ABSTRACT
Purpose: The purpose of this article is to apply theoretical frameworks to adherence behaviour and to guide the development of an intervention to increase adherence to prescribed home programmes.
Summary of Key Points: Delivering an effective intervention requires establishing one that is evidence based and of adequate dosage. Two-thirds of patients who receive home exercise prescriptions do not adhere to their home programme, which may contribute to their physiotherapy's being ineffective. The mediating concepts of self-efficacy (SE) and outcome expectations (OE) are common to the five relevant theories used to explain adherence to exercise: the health belief model, protection motivation theory, theory of reasoned action, theory of planned behaviour, and social cognitive theory.
Conclusion/Recommendations: Few intervention studies with any theoretical underpinning have examined adherence to exercise. Even fewer have been designed to affect and measure change in the theoretical mediators of SE and OE in patient populations. Physiotherapists must consider increasing adherence as a component of effective physiotherapy. Ongoing research is needed to increase our understanding of adherence to prescribed home programmes and to design interventions to affect theoretical mediators for increasing adherence.
Key Words: adherence, learning, motor, practice, theory
RÉSUMÉ
Objectif : L'objectif du présent article est d'appliquer des cadres théoriques aux comportements de fidélité au traitement et d'orienter l'élaboration d'une intervention visant à augmenter la fidélité aux programmes à domicile prescrits.
Sommaire des points clés : La mise en place d'une intervention efficace repose sur une démarche fondée sur des preuves et sur une dose suffisante. Deux-tiers des patients qui reçoivent des prescriptions d'exercice à domicile dérogent au programme, ce qui pourrait contribuer à l'inefficacité de la physiothérapie. Les concepts médiateurs d'autoefficacité et d'attentes en matière de résultats s'insèrent dans les cinq théories pertinentes utilisées pour expliquer la fidélité à un programme d'exercice : modèle de croyance à la santé, théorie de la motivation à la protection, la théorie de l'action raisonnée, la théorie du comportement axé sur un objectif et la théorie sociale cognitive.
Conclusion et recommandations : Il existe peu d'essais sur le terrain s'appuyant sur des fondements théoriques qui portent sur la fidélité aux programmes d'exercice. Il existe encore moins d'essais sur le terrain visant à provoquer et à mesurer le changement dans les facteurs médiateurs théoriques de l'autoefficacité et des attentes en matière de résultats dans les populations à l'étude. Les physiothérapeutes doivent envisager la fidélité accrue comme l'un des éléments d'une physiothérapie efficace. Il faut entreprendre des études continues afin d'augmenter notre compréhension de la fidélité aux programmes à domicile prescrits et de concevoir des interventions qui auront une incidence sur les facteurs médiateurs théoriques destinés à augmenter la fidélité.
Mots clés: fidélité, apprentissage, moteur, pratique, théorie
INTRODUCTION
Mr. A is a 68-year-old man who is seen at your outpatient physiotherapy clinic one year after right middle cerebral artery infarct. Following his stroke, he spent 2 weeks on an acute in-patient ward, 6 weeks in in-patient rehabilitation, and 6 weeks in a day hospital outpatient programme. His past medical history includes hypertension and hyperlipidemia. He is a retired grandfather who enjoys gardening. His goal is to improve his walking. He says he is having difficulty with his walking because his balance is “not quite there” and he tires easily. Mr. A arrives walking with a single-point cane.
After your assessment, you provide a programme of walking practice and plan to see Mr. A in 1 week. The next week, when Mr. A arrives for his appointment, he states that he has not had the time to practice his walking. What do you say? How effective was your prescribed therapy? How effective will it be next week?
The importance of the concept of motor skill practice in theories of brain neuroplasticity and motor learning is well established.1,2 The theory of brain neuroplasticity states that the adult brain is modifiable with experience and after injury;1 and practice of motor skills is integral to these structural and functional brain changes.1 The theory of brain neuroplasticity is supported by research using brain-mapping techniques (e.g., positron emission tomography, or PET) to view changes in brain topography corresponding with motor skill practice.1 Research supports motor learning theorists' propositions that the amount of practice is the most important factor in motor learning theory and that more practice is better.2 The goal of motor learning theorists is to optimize practice so that skill acquisition can take place efficiently.2
For motor learning, practice of therapist-prescribed activities must also take place outside of the therapy environment; hence, home programmes are prescribed.3 Patients' adherence to prescribed regimens is poor, however, and the effectiveness of home programmes is questionable.4–7 Based a meta-analysis of 569 studies from 1948 through 1998, Di Matteo8 calculated an average rate of non-adherence to medical treatment of 24.8%. According to this meta-analysis, rates of adherence to medical regimens that are more defined (e.g., taking medication), are higher than rates of adherence to more pervasive regimens (e.g., health behaviours).8 Studies investigating patients' rates of adherence to prescribed programmes of physical activity find that between one-third and two-thirds of patients do not follow their prescribed regimen.5–7 The true rate of non-adherence is likely higher, since many studies of adherence use self-report measures and patients may not report a lack of adherence.
