Abstract
Objective
To examine the relative validity of two Food Frequency Questionnaires (FFQs) developed for use in investigating diet and disease relationships within the adult African American population in the southern United States.
Design
Cross-sectional analyses of dietary nutrient intake data, comparing four 24-hour dietary recalls with a FFQ developed by the Lower Mississippi Delta Nutrition Intervention Research Initiative (Delta NIRI), and its shorter version adapted for use in the Jackson Heart Study (JHS).
Subjects
A representative subset of participants (n=499, 35-81 y) from the baseline JHS cohort (N=5,302) was selected for this study. Data collection took place between winter of 2000 and spring of 2004.
Statistical Analyses
Pearson's correlation coefficients (energy adjusted and de-attenuated) for 26 nutrients estimates from each of the FFQs, comparing them with the mean of four 24-hour dietary recalls. The ability of the FFQs to rank individuals based on nutrient intakes was compared to that of the mean of four 24-hour dietary recalls and attenuation coefficients were also calculated.
Results
Median nutrient intake estimates tended to be higher on the long and lower on the short FFQ compared to the median for the mean of four 24-hour dietary recalls. Energy adjusted and de-attenuated correlations of FFQ intake estimates with recalls ranged from 0.20 for sodium to 0.70 for carbohydrate for the short FFQ and from 0.23 for polyunsaturated fat to 0.75 for dietary fiber and magnesium for the long. Attenuation coefficients for men on average were 0.42 for the short and 0.49 for the long FFQ. For women, these were 0.31 for the short and 0.42 for the long FFQ.
Conclusions
Both FFQs appear to be reasonably valid for assessment of dietary intake of adult African Americans in the South. The Delta NIRI FFQ exhibited higher intake estimates and stronger correlations with recalls than the JHS FFQ for most nutrients analyzed, more so for women than men.
Keywords: Food Frequency Questionnaire, Dietary Recalls, Validation, African Americans, Diet
INTRODUCTION
The Jackson Heart Study (JHS) is a single site, longitudinal cohort study located in Jackson, Mississippi, with a mission to investigate risk factors associated with coronary vascular disease in African American populations. Investigation of diet as a chronic disease risk factor requires culturally sensitive and valid measurement instruments (1-6). Because an appropriate diet assessment tool could not be found at the initiation of the study, a new FFQ (7) that was previously created for use in assessing the diet of the Southern US population was used as a dietary assessment tool in the JHS (8). The Diet and Physical Activity Sub-Study (DPASS), a sub-study within the JHS was conducted to examine the validity of the dietary assessment instruments used in the JHS.
FFQs allow for assessment of the usual patterns of food intake over an extended period of time (9). They can also capture past dietary intake patterns and are considerably less expensive in both time and cost in comparison to other measurement tools which is an important consideration in studies involving large cohorts (10, 11). FFQs rely on recall from ‘generic’ memory, which may be more easily recalled than ‘episodic’ memory and are widely used dietary assessment tools and are vital to nutrition research, but because of the importance of cultural sensitivity, all require some adjustments and validation when used for a select cultural group (12). Measurement errors can adversely affect results arising from studies examining diet and disease associations (13). Thus, validation and calibration are both considered critical to the success of FFQs in accurately measuring dietary intake in subgroups of the population (9, 14).
The objectives of validation and calibration studies are to compare a new instrument against an accepted measure, and to quantify the measurement error (15). Validation of a FFQ refers to the degree to which the questionnaire measures the aspect of diet it was designed to measure (16). Calibration refers to the process whereby adjustments are made to measurements obtained using the FFQ, based on comparison with a more superior method, so as to obtain relatively unbiased estimates (16, 17). Factors affecting validity include respondent characteristics, questionnaire design and quantification, quality control, and the adequacy of the reference data. Because no gold standard is usually available, FFQs are most often compared with multiple 24-hour dietary recalls or diet records as the reference.
In this study, nutrient intakes assessed by the Delta Nutrition Intervention Research Initiative (NIRI) FFQ for use with African American adults in a Southern US population, as well as a shortened version of the questionnaire, were compared with four 24- hour dietary recalls. The overall goal of the study was to validate the two regionally specific FFQs against four 24- hour recalls.
SUBJECTS AND METHODS
Study Population
The men and women in this cross-sectional analysis were participants of the DPASS of the JHS. The JHS is a single-site prospective epidemiological investigation of cardiovascular disease among African-Americans from the Jackson, Mississippi metropolitan area. The JHS study design initially included participants from the Jackson cohort of the Atherosclerosis Risk in Communities study (18), a random component, a family component and later (in order to meet recruitment goals) a structured volunteer sample. Overall, 3,395 females and 1,907 males, with a mean age of 55 y, completed the baseline visit. Data collection for the JHS began in late 2000 and ended in early 2004. A more detailed description of the original study has been published elsewhere (19, 20) Study Design
A subset of participants (n=499) from the JHS cohort (N=5,302) was selected for the DPASS. The aim of DPASS was to provide data for validation of the diet and physical activity instruments used for the entire cohort of the JHS. DPASS investigators identified potential participants for DPASS based on specified criteria. The goal for recruitment for the DPASS was to include an equal number of men and women from younger (34-64 y) and older (65 y and older) age groups, from lower and higher socioeconomic status, and from lower and higher physical activity groups. Pre-screening for these enrollment criteria was conducted with data collected during the home induction visit. Details on this process have been published previously (8).
Participants who agreed to be part of the DPASS underwent extensive dietary assessment interviews. These included administration of the Delta NIRI JHS FFQ (a categorical subset of the Delta NIRI FFQ) during the initial clinic visit, followed by four 24-hour dietary recalls scheduled a month apart on average starting from a month after the initial clinic visit. Lastly, a week after administration of the last recall, participants were administered the original Delta NIRI FFQ. Although it was recognized that a random assignment to Delta NIRI JHS vs. Delta NIRI FFQs at the beginning and end would be an optimal design, the flow of the JHS research did not allow this. Rather, all participants in the JHS completed the Delta NIRI JHS FFQ as part of the standard data collection and a subset were then enrolled into DPASS. Protocols for both the JHS and the DPASS were approved by the University of Mississippi Medical Center's Institutional Review Board. All participants gave written informed consent prior to enrollment.
Twenty-four hour dietary recalls
The four 24-hour dietary recalls were scheduled approximately one month apart from each other, generally over a six month period. These were collected on a rolling basis, similar to admission to the DPASS. A participant was required to provide information on two week and two weekend days.
All dietary recalls were administered, by registered dietitians, who had been trained and certified to use the University of Minnesota Nutrition Data System for Research (NDS-R), version 4.04, 2001 (Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN) software used to collect the dietary recall information. All recalls were audio-taped allowing for immediate review of the entries. Five percent of these recordings were randomly selected for a second round of quality control checks by the principal investigator of the DPASS (8).
Food frequency questionnaires
Two FFQs were used to capture the dietary intake of the DPASS participants. The Delta NIRI JHS FFQ (short FFQ) is a 158 item questionnaire administered by trained JHS clinic staff to all participants of the JHS on the day of their clinic visit. The Delta NIRI FFQ (long FFQ) is a 283 item interviewer administered questionnaire that was completed one week after the last 24-hour dietary recall, from participants of the DPASS only.
The FFQs used in the JHS and DPASS cohorts were developed specifically for use in a southern population. Details regarding the development of the 283 item Delta NIRI FFQ have been published (7). Briefly, the FFQ was created using data from 24-hour dietary recalls administered to African American and white adults in the lower Mississippi Delta region in the year 2000. The methodology used for the development of this questionnaire was similar to the one used to create the modified 1989 NCI-Block FFQ (21), on which it was based. Foods that contributed at least 0.5 % to nutrients examined were included in the FFQ food list. Some of the regional foods that were included in the food list for the FFQ included foods such as grits, ham hocks, crawfish etc. The FOODS 2000 data revealed that there was tremendous variation in reported portion sizes. Therefore, four options for portion sizes were included on the FFQ. The medium size was based on the mode or the median of the FOODS 2000 data; the small portion was half the medium, the large portion was one and a half times the medium and the extra large was defined as twice or more of the medium serving size. The short FFQ was a categorical subset of the long FFQ, shortened to fit the time requirements of the JHS protocol, which allowed only 20 minutes for dietary assessment. This FFQ was designed to include all foods on the longer FFQ, by collapsing similar foods to combine line items and simplifying adjustment questions. The University of Minnesota Nutrition Data System for Research (NDS-R), version 5.0-35, 2004 (Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN) software was used to create the FFQ and recall database.
