There are limited data on survival patterns among patients with monoclonal gammopathy of undetermined significance (MGUS). In a study of 4,259 MGUS patients, the authors found that individuals diagnosed with MGUS in a clinical setting had a significantly reduced life expectancy. See related perspective article on page 1641.
Keywords: monoclonal gammopathy of undetermined significance, multiple myeloma, prognosis, survival, sex, older age, cause of death, population-based
Abstract
Background
There are limited data on survival patterns among patients with monoclonal gammopathy of undetermined significance.
Design and Methods
We compared the survival of 4,259 patients with monoclonal gammopathy of undetermined significance, collected from hematology outpatient units in Sweden, with the survival of the general population by computing relative survival ratios. We also compared causes of death in these patients with those in 16,151 matched controls.
Results
One-, 5-, 10-, and 15-year relative survival ratios were 0.98 (95% CI 0.97–0.99), 0.93 (0.91–0.95), 0.82 (0.79–0.84), and 0.70 (0.64–0.76), respectively. Younger age at diagnosis of the gammopathy was associated with a significantly lower excess mortality compared to that in older patients (p<0.001). The excess mortality among patients with gammopathy increased with longer follow-up (p<0.0001). IgM (versus IgG/A) gammopathy was associated with a superior survival (p=0.038). Patients with monoclonal gammopathy of undetermined significance had an increased risk of dying from multiple myeloma (hazards ratio (HR)=553; 95% CI 77–3946), Waldenström’s macroglobulinemia (HR=∞), other lymphoproliferative malignancies (6.5; 2.8–15.1), other hematologic malignancies (22.9; 8.9–58.7), amyloidosis (HR=∞), bacterial infections (3.4; 1.7–6.7), ischemic heart disease (1.3; 1.1–1.4), other heart disorders (1.5; 1.2–1.8), other hematologic conditions (6.9; 2.7–18), liver (2.1; 1.1–4.2), and renal diseases (3.2; 2.0–4.9).
Conclusions
Our finding of decreased life expectancy in patients with monoclonal gammopathy of undetermined significance, which was most pronounced in the elderly and explained by both malignant transformation and non-malignant causes, is of importance in the understanding and clinical management of this disease. The underlying mechanisms may be causally related to the gammopathy, but may also be explained by underlying disease that led to the detection of the hematologic disease. Our results are of importance since they give a true estimation of survival in patients with monoclonal gammopathy of undetermined significance diagnosed in clinical practice.
Introduction
Monoclonal gammopathy of undetermined significance (MGUS) is one of the most common pre-malignant conditions in western countries with a prevalence of 3.2% in the Caucasian general population 50 years of age or older.1 It is characterized by the presence of a monoclonal immunoglobulin (Ig) (M-protein) in individuals lacking evidence of multiple myeloma (MM) or other lymphoproliferative malignancies such as Waldenström’s macroglobulinemia (WM), primary amyloidosis, chronic lymphocytic leukemia (CLL), or B-cell lymphoma.2,3 A recent study based on 77,469 healthy adults enrolled in a nationwide population-based prospective cancer screening trial in the USA identified 71 individuals who developed MM during the course of the study. Using serially-collected pre-diagnostic serum samples obtained up to almost 10 years prior to the diagnosis of MM, all MM cases were found to have been preceded by MGUS.4 This finding establishes a key role for MGUS in the pathway to MM. Indeed, long-term follow-up of MGUS patients reveals an average 1% annual risk of developing lymphoproliferative malignancies.5,6 Additional data suggest that MGUS patients with an abnormal serum κ-λ free light chainratio, non-IgG MGUS and a high serum M-protein level (>1.5 g/dL) have a 58% absolute risk of developing MM at 20 years of follow-up, while, in sharp contrast, MGUS patients with none of these risk factors have only a 5% absolute risk of their disease progressing to MM.7 These observations show that the risk of MM progression among MGUS patients is highly heterogeneous and, in fact, the vast majority of MGUS patients will never develop a lymphoproliferative malignancy.7
Although there have been several investigations focusing on the risk of developing lymphoproliferative tumors following a diagnosis of MGUS,5–11 there are only limited data available on survival patterns among MGUS patients.5,6,10–12 Data from the Mayo Clinic showed that the median survival of MGUS patients was 8.1 years compared to 11.8 in the comparable US population.5 In a prior study from Denmark, 1,324 MGUS patients were found to have a 2-fold higher mortality compared to that of the general population.12 Similarly, a single center study from the Netherlands including 1,464 MGUS patients reported inferior survival among these patients than among a matched cohort without the disease.11
These and other smaller studies reported that the dominant causes of death among MGUS patients were hematologic malignancies, solid tumors, cardiovascular diseases, and infections.10,12,13 However, to our knowledge, no population-based, large study has been conducted to determine excess mortality patterns and simultaneously assess causes of death in MGUS patients compared to those in controls. Using population-based and hospital-based registries from Sweden, we identified a nationwide cohort of 4,259 MGUS patients diagnosed in 1986–2005. The aims of our study were to assess the patterns of survival among MGUS patients compared to the general population, and to classify and compare the causes of death in the MGUS patients and 16,151 matched controls.