Delivery of an effective home programme relies on establishing an evidence-based intervention and ensuring an adequate dosage.9 Establishing an evidence-based intervention continues to be a major goal in the evolution of physiotherapy. Ensuring an adequate dosage (i.e., adherence to the evidence-based intervention) has received significantly less attention. The cost of non-adherence by people with stroke in Ontario brings to the foreground the importance of increasing adherence rates. As estimated by Chan and Hayes, the direct costs of stroke in Ontario for the fiscal year April 1994 to March 1995 ranged from $431.4 million to $578.4 million.10 A 24.8% rate of non-adherence, as documented by DiMatteo,8 can thus be estimated to cost the province of Ontario between $106.99 million and $143.44 million per year. Today, this admittedly crude but conservative estimate of non-adherence is likely higher, given the ageing population and the expectation of an increase in the incidence of stroke.11 The risk that physiotherapy will be deemed ineffective is another consequence of non-adherence: many otherwise effective physiotherapy interventions may be abandoned because patients receive an insufficient dosage.9 A crucial question thus exists: How can physiotherapists ensure that an adequate dosage is established for effective intervention? To address this question, physiotherapists need to understand patients' lack of adherence and implement strategies to increase adherence to prescribed intervention programmes. The objectives of this paper are (1) to discuss the role of theory in understanding adherence behaviour, (2) to present theoretical frameworks to guide the development of an intervention to increase adherence behaviour, and (3) to review and discuss the applicability of current adherence interventions in increasing adherence to prescribed practice.
THE IMPORTANCE OF THEORY
If adherence to prescribed home programmes is to be increased, adherence behaviour must be understood. Explanations of adherence behaviour take the form of theories. A theory is a “coherent and non-contradictory set of statements, concepts or ideas that organizes, predicts and explains phenomena, events, behavior, etc.”12(p.2) Theories are commonly used in clinical fields. Phase I and II drug trials are an example of a definitive test of a number of interrelated theories from physiology (enzymatic function), pathology (disease pathways), and pharmacology.12 A theory is developed from the successes and failures of previous investigations.13 Employing a theoretical foundation as a first step to solving a clinical problem increases the likelihood of furthering prior successes and avoiding prior failures.13 To use a theory to understand, for example, adherence behaviour, and to examine the comprehensiveness of the theory to explain that behaviour, we must operationalize the theory: each concept is defined and then measured using an assessment tool, and the relationships or theoretical assumptions that exist between concepts are examined.
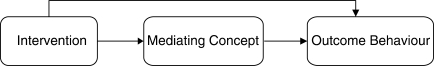
Using a theory to develop an intervention to effect change in an outcome begins with identifying the concepts within the theory that are mediators of change.14 A mediator is a concept, or a series of concepts, that can account for the effect an intervention produces on an outcome (see Figure 1). In a comprehensive theory, change in the mediator(s) must take place to produce a change in the outcome. Therefore, an intervention designed to target and produce a change in the mediators should ultimately effect change in an outcome.14 It is important to measure change in the mediator(s) to explain variability in the outcome and the effectiveness of the intervention. If an intervention produces a change in the outcome that is not explained by mediating concepts, the theoretical framework may not be complete and other mediators need to be identified.14
Figure 1.
The role of the mediator
UNDERSTANDING ADHERENCE BEHAVIOUR
There is a wealth of research on adherence to exercise. To date, researchers have identified more than 200 variables that correlate with adherence to exercise,7 which have been organized into the following categories:
the patient (e.g., beliefs, expectancies about health and treatment)
the disease (e.g., chronicity, severity, complicating factors)
treatment of the disease (e.g., complexity, duration, side effects)
the patient's relationship to the health care provider (e.g., supervision, provision of positive feedback, clear instructions and rationale for instructions, making a link between prescribed regimen and patients' own beliefs)6,13
Several general theoretical frameworks from the literature in health psychology are useful in understanding adherence to exercise: the health belief model,15 protection motivation theory,16,17 theory of reasoned action,18 theory of planned behaviour,19–21 self-efficacy theory,22 and social cognitive theory (SCT).23,24 These theories share common assumptions that are characteristic of cognitive-behavioural theories: that people (1) are able to use foresight, planning, and decision-making processes (cognitive processes), and (2) are goal directed and self-regulating (behaviour).13 Both assumptions emphasize the active role of the person.
In a physiotherapy setting, a patient's adherence is usually to a prescribed home programme for a treatment goal and during a treatment period when there is contact with the therapist or the therapy setting.7 Adherence behaviour is specific to a task (e.g., walking). The application of a theory to understand adherence behaviour is specific to factors of the adherence behaviour.7 Consider the clinical scenario with Mr. A. Some factors that make this application distinct are (1) the patient, Mr. A, who has experienced a significant loss of independence and who is pursuing improved walking ability in order to return to a previous level of function, ranging from basic activities of daily living (e.g., walking to access the bathroom) to more advanced functional activities (e.g., independent grocery shopping); (2) the type of activity for adherence (i.e., walking practice prescribed to make a progressive change in the patient's function); and (3) Mr. A's environment, which, especially in the presence of functional limitations, can either facilitate or impede adherence to walking practice. The paragraphs below illustrate each theory with application to the clinical example of Mr. A and adherence to prescribed walking practice. Theoretical concepts are given in italics.