Both the FFQs were interviewer administered. The JHS clinical staff administered the short FFQ, while DPASS registered dietitians administered the long FFQ. Interviewers of the short FFQ were trained to administer the questionnaire in 20-25 minutes. Administration of the short FFQs was timed and if the timing exceeded the allotted, re-training was conducted. Quality control checks were performed on both the short and the long FFQs. Similar to quality controls performed on the 24-hour dietary recalls, 5% of all the FFQ administrations were audio-taped and reviewed by the DPASS staff. Re-training of the clinical staff was conducted if errors in accuracy of the interviews were identified by the DPASS staff. Both of these FFQs are available upon request from the corresponding author.
Assessment of Covariates
Information on age, smoking status, and education level was collected by questionnaire at either the home induction visit or at the time of the participant's clinic visit. The variable on education level was based on a similar question that was present on the questionnaire administered at the home induction visit. The variable on smoking status was created using questions on cigarette smoking, specifically if the participant had smoked at least 400 cigarettes in his/her lifetime and if they smoked cigarettes currently. Participant height and weight were measured using physician quality measurement scales in an exam gown with no shoes by trained technicians at the clinic visit. Weight and height scales were of the Health o meter brand (model # 402KLS) obtained from Jarden Consumer Solutions (Florida, USA). Detailed information regarding the procedures used for the anthropometric procedures conducted at the clinic visit have been published elsewhere (20). Body Mass Index (BMI) was calculated as weight/height2 (kg/m2).
Statistical Analyses
DPASS participants who did not have either of the FFQs or less than four 24-hour dietary recalls (n=12) were excluded. Participants who reported energy intake outside the plausible range (≤ 600 or ≥ 4000 kcal/d) on any of the FFQs or on the mean of the four 24-hour dietary recalls (n=46), were excluded. Participants who had 5 or more questions on food items missing on the FFQs (n=5) were excluded from analyses resulting in a sample of 436 individuals.
Descriptive analyses were used to assess the demographics of the study population. Median intakes of 26 nutrients were calculated. All nutrients were log transformed prior to analyses. Nutrients (except energy) from each of the dietary assessment instruments that were studied were adjusted for energy intake from the same instrument using residual analyses. Reasons for energy adjustment have been described previously (22). Pearson correlations were computed to assess the associations between nutrient intakes as assessed by each of the FFQs and the mean of the 24-hour dietary recalls. Correlations between nutrients across instruments are a well accepted method for establishing the relative validity of FFQs. Day-to-day within person variation in the reference method (mean of the four 24-hour dietary recalls) can attenuate the correlations between nutrient intakes derived from the FFQs and the mean of the dietary recalls. The intra to inter-person variance for the nutrient intakes as estimated by the four 24-hour dietary recalls were also calculated and reviewed. The formula expressed below was used to calculate the de-attenuated correlation coefficients: rt = ro √(1+intrax/interx/nx), where ro is the observed correlation coefficient between the nutrient intake as determined from the mean of the four 24-hour dietary recalls and the FFQs, intrax is the intra-subject variation, interx is the inter-subject component of variance for each nutrient and nx is the number of days of dietary recalls, which in the present study was four days (23). Attenuation factors, which are equivalent to the slope of the linear regression of the mean of the 24-hour dietary recalls on each of the FFQs were also calculated for the energy adjusted transformed nutrients (24).
The ability of both the FFQs to rank dietary intakes of individuals in the population as compared to the mean of the recalls was also calculated. And lastly, Bland Altman plots were also examined to obtain a visual comparison of assessment using each of the FFQs and the mean of the four 24-hour dietary recalls (25). All analyses were conducted using SAS (SAS version 9.1, 2002-2003, SAS Institute, Cary, NC). Alpha for all analyses was set at the 0.05 level.
RESULTS
Of the 436 participants eligible for analysis, more than 60% (n=273) were women. Ages ranged between 35-81 y and did not differ significantly between men and women. (Table1). Mean age adjusted BMI was higher for women than men (32 vs. 29 kg/m2, P < 0.05). A lower percentage of women than men were current smokers (P < 0.05).
Table 1.
Demographic characteristics of participants in the Jackson Heart Study Diet and Physical Activity Sub-Study
| Characteristics | Men (n=163) | Women (n=273) |
|---|---|---|
| Agea (n=436) | 60.1(0.76) | 61.4 (0.58) |
| Body Mass Indexa,b, kg/m2 (n=435) | 29.4 (0.51) | 31.9 (0.39)* |
| Smoking Statusa, % (n=436) | ||
| Never | 51.5 | 74.7 |
| Former | 35.6 | 18.7 |
| Current | 12.9 | 6.6* |
| Educationa, % (n=433) | ||
| <12y | 19.9 | 16.5 |
| High School Diploma or GEDc | 20.5 | 19.1 |
| Vocational Degree or College with no degree | 13.7 | 18.4 |
| Associates/Bachelor's/Professional degree | 46.0 | 46.0 |
Values are Means (Standard Error of Mean) or Percentage for categorical data
Sex groups were compared by General Linear Models, adjusting for age
GED: General Education Development certificate
Different from men: P < 0.05
Median dietary intakes of the 26 nutrients estimated by the two FFQs and the mean of four 24-hour recalls are shown in Table 2. For illustration, median values for the FFQ that were 15% higher or lower than those reported for the recalls have been marked by a “¶”. Both FFQs appeared to overestimate vitamins C and B12 for men and women relative to the 24-hour recalls. For men, calcium intake was higher from both FFQs, vitamin A and folate was higher from the short FFQ and vitamin D by the long. For women, both FFQs estimated higher intakes of poly-unsaturated fat, vitamin D and sodium intakes. The long FFQ also estimated higher calcium, iron and zinc in women relative to the 24 hour recalls. Folate intakes were lower from the short FFQ than from the dietary recalls, in both women and men.
Table 2.
Median (25th, 75th Percentiles) dietary nutrient intakes of the participants in the Jackson Heart Study Diet and Physical Activity Sub-Study as measured by the dietary assessment instruments used in the study
| Nutrient | Men | Women | ||||
|---|---|---|---|---|---|---|
| Recalls | Short FFQa | Long FFQa | Recalls | Short FFQa | Long FFQa | |
| Energy (kcal) | 1985 (1645, 2407) |
