Abstract
Researchers have hypothesized that the impact of body mass index on chronic disease may be greater in Asians than in Whites; however, most studies are cross-sectional and have no White comparison group. The authors compared the associations with body mass index in Chinese Asians (n = 5,980), American Whites (n = 10,776), and American Blacks (n = 3,582) using prospective data from the People’s Republic of China Study (1983–1994) and the Atherosclerosis Risk in Communities Study (1987–1998). Slopes of risk differences over body mass index levels were compared among the three ethnic groups in adjusted analyses. The authors found larger associations with body mass index in Chinese Asians compared with American Whites and Blacks for hypertension (p < 0.05). The increase in the incidence of hypertension associated with a one-unit increase in body mass index over approximately 8 years of follow-up was 2.5, 1.7, and 1.8 percentage points for Chinese Asians, American Whites, and American Blacks, respectively. For diabetes, the estimates were 1.7, 1.1, and 1.6 percentage points for the same groups— higher in Chinese Asians than in American Whites (p < 0.05) but similar between Chinese Asians and American Blacks. Given the ethnic differences in associations, the results support advocacy of public health and medical actions toward obesity prevention and treatment in China.
Keywords: Asian continental ancestry group, body mass index, diabetes mellitus, ethnic groups, hypertension
The World Health Organization (1) and the National Institutes of Health (2) have provided guidelines using body mass index as the criterion measure for the cutpoints for overweight (25 kg/m2) and obesity (30 kg/m2). These recommendations have been rapidly adopted by many clinicians and researchers around the world. Nevertheless, it is currently controversial whether these cutpoints are suitable to be applied to Asian populations, and some Asian countries have begun to use lower cutpoints (3-7).
Although there are differences among Asian populations (8), Asian groups generally have a considerably higher percent body fat at the same body mass index compared with Caucasians of the same age and gender (8-14). Deurenberg et al. (12) have shown that, for the same level of fatness, age, and gender, mean body mass index in African Americans was 1.3 kg/m2 higher than in Caucasians, whereas mean body mass index in Chinese was 1.9 kg/m2 lower than in Caucasians.
Numerous studies have examined associations between body mass index and cardiovascular disease risk factors in Chinese Asians. However, we know of only two reports (15, 16) that have made direct comparisons with Caucasians, the group primarily represented in studies used to define overweight and obesity. Those two studies were limited by the use of cross-sectional data and quantified the impact of body mass index using absolute levels or a ratio measure (15, 16). We have shown (17) that the use of an absolute or ratio measure to compare groups can be misleading when the rates of disease in the reference category are very different. The objectives of this study were to evaluate and compare the association of body mass index with hypertension and diabetes among Asians living in China and Whites and Blacks living in the United States by use of prospective data and risk difference as the criterion measure.
MATERIALS AND METHODS
Study populations
Data for this work are from two studies, both of which recruited community-based samples. The People’s Republic of China (PRC) Study examined urban and rural populations in Beijing (northern China) and Guangzhou (southern China) (18). Baseline data were collected in 1983–1984, and follow-up examinations were conducted in 1987–1988 and 1993–1994. The Atherosclerosis Risk in Communities (ARIC) Study examined White and Black men and women in four US communities: Forsyth County, North Carolina,; Jackson, Mississippi; the northwestern suburbs of Minneapolis, Minnesota; and Washington County, Maryland (19). Baseline data were collected in 1987–1989, and three follow-up examinations were conducted at 3-year intervals. In order to make the studies more comparable, we did not use the data from the third ARIC Study examination (1993–1995). This resulted in the same number of examinations and a similar average follow-up time among Chinese Asians (8.2 years), American Whites (8.2 years), and American Blacks (7.9 years).
For the PRC Study cohort, only participants aged 45–64 years at baseline were included in the analysis (n = 6,575), matching the age range in the ARIC Study. Of the 15,792 ARIC Study participants, we excluded the 55 Blacks from Washington County, Maryland, or Minneapolis, Minnesota, and the 48 participants that classified their ethnicity as other than White or Black because they were too small in number to allow ethnic and field center-specific analyses. For both the PRC and the ARIC studies, participants were excluded if they were missing body mass index at baseline (n = 58), both follow-up visits (n = 1,760), or pertinent covariates (n = 108). Following these exclusions, 5,980 Chinese Asians, 10,776 American Whites, and 3,582 American Blacks remained in the sample. When examining incident hypertension and diabetes, we excluded baseline prevalent cases of that outcome. These studies were approved by the institutional review boards at each field center, and this analysis was approved by the University of North Carolina at Chapel Hill Public Health Institutional Review Board on research involving human subjects.
Measurements
The Collaborative Studies Coordinating Center at the University of North Carolina at Chapel Hill developed the protocols and training manuals for all measurements and handled the review, processing, and analyses of all data for both the ARIC and PRC studies. In both cohorts, the participant’s height (without shoes) and weight were measured in light clothing (PRC Study cohort) or scrub suit (ARIC Study cohort) by a beam balance scale. Body mass index was categorized into seven categories (3). Age, education, smoking status, and alcohol consumption were assessed by interviewer-administered questionnaires.
