients with early stage classical Hodgkin’s lymphoma included in the EORTC-GELA intergroup trials H6, H7, H8 and H9 (1982–2004)10–13 were analyzed. Patients were aged 15 to 70 years and presented with histologically proven, previously untreated, clinical stage I or II supradiaphragmatic Hodgkin’s lymphoma with World Health Organization (WHO) performance status grade 0–2. Patients with concomitant or previous malignancies were excluded as were patients with serious comorbidity. Between August 1982 and May 2004, 2362 men were enrolled and registered in the EORTC-GELA database. The studies were carried out in accordance with the Helsinki Declaration. Protocols and informed consent were approved by local ethical committees. Data from sperm quality examinations conducted prior to treatment were available for 474 men (20%). Of these 474 men, 35 participated in the H6, 77 in the H7, 181 in the H8 and 181 in the H9 trial. For 205 out of the 474 men, FSH values before treatment were also available.
Collection and analysis of data
Data on demographic and Hodgkin’s lymphoma-related variables were collected according to the EORTC-GELA study protocols. For each patient, demographic data, stage of the disease (I or II), presence of systemic (B-) symptoms, erythrocyte sedimentation rate (ESR) and smoking habits were recorded. Smoking was registered for patients in the H6, H8 and H9 trials and each patient was defined as a current smoker (yes or no, H6 trial), or as never smoker, ever smoker who had stopped smoking more than 10 years previously, ever smoker who had stopped smoking less than 10 years ago, current smoker for less than 10 years and current smoker for more than 10 years (H8 and H9 trials). For the current analysis, however, patients were re-coded as current or not current smokers. B-symptoms were defined as the presence of at least one of the following: weight loss of more than 10% of ideal body weight within the preceding 6 months, recurrent drenching night sweats during the preceding months and unexplained, persistent or recurrent fever exceeding 38°C for 8 days or more. For the H6 trial, B-symptoms were not further specified; for the H7, H8 and H9 trials a specification into the symptoms mentioned above was provided. Pre-treatment FSH concentration was also measured in some, but not in all, patients. Whether or not FSH was measured depended on the recruiting hospitals’ participation in toxicity analyses and was unrelated to patients’ characteristics; hence, there was no selection bias involved. FSH values were dichotomized (normal or elevated) according to the normal values given by the laboratories performing the analyses. Because normal values for FSH are different in each laboratory, FSH levels were normalized to render values comparable to one another by dividing FSH by the individual upper normal value provided.
Sperm quality examinations
Sperm analyses were carried out at the laboratories of the hospitals in which patients were treated. Patients were included between August 1982 and May 2004. During that period, no inter-laboratory quality control systems were available. Sperm analysis was performed before the semen was frozen. Sperm quality was defined according to WHO guidelines14 and divided into three categories: good quality if the sperm concentration was 20×106/mL or greater and motility 50% or greater; poor quality if the sperm concentration was less than 5×106/mL; and intermediate quality for all other concentrations except the complete absence of spermatozoa in the ejaculate, which was classified as azoospermia.
Statistics
The aim of the study was to analyze factors influencing sperm quality in untreated patients with Hodgkin’s lymphoma, and to analyze the relationship between FSH and sperm quality and sperm concentration. Ninety-five percent confidence intervals (95% CI) of the proportions of patients within sperm quality categories were calculated assuming a binomial distribution. An analysis of factors influencing sperm quality was performed using the Fisher’s exact test for categorical data or Kruskal-Wallis test for age and ESR. Logistic regression models (univariate and multivariate analyses) were constructed to assess the impact of independent co-variates on the sperm quality (good sperm quality and intermediate sperm quality grouped together versus poor sperm quality including azoospermia). Factors examined were: patient’s age at measurement (both as a continuous variable and divided into three groups ≤20 years versus 21–40 years versus >40 years), clinical stage (I versus II), B-symptoms (absent versus present), fever (absent versus present), weight loss (absent versus present), night sweats (absent versus present), ESR (<50 mm/h versus ≥50 mm/h) and smoking status (non-current smokers versus current smokers).
A Kruskal-Wallis test was used to analyze the relation between FSH and sperm quality. Spearman’s rank correlation coefficient was used to assess the correlation between FSH and sperm concentration. All statistical tests were two-sided, and a p value less than 0.05 was considered statistically significant. SAS statistical software (release 9.1 TS Level 1M3; SAS Institute, Cary, NC) was used to analyze data. Data were selected from files stored at the Clinical Research Unit, Centre François Baclesse, Caen, France and were updated on January 1, 2006.