1973 (1487, 2584) |
2018 (1488, 2670) |
1568 (1267, 1941) |
1647 (1272, 2149) |
1688 (1336, 2091) |
| Protein (g) | 80.1 (63.7, 98.8) |
72.5 (53.8, 94.9) |
74.2 (59.2, 95.3) |
59.4 (48.0, 73.3) |
55.6 (42.5, 76.6) |
61.2 (47.3, 77.8) |
| Carbohydrate (g) | 237 (188, 287) |
249 (186, 313) |
261 (198, 322) |
204 (163, 253) |
218 (169, 288) |
221 (171, 276) |
| Fat (g) | 78.5 (57.7, 97.4) |
73.4 (54.5, 110.8) |
76.8 (58.1,106.4) |
59.4 (48.0, 73.3) |
59.7 (43.8, 82.7) |
64.5 (48.3, 82.7) |
| Saturated fat (g) | 23.3 (16.6, 30.0) |
22.5 (15.3, 33.2) |
24.9 (16.5, 32.1) |
18.0 (14.1, 23.7) |
18.5 (13.0, 26.4) |
19.3 (14.3, 25.8) |
| Monounsaturated fat (g) | 31.6 (23.8, 39.5) |
28.5 (19.9, 40.8) |
29.6 (22.4, 40.7) |
24.1 (18.0, 31.9) |
22.1 (16.1, 31.0) |
25.0 (18.3, 32.6) |
| Polyunsaturated fat (g) | 15.2 (11.7, 20.1) |
16.4 (12.2, 23.9) |
17.1 (12.4, 23.6) |
12.0 (8.9, 16.8) |
14.0¶ (10.0, 19.9) |
14.4¶ (10.8, 19.1) |
| Cholesterol (mg) | 334 (233, 438) |
334 (206, 461) |
335 (233, 502) |
218 (161, 312) |
233 (157, 353) |
233 (168, 337) |
| Dietary Fiber (g) | 15.9 (11.0, 20.6) |
15.6 (12.0, 20.2) |
16.9 (12.6, 22.3) |
14.0 (10.4, 18.3) |
13.5 (10.6, 16.6) |
15.0 (12.0, 19.7) |
| Vitamin A (mcg REb) | 884 (591, 1586) |
1077¶ (773, 1279) |
999 (796, 1341) |
827 (556, 1231) |
863 (654, 1145) |
908 (677, 1198) |
| Vitamin E (mg of alpha tocopherol) | 6.29 (4.60, 8.28) |
6.59 (4.74, 8.85) |
6.52 (4.90, 9.35) |
5.37 (4.06, 7.13) |
5.61 (4.21, 7.99) |
5.83 (4.52, 7.93) |
| Vitamin D (mcg of calciferol) | 4.12 (2.59, 5.86) |
4.73 (3.43, 7.13) |
4.92¶ (3.36, 7.18) |
2.82 (1.98, 4.33) |
3.48¶ (2.33, 4.94) |
3.67¶ (2.58, 5.15) |
| Vitamin C (mg) | 80 (51, 131) |
98¶ (69, 145) |
98¶ (63, 147) |
84 (56, 124) |
100¶ (73, 142) |
103¶ (64, 144) |
| Folate (mcg) | 385 (299, 510) |
296¶ (229, 377) |
334 (247, 421) |
326 (255, 414) |
252¶ (193, 310) |
285 (226, 359) |
| Thiamin (mg) | 1.69 (1.30, 2.11) |
1.70 (1.27, 2.04) |
1.79 (1.33, 2.26) |
1.33 (1.06, 1.69) |
1.34 (0.98, 1.73) |
1.43 (1.13, 1.86) |
| Riboflavin (mg) | 1.75 (1.36, 2.19) |
1.79 (1.35, 2.35) |
1.90 (1.46, 2.43) |
1.42 (1.11, 1.78) |
1.38 (1.05, 1.87) |
1.47 (1.15, 1.90) |
| Niacin (mg) | 22.4 (17.3, 27.6) |
19.6 (14.9, 25.9) |
21.3 (16.2, 28.8) |
16.6 (13.2, 21.3) |
15.2 (11.8, 20.8) |
17.7 (13.6, 22.8) |
| Vitamin B6 (mg) | 1.81 (1.30, 2.31) |
1.79 (1.30, 2.18) |
1.94 (1.45, 2.53) |
1.48 (1.09, 1.80) |
1.42 (1.10, 1.82) |
1.65 (1.26, 2.13) |
| Vitamin B12 (mcg) | 4.06 (2.55, 5.65) |
5.31¶ (3.67, 7.93) |
5.27¶ (3.84, 7.30) |
2.65 (2.00, 3.96) |
3.92¶ (2.85, 5.95) |
4.21¶ (2.82, 5.74) |
| Calcium (mg) | 605 (452, 772) |
735¶ (540, 954) |
702¶ (550, 961) |
538 (408, 707 ) |
591 (466, 799) |
659¶ (480, 860) |
| Iron (mg) | 14.5 (11.0, 17.4) |
14.9 (11.2, 19.5) |
16.0 (11.9, 20.0) |
11.2 (8.7, 13.8) |
12.0 (8.9, 15.4) |
12.9¶ (10.4, 16.7) |
| Magnesium (mg) | 263 (203, 331) |
285 (216, 357) |
291 (232, 375) |
223 (175, 272) |
245 (195, 310) |
254 (209, 322) |
| Phosphorus (mg) | 1140 (926, 1480) |
1196 (895, 1585) |
1261 (986, 1552) |
911 (722, 1151) |
949 (746, 1293) |
1026 (832, 1284) |
| Zinc (mg) | 10.1 (7.9, 12.9) |
11.0 (7.9, 14.1) |
10.7 (8.5, 14.8) |
7.5 (5.9, 9.7) |
8.4 (5.9, 11.4) |
9.1¶ (7.0, 11.7) |
| Potassium (mg) | 2448 (1887, 3003) |
2699 (2073, 3286) |
2655 (2126, 3378) |
2129 (1672, 2557) |
2282 (1799, 2855) |
2286 (1838, 2879) |
| Sodium (mg) | 3282 (2533, 4156) |
3737 (2833, 4922) |
3578 (2661, 4652) |
2467 (1972, 3150) |
3081¶ (2197, 4371) |
2848¶ (2186, 3661) |
FFQ: Food Frequency Questionnaire
RE: Retinol Equivalents
The FFQ value is >15% different than the value of the median values for the average of the four 24-hour dietary recalls
Energy adjusted and de-attenuated correlations for macronutrient intakes between the short FFQ and dietary recalls ranged from 0.33 for poly-unsaturated fat to 0.70 for carbohydrate intake in men and 0.30 for poly-unsaturated fat to 0.49 for cholesterol intake in women (Table 3). For the long FFQ, these correlations with recalls for men ranged from 0.27 for poly-unsaturated fat to 0.75 for dietary fiber in men; and from 0.23 for poly-unsaturated fat to 0.61 for cholesterol intake in women. For women, long FFQ correlations were stronger than short FFQ correlations for all macronutrients except polyunsaturated fat. In contrast, for men several of the energy adjusted, de-attenuated macronutrient correlations with dietary recalls were higher for the short vs. the long FFQ. Exceptions were protein, cholesterol and dietary fiber where the long FFQ correlations with dietary recalls were greater than the short FFQ.
Table 3.
Pearson's correlations for energy and macronutrient intakes between the Food Frequency Questionnaires and the mean of four 24-hour dietary recalls for the participants in the Jackson Heart Study Diet and Physical Activity Sub-Study
| Nutrient | Men | Women | ||
|---|---|---|---|---|
| Short FFQa | Long FFQa | Short FFQa | Long FFQa | |
| Energy | 0.35 | 0.32 | 0.29 | 0.28 |
| De-attenuated | 0.41 | 0.38 | 0.33 | 0.33 |
| Protein | ||||
| Energy adjusted | 0.31 | 0.36 | 0.30 | 0.41 |
| Energy adjusted & de-attenuated | 0.39 | 0.45 | 0.37 | 0.50 |
| Carbohydrate | ||||
| Energy adjusted | 0.61 | 0.58 | 0.38 | 0.45 |
| Energy adjusted & de-attenuated | 0.70 | 0.67 | 0.44 | 0.53 |
| Fat | ||||
| Energy adjusted | 0.40 | 0.37 | 0.32 | 0.36 |
| Energy adjusted & de-attenuated | 0.49 | 0.46 | 0.39 | 0.44 |
| Saturated fat | ||||
| Energy adjusted | 0.45 | 0.42 | 0.29 | 0.45 |
| Energy adjusted & de-attenuated | 0.54 | 0.50 | 0.36 | 0.57 |
| Monounsaturated fat | ||||
| Energy adjusted | 0.41 | 0.37 | 0.28 | 0.34 |
| Energy adjusted & de-attenuated | 0.52 | 0.47 | 0.35 | 0.42 |
| Polyunsaturated fat | ||||
| Energy adjusted | 0.24 | 0.21 | 0.23 | 0.18 |
| Energy adjusted & de-attenuated. | 0.33 | 0.27 | 0.30 | 0.23 |
| Cholesterol | ||||
| Energy adjusted | 0.36 | 0.50 | 0.36 | 0.44 |
| Energy adjusted & de-attenuated | 0.46 | 0.65 | 0.49 | 0.61 |
| Dietary Fiber | ||||
| Energy adjusted | 0.35 | 0.60 | 0.36 | 0.47 |
| Energy adjusted & de-attenuated | 0.43 | 0.75 | 0.44 | 0.57 |
FFQ: Food Frequency Questionnaire
Energy adjusted and de-attenuated correlations for dietary vitamin and mineral intakes between the short FFQ and recalls ranged from 0.20 for sodium to 0.60 for magnesium for men and from 0.23 for zinc and sodium to 0.55 for magnesium for women. For the long FFQ, these ranged from 0.33 for sodium to 0.75 for magnesium for men and from 0.24 for vitamin A to 0.69 for magnesium for women. For both men and women, the long FFQ exhibited higher correlations with recalls than for most micronutrients as compared to the short FFQ. Exceptions included vitamins A, D, and C where correlations were comparable for both the FFQs for men; and vitamin A where correlations were higher with the short, and vitamin E, where they were comparable for both FFQs, for women (Table 4).
Table 4.