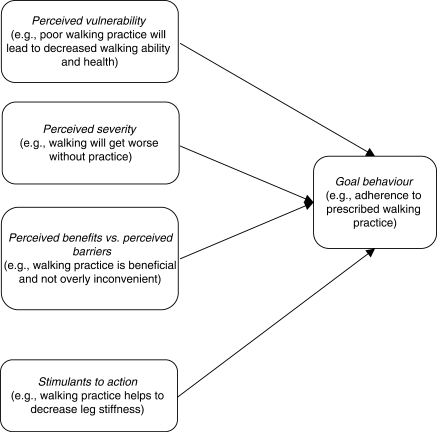
Health Belief Model
The health belief model was proposed by Rosenstock in 196615 (see Figure 2). According to this model, adherence to the prescribed walking practice is most likely to occur when Mr. A (1) perceives that his limited walking ability makes him more vulnerable to poorer health (perceived vulnerability), (2) perceives that his walking will get worse if he does not adhere to the prescribed walking practice (perceived severity), (3) believes that the prescription is beneficial and is not overly inconvenient (perceived benefits vs. perceived barriers), and (4) notices that on days when he does not practise walking, he experiences increased leg stiffness (stimulants to action). The health belief model has been revised by Rosenstock15 to incorporate the concept of self-efficacy within the concept of efficacy expectation. Efficacy expectation, in our example, is defined as Mr. A's belief that he is capable of adhering to the prescribed walking practice.15
Figure 2.
The health belief model
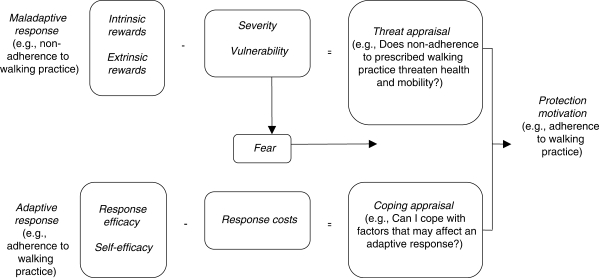
Protection Motivation Theory
Protection motivation theory was proposed by Rogers in 1983 (see Figure 3).16,17 According to this theory, adherence to prescribed walking practice is determined by Mr. A's overall appraisal of threats and coping. Threat appraisal requires Mr. A to decide whether not engaging in walking practice (maladaptive response) poses a threat to his health and mobility (severity/vulnerability). Mr. A's appraisal of threat also incorporates intrinsic and extrinsic rewards that may increase the probability of a maladaptive response (e.g., if he does not practice his walking, he can watch his favourite television shows and feel more rested from lying on the couch). Coping appraisal focuses on Mr. A's ability to cope with these threats and on factors that may increase or decrease the probability of an adaptive response (in this case, adherence to walking practice). Mr. A is likely to adhere to walking practice if he perceives adherence to be an effective means to improve his walking (response efficacy), if he believes that he is capable of adhering to the practice (self-efficacy), and if he perceives few, if any, response costs (e.g., muscle fatigue).
Figure 3.
Protection motivation theory
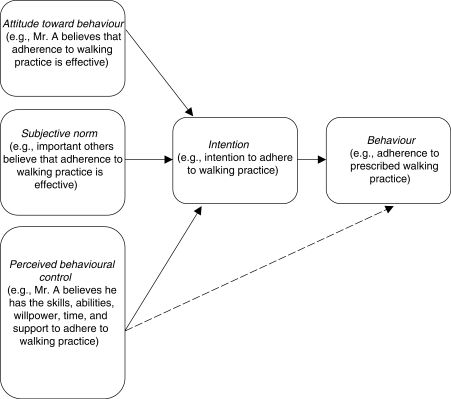
The Theory of Reasoned Action and the Theory of Planned Behaviour
The theory of reasoned action, proposed by Ajzen and Fishbein in 1980,18–20 states that Mr. A's intention to adhere to walking practice is established by his perception that adherence is effective (attitude toward the behaviour) and that other people important to him believe this also (subjective norm). The theory of reasoned action was renamed by Ajzen in 198519 as the theory of planned behaviour and revised to account for a third concept determining intention: perceived behavioural control (see Figure 4).19–21 Based on this revision, Mr. A's belief that he has the skills, abilities, willpower, time, and support needed to adhere to prescribed walking practice will strengthen his intention, and ultimately his actions, to adhere to his walking practice.
Figure 4.