Blood pressure was measured three times at each examination with a standard mercury sphygmomanometer on the right arm of the seated participant. The averages of the last two measures were used in our analyses. Participants were classified as having hypertension if they 1) self-reported that they were currently taking antihypertensive medication; 2) had a systolic blood pressure of 140 mmHg or higher; or 3) had a diastolic blood pressure of 90 mmHg or higher.
Study participants were instructed to fast for 12 hours prior to their clinic visit. Fasting blood samples were drawn, and serum glucose was measured by the hexokinase/glucose-6-phosphate dehydrogenase method in Beijing or Guangzhou (PRC Study cohort) or in Minnesota (ARIC Study cohort). Participants were categorized as having diabetes if they had a glucose level of 126 mg/dl or higher, reported taking diabetes medication, or reported that a physician had told them that they had diabetes.
Statistical analyses
Ethnic groups were analyzed separately by use of logistic regression (PROC LOGISTIC; SAS Institute, Inc., Cary, North Carolina). This approach was selected after log binomial (with log link), binomial (with identity link), and Poisson models were attempted but did not converge for all outcomes. Fully adjusted logistic models included covariates for gender, baseline age, education, smoking status, alcohol consumption, field center, and body mass index as either a categorical or a continuous variable. Because our interest was to show adjusted incidences and risk differences that were comparable across the ethnic groups, we adjusted estimates for a selected common group or adjusted to the overall mean where possible. Thus, estimated probabilities were calculated for a nonsmoker and a nondrinker at age 53.2 years (the mean age) and for the distribution of gender found in our combined samples (54 percent females). We also adjusted for education and field center, but these variables differed in the PRC and ARIC studies’ cohorts. In the ARIC Study, participants were from two (Blacks) or three (Whites) field centers, and education was categorized as less than high school graduate, high school graduate, or at least some college. In the PRC Study, Asians were from four field centers, and education was categorized as less than primary education, primary education, or at least secondary education. Weighted cumulative incidence was calculated by use of the proportion of participants in each field center by education group. Risk differences were calculated with the 18.5–<23.0 kg/m2 body mass index category as the referent. The delta method (20) was used to calculate the standard errors and 95 percent confidence intervals for the weighted cumulative incidences and risk differences. Comparisons of estimates in body mass index categories across the three ethnic group pairs (Chinese Asians versus American Whites, Chinese Asians versus American Blacks, and American Whites versus American Blacks) were done using Wald statistics with 1 df.
To summarize the risk difference results across body mass index categories, we constructed weighted least-squares regression models with the adjusted risk differences as the dependent variables and the ethnicity-specific median body mass index within each category as the independent variables. The weight was the inverse of the estimated variance for the adjusted risk difference. Wald statistics and p values were calculated with 1 df to compare ethnic group pairs. All analyses were performed using SAS, version 9.1, software (SAS Institute, Inc.).
RESULTS
The mean ages in ethnic-gender groups were similar and ranged from 50.9 to 54.7 years (table 1). In contrast, there were striking differences in body mass index among ethnicgender groups. Asian women had a lower mean body mass index (22.4 kg/m2) compared with White (26.6 kg/m2) and Black (30.8 kg/m2) women. In men, the mean body mass indexes were similar in Americans (27.4 kg/m2 in Whites and 27.8 kg/m2 in Blacks), which findings were considerably higher than that of Asian men (22.0 kg/m2). Few Americans had a body mass index less than 18.5 kg/m2, while few Asians had a body mass index greater than or equal to 30.0 kg/m2.
TABLE 1. Demographic characteristics at baseline among Chinese Asian, American White, and American Black women and men, the Atherosclerosis Risk in Communities Study (1987–1998) and the People’s Republic of China Study (1983–1994).
| Women |
Men |
|||||
|---|---|---|---|---|---|---|
| Chinese Asians (n = 3,049) |
American Whites (n = 5,706) |
American Blacks (n = 2,264) |
Chinese Asians (n = 2,931) |
American Whites (n = 5,070) |
American Blacks (n = 1,318) |
|
| Age, years (mean (SD*)) | 50.9 (4.4) | 53.9 (5.7) | 53.2 (5.7) | 51.1 (4.0) | 54.7 (5.7) | 53.6 (5.9) |
| Body mass index, kg/m2 (mean (SD)) | 22.4 (3.8) | 26.6 (5.4) | 30.8 (6.6) | 22.0 (3.3) | 27.4 (4.0) | 27.8 (4.9) |
| Body mass index category (%) | ||||||
| <18.5 kg/m2 | 15.2 | 1.2 | 0.8 | 13.8 | 0.2 | 0.9 |
| 18.5–<23.0 kg/m2 | 45.5 | 27.4 | 6.5 | 49.9 | 10.2 | 13.1 |
| 23.0–<25.0 kg/m2 | 16.8 | 18.0 | 10.0 | 16.5 | 16.6 | 14.4 |
| 25.0–<27.5 kg/m2 | 11.5 | 18.0 | 17.1 | 13.7 | 29.5 | 23.1 |
| 27.5–<30.0 kg/m2 | 7.5 | 12.6 | 17.8 | 5.0 | 21.4 | 20.3 |
| 30.0–<32.5 kg/m2 | 2.5 | 8.9 | 14.4 | 1.0 | 12.4 | 14.3 |
| ≥32.5 kg/m2 | 1.0 | 13.9 | 33.3 | 0.2 | 9.7 | 13.9 |
| Cigarette or leaf smoking status (% current) |
22.5 | 23.8 | 23.2 | 74.0 | 29.2 | 41.2 |
| Alcoholic beverage consumption status (% current) |
3.5 | 61.1 | 20.5 | 51.6 | 69.9 | 49.9 |
| Educational attainment (%) | ||||||
| Low | 54.7 | 15.4 | 38.9 | 12.6 | 16.9 | 41.3 |
| Medium | 34.3 | 43.1 | 23.0 | 65.2 | 29.3 | 18.9 |
| High | 11.0 | 41.5 | 38.1 | 22.2 | 53.8 | 39.8 |
SD, standard deviation.