Pearson's correlations for dietary vitamin and mineral intakes between the Food Frequency Questionnaires and the mean of four 24-hour dietary recalls for the participants in the Jackson Heart Study Diet and Physical Activity Sub-Study
| Nutrient | Men | Women | ||
|---|---|---|---|---|
| Short FFQa | Long FFQa | Short FFQa | Long FFQa | |
| Vitamin A | ||||
| Energy adjusted | 0.33 | 0.33 | 0.19 | 0.16 |
| Energy adjusted & de-attenuated | 0.42 | 0.43 | 0.27 | 0.24 |
| Vitamin E | ||||
| Energy adjusted | 0.21 | 0.32 | 0.26 | 0.26 |
| Energy adjusted & de-attenuated | 0.27 | 0.41 | 0.33 | 0.33 |
| Vitamin D | ||||
| Energy adjusted | 0.37 | 0.37 | 0.27 | 0.41 |
| Energy adjusted & de-attenuated | 0.49 | 0.48 | 0.36 | 0.57 |
| Vitamin C | ||||
| Energy adjusted | 0.44 | 0.45 | 0.35 | 0.47 |
| Energy adjusted & de-attenuated | 0.55 | 0.56 | 0.49 | 0.65 |
| Folate | ||||
| Energy adjusted | 0.35 | 0.43 | 0.33 | 0.38 |
| Energy adjusted & de-attenuated | 0.44 | 0.54 | 0.44 | 0.50 |
| Thiamin | ||||
| Energy adjusted | ||||
| 0.34 | 0.48 | 0.26 | 0.36 | |
| Energy adjusted & de-attenuated | ||||
| 0.45 | 0.64 | 0.34 | 0.46 | |
| Riboflavin | ||||
| Energy adjusted | 0.48 | 0.51 | 0.33 | 0.47 |
| Energy adjusted & de-attenuated | 0.59 | 0.62 | 0.40 | 0.58 |
| Niacin | ||||
| Energy adjusted | 0.43 | 0.46 | 0.26 | 0.31 |
| Energy adjusted & de-attenuated | 0.55 | 0.59 | 0.34 | 0.40 |
| Vitamin B6 | ||||
| Energy adjusted | 0.39 | 0.55 | 0.32 | 0.48 |
| Energy adjusted & de-attenuated | 0.49 | 0.70 | 0.40 | 0.59 |
| Vitamin B12 | ||||
| Energy adjusted | 0.29 | 0.36 | 0.18 | 0.35 |
| Energy adjusted & de-attenuated | 0.40 | 0.49 | 0.27 | 0.51 |
| Calcium | ||||
| Energy adjusted | 0.38 | 0.45 | 0.38 | 0.44 |
| Energy adjusted & de-attenuated | 0.48 | 0.57 | 0.49 | 0.56 |
| Iron | ||||
| Energy adjusted | 0.46 | 0.59 | 0.31 | 0.40 |
| Energy adjusted & de-attenuated | 0.57 | 0.73 | 0.37 | 0.49 |
| Magnesium | ||||
| Energy adjusted | 0.51 | 0.64 | 0.47 | 0.59 |
| Energy adjusted & de-attenuated | 0.60 | 0.75 | 0.55 | 0.69 |
| Phosphorus | ||||
| Energy adjusted | 0.37 | 0.47 | 0.32 | 0.50 |
| Energy adjusted & de-attenuated | 0.47 | 0.59 | 0.40 | 0.62 |
| Zinc | ||||
| Energy adjusted | 0.25 | 0.46 | 0.18 | 0.32 |
| Energy adjusted & de-attenuated | 0.35 | 0.64 | 0.23 | 0.41 |
| Potassium | ||||
| Energy adjusted | 0.30 | 0.50 | 0.34 | 0.49 |
| Energy adjusted & de-attenuated | 0.37 | 0.61 | 0.40 | 0.58 |
| Sodium | ||||
| Energy adjusted | 0.16 | 0.26 | 0.19 | 0.21 |
| Energy adjusted & de-attenuated | 0.20 | 0.33 | 0.23 | 0.27 |
FFQ: Food Frequency Questionnaire
In nutrition research, attenuation coefficients range between 0 and 1, with those closer to 0 indicating maximum attenuation and those closer to 1 indicating minimum attenuation (24). These coefficients are used to quantify the amount by which the log relative risk between the dietary exposure and disease outcome would be distorted because of measurement error in the FFQ. For the questionnaires used in the JHS, coefficients tended to be, but were not always, higher for the long than the short FFQ. For men, (Table 5), the energy adjusted attenuation coefficients for intake of macronutrients ranged from 0.25 for polyunsaturated fat to 0.70 for carbohydrate for the short FFQ; and from 0.23 for polyunsaturated fat to 0.75 for dietary fiber for the long FFQ. For micronutrients, these ranged from 0.13 and 0.27 for sodium for the short and long FFQs respectively to 0.8 for Vitamin A for the short and 0.75 for magnesium for the long FFQ. For women, attenuation coefficients for macronutrient intakes ranged from 0.21 for polyunsaturated fat to 0.50 for dietary fiber for the short FFQ; and from 0.20 for polyunsaturated to 0.63 for dietary fiber on the long FFQ. For micronutrients, these ranged from 0.13 for sodium to 0.54 for magnesium on the short FFQ and from 0.25 for sodium to 0.72 for magnesium for the long FFQ.
Table 5.
Attenuation coefficients for energy adjusted (except for energy intake itself) macro- and micronutrients for the participants in the Jackson Heart Study Diet and Physical Activity Sub-Study
| Nutrient | Men | Women | ||
|---|---|---|---|---|
| Short FFQa | Long FFQa | Short FFQa | Long FFQa | |
| Energy | 0.26 | 0.26 | 0.22 | 0.24 |
| Protein | 0.27 | 0.35 | 0.23 | 0.42 |
| Carbohydrate | 0.70 | 0.74 | 0.47 | 0.32 |
| Fat | 0.43 | 0.39 | 0.25 | 0.34 |
| Saturated fat | 0.50 | 0.47 | 0.22 | 0.44 |
| Monounsaturated fat | 0.47 | 0.40 | 0.23 | 0.32 |
| Polyunsaturated fat | 0.25 | 0.23 | 0.21 | 0.20 |
| Cholesterol | 0.34 | 0.46 | 0.32 | 0.43 |
| Dietary Fiber | 0.47 | 0.75 | 0.50 | 0.63 |
| Vitamin A | 0.81 | 0.68 | 0.37 | 0.28 |
| Vitamin E | 0.27 | 0.42 | 0.30 | 0.37 |
| Vitamin D | 0.46 | 0.45 | 0.29 | 0.48 |
| Vitamin C | 0.64 | 0.50 | 0.44 | 0.47 |
| Folate | 0.40 | 0.44 | 0.37 | 0.37 |
| Thiamin | 0.39 | 0.56 | 0.25 | 0.37 |
| Riboflavin | 0.45 | 0.52 | 0.29 | 0.50 |
| Niacin | 0.40 | 0.51 | 0.24 | 0.35 |
| Vitamin B6 | 0.47 | 0.62 | 0.45 | 0.58 |
| Vitamin B12 | 0.40 | 0.48 | 0.22 | 0.39 |
| Calcium | 0.38 | 0.41 | 0.38 | 0.42 |
| Iron | 0.46 | 0.61 | 0.32 | 0.41 |
| Magnesium | 0.68 | 0.75 | 0.54 | 0.72 |
| Phosphorus | 0.38 | 0.47 | 0.27 | 0.54 |
| Zinc | 0.28 | 0.53 | 0.19 | 0.37 |
| Potassium | 0.32 | 0.54 | 0.35 | 0.59 |
| Sodium | 0.13 | 0.27 | 0.13 | 0.25 |
FFQ: Food Frequency Questionnaire
The ability of the FFQs to classify individuals in the population into the same quartiles of dietary intake (for 10 of the nutrients) relative to the dietary recalls was also examined (Table 6). On average, both the FFQs classified more than 30% of the population into the same quartiles as the reference instrument. Misclassification of participants in opposite quartiles was less than or equal to 8% for both the FFQs for all nutrients tested, with the exception of vitamin E for the long FFQ (12% for men; 9% for women) and total energy and protein intake on the short FFQ (approx. 8% and 9% respectively, for women only).
Table 6.