Theory of planned behaviour
Self-Efficacy Theory
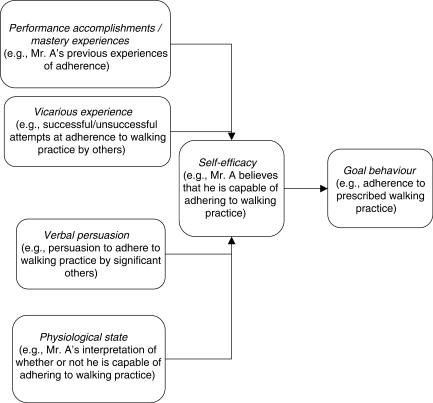
Self-efficacy theory was proposed by Bandura in 1977 (see Figure 5).22 Self-efficacy is defined as a person's belief in his or her ability to perform a specific task (self-efficacy for the task) and his or her ability to change him- or herself by exerting control over inner processes of goal setting, self-monitoring, incorporating feedback, problem solving, and self-evaluating (self-efficacy for self-regulation).25 According to self-efficacy theory, Mr. A will adhere to the prescribed walking practice if he believes that he is capable of performing the motor skill of walking and if he believes that he is capable of goal setting, self-monitoring, incorporating feedback, problem solving, and self-evaluating in order to adhere to his walking practice. His beliefs are influenced by (1) his previous experiences of adherence (mastery experiences), (2) his observations of successful or unsuccessful attempts at adherence by others (vicarious experience), (3) persuasion to adhere by significant others (verbal persuasion), and (4) how he interprets associated experiences (physiological state; e.g., if he feels anxious, he may interpret this as an indication of not being capable of adherence, but if he is able to overcome the anxiety, his belief in his capability to adhere may be strengthened).
Figure 5.
Self-efficacy theory
Social Cognitive Theory
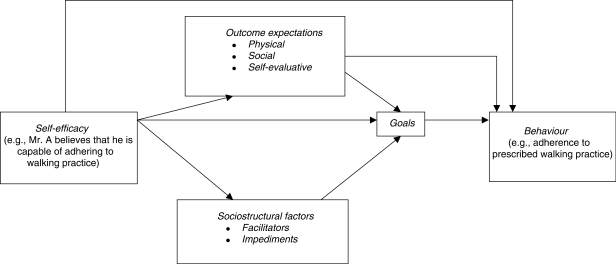
Social cognitive theory (SCT) was proposed by Bandura in 198623,24 (see Figure 6). According to this theory, Mr. A's belief that he is capable of adhering to the prescribed walking practice (self-efficacy) remains a key concept and mediator, influencing other concepts that affect adherence. Mr. A's self-efficacy influences his expectation of outcomes from adhering to the prescribed walking practice (outcome expectations), which then influences adherence. For example, with self-efficacy, Mr. A expects adherence to walking practice to improve his walking (physical outcomes), expects to be supported by society (social reactions), and expects adherence to walking practice to be self-satisfying (self-evaluative reactions). Outcome expectations can also be seen to play a mediating role in adherence to prescribed walking practice, because, with these positive expectations, Mr. A will likely adhere to a walking programme. Mr. A also considers his environment (sociostructural factors): a positive belief in his capability to adhere (self-efficacy) enables him to identify facilitators of adherence in his environment and to overcome various impediments. SCT proposes that positive perceptions of self-efficacy, outcome expectations, and sociostructural factors influence short-term goal setting; positive perceptions are reflected in higher attainable goals toward adherence.
Figure 6.
Social cognitive theory
Comparing the Theories
The health belief model,15 protection motivation theory,16,17 the theory of reasoned action,18 and the theory of planned behaviour19–21 are composed of concepts that have been defined as facets of the higher-order SCT constructs self-efficacy and outcome expectations23 (see Table 1). Most of these concepts are types of outcome expectations (e.g., perceived or expected severity/vulnerability, costs, and/or benefits).15–24 These theories posit direct15,23 and indirect16–20,23 relationships between outcome expectations and adherence (behaviour). A direct relationship between outcome expectations and adherence assumes that when outcome expectations increase, there is an increase in adherence. An indirect relationship between outcome expectation and adherence assumes that outcome expectation influences another theoretical concept, which then influences adherence. Concepts consistent with self-efficacy are found in all the theories outlined above except the theory of reasoned action.15–24 However, in the theory of planned behaviour, the concept of perceived behavioural control incorporates self-efficacy.19,20 The relationship between self-efficacy and adherence varies among theories; both direct15,19,20,23 and indirect16,17,19,20,23 relationships between self-efficacy and adherence have been proposed.
Table 1.
Overlapping Constructs of Social Cognitive Theory with Theories of Health Behaviour
| Theories of Health Behaviour | Social Cognitive Theory Constructs* |
|||
|---|---|---|---|---|
| Outcome Expectations | Self-Efficacy | Goals | Sociostructural Factors | |
| Health belief model | Perceived vulnerability, severity, benefits vs. barriers, stimulants to action | Efficacy expectations | – | – |
| Protection motivation theory | Coping appraisal, threat appraisal | Self-efficacy (incorporated within coping appraisal) | – | – |
| Theory of reasoned action | Intention | – | Intention | – |
| Theory of planned behaviour | Intention | Perceived behavioural control | Intention | – |
– indicates that the concept is not specifically represented in this theory.