Design and Methods
Patients and controls
Because MGUS is by definition an asymptomatic condition, it is usually diagnosed during a medical work-up for another cause. Consequently, in the general population, MGUS patients are identified within a broad range of medical specialties. In Sweden, a clinician who detects a patient with an M-protein will typically consult with a hematology specialist at a hospital-based center, and if needed, refer the patient for further work-up, especially to rule out an underlying malignancy.
MGUS is defined by the presence of a monoclonal immunoglobulin of less than 3 g/dL in serum, fewer than 10% plasma cells in the bone marrow, no evidence of other lymphoproliferative disorders, and the absence of clinical manifestations related to the monoclonal gammopathy.2 These criteria are essentially the same as those used in Swedish hospitals during the study period.
We established a nationwide MGUS cohort (as described in detail elsewhere)14 by retrieving information on all incident patients through a national network, which included all in- and outpatient units from major hospital-based hematology/oncology centers in Sweden. For all MGUS patients, we obtained information on sex, date of birth, date of diagnosis, and region/unit where the diagnosis was made. When available, we also collected information on MGUS subtype and concentration of the M-protein at diagnosis. In the present study, we included all MGUS patients diagnosed in outpatient units between 1986 and 2005. MGUS patients who were diagnosed with a previous hematologic malignancy or a lymphoproliferative malignancy within 6 months following the diagnosis of MGUS were excluded from the MGUS cohort. Follow-up commenced 6 months after the diagnosis of MGUS so patients who died within 6 months following the diagnosis were excluded from this study.
For each MGUS patient, four population-based controls (matched by sex, year of birth, and region) were chosen randomly from the Swedish Population database (cause of death analyses). All controls had to be alive at the time of diagnosis of MGUS in the corresponding case and not to have had a previous hematologic malignancy at the date of the corresponding case’s diagnosis.
Using the nationwide Cause of Death Registry, we obtained information on date and cause of death for all subjects (MGUS patients and controls) who had died up to December 31, 2006. We grouped causes of death into categories based on the International Classification of Diseases classification versions 9 and 10.
Approval was obtained from the Karolinska Institutional Review Board for this study. Informed consent was waived because we had no contact with study subjects. An exemption from Institutional Review Board review was obtained from the National Institutes of Health Office of Human Subjects Research because we used existing data without personal identifiers.
Statistical analysis
Relative survival ratios (RSR) were computed as measures of MGUS survival.15,16 RSR provide a measure of total excess mortality associated with a diagnosis of MGUS. One-, 5-, 10-, and 15-year RSR can be interpreted as the proportion of patients who survived their MGUS at 1, 5, 10, and 15 years, respectively. RSR is defined as the observed survival in the group of patients (in which all deaths are considered events) divided by the expected survival of a comparable group from the general population, which is assumed to be free of the condition in question. Expected survival was estimated using the Ederer II method17 from Swedish population life-tables stratified by age, sex, and calendar period.
One-, 5-, 10-, and 15-year RSR were calculated for two calendar periods: 1986–1995 and 1996–2005, and five age categories (<50, 50–59, 60–69, 70–79, and >80 years old). We constructed regression models with the goal of estimating the effect of the target factors previously defined in this article, while controlling for potential confounding factors. Poisson regression was used to model excess mortality.18 The estimates from this model are interpreted as excess mortality ratios; an excess mortality ratio of 1.5, for example, for males/females indicates that males experience 50% higher excess mortality than females.