The prevalences of smoking were similar among women, but among men, Asians were more likely (74.0 percent) to be current smokers than were Black (41.2 percent) or White (29.2 percent) men. In both genders, Whites were more likely to drink alcohol than were Blacks or Asians. The distribution of participants within the three educational categories varied across gender-ethnic groups. Most remarkable was the large gender difference in Asians with low educational attainment (54.7 percent of women vs. 12.6 percent of men).
Interactions between gender and body mass index for hypertension and diabetes were not found to be important in any ethnic group (p > 0.1 for all) and, therefore, genders were combined. Table 2 shows the adjusted baseline prevalence and the cumulative incidence of hypertension and diabetes. The estimates illustrate that the risk of diabetes and hypertension varied in these three ethnic groups even after adjustment for body mass index (23.0 kg/m2) and other covariates. For both hypertension and diabetes, the prevalence estimates shown were markedly higher in the American Blacks than in the American Whites or Chinese Asians. Note that prevalent cases at baseline were excluded from the calculation of cumulative incidence.
TABLE 2. Crude baseline prevalence and adjusted* baseline prevalence, cumulative incidence, and endpoint prevalence for hypertension and diabetes among Chinese Asians, American Whites, and American Blacks, the Atherosclerosis Risk in Communities Study (1987–1998) and the People’s Republic of China Study (1983–1994).
| Baseline prevalence |
Cumulative incidence |
|||||
|---|---|---|---|---|---|---|
| Cases/sample size (nos.)† |
Adjusted estimate |
95% confidence interval |
Cases/sample size (nos.)‡ |
Adjusted estimate |
95% confidence interval |
|
| Hypertension | ||||||
| Chinese Asians | 1,503/5,979 | 29.6 | 27.5, 31.7 | 1,300/4,476 | 30.9 | 28.4, 33.4 |
| American Whites | 3,448/10,769 | 22.5 | 20.9, 24.1 | 1,966/7,321 | 22.3 | 20.3, 24.2 |
| American Blacks | 2,055/3,577 | 44.2 | 41.0, 47.5 | 586/1,522 | 30.5 | 26.5, 34.6 |
| Diabetes | ||||||
| Chinese Asians | 116/4,643 | 2.7 | 1.9, 3.6 | 292/4,527 | 5.8 | 4.5, 7.1 |
| American Whites | 928/10,763 | 4.8 | 4.1, 5.5 | 855/9,835 | 4.3 | 3.7, 5.0 |
| American Blacks | 648/3,470 | 12.4 | 10.5, 14.3 | 435/2,822 | 8.7 | 7.0, 10.3 |
Adjusted to represent values for nonsmokers and nondrinkers at age 53.2 years with a body mass index of 23 kg/m2 and for the distributions of gender, education, and field center at baseline.
The sample size for hypertension prevalence at baseline excluded one Chinese Asian, seven American Whites, and five American Blacks who were missing hypertension status at baseline or at both follow-up visits. The sample size for diabetes prevalence at baseline excluded 1,337 Chinese Asians, 13 American Whites, and 112 American Blacks who were missing diabetes status at baseline or at both follow-up visits.
The sample size for hypertension incidence excluded 1,503 Chinese Asians, 3,448 American Whites, and 2,055 American Blacks with prevalent hypertension at baseline. The sample size for diabetes incidence excluded 116 Chinese Asians, 928 American Whites, and 648 American Blacks with prevalent diabetes at baseline.
Figure 1 shows the adjusted cumulative incidence of hypertension by body mass index category and ethnic group. Values were not shown where data were too sparse to obtain stable adjusted estimates. In every body mass index category in which data were available for comparison, the incidence of hypertension was higher in Asians than in Whites. Incidence also tended to be higher in Asians than in Blacks, although the differences were statistically significant only for the body mass index category of 25.0–<27.5 kg/m2.
FIGURE 1.