The SCT concepts of goals and sociostructural factors have also been defined as higher-order constructs.23 However, only the theory of planned behaviour identifies self-efficacy, outcome expectancies, and goals as integral to understanding adherence. The goals construct is represented by the concept of intention in the theory of planned behaviour. Intentions are essentially proximal goals (i.e., behaviour that will take place within a relatively short period).18–20,23 The goals construct in SCT can be either distal or proximal; SCT is therefore different from the theory of planned behaviour in its ability to predict behaviour that may occur later in time. Finally, in SCT the construct sociostructural factors (facilitators and impediments) represents the influence a person's environment has on adherence. In the theory of planned behaviour, the concept of perceived behavioural control combines both internal factors (the individual's ability, skills, and willpower) and external factors (time, money, cooperation from other people). There is no distinct concept that captures environmental influences.19,23,26 The importance of a separate concept to represent a person's environment in establishing an intervention—in this case, to increase adherence behaviour—is supported by theoretical models of intervention.5,27,28
SCT takes the most comprehensive approach to representing the concepts that are proposed to influence adherence behaviour. SCT is inclusive of concepts identified by the health belief model, protection motivation theory, the theory of reasoned action, and the theory of planned behaviour, as well as of concepts that these theories overlook. SCT also has the potential to be the most successful at predicting adherence behaviour over a longer period.23 The remainder of this paper, therefore, uses SCT as a theoretical framework to understand what factors influence adherence to prescribed walking practice in an adult population post stroke and to explore existing interventions to increase adherence to prescribed practice.
Utility of the SCT Framework for Facilitating Adherence to Therapy
To date, most of the research examining adherence interventions in health care has focused on broad health issues, often involving a goal of preventing or maintaining a behaviour.8 The development of adherence interventions for broad health issues is being addressed.8 Less is known, however, about applying an adherence intervention as an adjunct to a specific physiotherapy treatment (e.g., increasing adherence to prescribed walking practice in a patient after stroke). Research investigating adherence to physical activity in healthy adults provides support for the ability of SCT to define mediators that are highly predictive of change.26,29 A study by Dzewaltowski et al.26 compared SCT to the theories of reasoned action and planned behaviour in predicting participation in physical activity among healthy adults over a 4-week period. These researchers found that the SCT concepts of self-efficacy and self-evaluation (a form of outcome expectation) significantly predicted participation in physical activity. McAuley et al.29 examined the ability of the SCT concept of self-efficacy to make predictions with respect to long-term exercise adherence. Healthy older adults participated in a group exercise programme over a 6-month period; a model with self-efficacy as a mediator of long-term exercise maintenance was evaluated. In this study, participants who exercised more frequently during the 6-month structured programme had more social support and positive exercise experience. This resulted in enhanced self-efficacy at 6 months and higher levels of exercise participation at the 6- and 18-month follow-up. Self-efficacy at the end of the 6-month exercise programme was predictive of activity level at 18 months.
A literature review was performed to search for interventions that increase adherence to prescribed walking practice in a post-stroke population via mediating variables from SCT. The literature search included the following databases: Allied and Complementary Medicine (AMED) and PsychINFO from 1985 to July 2008; MEDLINE from 1966 to July 2008; and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) from 1982 to July 2008. The search strategy included the following search terms: (adherence or compliance or cooperation or participation) and (exercise or practice or physical activity or physical therapy or physiotherapy) and (cognitive behavioural or social cognitive), limited to (human and English language and all adult [19 plus years]). Abstracts were reviewed, and studies were selected if (1) participants were recruited from a post-stroke patient population or from a population that was functionally limited, in order to capture an adherence intervention aimed at a treatment goal as opposed to a preventive or maintenance goal (often characteristic of intervention for broad health issues); and (2) the adherence intervention was provided in a one-on-one format, similar to what would be provided to Mr. A.
Three studies met the criteria outlined above;30–32 these were then reviewed to identify a theoretical underpinning of SCT. In only one of the three studies32 was the intervention directed at changing the theoretical mediators of the adherence behaviour. This study, by Harnirattisai et al.,32 measured change in self-efficacy and outcome expectancy and change in adherence behaviour. Sixty-three patients scheduled for knee replacements were followed for up to 6 weeks postoperatively. Individual goal-based exercise programmes were established for all patients. The experimental group attended two 25-minute sessions in the first and second postoperative weeks. These sessions provided information on sources of self-efficacy information, self-monitoring, identifying barriers to exercise behaviour, and recruiting family support. The experimental group was also given written information related to these topics. Harnirattisai et al. reported increased adherence to exercise activities, measured by differences in mean change scores in the Physical Performance Test between the experimental and control groups. From baseline to postoperative week 6, change scores for standing balance were 2.00 ± 1.22 for the experimental group versus 1.09 ± 1.22 for the control group (Wilcoxon Rank Sum Statistic (T+) = 512.0, p = 0.016); for walking speed, 1.55 ± 1.02 vs. 0.76 ± 0.83 (T+ = 479.0, p = 0.004); and for chair stand, 2.36 ± 1.05 vs. 1.33 ± 1.02 (T+ = 450.0, p = 0.001). Self-efficacy for exercise increased for the experimental group, as measured by differences in the mean change score in the Self Efficacy for Exercise scale between the experimental and control groups from baseline to postoperative week 6 (4.13 ± 1.23 vs. 1.55 ± 1.54; T+ = 26.5, p < 0.001). Outcome expectancy for exercise also increased for the experimental group, as revealed by the difference in mean change score between the experimental and control groups from baseline to postoperative week 6 on the Outcome Expectations for Exercise scale (0.56 ± 0.50 for the experimental group versus 0.08 ± 0.30 for the control group; T+ = 16.4, p < 0.001) and on the Outcome Expectations for Exercises and Functional Activity scale (0.17 ± 0.37 vs. -0.19 ± 0.37; T+ = 12.1, p < 0.001).