We used Cox’s proportional hazards regression models to estimate the mortality rate ratio for each cause of death comparing MGUS patients to controls. A separate model was estimated for each cause of death. All calculations were performed using Stata version 10 (StataCorp 2007 Stata Statistical Software: Collage Station, TX, USA).
Results
Overall 4,259 MGUS patients (diagnosed 1986–2005) and 16,151 population-based controls were included in the study. The demographic and clinical characteristics of the MGUS patients and controls are shown in Table 1. The median age at diagnosis of MGUS was 70 years (range, 22–97 years). Among the MGUS patients, there were 1,822 (42.8%), 493 (11.6%), 523 (12.3%), and 2 (0.02%) diagnosed with MGUS subtypes IgG, IgA, IgM, and IgD, respectively. Information on MGUS subtype was missing for 1,419 patients (33.3%). Data on M-protein concentration were available for 2,436 (57.2%) patients; the median concentration was 0.8 g/dL (interquartile range, 0.5–1.5 g/dL). The median M-protein concentration was the same in the two calendar periods 1986–1995 and 1996–2005.
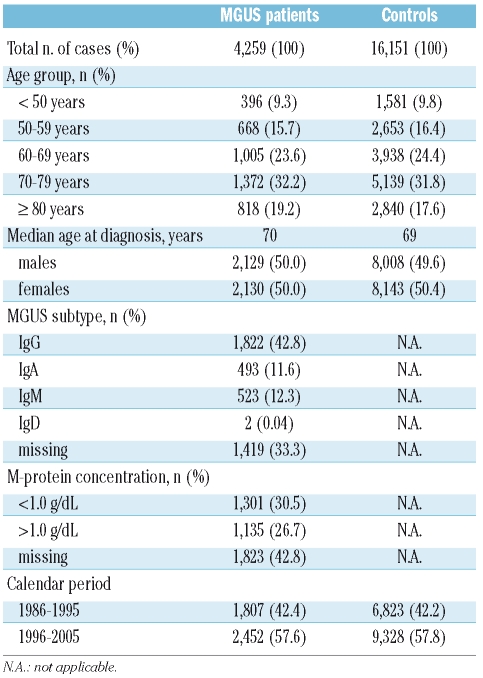
Table 1.
Characteristics of the MGUS patients and matched controls.
Patterns of survival
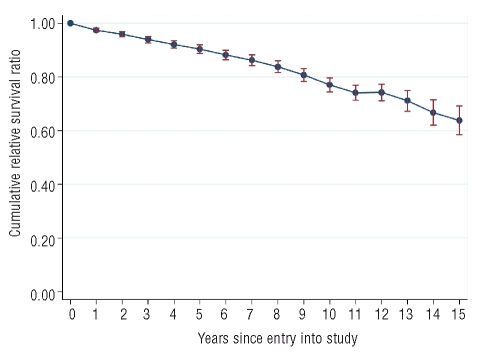
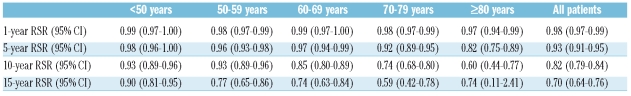
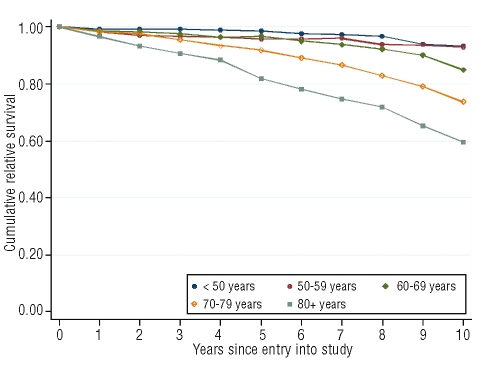
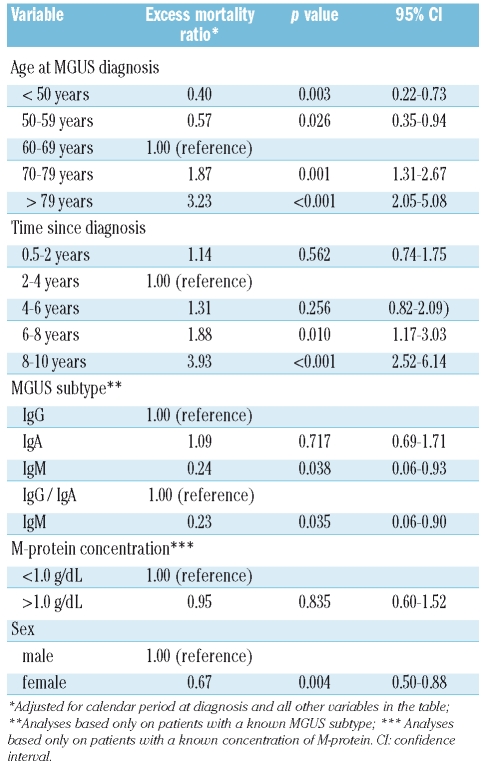
The median follow-up time was 5.6 years and 1,565 (37%) deaths were observed among the MGUS patients. When we estimated the cumulative RSR for the entire MGUS cohort, the 1-year, 5-year, 10-year, and 15-year RSR were 0.98 (95% CI 0.97–0.99), 0.93 (0.91–0.95), 0.82 (0.79–0.84), and 0.70 (0.64–0.76), respectively (Figure 1 and Table 2). When we evaluated survival patterns by age, we found that the youngest age category (<50 years) had 1-year, 5-year, 10-year, and 15-year RSR of 0.99 (95% CI 0.97–1.00), 0.98 (95% CI 0.96–1.00), 0.93 (95% CI 0.89–0.96), and 0.90 (95% CI 0.81–0.95), respectively (Figure 2 and Table 2). For the oldest age category (>80 years), the 1-year, 5-year, 10-year, and 15-year RSR were 0.97 (95% CI 0.94–0.99), 0.82 (95% CI 0.75–0.89), 0.60 (95% CI 0.44–0.77), and 0.74 (95% CI 0.11–2.41), respectively. Internal comparison analyses (Table 3) showed that younger age at the time of the MGUS being diagnosed was associated with a significantly lower excess mortality (p<0.001). The excess mortality among MGUS patients increased