Adjusted cumulative incidence (and 95% confidence interval) for hypertension by body mass index categories and ethnicity, the Atherosclerosis Risk in Communities Study (1987–1998) and the People’s Republic of China Study (1983–1994). Point estimates for the same body mass index categories are shifted slightly in the horizontal plane so that confidence intervals are clearly visible.
The incidence of diabetes tended to be higher in Asians than in Whites (figure 2). The incidence of diabetes was very similar between Asians and Blacks with a body mass index below 25.0 kg/m2, but at or above a body mass index of 25.0 kg/m2 Asians tended to have higher estimates. When modeling continuous body mass index (table 2), we found that the incidence rate for diabetes tended to be higher in Blacks than in Asians at a body mass index of 23.0 kg/m2. This discrepancy was likely driven by differences in the modeling (continuous vs. categorical body mass index), and none of the trends mentioned was statistically significant. The confidence intervals were wide for the highest body mass index category (30.0–<32.5 kg/m2) in Asians, likely due to small numbers (16 cases of diabetes out of 64 eligible participants). Although the sample size was small, the distribution of the covariates did permit the estimation of a rate.
FIGURE 2.
Adjusted cumulative incidence (and 95% confidence interval) for diabetes by body mass index categories and ethnicity, the Atherosclerosis Risk in Communities Study (1987–1998) and the People’s Republic of China Study (1983–1994). Point estimates for the same body mass index categories are shifted slightly in the horizontal plane so that confidence intervals are clearly visible.
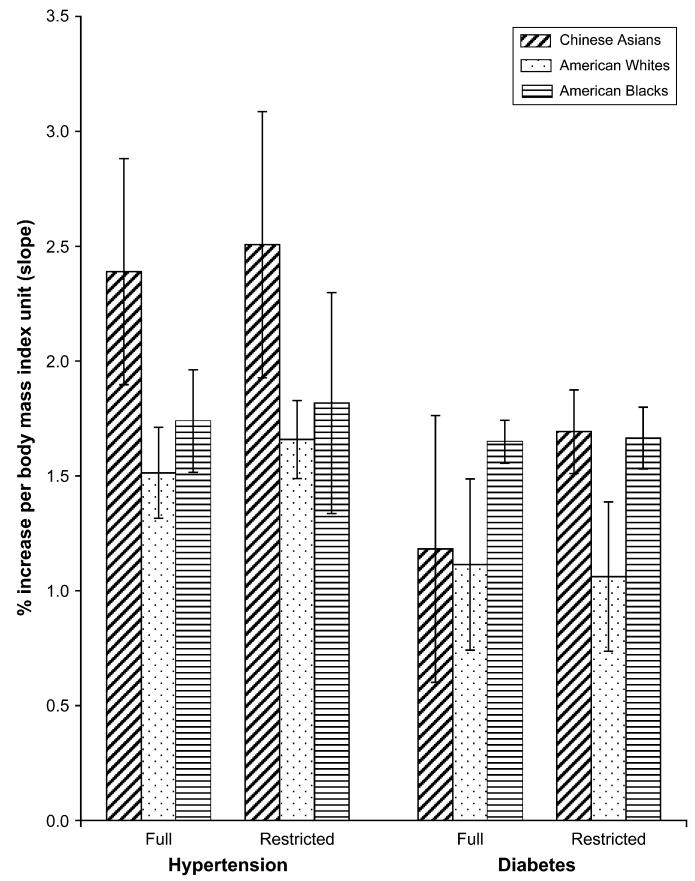
Adjusted risk differences for hypertension and diabetes are shown in table 3. The confidence intervals of the risk difference estimates within the body mass index categories were wide, but the estimates were greater than zero in the categories above the reference level and increased in a monotonic fashion. Figure 3 shows the calculated slopes of the risk differences over the full and restricted body mass index ranges. The restricted range included only the body mass index categories in which all ethnic groups had adequate data for adjusted analyses (18.5–<30.0 kg/m2 for hypertension and 18.5–<32.5 kg/m2 for diabetes). The latter estimates are shown to make the analyses across ethnic groups more comparable and to reduce the potential impact of the extremely different body mass index distributions among the ethnic groups.
TABLE 3. Adjusted risk differences* and 95% confidence intervals for hypertension and diabetes among Chinese Asians, American Whites, and American Blacks by body mass index categories, the Atherosclerosis Risk in Communities Study (1987–1998) and the People’s Republic of China Study (1983–1994).