To gain a more comprehensive understanding of which interventions are effective for increasing practice in patient populations or in persons with functional limitations, the search criteria were broadened to include adherence interventions in group settings (i.e., we omitted selection criterion #2, but included patient populations where adherence was aimed at achieving a treatment goal). One study met these criteria.33 The adherence intervention in this study was based on SCT, but theoretical mediators of adherence were not assessed or measured for change. A group of 147 participants eligible for cardiac rehabilitation was randomized into one of two treatment groups: traditional cardiac rehabilitation (CRP) or group-mediated cognitive–behavioural intervention (GMCB). Both treatment groups had the same forms of exercise and equal numbers of contact hours over a 3-month period. The CRP group exercised 3 days per week for 3 months at the cardiac rehabilitation centre, and participants were asked to try to exercise also on days that they were not at the centre. The objective of the GMCB intervention was to wean participants from dependence on the centre-based exercise sessions to independence with self-regulation of home-based activities. Centre-based exercise sessions were scheduled twice per week during the first and second month, and once per week during the third month. After each session, participants in the GMCB intervention received 20 to 25 minutes of information and counselling on self-monitoring, goal setting, and strategies to overcome barriers and lapses related to physical activity; counselling was also aimed at raising participants' awareness of their progress. At the 3-month follow-up, adherence, measured by attendance at the centre and also by participation in the home programme for the GMCB group, had increased for the GMCB group (mean (SE) = 90.88% (2.65)) compared to the CRP group (mean (SE) = 77.88% (2.04)).
Because few studies had examined adherence to a specific physiotherapy goal in a patient population, selection criteria were broadened further to include studies that recruited participants from healthy adult populations (i.e., we omitted selection criterion #1). Abstracts were screened to identify studies that had some SCT underpinning. Four studies met these revised criteria.34–37 In each of these studies, an exercise maintenance phase followed the adherence intervention phase; successful maintenance involved participating in regular physical activity for at least 6 months following the end of an intervention.34 In these studies, follow-up for the maintenance phase ranged from 5 weeks to 12 months. Adherence interventions provided sources of self-efficacy34–36 and education on self-regulation skills.35,37 The experimental group in each study had significantly higher adherence than the control group. Across these studies, self-efficacy,34–37 outcome expectations,35 perceived benefits and barriers,34 and self-regulation35 were measured. Findings of these studies included an increase in self-efficacy,34–37 improved outcome expectations,35 and fewer barriers to physical activity34 for those participants with higher adherence. These studies also acknowledged35,36 and provided evidence35 for an emerging role of self-regulation, defined by Hallam et al.37(p.89) as “the skills used by the participant to implement exercise intentions and to overcome personal and situational barriers to a regular exercise programme.” Many theorists agree with Bandura22,38,39 that there are different types of self-efficacy, differentially related to degrees of exercise involvement. Self-efficacy theory defines self-efficacy as a person's belief in his or her ability to perform a specific task (self-efficacy for the task) and to change him- or herself by exerting control over inner processes of goal setting, self-monitoring, incorporating feedback, problem solving, and self-evaluating (self-efficacy for self-regulation). Task self-efficacy is viewed as a type of self-efficacy required for the initiation of the behaviour; self-efficacy for self-regulation is required for the maintenance of the behaviour. As these studies revealed,35,36 the role of self-efficacy for self-regulation becomes more prominent, while self-efficacy for the task assumes a less prominent role, once the adherence intervention phase ends and the exercise maintenance phase begins.
SUMMARY
It is evident from the literature review that few studies have used cognitive–behavioural interventions or specific social cognitive theory–based interventions to increase adherence to prescribed practice to a specific physiotherapy treatment goal in patient populations. Extrapolating from studies of healthy participants to attempt to understand adherence to prescribed practice in patient populations reveals the complex nature of adherence. In a clinical setting, a patient's adherence is usually to a prescribed programme toward a treatment goal during a period of contact with the therapist or the therapy setting.7 In studies of healthy participants, the objective of the adherence intervention is to facilitate long-term maintenance of physical activity such that contact with a therapist or programme instructor becomes minimal or absent.7
Using a theoretical framework to develop a theory-based intervention requires operationalizing the theory, identifying mediators, and designing interventions to target those mediators. Operationalizing a theory involves defining and measuring each concept and examining the relationships or theoretical assumptions that exist within each concept. A test of an intervention that targets the mediators of a theory must not only measure the primary outcome of the intervention but also measure the mediators to ensure that the intervention actually did what it was designed to do. The literature review found that few studies operationalized theory; instead, in an attempt to define and measure a concept, many studies completely detached theoretical concepts from their contextual framework, with no appreciation for the definition provided by the theoretical framework. Even fewer intervention studies revealed an appreciation for the role of a mediator. For example, interventions in such studies might be directed at the mediator self-efficacy to increase adherence, but only adherence was measured. Authors of these studies could only assume that the intervention was successful at targeting self-efficacy and effecting a change in adherence.30,31,40 Those studies that implemented SCT-based interventions32,34–36 used the four sources of self-efficacy (mastery experiences, vicarious experience, verbal persuasion, and physiological state), problem solving around barriers to adherence, and education on goal setting to guide adherence intervention. Identification of outcome expectations and socio-structural factors and education targeting these concepts were also used in an effort to increase adherence. Intervention sessions varied from 15 minutes to 1 hour in length and took place approximately once every 2 weeks.