with a longer follow-up (p<0.001). We also found that IgM (versus IgG/A) MGUS was associated with a superior survival (p=0.038). However, we did not find any difference in survival in relation to M-protein concentration (above/below 1.0 g/dL or above/below 1.5 g/L). Even within each MGUS subtype (IgG, IgA, and IgM), there was no difference in survival in relation to M-protein concentration at diagnosis (Table 3). Finally, the evaluation of survival patterns by sex, showed that females had a lower excess mortality than males (Table 3).
Figure 1.
Relative survival ratios for MGUS patients.
Table 2.
One-, 5-, 10- and 15-year relative survival ratios (RSR) in 4,259 MGUS patients, stratified by age at diagnosis.
Figure 2.
Relative survival ratios for MGUS patients, stratified by age.
Table 3.
Excess mortality ratios and 95% CI during the first 10 years after MGUS diagnosis, by age at diagnosis, time since diagnosis, MGUS subtype, concentration of M-protein at diagnosis, and sex.
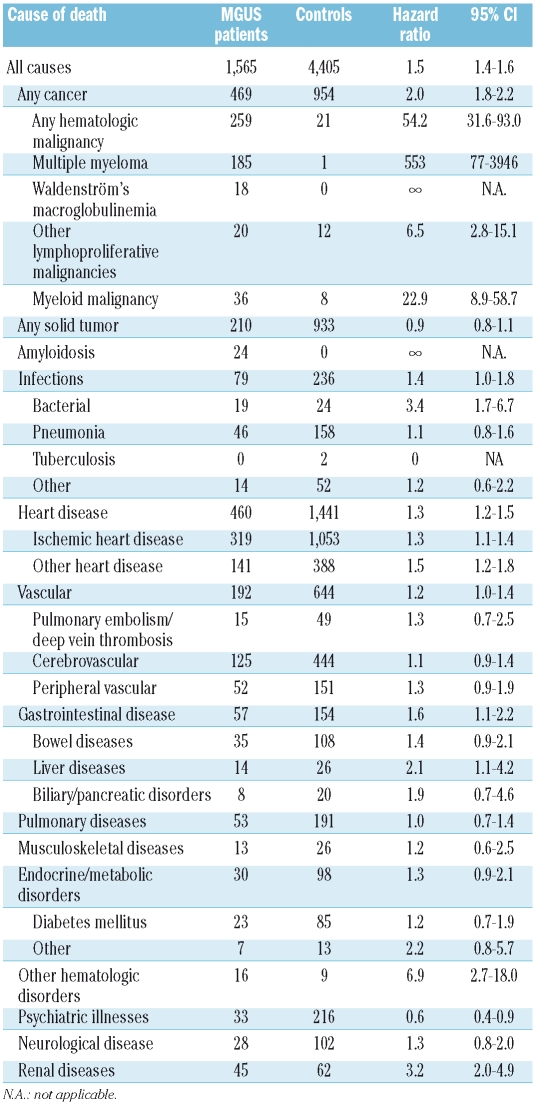
Causes of death
As shown in Table 4, compared to controls, MGUS patients had an increased risk of dying from MM (hazards ratio [HR]=553; 95% CI 77–3946), WM (18 cases and 0 controls, HR=infinity), other lymphoproliferative malignancies (HR=6.5; 95% CI 2.8–15.1) and other hematologic malignancies (most commonly, acute myeloid leukemia) (RR=22.9; 95% CI 8.9–58.7). However, there was no increased risk of dying from solid tumors (HR=0.9; 95% CI 0.8–1.1). Furthermore, compared to controls, we found that MGUS patients had an increased risk of dying of amyloidosis (24 cases and 0 controls, HR=infinity), bacterial infections (HR=3.4; 95% CI 1.7–6.7), ischemic heart disease (HR=1.3; 95% CI 1.1–1.4), other heart disorders (mainly congestive heart failure, heart valve diseases, cardiomyopathy, and arrhythmias) (HR=1.5; 95% CI 1.2–1.8), liver diseases (typically, liver failure and cirrhosis) (HR=2.1; 95% CI 1.1–4.2), other hematologic disorders (most frequently hemolytic anemia and aplastic anemia) (HR=6.9; 95% CI 2.7–18), and renal diseases (mainly renal failure and glomerular diseases) (HR=3.2; 95% CI 2.0–4.9) (Table 4).
Table 4.
Causes of death among MGUS patients and controls and hazard ratios and 95% CI as measures of excess risk of dying among MGUS patients versus controls.