Results
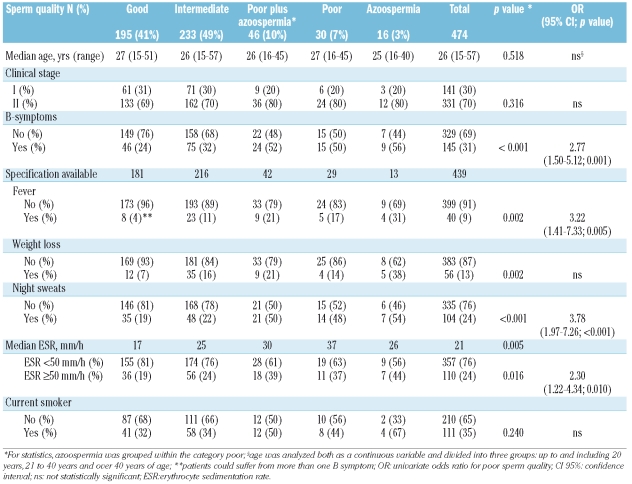
Data from 474 male patients with early stage Hodgkin’s lymphoma and a median age of 26 years (range, 15–57 years) were available (Table 1). The patients came from France (57%), the Netherlands (31%), Belgium (7%), and the remaining 5% from Slovenia, Switzerland, Portugal, Italy, Poland, the United Kingdom and Croatia. Seventy percent had stage II disease and 31% had B-symptoms. The median sperm concentration was 40×106/mL (range, 0–345×106/mL). The median motility was 50% (range, 0–90%). WHO-defined sperm quality was good, intermediate and poor (concentration ≥20×106/mL and motility ≥50% for good, concentration >5×106/mL for intermediate, and concentration <5×106/mL but >0 for poor) in 41% (95% CI, 37–46%), 49% (95% CI, 45–54%) and 7% (95% CI, 4–9%) of patients, respectively, whereas 3% (95% CI, 2–5%) of the patients were azoospermic.
Table 1.
Patients’ characteristics in relation to sperm quality.
For 77 (16%) of the patients, measurements of sperm quality after treatment were also available. Interestingly, in two patients who were azoospermic before treatment we observed a complete recovery to normal sperm quality after treatment (one patient at 18 months after treatment, the other at 38 months after treatment). The first patient was treated with six cycles of MOPP/ABV hybrid (mechlorethamine, vincristine, pro-carbazine, prednisone, doxorubicin, bleomycin, vinblastine) chemotherapy and involved-field radiotherapy, the second with six cycles of EBVP (epirubicin, bleomycin, vinblastine, prednisone) chemotherapy and involved-field radiotherapy.
No relation was found between sperm quality and age, clinical stage (I or II) or smoking. However, the presence of B-symptoms and elevated ESR were linked with poor sperm quality (p<0.001 and p=0.005). Each of the three single B-symptoms (fever, weight loss and night sweats) separately also had a statistically significant negative effect on sperm quality. By univariate logistic regression, however, weight loss did not yield a statistically significant result whereas the association of fever and night sweats with poor sperm quality remained statistically significant (Table 1). We performed multivariate logistic regression analysis with B-symptoms and ESR greater than 50 mm/h as independent factors, resulting in B-symptoms as the only remaining explaining variable (odds ratio (OR) 2.64, 95% CI 1.54–4.54; p=0.003). Including fever, night sweats and ESR greater than 50 mm/h in the model showed that night sweats was the only remaining explaining variable (OR 3.78, 95% CI 2.19–6.54; p<0.001).
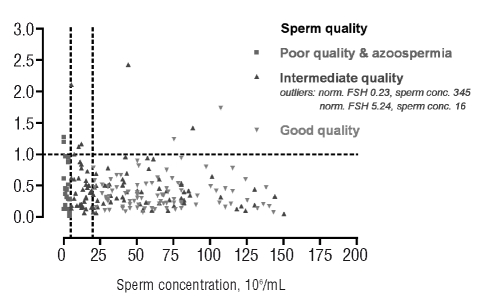
Of the 474 patients, 205 (43%) had pre-treatment data on FSH available. The relation between FSH and sperm concentration is plotted in Figure 1. Pre-treatment FSH was elevated in only ten (5%) of the patients, of whom four had a normal sperm concentration (≥20×106/mL), four had a sperm concentration between 5×106/mL and 20×106/mL and two were azoospermic. The medians of normalized FSH values were not statistically different for the three sperm quality categories (p=0.328). Spearman’s correlation for FSH and sperm concentration was −0.139 (p=0.047).