| Body mass index categories |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <18.5 |
18.5–<23.0 |
23.0–<25.0 |
25.0–<27.5 |
27.5–<30.0 |
30.0–<32.5 |
≥32.5 |
||||||||
| Adjusted risk (%) |
95% confidence interval |
Adjusted risk (%) |
95% confidence interval |
Adjusted risk (%) |
95% confidence interval |
Adjusted risk (%) |
95% confidence interval |
Adjusted risk (%) |
95% confidence interval |
Adjusted risk (%) |
95% confidence interval |
Adjusted risk (%) |
95% confidence interval |
|
| Hypertension | ||||||||||||||
| Chinese Asians | −5.8 | −22.9, 11.2 | 0.0 | Referent | 7.5 | −7.2, 22.1 | 17.3 | −13.7, 48.2 | 18.1 | −26.7, 63.0 | ||||
| American Whites | 0.0 | Referent | 4.5 | −2.6, 11.5 | 7.6 | −2.6, 17.8 | 10.7 | −4.1, 25.5 | 14.1 | −7.8, 36.0 | 16.3 | −8.7, 41.3 | ||
| American Blacks | 0.0 | Referent | 6.8 | −5.9, 19.5 | 8.6 | −4.9, 22.1 | 11.6 | −5.8, 28.9 | 16.6 | −8.6, 41.8 | 24.5 | −1.2, 50.2 | ||
| Diabetes | ||||||||||||||
| Chinese Asians | −1.6 | −24.7, 21.5 | 0.0 | Referent | 4.9 | −30.6, 40.4 | 9.7 | −57.3, 76.6 | 14.5 | −94.3, 123.3 | 18.9 | −186.7, 224.5 | ||
| American Whites | 1.9 | −34.8, 38.5 | 0.0 | Referent | 1.7 | −6.0, 9.4 | 4.6 | −10.1, 19.3 | 8.8 | −17.5, 35.2 | 14.1 | −27.0, 55.2 | 21.4 | −29.2, 72.0 |
| American Blacks | 0.0 | Referent | 5.1 | −17.3, 27.6 | 7.6 | −17.9, 33.0 | 12.1 | −23.1, 47.3 | 15.2 | −29.9, 60.4 | 23.7 | −26.9, 74.2 | ||
Adjusted to represent values for nonsmokers and nondrinkers at age 53.2 years and for the distributions of gender, education, and field center at baseline. Risk differences were calculated by body mass index category 18.5−<23.0 as the referent.
FIGURE 3.
Percent increase per body mass index unit (and 95% confidence interval) from weighted least-squares regression of risk differences for hypertension and diabetes over full and restricted (18.5–<30.0 kg/m2) body mass index ranges by ethnicity, the Atherosclerosis Risk in Communities Study (1987–1998) and the People’s Republic of China Study (1983–1994).
For hypertension, the slope was steepest in the Asians and similar between Whites and Blacks. All tests for trend were statistically significant at p < 0.05. For each body mass index increment, the incidence of hypertension over approximately 8 years of follow-up increased by 2.5, 1.7, and 1.8 percentage points for Asians, Whites, and Blacks, respectively, in the restricted analysis.
For diabetes, the estimate of the slope in Asians tended to be higher in the restricted compared with the full analysis. Asians and Whites had similar slopes in the full analysis, whereas, in the restricted analysis, the slope was higher in the Asians. In the restricted analysis, the estimates increased by 1.7, 1.1, and 1.6 percentage points per body mass index unit for Asians, Whites, and Blacks, respectively. There were no differences between Asians and Blacks in either analysis; however, the slope tended to be higher in the Blacks than in the Whites in both analyses.
DISCUSSION
This analysis presents evidence that the difference in the incidence of hypertension and diabetes associated with body mass index was greater in Chinese Asians than in American Whites. For hypertension, this was true with or without the data restricted to a common body mass index range. However, for diabetes, the difference was seen only when comparing Asians and Whites over the same body mass index range. In contrast, when studied over the same body mass index range, the risk associated with body mass index was similar in Asians and Blacks for both diabetes and hypertension.
The published study that is probably the most comparable with the one presented here examined cross-sectional associations between body mass index and hypertension in data from the China Health and Nutrition Survey (1997), the Third National Health and Nutrition Examination Survey (1988–1994), and the Cebu Longitudinal Health and Nutrition Survey (15). The authors compared absolute rates and odds ratios among Chinese adults living in China; nonHispanic White, non-Hispanic Black, or Mexican-American adults living in the United States; and Filipino women living in the Philippines. A higher body mass index was associated with a higher prevalence of hypertension in all ethnic groups. Further, results suggested a stronger association between body mass index and hypertension in Chinese men and women compared with non-Hispanic Whites. NonHispanic Blacks and Filipino women had a higher prevalence of hypertension at every level of body mass index examined compared with non-Hispanic Whites and Mexican Americans. These results are in agreement with our results showing higher body mass index-adjusted prevalence estimates in Chinese Asians compared with American Whites, but not compared with American Blacks.
An additional study that compared Asians of Chinese descent with Caucasians of European descent used data from four ethnic groups living in Canada (16). The investigators used principal components factor analysis to examine associations between body mass index and the prevalence of factors related to glucose metabolism, lipid metabolism, and blood pressure. For a given body mass index, elevated levels of glucose-related factors were more likely to be present in South Asians, Chinese, and Aboriginals compared with Caucasians. Elevated levels of blood pressure were observed more often in Chinese than in Caucasians across body mass index levels. Analyses were conducted on the absolute levels of the factors, and therefore increases due to body mass index were not separated from ethnic differences due to other variables. For example, across body mass index levels, the glucose factor was consistently higher in Chinese than in Caucasians, but since the slopes of the associations appeared to be similar, there was no indication that the body mass index-associated risk differed between the groups.