When comparing causes of death stratified by age at diagnosis (below or above 60 years old), the risk estimates followed similar patterns as those resulting from the main analyses. We did, however, find a higher proportion of hematologic malignancies, amyloidosis, and liver disorders in younger MGUS patients than in older MGUS patients. We also found a higher proportion of heart disease and vascular disorders in older MGUS patients than in younger ones (data not shown). For example hematologic malignancy was the underlying cause of death in 35%, 34%, 22%, 16%, and 11% of the patients in the age categories under 50, 50–59, 60–69, 70–79, and over 79 years old, respectively, whereas heart disease was the underlying cause of death in 10%, 13%, 20%, 32%, and 35% in the corresponding age categories. The main causes of death according to MGUS subtype were essentially the same, except that MGUS patients who subsequently died from WM predominantly had IgM MGUS and those who died from MM typically had IgG/IgA MGUS. Causes of death were similar between the two calendar periods, 1986–1995 and 1996–2005 (data not shown).
Discussion
In this large nationwide study including more than 4,000 MGUS patients diagnosed in a clinical context at outpatient units in Sweden between 1986 and 2005, we show that individuals with MGUS have a poorer survival than the general population. In accordance with the literature,5,6 major causes of the observed excess mortality were MM, WM, and other lymphoproliferative diseases including amyloidosis. In addition, we found that MGUS patients had an increased risk of dying from myeloid malignancies, bacterial infections, heart diseases, liver disorders, and renal diseases. The explanations of our findings probably include a combination of pathogenic mechanisms related to MGUS as well as factors related to the underlying disease which led to medical work-up and detection of MGUS.
We found that 10 and 15 years after diagnosis, MGUS patients have RSR of 82% and 70%, respectively. Prior studies have also shown a lower life expectancy in MGUS patients;5,6,10–12,19,20 however, in none of these were causes of death among MGUS patients compared to those of matched controls. Our finding of an increasing excess mortality rate with time from diagnosis is novel and in contrast to the results of a study from Denmark.12 The discrepancy between these studies may involve selection mechanisms. Furthermore, we found that the excess mortality associated with having MGUS was four times higher after 8–10 years of follow-up than after 2–4 years.