Quantification of dietary intakes of the Jackson Heart Study Diet and Physical Activity Sub-Study participants into quartiles: Comparing the Food Frequency Questionnaires and the mean of four 24-hour dietary recalls
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Short FFQa | Long FFQa | Short FFQa | Long FFQa | |||||
| Nutrient | Same Quartile (%) |
Opp. Quartile (%) |
Same Quartile (%) |
Opp. Quartile (%) |
Same Quartile (%) |
Opp. Quartile (%) |
Same Quartile (%) |
Opp. Quartile (%) |
| Energy | 38.0 | 4.9 | 31.9 | 8.0 | 31.5 | 8.4 | 31.1 | 6.9 |
| Protein | 35.0 | 6.1 | 33.1 | 6.7 | 38.8 | 8.8 | 34.8 | 6.2 |
| Carbohydrate | 35.6 | 3.7 | 38.6 | 7.4 | 36.3 | 7.3 | 39.9 | 5.9 |
| Fat | 36.2 | 4.9 | 35.0 | 6.1 | 32.6 | 7.3 | 35.5 | 5.5 |
| Saturated Fat | 31.3 | 2.4 | 28.2 | 4.3 | 28.9 | 6.6 | 31.5 | 6.6 |
| Fiber | 35.0 | 5.5 | 43.5 | 1.8 | 34.1 | 6.2 | 38.1 | 4.8 |
| Vitamin E | 31.3 | 6.7 | 39.3 | 12.2 | 29.7 | 7.3 | 31.9 | 9.1 |
| Vitamin C | 34.3 | 3.7 | 37.4 | 2.4 | 33.7 | 4.8 | 42.1 | 3.7 |
| Calcium | 39.3 | 4.3 | 44.8 | 2.4 | 37.7 | 4.8 | 37.0 | 2.2 |
| Iron | 31.9 | 7.4 | 42.3 | 4.9 | 34.8 | 8.0 | 34.4 | 5.1 |
FFQ: Food Frequency Questionnaire
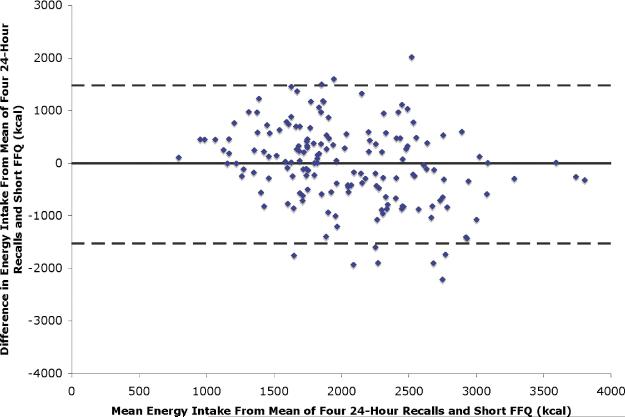
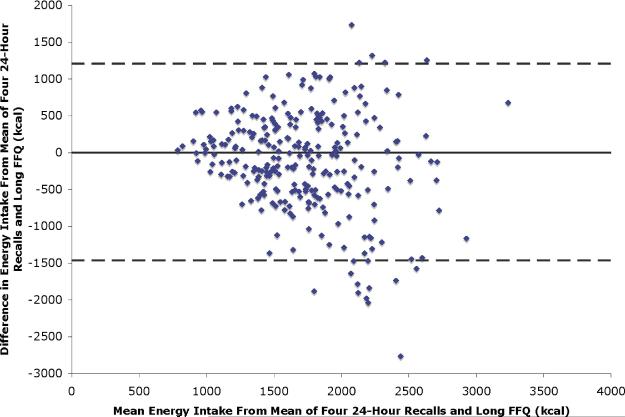
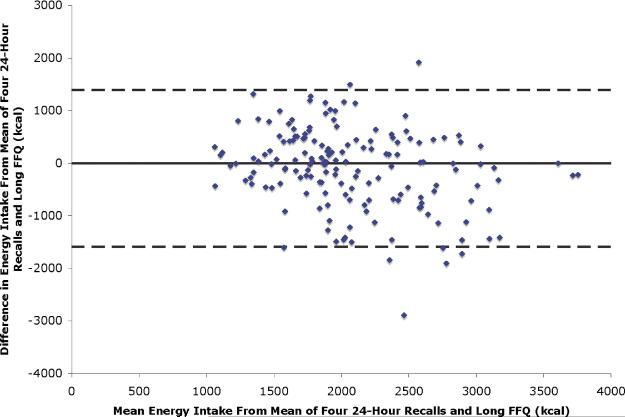
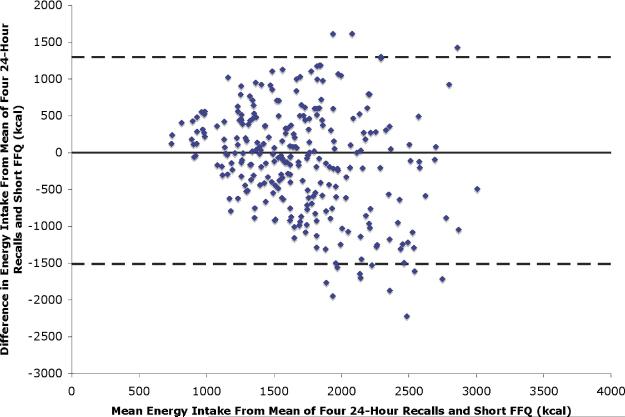
Bland Altman plots (Figures 1-4) demonstrated that for men, for both the short and the long FFQ (Figures 1, 2), there was no trend in the differences between the measurements using the FFQ and the recalls over the range of measurements. For women, (Figures 3, 4) as energy intake increased the difference between the measurements also increased. However, no systematic trend was seen in the scatter plots.
Figure 1.
Bland-Altman plot of the difference between energy intake from Mean of Four-24 Hour Dietary Recalls and the short FFQ against the mean of the two for the male participants of the JHS-DPASS conducted in Jackson, Mississippi, 2000-2004.
 Difference (energy intake from Mean of Four-24 Hour Dietary Recalls - the short FFQ)
Difference (energy intake from Mean of Four-24 Hour Dietary Recalls - the short FFQ)
------- 95% limits of agreement
FFQ: Food Frequency Questionnaire
JHS-DPASS: Jackson Heart Study- Diet and Physical Activity Sub-Study
Figure4.
Bland-Altman plot of the difference between energy intake from Mean of Four-24 Hour Dietary Recalls and the long FFQ against the mean of the two for the female participants of the JHS-DPASS conducted in Jackson, Mississippi, 2000-2004.
 Difference (energy intake from Mean of Four-24 Hour Dietary Recalls - the long FFQ)
Difference (energy intake from Mean of Four-24 Hour Dietary Recalls - the long FFQ)
------- 95% limits of agreement
FFQ: Food Frequency Questionnaire
JHS-DPASS: Jackson Heart Study- Diet and Physical Activity Sub-Study
Figure 2.
Bland-Altman plot of the difference between energy intake from Mean of Four-24 Hour Dietary Recalls and the long FFQ against the mean of the two for the male participants of the JHS-DPASS conducted in Jackson, Mississippi, 2000-2004.
 Difference (energy intake from Mean of Four-24 Hour Dietary Recalls - the long FFQ)
Difference (energy intake from Mean of Four-24 Hour Dietary Recalls - the long FFQ)
------- 95% limits of agreement
FFQ: Food Frequency Questionnaire
JHS-DPASS: Jackson Heart Study- Diet and Physical Activity Sub-Study
Figure 3.
Bland-Altman plot of the difference between energy intake from Mean of Four-24 Hour Dietary Recalls and the short FFQ against the mean of the two for the female participants of the the JHS-DPASS conducted in Jackson, Mississippi, 2000-2004.
 Difference (energy intake from Mean of Four-24 Hour Dietary Recalls - the short FFQ)
Difference (energy intake from Mean of Four-24 Hour Dietary Recalls - the short FFQ)
------- 95% limits of agreement
FFQ: Food Frequency Questionnaire
JHS-DPASS: Jackson Heart Study- Diet and Physical Activity Sub-Study
DISCUSSION
Dietary intake is a modifiable risk factor for chronic disease. The FFQ is the instrument of choice for assessing diet in large epidemiological studies because of its ease of administration, relative low cost and ability to rank individuals based on dietary intake (26). Minority and ethnic sub-groups, like African Americans in the South, have different dietary patterns as compared to the general US population. Exclusion of ethnic and minority foods can lead to extensive misclassification of dietary intakes of such populations (14, 27).
Relative to 24-hour dietary recalls, the FFQs used in the DPASS of the JHS appear to provide valid estimates of most macro and micronutrients. Further, the mean intakes of macronutrients obtained by 24-hour dietary recall in this population were similar to those reported among participants of a diet survey conducted in the lower Mississippi Delta, expanding generalizability of the results to the region (28). On comparing the median dietary intakes with those reported for the general US population in the National Health and Nutrition Examination Survey 2001-2002 (29) there were several nutrients where differences in estimated mean intakes were 10% or greater. For men and women, these included riboflavin, vitamin B12, phosphorous, zinc and calcium. For men only, these included vitamins E and B6, magnesium, iron, zinc, calcium and potassium. Higher relative intakes were observed for vitamin C for women.