Two additional studies (18, 21) that included Chinese Asians and Whites reported the prevalence of hypertension and the mean body mass index, but they did not show the prevalence of hypertension adjusted for body mass index or examine the associations between body mass index and hypertension. Hu et al. (21) examined the prevalence of hypertension, overweight, and obesity in Whites living in Finland and Chinese in China and found that the prevalences of hypertension, overweight, and obesity were all higher in the Finnish sample; however, associations between body mass index and hypertension were not examined. Similarly, a 1992 report (18) from the baseline examination of the PRC Study contrasted mean body mass index levels and the prevalence of hypertension in Chinese Asians and non-Hispanic Whites and non-Hispanic Blacks from the Second National Health and Nutrition Examination Survey (1976–1980). Although there were numerous differences in the exclusion criteria and the definitions of variables between that study and the work presented here, those investigators also found that body mass index levels were higher in both American groups than in the Chinese and that the crude prevalence of hypertension was highest in non-Hispanic Blacks, intermediate in non-Hispanic Whites, and lowest in the Chinese men and women. The differences observed in hypertension prevalence among ethnic groups were likely driven by the very different body mass index distributions, as well as by other factors.
Although the current study did find higher body mass index-adjusted incidence rates of hypertension and diabetes in Chinese Asians than in American Whites and American Blacks, the baseline prevalence rates were not always higher in Chinese Asians. In fact, the body mass index-adjusted prevalences of hypertension and diabetes were much greater in American Blacks than in Chinese Asians and American Whites. American Blacks may have been more sensitive to body mass index at a younger age than Chinese Asians and American Whites, or they may have had a higher prevalence of hypertension for reasons unrelated to body mass index (22, 23).
Several studies have shown that body composition (8, 12) and risks associated with obesity (16, 24, 25) can differ in Asians depending on the geographic location or nationality of the sample studied. Similarly, Whites (12) and Blacks (26) in diverse environments are different. The environmental and social differences between China and the United States are vast, and some of these differences likely influence the impact of body mass index on hypertension and diabetes. Many important covariates may not have been measured, and covariates that were measured and included in models may not have been comparable. For instance, a college education may not carry the same significance for health outcomes in China as in the United States, and the cigarettes smoked in the two locales are likely to be of different brands and potentially different levels of nicotine and other active ingredients. In this analysis, we cannot differentiate the impact of environmental and social differences from any genetic differences between the groups, and no attempt is made to do so. In addition, the baseline data studied here were collected approximately two decades ago and may not well represent either the Chinese or the American population today.
Another limitation of this study was that the subjects studied were not selected as a nationally representative sample in either China or the United States, although they were representative of their communities. The study designs of the PRC and the ARIC studies were not perfectly matched, and visits took place in different years and at different intervals. This is of some concern, although the total follow-up time was very similar for Chinese Asians (8.2 years), American Whites (8.2 years), and American Blacks (7.9 years).
This work has numerous strengths. We were fortunate to identify data collected using the same coordinating center and similar methodologies in diverse populations. Repeated measures over time that included laboratory and clinical assessments collected with comparable high-quality methods provided a rich resource for this work. The longitudinal design used here allowed us to establish that the exposure preceded the disease. In cross-sectional studies of associations between obesity and morbid outcomes, there is potential for reverse causality because illness or even the presence of a risk factor can result in metabolic changes (e.g., glucose tolerance) and behavioral changes (e.g., diet and physical activity), which can in turn influence body weight.
To our knowledge, this is the first study to compare associations of cardiovascular disease risk factors with body mass index between Asians and other ethnic groups by use of risk difference as the criterion measure. Although no one measure of effect is uniformly superior, we feel a comparison of risk differences is the best approach for studies comparing body mass index-associated risk factors in diverse groups in which the rates of disease vary in the body mass index reference group (17). Another strength of our analysis was the restriction of body mass index levels to a common range in which all three ethnic groups were adequately represented. The results were somewhat different in the full analysis compared with the analysis of the restricted range. The distributions of body mass index are extremely different between Chinese Asians and American Whites and Blacks. The restricted analysis was more comparable across groups and included the range of body mass index most relevant to weight concerns in Asians.
Investigators who support the need for lower cutpoints for obesity among Asian populations often point to data that show increased risk of disease-related outcomes at body mass indexes lower than 25.0 kg/m2 (16, 27-31). Implicit in their arguments is the assumption that, among individuals of European descent (the primary population studied in the derivation of the cutpoints of 25 and 30 kg/m2), there is a threshold at a body mass index of 25.0 kg/m2 where the slope of the association between body mass index and disease risk converts from flat to positive (7). Our results do not support this argument and, although differences were not statistically significant, for both outcomes examined here, the rates in the 23.0–<25.0 kg/m2 group were consistently higher than those in the 18.5–<23.0 kg/m2 group in all ethnic groups, and there was a statistically significant trend over body mass index levels.