Based on studies with long-term follow-up the main causes of deaths in MGUS patients are malignant diseases, cardiovascular and cerebrovascular diseases and infections.10,12,13 In our study, we confirmed that MGUS patients had an increased risk, compared to that of controls, of dying from lymphoproliferative disorders,5,6 and in addition we found an excess risk of death from myeloid malignancies (mainly acute myeloid leukemia) and a wide variety of non-malignant disorders.
Importantly, we found that the excess mortality among MGUS patients was strongly dependent on age at diagnosis, as had been observed in a Dutch11 but not in the Danish study.12 In our study, at 5 years of follow-up, younger MGUS patients had a RSR of 98%, while older (>80 years) MGUS patients had a 5-year RSR of 82%. The main causes of death in younger patients were lymphoproliferative malignancies, amyloidosis, and liver disorders, whereas cardiovascular diseases dominated in elderly MGUS patients. The observed age-related difference in survival patterns and causes of death may have implications for the management of MGUS, and support a risk-adapted strategy for follow-up and intervention in patients with this disease.
To our knowledge, we are the first to report that patients with IgM MGUS patients have a better survival than those with MGUS of the IgG and IgA subtypes. Schaar et al. did not observe any difference in survival by MGUS subtype.11 It was reported that the risk of malignant transformation was higher for IgM MGUS than for IgG MGUS.5 In our study, we found similar cause-of-death patterns by MGUS subtype, except that MGUS patients who subsequently died because of WM predominantly had IgM MGUS whereas those who died from MM typically had IgG/IgA MGUS. High M-protein concentration at diagnosis has been reported to predict a poorer outcome in MM and MGUS.5,6,9 We, however, in accordance with another study on MGUS,11 did not observe such an association between M-protein concentration at diagnosis and survival. Our study has several strengths, including its large size as well as the application of high-quality data from Sweden in a population with access to standardized universal medical health care during the entire study period.
Our study had a register-based cohort design, which ensured a population-based setting and generalization of our findings. As reported previously,21 the MGUS diagnoses in the study were established at hematology/oncology units, typically including a bone marrow examination. In addition, ascertainment and diagnostic accuracy for lymphoproliferative disorders is very high in Sweden.22
The limitations of the study include lack of information on potential confounders (although the matched design and analyses ensured adjustment for sex, age, and geography), and lack of detailed clinical data including co-morbidity. Because we did not screen for MGUS, we did not identify all MGUS cases in Sweden during the study period. Also, since our MGUS cases were defined in a clinical setting, they might have had higher M-protein concentrations than those of cases identified in a screening study. As already pointed out, the observed excess mortality among MGUS patients may, at least to a certain degree, reflect various underlying medical illnesses that contributed to the medical work-up eventually leading to the detection of MGUS. To better define the role of pathogenic mechanisms that are specific for MGUS and their influence on mortality, we are planning an MGUS screening-based mortality study. We believe that these two studies will provide different insights and shed light on clinical and scientific perspectives, respectively. To minimize such influences, MGUS patients with a diagnosis of a lymphoproliferative malignancy and/or who died within 6 months following the diagnosis of the MGUS were excluded from our analyses. Furthermore, we did not include patients diagnosed during an inpatient visit. There may be inaccuracies in the specified causes of death, which were based on death certificates. However, because we compared causes of death between cases and matched controls using data obtained from the same registries, the ascertainment should be non-differential and the relative risks should not be biased. An important aspect to bear in mind when interpreting our results is that we included MGUS patients diagnosed in an outpatient setting in standard clinical practice. Consequently, our findings are relevant to clinicians managing MGUS patients, since MGUS is associated with an excess mortality, not only restricted to MM and other lymphoproliferative disorders, but also to other non-malignant diseases. It cannot be ruled out that the observed increased risk of dying due to bacterial infections, renal, and heart diseases, at least in some cases, might be reflections of early MM, amyloidosis or another lymphoproliferative malignancy. This emphasizes how important it is that clinicians suspect a potential transformation to MM or another lymphoproliferative disorder when encountering new clinical signs or symptoms in a patient with MGUS.