The present study used energy adjusted and energy adjusted and de-attenuated correlations between FFQ estimates and the mean of 4-24 hour dietary recalls to establish the relative validity of the questionnaires. Concern has been expressed that comparisons with self-reported methods are prejudiced with bias at the individual level which correlates across methods (30, 31). An alternate model was, therefore, proposed by Kipnis et al. (32) which allows for correlations in biases of the reference instruments and the FFQ. However, studies have suggested that this model may overestimate the correlations between reference instruments and FFQs (33).
The use of biomarkers is an important though not always feasible way to validate dietary assessment methods, as recovery biomarkers are only available for a few nutrients (34). In many studies, including this one, the use of doubly labeled water as a recovery biomarker for total energy intake was not possible due to design and cost issues. Correlational biomarkers, including many serum nutrients are also useful, and some of these were examined in this study population (35). After adjustment for covariates, correlations between serum and dietary measures of carotenoids, for the short FFQ and the long FFQ, respectively, were: 0.35 and 0.21 for alpha-carotene; 0.26 and 0.28 for total (diet plus supplements) beta-carotene; 0.17 and 0.20 for dietary beta-carotene; 0.34 and 0.26 for beta-cryptoxanthin; 0.15 and 0.17 for lutein plus zeaxanthin; and 0.19 and 0.14 for lycopene (35). These are comparable with correlations with other populations, using other FFQs (36, 37).
The energy adjusted and de-attenuated correlations for the comparison between nutrient intakes from the 4 24-hour recalls and the FFQs ranged from 0.20-0.70 for the short FFQ, and from 0.23-0.75 for the long FFQ. On average, the correlation for these nutrients was around 0.4. For women, nutrients with correlations below 0.4 with the short FFQ included energy, protein, total fat, saturated, monounsaturated and polyunsaturated fats, vitamins A, E, D, thiamin, niacin, vitamin B 12, iron, zinc and sodium; while for the long FFQ, these included only energy, poly-unsaturated fat, vitamins A, E and sodium. For men, nutrients with correlations below 0.4 for the short FFQ included protein, polyunsaturated fat, vitamin E, zinc, potassium and sodium; and for the long FFQ, only energy, polyunsaturated fat and sodium. These results, particularly for the long FFQ, are comparable to those reported by similar validation studies (38-43). The FFQs consistently underperformed for polyunsaturated fat and sodium. Reasons for lower correlations for polyunsaturated fat may include the irregular distribution of oils used in food preparation. For sodium these may include variation in content of processed foods and difficulty in estimation of added salt in cooking and at the table. Dietary estimation of sodium intake is known to be difficult, with 24-hour urinary excretion of sodium considered to be the best method (44).
In the present study, men tended to have higher attenuation coefficients, and correlations with 24 hour recalls, than women. Similar observations were also made by Millen et al for food groups (24). They attributed these finding to greater differential misclassification by women than by men (45). The range of attenuation coefficients was similar to those reported by other studies (43, 46, 47). Lower attenuation coefficients, reflecting greater attenuation, were seen for energy and nutrients like polyunsaturated fat and sodium, which also demonstrated lower Pearson correlation coefficients between recall and FFQ estimates.
Finally, the percentages of participants correctly classified into the same, as well as opposite, quartiles were also comparable to those reported by other validation studies(48-50). For example, for dietary fat, the 60 and 100 item National Cancer Institute questionnaires were able to correctly classify around 40% of the study population in the same percentiles as the reference instrument. Though the correlation coefficients for the short FFQ tended to be lower than for the long FFQ, the ability of both FFQs to rank individuals in the population did not differ greatly.
Time constraints and participant burden are critical research issues, and there is, therefore, great demand for shorter instruments. Previous research has shown differing outcomes regarding the validity or shorter diet assessment tools (38, 50, 51), but all document the need (52). In a study comparing the effects of length and clarity on response rates and data quality for two FFQS, the 36- page Diet History Questionnaire was compared to a much shorter 16-page FFQ. The results indicated that the shorter questionnaire did not outperform the longer Diet History Questionnaire in terms of response rate and data quality (50). Validation results from the comparison of a one page rapid Food Screener (developed specifically for estimating fat, fiber, fruit and vegetable intake) with a full length validated questionnaire showed that the shorter questionnaire provided relatively accurate rankings of selected nutrient intakes (53).
A criticism of FFQs, is that their lack of detail, relative to the more complete information obtained by diet record, can lead to lack of accuracy, as demonstrated for the assessment of energy and protein intake in the OPEN biomarker study (45). However, it is also noteworthy that these estimations have been shown to improve with energy adjustment (54), and it is important to note that the FFQ remains the most cost-effective way to rank usual nutrient intakes in population studies.
Assessment of dietary intake has always been an important component of the typical role of registered dietitians. When debating limitations of dietary assessment instruments, most nutrition researchers agree that there is no perfect measurement tool. (55, 56). In large population studies, FFQ measures must be compared with other more accurate measures, such as in the JHS model with four 24-hour recalls and available biomarkers, to ensure validity within the population to which it is applied (57).
A limitation of the present study, as in most validation studies, is that results may not be generalizable to other populations. The all African American DPASS cohort was well educated and highly motivated, as evidenced by the completion of an initial short FFQ, followed by 4 24-hour recalls and the long FFQ.
With the critical health statistics related to the rise of obesity and the documented relationship of obesity to numerous chronic diseases, it is important to have assessment tools which are valid and reliable for minority populations. This is especially true in the African American community because of the close connection of many food items and preparation methods that are so closely associated to the culture itself. The FFQs this study investigated will provide nutrition practitioners with useful tools for assessment of usual dietary intake in African Americans. The open-ended component provides ongoing capture and evaluation of the variation of intake in this important population. Use of such FFQs will enable professionals to implement prevention and treatment models to change the regional and national trends that stimulated the need for the important work being accomplished by the JHS investigators. Clinical care will be positively impacted by being able to better identify cultural food patterns that promote disease states such as heart disease.
CONCLUSIONS
More investigation is needed to better describe the scope of the relationships between diet and cardiovascular in African Americans. Because the short FFQ in this study is a categorical subset of the long FFQ, both allow for assessment of the full range of nutrients.
In summary, the Delta NIRI FFQ exhibited relatively higher correlations on 26 nutrients of interest, but that both the Delta NIRI FFQ and its subset, the Delta NIRI JHS FFQ were useful in assessing intakes within the adult African American community in the Southern US. Having these valid and culturally sensitive instruments will provide future researchers with greater flexibility in research design and expand the diet association investigative capabilities within studies focusing on African American populations.
Abbreviations used
- FFQ
Food Frequency Questionnaire
- US
United States
- Delta NIRI
Delta Nutrient Intervention Research Initiative
- JHS
Jackson Heart Study
- DPASS
Diet and Physical Activity Sub-Study
- RE
Retinol Equivalents
Contributor Information
Teresa C. Carithers, Department of Family & Consumer Sciences The University of Mississippi P.O. Box 1848 University, MS 38677-1848 Phone: (662) 915-7372 Fax: (662) 915-7039 carither@olemiss.edu.
Sameera A. Talegawkar, Dietary Assessment and Epidemiology Research Department JM USDA HNRCA at Tufts University 711 Washington Street Boston, MA 02111 Phone: (617) 216-4587 Fax: (617) 556-3344 sameera.talegawkar@alumni.tufts.edu.
Marjuyua L. Rowser, College of Human Environmental Sciences University of Alabama P.O. Box 870158 Tuscaloosa, AL 35487-0158 mrowser@ches.ua.edu.
Olivia R. Henry, Division of Digestive Diseases University of Mississippi Medical Center 2500 North State St. Jackson, MS 39216 ohenry@medicine.umsmed.edu.
Patricia M. Dubbert, G.V. (Sonny) Montgomery Veterans Affairs Medical Center and Departments of Medicine, Preventive Medicine, and Psychiatry University of Mississippi School of Medicine Mental Health (11M), 1500 E. Woodrow Wilson Dr. Jackson, MS 39216 Phone: 601-364-1350 Fax: 601-364-1395 patricia.Dubbert@med.va.gov
Margaret L Bogle, Delta NIRI USDA, Agricultural Research Service 900 S. Shackleford Road, Ste. 509 Little Rock, AR 72211 Phone: (501) 954-8882 Fax: (501) 954-9596 Margaret.bogle@ars.usda.gov.