The World Health Organization Expert Consultation on appropriate body mass index for Asian populations (3) made a distinction between the cutpoints used to define a disease, such as obesity, and the cutpoint chosen for public health and medical action within a country. We have previously published our rationale for discouraging the use of different cutpoints to define obesity in different ethnic groups (7). Nevertheless, we support the use of different body mass index cutoffs to indicate action levels in different countries. We support advocacy of public health and medical actions in China to reduce excess weight and prevent excess weight gain. The distribution of body mass index in China is rapidly moving to the right (32, 33), and it is appropriate to emphasize the consequences of this shift on the health of the Chinese population. It is our hope that studies such as this that demonstrate the increased risk of development of hypertension and diabetes with increasing body mass index among Chinese Asians will stimulate these efforts.
ACKNOWLEDGMENTS
The Atherosclerosis Risk in Communities (ARIC) Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts N01-HC-55015, N01-HC-55016, N01-HC-55018, N01-HC-55019, N01-HC-55020, N01-HC-55021, and N01-HC-55022. The People’s Republic of China (PRC) Study was carried out by the National Heart, Lung, and Blood Institute under contracts N01-HV-12243, N01-HV-08112, and N01-HV-59224 with the University of North Carolina, Chapel Hill, North Carolina, and the People’s Republic of China Ministry of Public Health, the Cardiovascular Institute and Fu Wai Hospital, Chinese Academy of Medical Sciences, Beijing, and the Guangdong Provincial Cardiovascular Institute, Guangzhou. This research was supported in part by a grant (RR00046) from the General Clinical Research Centers’ program of the Division of Research Resources, National Institutes of Health, and by a grant (R01 DK069678) from the National Institute of Diabetes and Digestive and Kidney Diseases.
The authors thank the staff of the ARIC Study and the staff of the PRC Study for their important contributions.
Abbreviations
- ARIC
Atherosclerosis Risk in Communities
- PRC
People’s Republic of China
Footnotes
Conflict of interest: none declared.
REFERENCES
- 1.Hu FB, Wang B, Chen C, et al. Body mass index and cardiovascular risk factors in a rural Chinese population. Am J Epidemiol. 2000;151:88–97. doi: 10.1093/oxfordjournals.aje.a010127. [DOI] [PubMed] [Google Scholar]
- 2.National Institutes of Health Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. Obes Res. 1998;6(suppl 2):51S–209S. [PubMed] [Google Scholar]
- 3.WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 4.Misra A. Revisions of cutoffs of body mass index to define overweight and obesity are needed for the Asian-ethnic groups. Int J Obes Relat Metab Disord. 2003;27:1294–6. doi: 10.1038/sj.ijo.0802412. [DOI] [PubMed] [Google Scholar]
- 5.Stevens J. BMI cutoffs for obesity should not vary by ethnic group. In: Medeiros-Neto G, Halpern A, Bouchard C, editors. Progress in obesity research: 9. Chap 116. John Libbey Eurotext Ltd; Montrouge, France: 2003. pp. 554–7. [Google Scholar]
- 6.Stevens J. Ethnic-specific cutpoints for obesity vs country-specific guidelines for action. Int J Obes Relat Metab Disord. 2003;27:287–8. doi: 10.1038/sj.ijo.0802255. [DOI] [PubMed] [Google Scholar]
- 7.Stevens J. Ethnic-specific revisions of body mass index cutoffs to define overweight and obesity in Asians are not warranted. Int J Obes Relat Metab Disord. 2003;27:1297–9. doi: 10.1038/sj.ijo.0802417. [DOI] [PubMed] [Google Scholar]
- 8.Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3:141–6. doi: 10.1046/j.1467-789x.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- 9.Gurrici S, Hartriyanti Y, Hautvast JG, et al. Relationship between body fat and body mass index: differences between Indonesians and Dutch Caucasians. Eur J Clin Nutr. 1998;52:779–83. doi: 10.1038/sj.ejcn.1600637. [DOI] [PubMed] [Google Scholar]
- 10.Norgan NG. Population differences in body composition in relation to the body mass index. Eur J Clin Nutr. 1994;48(suppl 3):S10–25. discussion S26-7. [PubMed] [Google Scholar]
- 11.Wang J, Thornton JC, Russell M, et al. Asians have lower body mass index (BMI) but higher percent body fat than do whites: comparisons of anthropometric measurements. Am J Clin Nutr. 1994;60:23–8. doi: 10.1093/ajcn/60.1.23. [DOI] [PubMed] [Google Scholar]
- 12.Deurenberg P, Yap M, van Staveren WA. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord. 1998;22:1164–71. doi: 10.1038/sj.ijo.0800741. [DOI] [PubMed] [Google Scholar]