In summary, we found that individuals diagnosed with MGUS in a clinical setting had a significantly reduced life expectancy. The rate of transformation of MGUS to MM or other lymphoproliferative diseases is 1% per year;5,6 however, the majority of MGUS patients are diagnosed as a result of a clinical investigation for different medical reasons, and were found to die from other causes. The observed excess mortality was particularly pronounced among elderly MGUS patients. Besides the well-known increased risk of dying from MM and other lymphoproliferative diseases, we found an excess risk of dying from bacterial infections, and heart, liver, and kidney diseases. Our findings show that a diagnosis of MGUS is of significance, not only with regard to the increased risk of malignant transformation but also with regard to an excess mortality from other causes. The observed cause-of-death patterns varied depending on the age of the patients at the time the diagnosis of MGUS was made, and this may have clinical implications. Future studies are needed to provide new insights into the pathogenesis of MGUS and find better predictors of the development of lymphoproliferative malignancies and other morbidities. It is to be hoped that such knowledge would lead to early actions to prevent or delay the progression of MGUS and complications of this disorder.
Acknowledgments
the authors thank Ms. Shiva Ayobi, The National Board of Health and Welfare, Stockholm, Sweden; Ms. Susanne Dahllöf, Statistics Sweden, Örebro, Sweden; and Ms. Charlotta Ekstrand, Ms. Molly Collin and Ms. Lisa Camner, Karolinska Institutet, Stockholm, Sweden, for invaluable ascertainment of MGUS data.
Footnotes
Funding: this research was supported by the Intramural Research Program of the NIH and the National Cancer Institute, and by grants from the Swedish Cancer Society, Stockholm County Council, and the Karolinska Institutet Foundations.
Authorship and Disclosures
SYK, MB, IT, and OL designed the study; SYK, MB, IT, and OL obtained data and initiated this work; TMLA, SE, and PWD performed all the statistical analyses. All the authors were involved in analysis and interpretation of the results; SYK and OL wrote the report. All authors read, gave comments, and approved the final version of the manuscript. All the authors had full access to the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
The authors reported no potential conflicts of interest.
References
- 1.Kyle RA, Therneau TM, Rajkumar SV, Larson DR, Plevak MF, Offord JR, et al. Prevalence of monoclonal gammopathy of undetermined significance. N Engl J Med. 2006;354:1362–9. doi: 10.1056/NEJMoa054494. [DOI] [PubMed] [Google Scholar]
- 2.Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. Br J Haematol. 2003;121:749–57. [No authors listed] [PubMed] [Google Scholar]
- 3.Kyle RA. Monoclonal gammopathy of undetermined significance. Natural history in 241 cases. Am J Med. 1978;64:814–26. doi: 10.1016/0002-9343(78)90522-3. [DOI] [PubMed] [Google Scholar]
- 4.Landgren O, Kyle RA, Pfeiffer RM, Katzmann JA, Caporaso NE, Hayes RB, et al. Monoclonal gammopathy of undetermined significance (MGUS) preceding multiple myeloma: a prospective study. Blood. 2009;113:5412–7. doi: 10.1182/blood-2008-12-194241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kyle RA, Therneau TM, Rajkumar SV, Offord JR, Larson DR, Plevak MF, et al. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med. 2002;346:564–9. doi: 10.1056/NEJMoa01133202. [DOI] [PubMed] [Google Scholar]
- 6.Kyle RA, Therneau TM, Rajkumar SV, Offord JR, Larson DR, Plevak MF, et al. Long-term follow-up of IgM monoclonal gammopathy of undetermined significance. Blood. 2003;102:3759–64. doi: 10.1182/blood-2003-03-0801. [DOI] [PubMed] [Google Scholar]