Figure 1.
Sperm quality and FSH level before treatment. Sperm quality was divided into three categories: good quality if concentration of spermatozoa was ≥20×106/mL and motility ≥50%; poor quality if concentration of spermatozoa was <5×106/mL; intermediate quality for all other concentrations, except azoospermia. First vertical reference line: sperm concentration: 5×106/mL. Second vertical reference line: sperm concentration: 20×106/mL. Horizontal reference line: FSH: upper normal value; values above this line indicate elevated FSH and values below this line indicate non-elevated FSH. Two outliers are present; norm. FSH: normalized FSH.
Discussion
This study involved a very large group of male patients whose sperm quality was analyzed before the start of treatment for Hodgkin’s lymphoma. It appeared that, with modern fertilization techniques, fatherhood could be guaranteed for 97% of patients.
Sperm quality was not analyzed in all patients. This was mainly dependent on the local hospitals and coordinating physicians, and not on the patients’ characteristics. To render data from a wide time span and many different hospitals comparable, only data on sperm concentration and progressive motility were analyzed. Sperm morphology assessment was considered more subjective and thus less easily comparable between laboratories than simple cell counts.
Ninety percent of patients with early stage Hodgkin’s lymphoma had WHO-defined good or intermediate sperm quality at disease presentation, whereas 7% of patients had poor sperm quality and 3% of patients were azoospermic. The median sperm concentration was 40×106/mL and the median sperm motility was 50%. These values are seemingly normal, but probably slightly below those in general population controls, although data from such populations are limited. In fact, most data on sperm quality in the general population have been collected from selected groups of fertile men volunteering as sperm donors or undergoing vasectomy procedures.15,16 Moreover, sperm quality differs regionally17 and is considered to be time-dependent, having diminished over time during the last decades in developed countries.18,19 This last fact might be important as sperm analysis took place between 1982 and 2004. Finally, since sperm concentration and motility are not normally distributed, median values were used in the present study20 instead of mean values frequently used by others, hampering easy numerical comparisons.21–24
There are only few data concerning a non-selected population, i.e. a population without proven fertility, against which to compare those of the patients in our study. The only two completely random samples came from Denmark, but the sperm quality of men in this country is reputed to be among the lowest in Europe.25 It appeared that the median concentration and motility of sperm from our study population were in line with those of sperm from non-selected, young Danish men, either undergoing an examination for military service26 or being Danish trade union members without children or known fertility problems.27
Nowadays, patients with intermediate or poor quality sperm are still eligible to enter sperm cryopreservation programs with a view to subsequent in vitro fertilization or intracytoplasmatic sperm injection. The only serious problem for future fertility encountered in our study cohort was constituted by the 3% of cases with azoospermia, since this obviously excludes cryopreservation.28 The incidence of azoospermia in the general population is not known, but is often assumed to be 2%, mainly based on a study conducted on forensic evidence from 519 rape cases.29
Compared to previous studies in patients with Hodgkin’s lymphoma, our data showed better sperm quality than in some analyses,6,30 but worse quality than in others.7,31,32 Our study was, however, based on data from by far the largest series studied up date; this offered not only a more reliable estimation of sperm quality but also the opportunity to study factors influencing sperm quality. Neither of the two groups5,32 that tried to analyze the influence of B-symptoms and fever on sperm quality before treatment found a significant difference between patients with or without these manifestations, most probably due to limited sample sizes (92 and 94 patients, respectively). Our data show that poor sperm quality is strongly associated with the presence of B-symptoms, in particular fever and night sweats, which might in part be related to the well-known adverse effect of elevated scrotal temperature on spermatogenesis.33 Given that patients with fever nearly always had night sweats as well, it was not possible to determine which of the individual B-symptoms had the strongest impact. Another limitation of our study is that only patients with early stage disease were enrolled: two other studies30,34 previously showed that advanced-stage disease has a greater negative effect than early-stage disease on semen quality.