DIRECTIONS FOR FUTURE RESEARCH
Physiotherapists must consider trying to increase patient adherence as a component of effective physiotherapy. Research is needed
to explore theoretical frameworks and apply theory to increase our understanding of patients' non-adherence to prescribed programmes;
to explore whether one theory (e.g., social cognitive theory) is the most comprehensive for all patient populations, or whether other theories provide better explanations for non-adherence in other patient populations;
to develop an adherence intervention derived from a theoretical framework and to test the success of the adherence intervention by measuring both the primary outcome of adherence and change in theoretical mediators; and
to provide physiotherapists with strategies that do not require the acquisition of a complex complementary skill set and can be incorporated into their practice to facilitate a patient's adherence to a prescribed programme.
Sirur R, Richardson J, Wishart L, Hanna S. The role of theory in increasing adherence to prescribed practice. Physiother Can. 2009; 61:68-77.
REFERENCES
- 1.Ploughman M. A review of brain neuroplasticity and implications for the physiotherapeutic management of stroke. Physiother Can. 2002;54:164–76. [Google Scholar]
- 2.Wishart L, Lee T, Ezekiel H, Marley T, Lehto N. Application of motor learning principles: the physiotherapy client as a problem-solver, 1: concepts. Physiother Can. 2000;52:229–32. [Google Scholar]
- 3.Marley T, Ezekiel H, Lehto N, Wishart L, Lee T. Application of motor learning principles: the physiotherapy client as a problem-solver, 2: scheduling practice. Physiother Can. 2000;53:315–20. [Google Scholar]
- 4.Osmotherly P, Higginbotham N. Assessing patient intention to perform a home based exercise programme for back and shoulder pain. Physiother Theory Pract. 2004;20:57–71. [Google Scholar]
- 5.Jensen G, Lorish C. Promoting patient cooperation with exercise programs: linking research, theory, and practice. Arthrit Care Res. 1994;7:181–9. doi: 10.1002/art.1790070405. [DOI] [PubMed] [Google Scholar]
- 6.Sluijs E, Kok G, van der Zee J. Correlates of exercise compliance in physical therapy. Phys Ther. 1993;73:771–82. doi: 10.1093/ptj/73.11.771. [DOI] [PubMed] [Google Scholar]
- 7.Sluijs E, Knibbe J. Patient compliance with exercise: different theoretical approaches to short-term and long-term compliance. Patient Educ Couns. 1991;17:191–204. [Google Scholar]
- 8.Di Matteo M. Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 9.Portney L, Watkins M. Foundations of clinical research. 2nd. Norwalk, CT: Appleton and Lange; 2000. [Google Scholar]
- 10.Chan B, Hayes B. Cost of stroke in Ontario, 1994/95. Can Med Assoc J. 1998;159:S2–8. [Google Scholar]
- 11.Heart and Stroke Foundation of Canada. The growing burden of heart disease and stroke. Ottawa: The Foundation; 2003. [Google Scholar]
- 12.Eccles M, Grimshaw J, Walker A, Johnston M, Pitts N. Changing the behavior of healthcare professionals: the use of theory in promoting the uptake of research findings. J Clin Epidemiol. 2005;58:107–12. doi: 10.1016/j.jclinepi.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Brawley L, Culos-Reed S. Studying adherence to therapeutic regimens: overview, theories, recommendations. Control Clin Trials. 2000;21:156S–63S. doi: 10.1016/s0197-2456(00)00073-8. [DOI] [PubMed] [Google Scholar]
- 14.Baranowski T, Lin L, Wetter D, Resnicow K, Hearn M. Theory as mediating variables: why aren't community interventions working as desired? Ann Epidemiol. 1997;S7:S89–95. [Google Scholar]
- 15.Rosenstock I, Strecher V, Becker M. Social learning theory and the health belief model. Health Educ Quart. 1988;15:171–83. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 16.Searle A, Vedhara K, Norman P, Frost A, Harrad R. Compliance with eye patching in children and its psychosocial effects: a qualitative application of protection motivation theory. Psychol Health Med. 2000;5:42–54. [Google Scholar]
- 17.McLendon B, Prentice-Dunn S. Reducing skin cancer risk: an intervention based on protection motivation theory. J Health Psychol. 2001;6:321–8. doi: 10.1177/135910530100600305. [DOI] [PubMed] [Google Scholar]
- 18.Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice Hall; 1980. [Google Scholar]