Herman A. Taylor, Jr., University of Mississippi Medical Center Principal Investigator, Jackson Heart Study 350 West Woodrow Wilson Drive, Suite #701 Jackson, MS 39213 Phone: (601) 979-8744 Fax: (601) 979 8750 htaylor@medicine.umsmed.edu.
Katherine L. Tucker, Dietary Assessment and Epidemiology Research Department JM USDA HNRCA at Tufts University 711 Washington Street Boston, MA 02111 Phone: (617) 556-33 Fax: 617-556-3344 Katherine.tucker@tufts.edu.
REFERENCES
- 1.Kumanyika SK, Morssink C, Agurs T. Models for dietary and weight change in African-American women: identifying cultural components. Ethn Dis. 1992;2:166–175. [PubMed] [Google Scholar]
- 2.Airhihenbuwa CO, Kumanyika S, Agurs TD, Lowe A, Saunders D, Morssink CB. Cultural aspects of African American eating patterns. Ethn Health. 1996;1:245–260. doi: 10.1080/13557858.1996.9961793. [DOI] [PubMed] [Google Scholar]
- 3.Kroke A, Klipstein-Grobusch K, Voss S, Moseneder J, Thielecke F, Noack R, Boeing H. Validation of a self-administered food-frequency questionnaire administered in the European Prospective Investigation into Cancer and Nutrition (EPIC) Study: comparison of energy, protein, and macronutrient intakes estimated with the doubly labeled water, urinary nitrogen, and repeated 24-h dietary recall methods. Am J Clin Nutr. 1999;70:439–447. doi: 10.1093/ajcn/70.4.439. [DOI] [PubMed] [Google Scholar]
- 4.Payne TJ, Wyatt SB, Mosley TH, Dubbert PM, Guiterrez-Mohammed ML, Calvin RL, Taylor HA, Jr., Williams DR. Sociocultural methods in the Jackson Heart Study: conceptual and descriptive overview. Ethn Dis. 2005;15:S6–38-48. [PubMed] [Google Scholar]
- 5.Teufel NI. Development of culturally competent food-frequency questionnaires. Am J Clin Nutr. 1997;65:1173S–1178S. doi: 10.1093/ajcn/65.4.1173S. [DOI] [PubMed] [Google Scholar]
- 6.Coates RJ, Monteilh CP. Assessments of food-frequency questionnaires in minority populations. Am J Clin Nutr. 1997;65:1108S–1115S. doi: 10.1093/ajcn/65.4.1108S. [DOI] [PubMed] [Google Scholar]
- 7.Tucker KL, Maras J, Champagne C, Connell C, Goolsby S, Weber J, Zaghloul S, Carithers T, Bogle ML. A regional food-frequency questionnaire for the US Mississippi Delta. Public Health Nutr. 2005;8:87–96. [PubMed] [Google Scholar]
- 8.Carithers T, Dubbert PM, Crook E, Davy B, Wyatt SB, Bogle ML, Taylor HA, Jr., Tucker KL. Dietary assessment in African Americans: methods used in the Jackson Heart Study. Ethn Dis. 2005;15:S6–49-55. [PubMed] [Google Scholar]
- 9.Subar AF. Developing dietary assessment tools. J Am Diet Assoc. 2004;104:769–770. doi: 10.1016/j.jada.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Kushi LH. Gaps in epidemiologic research methods: design considerations for studies that use food-frequency questionnaires. Am J Clin Nutr. 1994;59:180S–184S. doi: 10.1093/ajcn/59.1.180S. [DOI] [PubMed] [Google Scholar]
- 11.Block G. Human dietary assessment: methods and issues. Prev Med. 1989;18:653–660. doi: 10.1016/0091-7435(89)90036-4. [DOI] [PubMed] [Google Scholar]
- 12.Block G, Mandel R, Gold E. On food frequency questionnaires: the contribution of open-ended questions and questions on ethnic foods. Epidemiology. 2004;15:216–221. doi: 10.1097/01.ede.0000112144.77106.bf. [DOI] [PubMed] [Google Scholar]
- 13.Fraser GE. A search for truth in dietary epidemiology. Am J Clin Nutr. 2003;78:521S–525S. doi: 10.1093/ajcn/78.3.521S. [DOI] [PubMed] [Google Scholar]
- 14.Tucker KL, Bianchi LA, Maras J, Bermudez OI. Adaptation of a food frequency questionnaire to assess diets of Puerto Rican and non-Hispanic adults. Am J Epidemiol. 1998;148:507–518. doi: 10.1093/oxfordjournals.aje.a009676. [DOI] [PubMed] [Google Scholar]
- 15.Kaaks R, Plummer M, Riboli E, Esteve J, van Staveren W. Adjustment for bias due to errors in exposure assessments in multicenter cohort studies on diet and cancer: a calibration approach. Am J Clin Nutr. 1994;59:245S–250S. doi: 10.1093/ajcn/59.1.245S. [DOI] [PubMed] [Google Scholar]
- 16.Willett WC. Nutritional Epidemiology. 2nd ed. Oxford University Press Inc.; New York: 1998. pp. 101–147. [Google Scholar]
- 17.Thompson FE, Midthune D, Subar AF, Kipnis V, Kahle LL, Schatzkin A. Development and evaluation of a short instrument to estimate usual dietary intake of percentage energy from fat. J Am Diet Assoc. 2007;107:760–767. doi: 10.1016/j.jada.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 18.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives The ARIC investigators. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 19.Taylor HA., Jr The Jackson Heart Study: an overview. Ethn Dis. 2005;15:S6–1-3. [PubMed] [Google Scholar]
- 20.Taylor HA, Jr., Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, Nelson C, Wyatt SB. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15:S6–4-17. [PubMed] [Google Scholar]
- 21.Kristal AR, Shattuck AL, Henry HJ, Fowler AS. Rapid assessment of dietary intake of fat, fiber, and saturated fat: validity of an instrument suitable for community intervention research and nutritional surveillance. Am J Health Promot. 1990:288–295. doi: 10.4278/0890-1171-4.4.288. [DOI] [PubMed] [Google Scholar]
- 22.Willett WC, Howe GR, Kushi LH. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65:1220S–1228S. doi: 10.1093/ajcn/65.4.1220S. discussion 1229S-1231S. [DOI] [PubMed] [Google Scholar]
- 23.Willett WC. Nutritional Epidemiology. 2nd ed. Oxford University Press Inc.; New York: 1998. pp. 302–320. [Google Scholar]
- 24.Millen AE, Midthune D, Thompson FE, Kipnis V, Subar AF. The National Cancer Institute diet history questionnaire: validation of pyramid food servings. Am J Epidemiol. 2006;163:279–288. doi: 10.1093/aje/kwj031. [DOI] [PubMed] [Google Scholar]
- 25.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 26.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Hennekens CH, Speizer FE. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122:51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 27.Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A databased approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 28.Champagne CM, Bogle ML, McGee BB, Yadrick K, Allen HR, Kramer TR, Simpson P, Gossett J, Weber J. Dietary intake in the lower Mississippi delta region: results from the Foods of our Delta Study. J Am Diet Assoc. 2004;104:199–207. doi: 10.1016/j.jada.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 29.Moshfegh A, Goldman J, Cleveland L. What We Eat in America, NHANES 2001-2002: Usual Nutrient Intakes from Food Compared to Dietary Reference Intakes. US Department of Agriculture, Agricultural Research Service; 2005. [Google Scholar]
- 30.Livingstone MB, Prentice AM, Strain JJ, Coward WA, Black AE, Barker ME, McKenna PG, Whitehead RG. Accuracy of weighed dietary records in studies of diet and health. BMJ. 1990;300:708–712. doi: 10.1136/bmj.300.6726.708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heitmann BL, Lissner L. Dietary underreporting by obese individuals--is it specific or non-specific? BMJ. 1995;311:986–989. doi: 10.1136/bmj.311.7011.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kipnis V, Carroll RJ, Freedman LS, Li L. Implications of a new dietary measurement error model for estimation of relative risk: application to four calibration studies. Am J Epidemiol. 1999;150:642–651. doi: 10.1093/oxfordjournals.aje.a010063. [DOI] [PubMed] [Google Scholar]