Previously we observed that elevated FSH levels correlate well with poor spermatogenesis after treatment,35 but in our present study this relationship apparently did not exist before treatment. This is confirmed by the scarce observations in the literature5,6,30 and means that whereas semen quality after cancer therapy is poor due to damage to the gonadal structures, there must be another reason to explain diminished sperm quality before treatment. Poor sperm quality in cancer patients is assumed to be related to hypothalamic dysfunction caused by the systemic illness, catabolic state and malnutrition.8,36 In addition, there is a postulated effect of both circulating cytokines30 and an imbalance of sub-populations of T lymphocytes, which may be involved in spermatogenesis.9 Here, we have shown that fever, if present, contributes as well in patients with Hodgkin’s lymphoma. The fact that sperm quality is threatened by two completely different mechanisms before and after treatment means that even in patients with very poor quality sperm before treatment, fertility after treatment could be excellent if cancer therapy (for instance ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) chemotherapy) is not gonadotoxic.35 Our finding of two patients who were azoospermic before treatment but had normal sperm quality after treatment is in agreement with this theory. Thus, it is still worthwhile selecting non-gonadotoxic therapy for men with Hodgkin’s lymphoma, even if they are infertile before treatment.
A large Life Situation Questionnaire has been designed by the EORTC-GELA Lymphoma Group to further analyze fertility and fatherhood after therapy among patients with Hodgkin’s lymphoma.
In conclusion, in most patients with early stage Hodgkin’s lymphoma, sperm quality before treatment is not a problematic issue and cryopreservation should be encouraged.
Appendix
Patients were included by the following centers
France (n=270), Institut Gustave Roussy, Villejuif, (n=37) (P. Carde, C. Fermé); Hôpital Saint-Louis, Paris (n=21), (P. Brice); CHU Nancy Hôpital Brabois, Vandoeuvre-les-Nancy (n=18) (P. Léderlin); Centre François Baclesse, Caen (n=16) (A. Tanguy); Institut Bergonié, Bordeaux (n=13) (H. Eghbali); CHU de Besançon Hôpital Jean Minjoz, Besançon (n=12) (L. Voillat); CHU Clémenceau, Caen (n=11) (O. Reman); Centre Hospitalier René Dubos, Pontoise (n=11) (Y.J.P. Kerneis); Centre Hospitalier de Chambéry, Chambéry (n=10) (M. Blanc); Hôpital Henri Mondor, Créteil (n=7) (M. Diviné); Hôpital Saint-Antoine, Paris (n=7) (M. Aoudjhane); Centre Hospitalier Lyon Sud, Pierre-Bénite (n=7) (G. Salles); Centre Alexis Vautrin, Vandoeuvre-les-Nancy (n=7) (T. Conroy); CHRU de Lille Hôpital Claude Huriez, Lille (n=6) (F. Morschauser); Hôpital Edouard Herriot, Lyon (n=6) (J. Troncy); Centre Léon Bérard, Lyon (n=5) (C. Sebban); CHU Saint-Etienne Hôpital Nord, Saint-Etienne (n=5) (J. Jaubert); Hôpital Bicêtre, Le Kremlin-Bicêtre (n=4) (G. Tertian); Institut J. Paoli & I. Calmettes, Marseille (n=4) (R. Bouabdallah); Centre Hospitalier Régional de Metz-Thionville, Metz (n=4) (B. Christian); Centre Antoine Lacassagne, Nice (n=4) (A. Thyss); Centre René Huguenin, Saint-Cloud (n=4) (M. Janvier); Centre Médico-Chirurgical Foch, Suresnes (n=4) (E. Baumelou); Centre Hospitalier d’Annecy, Annecy (n=3) (C. Martin); Hôpital Gilles de Corbeil, Corbeil-Essonnes (n=3) (A. Devidas); CHU Dijon, Dijon (n=3) (R.O. Casanovas); Centre Georges-François Leclerc, Dijon (n=3) (P. Fargeot); CHU de Limoges Hôpital Dupuytren, Limoges (n=3) (D. Bordessoule); Hôpital Pitié-Salpétrière, Paris (n=3) (J. Gabarre); Centre Hospitalier de Compiègne, Compiègne (n=2) (D. Zylberait); Centre Hospitalier de Dunkerque, Dunkerque (n=2) (M. Wetterwald); Clinique du Mail, Grenoble (n=2) (D. Assouline); CHU de Montpellier Saint-Eloi, Montpellier (n=2) (P. Quittet); Centre Val d’Aurelle Paul Lamarque, Montpellier (n=2) (M. Fabbro); Institut Curie, Paris (n=2) (J. Dumont); Hôpital