- 7.Rajkumar SV, Kyle RA, Therneau TM, Melton LJ, 3rd, Bradwell AR, Clark RJ, et al. Serum free light chain ratio is an independent risk factor for progression in monoclonal gammopathy of undetermined significance. Blood. 2005;106:812–7. doi: 10.1182/blood-2005-03-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kyle RA, Rajkumar SV, Therneau TM, Larson DR, Plevak MF, Melton LJ. 3rd. Prognostic factors and predictors of outcome of immunoglobulin M monoclonal gammopathy of undetermined significance. Clin Lymphoma. 2005;5:257–60. doi: 10.3816/clm.2005.n.011. [DOI] [PubMed] [Google Scholar]
- 9.Kyle RA, Remstein ED, Therneau TM, Dispenzieri A, Kurtin PJ, Hodnefield JM, et al. Clinical course and prognosis of smoldering (asymptomatic) multiple myeloma. N Engl J Med. 2007;356:2582–90. doi: 10.1056/NEJMoa070389. [DOI] [PubMed] [Google Scholar]
- 10.Kyle RA, Therneau TM, Rajkumar SV, Larson DR, Plevak MF, Melton LJ. 3rd. Long-term follow-up of 241 patients with monoclonal gammopathy of undetermined significance: the original Mayo Clinic series 25 years later. Mayo Clin Proc. 2004;79:859–66. doi: 10.4065/79.7.859. [DOI] [PubMed] [Google Scholar]
- 11.Schaar CG, le Cessie S, Snijder S, Franck PF, Wijermans PW, Ong C, Kluin-Nelemans H. Long-term follow-up of a population based cohort with monoclonal proteinaemia. Br J Haematol. 2009;144:176–84. doi: 10.1111/j.1365-2141.2008.07423.x. [DOI] [PubMed] [Google Scholar]
- 12.Gregersen H, Ibsen J, Mellemkjoer L, Dahlerup J, Olsen J, Sorensen HT. Mortality and causes of death in patients with monoclonal gammopathy of undetermined significance. Br J Haematol. 2001;112:353–7. doi: 10.1046/j.1365-2141.2001.02533.x. [DOI] [PubMed] [Google Scholar]
- 13.Pasqualetti P, Festuccia V, Collacciani A, Casale R. The natural history of monoclonal gammopathy of undetermined significance. A 5-to 20-year follow-up of 263 cases. Acta Haematol. 1997;97:174–9. doi: 10.1159/000203676. [DOI] [PubMed] [Google Scholar]
- 14.Kristinsson SY, Bjorkholm M, Goldin LR, McMaster ML, Turesson I, Landgren O. Risk of lymphoproliferative disorders among first-degree relatives of lymphoplasmacytic lymphoma/Waldenstrom macroglobulinemia patients: a population-based study in Sweden. Blood. 2008;112:3052–6. doi: 10.1182/blood-2008-06-162768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dickman PW, Adami HO. Interpreting trends in cancer patient survival. J Intern Med. 2006;260:103–17. doi: 10.1111/j.1365-2796.2006.01677.x. [DOI] [PubMed] [Google Scholar]
- 16.Henson DE, Ries LA. The relative survival rate. Cancer. 1995;76:1687–8. doi: 10.1002/1097-0142(19951115)76:10<1687::aid-cncr2820761002>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 17.Hakulinen T. Cancer survival corrected for heterogeneity in patient withdrawal. Biometrics. 1982;38:933–42. [PubMed] [Google Scholar]
- 18.Dickman PW, Sloggett A, Hills M, Hakulinen T. Regression models for relative survival. Stat Med. 2004;23:51–64. doi: 10.1002/sim.1597. [DOI] [PubMed] [Google Scholar]
- 19.Blade J, Lopez-Guillermo A, Rozman C, Cervantes F, Salgado C, Aguilar JL, et al. Malignant transformation and life expectancy in monoclonal gammopathy of undetermined significance. Br J Haematol. 1992;81:391–4. doi: 10.1111/j.1365-2141.1992.tb08245.x. [DOI] [PubMed] [Google Scholar]
- 20.van de Poel MH, Coebergh JW, Hillen HF. Malignant transformation of monoclonal gammopathy of undetermined significance among out-patients of a community hospital in southeastern Netherlands. Br J Haematol. 1995;91:121–5. doi: 10.1111/j.1365-2141.1995.tb05256.x. [DOI] [PubMed] [Google Scholar]
- 21.Landgren O, Kristinsson SY, Goldin LR, Caporaso NE, Blimark C, Mellqvist UH, et al. Risk of plasma cell and lymphoproliferative disorders among 14621 first-degree relatives of 4458 patients with mono-clonal gammopathy of undetermined significance in Sweden. Blood. 2009;114:791–5. doi: 10.1182/blood-2008-12-191676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Turesson I, Linet MS, Björkholm M, Kristinsson SY, Goldin LR, Caporaso NE, et al. Ascertainment and diagnostic accuracy for hematopoietic lymphoproliferative malignancies in Sweden 1964–2003. Int J Cancer. 2007;121:2260–6. doi: 10.1002/ijc.22912. [DOI] [PubMed] [Google Scholar]