- 33.Fraser GE, Butler TL, Shavlik D. Correlations between estimated and true dietary intakes: using two instrumental variables. Ann Epidemiol. 2005;15:509–518. doi: 10.1016/j.annepidem.2004.12.012. [DOI] [PubMed] [Google Scholar]
- 34.Potischman N, Freudenheim JL. Biomarkers of nutritional exposure and nutritional status: an overview. J Nutr. 2003;133(Suppl 3):873S–874S. doi: 10.1093/jn/133.3.873S. [DOI] [PubMed] [Google Scholar]
- 35.Talegawkar SA, Johnson EJ, Carithers TC, Taylor HA, Bogle ML, Tucker KL. Carotenoid intakes, assessed by food-frequency questionnaires (FFQs), are associated with serum carotenoid concentrations in the Jackson Heart Study: validation of the Jackson Heart Study Delta NIRI Adult FFQs. Public Health Nutr. 2008;11:989–997. doi: 10.1017/S1368980007001310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tucker KL, Chen H, Vogel S, Wilson PW, Schaefer EJ, Lammi-Keefe CJ. Carotenoid intakes, assessed by dietary questionnaire, are associated with plasma carotenoid concentrations in an elderly population. J Nutr. 1999;129:438–445. doi: 10.1093/jn/129.2.438. [DOI] [PubMed] [Google Scholar]
- 37.Bermudez OI, Ribaya-Mercado JD, Talegawkar SA, Tucker KL. Hispanic and non-Hispanic white elders from Massachusetts have different patterns of carotenoid intake and plasma concentrations. J Nutr. 2005;135:1496–1502. doi: 10.1093/jn/135.6.1496. [DOI] [PubMed] [Google Scholar]
- 38.Stram DO, Hankin JH, Wilkens LR, Pike MC, Monroe KR, Park S, Henderson BE, Nomura AM, Earle ME, Nagamine FS, Kolonel LN. Calibration of the dietary questionnaire for a multiethnic cohort in Hawaii and Los Angeles. Am J Epidemiol. 2000;151:358–370. doi: 10.1093/oxfordjournals.aje.a010214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kumanyika SK, Mauger D, Mitchell DC, Phillips B, Smiciklas-Wright H, Palmer JR. Relative validity of food frequency questionnaire nutrient estimates in the Black Women's Health Study. Ann Epidemiol. 2003;13:111–118. doi: 10.1016/s1047-2797(02)00253-3. [DOI] [PubMed] [Google Scholar]
- 40.Boucher B, Cotterchio M, Kreiger N, Nadalin V, Block T, Block G. Validity and reliability of the Block98 food-frequency questionnaire in a sample of Canadian women. Public Health Nutr. 2006;9:84–93. doi: 10.1079/phn2005763. [DOI] [PubMed] [Google Scholar]
- 41.Iqbal R, Ajayan K, Bharathi AV, Zhang X, Islam S, Soman CR, Merchant AT. Refinement and validation of an FFQ developed to estimate macro- and micronutrient intakes in a south Indian population. Public Health Nutr. 2008:1–7. doi: 10.1017/S1368980008001845. [DOI] [PubMed] [Google Scholar]
- 42.Jain MG, Rohan TE, Soskolne CL, Kreiger N. Calibration of the dietary questionnaire for the Canadian Study of Diet, Lifestyle and Health cohort. Public Health Nutr. 2003;6:79–86. doi: 10.1079/PHN2002362. [DOI] [PubMed] [Google Scholar]
- 43.Thompson FE, Kipnis V, Midthune D, Freedman LS, Carroll RJ, Subar AF, Brown CC, Butcher MS, Mouw T, Leitzmann M, Schatzkin A. Performance of a food-frequency questionnaire in the US NIH-AARP (National Institutes of Health-American Association of Retired Persons) Diet and Health Study. Public Health Nutr. 2008;11:183–195. doi: 10.1017/S1368980007000419. [DOI] [PubMed] [Google Scholar]
- 44.Day N, McKeown N, Wong M, Welch A, Bingham S. Epidemiological assessment of diet: a comparison of a 7-day diary with a food frequency questionnaire using urinary markers of nitrogen, potassium and sodium. Int J Epidemiol. 2001;30:309–317. doi: 10.1093/ije/30.2.309. [DOI] [PubMed] [Google Scholar]
- 45.Subar AF, Kipnis V, Troiano RP, Midthune D, Schoeller DA, Bingham S, Sharbaugh CO, Trabulsi J, Runswick S, Ballard-Barbash R, Sunshine J, Schatzkin A. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: the OPEN study. Am J Epidemiol. 2003;158:1–13. doi: 10.1093/aje/kwg092. [DOI] [PubMed] [Google Scholar]
- 46.Johansson I, Hallmans G, Wikman A, Biessy C, Riboli E, Kaaks R. Validation and calibration of food-frequency questionnaire measurements in the Northern Sweden Health and Disease cohort. Public Health Nutr. 2002;5:487–496. doi: 10.1079/phn2001315. [DOI] [PubMed] [Google Scholar]
- 47.Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, McIntosh A, Rosenfeld S. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires : the Eating at America's Table Study. Am J Epidemiol. 2001;154:1089–1099. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- 48.Sevak L, Mangtani P, McCormack V, Bhakta D, Kassam-Khamis T, dos Santos Silva I. Validation of a food frequency questionnaire to assess macro- and micro-nutrient intake among South Asians in the United Kingdom. Eur J Nutr. 2004;43:160–168. doi: 10.1007/s00394-004-0454-6. [DOI] [PubMed] [Google Scholar]
- 49.Shu XO, Yang G, Jin F, Liu D, Kushi L, Wen W, Gao YT, Zheng W. Validity and reproducibility of the food frequency questionnaire used in the Shanghai Women's Health Study. Eur J Clin Nutr. 2004;58:17–23. doi: 10.1038/sj.ejcn.1601738. [DOI] [PubMed] [Google Scholar]
- 50.Potischman N, Carroll RJ, Iturria SJ, Mittl B, Curtin J, Thompson FE, Brinton LA. Comparison of the 60- and 100-item NCI-block questionnaires with validation data. Nutr Cancer. 1999;34:70–75. doi: 10.1207/S15327914NC340110. [DOI] [PubMed] [Google Scholar]
- 51.Thompson FE, Kipnis V, Subar AF, Krebs-Smith SM, Kahle LL, Midthune D, Potischman N, Schatzkin A. Evaluation of 2 brief instruments and a food-frequency questionnaire to estimate daily number of servings of fruit and vegetables. Am J Clin Nutr. 2000;71:1503–1510. doi: 10.1093/ajcn/71.6.1503. [DOI] [PubMed] [Google Scholar]
- 52.Monsen ER, Van Horn L. Research Successful Approaches. 3rd ed. American Dietetic Association; 2008. pp. 190–191. [Google Scholar]
- 53.Subar AF, Ziegler RG, Thompson FE, Johnson CC, Weissfeld JL, Reding D, Kavounis KH, Hayes RB. Is shorter always better? Relative importance of questionnaire length and cognitive ease on response rates and data quality for two dietary questionnaires. Am J Epidemiol. 2001;153:404–409. doi: 10.1093/aje/153.4.404. [DOI] [PubMed] [Google Scholar]
- 54.Kipnis V, Subar AF, Midthune D, Freedman LS, Ballard-Barbash R, Troiano RP, Bingham S, Schoeller DA, Schatzkin A, Carroll RJ. Structure of dietary measurement error: results of the OPEN biomarker study. Am J Epidemiol. 2003;158:14–21. doi: 10.1093/aje/kwg091. discussion 22-16. [DOI] [PubMed] [Google Scholar]
- 55.Kristal AR, Peters U, Potter JD. Is it time to abandon the food frequency questionnaire? Cancer Epidemiol Biomarkers Prev. 2005;14:2826–2828. doi: 10.1158/1055-9965.EPI-12-ED1. [DOI] [PubMed] [Google Scholar]
- 56.Thompson FE, Subar AF, Brown CC, Smith AF, Sharbaugh CO, Jobe JB, Mittl B, Gibson JT, Ziegler RG. Cognitive research enhances accuracy of food frequency questionnaire reports: results of an experimental validation study. J Am Diet Assoc. 2002;102:212–225. doi: 10.1016/s0002-8223(02)90050-7. [DOI] [PubMed] [Google Scholar]
- 57.Brown D. Do food frequency questionnaires have too many limitations? J Am Diet Assoc. 2006;106:1541–1542. doi: 10.1016/j.jada.2006.07.020. [DOI] [PubMed] [Google Scholar]