Necker, Paris (n=2) (R. Delarue); Centre Henri Becquerel, Rouen (n=2) (A. Stamatoullas); Centre Hospitalier de Valence, Valence (n=2) (P-Y. Péaud); Centre d’Oncologie et de Radiothérapie de Chaumont-le-Bois, Chaumont (n=1) (G. Dupont); Hôpital Pasteur, Colmar (n=1) (B. Audhuy); Hotel-Dieu du Creusot, Le Creusot (n=1) (Dr. Gabez); Centre Hospitalier Robert Boulin, Libourne (n=1) (K. Bouabdallah); CHU Hôpital l’Archet, Nice (n=1) (P. Heudier); Hôpital Cochin, Paris (n=1) (F. Dreyffus); Hotel-Dieu, Paris (n=1) (A. Delmer); Hôpital Lariboisière, Paris (n=1) (J-M. Zini); CHU de Bordeaux Hôpital Haut-Lévèque, Pessac (n=1) (G. Marit); Hôpital de Saint-Germain-en-Laye, Saint-Germain-en-Laye (n=1) (M. Azagury); CHU de Toulouse Hôpital Purpan, Toulouse (n=1) (M. Attal). The Netherlands (n=147) Leids Universitair Medisch Centrum, Leiden (n=32) (J.C. Kluin-Nelemans, R. Willemze); NKI, Antoni van Leeuwenhoek Ziekenhuis, Amsterdam (n=16) (J.W. Baars) Erasmus Medisch Centrum, Rotterdam (n=15) (P.J. Lugtenburg, M.B. van ’t Veer); Medisch Spectrum Twente, Enschede (n=9) (J.H. Meerwaldt); Universitair Medisch Centrum Utrecht, Utrecht (n=9) (A. Hagenbeek); Isala Klinieken, Zwolle (n=7) (R. van Marwijk Kooy); St Antonius Ziekenhuis, Nieuwegein (n=6) (D.H. Biesma); Academisch Medisch Centrum, Amsterdam (n=5) (M.H.J. van Oers); Onze Lieve Vrouwe Gasthuis, Amsterdam (n=5) (K.J. Roozendaal); Medisch Centrum Leeuwarden, Leeuwarden (n=5) (P. Joosten); Meander Medisch Centrum location Lichtenberg, Amersfoort (n=4) (M.H.H. Kramer); Universitair Medisch Centrum Groningen, Groningen (n=4) (G.W. van Imhoff); Reinier de Graaf Gasthuis, Delft (n=3) (E.F.M. Posthuma); HagaZiekenhuis location Leyweg, Den Haag (n=3) (P.W. Wijermans); Amphia Ziekenhuis location Molengracht, Breda (n=2) (A.C.J.M. Holdrinet); Jeroen Bosch Ziekenhuis, Den Bosch (n=2) (H.A.M. Sinnige); HagaZiekenhuis location Rode Kruis, Den Haag (n=2) (W.A. van Deijk); Catharina Ziekenhuis, Eindhoven (n=2) (G-J. Creemers); Groene Hartziekenhuis, Gouda (n=2) (R.F.A. Simonis); Spaarne Ziekenhuis, Hoofddorp (n=2) (C.A.M. de Swart); Diaconessenhuis, Leiden (n=2) (H. van Slooten); St Anna Ziekenhuis, Geldrop (n=1) (R.E.H. Smeets); Martini Ziekenhuis, Groningen (n=1) (H. Piersma); Atrium Medisch Centrum location Heerlen, Heerlen (n=1) (M. Fickers); Tergooiziekenhuizen locatie Hilversum; Hilversum (n=1) (H.M. Muller); Medisch Centrum Haaglanden location Antoniushove, Leidschendam (n=1) (M.G. Herben); Universitair Medisch Centrum St Radboud, Nijmegen (n=1) (J. Raemaekers); Maasland Ziekenhuis, Sittard (n=1) (H.N.L.M. Bron); Ziekenhuis Bernhoven, location Veghel, Veghel (n=1) (L.H. Hulsteijn); Máxima Medisch Centrum location Veldhoven (n=1) (J.J. Keuning); Diaconessenhuis, Voorburg (n=1), (E.F.M. Posthuma). Belgium (n=35) UZ Gasthuisberg, Leuven (n=13) (J. Thomas); Universitair Ziekenhuis Antwerpen, Edegem (n=6) (W. Schroyens); Institut Jules Bordet, Bruxelles (n=4) (D. Bron); Centre Hospitalier Notre Dame et Reine Fabiola, Charleroi (n=3) (M. André); Cliniques Universitaires Saint-Luc, Bruxelles (n=2) (A. Ferrant); Cliniques Universitaires de Mont-Godinne, Yvoir (n=2) (A. Bosly); ZNA Middelheim, Antwerpen (n=1) (R. de Bock, P. Meijnders); AZ St Jan, Brugge (n=1) (A. van Hoof); Hôpital Saint-Joseph, Gilly (n=1) (P. Mineur); Centre Hospitalier Régional Clinique Saint-Joseph, Mons (n=1) (D. Boulet); Clinique Sainte-Elisabeth, Namur (n=1) (V. Mathieux). Other countries (n=22) Slovenia, Institut of Oncology, Ljubljana (n=9) (R. Tomsac, M. Vovk); Switzerland, CHU Vaudois, Lausanne (n=4) (N. Ketterer); Portugal, Instituto Portugues de Oncologia, Porto (n=3) (F. Viseu); Poland, Curie Memorial Cancer Centre, Warsaw (n=2) (J. Meder, J. Walewski); Croatia, University, Hospital Rebro, Zagreb (n=1) (I. Aurer); Italy, Centro di Riferimento Oncologico, Aviano (n=1) (U. Tirelli); Italy, Ospedale S. Maria Delle Croci, Ravenna (n=1) (G. Rosti); United Kingdom, General Hospital, Southampton (n=1) (M. Whitehouse).