- 13.Rush E, Plank L, Chandu V, et al. Body size, body composition, and fat distribution: a comparison of young New Zealand men of European, Pacific Island, and Asian Indian ethnicities. N Z Med J. 2004;117:U1203. [PubMed] [Google Scholar]
- 14.Rush EC, Goedecke JH, Jennings C, et al. BMI, fat and muscle differences in urban women of five ethnicities from two countries. Int J Obes (Lond) 2007;31:1232–9. doi: 10.1038/sj.ijo.0803576. [DOI] [PubMed] [Google Scholar]
- 15.Colin Bell A, Adair LS, Popkin BM. Ethnic differences in the association between body mass index and hypertension. Am J Epidemiol. 2002;155:346–53. doi: 10.1093/aje/155.4.346. [DOI] [PubMed] [Google Scholar]
- 16.Razak F, Anand SS, Shannon H, et al. Defining obesity cut points in a multiethnic population. Circulation. 2007;115:2111–18. doi: 10.1161/CIRCULATIONAHA.106.635011. [DOI] [PubMed] [Google Scholar]
- 17.Stevens J, Juhaeri, Cai J, et al. The effect of decision rules on the choice of a body mass index cutoff for obesity: examples from African American and white women. Am J Clin Nutr. 2002;75:986–92. doi: 10.1093/ajcn/75.6.986. [DOI] [PubMed] [Google Scholar]
- 18.People’s Republic of China-United States Cardiovascular and Cardiopulmonary Epidemiology Research Group An epidemiological study of cardiovascular and cardiopulmonary disease risk factors in four populations in the People’s Republic of China. Baseline report from the P.R.C.-U.S.A. Collaborative Study. Circulation. 1992;85:1083–96. doi: 10.1161/01.cir.85.3.1083. [DOI] [PubMed] [Google Scholar]
- 19.The ARIC investigators The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 20.Oehlert GW. A note on the delta method. Am Stat. 1992;46:27–9. [Google Scholar]
- 21.Hu G, Pekkarinen H, Halonen P, et al. Different worlds, different tasks for health promotion: comparisons of health risk profiles in Chinese and Finnish rural people. Health Promot Int. 2001;16:315–20. doi: 10.1093/heapro/16.4.315. [DOI] [PubMed] [Google Scholar]
- 22.Manton KG, Poss SS, Wing S. The black/white mortality crossover: investigation from the perspective of the components of aging. Gerontologist. 1979;19:291–300. doi: 10.1093/geront/19.3.291. [DOI] [PubMed] [Google Scholar]
- 23.Wing S, Manton KG, Stallard E, et al. The black/white mortality crossover: investigation in a community-based study. J Gerontol. 1985;40:78–84. doi: 10.1093/geronj/40.1.78. [DOI] [PubMed] [Google Scholar]
- 24.Bell CA, Adair LS, Popkin BM. Ethnic differences in the association between body mass index and hypertension. Am J Epidemiol. 2002;155:346–53. doi: 10.1093/aje/155.4.346. [DOI] [PubMed] [Google Scholar]
- 25.Nakagami T, Qiao Q, Carstensen B, et al. Age, body mass index and type 2 diabetes—associations modified by ethnicity. Diabetologia. 2003;46:1063–70. doi: 10.1007/s00125-003-1158-9. [DOI] [PubMed] [Google Scholar]
- 26.Luke A, Durazo-Arvizu R, Rotimi C, et al. Relation between body mass index and body fat in black population samples from Nigeria, Jamaica, and the United States. Am J Epidemiol. 1997;145:620–8. doi: 10.1093/oxfordjournals.aje.a009159. [DOI] [PubMed] [Google Scholar]
- 27.Lin S, Cheng TO, Liu X, et al. Impact of dysglycemia, body mass index, and waist-to-hip ratio on the prevalence of systemic hypertension in a lean Chinese population. Am J Cardiol. 2006;97:839–42. doi: 10.1016/j.amjcard.2005.09.133. [DOI] [PubMed] [Google Scholar]
- 28.Bei-Fan Z. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults: study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Asia Pac J Clin Nutr. 2002;11(suppl 8):S685–93. [PubMed] [Google Scholar]
- 29.Weng X, Liu Y, Ma J, et al. Use of body mass index to identify obesity-related metabolic disorders in the Chinese population. Eur J Clin Nutr. 2006;60:931–7. doi: 10.1038/sj.ejcn.1602396. [DOI] [PubMed] [Google Scholar]
- 30.Wildman RP, Gu D, Reynolds K, et al. Appropriate body mass index and waist circumference cutoffs for categorization of overweight and central adiposity among Chinese adults. Am J Clin Nutr. 2004;80:1129–36. doi: 10.1093/ajcn/80.5.1129. [DOI] [PubMed] [Google Scholar]
- 31.Zhou BF. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases—report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed Environ Sci. 2002;15:245–52. [PubMed] [Google Scholar]
- 32.Ji CY. Report on childhood obesity in China (4) prevalence and trends of overweight and obesity in Chinese urban school-age children and adolescents, 1985–2000. Biomed Environ Sci. 2007;20:1–10. [PubMed] [Google Scholar]
- 33.Wang H, Du S, Zhai F, et al. Trends in the distribution of body mass index among Chinese adults, aged 20–45 years (1989–2000) Int J Obes (Lond) 2007;31:272–8. doi: 10.1038/sj.ijo.0803416. [DOI] [PubMed] [Google Scholar]