- 19.Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckman J, editors. Action-control: from cognition to behavior. Heidelberg: Springer; 1985. pp. 11–39. [Google Scholar]
- 20.Ajzen I. The theory of planned behavior. Organ Behav Hum Dec. 1991;50:179–211. [Google Scholar]
- 21.Courneya K, McAuley E. Cognitive mediators of the social influence–exercise adherence relationship: a test of the theory of planned behavior. J Behav Med. 1995;18:499–515. doi: 10.1007/BF01904776. [DOI] [PubMed] [Google Scholar]
- 22.Bandura A. Self-efficacy: the exercise of control. New York: Freeman; 1997. [Google Scholar]
- 23.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;3:143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 24.Bandura A. Social foundations of thought and action. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 25.Baumeister RF, Vohs KD. Understanding self-regulation: an introduction. In: Baumeister RF, Vohs KD, editors. Handbook of self-regulation: research, theory, and applications. New York: Guilford Press; 2004. pp. 1–9. [Google Scholar]
- 26.Dzewaltowski DA, Noble JM, Shaw JM. Physical activity participation: social cognitive theory versus the theories of reasoned action and planned behavior. J Sport Exerc Psychol. 1990;12:388–405. doi: 10.1123/jsep.12.4.388. [DOI] [PubMed] [Google Scholar]
- 27.Lawton M. Albany. 2nd. NY: Plenum Press; 1986. Environment and aging; pp. 10–9. [Google Scholar]
- 28.Stewart D. The new ICF: international classification of functioning, disability and health. Concepts and implementation issues for occupational therapists. OT NOW. 2002 Jul–Aug;:17–21. [Google Scholar]
- 29.McAuley E, Jerome GJ, Elavsky S, Marquez DX, Ramsey SN. Predicting long-term maintenance of physical activity in older adults. Prev Med. 2003;37:110–8. doi: 10.1016/s0091-7435(03)00089-6. [DOI] [PubMed] [Google Scholar]
- 30.Jette AM, Rooks D, Lachman M, Lin TH, Levenson C, Heislein D, et al. Home-based resistance training: predictors of participation and adherence. Gerontologist. 1998;38:412–21. doi: 10.1093/geront/38.4.412. [DOI] [PubMed] [Google Scholar]
- 31.Duncan K, Pozehl B. Effects of an exercise adherence intervention on outcomes in patients with heart failure. Rehabil Nurs. 2003;28:117–22. doi: 10.1002/j.2048-7940.2003.tb01728.x. [DOI] [PubMed] [Google Scholar]
- 32.Harnirattisai T, Johnson RA. Effectiveness of a behavioral change intervention in Thai elders after knee replacement. Nurs Res. 2005;54:97–107. doi: 10.1097/00006199-200503000-00004. [DOI] [PubMed] [Google Scholar]
- 33.Rejeski WJ, Foy CG, Brawley LR, Brubaker PH, Focht BC, Norris JL, et al. Older adults in cardiac rehabilitation: a new strategy for enhancing physical function. Med Sci Sport Exerc. 2002;34:1705–13. doi: 10.1097/00005768-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 34.Bock BC, Marcus BH, Pinto BM, Forsyth LH. Maintenance of physical activity following an individualized motivationally tailored intervention. Ann Behav Med. 2001;23:79–87. doi: 10.1207/S15324796ABM2302_2. [DOI] [PubMed] [Google Scholar]
- 35.Segura OE, Donaghy M. A cognitive-behavioral intervention to increase adherence of adult women exercisers. Adv Physiother. 2004;6:84–92. [Google Scholar]
- 36.McAuley E, Courneya KS, Rudolph DL, Lox CL. Enhancing exercise adherence in middle-aged males and females. Prev Med. 1994;23:489–506. doi: 10.1006/pmed.1994.1068. [DOI] [PubMed] [Google Scholar]
- 37.Hallam JS, Petosa R. The long-term impact of a four-session work-site intervention on selected social cognitive theory variables linked to adult exercise adherence. Health Educ Behav. 2003;31:88–100. doi: 10.1177/1090198103259164. [DOI] [PubMed] [Google Scholar]
- 38.Kirsch I. Self-efficacy and outcome expectancy: a concluding commentary. In: Maddux JE, editor. Self-efficacy, adaptation, and adjustment: theory, research, and application. New York: Plenum Press; 1995. pp. 318–45. [Google Scholar]
- 39.Maddux JE, Gosselin JT. Self-efficacy. In: Leary MR, Tagney JP, editors. Handbook of self and identity. New York: Guilford Press; 2003. pp. 218–38. [Google Scholar]
- 40.Baranowski T, Anderson C, Carmack C. Mediating variable framework in physical activity interventions: how are we doing? how might we do better? Am J Prev Med. 1998;15:266–97. doi: 10.1016/s0749-3797(98)00080-4. [DOI] [PubMed] [Google Scholar]