Footnotes
Funding: this work was supported by a research grant from the Lance Armstrong Foundation.
Authorship and Disclosures
MK and HKN were the principal investigators and take primary responsibility for the paper. MK, MHA and HKN designed the research. JR, PC, EN, CF, JT, HE, PB, CB and HKN recruited the patients. MK, NH, JEA and MHA analyzed the data. JR, CF, MHA and HKN co-ordinated the research. MK, JEA, MHA and HKN wrote the paper. All authors approved the final version of the paper.
Parts of the data in this article were presented at the 7th International Symposium on Hodgkin lymphoma on November 5th 2007 in Cologne, Germany (Haematologica 2007; 92 (Suppl 5):47abstr P047).
The authors report no potential conflicts of interest.
References
- 1.Sieber M, Rueffer U, Josting A, Diehl V. Treatment of Hodgkin’s disease: current strategies of the German Hodgkin’s Lymphoma Study Group. Ann Oncol. 1999;10 (Suppl 6):23–9. [PubMed] [Google Scholar]
- 2.Raemaekers J, Kluin-Nelemans H, Teodorovic I, Meerwaldt C, Noordijk E, Thomas J, et al. The achievements of the EORTC Lymphoma Group. European Organization for Research and Treatment of Cancer. Eur J Cancer. 2002;38 (Suppl 4):S107–13. doi: 10.1016/s0959-8049(01)00446-4. [DOI] [PubMed] [Google Scholar]
- 3.Brusamolino E, Bacigalupo A, Barosi G, Biti G, Gobbi PG, Levis A, et al. Classical Hodgkin’s lymphoma in adults: guidelines of the Italian Society of Hematology, the Italian Society of Experimental Hematology, and the Italian Group for Bone Marrow Transplantation on initial work-up, management and follow-up. Haematologica. 2009;94:550–65. doi: 10.3324/haematol.2008.002451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitehead E, Shalet SM, Blackledge G, Todd I, Crowther D, Beardwell CG. The effects of Hodgkin’s disease and combination chemotherapy on gonadal function in the adult male. Cancer. 1982;49:418–22. doi: 10.1002/1097-0142(19820201)49:3<418::aid-cncr2820490304>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 5.Viviani S, Ragni G, Santoro A, Perotti L, Caccamo E, Negretti E, et al. Testicular dysfunction in Hodgkin’s disease before and after treatment. Eur J Cancer. 1991;27:1389–92. doi: 10.1016/0277-5379(91)90017-8. [DOI] [PubMed] [Google Scholar]
- 6.Sieniawski M, Reineke T, Josting A, Nogova L, Behringer K, Halbsguth T, et al. Assessment of male fertility in patients with Hodgkin’s lymphoma treated in the German Hodgkin Lymphoma Study Group (GHSG) clinical trials. Ann Oncol. 2008;19:1795–801. doi: 10.1093/annonc/mdn376. [DOI] [PubMed] [Google Scholar]
- 7.Marmor D, Elefant E, Dauchez C, Roux C. Semen analysis in Hodgkin’s disease before the onset of treatment. Cancer. 1986;57:1986–7. doi: 10.1002/1097-0142(19860515)57:10<1986::aid-cncr2820571017>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal A, Allamaneni SS. Disruption of spermatogenesis by the cancer disease process. J Natl Cancer Inst Monogr. 2005;34:9–12. doi: 10.1093/jncimonographs/lgi005. [DOI] [PubMed] [Google Scholar]
- 9.Barr RD, Clark DA, Booth JD. Dyspermia in men with localized Hodgkin’s disease. A potentially reversible, immune-mediated disorder. Med Hypotheses. 1993;40:165–8. doi: 10.1016/0306-9877(93)90205-5. [DOI] [PubMed] [Google Scholar]
- 10.Carde P, Hagenbeek A, Hayat M, Monconduit M, Thomas J, Burgers MJ, et al. Clinical staging versus laparotomy and combined modality with MOPP versus ABVD in early-stage Hodgkin’s disease: the H6 twin randomized trials from the European Organization for Research and Treatment of Cancer Lymphoma Cooperative Group. J Clin Oncol. 1993;11:2258–72. doi: 10.1200/JCO.1993.11.11.2258. [DOI] [PubMed] [Google Scholar]
- 11.Noordijk EM, Carde P, Dupouy N, Hagenbeek A, Krol AD, Kluin-Nelemans JC, et al. Combined modality therapy for all patients with clinical stage I–II Hodgkin's lymphoma. Long term results of the EORTC H7 randomized controlled trials (1988–1993) J Clin Oncol. 2006;24:3128–35. doi: 10.1200/JCO.2005.05.2746. [DOI] [PubMed] [Google Scholar]
- 12.Ferme C, Eghbali H, Meerwaldt JH, Rieux C, Bosq J, Berger F, et al. Chemotherapy plus involved-field radiation in early-stage Hodgkin’s disease. N Engl J Med. 207;357:1916–27. doi: 10.1056/NEJMoa064601. [DOI] [PubMed] [Google Scholar]
- 13.Thomas J, Ferme C, Noordijk E, van 't Veer MB, Brice P, Diviné M, et al. Results of the EORTC-GELA H9 randomized trials: the H9-F trial (comparing 3 radiation dose levels) and H9-U trial (comparing 3 chemotherapy schemes) in patients with favorable or unfavorable early stage Hodgkin’s lymphoma (HL) Haematologica 20079227.[Abstract]17229632 [Google Scholar]
- 14.World Health Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 4th ed. Cambridge: Cambridge University Press; 2000. [Google Scholar]
- 15.Auger J, Kunstmann JM, Czyglik F, Jouannet P. Decline in semen quality among fertile men in Paris during the past 20 years. N Engl J Med. 1995;332:281–5. doi: 10.1056/NEJM199502023320501. [DOI] [PubMed] [Google Scholar]
- 16.Auger J, Jouannet P. Evidence for regional differences of semen quality among fertile French men. Fédération Française des Centres d’Etude et de Conservation des Oeufs et du Sperme humains. Hum Reprod. 1997;12:740–5. doi: 10.1093/humrep/12.4.740. [DOI] [PubMed] [Google Scholar]
- 17.Jorgensen N, Andersen AG, Eustache F, Irvine DS, Suominen J, Petersen JH, et al. Regional differences in semen quality in Europe. Hum Reprod. 2001;16:1012–9. doi: 10.1093/humrep/16.5.1012. [DOI] [PubMed] [Google Scholar]
- 18.Carlsen E, Giwercman A, Keiding N, Skakkebaek NE. Evidence for decreasing quality of semen during past 50 years. BMJ. 1992;305:609–13. doi: 10.1136/bmj.305.6854.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Swan SH, Elkin EP, Fenster L. The question of declining sperm density revisited: an analysis of 101 studies published 1934–1996. Environ Health Perspect. 2000;108:961–6. doi: 10.1289/ehp.00108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berman NG, Wang C, Paulsen CA. Methodological issues in the analysis of human sperm concentration data. J Androl. 1996;17:68–73. [PubMed] [Google Scholar]
- 21.Schwartz D, Mayaux MJ, Spira A, Moscato ML, Jouannet P, Czyglik F, et al. Semen characteristics as a function of age in 833 fertile men. Fertil Steril. 1983;39:530–5. doi: 10.1016/s0015-0282(16)46946-3. [DOI] [PubMed] [Google Scholar]
- 22.Vierula M, Niemi M, Keiski A, Saaranen M, Saarikoski S, Suominen J. High and unchanged sperm counts of Finnish men. Int J Androl. 1996;19:11–7. doi: 10.1111/j.1365-2605.1996.tb00427.x. [DOI] [PubMed] [Google Scholar]
- 23.Van Waeleghem K, De Clercq N, Vermeulen L, Schoonjans F, Comhaire F. Deterioration of sperm quality in young healthy Belgian men. Hum Reprod. 1996;11:325–9. doi: 10.1093/humrep/11.2.325. [DOI] [PubMed] [Google Scholar]
- 24.Bujan L, Mansat A, Pontonnier F, Mieusset R. Time series analysis of sperm concentration in fertile men in Toulouse, France between 1977 and 1992. BMJ. 1996;312:471–2. doi: 10.1136/bmj.312.7029.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jorgensen N, Asklund C, Carlsen E, Skakkebaek NE. Coordinated European investigations of semen quality: results from studies of Scandinavian young men is a matter of concern. Int J Androl. 2006;29:54–61. doi: 10.1111/j.1365-2605.2005.00635.x. [DOI] [PubMed] [Google Scholar]
- 26.Andersen AG, Jensen TK, Carlsen E, Jorgensen N, Andersson AM, Krarup T, et al. High frequency of sub-optimal semen quality in an unselected population of young men. Hum Reprod. 2000;15:366–72. doi: 10.1093/humrep/15.2.366. [DOI] [PubMed] [Google Scholar]
- 27.Bonde JP, Ernst E, Jensen TK, Hjollund NH, Kolstad H, Henriksen TB, et al. Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners. Lancet. 1998;352:1172–7. doi: 10.1016/S0140-6736(97)10514-1. [DOI] [PubMed] [Google Scholar]
- 28.Naysmith TE, Blake DA, Harvey VJ, Johnson NP. Do men undergoing sterilizing cancer treatments have a fertile future? Hum Reprod. 1998;13:3250–5. doi: 10.1093/humrep/13.11.3250. [DOI] [PubMed] [Google Scholar]
- 29.Willott GM. Frequency of azoospermia. Forensic Sci Int. 1982;20:9–10. doi: 10.1016/0379-0738(82)90099-8. [DOI] [PubMed] [Google Scholar]
- 30.Rueffer U, Breuer K, Josting A, Lathan B, Sieber M, Manzke O, et al. Male gonadal dysfunction in patients with Hodgkin’s disease prior to treatment. Ann Oncol. 2001;12:1307–11. doi: 10.1023/a:1012464703805. [DOI] [PubMed] [Google Scholar]
- 31.Blackhall FH, Atkinson AD, Maaya MB, Ryder WD, Horne G, Brison DR, et al. Semen cryopreservation, utilisation and reproductive outcome in men treated for Hodgkin’s disease. Br J Cancer. 2002;87:381–4. doi: 10.1038/sj.bjc.6600483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fitoussi O, Eghbali H, Tchen N, Berjon JP, Soubeyran P, Hoerni B. Semen analysis and cryoconservation before treatment in Hodgkin’s disease. Ann Oncol. 2000;11:679–84. doi: 10.1023/a:1008353728560. [DOI] [PubMed] [Google Scholar]
- 33.Carlsen E, Andersson AM, Petersen JH, Skakkebaek NE. History of febrile illness and variation in semen quality. Hum Reprod. 2003;18:2089–92. doi: 10.1093/humrep/deg412. [DOI] [PubMed] [Google Scholar]
- 34.Gandini L, Lombardo F, Salacone P, Paoli D, Anselmo AP, Culasso F, et al. Testicular cancer and Hodgkin’s disease: evaluation of semen quality. Hum Reprod. 2003;18:796–801. doi: 10.1093/humrep/deg163. [DOI] [PubMed] [Google Scholar]
- 35.van der Kaaij MA, Heutte N, Le Stang N, Raemaekers JM, Simons AH, Carde P, et al. Gonadal function in males after chemotherapy for early-stage Hodgkin’s lymphoma treated in four subsequent trials by the European Organization for Research and Treatment of Cancer: EORTC Lymphoma Group and the Groupe d’Etude des Lymphomes de l’Adulte. J Clin Oncol. 2007;25:2825–32. doi: 10.1200/JCO.2006.10.2020. [DOI] [PubMed] [Google Scholar]
- 36.Botchan A, Hauser R, Gamzu R, Yogev L, Lessing JB, Paz G, et al. Sperm quality in Hodgkin’s disease versus non-Hodgkin’s lymphoma. Hum Reprod. 1997;12:73–6. doi: 10.1093/humrep/12.1.73. [DOI] [PubMed] [Google Scholar]